Abstract
The purpose of the study was to investigate patients with proximal interphalangeal (PIP) joint replacements regarding postoperative function, pain, complications and incidence of reoperations. From 2000 to 2007, 23 patients (11 male, 12 female) with an average age of 47 years (19–72 years) who had symptomatic posttraumatic (15) or idiopathic arthritis (nine) in 24 PIP joints underwent unconstrained PIP joint replacements (formerly AVANTA, now Small Bone InnovationsTM). All 23 patients were instructed in special hand exercises starting the first postoperative day. Thirteen of 23 patients had previous operations. The median history of pain was 12 months (2–120). Fourteen of 24 prostheses needed reoperations (58%): teno-arthrolysis (9×), PIP tenodesis (one in three with swan neck deformity) and explantation (four with infections/loosening). The four explantations resulted in a PIP joint arthrodesis in all cases. Twenty-two patients were available for follow-up at an average of 27 months (4–73 months) postoperatively. The median postoperative pinch grip was 7.6 lbs (4–28 lbs), and the disabilities of the arm, shoulder and hand score was 24 (1–58). The active range of motion of the PIP joint was 33° preoperatively (min 0°, max 75°) and 54° postoperatively (min 0°, max 90°). On the Visual Analogue Pain Scale (VAS, range 0–10), seven patients had mild (VAS 1–3) and four moderate pain (VAS 4–7) in the finger on exercise. Seventy percent were overall satisfied with operation and functional results. The results of surface replacement arthroplasty of the PIP joint are overall satisfying; however, postoperative complications and incidence of reoperations are noticeable and should be mentioned to the patients in the preoperative setting.
Keywords: Proximal interphalangeal joint surface replacement arthroplasty, Arthritis of the PIP joint
Introduction
In symptomatic posttraumatic or idiopathic arthritis of the proximal interphalangeal joints as well as in rheumatoid arthritis of the finger joints, proximal interphalangeal (PIP) joint replacement is an established alternative to joint arthrodesis.
The precondition is an intact or reconstructable central dorsal aponeurosis, intact collateral ligaments and a good bone stock of the finger.
One of the advantages of PIP joint replacement is maintenance of the joint motion with diminished pain; the disadvantages can be loosening, dislocation and pain.
The purpose of the study was to investigate patients with unconstrained prosthetic PIP joint replacements (Small Bone InnovationsTM) regarding postoperative function, pain, satisfaction, complications and incidence of reoperations.
Materials and Methods
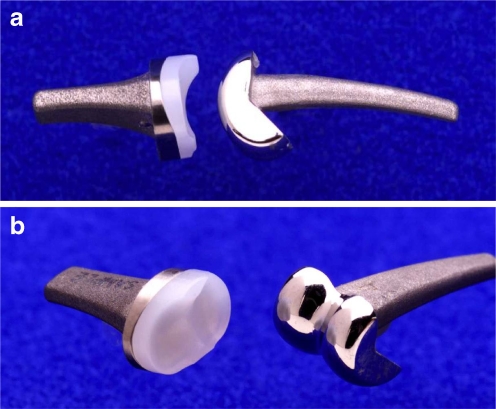
From 2000 to 2007, 23 patients with symptomatic posttraumatic or idiopathic arthritis of the PIP joint underwent 24 PIP joint replacements (formerly AVANTA, now Small Bone InnovationsTM; Fig. 1a–b, Table 1). Eleven male and 12 female patients with an average age of 47 years (19–72 years) were treated with 24 PIP prostheses for posttraumatic (15) or idiopathic arthritis (nine) of the PIP joint. All patients complained of pain, deformity or limited motion (Fig. 2). The median history of pain before PIP joint replacement was 12 months (2–120).
Figure 1.
a SBi PIP joint prosthesis, lateral view, b SBi PIP joint prosthesis, antero-lateral view.
Table 1.
Patient data.
| 23 patients: | 24 SBi PIP prostheses |
| Men/women: | 11/12 |
| Age at operation: | 47 (range 19–72 years) |
| Posttraumatic arthritis: | 15 |
| Idiopathic arthritis: | 9 |
| Mean history of pain: | 12 months (range 2–120 months) |
| Follow-up: | 27 months (range 4–73 months) |
Figure 2.

X-ray showing arthritis of the proximal interphalangeal joint (PIP), lateral view.
In 12 patients, the right hand was operated on, specifically the index finger (one), the middle finger (seven), the ring finger (two) and the little finger (two). In 12 patients, the left hand was operated on, specifically the index finger (one), the middle finger (six), the ring finger (three) and the little finger (two).
At an average of 27 months (4–73 months) postoperatively, 22 of 23 patients were available for follow-up and assessed for active range of motion (difference between active extension and flexion of the PIP joint), disabilities of the arm, shoulder and hand (DASH) score, grip strength (lbs), pain (Visual Analogue Scale, VAS; range 0–10), complications, radiologic outcome and reoperations. All patients were instructed in special hand exercises starting the first postoperative day in our hospital using custom-made splints (Table 2, Fig. 3).
Table 2.
Postoperative PIP therapy guideline.
| Day 1 | Active flexion and extension in the distal interphalangeal joint with PIP in 10° flexion (custom-made thermoplastic splint) |
| Day 2 | Special exercise splint with extension/flexion PIP: 0–10–50° |
| Week 3 | Active flexion PIP: 0–0–60°, no PIP extension limit |
| Week 4 | Active flexion PIP: 0–0–70° |
| Week 6 | Full active motion allowed |
| Week 7 | Only a splint during the night for half a year, e.g. finger-bending splint |
| Week 8 | Start of occupational therapy |
| Weeks 8–12 | Increasing occupational therapy |
| Week 12 | Full power allowed |
Figure 3.
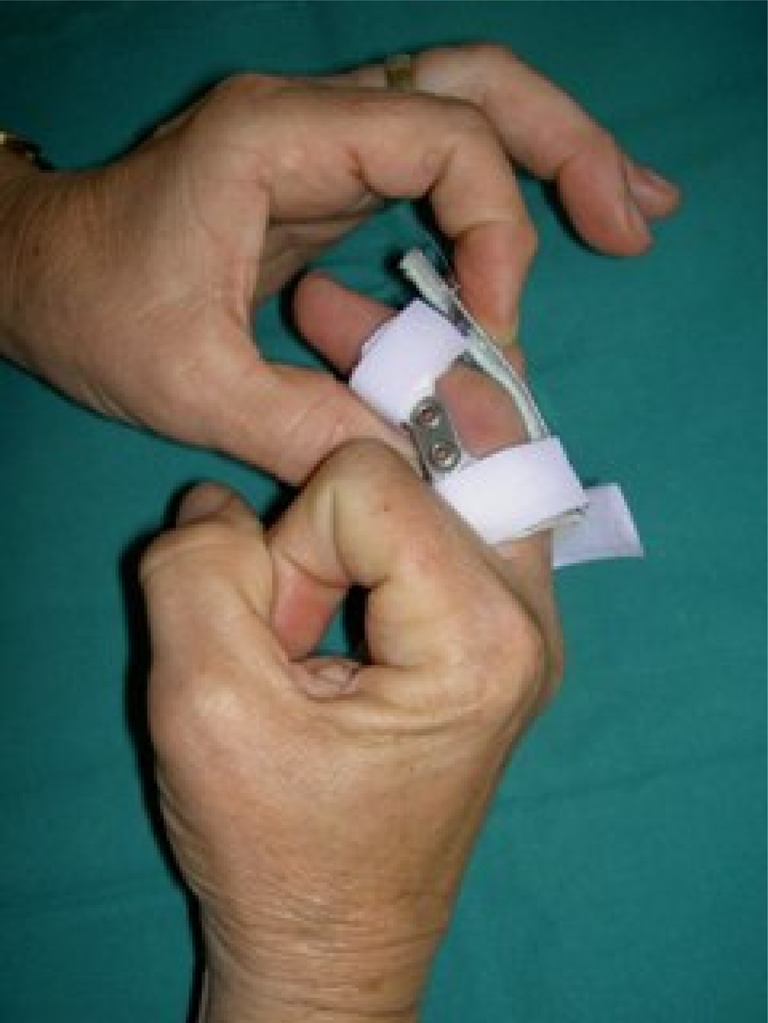
Special custom-made exercise splint for the finger postoperatively.
With regard to pinch grip, VAS, DASH and patient satisfaction preoperative data were naturally not available in all cases of this retrospective study, so that we concentrated our results on the patients’ postoperative parameters in these items (Table 5).
Table 5.
Results postoperatively.
| Follow-up on 23 PIP joints: | Range | Median | Percent |
|---|---|---|---|
| Pinch grip (lbs) | 4–28 | 7.6 | – |
| Pain free at rest (VAS) | – | – | 84% |
| Pain free on exercise (VAS) | – | – | 42% |
| DASH | 1–58 | 24 | – |
| Patient satisfaction | – | – | 70% |
Operation Technique
The operation is performed in brachial plexus anaesthesia. An upper arm tourniquet 300 mmHg is used. Starting with a dorsal approach, the central dorsal aponeurosis is lifted using Chamay’s technique (on the basis of the middle phalanx pedicled tendon flap; Fig. 4). After minimal resection of the articular surface with an oscillating saw, preserving the collateral ligaments, the medullary cavity is opened by a reamer and gradually enlarged with an awl. The ‘trial’ prosthesis is inserted followed by an X-ray control under PIP joint motion, testing if subluxation occurs. After flushing the joint, the final prosthesis is inserted in press-fit technique (Fig. 5), and reconstruction of the collateral ligaments is performed if necessary (Fig. 6). For suturing of the central dorsal aponeurosis, 3-0 resorbable suture material is used. A posterior forearm splint is applicated with PIP joint in 0–10° flexion. Antibiotics are recommended and non-steroidal anti-inflammatory drugs for 5 days postoperatively.
Figure 4.

Chamay’s technique to lift the central dorsal aponeurosis (on the basis of the middle phalanx pedicled tendon flap).
Figure 5.

Insertion of the final prosthesis.
Figure 6.

Reconstruction of the collateral ligaments.
Results
Clinical Examination/Retrospective Analysis
Twenty-two patients with 23 unconstrained PIP joint prostheses were clinically examined. Four fingers were not included in the functional results because the prostheses have been already explanted due to infection (one), loosening (two) and migration (one).
In the statistics concerning social history, previous operations, complications and reoperations, all 23 patients with 24 PIP joint prostheses are considered.
Social History/Demographic Data
Five of the 15 posttraumatic cases were industrial accidents; ten of the 23 patients were craftsmen by profession; seven patients were housewives or retired.
Previous Operations
Thirteen of 23 patients had previous operations; ten of the 15 patients with posttraumatic arthritis had osteosynthesis-like k-wires, screws or external fixators in the past.
Three of nine patients with idiopathic arthritis had the following previous operations: one silicone prosthesis implanted in 1999 in the USA, one extensor tendon suture and one denervation of the finger.
Intraoperative Complications
In four fingers, the prosthesis was cemented (three proximally, one distally) because of intraoperative fissure of the bone while inserting the prosthesis in two cases and because of the changing of PIP prosthesis in one case.
Postoperative Complications and Reoperations
In 14 of 24 prostheses a reoperation was performed (58%): a teno-arthrolysis of the PIP joint in nine cases, a PIP tenodesis with the radial slip of the superficial tendon in one case with a swan neck deformity and an explantation of four prostheses in three patients with clinical signs of infection (1) and radiological signs of prosthetic loosening (2) respectively migration (1). The four explantations resulted in a PIP joint arthrodesis in all cases (Table 3).
Table 3.
Reoperations on 24 PIP joints.
| 14 reoperations on 24 PIP joints (58%): | ||
|---|---|---|
| 9 | Tendon adhesions | ► 9 tenolysis |
| 1 | Infections | |
| 2 | Prosthesis loosening | |
| 1 | Prosthesis migration | ► 4 arthrodesis |
| 3 | Swan neck deformity | ► 1 PIP tenodesis |
With teno-arthrolysis, we mean tenolysis together with arthrolysis of the PIP joint when needed. Most of the time, mainly tenolysis was performed to release the central tendon.
Functional Outcome of 22 Patients with 23 Prostheses at Follow-Up Investigation
The median postoperative pinch grip was 7.6 lbs (4–28) and the DASH score was 24 (1–58).
The active range of motion of the PIP joint was 33° preoperatively (min 0°, max 75°) and 54° postoperatively (min 0°, max 90°), so that we have a functional profit of 21° pre-/postoperatively including the functional results after reoperations.
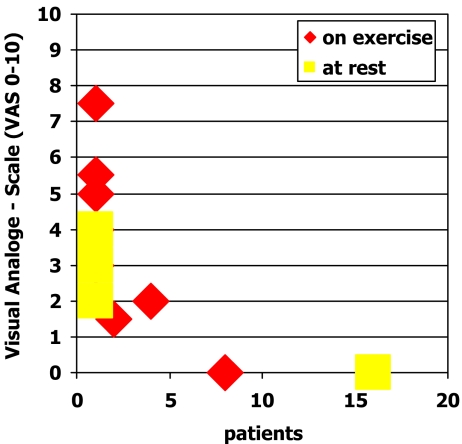
On the Visual Analogue Pain Scale (VAS 0–10), seven of 22 patients had mild pain (VAS 1–3) and four had moderate pain (VAS:4–7) in the finger on exercise. Eighty-four percent of the patients were pain free at rest and 42% pain free on exercise. Seventy percent were overall satisfied with the operation and functional results—they would undergo the same operation again (Tables 4 and 5, Fig. 7).
Table 4.
Active range of motion on 23 PIP joints
| Active range of motion (°)—23 PIP joints | 33° preop. (flexion = 0° min to 75° max) |
| 54° postop. (flexion = 0° min to 90° max) | |
| ► Functional profit of 21° |
Figure 7.
Evaluation of pain on the Visual Analogue Scale (VAS 0–10).
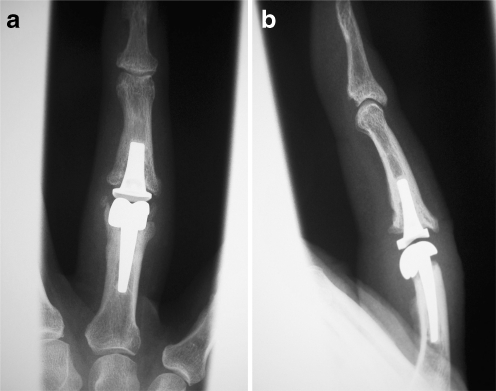
Radiologic Signs at Follow-Up
Nineteen PIP joint prostheses showed no signs of migration or loosening (Fig. 8a–b).
Figure 8.
a X-ray after SBi PIP prosthesis with no signs of migration or loosening, 33 months postoperatively, anterior–posterior view. b No signs of migration or loosening, 33 month postoperatively, lateral view.
Four of 23 PIP joints showed signs of heterotopic bone formation (osteophytes; three of four after posttraumatic, one after idiopathic arthritis). Two of these four prostheses with periarticular ossifications showed additional signs of migration. Three of the four patients with heterotopic bone formation were workers.
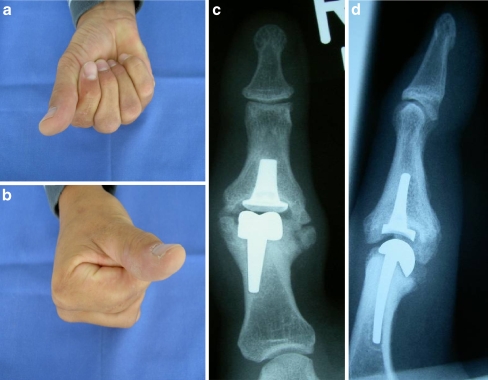
Clinical Outcome of Patients with Radiologic Signs of Migration and Osteophytes
One of the two prostheses showing migration was explanted 28 months postoperatively. Before the explantation, the patient was pain free at rest, had mild pain on exercise (VAS 3), had a pinch grip of 6 lbs, a PIP range of motion of 10° and a DASH score of 20. The other patient showing PIP joint migration and osteophytes was pain free at rest, had only mild pain on exercise (VAS 2), a strong pinch grip of 28 lbs, a range of motion of 20°, a DASH score of 8 and was satisfied with the result. He had no reoperation so far (Fig. 9a–d).
Figure 9.
a–b Clinical picture of a patient’s right hand making a fist (anterior–posterior and lateral view). The SBi PIP joint prosthesis in the index finger shows migration and osteophytes on X-ray. The patient was pain free at rest, had only mild pain on exercise (VAS 2), a strong pinch grip of 28 lbs, a range of motion of 20°, a DASH score of 8 and was satisfied with the result. He had no reoperation so far. c,d X-ray image of right index finger showing osteophytes and slight migration of the PIP prosthesis, posterior–anterior view.
Discussion
The PIP is not a pure hinge joint. It has a natural range of motion of 0–100° with a roll and glide movement around an imaginary screw axis with a variable centre of rotation due to the alternating tensing and relaxing mechanism of the collateral ligament system [23]. Arthritis of the PIP joint was often treated with arthrodesis in former times. Many alternatives to arthrodesis of the PIP joint have been developed such as resection interposition arthroplasty [15], joint denervation [18], synovectomy and free transplantation of vacularised toe joints [20].
To maintain function, joint stability and a painless range of motion, several models of PIP joint prosthesis were developed [4, 5, 23]. Constrained silicone prosthesis with hinge joints, originally developed for patients with rheumatoid arthritis, as well as semiconstrained prosthetic systems used in posttraumatic and idiopathic arthritis often led to joint instability and prosthetic fractures.
The first unconstrained prosthesis was introduced in 1979 by Ronald Linscheid, Mayo Clinic, USA. He developed the SBi (Small Bone Innovation, New York, USA) surface replacement (SR; formerly AVANTA Orthopedics, San Diego, CA, USA). The distal component has an articular surface of high-density polyethylene polymer fixed to a titanium base and stem, and the proximal component is a cast chromium cobalt alloy with a polished articular surface and a shot-blasted stem (Fig. 1a–b).
This unconstrained model mimics the bicondylar anatomic shape and allows an implantation technique that preserves bone and collateral ligaments. The prosthetic design and biomechanics was developed on several cadaver fingers [28].
In review of literature, the range of motion after PIP joint replacement is quite satisfying but best results are achieved in patients with degenerative and posttraumatic arthritis compared to patients with rheumatoid arthritis. The median active range of motion is mentioned between 30° and 47° for the pyrocarbon prosthesis (ASCENSIONTM), 30–44° for silicone prosthesis, 47° for AVANTA SBi, 29–60° for a ceramic prosthesis (Moje®) and 29–37° for vascularised toe joint transfer [2, 24, 25, 27, 30].
In the literature, pain reduction after PIP joint replacement is achieved in all cases, grip strength is equal or better than before operation and patient satisfaction is up to 80% [2, 11, 17].
Common postoperative complications with PIP joint replacement mentioned in the literature are (1) tendon adhesions leading to loss of motion, (2) migration of the prosthesis/heterotopic bone formation/aseptic prosthesis loosening, (3) swan neck deformity and (4) infection of the implant bed [10, 13, 14, 21, 25, 27].
We had to reoperate on 14 of 24 PIP joints (58%) mainly because of extensor tendon adhesions (nine of 14). Since we thought that a different dorsal approach could improve the frequency of tenolysis, we changed from Chamay to a longitudinal incision of the central dorsal aponeurosis. Seven of 14 patients had a dorsal approach after Chamay and two of five after a longitudinal incision of the extensor tendon needed a tenolysis in our series. There was no difference in the two types of dorsal approach.
The operative approach has always been a point of discussion in finger-joint replacement therapy [7]. Some authors prefer the dorsal approach [1, 23] and some the palmar approach [6, 9] stating they would have less rates of tenolysis because the extensor tendon apparatus remains intact. Herren et al. found a significant smaller range of motion in pyrocarbon prosthesis after the dorsal approach (32°) compared to the palmar approach (53°) [9]. A typical disadvantage of the palmar approach is the bowstring of the flexor tendon and the dorsal subluxation of the base of the middle phalanx producing a swan neck deformity because the palmar plate has to be incised [6].
A rate of about 6–62% reoperations and 4–8% tenolysis after PIP joint replacement is mentioned in the literature [2, 9, 11, 17, 24, 26, 27, 29].
Migration of the prosthesis and heterotopic bone formation around the prosthesis are also common problems [8]. We saw heterotopic bone formation (osteophytes) in four of 23 prostheses (three of four after posttraumatic, one after idiopathic arthritis). Two of these four prostheses with heterotopic bone formation showed additional signs of migration. One of these two prostheses had to be explanted; the radiologic changes of the other prostheses was without clinical relevance. Three of the four patients with heterotopic bone formation in our series were workers.
In the literature, migration of pyrocarbon prosthesis is mentioned as 21% [17], 40% [2] and 47% [9] without clinical relevance. Also, radiolucent lines typical for pyrocarbon prosthesis were seen [9, 26].
Loosening rates leading to reoperations are about 4% in SBi [24], 8–14% in pyrocarbon [2, 13, 19] and about 10% in ceramic implants [22].
Heterotopic bone formation is mentioned by few patients [23, 24] up to 13% [17], 16% [27] and 100% after 5 years [8]. The clinical relevance is not definitely ruled out so far.
Since only a few follow-up examinations concerning the SBi prosthesis or similar prosthesis are published, a direct comparison to our results is difficult [3, 12, 16, 24]. In the largest series, 82 PIP joint prostheses were investigated (46 degenerative, 17 posttraumatic, 19 rheumatoid arthritis) [24]. The mean PIP range of motion was 31° pre- and 47° postoperatively at an average follow-up of 64 months. Seventy percent were free of pain; in 11 fingers, 12 (15%) secondary procedures such as tenolysis of the extensor tendon had been necessary and an additional two revisions with implantation of new prosthesis because of dislocation (one patient had rheumatoid arthritis). Three prostheses showed radiologic signs of loosening and only a few patients showed heterotopic bone formation; however, no reoperation was needed. The best results were seen in patients with posttraumatic and degenerative arthritis.
We implanted PIP joint prosthesis in two index fingers and 13 middle fingers. Despite the fact that there is a lot of stress to the index and middle finger, we would even recommend PIP joint replacement in these patients. Precondition for PIP joint replacement is a good compliance of the patient concerning the regular postoperative physical therapy and a profession without heavy hand load. For example, a heavy worker will probably benefit more from a PIP joint arthrodesis compared to a secretary. We could not see any correlation with index or ring finger since explantation was likewise needed in an index, middle, ring and small finger.
In rheumatoid fingers, we think that this PIP implant design is problematic because unconstrained prostheses demand an intact ligamentotaxis, which is a problem in rheumatoid patients. Rheumatoid fingers represent special biomechanics with swan neck or boutonniere deformity; such patients are not included in our study.
We consider the painful posttraumatic or degenerative arthritis of the PIP joint with a moderate functional loss including an intact or reconstructable central dorsal aponeurosis, intact collateral ligaments and a good bone stock of the finger the best indication for surgery.
Our results are comparable with the current literature concerning range of motion and pain relief, but our rate of reoperation leading to four explantations and PIP arthrodesis is noticeable.
This can be explained by the fact that many of our patients (ten of 23) are workers with permanent heavy hand overload and therefore possibly bring more stress on the non-axial forces of the prosthesis leading to heterotopic bone formation on the X-ray in three of four workers in our series. Interestingly, only one of these three workers with osteophytes showed signs of loosening of the PIP joint resulting in an explantation of the prosthesis.
Thus, long-term follow-up investigations are needed to rule out the clinical relevance and biodynamic impact of such heterotopic bone formation.
Moreover, we assume that the patient’s compliance concerning the regular physical therapy decreases during their common daily working activities leading to additional problems like tendon adhesions, gradual loss of motion and reoperations as seen in our series and in the literature. Maybe the development of more sophisticated tools for a different operative approach will also improve the clinical outcome and reduce the postoperative complications in patients with PIP joint replacement.
Conclusion
In symptomatic posttraumatic or idiopathic arthritis of the PIP joints as well as in rheumatoid arthritis of the finger joints, PIP joint replacement is an established alternative to joint arthrodesis, leading to a good range of motion and pain relief in selected cases.
Due to the noticeable complications and reoperation rate, one could consider PIP arthroplasty in young, physically demanding patients to be a relative contraindication.
Long-term follow-up investigations are needed to rule out the clinical relevance and biodynamic impact of heterotopic bone formation around the PIP prosthesis.
We also think that the alternative for a palmar approach should be taken under investigation in the medical industrial companies and more sophisticated tools and instruments for such an approach need to be developed.
Reference
- 1.Bickel KD. The dorsal approach to silicone implant arthroplasty of the proximal interphalangeal joint. J Hand Surg [Br] 2007;32(6):909–913. doi: 10.1016/j.jhsa.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 2.Bravo CJ, Rizzo M, Hormel KB, et al. Pyrolytic carbon proximal interphalangeal joint arthroplasty: results with a minimum two-year follow-up evaluation. J Hand Surg [Br] 2007;32(1):1–11. doi: 10.1016/j.jhsa.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 3.Condamine JL, Fourquet M, Marcucci L, et al. Lárthrose primitive metacarpo-phalangienne et interphalanienne proximale a la main. Indications et resultats de vingt.sept arthroplasies DJOA. Ann Chir Main. 1997;16:66–78. doi: 10.1016/s0753-9053(97)80021-x. [DOI] [PubMed] [Google Scholar]
- 4.Daecke W, Streich N, Schneider S, et al. The role of alloarthroplasty in hand surgery. Alloarthroplasty versus additional procedures. Unfallchirurg. 2005;108:119–126. doi: 10.1007/s00113-004-0867-y. [DOI] [PubMed] [Google Scholar]
- 5.Deb R, Sauerbier M, Rauschmann MA. History of arthroplasty in finger joints. Orthopäde. 2003;32:770–778. doi: 10.1007/s00132-003-0518-y. [DOI] [PubMed] [Google Scholar]
- 6.Duncan SF, Merritt MV, Kakinoki R. The volar approach to proximal interphalangeal joint arthroplasty. Tech Hand Up Extrem Surg. 2009;13(1):47–53. doi: 10.1097/BTH.0b013e31818c0f71. [DOI] [PubMed] [Google Scholar]
- 7.Fahmy NR, Lavender A, Brew C. A conservative approach for proximal interphalangeal joint arthroplasty. J Hand Surg [Br] 2001;26(3):235–237. doi: 10.1054/jhsb.2000.0541. [DOI] [PubMed] [Google Scholar]
- 8.Gülke J, Wachter NJ, Mentzel M. DIGITOS—prosthesis for the proximal interphalangeal joint—long term results. Handchir Mikrochir Plast Chir. 2007;39:257–262. doi: 10.1055/s-2006-924740. [DOI] [PubMed] [Google Scholar]
- 9.Herren DB, Schindele S, Goldhahn J, et al. Problematic bone fixation with pyrocarbon implants in proximal interphalangeal joint replacement: short-term results. J Hand Surg [Br] 2006;31B(6):643–651. doi: 10.1016/j.jhsb.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Iselin F, Conti E. Long-term results of proximal interphalangeal joint resection arthroplasties with a silicone implant. J Hand Surg [Am] 1995;20:595–597. doi: 10.1016/S0363-5023(95)80178-2. [DOI] [PubMed] [Google Scholar]
- 11.Jennings CD, Livingstone DP. Surface replacement arthroplasty of the proximale interphalangeal joint using the PIP–SRA implant: results, complications and revisions. J Hand Surg [Am] 2008;33(9):15651.e1–15651.e11. doi: 10.1016/j.jhsa.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Johnstone BR. Proximale interphalangeal joint surface replacement arthroplasty. Hand Surg. 2001;6(1):1–11. doi: 10.1142/S021881040100045X. [DOI] [PubMed] [Google Scholar]
- 13.Lang E, Schmidt A, Ishida A, et al. A contribution to the alloplastic replacement of the proximale interphalangeal joint. Experience with a new prosthesis. Handchir Mikrochir Plast Chir. 2000;32:44–50. doi: 10.1055/s-2000-19244-1. [DOI] [PubMed] [Google Scholar]
- 14.Lin HH, Wyrick JD, Stern PJ. Proximale interphalangeal joint silicone replacement arthroplasty: clinical results using an anterior approach. J Hand Surg [Am] 1995;20:123–132. doi: 10.1016/S0363-5023(05)80070-X. [DOI] [PubMed] [Google Scholar]
- 15.Lin SY, Cy C, Lin GT, et al. Volar plate interposition arthroplasty for posttraumatic arthritis of the finger joints. J Hand Surg [Am] 2008;33(1):35–39. doi: 10.1016/j.jhsa.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 16.Lundborg G, Branemark PI. Osseointegrated proximal interphalangeal joint prosthesis with a replaceable flexible joint spacer—long term results. Scand J Plast Reconstr Hand Surg. 2000;34:345–353. doi: 10.1080/02844310050159927. [DOI] [PubMed] [Google Scholar]
- 17.Meier R, Schulz M, Krimmer H, et al. Proximal interphalangeal joint replacement with pyrolytic carbon prostheses. Oper Orthop Traumatol. 2007;19:1–15. doi: 10.1007/s00064-007-1192-8. [DOI] [PubMed] [Google Scholar]
- 18.Merk R, Rudigier J. Denervation of finger joints as an alternative procedure to arthrodesis or endoprosthesis. Handchir Mikrochir Plast Chir. 2002;34:182–186. doi: 10.1055/s-2002-33689. [DOI] [PubMed] [Google Scholar]
- 19.Nunley RM, Boyer MI, Goldfarb A. Pyrolytic carbon arthroplasty for posttraumatic arthritis of the proximal interphalangeal joint. J Hand Surg [Am] 2006;31(9):1468–1474. doi: 10.1016/j.jhsa.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 20.Pei GX, Ren GH, Ren YJ. Reconstruction of phalangeal articulations of the hand with vascularised phalangeal articulations of the foot. Injury. 2008;39(Suppl 2):109–115. doi: 10.1016/j.injury.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 21.Pellegrini VD, Burton RI. Osteoarthritis of the proximal interphalangeal joint of the hand: arthroplasty or fusion? J Hand Surg [Am] 1990;15:194–209. doi: 10.1016/0363-5023(90)90096-A. [DOI] [PubMed] [Google Scholar]
- 22.Pettersson K, Wagnsjö P, Hulin E. Replacement of proximal interphalangeal joints with new ceramic arthroplasty: a prospective series of 20 proximal interphalangeal joint replacements. Scand J Plast Reconstr Surg Hand Surg. 2006;40:291–296. doi: 10.1080/02844310600940679. [DOI] [PubMed] [Google Scholar]
- 23.Sauerbier M, Linscheid RL. Proximal interphalangeal joint. In: Weiss A-PC, Hastings H, editors. Surgery of the arthritic hand and wrist, chapter 5. Philadelphia: Lippincott Williams & Wilkins; 2002. pp. 65–74. [Google Scholar]
- 24.Sauerbier M, Cooney WP, Berger RA, et al. Surface replacement arthroplasty of the proximale interphalangeal joint—long term results and surgical technique. Handchir Mikrochir Plast Chir. 2000;32:411–418. doi: 10.1055/s-2000-10913. [DOI] [PubMed] [Google Scholar]
- 25.Squitieri L, Chung KC. A systematic review of outcomes and complications of vascularized toe joint transfer, silicone arthroplasty, and pyrocarbon arthroplasty for posttraumatic joint reconstruction of the finger. Plast Reconstr Surg. 2008;121(5):1697–1707. doi: 10.1097/PRS.0b013e31816aa0b3. [DOI] [PubMed] [Google Scholar]
- 26.Stütz N, Meier R, Krimmer H. Pyrocarbon prosthesis for proximal interphalangeal joint replacement. Experience after one year. Unfallchirurg. 2005;108:365–369. doi: 10.1007/s00113-004-0891-y. [DOI] [PubMed] [Google Scholar]
- 27.Takigawa S, Meletiou S, Sauerbier M, et al. Long-term assessment of Swanson implant arthroplasty in the proximal interphalangeal joint of the hand. J Hand Surg [Am] 2004;29A(5):785–795. doi: 10.1016/j.jhsa.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 28.Uchiyama S, Cooney WP, Linscheid RL, et al. Kinematics of the proximal interphalangeal joint of the finger after surface replacement. J Hand Surg [Am] 2000;25(2):305–312. doi: 10.1067/jhsu.2000.jhsu25a0305. [DOI] [PubMed] [Google Scholar]
- 29.Wesemann A, Flügel M, Marmarvar M. Moje prosthesis for the proximal interphalangeal joint. Handchir Mikrochir Plast Chir. 2008;40(3):189–196. doi: 10.1055/s-2007-965476. [DOI] [PubMed] [Google Scholar]
- 30.Wüstner-Hofmann MC, Hofman AK, Bassetto F, et al. Medium term experience of the Moje ceramic implant for the proximal interphalangeal joint. Riv Ital Chir Plastica Clin Exp PS. 2004;36:119–124. [Google Scholar]