Abstract
Objectives
To examine whether people who expect to live longer engage in healthier behaviors relative to people who expect to live shorter lives.
Methods
Patients (994 Black-Americans, 373 White-Americans) from a publicly-funded clinic estimated their expected survival age and reported their health behaviors (alcohol, tobacco, and drug use, sexual behaviors, physical activity and sleep).
Results
Subjective life expectancy (SLE) was a significant predictor of health behavior for both men and women. Race moderated the SLE-health behavior relation but only for alcohol and tobacco use.
Conclusions
Future research should explore the potential health benefits of shifting SLE from a more limited to an expansive perspective.
Keywords: life expectancy, health behaviors, race, gender, United States
INTRODUCTION
If I knew I was going to live this long, I’d have taken better care of myself.—Mickey Mantle
Awareness of time, consideration of the future, and willingness to make present sacrifices to enhance the future (i.e., delay of gratification)1 are essential to human survival.2 Behaving in ways that increases future survival chances are adaptive providing it does not interfere with imminent survival needs. But, as people age and perceive their time as limited, they are often motivated to engage in goal-directed behaviors that are focused on the present rather than the distant future.3 According to socioemotional selectivity theory (SST),3 subjective life expectancy, not chronological age, is the catalyst for this reprioritization of goals. SST postulates that people with expansive time perspectives prioritize life goals that optimize the future, such as seeking physical fitness information and adopting an exercise regimen, whereas those with a limited time perspective prioritize emotion-laden goals with more immediate results.4
Subjective life expectancy (SLE; i.e., the age to which a person expects to live less their current age) may be an important motivational factor in health behavior. As postulated by SST,3, 4 we assume that the perception of time remaining impacts goal prioritization (i.e., a causal relationship between SLE and health behaviors). Given that nearly half of the leading causes of mortality within the United States can be attributed to modifiable health behaviors,5 SLE is likely to have a direct effect on health-related behavior, health information seeking, and medical care. For example, Ziegelmann, Lippke, and Schwarzer6 examined physical exercise intentions and goal attainment among outpatient orthopedic rehabilitation patients with an expansive versus a limited SLE. Consistent with SST, Ziegelmann et al.6 found participants with an expansive time perspective had higher levels of exercise intentions and goal attainment than those with a limited time perspective 6- and 12-months after discharge. Similarly, a recent review found SLE to be associated with health-related information-seeking and decision-making skills such that when people hold a limited versus an expansive SLE they seek less health information and avoid or defer making health decisions.4 Despite these findings, it is unclear how SLE is associated with actuarial estimates of life expectancy, and whether SLE influences both individual-level (e.g., alcohol use) and partner-dependent (e.g., unprotected sex) health behaviors.
Actuarial life expectancies (i.e., estimates of life expectancy based on age, race, and sex within a given population) are readily disseminated through government agencies. Although subjective and actuarial life expectancies are correlated,7, 8 SLE may have a greater influence on health behavior than knowledge about one’s own actuarial estimate. Unlike actuarial estimates, SLE is related to perceived length of remaining years regardless of age and may be motivated by a need to experience greater emotional well-being.3, 4, 9 Moreover, research examining self-assessed health (SAH) suggests that perceptions of better health are associated with both physical (e.g., activity level) and psychological factors (e.g., happiness, optimism).10 Thus, an individual who overestimates his/her actuarial life expectancy likely holds positive expectations of the future (including future good health), whereas underestimating actuarial life expectancy may indicate an individual’s uncertainty about the future (and possibly future poor health). These estimates may also reflect race- and gender-based socioeconomic differences and health disparities.
Actuarial life expectancy for Black Americans has been consistently lower than White Americans. Current actuarial life expectancy tables indicate that Black men are expected to live 69.5 years compared to 75.7 years for White men. Black women have an actuarial life expectancy of 76.5 years whereas White women are expected to live 80.8 years.11 Not only do Blacks live fewer years than Whites, those years are spent living with a higher proportion of chronic health problems.12 The life expectancy gap between Blacks and Whites persists, in part, because Blacks are disproportionately affected by cardiovascular-related diseases, diabetes, and HIV.13, 14 Limited access to health care, inadequate medical coverage, and other socioeconomic issues may further influence Black Americans’ health outcomes and subsequent life expectancy.15 Likewise, the gap between men and women’s life expectancy remains because men experience higher rates of cardiovascular-related diseases, chronic liver disease, diabetes, cancer, and other health problems compared with women.14
Although Black-Americans have shorter actuarial life expectancies, paradoxically, several studies suggest that both Black-Americans tend to overestimate their life expectancy to a greater extent than do White-Americans. Similarly men have shorter actuarial life expectancies but overestimate their life expectancy compared with women..7, 8, 16, 17 In a sample of Dutch adults, men overestimated their life expectancy by 7 years whereas women overestimated their life expectancy by only 1.7 years.7 After adjusting for socioeconomic status and health indicators (e.g., self-assessed health), Mirowsky8 found that U.S. men overestimated their life expectancy by 3 years whereas Black Americans overestimated their life expectancy by 6 years.
In summary, research on life expectancy suggests that (a) people with expansive time perspectives prioritize goals that optimize the future whereas those with a limited time perspective prioritize goals with immediate outcomes,4 (b) people’s subjective estimates of life expectancy are related to health outcomes and current health behaviors,6, 18 and (c) actuarial life expectancy for Black-Americans is lower than White-Americans, but paradoxically Black-Americans expect to live longer (i.e., more expansive SLE) than White-Americans; similarly, men have lower actuarial life expectancies but expect to live longer than women.8 Therefore, the goals of this study were to: (a) confirm prior research demonstrating that discrepancies between subjective and actuarial life expectances vary by race and gender within a sample of STD clinic patients at risk for a variety of health problems (e.g., substance use, depression) that may increase their risk for HIV,19, 20 (b) investigate the association between life expectancy and health behaviors, and (c) examine race as a moderator of this association. We hypothesized that holding an expansive subjective life expectancy (i.e., expecting to live a longer life; perceiving the future as indeterminate) would be positively associated with health promoting behaviors. In addition, we explored the role of race (Black- and White-Americans) as a potential moderator of the association between life expectancy and health behaviors. Because women and men report differences on a variety of health behaviors (e.g., alcohol use),21 analyses are stratified by sex.
METHODS
Participants and Procedures
Participants were 1,367 Black- or White-American patients (46% female, 73% Black, mean age = 29.46 years) attending a publicly-funded sexually transmitted disease (STD) clinic in Rochester, NY. Data for the current study were collected as part of a randomized controlled trial (RCT) evaluating intervention programs to reduce sexual risk among patients attending a publicly-funded sexually transmitted disease (STD) clinic.22 To be eligible for the RCT, patients needed to report (a) age 18 or older; (b) sexual risk behavior during the past 90 days (e.g., vaginal or anal sex without a condom, having more than one sexual partner); and (c) willingness to be tested for HIV. Patients were excluded if they were (a) infected with HIV (HIV+ patients were referred for more comprehensive services appropriate to their needs); (b) mentally impaired; (c) receiving inpatient substance abuse treatment; and (d) planning to move within the next year. STD clinics provide an opportune venue to recruit patients who are disproportionate at risk for a variety of health threats (e.g., high levels of alcohol and drug use, depression) that may exacerbate their risk for HIV.23–25 Patients who self-identified as either Black (African-American) or White (European-American) race were included in the analyses.
Eligible patients met with a research assistant in a private exam room and were given details about the study; those who were interested provided written consent. Consenting patients completed an audio-computer assisted self-interview on a laptop computer, and were reimbursed $20 for their time (the intervention was not initiated until after the completion of the baseline measures). Detailed procedures for the RCT are available elsewhere.22 The study protocol was approved by Institutional Review Boards of the participating institutions and, to protect participant privacy, a Federal Certificate of Confidentiality was obtained.
Measures
Baseline surveys assessed (a) demographic information (e.g., gender, ethnicity, age), (b) health behaviors (e.g., physical activity, smoking frequency), and (c) additional measures (e.g., life expectancy, self-assessed health) as part of the larger RCT.
Life Expectancy and Discrepancy
Consistent with Mirowsky,8 longevity is defined as survival age (i.e., the age to which a person expects to live), whereas life expectancy refers to the number of years that remain (i.e., survival age minus current age). Therefore, subjective life expectancy was calculated by subtracting the participant’s current age from their maximum age (e.g., 79 if participant responded 70 to 79 years) in response to the subjective longevity question, “How long do you think you will live?” (Responses were given in 10 year intervals beginning with age 20 to 29, age 30 to 39 and so forth.) Actuarial rates corresponding to current age, sex, and race were extracted from the U.S. National Center for Health Statistics.11 Actuarial life expectancy was subtracted from SLE to create a discrepancy score.
Self-Assessed Health
Self-assessed health was assessed by asking participants “In general, how would you describe your health during the past month?” using a 5-point scale, with response options ranging from poor to excellent.
Health Behaviors
Alcohol use
Alcohol use was assessed by asking participants the number of standard drinks (defined as 12 oz of beer, 6 oz. of malt liquor, 4 to 5 oz. of wine, or 1 to 1.5 oz. of hard liquor/shot)26 they consumed on a typical drinking day in the past 3 months. To assess heavy episodic drinking, separate questions asked men (women) how many times, in the past 3 months, they consumed 5 or more (4 or more) drinks on one occasion.27
Tobacco use
Cigarette smoking was assessed using two measures: frequency of cigarette smoking in the past 3 months (never, one time per month, one time per week, several times per week, and every day) and the number of cigarettes smoked per day. To further examine tobacco use, we created we categorized participants who indicating using any amount of tobacco in the past month as current smokers (1) vs. non-smokers (0).
Drug use
Because use of individual drugs (other than marijuana) was relatively infrequent, participants who indicated any drug use (e.g., “once a month” or more frequently) were categorized as using illegal drugs (1 = other drug use, 0 = none).
Sexual behaviors
Participants were asked several questions regarding their sexual behaviors. All questions have been used previously, 19, 28, 29 and followed published guidelines to optimize data quality 30. Composite indices were computed as follows: (a) proportion of unprotected sexual events in past 3 months (number of times vaginal or anal sex occurred without a condom divided by the total number of sexual events), (b) number of sexual partners in the past 3 months, and (c) whether a condom was used during the last sexual event.
Physical activity
Participants indicated the frequency of participating in moderate (e.g., walking briskly, physical labor) or vigorous physical activity (e.g., jogging, aerobics, playing basketball) on a 4-point scale, with response options ranging from never to everyday. Responses from the moderate and vigorous physical activity items were averaged.
Sleep duration
Sleep duration was assessed by asking participants to indicate the average number of hours they sleep per night.
Additional measures
Participants completed additional measures (e.g., sex-related behavioral skills) as part of the larger RCT (not reported in this study). Finally, participants were asked demographic questions (gender, ethnicity, age, income, education, and employment).
Data Management and Analysis
Summary statistics (means, standard deviations, frequencies) describe sociodemographic characteristics and health behaviors for the overall sample, and by race and gender. Subjective-actuarial life expectancy discrepancy and self-assessed health (SAH) were analyzed using a 2 (race: Black, White) × 2 (sex: women, men) analysis of variance (ANOVA). To examine health behaviors more broadly, we created a composite risk index ranging from 0 to 5; participants received 1 point for each of the following behaviors if they reported (a) at least 1 binge drinking episode, (b) being a current smoker, (c) failure to use condoms 100% of the time, (d) engaging in moderate or vigorous physical activity occasionally or less (reported moderate/vigorous physical activity less than a few times per month), and (e) any illegal drug use.
A series of hierarchical multivariate and logistic regression analyses examined the association between life expectancy and health behaviors, including our composite risk index. Because of the well-documented health disparities by race in the U.S., race was included as a moderator of life expectancy and health behaviors. SAH and demographic variables associated with health behaviors (education: 1 = high school or less, 0 = college or higher; employment: 1 = unemployed, 0 = employed; and income: 1 = less than or equal to $15,000 per year, 0 = more than $15,000 per year) were entered at Step 1, the main effects of life expectancy (continuous variable of SLE) and race (1 = Blacks, 0 = Whites) were entered at Step 2, and the life expectancy × race interaction term entered in Step 3. Life expectancy was mean centered to minimize multicollinearity among predictors. Because most of the health behaviors differed by gender, all analyses were conducted separately for women and men. For all variables, the data were examined for skewness and those exhibiting significant positive skew (i.e., alcohol consumption, heavy (episodic) drinking frequency, total number of sexual partners) were transformed using a log10 transformation to approximate normality31.
RESULTS
Characteristics of the Sample
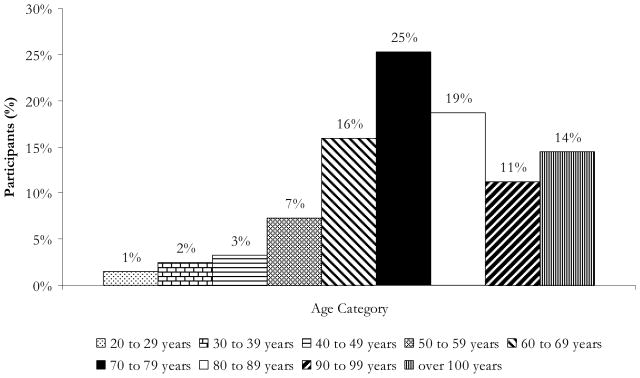
Participants in the RCT were excluded from the analyses only if they did not (a) identify themselves as Black or White (n = 116), or (b) respond to the subjective life expectancy question (n = 9). Table 1 reports the summary characteristics and health behaviors of the final sample (n = 1,367) by race and gender. As shown in Figure 1, most participants thought they would live until their 60s (16%), 70s (25%), or 80s (19%). Participants rated their health in the past month as good (35%), very good (29%), fair (18%), excellent (14%), or poor (4%). On average, participants consumed 2.70 drinks (SD = 2.84) during a typical week, and engaged in heavy episodic drinking 3.66 times (SD = 5.76) in the past 3 months. Participants used tobacco several times per week (M = 4.64, SD = 0.84) in the past 3 months; smokers (31% of the sample) reported smoking an average of 9.51 cigarettes (SD = 6.84) per day. Fifty-two percent reported using drugs other than alcohol or tobacco in the past 3 months. During the past 3 months, 66% of participants’ sexual events were unprotected, participants had 2.91 sexual partners (SD = 2.39), and 26% used a condom during the last sexual event. Participants reported engaging in moderate and/or vigorous physical activity a few times per month (M = 1.64, SD = 0.80) and slept an average of 6.65 hours per night (SD = 2.32). Finally, our composite risk index indicated that participants were of average risk (M = 2.66, SD = 1.13; range = 0–5).
Table 1.
Summary Characteristics by Race and Gendera
| Overall | Blacks | Whites | |||
|---|---|---|---|---|---|
| Women | Men | Women | Men | ||
| N = 1,367 | n = 465 | n = 529 | n = 164 | n = 209 | |
| Age | 29.43 | 28.71 | 30.59 | 27.88 | 29.30 |
| Subjective life expectancy | 52.30 | 55.00 | 51.32 | 51.66 | 49.27 |
| Actuarial life expectancy | 46.82 | 49.46 | 41.84 | 53.85 | 48.02 |
| Subjective longevity | 81.73 | 83.71 | 81.91 | 79.55 | 78.57 |
| Actuarial longevityb | 76.25 | 78.17 | 72.44 | 81.74 | 77.32 |
| Subjective – actuarial discrepancy | 5.48 | 05.54 | 9.48 | −2.19 | 1.25 |
| Self-Assessed Health | 3.30 (1.04) | 3.12 (1.05) | 3.37 (1.08) | 3.21 (0.89) | 3.61 (0.93) |
| Income (% less than $15,000/yr) | 55% | 69% | 55% | 54% | 26% |
| Employment (% unemployed) | 51% | 59% | 56% | 45% | 24% |
| Education (% high school or less) | 61% | 70% | 70% | 46% | 32% |
| Marital status (% unmarried) | 93% | 94% | 94% | 90% | 93% |
| Alcohol, Tobacco, and Other Drug Use | |||||
| Alcohol use, quantity per drinking day | 2.70 (2.84) | 2.02 (2.50) | 2.46 (2.48) | 2.89 (2.71) | 4.69 (3.54) |
| Alcohol use, frequency of heavy drinking | 3.66 (5.76) | 2.00 (3.49) | 2.93 (4.88) | 4.79 (6.78) | 8.30 (8.00) |
| Smoking frequency | 4.64 (0.84) | 4.72 (0.72) | 4.68 (0.77) | 4.71 (0.80) | 4.41 (1.08) |
| Smoking quantity (cigarettes/day; n = 427) | 9.51 (6.84) | 7.75 (5.32) | 8.81 (6.05) | 10.76 (6.53) | 12.34 (9.01) |
| Drug use (% yes) | 52% | 46% | 55% | 53% | 58% |
| Sexual Risk | |||||
| Unprotected sex (M %) | 0.66 (0.33) | 0.69 (0.32) | 0.62 (0.32) | 0.68 (0.36) | 0.69 (0.34) |
| Sexual partners (number) | 2.90 (2.39) | 2.60 (2.39) | 3.29 (2.43) | 2.76 (2.49) | 2.67 (2.03) |
| Condom use at last sex (% yes) | 26% | 22% | 31% | 30% | 19% |
| Exercise and Sleep | |||||
| Physical activity frequency | 1.64 (0.80) | 1.42 (0.81) | 1.76 (0.75) | 1.54 (0.79) | 1.94 (0.79) |
| Sleep (hrs/night) | 6.65 (2.32) | 6.82 (2.77) | 6.55 (2.42) | 6.60 (1.49) | 6.56 (1.20) |
| Composite Risk Index (range = 0 to 5) | 2.66 (1.13) | 2.58 (1.14) | 2.56 (1.15) | 2.88 (1.08) | 2.92 (1.05) |
Numbers represent means (and standard deviations) unless otherwise indicated.
Extracted from the U.S. National Center for Health Statistics (Table 103; http://www.census.gov/compendia/statab/tables/09s0103.pdf)
Figure 1.
Proportion of participants’ expected survival age by age category.
Black and White participants did not differ with respect to age or marital status (all Ps >.05) but did vary according to education level, employment status, and income. Compared to Whites, Blacks were more likely to report (a) having completed high school or less (70% vs. 38%), (b) being unemployed (58% vs. 34%), and (c) earning less than $15,000 per year (61% vs. 38%) (all Ps <.05). Therefore, we controlled for education, employment, and income in all of the regression analyses.
Subjective and Actuarial Life Expectancy
Subjective-actuarial discrepancy estimates are provided in Table 1. As expected, the subjective and actuarial life expectancy scores were significantly correlated (r = .40, P <.001). A 2 (race: Black, White) × 2 (sex: women, men) analysis of variance (ANOVA) revealed a main effect (but no interaction) for race and sex such that Blacks (M = 7.64 years, SD = 19.19) overestimated their life expectancies (i.e., subjective minus actuarial discrepancy) compared with Whites (M = −0.26 years, SD = 15.65), and men (M = 7.14 years, SD = 19.06) overestimated their life expectancies compared with women (M = 3.53, SD = 17.91), Fs (1, 1363) = 51.51 and 10.98, Ps < .001 and <.01, respectively. After controlling for education, employment, income, and SAH in regression analyses, we find men overestimated their life expectancies by approximately 3 years (B = 3.45, SE = 0.95, β = .10, P <.001) and Blacks overestimated their life expectancies by approximately 8 years (B = 8.31, SE = 1.10, β = .21, P <.001).
Self-Assessed Health
Self-assessed health (SAH) was examined using a 2 (race: Black, White) × 2 (sex: women, men) analysis of variance (ANOVA). A main effect (but no interaction) for race and sex was found such that Whites (M = 3.43, SD = 0.94) and men (M = 3.44, SD = 1.05) rated their current health higher than Blacks (M = 3.26, SD = 1.07) and women (M = 3.14, SD = 1.01), Fs (1, 1363) = 6.75 and 26.63, Ps <.01 and <.001, respectively. As expected, SAH was significantly correlated with SLE (r = .19, P <.001) and thus we controlled for SAH in regression analyses.
Health Behaviors
Tables 2 and 3 summarize the results of the regression analyses examining the association between health behaviors and SLE and race. To ease interpretation of results and reduce multicolliniearity, continuous variables (SAH, SLE) were mean centered and interaction terms were created by multiplying mean centered SLE by race.32
Table 2.
Hierarchical Multiple Regression Analyses Examining the Effects of Subjective Life Expectancy (SLE) and Race on Health Behaviorsa
| Step 1 | Step 2 | Step 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Subjective LE | Race | SLE × Race | |||||||
| Variable | R2 | R2 | B (SE) | β | B (SE) | β | R2 | B (SE) | B |
| Women (n = 629) | |||||||||
| Alcohol use, quantity per drinking day | .01 | .04 | −.30 (.11) | −.11*** | −.79 (.24) | −.13*** | .05 | −.70 (.26) | −.24*** |
| Alcohol use, frequency of heavy episodic drinking | .02 | .08 | −.34 (.19) | −.07†** | −2.60 (.43) | −.24*** | .09 | −.52 (.47) | −.10*** |
| Smoking frequency | .04 | .09 | −.16 (.05) | −.22*** | −.02 (.12) | −.01*** | .11 | .24 (.12) | .29*** |
| Smoking quantity (cigarettes/day) | .04 | .13 | −1.20 (.41) | −.21*** | −2.94 (.96) | −.24*** | .14 | 1.12 (.93) | .17*** |
| Unprotected sex (proportion) | .01 | .01 | −.02 (.01) | −.06*** | .01 (.03) | .01*** | .01 | .02 (.03) | .05*** |
| Sexual partners (number) | .04 | .05 | −.19 (.10) | −.08*** | −.31 (.22) | −.06*** | .05 | −.17 (.24) | −.06*** |
| Physical activity frequency | .05 | .05 | −.02 (.03) | −.03*** | −.07 (.07) | −.04*** | .05 | .05 (.08) | .06*** |
| Sleep quantity (hrs/night) | .04 | .04 | .01 (.10) | .00*** | .10 (.23) | .02*** | .04 | .26 (.25) | .09*** |
| Composite Risk Index | .06 | .08 | −.09 (.05) | −.08†** | −.34 (.10) | −.13*** | .08 | −.09 (.11) | −.07*** |
| Men (n = 738) | |||||||||
| Alcohol use, quantity per drinking day | .03 | .12 | .01 (.11) | .01*** | −2.23 (.25) | −.34*** | .13 | −.74 (.25) | −.22*** |
| Alcohol use, frequency of heavy episodic drinking | .04 | .15 | .10 (.23) | .02*** | −5.17 (.53) | −.36*** | .16 | −.56 (.52) | −.08*** |
| Smoking frequency | .08 | .10 | −.14 (.06) | −.15*** | .05 (.13) | .03*** | .13 | .34 (.12) | .32*** |
| Smoking quantity (cigarettes/day) | .03 | .14 | −1.06 (.46) | −.14*** | −5.02 (1.07) | −.33*** | .15 | 1.47 (.99) | .17*** |
| Unprotected sex (proportion) | .01 | .02 | .01 (.01) | .04*** | −.09 (.03) | −.12*** | .02 | .02 (.03) | .05*** |
| Sexual partners (number) | .01 | .02 | −.10 (.09) | −.04*** | .54 (.21) | .10*** | .02 | .02 (.21) | .11*** |
| Physical activity frequency | .08 | .09 | .06 (.03) | .08*** | −.12 (.07) | −.07†** | .09 | .02 (.06) | .03*** |
| Sleep quantity (hrs/night) | .02 | .03 | .22 (.08) | .10*** | −.04 (.19) | −.01*** | .03 | −.01 (.19) | −.01*** |
| Composite Risk Index | .04 | .07 | .01 (.04) | .01*** | −.49 (.10) | −.19*** | .08 | −.23 (.10) | −.18*** |
P <.10.
P <.05.
P <.01.
P<.001.
Self-assessed health, education, employment, and income were entered in Step 1 as control variables, the main effects of SLE and race (1 = Black, 0 = White) were entered in Step 2, and the SLE × race interaction was entered in Step 3.
Table 3.
Logistic Regression Analyses Examining the Effects of Race and SLE on Health Behaviorsa
| Step 1 | Step 2 | Subjective LE | Race | Step 3 | Subjective LE × Race | ||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | R2 | R2 | OR | 95% CI | OR | 95% CI | R2 | OR | 95% CI |
| Women (n = 629) | |||||||||
| Current smokers | .03 | .05 | 0.85 | 0.71, 1.02 | 1.79 | 1.21, 2.67 | .05 | 1.07 | 0.70, 1.64 |
| Drug use | .06 | .08 | 0.85 | 0.72, 1.01 | 1.51 | 1.03, 2.21 | .09 | 1.52 | 0.98, 2.36 |
| Condom use at last sex | .03 | .07 | 1.48 | 1.20, 1.81 | 1.45 | 0.95, 2.21 | .07 | 0.91 | 0.57, 1.48 |
| Men (n = 738) | |||||||||
| Current smokers | .02 | .06 | 2.38 | 1.62, 3.48 | 1.05 | 0.90, 1.24 | .06 | .89 | 0.62, 1.27 |
| Drug use | .02 | .03 | 1.23 | 0.96, 1.30 | 1.29 | 0.90, 1.85 | .03 | 0.76 | 0.53, 1.09 |
| Condom use at last sex | .01 | .03 | 1.03 | 0.87, 1.23 | 0.47 | 0.30, 0.73 | .03 | 1.06 | 0.68, 1.64 |
Self-assessed health, education, employment, and income were entered in Step 1 as control variables, the main effects of SLE and race (1 = Black, 0 = White) were entered in Step 2, and the SLE × race interaction was entered in Step 3. Pseudo-R2 (i.e., Nagelkerke R2) is reported in logistic regression.
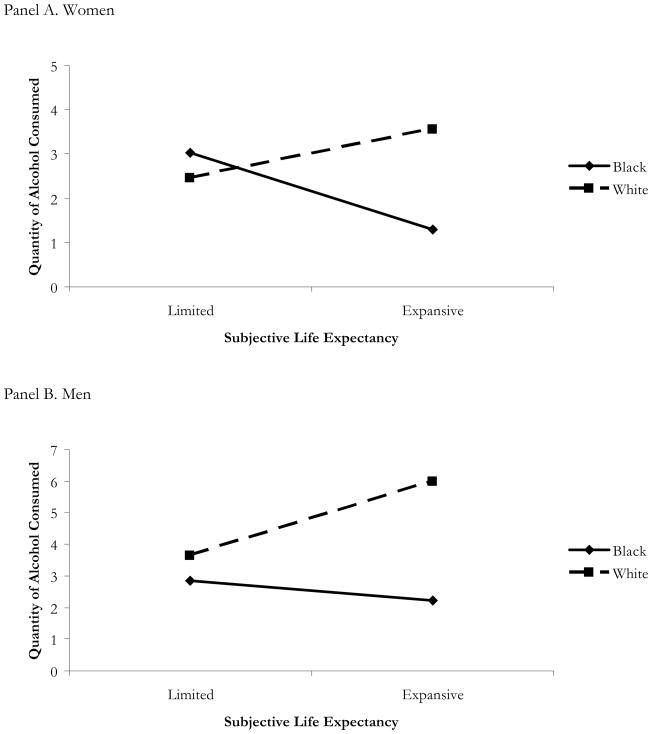
Alcohol use
SLE was related to alcohol use among women, but not men; women with an expansive SLE consumed less alcohol per day or had fewer episodes of heavy drinking. For both women and men, race was related to alcohol use such that Blacks consumed less alcohol and had fewer episodes of heavy drinking than Whites. An interaction between SLE and race was found for alcohol consumption; that is, Black women and men consumed less alcohol whereas White women and men consumed more alcohol (β = −0.24, P <.01 for women and β = −0.22, P <.01 for men) if they held an expansive, rather than limited, SLE (see Figure 2).
Figure 2.
Interaction of subjective life expectancy and race predicting quantity of alcohol consumption in women (panel A) and men (panel B). Note. Subjective life expectancy is centered; limited and expansive subjective life expectancy refers to values −2 and +2 SD from the mean, respectively.
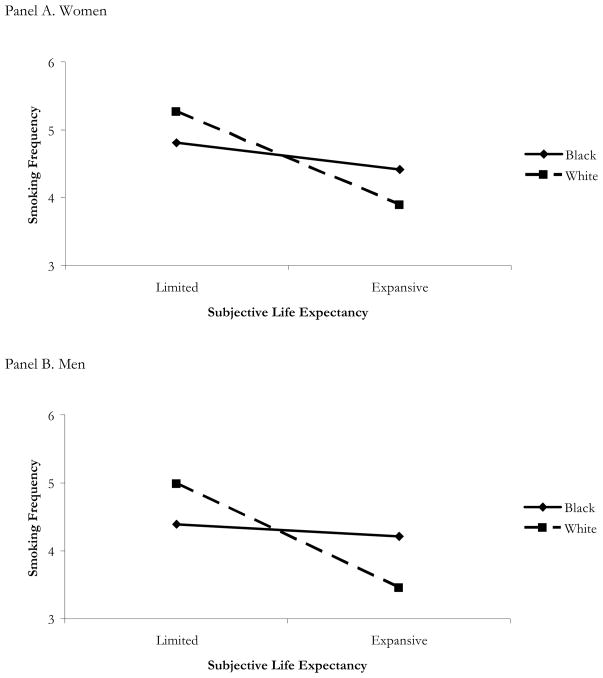
Tobacco use
For both women and men, SLE was associated with lower tobacco use; that is, STD clinic patients with an expansive SLE reported lower frequency and quantity of tobacco use and were less likely to smoke. Race was associated with smoking quantity, but not smoking frequency, such that Blacks smoked fewer cigarettes per day than did Whites. Among women, the odds of being a current smoker increased if the woman was Black (Table 3). The interaction between SLE and race was significant for smoking frequency such that an expansive SLE was associated with a higher frequency of cigarette smoking for Blacks (β = 0.29, P <.05 for women and β = 0.32, P <.01 for men) and a lower frequency for Whites (Figure 3).
Figure 3.
Interaction of subjective life expectancy and race predicting smoking frequency in women (panel A) and men (panel B). Note. Subjective life expectancy is centered; limited and expansive subjective life expectancy refers to values −2 and +2 SD from the mean, respectively.
Drug use
Race was related to drug use among women (see Table 3), but not men; the odds of drug use increased if she was a Black-American. No significant SLE × race interactions were found.
Sexual behaviors
Among women, SLE was negatively related to the number of sexual partners in the past 3 months (Table 2) and positively related to condom use at last sexual event (Table 3), thus, women with an expansive SLE had fewer sexual partners and were more likely to report using a condom during their last sexual event. Race was related to sexual behaviors for men (but not women) such that being Black was associated with a lower proportion of unprotected sex, more sexual partners, and not using a condom during the last sexual event compared to Whites. No interactions were found between SLE and race for either women or men.
Physical activity
SLE was not associated with physical activity for women but was positively associated among men such that men with an expansive SLE reported engaging in more physical activity. Race was associated with physical activity in men only; Black men reported less physical activity compared to White men. No significant interactions were found.
Sleep
Among men only, SLE was positively associated with sleeping such that men with an expansive SLE reported sleeping more hours per night compare to men with a limited SLE. No significant main effects of race or interactions were found for women or men.
Composite risk index
Among women only, SLE was negatively associated with composite risk such that women with an expansive SLE reported engaging in fewer risky health behaviors. For both men and women, race was negatively related to composite risk; Black women and men engaged in fewer risky health behaviors compared with White women and men. A significant interaction between SLE and race was found for men such that Black men engaged in fewer risky health behaviors if they held an expansive vs. a limited SLE (β = −.23, P =.02).
DISCUSSION
In this study, we extended prior research on life expectancies by (a) examining the association between life expectancy and multiple health behaviors, (b) investigating this association among an at-risk group of patients at a public health clinic, and (c) exploring race as a moderator of the life expectancy-health association. Consistent with prior research,8 Black-Americans and men overestimated their subjective life expectancies (by approximately 8 and 3 years, respectively), after controlling for education, employment, income, and self-assessed health. Our findings show that SLE was a strong predictor of health behaviors among both women and men. Among women, SLE predicted less alcohol and tobacco use, current smoking status, fewer sexual partners, the use of a condom at last sex occasion, and fewer risky health behaviors. For men, SLE predicted less tobacco use, physical activity, and more sleep and more risky health behaviors.
After controlling for socioeconomic status (education, employment, and income) and self-assessed health, race moderated the association between life expectancy and health but only for quantity of alcohol consumed and smoking frequency. Holding an expansive SLE and being Black predicted reduced alcohol consumption but increased smoking frequency among women and men. Among men, but not women, race moderated the association between SLE and composite risk index such that holding an expansive SLE and being Black predicted fewer risky health behaviors.
Several studies suggest that optimism, even if unrealistic, is generally adaptive.3, 33, 34 In the current study, our results suggest that holding an expansive SLE is related to fewer health risk behaviors and more health promotion behaviors. Yet, results of our research suggest disadvantages of optimism; optimism among Black-Americans predicted more alcohol, tobacco, and drug use. These findings corroborate prior research on tobacco use showing that smokers who were unrealistically expansive about their life expectancy relative to non-smokers had fewer intentions to quit smoking.35 It is unclear, however, why optimism among Blacks, rather than Whites, might be associated with health-damaging behaviors. Perhaps expansive Blacks, who are more frequently lower in socioeconomic status than Whites,36 use substances to maintain optimism and cope with poverty, discrimination, and other social disadvantage.37 Alternatively, with respect to tobacco use, aggressive marketing practices of tobacco companies in low income neighborhoods38–40 may further promote the use of tobacco as normative among Blacks. Social and structural factors such as the greater availability of health-damaging substances in low-income environments41 coupled with limited housing may overwhelm individual-level social-cognitive predictors of health behaviors.42
Nonetheless, our results indicate that further examination of how race impacts the association between SLE and alcohol and tobacco is needed. Continued research examining the motivational mechanisms involved in SLE will improve our understanding of SLE, how SLE functions, and potential benefits of SLE. Future research should examine the potential benefits of using interventions aimed at shifting subjective life expectancies from a more limited to an expansive perspective (i.e., shifting to a perspective that prioritize life goals to optimize the future).4 Initial research shows the benefits of using a time perspective intervention to enhance long-term thinking about physical activity among a mixed-race sample of young adults.43 Consistent with SST,3 these interventions might focus on maximizing positively valenced emotions thought to be important among those with present-oriented goals. For example, Löchenhoff and Carstensen4 suggest that presenting health information in a positive framework, rather than a negative or neutral one, might enable participants to opt for health-promoting behaviors (e.g., message framing).44
Limitations
The limitations of this study should be considered in interpreting these findings. First, as with any study conducted at a single site or with any one sub-population, our sample of predominately Black-American STD clinic patients may not be representative. Thus, our findings should be considered preliminary. However, examining the association between life expectancy and health behaviors among at-risk clinic patients is valuable given the health threats and disparities evident in low-income urban communities. Second, the cross-sectional nature of the data prevents casual conclusions (i.e., perceptions of life expectancy may precede or follow health behaviors). Third, data were gathered from self-reports of health behaviors; self-report is an imperfect indicator of actual behavior. Fourth, our measure of life expectancy included a range of ages rather than a specific age estimate. This approach reduced the full range of the data but was more feasible for respondents. To minimize the impact of the range of responses, we selected the maximum age a person expected to live (rather than a lower value within the specified range). Despite our approximate measure of SLE, our findings were consistent with research obtaining precise age estimates of life expectancy.7, 8 With more precise age estimates, it is likely the observed effects would be stronger but future research will need to confirm this hypothesis. Finally, we did not assess other factors (e.g., family medical history, longevity of other family members) that may account for the association between life expectancy and health behaviors.
Conclusions
Individuals’ perceptions of their life expectancies appear to influence their health behaviors. The association between life expectancy and health is moderated by race for alcohol and tobacco use; that is, Blacks with an expansive time perspective use more alcohol and tobacco than Whites. Health promotion programs should include discussions of the influences of time perspectives on health behaviors as well as the association between health behaviors and preventable morbidity and mortality.5
Acknowledgments
We thank the participants, clinic nurses and staff, and our research team.
Funding: This research was funded by a grant from the National Institute of Mental Health (R01-MH068171) to Michael P. Carey.
References
- 1.Klineberg SL. Future time perspective and the preference for delayed reward. J Pers Soc Psychol. 1968;8:253–257. doi: 10.1037/h0025581. [DOI] [PubMed] [Google Scholar]
- 2.Suddendorf T, Busby J. Making decisions with the future in mind: Developmental and comparative identification of mental time travel. Learn Motiv. 2005;36:110–125. [Google Scholar]
- 3.Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously. A theory of socioemotional selectivity. Am Psychol. 1999;54:165–181. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- 4.Löchenhoff CE, Carstensen LL. Socioemotional selectivity theory, aging, and health: the increasingly delicate balance between regulating emotions and making tough choices. J Pers. 2004;72:1395–1424. doi: 10.1111/j.1467-6494.2004.00301.x. [DOI] [PubMed] [Google Scholar]
- 5.Mokdad AH, Marks JS, Stroup DF, et al. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 6.Ziegelmann JP, Lippke S, Schwarzer R. Subjective Residual Life Expectancy in Health Self-Regulation. J Gerontol B Psychol Sci Soc Sci. 2006:P195–p201. doi: 10.1093/geronb/61.4.p195. [DOI] [PubMed] [Google Scholar]
- 7.Brouwer WBF, van Exel NJA. Expectations regarding length and health related quality of life: Some empirical findings. Soc Sci Med. 2005;61:1083–1094. doi: 10.1016/j.socscimed.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 8.Mirowsky J. Subjective life expectancy in the US: correspondence to actuarial estimates by age, sex and race. Soc Sci Med. 1999;49:967–979. doi: 10.1016/s0277-9536(99)00193-8. [DOI] [PubMed] [Google Scholar]
- 9.Mirowsky J, Ross CE. Socioeconomic status and subjective life expectancy. Soc Psychol Q. 2000;63:133–151. [Google Scholar]
- 10.Benyamini Y, Leventhal EA, Leventhal H. Elderly people’s ratings of the importance of health-related factors to their self-assessments of health. Soc Sci Med. 2003;56:1661–1667. doi: 10.1016/s0277-9536(02)00175-2. [DOI] [PubMed] [Google Scholar]
- 11.Bureau USC. [Accessed June 9, 2009.];Statistical Abstract of the United States. 2009 Available: http://www.census.gov/compendia/statab/overview.html.
- 12.Hayward MD, Heron M. Racial inequality in active life among adult Americans. Demography. 1999;36:77–91. [PubMed] [Google Scholar]
- 13.Harper S, Lynch J, Burris S, et al. Trends in the black-white life expectancy gap in the United States, 1983–2003. JAMA. 2007;297:1224–1232. doi: 10.1001/jama.297.11.1224. [DOI] [PubMed] [Google Scholar]
- 14.Kung HC, Hoyert DL, Xu J, et al. Deaths: final data for 2005. Natl Vital Stat Rep. 2008;56:1–120. [PubMed] [Google Scholar]
- 15.Council NMA. [Accessed June 9, 2009.];African Americans, health disparities and HIV/AIDS: Recommendations for confronting the epidemic in Black America (on-line) Available: http://www.nmac.org/index/grpp-publications.
- 16.Hurd MD, McGarry K. Evaluation of the subjective probabilities of survival in the health and retirement study. J Hum Resour. 1995;30:S268–S292. [Google Scholar]
- 17.Joubert CE. Happiness, time consciousness, and subjective life expectancy. Percept Mot Skills. 1992;74:649–650. doi: 10.2466/pms.1992.74.2.649. [DOI] [PubMed] [Google Scholar]
- 18.Ross CE, Mirowsky J. Family relationships, social support and subjective life expectancy. J Health Soc Behav. 2002;43:469–489. [PubMed] [Google Scholar]
- 19.Williams MJ, Grimley DM. Depressive symptoms and interpersonal victimization among African American women attending an urban STD clinic. Womens Health Issues. 2008;18:375–380. doi: 10.1016/j.whi.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 20.Zenilman JM, Hook EW, 3rd, Shepherd M, et al. Alcohol and other substance use in STD clinic patients: relationships with STDs and prevalent HIV infection. Sex Transm Dis. 1994;21:220–225. doi: 10.1097/00007435-199407000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Wilsnack RW, Vogeltanz ND, Wilsnack SC, et al. Gender differences in alcohol consumption and adverse drinking consequences: cross-cultural patterns. Addiction. 2000;95:251–265. doi: 10.1046/j.1360-0443.2000.95225112.x. [DOI] [PubMed] [Google Scholar]
- 22.Carey MP, Vanable PA, Senn TE, et al. Evaluating a two-step approach to sexual risk reduction in a publicly-funded STI clinic: rationale, design, and baseline data from the Health Improvement Project-Rochester (HIP-R) Contemp Clin Trials. 2008;29:569–586. doi: 10.1016/j.cct.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Appel PW, Piculell R, Jansky HK, et al. Assessing alcohol and other drug problems (AOD) among sexually transmitted disease (STD) clinic patients with a modified CAGE-A: implications for AOD intervention services and STD prevention. Am J Drug Alcohol Abuse. 2006;32:225–236. doi: 10.1080/00952990500479555. [DOI] [PubMed] [Google Scholar]
- 24.Cook RL, Comer DM, Wiesenfeld HC, et al. Alcohol and drug use and related disorders: An underrecognized health issue among adolescents and young adults attending sexually transmitted disease clinics. Sex Transm Dis. 2006;33:565–570. doi: 10.1097/01.olq.0000206422.40319.54. [DOI] [PubMed] [Google Scholar]
- 25.MacKenzie TD, Steiner JF, Davidson AJ, et al. Tobacco use and other risk behaviors among adolescents in an STD clinic. Prev Med. 1998;27:792–797. doi: 10.1006/pmed.1998.0359. [DOI] [PubMed] [Google Scholar]
- 26.Dufour MC. What is moderate drinking? Defining “drinks” and drinking levels. Alcohol Res Health. 1999;23:5–14. [PMC free article] [PubMed] [Google Scholar]
- 27.Wechsler H, Dowdall GW, Davenport A, et al. A gender-specific measure of binge drinking among college students. Am J Public Health. 1995;85:982–985. doi: 10.2105/ajph.85.7.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carey MP, Braaten LS, Maisto SA, et al. Using information, motivational enhancement, and skills training to reduce the risk of HIV infection for low-income urban women: a second randomized clinical trial. Health Psychol. 2000;19:3–11. doi: 10.1037//0278-6133.19.1.3. [DOI] [PubMed] [Google Scholar]
- 29.Jaworski BC, Carey MP. Effects of a brief, theory-based STD-prevention program for female college students. J Adolesc Health. 2001;29:417–425. doi: 10.1016/s1054-139x(01)00271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weinhardt LS, Forsyth AD, Carey MP, et al. Reliability and validity of self-report measures of HIV-related sexual behavior: progress since 1990 and recommendations for research and practice. Arch Sex Behav. 1998;27:155–180. doi: 10.1023/a:1018682530519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tabachnick BG, Fidell LS. Using multivariate statistics. 5. Boston: Allyn & Bacon; 2007. [Google Scholar]
- 32.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA US: Sage Publications, Inc; 1991. [Google Scholar]
- 33.Taylor SE, Kemeny ME, Aspinwall LG, et al. Optimism, coping, psychological distress, and high-risk sexual behavior among men at risk for acquired immunodeficiency syndrome (AIDS) J Pers Soc Psychol. 1992;63:460–473. doi: 10.1037//0022-3514.63.3.460. [DOI] [PubMed] [Google Scholar]
- 34.Taylor SE, Brown JD. Illusion and well-being: a social psychological perspective on mental health. Psychol Bull. 1988;103:193–210. [PubMed] [Google Scholar]
- 35.Dillard AJ, McCaul KD, Klein WM. Unrealistic optimism in smokers: implications for smoking myth endorsement and self-protective motivation. J Health Commun. 2006;11:93–102. doi: 10.1080/10810730600637343. [DOI] [PubMed] [Google Scholar]
- 36.Isaacs JB, Sawhill IV, Haskins R. [Accessed June 8, 2009.];Getting ahead or losing ground: Economic mobility in America (on-line) Available: http://www.economicmobility.org/assets/pdfs/PEW_EMP_GETTING_AHEAD_FULL.pdf.
- 37.Blake WM, Darling CA. The dilemmas of the African American male. J Black Stud. 1994;24:402–415. [Google Scholar]
- 38.Lee D, Turner N, Burns J, et al. Tobacco use and low-income African Americans: policy implications. Addict Behav. 2007;32:332–341. doi: 10.1016/j.addbeh.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 39.Lee D, Cutler BD, Burns J. The marketing and demarketing of tobacco products to low-income African-Americans. Health Mark Q. 2004;22:51–68. doi: 10.1300/j026v22n02_04. [DOI] [PubMed] [Google Scholar]
- 40.Yerger VB, Przewonznik J, Malone RE. Racialized geography, corporate activity, and health disparities: Tobacco industry targeting of inner cities. J Health Care Poor Underserved. 2007;18:10–38. doi: 10.1353/hpu.2007.0120. [DOI] [PubMed] [Google Scholar]
- 41.Farley T, Cohen DA. Prescription for a health nation: A new approach to improving our lives by fixing our everyday world. Boston: Beacon Press; 2005. [Google Scholar]
- 42.Aral SO, Adimora AA, Fenton KA. Understanding and responding to disparities in HIV and other sexually transmitted infections in African Americans. Lancet. 2008;372:337–340. doi: 10.1016/S0140-6736(08)61118-6. [DOI] [PubMed] [Google Scholar]
- 43.Hall PA, Fong GT. The effects of a brief time perspective intervention for increasing physical activity among young adults. Psychol Health. 2003;18:685–706. [Google Scholar]
- 44.Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: The role of message framing. Psychol Bull. 1997;121:3–19. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]