Abstract
Objectives. We examined trends in tuberculosis (TB) cases and case rates among US- and foreign-born children and adolescents and analyzed the potential effect of changes to overseas screening of applicants for immigration to the United States.
Methods. We analyzed TB case data from the National Tuberculosis Surveillance System for 1994 to 2007.
Results. Foreign-born children and adolescents accounted for 31% of 18 659 reported TB cases in persons younger than age 18 years from 1994 to 2007. TB rates declined 44% among foreign-born children and adolescents (20.3 per 100 00 to 11.4 per 100 000 population) and 48% (2.1 per 100 000 to 1.1 per 100 000) among those who were born in the United States. Rates were nearly 20 times as high among foreign-born as among US-born adolescents. Among foreign-born children and adolescents with known month of US entry (88%), more than 20% were diagnosed with TB within 3 months of entry.
Conclusions. Marked disparities in TB morbidity persist between foreign- and US-born children and adolescents. These disparities and the high proportion of TB cases diagnosed shortly after US entry suggest a need for enhanced pre- and postimmigration screening.
Tuberculosis (TB) case rates continue to decline in the United States and were recently recorded at their lowest level since national recording began in 1953.1 Although annual TB incidence among US-born persons is declining, the number of new cases reported each year among foreign-born persons has been relatively stable over the past decade; foreign-born persons accounted for almost 60% of TB cases reported in the United States in 2008.1 TB in foreign-born persons in the United States is largely attributable to acquisition of latent TB infection (LTBI) in TB-endemic countries of origin and subsequent activation of disease after US arrival.2 The large burden of TB among foreign-born persons in the United States likely reflects the persistently large burden of TB in many other countries.3
An estimated 11% of all TB cases worldwide occur in children younger than age 15 years.4 In TB-endemic settings, acquisition of TB infection often occurs in childhood because children are more likely to have frequent and close contact with adults with infectious TB.5,6 Compared with adult rates of progression from infection to disease (historically 5%–10% progress to disease), rates are higher for children of all ages and highest for infants younger than 1 year (43%) and children aged 1 to 5 years (24%).4,7,8 Furthermore, children who become infected with TB but do not progress to disease in childhood represent a potential pool for disease in adulthood.4,7 Elucidating the epidemiology of TB in foreign-born children could therefore facilitate efforts to improve children's health and control TB by preventing future disease.
TB cases are generally reported in the broad age categories of children (defined as < 15 years) and adults (≥ 15 years).2,9,10 However, adolescents are an important group to study because TB rates rise in adolescence following the decline seen in the elementary school years.11 In addition, adolescents are more likely to present with adult-type pulmonary TB (characterized by disease in the lung apices and a tendency to form cavitary lesions).11 As a result, adolescents are more likely than are younger children to transmit TB to others.8,11
As part of an effort to limit importation of TB disease, the Centers for Disease Control and Prevention in 2007 published revised requirements for overseas medical screening of applicants for US immigration.12 All persons aged 15 years or older continue to be screened with chest radiographs. Revised technical instructions now require a tuberculin skin test (TST) for all applicants aged 2 to 14 years who live in countries with a large TB burden. Chest radiographs are performed for those whose TST is positive.12 The potential effect of these changes is not known.
We sought to describe the epidemiology of TB among foreign- and US-born children and adolescents in terms of demographic and clinical characteristics and to analyze the potential effect of the 2007 changes to the instructions for overseas screening of applicants for immigration to the United States.
METHODS
We analyzed all verified cases of TB reported via a standardized Report of a Verified Case of TB (RVCT) form to the US National TB Surveillance System (NTSS) between January 1, 1994, and December 31, 2007. Verified cases consisted of all incident TB disease episodes meeting criteria for public health surveillance as defined by laboratory or clinical evidence of active disease attributable to Mycobacterium tuberculosis complex.10 Case reports contained demographic, clinical, laboratory, and treatment information and, for foreign-born persons, information on country of birth and month and year of entry into the United States. Consistent with US Census Bureau definitions, US-born persons were defined as persons born in the United States, Puerto Rico, or US outlying area or born abroad to US parents; all other persons were defined as foreign born.13
For age at TB diagnosis, we used the categories children (< 13 years), adolescents (13–17 years), and adults (≥ 18 years). Children were further divided into 3 age categories corresponding to the known age-specific disease patterns of TB among children: younger than 1 year, 1 to 4 years, and 5 to 12 years.
For our analysis of the effect of policy changes for preimmigration screening, we grouped foreign-born children and adolescents into the 3 age categories used in overseas screening regulations: younger than 2 years, 2 to 14 years, and 15 to 17 years. To analyze the potential effect of preimmigration screening, we evaluated TST and chest radiograph results as well as country of origin for cases of TB among foreign-born children and adolescents diagnosed within 3 months of US entry; cases diagnosed within 3 months of US entry were assumed to be missed prevalent disease at the time of entry. We also analyzed data for persons entering the country as children or adolescents (defined as younger than 18 years at the time of US entry) by their number of years in the United States prior to TB diagnosis, to determine the proportion of cases diagnosed in the years immediately following US entry (< 1 year or 1–4 years) versus the proportion of TB cases diagnosed later (5–9 years or ≥ 10 years).
We used population estimates from the annual March supplement of the US Census Bureau's Current Population Survey for 1994 to 2007 to calculate all TB case rates.13
RESULTS
From 1994 to 2007, 245 853 verified new cases of TB were reported to the NTSS; we excluded 110 with missing data on age and 1241 with missing data on origin (US born versus foreign born). Of the 244 502 TB cases with known age and origin, 18 659 (8%) were among children and adolescents. Of these, 5806 (31%) occurred in foreign-born persons. Among adults during this period, 225 843 new verified TB cases with known origin were recorded, of which 104 045 (46%) were among foreign-born persons.
Characteristics of Persons With Tuberculosis
For both US- and foreign-born children and adolescents, overall TB rates per 100 000 population were highest among children younger than 5 years. The greatest disparity we observed between foreign- and US-born persons occurred among adolescents: rates were nearly 20 times as high among foreign-born as among US-born adolescents. Young children aged 1 to 4 years accounted for the most TB cases among US-born children and adolescents (48%); among their foreign-born peers, the largest proportion occurred in adolescents (45%; Table 1).
TABLE 1.
Tuberculosis Cases and Case Rates Among US- and Foreign-Born Children and Adolescents Reported to the National TB Surveillance System: United States, 1994–2007
| US Born (n = 12853) |
Foreign Born (n = 5806) |
||||
| No. (%) | Rateb | No. (%) | Rateb | Rate Ratioa | |
| Age Group, y | |||||
| < 1 | 1348 (10) | 2.5 | 110 (2) | 32.2 | 12.9 |
| 1–4 | 6225 (48) | 2.8 | 1224 (21) | 30.5 | 10.9 |
| 5–12 | 3202 (25) | 0.7 | 1856 (32) | 10.8 | 15.4 |
| 13–17 | 2078 (16) | 0.8 | 2616 (45) | 15.0 | 18.8 |
Note. Comparative figures for adults (≥ 18 years) were US born, n = 121 798, rate = 4.9; foreign born, n = 104 045, rate = 28.0; rate ratio = 5.7.
Foreign-born versus US-born case rates.
Per 100 000 population.
TB rates among US-born children and adolescents declined 48%, from 2.1 per 100 000 population in 1994 to 1.1 per 100 000 in 2007. The number of TB cases declined 46%, from 1386 to 749. TB rates also declined among foreign-born children and adolescents (44%, from 20.3 per 100 000 to 11.4 per 100 000 population) but remained higher than among US-born young people, with increasing disparities among the older age groups. The number of TB cases among foreign-born children and adolescents declined 33%, from 522 in 1994 to 352 in 2007. By contrast, the number of TB cases among foreign-born adults during this period increased slightly, from 7233 in 1994 to 7469 in 2007; the TB rate among foreign-born adults declined 40% during this period, from 36.3 per 100 000 to 21.8 per 100 000 population (Table 2).
TABLE 2.
Changes in Tuberculosis Case Rates Among US- and Foreign-Born Persons Between 1994 and 2007: United States
| US Born |
Foreign Born |
||||||||
| Age Group, y | No. | Population | Rateb | % Change | No. | Population | Rateb | % Change | Rate Ratioa |
| < 1 y | −18 | −64 | |||||||
| 1994 | 136 | 3 971 344 | 3.4 | 6 | 13 143 | 45.7 | 13.4 | ||
| 2007 | 114 | 4 004 345 | 2.8 | 6 | 36 189 | 16.6 | 5.9 | ||
| 1–4 y | −55 | −53 | |||||||
| 1994 | 717 | 16 196 537 | 4.4 | 126 | 288 748 | 43.6 | 9.9 | ||
| 2007 | 318 | 16 140 031 | 2.0 | 63 | 310 275 | 20.3 | 10.2 | ||
| 5–12 y | −58 | −58 | |||||||
| 1994 | 343 | 29 733 594 | 1.2 | 203 | 1 134 380 | 17.9 | 14.9 | ||
| 2007 | 167 | 30 699 415 | 0.5 | 99 | 1 311 532 | 7.5 | 15.0 | ||
| 13–17 y | −36 | −22 | |||||||
| 1994 | 190 | 17 294 315 | 1.1 | 187 | 1 131 164 | 16.5 | 15.0 | ||
| 2007 | 150 | 20 209 083 | 0.7 | 184 | 1 440 846 | 12.8 | 18.3 | ||
| 0–17y | −48 | −44 | |||||||
| 1994 | 1386 | 67 195 970 | 2.1 | 522 | 2 567 435 | 20.3 | 9.7 | ||
| 2007 | 749 | 71 052 874 | 1.1 | 352 | 3 098 842 | 11.4 | 10.4 | ||
| ≥ 18 y | −70 | −40 | |||||||
| 1994 | 15 006 | 169 102 131 | 8.9 | 7233 | 19 932 874 | 36.3 | 4.1 | ||
| 2007 | 5076 | 187 634 769 | 2.7 | 7469 | 34 270 338 | 21.8 | 8.1 | ||
Foreign-born versus US-born case rates.
Per 100 000 population.
Among racial/ethnic groups, Hispanics accounted for the highest percentage of TB cases among both foreign-born (46%) and US-born (39%) children and adolescents and the second highest percentage among foreign-born adults (37%). Only 12% of US-born adult TB cases occurred among Hispanics (Table 3).
TABLE 3.
Demographic and Clinical Characteristics of US- and Foreign-Born Persons With Tuberculosis: United States, 1994–2007
| Children and Adolescents |
Adults |
||||
| US Borna, No. (%) | Foreign Bornb, No. (%) | US Bornc, No. (%) | Foreign Bornd, No. (%) | ||
| Male | 6 435 (50) | 2 947 (51) | 81 189 (67) | 62 182 (60) | |
| Median age, y | 3 | 11 | 50 | 41 | |
| Race/ethnicity | |||||
| Hispanice | 4 952 (39) | 2 664 (46) | 14 355 (12) | 38 435 (37) | |
| Non-Hispanic White | 1 491 (12) | 377 (6) | 45 600 (37) | 6 499 (6) | |
| Non-Hispanic Black or African American | 4 865 (38) | 1 211 (21) | 56 195 (46) | 12 324 (12) | |
| Non-Hispanic American Indian or Native Alaskan | 300 (2) | 3 (< 1) | 2 751 (2) | 67 (< 1) | |
| Non-Hispanic Asian or Pacific Islander | 1 049 (8) | 1 494 (26) | 2 321 (2) | 46 005 (44) | |
| Site of disease | |||||
| Pulmonary only | 9 074 (71) | 4 178 (72) | 93 457 (77) | 72 621 (70) | |
| Extrapulmonary only | 2 746 (21) | 1 337 (23) | 18 881 (16) | 23 251 (22) | |
| Both | 1 028 (8) | 291 (5) | 9 413 (8) | 8 150 (8) | |
| Sputum culture positivef | 1 526 (42) | 1 397 (45) | 75 960 (79) | 60 706 (73) | |
| Other culture positiveg | 2 609 (52) | 859 (48) | 39 217 (82) | 33 519 (81) | |
| Drug susceptibility testing doneh | 3 666 (94) | 2 049 (97) | 97 922 (95) | 82 995 (97) | |
| Drug resistancei | |||||
| None | 3 115 (85) | 1 633 (80) | 88 665 (91) | 68 164 (82) | |
| INH resistant | 226 (6) | 242 (12) | 4 948 (5) | 9 294 (11) | |
| MDRj | 54 (1) | 48 (2) | 1 023 (1) | 1 503 (2) | |
| XDRk | 1 (2) | 1 (2) | 16 (2) | 23 (2) | |
| HIV statusl | |||||
| No result | 9 730 (76) | 4 037 (70) | 55 728 (46) | 59 939 (58) | |
| Positive | 121 (4) | 41 (2) | 16 737 (25) | 5 503 (12) | |
| Negative | 2 989 (95) | 1 722 (97) | 49 198 (74) | 38 537 (87) | |
| Indeterminate | 13 (< 1) | 6 (< 1) | 135 (< 1) | 66 (< 1) | |
| Alive at diagnosis | 12 814 (99.7) | 5 790 (99.7) | 116 357 (96) | 102 427 (98) | |
| Outcomem | |||||
| Completed treatment | 11 640 (91) | 5 179 (89) | 88 589 (76) | 81 281 (79) | |
| Died | 69 (1) | 25 (< 1) | 14 789 (13) | 5 017 (5) | |
| Othern | 1 105 (9) | 514 (9) | 12 979 (11) | 16 129 (16) | |
Note. INH =isoniazid ; MDR = multidrug resistant; TB = tuberculosis; XDR = extensively drug resistant.
n = 12 853, or 69%.
n = 5806, or 31%.
n = 121 798, or 54%.
n = 104 045, or 46%.
May be of any race or multiple races.
For persons in each group who had sputum culture result: US-born children and adolescents, n = 3644; foreign-born children and adolescents, n = 3128; US-born adults, n = 95 925; foreign-born adults, n = 82 869.
For persons in each group who had other culture result (gastric aspirates and tissues or fluids other than sputum): US-born children and adolescents, n = 5010; foreign-born children and adolescents, n = 1795; US-born adults, n = 47 692; foreign-born adults, n = 41 217.
For persons with a positive culture.
For persons who were tested for drug susceptibility because of initial susceptibility test results.
Resistant to at least isoniazid and rifampin.
Resistant to at least isoniazid and rifampin among first-line anti-TB drugs, resistant to any fluoroquinolone (e.g., ciprofloxacin or ofloxacin), and resistant to at least 1 second-line injectable drug (e.g., amikacin, capreomycin, or kanamycin). Percentage XDR uses MDR TB as denominator.
Positive, negative, and indeterminate figures are for persons who had a known HIV test result; all California data were reported as no result.
For persons alive at diagnosis: US-born and adolescents, n = 12 814, foreign-born and adolescents, n = 5790; US born adults, n = 116 357; foreign-born adults, n = 102 427.
Moved, lost to follow-up, uncooperative or refused, other, unknown, or missing.
The median age was 3 years for US-born and 11 years for foreign-born children and adolescents with TB. Proportions of pulmonary and extrapulmonary disease were similar among US- and foreign-born children and adolescents. Foreign-born children and adolescents were more likely to have sputum culture-positive disease, consistent with the older median age in this group. Compared with adults, children and adolescents (both US and foreign born) were less likely to have culture-positive disease. Among all children and adolescents, approximately 95% who had a positive culture had also been tested for drug susceptibility. Foreign-born children and adolescents had a higher percentage of drug-resistant TB overall (20% vs 15%), isoniazid-resistant TB (12% vs 6%), and multidrug-resistant TB (2% vs 1%) than did US-born children and adolescents. We observed similar patterns in adults (Table 3).
HIV test results were not reported to the NTSS for most US-born (76%) and foreign-born (70%) children and adolescents. Of those with an HIV result reported, 4% of US-born and 2% of foreign-born children and adolescents had a positive result (Table 3).
Very few children died before TB diagnosis, and both US- and foreign-born children and adolescents had better treatment outcomes than did adults. Among those who were alive at diagnosis, approximately 90% of children and adolescents completed treatment; proportions were similar among the US born (91%) and foreign born (89%). During the 14-year study period, among those alive at diagnosis, 69 (1%) US-born and 25 (< 1%) foreign-born children and adolescents died during TB treatment; 14 789 (13%) US-born and 5017 (5%) foreign-born adults died during TB treatment (Table 3).
Potential Effect of Overseas Screening
Data on month of entry to the United States was available for 88% (5133 of 5806) of foreign-born children and adolescents. Of these, 37% (152 of 414) who were younger than 2 years, 27% (791 of 2978) who were aged 2 to 14 years, and 20% (340 of 1741) who were aged 15 to 17 years were diagnosed with TB disease within 3 months of entry to the United States. Among those diagnosed with TB disease within 3 months of entry for whom a result was recorded, 93% who were aged 2 to 14 years (those who would be screened for TB with TST under the revised technical instructions) had a positive TST at the time of TB diagnosis, and 93% who were aged 15 to 17 years (those who would be screened with a chest radiograph) had an abnormal chest radiograph. Among children younger than 2 years (not routinely screened with either TST or chest radiograph), 87% had a positive TST and 93% had an abnormal chest radiograph at the time of TB diagnosis (see Table A, available as a supplement to the online version of this article at http://www.ajph.org).
The countries that accounted for the most TB cases diagnosed within 3 months of US entry during the first half of the study period (1994–2000) were, among children younger than 2 years, Mexico, Russia, Philippines, Vietnam, China, and Bosnia–Herzegovina (the latter 2 in equal numbers); among children and adolescents aged 2 to 14 years, Mexico, Philippines, Somalia, Vietnam (the latter 2 in equal numbers), Russia, and Ethiopia; among adolescents aged 15 to 17 years, Mexico, Philippines, Somalia, Vietnam, and Haiti; and among adults, Philippines, Vietnam, Mexico, India, and China.
In 2001 to 2007, Mexico accounted for the most TB cases diagnosed within 3 months of US entry among children in all age categories; among adolescents, an equal number of these cases originated in Mexico and the Philippines; the Philippines accounted for the most of these cases among adults. During this period, the proportion of cases diagnosed within 3 months of US entry among children younger than 2 years coming from China increased from the first half of the study period, with China becoming second only to Mexico.
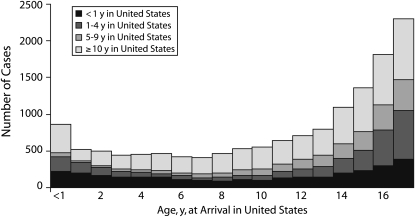
Among all foreign-born persons who entered the country when they were younger than 18 years, 17% to 26% were diagnosed with TB within 1 year of US entry. The most TB cases diagnosed more than 1 year after US entry occurred among those who entered as adolescents: 24% were diagnosed 1 to 4 years after US entry, 19% were diagnosed 5 to 9 years after US entry, and 40% were diagnosed 10 or more years after US entry (Figure 1).
FIGURE 1.
Tuberculosis cases among foreign-born persons who were younger than 18 years at time of US entry, by age at US arrival and number of years in the United States prior to TB diagnosis: 1994–2007.
DISCUSSION
Foreign-born children and adolescents living in the United States experience markedly higher rates of TB than do their US-born peers. We found that TB rates among foreign-born children and adolescents were 10 to 20 times as high as among US-born children and adolescents, with the highest rates among the youngest age groups and the greatest disparity among adolescents. Despite greater than 40% reductions in TB rates among both US- and foreign-born children and adolescents during the 14-year study period, disparities in TB rates between US- and foreign-born children and adolescents persist.
High TB rates among infants and young children reflect the increased risk of progression from recent TB infection to disease. Smaller disparities in TB rates seen in younger age groups may reflect a higher risk for TB exposure among US-born children of foreign-born parents from TB-endemic regions than among US-born children of US-born parents. Hispanics accounted for almost 40% of TB cases among US-born children and adolescents but only 12% of TB cases among US-born adults, suggesting that US-born children's risk for TB may be at least partially determined by their families' country of origin. In adolescence, TB resulting from activation of LTBI becomes more common. The disparity in TB rates we observed between US- and foreign-born adolescents likely reflects higher rates of LTBI among foreign-born adolescents and may represent missed opportunities for identification and treatment of LTBI.
Our analyses suggest that overseas screening of immigration applicants aged 2 to 14 years with TST followed by chest radiograph under the 2007 revisions to the Centers for Disease Control and Prevention screening requirements could enhance the identification of prevalent TB disease and LTBI in this age group. However, it is not known how many children would need to be screened to identify those with disease and what the most cost-effective approach to screening would be. Furthermore, it is not possible to determine the magnitude of the impact of the revised overseas screening requirements because the current NTSS data do not include information on immigration status. The Department of Homeland Security estimates that approximately 62% of foreign-born persons living in the United States were legal residents in 2007.14 All persons entering the country outside of formal immigration processes would not be subject to screening, including students or other temporary visitors.
The revised technical instructions requiring TST for children living in large TB-burden countries do not apply to children younger than 2 years, an important group because the highest TB rates were observed among the youngest age groups. As under the old rules, children younger than 2 years old are evaluated for TB with history and physical examination, and only those who are symptomatic or who have known contact of someone with recently diagnosed TB get a TST.
A potentially important group of young foreign-born children on which to focus may be international adoptees who are younger than 2 years when they come to the United States. For the fiscal years 2004 to 2007, the largest number of adoptions to the United States were from China, followed by Guatemala and Russia.15 We found that in 2001 to 2007, China was the country of origin, second only to Mexico, of the most TB cases among foreign-born children younger than 2 years old diagnosed within 3 months of US entry. Russia was among the top 5 countries and Guatemala among the top 10 countries, which may reflect international adoption patterns prevalent at the time. Prompt, regular postimmigration screening for TB could identify TB disease or LTBI and lead to appropriate treatment. Consistent with American Academy of Pediatrics and Centers for Disease Control and Prevention recommendations, children and adolescents from countries with a large TB burden—including international adoptees—should be targeted for TB testing subsequent to immigration.16 Efforts to find and treat LTBI in these children could substantially reduce the risk for the development of disease over time and thereby avert future TB cases.
During our study period, up to one quarter of foreign-born persons entering the country during childhood or adolescence were diagnosed with TB within 1 year of US entry. Among persons entering the country during infancy and early childhood who went on to develop TB, approximately half were diagnosed within 5 years of US entry; most of the others were diagnosed more than 10 years after US entry. Among persons entering the country later in childhood or during adolescence, increasing proportions of TB cases were diagnosed more than 1 year after US entry. These findings highlight the need for strategies to implement screening both in the period immediately after immigration and in subsequent years for foreign-born children and adolescents from countries with a large TB burden. TB prevention and control should be enhanced with resources to conduct testing and treatment interventions for populations at high risk for TB and with collaborative research and programs to improve case management, contact investigation, and treatment and diagnostic tools.1
Unfortunately, data reported to the NTSS during the study period did not include information on parents' place of birth or on travel to TB-endemic areas; therefore, we could not ascertain whether US-born children and adolescents of foreign-born parents might be at higher risk for TB because of travel or family history. No data were available on TB screening prior to US entry or on adoption to the United States. Data were also not available for how TB cases were identified—as part of a contact investigation, by targeted testing for TB, or by evaluation of clinical signs and symptoms suggestive of TB. As a result, we could not identify at a national level how successful efforts to screen children and adolescents at risk for TB are and what missed opportunities might exist.
Revisions to the RVCT form could play a critical role in this area. This form, used by local and state TB programs to report cases of TB to the NTSS, was revised in 2008, and implementation of the new form began in January 2009. Key changes include, for all TB cases, the addition of measures to identify source cases or previous TB episodes, primary reason evaluated for TB (e.g., contact with an infectious person, incomplete treatment of latent TB, targeted testing, or symptoms), and country of birth (including persons classified as US born who were born overseas). For TB cases in persons younger than 15 years at diagnosis, the revised form also records country of birth for primary guardians (parents or guardians) and travel history (for those who have lived outside the United States for more than 2 months).17 As data are collected through the revised RVCT, we will be better able to assess the effect of efforts to reduce TB among foreign-born children and adolescents and to identify additional opportunities for intervention among children and adolescents who travel to countries with a large TB burden and among US-born children and adolescents whose foreign-born parents are from these countries.
Improving our understanding of TB among children and adolescents is critical to the goal of TB elimination and an essential step toward ensuring that children will no longer suffer from this preventable disease. Our efforts to eliminate childhood TB will pay dividends far into the future.
Acknowledgments
We acknowledge the local and state TB programs, which are the sources of all reported TB data, and the surveillance team of the Surveillance, Epidemiology, and Outbreak Investigations Branch of the Division of Tuberculosis Elimination for their support of this work.
Human Participant Protection
The protocol for this project was reviewed by the Centers for Disease Control and Prevention and determined to be public health surveillance and not human participants research requiring oversight by an institutional review board.
References
- 1.Trends in tuberculosis—United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58(10):249–253 [PubMed] [Google Scholar]
- 2.Cain KP, Benoit SR, Winston CA, Mac Kenzie WR. Tuberculosis among foreign-born persons in the United States. JAMA. 2008;300(4):405–412 [DOI] [PubMed] [Google Scholar]
- 3.Global Tuberculosis Control: Epidemiology, Strategy, Financing. WHO Report 2009. Geneva, Switzerland: World Health Organization; 2009. WHO/HTM/TB/2009.411. Available at: http://www.who.int/tb/publications/global_report/2009/en/index.html. Accessed April 23, 2010 [Google Scholar]
- 4.Nelson LJ, Wells CD. Global epidemiology of childhood tuberculosis. Int J Tuberc Lung Dis. 2004;8(5):636–647 [PubMed] [Google Scholar]
- 5.Marais BJ, Obihara CC, Warren RM, Schaaf HS, Gie RP, Donald PR. The burden of childhood tuberculosis: a public health perspective. Int J Tuberc Lung Dis. 2005;9(12):1305–1313 [PubMed] [Google Scholar]
- 6.Marais BJ. Tuberculosis in children. Pediatr Pulmonol. 2008;43(4):322–329 [DOI] [PubMed] [Google Scholar]
- 7.Feja K, Saiman L. Tuberculosis in children. Clin Chest Med. 2005;26(2):295–312, vii [DOI] [PubMed] [Google Scholar]
- 8.Marais BJ, Gie RP, Schaaf HS, et al. The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004;8(4):392–402 [PubMed] [Google Scholar]
- 9.Guidance for National Tuberculosis Programmes on the Management of Tuberculosis in Children. Geneva, Switzerland: World Health Organization; 2006. WHO/HTM/TB/2006.371. Available at: http://whqlibdoc.who.int/hq/2006/WHO_HTM_TB_2006.371_eng.pdf. Accessed April 23, 2010 [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention Reported tuberculosis in the United States, 2007. 2008. Available at: http://www.cdc.gov/tb/statistics/reports/2007/default.htm. Accessed November 27, 2009
- 11.Donald PR, Maher D, Qazi S. A Research Agenda for Childhood Tuberculosis. Geneva, Switzerland: World Health Organization, 2007. WHO/HTM/TB/2007.381. Available at: http://whqlibdoc.who.int/hq/2007/WHO_HTM_TB_2007.381_eng.pdf. Accessed April 23, 2010 [Google Scholar]
- 12.CDC Immigration Requirements: Technical Instructions for Tuberculosis Screening and Treatment. Atlanta, GA: Centers for Disease Control and Prevention; 2007. Available at: http://www.cdc.gov/immigrantrefugeehealth/exams/ti/panel/tuberculosis-panel-technical-instructions.html. Accessed April 23, 2010 [Google Scholar]
- 13.US Census Bureau Current Population Survey. Annual estimates of the United States foreign-born and native resident populations. 2008. Available at: http://dataferrett.census.gov. Accessed January 22, 2009
- 14.Hoeffer M, Rytina N, Baker BC. Estimates of the unauthorized immigrant population residing in the United States: January 2007. Washington, DC: US Dept of Homeland Security, Office of Immigration Statistics; 2008. Available at: http://www.dhs.gov/xlibrary/assets/statistics/publications/ois_ill_pe_2007.pdf. Accessed April 23, 2010 [Google Scholar]
- 15.US Dept of State Intercountry adoption: total adoptions to the United States. Washington, DC: US Dept of State, Office of Children's Issues, 2009. Available at: http://adoption.state.gov/news/total_chart.html. Accessed February 17, 2009 [Google Scholar]
- 16.Pediatric Tuberculosis Collaborative Group Targeted tuberculin skin testing and treatment of latent tuberculosis infection in children and adolescents. Pediatrics. 2004;114:1175–1201 [Google Scholar]
- 17.Centers for Disease Control and Prevention The revised Report of Verified Case of Tuberculosis fact sheet. 2009. Available at: http://www.cdc.gov/tb/publications/factsheets/statistics/rvct.htm. Accessed February 17, 2009