Abstract
Objectives. We compared completion rates for adolescent immunization series administered at school-based health centers (SBHCs) to completion rates for series administered at community health centers (CHCs) within a single integrated delivery system.
Methods. We performed a retrospective analysis of data from an immunization registry for patients aged 12–18 years. Patients were assigned to either an SBHC or a CHC during the study interval based on utilization. We used bivariate analysis to compare immunization series completion rates between the 2 groups and multivariate analysis to compare risk factors for underimmunization. We performed subanalyses by ages 12–15 years versus ages 16–18 years for human papillomavirus (HPV) and for the combination of HPV; tetanus, diptheria, and pertussis (Tdap); and tetravalent meningococcus virus.
Results. SBHC users had significantly higher completion rates (P < .001) for hepatitis B, Tdap, inactivated poliovirus, varicella, measles/mumps/rubella, and HPV for ages 16–18 years, and for the combination of HPV, Tdap, and MCV4 for ages 16–18 years. CHC users had higher completion rates for tetanus and diphtheria.
Conclusions. SBHCs had higher completion rates than did CHCs for immunization series among those aged 12–18 years, despite serving a population with limited insurance coverage.
Immunizations have been a cornerstone of pediatric preventive care for decades, especially for infectious disease prevention in infants and young children. New vaccine developments have made it possible to administer vaccines against specific preventable diseases in children and adolescents, such as the tetravalent meningococcus virus (MCV4) vaccine and the human papillomavirus (HPV) vaccine, and to boost resistance to tetanus, diptheria, and pertussis (the Tdap vaccine). Recommended vaccines include single-dose regimens and multidose series. It is crucial to deliver these vaccines either before existing immunity wanes or before the risk of exposure.1,2
Immunizing children and adolescents presents challenges within our current system of health care delivery. This is true for all immunizations but particularly so for the administration of multidose vaccine series. Numerous authors have identified systemic, parental, and patient barriers to vaccine administration.3–8 School-based health centers (SBHCs), primary care clinics located in schools, have been shown to improve rates of child and adolescent immunization.9,10 SBHCs are an optimal model for delivery of adolescent primary care around the country, and many SBHCs currently deliver immunizations.11 However, little is known about the success of this model in completing vaccine series.
In a retrospective analysis, we examined immunization series completion rates of children and adolescents aged 12 to 18 years within an integrated health care system that delivered care via both SBHCs and community health centers (CHCs). We compared the completion rates of patients who received care primarily through SBHCs with the completion rates of patients who received care primarily through CHCs.
METHODS
Denver Health is an integrated multilevel health system that includes 8 community health centers and 12 SBHCs in addition to inpatient and emergency care provided in the hospital setting. Patients seen throughout the system are registered in a central database. As a result, the same immunization registry is shared across all sites of care. All data are stored by site of care via site-specific registration codes.
Study Design
We conducted a retrospective cohort analysis of children and adolescents who received care within the Denver Health system. We obtained data from the Denver Health immunization registry and administrative database.
We selected all patients who were aged 12 to 18 years at the time of their last visit to a Denver Health CHC or SBHC during the study interval, which lasted from August 1, 2006, through July 31, 2008. We calculated the total number of visits these patients made within the Denver Health system during the study interval. Patient primary language, race/ethnicity, and gender were self-identified. Because of the low number of patients who spoke neither English nor Spanish, we used English, Spanish, and other as the primary language categories. We used billing data to determine payer source (insured, uninsured, and unknown). The insured category was further divided into private, Medicaid, and Child Health Plan Plus (Colorado's state child health plan).
All individuals were placed initially into 1 of 3 categories: exclusively SBHC users, exclusively CHC users, or both SBHC and CHC users. For patients who used both clinical settings, we decided a priori to classify them into either the SBHC group or the CHC group, depending on which clinic they used the most. Thus, all patients were ultimately classified as either SBHC users or CHC users. Vaccine records were analyzed to determine which patients had completed each of the recommended immunization series. Individuals were considered to be up to date if the appropriate number of vaccinations were obtained for each immunization as recommended by the Advisory Committee on Immunization Practices.2
Data Analysis
A bivariate analysis was conducted to compare immunization series completion rates of SBHC users with immunization series completion rates of CHC users. Individual multivariate logistic regression was also conducted to control for other factors contributing to immunization series completion. We used the following variables for this analysis: age, number of visits, primary language, race/ethnicity, gender, payer source, and site of care. Finally, we performed a subanalysis to assess series completion rates for the vaccines specific to female adolescents: HPV/Tdap/MCV4 (i.e., 3-1-1) and HPV alone. For this subanalysis, patients were stratified by age into 2 groups: ages 12 to 15 years and ages 16 to 18 years. This subanalysis consisted of an additional multivariate logistic regression limited to females, stratified by the age groupings listed above, and stratified by the remaining confounders used in the initial regression.
We assessed all multivariate models for multicollinearity by analysis of eigenvalues, and we assessed tolerance and goodness of fit on the basis of case profile deletion statistics. None of the models were subject to multicollinearity on the basis of exceeding minimum standard thresholds. Graphical interpretation of Pearson residuals and deviance residuals versus estimated probability did not reveal any systematic patterns of variation. All individual observations with large residuals were examined; these were not excluded from the models because the covariate values were feasible. Analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC).
RESULTS
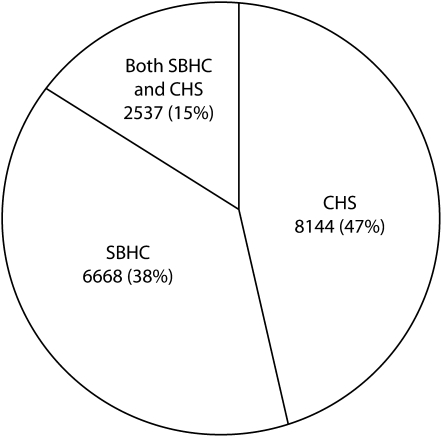
There were 17 349 children and adolescents aged 12 to 18 years who received care in the Denver Health system during the study interval: 8144 (47%) at CHCs, 6668 (38%) at SBHCs, and 2537 (15%) at both (Figure 1). After those who used both sites were classified on the basis of which site they visited the most, there were 9132 (53%) CHC users and 8217 (47%) SBHC users.
FIGURE 1.
Study sample by primary site of care: patients aged 12–18 years, Denver Health system, 2006–2008.
Note. SBHC = school-based health center; CHC = community health center.
Patients in both site categories were similar in age, but other patient characteristics differed significantly between the categories (Table 1). CHC patients were more likely to be female (57% vs 52%; P < .001), whereas SBHC patients were more likely to have multiple visits (73% vs 66%; P < .001), be Hispanic (72% vs 64%; P < .001), and be uninsured (43% vs 3%; P < .001).
TABLE 1.
Demographic Characteristics: Patients Aged 12–18 Years, Denver Health System, 2006–2008
| Primary Site of Care |
|||
| SBHC (n = 8317), % | CHC (n = 9032), % | P valuea | |
| Age, y | < .001 | ||
| 12 | 12.05 | 15.05 | |
| 13 | 14.64 | 13.44 | |
| 14 | 18.16 | 13.74 | |
| 15 | 17.16 | 13.90 | |
| 16 | 15.43 | 14.77 | |
| 17 | 15.29 | 15.30 | |
| 18 | 7.27 | 13.81 | |
| Gender | < .001 | ||
| Male | 48.02 | 42.91 | |
| Female | 51.98 | 57.09 | |
| Primary language | < .001 | ||
| English | 64.16 | 65.01 | |
| Spanish | 34.12 | 31.91 | |
| Other/unknown | 1.72 | 3.08 | |
| Race/ethnicity | < .001 | ||
| White | 8.28 | 8.82 | |
| Black | 11.80 | 19.54 | |
| Hispanic | 71.66 | 64.16 | |
| Other/unknown | 8.26 | 7.47 | |
| Payer source | < .001 | ||
| Insured | 50.46 | 94.22 | |
| Uninsured | 43.00 | 3.01 | |
| Unknown | 6.54% | 2.77 | |
| No. visits | < .001 | ||
| 1 | 26.85 | 34.70 | |
| 2 | 19.44 | 20.47 | |
| 3–5 | 31.41 | 27.15 | |
| > 5 | 22.30 | 17.68 | |
Note. SBHC = school-based health center; CHC = community health center.
By the χ2 test.
Children and adolescents seen in SBHCs were more likely to be up to date for the following immunizations: hepatitis B (vs 84%; P < .001), Tdap (71% vs 62%; P < .001), varicella (20% vs 13%; P < .001), measles/mumps/rubella (89% vs 83%; P < .001), HPV for patients aged 16 to 18 years (18% vs 12%; P < .001), and the HPV/Tdap/MCV4 immunization series for female patients aged 16 to 18 years (17% vs 11%; P < .001) (Table 2). SBHC users were more likely to complete series that required multiple doses (hepatitis B, Tdap, varicella, and HPV for patients aged 16 to 18 years), with the exception of hepatitis A. CHC users were more likely to be up to date for tetanus/diphtheria vaccinations. There were no differences by site of care for hepatitis A or MCV4 vaccinations. After using multivariate analysis to adjust for demographic and socioeconomic factors, we found no change in the differences noted above in up-to-date rates by site of care, except for HPV, which was affected by age. SBHCs appeared to be a favorable site for HPV vaccination (unadjusted odds ratio [OR] = 1.20; 95% confidence interval [CI] = 1.07, 1.34). The effect was not seen when adjusting for age and the other covariates (OR = 1.03; 95% CI = 0.90, 1.18).
TABLE 2.
Vaccination Completion Rates by Primary Site of Care: Patients Aged 12–18 Years, Denver Health System, 2006–2008
| Unadjusted Analysis |
Adjusted Analysisa |
|||||
| Vaccinations | SBHC, % | CHC, % | OR (95% CI) | P value | OR (95% CI) | P value |
| Hepatitis A | 54.29 | 50.32 | 1.17 (1.10, 1.24) | < .001 | 1.04 (0.97, 1.12) | .25 |
| Hepatitis B | 92.83 | 83.90 | 2.49 (2.25, 2.75) | < .001 | 2.56 (2.25, 2.90) | < .001 |
| Td | 49.12 | 53.42 | 0.84 (0.79, 0.89) | < .001 | 0.81 (0.75, 0.87) | < .001 |
| Tdap | 71.12 | 61.66 | 1.53 (1.44, 1.63) | < .001 | 1.36 (1.25, 1.47) | < .001 |
| MCV4 | 64.13 | 61.06 | 1.14 (1.07, 1.21) | < .001 | 0.99 (0.92, 1.07) | .83 |
| IPV | 94.84 | 84.92 | 3.27 (2.92, 3.66) | < .001 | 3.05 (2.66, 3.51) | < .001 |
| Varicella | 19.72 | 12.93 | 1.65 (1.52, 1.79) | < .001 | 1.7 (1.54, 1.86) | < .001 |
| MMR | 89.19 | 82.86 | 1.71 (1.56, 1.86) | < .001 | 1.61 (1.45, 1.79) | < .001 |
| HPVb | 17.53 | 15.07 | 1.2 (1.07, 1.34) | < .001 | 1.03 (0.90, 1.18) | .66 |
| Patients aged 12–15 y | 17.16 | 18.13 | 0.94 (0.84, 1.08) | .36 | 0.71 (0.59, 0.85) | < .001 |
| Patients aged 16–18 y | 18.09 | 12.13 | 1.6 (1.35, 1.89) | < .001 | 1.67 (1.37, 2.05) | < .001 |
| HPV/Tdap/MCV4b | ||||||
| Patients aged 12–15 y | 16.62 | 17.70 | 0.93 (0.80, 1.07) | 0.31 | 0.7 (0.58, 0.84) | < .001 |
| Patients aged 16–18 y | 17.34 | 11.44 | 1.62 (1.37, 1.93) | < .001 | 1.69 (1.38, 2.08) | < .001 |
Note. SBHC = school-based health center; CHC = community health center; OR = odds ratio; CI = confidence interval; Td = tetanus/diphtheria; Tdap = tetanus/diphtheria/pertussis; MCV4 = tetravalent meningococcus virus; IPV = inactivated poliovirus; MMR = measles/mumps/rubella; HPV = human papillomavirus.
Adjusted for age, gender, primary language, race/ethnicity, payer source, number of visits in prior 2 years, and modeling the likelihood of vaccination for SBHC compared with the likelihood of vaccination for CHC.
Limited to females; adjusted analysis is not further adjusted for gender or age (stratified analysis only).
DISCUSSION
In this analysis of an urban integrated health delivery system, we found SBHCs to be superior to CHCs as a setting for completion of adolescent immunization series, even after adjusting for significant demographic differences. Children and adolescents who used SBHCs and CHCs in the same health delivery system and who initiated a vaccine series were more likely to complete the series if they primarily used SBHCs as opposed to primarily using CHCs. Likewise, children and adolescents were also more likely to have received single-dose vaccines if they were SBHC patients. These findings are paradoxical, because 43% of the SBHC users were uninsured. Both settings reported up-to-date rates that exceeded many national estimates. Compared with the most recent national estimates, up-to-date rates were mixed in both settings.1
Our findings show that SBHCs may have the ability to overcome utilization barriers in a way not previously documented in other clinical settings, even when serving populations that suffer from significant health disparities. Both of the clinic settings we analyzed serve a large urban population that is primarily Latino. Many of these patients do not speak English; most of them have insurance coverage through a public entity (Medicaid or SCHIP) or are uninsured. Each of these characteristics has been associated with poor access to care.12,13
Additionally, our study focused on children and adolescents within this high-risk population. Although vaccine rates are more poorly documented for this age group than for others, most assessments suggest that adolescents are at risk for underimmunization.1,14 Our findings suggest that SBHCs may provide a particular benefit in terms of helping older adolescents complete the HPV/Tdap/MCV4 vaccine series, which is initiated during the teen years. Although recent findings suggest improvements in the completion rates of these vaccines, our study indicates that there may be an advantage in using the SBHC setting to deliver this series. In our analysis, SBHC users had Tdap and MCV4 rates that were far superior to national rates and HPV completion rates that were at least equal.1
Strengths and Limitations
One strength of our study is its large sample size of more than 17 000 adolescents. In addition, the sample population was part of a larger population that experiences many health disparities.
The methodology used to assign patients who had visited both kinds of clinics to a clinic site was decided a priori, but our analysis represents a snapshot in time. There was no intention-to-treat analysis performed. Therefore, it is possible that up-to-date rates in both categories are underrepresented.
Not all SBHCs are vertically integrated into larger health systems, as were the SBHCs in this study, so our findings may not be generalizable to all SBHCs. Likewise, not all SBHCs can bill at the same rate, and some cannot bill at all. Our study took place in clinic settings that bill as Federally Qualified Health Centers, a status that maximizes Medicaid payment.
Overcoming Barriers to Adolescent Immunization
Researchers have postulated a number of barriers to immunizing adolescents.3–8 These barriers can be classified as health care system barriers, parental barriers, and adolescent barriers. Health care system barriers include inconsistent policies guiding administration of vaccine recommendations, incomplete implementation of recommendations to include administration of vaccine to adolescents during routine visits, providers not providing vaccine, providers lacking sufficient time to assess immunization status, the high cost of vaccine, low remuneration for administering vaccines, lack of health insurance coverage, lack of access to care, missed opportunities when the health care system is accessed, provider discomfort in providing care to adolescents, adolescents accessing multiple providers, and the lack of a registry or other system to determine patients' immunization needs.3–8 Parental barriers include a perception of adolescents being in good health and thus not requiring health care, parents' inability to miss work to take adolescents to care providers, lack of insurance, lack of awareness of vaccine benefits, distrust of vaccines, and the perception that there are too many vaccines from which to choose.3–5 Barriers for adolescents include adolescent-specific cognitive developmental stages when they may be less accepting of recommendations, distrust of vaccines, lack of confidential services, discomfort with provider, lack of awareness, perception of good health not requiring vaccination, lack of insurance, and need for parental consent when adolescents are seen independently.3–5,8
Strategies to address the administration of vaccines to children and adolescents have evolved as more adolescent-specific vaccines have come to market. SBHCs offer a unique setting that offsets at least some of the barriers to adolescent immunization. For example, many SBHCs deliver immunizations free of charge, target medically underserved youth (many of whom are uninsured or underinsured), eliminate the need for parents to miss work, and offer a setting that young persons trust and where they feel safe.11 Also, SBHCs can capitalize on the fact that students attend school on a daily basis and are therefore a “captive audience.” This might be a reason for the success of the SBHC model of immunization delivery. Likewise, SBHCs are ideal for the use of immunization registries, which have been shown to be an effective strategy for populations who receive health care at multiple sites.15,16
There is much to be learned from the successes of infant and toddler vaccination. For example, the practice of making frequent visits to a primary care provider for anticipatory guidance and linked immunizations is not well established among adolescents. Younger adolescents make only a small number of visits to pediatricians for primary preventive care, and older adolescents make even fewer visits.17 Routine preventive care visits and an immunization registry are strategies used to address the challenges of effectively administering multidose vaccine series.18
SBHCs have been found to enhance overall access to care.10 Additionally, SBHC patients have been found to make more primary care visits to SBHCs than to pediatricians, family practices, or community health centers; to be less likely to be insured; and to be more likely to have received a preventive care visit including immunizations.9 SBHCs are uniquely positioned to overcome traditional barriers because they are more likely to be located in schools that enroll low-income adolescents and that serve racially and ethnically diverse student populations. SBHCs have the infrastructure, resources, and on-site primary care providers necessary for the provision of comprehensive primary care services.11
Conclusions
There are a number of reasons why SBHCs may be superior to CHCs as a setting for delivering vaccines to traditionally underserved populations. First, SBHCs can see patients for multiple visits much more easily than CHCs can (the “captive audience” phenomenon). Given the difficulty that our study population faces in accessing care (including follow-up), the ability to provide multiple visits cannot be overstated. A related advantage is SBHCs' ability to institute a reminder recall system. This methodology has been well documented as a way to improve series completion.11 Instituting a reminder recall system may be more achievable within an SBHC setting because SBHCs serve a patient population that is finite and limited in its ability to migrate. It may also be easier to institute a tracking system within a school setting.
SBHCs vary greatly in their financial structures, but many (including the ones in this study) see patients regardless of their ability to pay. This characteristic of SBHCs eliminates cost as a barrier to immunization delivery. Finally, SBHCs can eliminate barriers to care delivery that other settings do not address. For example, SBHCs do not require parents to miss work or find transportation to and from a clinical setting. Also, patients' time away from class can be minimized because they do not need to leave campus to receive services.
Many SBHCs lack the appropriate funding to create sustainable programs, much less plan for expansion. Currently, there are no federal dollars specifically dedicated to the operational costs of SBHCs. Many private payers and some public programs do not reimburse for services received within SBHCs. New policies should be promoted to enhance the financial viability of SBHCs, allowing them to expand and deliver more care, including immunizations to children, adolescents, and other underserved populations.
Acknowledgments
We thank Carolyn Jagunich for her assistance with data analysis and Matt Daley, MD, for his critique of the article.
Human Participant Protection
The institutional review board of the University of Colorado Health Sciences Center approved this study protocol.
References
- 1.Centers for Disease Control and Prevention National, state, and local area vaccination coverage among adolescents aged 13–17 years—United States, 2008. MMWR Morb Mortal Wkly Rep. 2009;58(36):997–1001 [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics Committee on Infectious Diseases Recommended childhood and adolescent immunization schedules—United States, 2009. Pediatrics. 2009;123(1):189–190 [DOI] [PubMed] [Google Scholar]
- 3.Brabin L, Greenberg DP, Hessel L, Hyer R, Ivanoff B, Van Damme P. Current issues in adolescent immunization. Vaccine. 2008;26(33):4120–4134 [DOI] [PubMed] [Google Scholar]
- 4.Broder KR, Cohn AC, Schwartz B, et al. Adolescent immunizations and other clinical preventive services: a needle and a hook? Pediatrics. 2008;121(suppl 1):S25–S34 [DOI] [PubMed] [Google Scholar]
- 5.Ford CA, English A, Davenport AF, Stinnett AJ. Increasing adolescent vaccination: barriers and strategies in the context of policy, legal, and financial issues. J Adolesc Health. 2009;44(6):568–574 [DOI] [PubMed] [Google Scholar]
- 6.Lindley MC, Boyer-Chu L, Fishbein DB, et al. The role of schools in strengthening delivery of new adolescent vaccinations. Pediatrics. 2008;121(suppl 1):S46–S54 [DOI] [PubMed] [Google Scholar]
- 7.Schaffer SJ, Fontanesi J, Rickert D, et al. How effectively can health care settings beyond the traditional medical home provide vaccines to adolescents? Pediatrics. 2008;121(suppl 1):S35–S45 [DOI] [PubMed] [Google Scholar]
- 8.Szilagyi PG, Rand CM, McLaurin J, et al. Delivering adolescent vaccinations in the medical home: a new era? Pediatrics. 2008;121(suppl 1):S15–S24 [DOI] [PubMed] [Google Scholar]
- 9.Allison MA, Crane LA, Beaty BL, Davidson AJ, Melinkovich P, Kempe A. School-based health centers: improving access and quality of care for low-income adolescents. Pediatrics. 2007;120(4):e887–e894 [DOI] [PubMed] [Google Scholar]
- 10.Deuson RR, Hoekstra EJ, Sedjo R, et al. The Denver school-based adolescent hepatitis B vaccination program: a cost analysis with risk simulation. Am J Public Health. 1999;89(11):1722–1727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daley MF, Curtis CR, Pyrzanowski J, et al. Adolescent immunization delivery in school-based health centers: a national survey. J Adolesc Health. 2009;45(5):445–452 [DOI] [PubMed] [Google Scholar]
- 12.Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for Latino children. Arch Pediatr Adolesc Med. 1998;152(11):1119–1125 [DOI] [PubMed] [Google Scholar]
- 13.Flores G, Fuentes-Afflick E, Barbot O, et al. The health of Latino children: urgent priorities, unanswered questions, and a research agenda. JAMA. 2002;288(1):82–90 [DOI] [PubMed] [Google Scholar]
- 14.Rodewald LE, Orenstein WA. Vaccinating adolescents—new evidence of challenges and opportunities. J Adolesc Health. 2009;45(5):427–429 [DOI] [PubMed] [Google Scholar]
- 15.Kempe A, Beaty BL, Steiner JF, et al. The regional immunization registry as a public health tool for improving clinical practice and guiding immunization delivery policy. Am J Public Health. 2004;94(6):967–972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilcox SA, Koepke CP, Levenson R, Thalheimer JC. Registry-driven, community-based immunization outreach: a randomized controlled trial. Am J Public Health. 2001;91(9):1507–1511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rand CM, Shone LP, Albertin C, Auinger P, Klein JD, Szilagyi PG. National health care visit patterns of adolescents: implications for delivery of new adolescent vaccines. Arch Pediatr Adolesc Med. 2007;161(3):252–259 [DOI] [PubMed] [Google Scholar]
- 18.Nelson JC, Bittner RC, Bounds L, et al. Compliance with multiple-dose vaccine schedules among older children, adolescents, and adults: results from a vaccine safety datalink study. Am J Public Health. 2009;99(suppl 2):S389–S397 [DOI] [PMC free article] [PubMed] [Google Scholar]