Abstract
Objectives. We examined whether individual and neighborhood characteristics associated with smoking were also predictive of exposure to smoking prevention education in schools, to determine whether education programs were targeted appropriately to reach neighborhoods with the greatest need.
Methods. We merged data from 2 sources—the 2005 Virginia Youth Tobacco Survey (n = 2208) and the Census 2000 School District Demographics Project—and used binary multilevel models with random effects to determine whether the same demographic characteristics and neighborhood characteristics predicted both adolescent smoking and exposure to prevention programs.
Results. We found that although light, medium, and heavy smoking rates were higher in neighborhoods of lower socioeconomic status (relative risk ratio = 1.49, 1.36, and 1.65, respectively), prevention programs were less available in those areas (odds ratio = 0.82).
Conclusions. Our study indicates that school prevention programs are not being effectively targeted and that more effective ways to reach high-risk and disadvantaged neighborhoods are needed.
Tobacco use is the most common cause of preventable death in the United States, and most tobacco users initiate use before they are aged 18 years.1–3 Reducing adolescent smoking initiation is therefore an important health education goal. In 2005, 23% of high school students reported current smoking; the US Department of Health and Human Services has set a national health objective of reducing that prevalence to less than 16% by 2010.2,4 To accomplish this goal and to reduce health inequities, both individual and environmental indicators must be identified to target education interventions efficiently.
Several national studies of adolescent tobacco use have noted differences in school and neighborhood rates of tobacco use.5,6 Neighborhood factors of interest for smoking and health behaviors have often included social disorganization, poverty, and race. For example, neighborhood disorganization indicators (e.g., percentage of people seeking work or in households without access to a car) appear to have an independent effect on individual smoking status even after a large range of individual characteristics are taken into account.6 Other studies have found that neighborhood socioeconomic factors and ethnicity affect smoking behaviors.5,7 However, inconsistent and sometimes weak associations between neighborhood factors and adolescent smoking have been observed, perhaps as a result of the different ways in which neighborhood-level variables were operationalized.8
Because smoking prevalence can vary dramatically between neighborhoods and schools, it is critical for us to understand neighborhood-level characteristics for areas with extremely high or low smoking prevalence.9 This will help state and local decision makers to adopt prevention programming that is appropriate for its target audience and to employ effective strategies to focus limited funding for prevention programs efficiently. Poorly targeted interventions may even exacerbate existing inequalities in smoking-related health, but programs that penetrate deeply into disadvantaged communities can help reduce not only overall smoking but inequalities in health.10
We examined the following hypotheses: (1) adolescent smoking is associated with individual characteristics (e.g., age, race) and neighborhood-level characteristics (e.g., urban versus rural, race/ethnicity, socioeconomic demographics), and (2) these same individual and neighborhood-level characteristics will predict less exposure to prevention education programs in schools.
METHODS
We merged data from 2 sources: the 2005 Virginia Youth Tobacco Survey and the Census 2000 School District Demographics Project. The 2005 Virginia Youth Tobacco Survey data sampling procedures were developed by Virginia Commonwealth University and the Centers for Disease Control and Prevention. A sample of all public high schools (grades 9–12) and of all public middle schools (grades 6–8) in Virginia were selected through use of a 2-stage cluster sampling design to produce representative samples of middle and high school students. The first-stage sampling frame selected schools with a probability of selection proportional to their enrollment and the second stage selected classes using equal probability sampling with a random start. The parents of students in classes included in the sample frame were notified of the survey by letter, given a description of the survey and its purpose, and told that their child's participation was completely voluntary and anonymous.11
The Virginia Youth Tobacco Survey was administered in class by trained survey administrators from September 2005 through January 2006. Students were reassured during the administration of the survey that their participation was voluntary and that the information they provided would be kept private. Students who declined were excused. The paper-and-pencil survey did not include any identifying information. Of the 100 schools selected from the sampling frame of Virginia public schools, 64 agreed to participate. Responding schools were diverse in terms of geography and demographics. Of the 2816 eligible students in the randomly chosen classes, 2361 (84%) returned usable questionnaires. The final sample included over 1000 students from 29 high schools and over 1000 students from 35 middle schools. Of the 2214 respondents included in the final Virginia Youth Tobacco Survey data set, 2208 had complete data on study measures; these students comprised the study's subject population.
To obtain information on neighborhood characteristics, we retrieved available aggregate census data at the school-district level from the School District Demographics Project for each Virginia school district in the Virginia Youth Tobacco Survey sample. The School District Demographics Project was developed by the National Center for Education Statistics of the US Department of Education to provide access to information about school district demographic resources and characteristics for each US public school district. Using the School District Demographics Project, we collected several measures of neighborhood-level data that focused on local resources and structure, including the following: rurality versus urbanicity, employment rate, proportion of families with income below the federal poverty level, proportion unemployed, proportion with a high school education or higher, proportion of owner-occupied housing, proportion with no vehicle, proportion of single-parent families, and proportion of Black residents. These data were then merged with the original data set on the basis of its sampling frame (by the school district of each participating school).
All analyses accounted for effects of the complex sampling design on the calculations for sampling variances and confidence intervals.11 Preliminary analyses also incorporated weights, which were designed by Virginia Commonwealth University to account for chance of selection, nonresponse, and demographics; however, the weights were close to 1 and did not influence the models or the significance of results.
Measures
Outcomes.
“Current smoker” was measured as a categorical variable, with respondents who indicated that they “did not smoke cigarettes during the past 30 days” coded as nonsmokers, those who smoked on 1 to 5 of the past 30 days coded as light smokers, those who smoked on 6 to 19 of the past 30 days coded as medium smokers, and those who smoked on 20 to all of the past 30 days coded as heavy smokers. Tobacco education in school was measured as a dichotomous variable based on responses to the question, “During this school year, were you taught in any of your classes about the dangers of tobacco use?”
Individual-level demographics.
Age was measured as a continuous variable, and race/ethnicity was defined as non-Latino White (referent) versus Black or other. Unfortunately, no socioeconomic status data were included in the individual surveys.
School district–level variables.
The percentage of residents reporting Black race or ethnicity in the district was standardized, and districts were categorized as urban if 80% or more of the residents were living in urban areas. The remaining 8 district-level variables representing local economic and social characteristics were standardized and reverse coded where appropriate before exploratory factor analysis suggested 2 distinct factors.12 We further examined the 2 homogeneous item sets from the factors as potential scales. We evaluated internal consistency and reduced items using Cronbach α coefficients for each grouping. These analyses resulted in 2 scales, which were each standardized to a mean of 0 and standard deviation of 1, as follows: (1) socioeconomic disadvantage (α = 0.90), comprising percentage of families in poverty, percentage unemployed, and percentage with a high school education (reverse coded), and (2) social disorganization (α = 0.89), comprising percentage of single-parent families, percentage of homes with no vehicle, and percentage of owner-occupied housing units (reverse coded).
Analyses
We used tabular analyses to examine sample characteristics. To better understand who was being reached by prevention efforts and whether high-risk adolescents were being served, we used multinomial and binary multilevel models with random effects to determine whether demographic characteristics and neighborhood characteristics predicted smoking and exposure to prevention programs. We ran these models using the proc glimmix procedure13 add-on in SAS version 9.1 (SAS Institute Inc, Cary, North Carolina). This procedure can fit models with data correlations using generalized linear mixed models, and it can also fit models when the responses are not normally distributed. For example, binary multilevel models are similar conceptually to linear multilevel models in many ways. However, yij is a binary outcome (for individual i in neighborhood j) that is assumed to have a Bernoulli distribution.14 The outcome modeled is then the log odds of yij equaling 1. The general form of the model can be expressed with the following 2 equation levels:
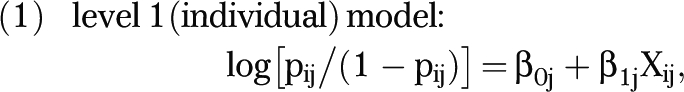 |
where pij is the probability that yij = 1 and xij is an explanatory variable at the individual level, and
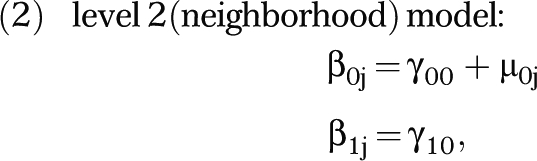 |
where μ0j is the random effect at level 2 and is distributed N(0, σ2u), and γ00 and γ10 are fixed effects for the intercept and the coefficient for xij, respectively.
The level 1 and level 2 equations can then be combined into a single equation:
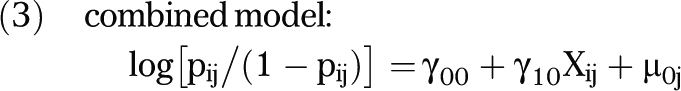 |
This basic binary random intercept hierarchical model was the basis of the education outcome analyses, with the addition of multiple level-1 and level-2 variables, including respondent's age and race/ethnicity (level 1) and the neighborhood's percentage of Black residents, urban status, and socioeconomic disadvantage score (level 2). For the nominal “current smokers” outcome, the procedure was similar but used a generalized logit model that allowed more than 2 outcome categories and produced risk ratios.
RESULTS
About 38% of respondents were of minority race/ethnicity, and their ages ranged from 11 to 18 years (mean = 14). Over 65% lived in an urban neighborhood; Table 1 shows the neighborhood characteristics of respondents. When using a multilevel model, it is important to examine the structure of the level-2 data. There were 61 groups (i.e., schools) in the complete data set. The largest group contained 174 observations (i.e., individual adolescents) and the smallest contained 11, with an average of 36 per group. Over 80% of the groups contained 20 or more observations. No group contained only a single observation, so a random effects model should be appropriate.14
TABLE 1.
Neighborhood Characteristics of Respondents: Virginia Youth Tobacco Survey, 2005, and the Census 2000 School District Demographics Project
| % of Respondents (n = 2208) |
|||
| Neighborhood Characteristic | Mean (SD) | Maximum | Minimum |
| Black | 19.0 (15.7) | 50.5 | 0.3 |
| Urban | 73.7 (33.5) | 100.0 | 0.0 |
| Social organization indicators | |||
| Homes with no vehicle | 7.3 (4.7) | 17.3 | 2.5 |
| Single-parent families | 27.6 (11.6) | 52.3 | 15.2 |
| Owner-occupied housing units | 69.0 (13.1) | 86.6 | 39.1 |
| Socioeconomic indicators | |||
| Unemployed | 4.3 (2.5) | 12.7 | 2.0 |
| Families in poverty | 7.1 (4.9) | 20.3 | 1.7 |
| High school education | 81.9 (9.2) | 92.5 | 58.9 |
Multilevel multinomial and binary logistic models of smoking and tobacco education were used to calculate relative risk ratios and odds ratios. In the analyses for tobacco education, we controlled for current smoking to ensure that results were not an artifact of smokers' being less likely or willing to recall tobacco education experiences. The variables indicating neighborhood urban status, proportion of Black residents, and social disorganization were not significant for either outcome and did not make substantial changes in the effects of socioeconomic disadvantage, so they were dropped from the final analyses.
Of the respondents, 6.1% were light smokers, 2.3% were medium smokers, and 5.6% were heavy smokers. Older adolescents had higher relative risks of being a light, medium, or heavy cigarette smoker than did younger adolescents. For example, the relative risk of heavy smoking increased by an average of 77% for each additional year of age. Black adolescents had a lower relative risk of heavy smoking than did White adolescents (relative risk ratio = 0.34). Adolescents in neighborhoods that were socioeconomically disadvantaged had significantly higher relative risks of being a light, medium, or heavy cigarette smoker compared with those from more advantaged neighborhoods (a relative risk increase of 49%, 36%, and 65%, respectively, for each standard deviation of socioeconomic disadvantage; Table 2).
TABLE 2.
Relative Risk Ratios (RRRs) and 95% Confidence Intervals (CIs) for Current Smoking: Virginia Youth Tobacco Survey, 2005, and the Census 2000 School District Demographics Project
| Variable | Light Smokers, RRR (95% CI) | Medium Smokers, RRR (95% CI) | Heavy Smokers, RRR (95% CI) |
| Age, y | 1.28 (1.17, 1.40) | 1.85 (1.54, 2.22) | 1.77 (1.58, 1.99) |
| Race/ethnicity | |||
| Non-Latino White (Ref) | 1.00 | 1.00 | 1.00 |
| Black | 0.72 (0.47, 1.12) | 0.69 (0.32, 1.50) | 0.34 (0.19, 0.59) |
| Other | 0.47 (0.24, 0.92) | 1.06 (0.46, 2.45) | 0.44 (0.22, 0.90) |
| Socioeconomic disadvantagea | 1.49 (1.25, 1.78) | 1.36 (0.95, 1.96) | 1.65 (1.37, 1.98) |
Note. Light smokers smoked on 1–5 of the past 30 days; medium smokers smoked on 6–19 of the past 30 days; heavy smokers smoked on ≥ 20 of the past 30 days. Total number of respondents was 2208. For all RRRs, P < .05 for fixed-effect F test.
Standardized to a mean of 0 and standard deviation of 1.
Most respondents (80.9%) reported receiving tobacco education in school. Older adolescents had higher odds of tobacco education than did younger adolescents; the odds of tobacco education increased by an average of 14% for each additional year of age. Adolescents in neighborhoods that were socioeconomically disadvantaged had significantly lower odds of tobacco education in school than did those from more advantaged neighborhoods, with the odds decreasing by 18% for each standard deviation of socioeconomic disadvantage (Table 3). This means that if a student from an average neighborhood has an 81% probability of receiving tobacco education, then a student from a neighborhood 1 standard deviation more socioeconomically disadvantaged would have a 78% probability (risk ratio = 0.96).
TABLE 3.
Odds Ratios (ORs) and 95% Confidence Intervals (CIs) for Receiving Smoking Education in School: Virginia Youth Tobacco Survey, 2005, and the Census 2000 School District Demographics Project
| Variable | OR (95% CI) |
| Age, y | 1.14* (1.07, 1.23) |
| Race/ethnicity | |
| Non-Latino White (Ref) | 1.00 |
| Black | 1.07 (0.80, 1.44) |
| Other | 0.75 (0.55, 1.02) |
| Socioeconomic disadvantagea | 0.82* (0.70, 0.95) |
Note. Total number of respondents was 2208.
Standardized to a mean of 0 and standard deviation of 1.
*P < .05 for fixed-effect F test (with control for light, medium, and heavy smoking).
DISCUSSION
We found that although adolescents in socioeconomically disadvantaged neighborhoods reported significantly higher relative risks of smoking, tobacco education programs did not appear to reach these higher-risk students; those in disadvantaged neighborhoods had significantly lower odds of reporting receipt of tobacco education. Therefore, there may be a mismatch between indicators of need for tobacco prevention education and the actual targeting and successful implementation of those services.
The results showing that students in low-income neighborhoods reported less exposure to tobacco prevention programs concur with a national survey of counties that found that low-income counties had fewer tobacco cessation programs.15 This combination of disparities in prevention and cessation programs is particularly disturbing when one considers the results of this study and other research indicating that low-income neighborhoods have higher smoking rates and therefore are most in need of interventions to ameliorate health inequities.5–7
Many barriers may make students in socioeconomically disadvantaged neighborhoods less likely to receive smoking prevention education, thus exacerbating health inequalities. For a student to receive smoking prevention education, several factors need to come together. First, someone at the school must choose to implement a smoking prevention program; second, that program must be funded; and third, the program must be implemented with fidelity. Health intervention education programs in schools are often funded through grants from various organizations. For example, the Virginia Tobacco Settlement Foundation has provided grants to several school districts in Virginia. Such program participants represent a self-selected group of communities who have the capacity and resources to put together a competitive grant proposal. Furthermore, some funding may come from sources that specify the type of program that can be used. For example, grants from the tobacco industry itself may promote more generalized goals such as life-skills training, therefore diluting more specific and effective tobacco prevention messages.16 Districts in greatest need of support may be more likely to accept funding from these types of sources.
Improved funding is only one input and cannot alone ensure that good programs reach a broad set of students in a district. Support for a tobacco prevention program and the capacity to maintain implementation fidelity so that students receive the intended intervention can depend on multiple factors that may vary with community characteristics and resources.17 Furthermore, schools in disadvantaged neighborhoods may face additional competing educational challenges that could limit the amount of time available for, or the priority given to, a tobacco education program. A review of school drug abuse prevention programs found that most instructors did not cover the entire intervention curriculum and that program fidelity was related to a range of key elements, including training, program design, and school organization.18 Process evaluations of tobacco prevention programs also indicate that school capacity and leadership factors predict adherence and the extent of activity dedicated to implementation.19 Therefore, beyond funding issues, the provision of implementation support, capacity building, training, and technical assistance may all play a role in improving implementation fidelity.17
Although reported smoking rates are higher in neighborhoods with socioeconomic disadvantage indicators, receipt of school-based interventions appears significantly less common, indicating that we may not be targeting and implementing school programs effectively. Policymakers should be aware that those who need assistance most may be the ones least able to apply for help or implement programs. School administrators and teachers in schools serving areas of low socioeconomic status may find it difficult to justify spending scarce time and resources on tobacco prevention programs or even grant-writing efforts. Policymakers and funding providers should conduct needs analyses not only to identify areas targeted for new programs on the basis of health, economic, and smoking inequities but also to assess capacity-building needs before program funding is distributed. School systems most in need of interventions are also likely to be in need of extra resources, both to apply for funding and to implement the programs.
Rather than relying only on broadly targeted calls for proposals, programs could partner with specific high-need local communities to provide planning and implementation assistance and capacity building to improve sustainability and the ability to pursue future funding opportunities. Extra funding, structural support, and other resources could be earmarked specifically for economically disadvantaged areas. Using funds for the hiring of district-level personnel to coordinate grant writing and program implementation could be an effective way to get the resources to those districts in need. Through analysis of the types of programs that seem to work most effectively in which contexts, policymakers can target those districts that most need interventions with context-tailored programs.
School-based smoking education and prevention programs have received mixed evaluations in the literature. Although many evaluations have found significant reductions in smoking, the impact may be small or may diminish with time.20–25 There is still a substantial need for high-quality longitudinal studies of smoking prevention education that examine not only the long-term impact, but also assess differences between programs and their underlying theoretical foundations and determine how these may influence effectiveness.20,26 Neighborhood contexts may be an important factor in how well different types of education programs perform. Therefore, research on neighborhood indices should be used not only to determine where programs should be targeted, but also to examine the efficacy of different types of programs in different contexts. Such research would be very helpful in efforts to reduce health disparities.
Limitations
This study has several limitations. Its results were based on secondary data, which restricted the variables that could be included. Unfortunately, no individual-level socioeconomic status data were collected in the tobacco survey, so we could not control for these effects on smoking. Therefore, the results for the neighborhood socioeconomic disadvantage scale likely also proxy for some individual-level effects and should be interpreted as a useful neighborhood-level indicator rather than as evidence of a neighborhood effect. We assessed tobacco use by self-reports of adolescents, which may introduce recall error; however, studies with adolescents have shown the validity of self-reports of tobacco use.27–29 Furthermore, a reliability study of the Youth Risk Behavior Survey, which has many questions in common with the Virginia Youth Tobacco Survey, found that none of the 13 tobacco-related items differed significantly between measurements taken about 2 weeks apart, and that tobacco use items had an average κ of 68.8%, indicating a significantly higher reliability than those of other topics examined, such as injuries, violence, diet, and physical activity.30
The implementation fidelity of prevention education is commonly compromised, leading to a possible disconnect between funding of prevention, adoption at the school level, and actual receipt and dose of prevention intervention at the student level.31 Thus, finding the appropriate measure for successfully implemented programming can be difficult. Social desirability bias is particularly an issue when implementers such as teachers or administrators are relied on to report programming adherence.32 For example, a study of implementation fidelity comparing teacher self-report to classroom observation found that teacher self-report was not a valid measure for describing the extent of program implementation.33 Therefore, we operationalized tobacco educational intervention using the self-reports of adolescents in response to a broadly worded question designed to capture any classroom content focused on the dangers of tobacco.
These adolescent self-reports may also suffer from recall error but are less likely to be influenced by social desirability bias. Adolescent self-reports of receiving care and education have been shown to be a valid and reliable method for determining prevention service delivery. In a clinic study that compared self-reports with audiotapes of clinic visits adolescents' recall accuracy of whether they received tobacco counseling by the clinician was 86% 2 to 6 weeks after the visit and 80% 5 to 7 months after the clinic visit.34 Another benefit of using students' self-report of prevention education is that recall of program details is an indicator of a participant's responsiveness, and this output indicates that, at the very least, a school has successfully implemented a memorable prevention program that has penetrated to the individual student level.32 Externally trained classroom observers may be preferable to all forms of self-report from implementers and participants,32 but this would be very costly to implement on a statewide scale. However, future research may benefit from including some level of measure verification through trained observers.
This study is not intended to address causal inference. Multilevel studies of observational neighborhood characteristics have many drawbacks in answering causal questions.35 However, they are very well-suited to identifying indicators to target intervention strategies. This study used neighborhood data compiled at the school-district level, which can be a limitation because schools often span diverse demographic profiles. However, there are also substantial between-district differences within the state of Virginia, as shown in the ranges in Table 1, reflecting different access to community resources across schools in this study. This is exactly the type of regional or neighborhood effect that multilevel modeling is ideal for exploring.
Conclusions
This study shows that district-level data can be used as indicators of higher risk and as tools to help target future educational interventions. They are also useful in exploring disparities between more- and less-advantaged school districts. When low income and other related factors are associated not only with higher risk factors but also with lower levels of preventive services, the situation may further aggravate persistent gaps in long-term health status.
Acknowledgments
Support for this research was provided by the Virginia Tobacco Settlement Foundation and the Virginia Youth Tobacco Project.
We extend appreciation to A. P. C. Weintraub for his assistance.
Human Participant Protection
This study was approved by the Virginia Tech institutional review board.
References
- 1.Centers for Disease Control and Prevention Annual smoking attributable mortality, years of potential life lost, and productivity losses, United States, 1997 to 2001. MMWR Morb Mortal Wkly Rep. 2005;54(25):625–628 [PubMed] [Google Scholar]
- 2.Healthy People 2010: Understanding and Improving Health. Washington, DC: Dept of Health and Human Services; 2000 [Google Scholar]
- 3.Marshall L, Schooley M, Ryan H, et al. Youth tobacco surveillance—United States, 2001–2002. MMWR Surveill Summ. 2006;55(3):1–56 [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Cigarette use among high school students, United States, 1991 to 2005. MMWR Morb Mortal Wkly Rep. 2006;55(26):724–726 [PubMed] [Google Scholar]
- 5.Datta GD, Subramanian SV, Colditz GA, Kawachi I, Palmer JR, Rosenberg L. Individual, neighborhood, and state-level predictors of smoking among US black women: a multilevel analysis. Soc Sci Med. 2006;63(4):1034–1044 [DOI] [PubMed] [Google Scholar]
- 6.Duncan C, Jones K, Moon G. Smoking and deprivation: are there neighbourhood effects? Soc Sci Med. 1999;48(4):497–505 [DOI] [PubMed] [Google Scholar]
- 7.Ennett ST, Flewelling RL, Lindrooth RC, Norton EC. School and neighborhood characteristics associated with school rates of alcohol, cigarette, and marijuana use. J Health Soc Behav. 1997;38(1):55–71 [PubMed] [Google Scholar]
- 8.Nowlin PR, Colder CR. The role of ethnicity and neighborhood poverty on the relationship between parenting and adolescent cigarette use. Nicotine Tob Res. 2007;9(5):545–556 [DOI] [PubMed] [Google Scholar]
- 9.Peterson AV, Jr, Kealey KA, Mann SL, Marek PM, Sarason IG. Hutchinson Smoking Prevention Project: long-term randomized trial in school-based tobacco use prevention—results on smoking. J Natl Cancer Inst. 2000;92(24):1979–1991 [DOI] [PubMed] [Google Scholar]
- 10.Bauld L, Judge K, Platt S. Assessing the impact of smoking cessation services on reducing health inequalities in England: observational study. Tob Control. 2007;16(6):400–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Virginia Tobacco Settlement Foundation Tobacco Use Among Virginia's Middle and High School Students: Results of the 2005 Youth Tobacco Survey. Richmond, VA: Community Health Research Initiative, Survey and Evaluation Research Laboratory, Virginia Commonwealth University; 2006 [Google Scholar]
- 12.DeVellis RF. Scale Development: Theory and Applications. Newbury Park, CA: Sage Publications Inc; 1991 [Google Scholar]
- 13.SAS Institute Inc Production GLIMMIX procedure. Available at: http://support.sas.com/rnd/app/da/glimmix.html. Accessed October 30, 2009
- 14.Guo G, Zhao H. Multilevel modeling for binary data. Annu Rev Sociol. 2000;26:441–462 [Google Scholar]
- 15.Curry SJ, Emery S, Sporer AK, et al. A national survey of tobacco cessation programs for youths. Am J Public Health. 2007;97(1):171–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mandel LL, Bialous SA, Glantz SA. Avoiding “truth”: tobacco industry promotion of life skills training. J Adolesc Health. 2006;39(6):868–879 [DOI] [PubMed] [Google Scholar]
- 17.Gingiss PM, Roberts-Gray C, Boerm M. Bridge-it: a system for predicting implementation fidelity for school-based tobacco prevention programs. Prev Sci. 2006;7(2):197–207 [DOI] [PubMed] [Google Scholar]
- 18.Dusenbury L, Brannigan R, Falco M, Hansen WB. A review of research on fidelity of implementation: implications for drug abuse prevention in school settings. Health Educ Res. 2003;18(2):237–256 [DOI] [PubMed] [Google Scholar]
- 19.Roberts-Gray C, Gingiss PM, Boerm M. Evaluating school capacity to implement new programs. Eval Program Plann. 2007;30(3):247–257 [DOI] [PubMed] [Google Scholar]
- 20.Thomas R, Perera R. School-based programmes for preventing smoking. Cochrane Database Syst Rev. 2006 Jul 19;3:CD001293. [DOI] [PubMed] [Google Scholar]
- 21.Hoeflmayr D, Hanewinkel R. Do school-based tobacco prevention programmes pay off? The cost-effectiveness of the “Smoke-Free Class Competition.” Public Health. 2008;122(1):34–41 [DOI] [PubMed] [Google Scholar]
- 22.Ranney L, Melvin C, Lux L, McClain E, Morgan L, Lohr KN. Tobacco use: prevention, cessation, and control. Evid Rep Technol Assess (Full Rep). 2006 Jun;(140):1–120 [PMC free article] [PubMed] [Google Scholar]
- 23.Brown CH, Guo J, Singer LT, Downes K, Brinales JM. Examining the effects of school-based drug prevention programs on drug use in rural settings: methodology and initial findings. J Rural Health. 2007;23(suppl):29–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Flay BR. Psychosocial approaches to smoking prevention: a review of findings. Health Psychol. 1985;4(5):449–488 [DOI] [PubMed] [Google Scholar]
- 25.Dobbins M, DeCorby K, Manske S, Goldblatt E. Effective practices for school-based tobacco use prevention. Prev Med. 2008;46(4):289–297 [DOI] [PubMed] [Google Scholar]
- 26.Botvin GJ, Griffin KW. School-based programmes to prevent alcohol, tobacco and other drug use. Int Rev Psychiatry. 2007;19(6):607–615 [DOI] [PubMed] [Google Scholar]
- 27.Martin GL, Newman IM. Assessing the validity of self-reported adolescent cigarette smoking. J Drug Educ. 1988;18(4):275–284 [DOI] [PubMed] [Google Scholar]
- 28.Williams CL, Eng A, Botvin GJ, Hill P, Wynder EL. Validation of students' self-reported cigarette smoking status with plasma cotinine levels. Am J Public Health. 1979;69(12):1272–1274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wills TA, Cleary SD. The validity of self-reports of smoking: analyses by race/ethnicity in a school sample of urban adolescents. Am J Public Health. 1997;87(1):56–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 youth risk behavior survey questionnaire. J Adolesc Health. 2002;31(4):336–342 [DOI] [PubMed] [Google Scholar]
- 31.Skager R. Replacing ineffective early alcohol/drug education in the United States with age-appropriate adolescent programmes and assistance to problematic users. Drug Alcohol Rev. 2007;26(6):577–584 [DOI] [PubMed] [Google Scholar]
- 32.Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control? Clin Psychol Rev. 1998;18(1):23–45 [DOI] [PubMed] [Google Scholar]
- 33.Resnicow K, Davis M, Smith M, et al. How best to measure implementation of school health curricula: a comparison of three measures. Health Educ Res. 1998;13(2):239–250 [DOI] [PubMed] [Google Scholar]
- 34.Klein JD, Graff CA, Santelli JS, Hedberg VA, Allan MJ, Elster AB. Developing quality measures for adolescent care: validity of adolescents' self-reported receipt of preventive services. Health Serv Res. 1999;34(1 pt 2):391–404 [PMC free article] [PubMed] [Google Scholar]
- 35.Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med. 2004;58(10):1929–1952 [DOI] [PubMed] [Google Scholar]


