Abstract
Objectives. We examined whether improvements in pediatric health-related quality of life (HRQOL) stemming from use of school-based health centers (SBHCs) resulted in lower Medicaid costs.
Methods. We analyzed data on 290 students from a 3-year, longitudinal SBHC evaluation conducted in Cincinnati, Ohio, in 2000 to 2003, including 71 with a mental health diagnosis and 31 with asthma, who had linked Ohio Medicaid records. HRQOL was measured using the Pediatric Quality of Life Inventory. Panel regression examined whether changes in parent-reported and student self-reported HRQOL predicted changes in Medicaid costs.
Results. After adjustment for gender, age, SBHC status, and Medicaid type, we found cost reductions for every 1-point increase of parent-reported total ($36.39; P < .01), physical ($35.36; P < .05), and psychosocial ($25.94; P < .01) HRQOL. Significant cost reductions were also associated with student-reported total ($8.94; P < .05) and psychosocial ($7.79; P < .05) HRQOL increases. These effects were significant among the asthma subgroup but not the mental health subgroup. Physical HRQOL ($6.12; P = .27) effects were not significant.
Conclusions. Improvements in pediatric HRQOL translate into lower Medicaid costs, supporting the use of HRQOL as an outcome for evaluating SBHCs.
School-based health centers (SBHCs) have steadily increased in numbers across the United States over the last 3 decades.1–4 The most recent SBHC census, conducted in 2004 to 2005 by the National Assembly of School Based Health Care, identified more than 1709 SBHC programs in the United States.4 This shift in the delivery of health care for children is premised on the assumption that access to health services in school increases access to health care and improves health status among children, especially for those children whose access to care is otherwise limited.5–9 Health status is often measured by health-related quality of life (HRQOL), which attempts to tap the current health perception of individuals.
HRQOL has been demonstrated in both social scientific and clinical research to predict future health status, health care utilization and costs, and even mortality.10–17 For example, a study linking the 1992 Medicare Current Beneficiary Survey with the 1993 Medicare Continuous History Survey found that a person's response to a self-rated health question accurately predicted that individual's respective use of health care services over the next year.15 Only a few studies, however, have examined the connection between HRQOL and health care utilization and health care cost savings among children.
The link between HRQOL and utilization among Canadian adolescents was examined by Vingilis et al. with a single measure of perceived general health status that asked children to rank their answer on a 5-point scale from excellent to poor.18 They found that reductions in perceived health over time were associated with increases in physician services and declines in dental care. This anomaly in usage across service providers may reflect differences between preventive dental care (representing the majority of dental services), which is not covered by publicly funded Canadian Medicare, and insured, curative health services.
Seid et al. examined how pediatric HRQOL predicted health care costs 6 months, 12 months, and 2 years after measurement.19 They used parent proxy reports of both physical and psychosocial children's HRQOL, as measured by the Pediatric Quality of Life Inventory (PedsQL), controlled for age, gender, and chronic health conditions, and found that lower ratings of physical HRQOL predicted significantly higher subsequent costs at every interval. Children with chronic health conditions generally accounted for the greatest proportion of subsequent health care spending. Notably, when the researchers broke down the PedsQL into its 2 dimensions, physical HRQOL and psychosocial HRQOL, they found that the latter was not significantly associated with health care spending, contradicting the theory that health perceptions among youth may extend beyond physical symptoms.13,18 Seid et al. conducted the most thorough assessment to date among youths, but they did not examine changes in HRQOL and changes in costs, and their reliance on parental proxy reports was a significant limitation.
Although these studies indicate a link between health perceptions, utilization, and cost, it is still not clear whether changes in perceived health status translate into changes in actual health care costs. We reexamined a prospective 3-year longitudinal study that used the PedsQL to assess whether changes in student self-reported HRQOL and parent proxy–reported pediatric HRQOL predicted changes in Medicaid medical claim expenses. This previous study found that students who used SBHCs showed improvements over time in self-reported HRQOL that were not seen in students who did not use SBHCs or students in comparison schools.20,21 We also separately analyzed disease-specific subgroups of children—those who had a diagnosis of asthma or mental health disorder—to determine whether a different relationship between HRQOL and health care costs existed for these groups.
METHODS
The data came from 2 studies, a health outcomes study21,22 and a Medicaid cost and utilization study,23–25 conducted during the 2000 to 2001 through 2002 to 2003 school years to evaluate the efficacy and efficiency of SBHCs in 2 school districts in the Greater Cincinnati, Ohio, area during their first 3 years of operation. Each SBHC was open Monday through Friday and operated during the school year from September to May. Any medical request during the weekend was directed to neighborhood health centers or other primary care physicians. SBHC staff included at least 1 nurse practitioner and a collaborating physician. All SBHCs provided mental health and psychiatric referrals, 3 provided behavior and mental health assessments and crisis intervention, and 2 provided individual counseling and had an on-site social worker or counselor. Full details on the structural attributes of each SBHC are available from the authors.
The health outcomes study examined changes in student HRQOL over 3 years across 4 school districts in the Greater Cincinnati and northern Kentucky area with SBHCs (7 schools in total) and 2 comparison school districts (6 schools in total) matched on urban–rural status, percentage of non-White students, and percentage of students participating in a free or reduced-price school lunch program (37–88%; mean = 63.5%).21 The health outcomes study conducted a survey of 1360 randomly selected parent–student pairs in year 1 stratified across SBHC schools and the matched comparison schools. Both parents and students were administered the PedsQL annually over the 3-year period.
The Medicaid cost study used Ohio school enrollment databases to identify student names and demographics for each school year from the intervention and comparison schools.23,24 Medicaid enrollment categories were aid for the disabled or blind, Aid to Families with Dependent Children, State Children's Health Insurance Plan, and Medicaid managed care organizations. Over the course of the study, the state insurance plan covered children with family incomes up to 200% of the federal poverty level. The school enrollment files were matched to the Ohio Medicaid claims database, yielding a study sample of 9240 unique students across the Ohio SBHC and comparison school districts. These records were linked to the Ohio Medicaid medical claims databases of those using Medicaid during these 3 years to identify a total of 5069 students. Thirteen students who switched between SBHC intervention and non-SBHC intervention schools within these 3 years were excluded from our analysis.
We linked the health outcomes survey data sources for parent proxy and student self-reported HRQOL assessments to the Medicaid claims data covering pharmacy, medical, hospital inpatient, emergency visit, and outpatient institutional claims.25 The resulting match yielded 290 students in year 1 with both parent and student HRQOL assessments (Table 1). Of these, we also identified 2 chronic illness subsamples of students from Medicaid claims data: 1 group with a mental health disorder and another group with asthma. The mental health subsample consisted of 71 students in year 1 with Medicaid diagnoses indicated by the International Classification of Disease, Ninth Revision Clinical Modification codes 290.XXX through 316.XXX.26 Mental health disorders included attention deficit hyperactive, depressive, conduct, emotional, adjustment, and other disorders. The asthma subgroup consisted of 39 students in year 1 who had Medicaid medical claim data with diagnoses indicated by the 493.XXX code in either hospital institutional or physician clinic medical claims. The sample sizes for all groups decreased every year through attrition and varied across parent proxy and student self-reported HRQOL. However, a previous analysis of overall attrition of the health outcomes survey sample indicated no significant difference in previous HRQOL scores between those retained in the sample and those lost to follow-up across SBHC groups.21
TABLE 1.
Longitudinal Combined Analysis of Medicaid Costs From 2 Studies of School-Based Health Centers: Health Outcomes Study and Medicaid Cost Study, Greater Cincinnati Area, Ohio, and Northern Kentucky, 2000–2003
| Year 1 |
Year 2 |
Year 3 |
||||
| No. Students/No. Parents | Medicaid Health Care Costs, $, Mean (SD) | No. Students/No. Parents | Medicaid Health Care Costs, $, Mean (SD) | No. Students/No. Parents | Medicaid Health Care Costs, $, Mean (SD) | |
| Total sample | 290/290 | 1077 (2829) | 247/283 | 1400 (3405) | 146/151 | 1197 (2012) |
| Asthma subsample | 39/39 | 1735 (2063) | 34/42 | 1452 (1561) | 29/29 | 1501 (2179) |
| Mental health subsample | 71/71 | 1721 (1874) | 67/74 | 2622 (5358) | 41/42 | 2193 (2892) |
Note. Sample size for costs was based on parent reports for each year.
Measures
Annual total health care reimbursement per student was defined as the total dollar amount that Medicaid paid for emergency, inpatient, and outpatient care; physician encounters; mental health services; prescription drugs; laboratory procedures; and diagnoses during each school year. For each Medicaid claim reimbursement during these 3 years, we adjusted total health care reimbursement by the medical component of the Consumer Price Index as the dollar value in 2003 according to data from the Bureau of Labor Statistics. For this study, we calculated the inflation-adjusted discount rate with a 3% discount rate and each annual index rate.27 These annual rates of change were 4.6% in 2002, 4.7% in 2001, and 4.2% in 2000.28,29 We extracted the total costs for all services from the Medicaid medical claims database for September 2000 to May 2003. Because of delays for medical claims processing and the implementation of the Health Insurance Portability and Accountability Act regulation changes, we were unable to collect Medicaid claims data for June 2003 to August 2003, resulting in only 9 months of Medicaid data for year 3. To adjust for this, we estimated the sum of total costs for the final full year to be the total in the first 3 quarters multiplied by 4 and then divided by 3 for the time series repeated measures.
Pediatric HRQOL was assessed annually from 2000 to 2003 with the 23-item PedsQL, version 4.0, a field-tested, age-standardized tool designed for use with community and school populations.30–32 Parents completed an annual telephone questionnaire that included the proxy PedsQL measure of their child as well as additional demographic data. Students were administered the PedsQL in person at their school by the SBHC evaluation project staff. The PedsQL provides a measure of students’ overall HRQOL in a range from 0 to 100, which can also be decomposed into a physical (8 items) and a psychosocial (15 items) dimension. The reliability coefficients for the scales for both students and parent proxies were consistent with previous work.30,31 The minimal clinically important differences on the PedsQL 4.0 for the total scale and the physical and psychosocial dimensions are 4.36, 6.66, and 5.30 for student self-report and 4.50, 6.92, 5.49 for parent report, respectively.31
Covariates included child age as of September 30, 2002, which was treated as a constant within individuals over time. Gender was also coded as a dichotomous variable and treated as a constant over time. Medicaid type was coded as a categorical variable to separate children on the State Children's Health Insurance Plan from children on Medicaid as a proxy measure for household income. SBHC status was coded as 2 categorical variables to compare students in schools in which there was a SBHC who had used the SBHC services at least once in the 3-year study period with students in the SBHC schools who did not use the services and with students in the comparison schools.
Data Analysis
The cost-effectiveness analysis measured changes in costs in dollars associated with changes in HRQOL scores over the 3 years. This measure has been widely used for health care decision-making.27 We computed general linear panel regression models so as to examine changes in total Medicaid costs predicted separately by parent proxy–reported and student self-reported total PedsQL score as well as across individual physical health and psychosocial health dimensions. This technique treats missing data in a pairwise fashion, maximizing the number of respondent-by-time data points in the analysis. We adjusted all regression models for student age, gender, Medicaid type, and SBHC status. The regression coefficient for HRQOL represented the dollar change in Medicaid costs for every 1-point change in the PedsQL.
To assess whether the relationship between Medicaid costs and the PedsQL differed across SBHC groups, we examined an additional set of regression equations for parent and student reports testing a multiplicative term between PedsQL score and SBHC group. For all analyses, we used SAS 9.1 PROC GENMOD, specifying a normal distribution for total costs.33
RESULTS
For the annual Medicaid costs incurred, the total sample averaged $1077 in year 1, $1400 in year 2, and $1197 in year 3 (Table 1). Both the mental health and asthma subsamples had higher year 1 costs than did the total sample, but they were very similar to one another. In year 2, Medicaid costs for the mental health subsample rose sharply, and the costs for the asthma subsample declined to a level similar to that of the total sample. In year 3, Medicaid costs for the mental health subsample declined slightly but remained higher than in year 1, and the costs for the asthma subsample increased just slightly from year 2 but remained below the costs for year 1.
Table 2 presents the total, physical, and psychosocial PedsQL scores for both parent proxy ratings and student self-reports across time for the total sample as well as for each subsample. For the total sample, parent ratings were higher than were student self-ratings across all measures and across each year. Moreover, both parents and students rated their physical health higher than their psychosocial health. In the mental health subsample, this pattern was present but less pronounced in years 1 and 2. In year 3, however, parent ratings were consistently lower than were their children's ratings across all measures of the PedsQL. In the subsample diagnosed with asthma, the pattern was consistent with the total sample across all measures and years.
TABLE 2.
Parent-Reported and Student Self-Reported Health-Related Quality of Life Scores, by Year: Health Outcomes Study, Greater Cincinnati Area, Ohio, and Northern Kentucky, 2000–2003
| Health-Related Quality of Life | Year 1, Mean (SD) | Year 2, Mean (SD) | Year 3, Mean (SD) |
| Total sample | |||
| Parent proxy report | |||
| Total | 82.40 (14.06) | 78.67 (14.82) | 79.88 (14.14) |
| Physical | 88.68 (14.59) | 85.55 (15.69) | 86.63 (16.22) |
| Psychosocial | 79.06 (16.12) | 74.98 (16.65) | 76.27 (15.60) |
| Student self-report | |||
| Total | 73.36 (15.33) | 73.44 (15.57) | 76.74 (14.64) |
| Physical | 80.52 (16.01) | 81.26 (16.63) | 84.14 (14.89) |
| Psychosocial | 69.55 (17.46) | 69.27 (17.49) | 72.78 (16.33) |
| Mental health subsample | |||
| Parent proxy report | |||
| Total | 76.29 (16.34) | 71.93 (16.49) | 73.80 (14.55) |
| Physical | 85.32 (17.51) | 80.91 (18.61) | 83.32 (18.50) |
| Psychosocial | 71.48 (18.31) | 67.14 (17.93) | 68.70 (16.60) |
| Student self-report | |||
| Total | 74.37 (16.64) | 71.39 (17.97) | 75.58 (17.06) |
| Physical | 82.43 (17.41) | 80.88 (18.99) | 85.37 (17.02) |
| Psychosocial | 70.07 (18.51) | 66.34 (20.24) | 70.37 (19.57) |
| Asthma subsample | |||
| Parent proxy report | |||
| Total | 81.24 (15.71) | 76.64 (13.21) | 78.64 (13.43) |
| Physical | 86.55 (16.20) | 79.78 (15.97) | 83.17 (14.22) |
| Psychosocial | 78.44 (17.52) | 74.95 (14.58) | 76.21 (14.83) |
| Student self-report | |||
| Total | 75.47 (14.02) | 72.57 (13.09) | 74.70 (13.35) |
| Physical | 82.93 (12.16) | 78.95 (15.43) | 82.22 (16.18) |
| Psychosocial | 71.50 (16.56) | 69.17 (13.59) | 70.68 (14.21) |
Note. The Pediatric Quality of Life Inventory, version 4.0, was used to measure health-related quality of life; score range = 0–100.
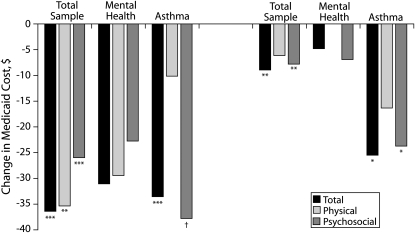
In Figure 1, we plotted the adjusted regression coefficients to show how changes in the PedsQL were associated with changes in total Medicaid costs. After adjustment for gender, age, Medicaid type, and SBHC status, parent proxy reports for the total sample yielded statistically significant reductions in the amount of $36.39 (P < .01) for every 1-point increase in total HRQOL. The reductions in Medicaid costs for physical ($35.36; P < .05) and psychosocial ($25.96; P < .01) HRQOL were also significant. We also found significant Medicaid cost reductions for every 1-point increase in student-reported total ($8.94; P < .05) and psychosocial ($7.79; P < .05) HRQOL. A 1-point increase in student-reported physical health was associated with a nonsignificant decrease in Medicaid costs of $6.12 (P = .27).
FIGURE 1.
Estimated average change in Medicaid cost for every 1-point increase on parent-reported and student self-reported total, physical dimension, and psychosocial dimension Pediatric Quality of Life Inventory scores: Health Outcomes Study and Medicaid Cost Study, Greater Cincinnati area, Ohio, and northern Kentucky, 2000–2003.
Note. Unstandardized regression coefficients reported adjusted for child gender, age, Medicaid versus State Children's Health Insurance Plan, and school-based health center status.
*P < .10; **P < .05; ***P < .01; †P < .001, 2-tailed.
We detected no significant effects of HRQOL scores on Medicaid costs for either the parent or student reports among the mental health subsample. However, with the exception of student-reported physical HRQOL, all analyses showed declines in costs that were similar to but slightly lower than those of the total sample. For the asthma subsample, increases in both total HRQOL and psychosocial HRQOL were significantly associated with decreases in total Medicaid costs. The reductions in costs were greater for parent than for student reports of higher total ($33.55 vs $25.49) and psychosocial ($37.80 vs $23.73) HRQOL. Physical HRQOL was not significantly associated with Medicaid cost reductions for either the parent or student reports, although we detected a trend toward a decrease in costs.
In our analysis of whether the relationship between Medicaid costs and the PedsQL differed across SBHC groups, the overall interaction term was nonsignificant in all regression models (P > .05), indicating that the relationship between changes in HRQOL and changes in Medicaid costs was independent of SBHC status (data not shown).
DISCUSSION
Development and use of instruments to measure HRQOL have become priorities in the study of pediatric populations. Some argue that pediatric HRQOL is 1 of the most important outcomes for clinical studies,34,35 and evidence among adults linking HRQOL with subsequent health status, health care utilization and costs, and even mortality supports this belief.10–13,15,16,36 Evaluations of SBHCs have generally used HRQOL as a central outcome to argue effectiveness of the intervention. But whether improvements in perceived health status and HRQOL resulting from clinical and community interventions translate into reductions in actual health care costs is less clear.
We analyzed data from a previous community-level SBHC intervention evaluation study21 to identify whether the improvements shown in that study could be linked to reductions in Medicaid costs. We used the PedsQL to show that improvements in HRQOL scores over time translated into significant concomitant cost savings for both the total sample and the subsample of children with asthma. The original SBHC outcome evaluation study, which used these data, found significant increases in student self-reported total (3.4 points; from 74.1 to 77.5) and psychosocial (4.1 points; from 69.6 to 73.7) PedsQL among the SBHC users but not among other students. The overall average Medicaid cost savings per student who used an SBHC equated to $30.40 (3.4 × $8.94) for total PedsQL and $31.40 (4.1 × $7.79) for psychosocial PedsQL. Extrapolating this cost reduction to the entire population of 1709 SBHCs nationwide4 suggests that possible cost savings to Medicaid could be significant. The nonsignficant interaction indicates that these savings should be realized for anyone who demonstrates an improvement regardless of SBHC status. Only the SBHC users, however, showed this reduction in costs.
Although our findings demonstrated a link between changes in HRQOL and health care costs, it is unclear what factors determine perceived health among children and youths. When we broke down the PedsQL into its 2 principal dimensions, physical HRQOL and psychosocial HRQOL, our results contradicted previous work by Seid et al., who found that the psychosocial dimension was not significantly associated with utilization 6, 12, and 24 months later.19 Conversely, we found that changes in psychosocial HRQOL were more strongly associated with changes in Medicaid costs than were changes in physical HRQOL.
Theoretically, the strength of the link between the psychosocial dimension and Medicaid costs supports previous work in the area of perceived health status among youths. Mechanic and Hansell argue that health appraisals among youths are not differentiated by varying dimensions of actual well-being but instead focus on youths' overall life appraisals.37 Vingilis et al. found support for a model that attributed adolescent health perceptions to structural (i.e., family financial status), social (family and school relations), emotional (self-esteem), and behavioral (tobacco use) factors.38 This model has been replicated with national data from the United States and Canada.18,39 Health perceptions among youths appear to extend beyond physical symptomatology, manifesting somatic expressions of social and structural factors such as socioeconomic hardship and life stress.13
The beneficial effects we identified of SBHCs on HRQOL, especially a psychosocial dimension of HRQOL, provide additional support for this previous work. That is, the presence of an SBHC has been shown in other studies to improve access, negating financial and other barriers to care (structural)5,20; to provide students with additional school support and emotional counseling40; and to help dampen the uptake of adverse behaviors such as tobacco use and risky sexual activity.8,41,42 SBHCs may be 1 facet contributing to improved health self-appraisals among youths that reflect daily lived experiences or the psychosocial dimensions and not necessarily specific symptomatology or the physical dimensions.18,37
One limitation of our study was the specific sample of students from kindergarten to grade 8 enrolled in both Greater Cincinnati public schools and the Ohio Medicaid program. This specific sample did not allow us to generalize our findings to older students or students across other districts. However, we see no reason why other regions would experience different effects. Our primary data sources were the HRQOL survey data and Medicaid medical claims database, so we were unable to assess whether these results would apply to children and adolescents covered by other insurance plans or with no insurance. Because of limitations in the Medicaid claims data, we were unable to measure any other clinical parameters for mental health and asthma treatments. The pediatric HRQOL scores were used as a proxy to measure the changes in students' perceived physical and psychosocial behaviors. Finally, with the high level of attrition over the 3-year study period,21 the statistical power to examine changes in HRQOL across groups may have been insufficient; we were thus cautious about some findings. However, this would only serve to amplify the significance of the findings reported here, because fewer cases attenuate statistical power, making statistically significant effects less likely to appear.
The PedsQL was developed as a tool for large population-based and clinical research studies to assess differences across groups and changes over time resulting from various interventions. Over the years, the PedsQL has been demonstrated to be a valid and reliable instrument to suit these needs.30–32 Regardless of whether the PedsQL's health appraisal derives from a specific or general nosology or from some somatic expressions of social and structural factors such as socioeconomic hardship and life stress, changes over time in both parent proxy reports and student self-reports, especially in the psychosocial dimension, were associated with concomitant changes in health care costs. Therefore, our results support the use of improvements in the PedsQL in evaluations of SBHCs as an outcome proxy measure associated with more tangible outcomes, specifically reductions in health care costs.
Acknowledgments
Terrance J. Wade is supported by the Canada Research Chairs program. This research was supported by the Health Foundation of Greater Cincinnati (HFGC).
We thank the participating school districts, the school-based health centers and their staff, and all the students and parents who participated in this evaluation project. We also thank Kathryn Keller, Ann McCracken, and Patricia O'Connor at the HFGC; the Ohio Department of Job and Family Services for providing access to the Ohio Medicaid Claims database; Tracy Huentelman and Kristin Line, for coordinating the research studies; Mona Mansour, Raymond Jang, and Robert Cluxton, for research study consultation; and Mona Ho, Gregory Roth, Tony Leonard, and Beth-Ann Witherow for database programming support.
Human Participant Protection
The SBHC Outcomes Study was approved by the Cincinnati Children's Hospital Medical Center institutional review board, and the Medicaid Cost and Utilization Study was approved by the University of Cincinnati Medical Center institutional review board.
References
- 1.Brindis CD, Klein J, Schlitt J, Santelli J, Juszczak L, Nystrom RJ. School-based health centers: accessibility and accountability. J Adolesc Health. 2003;32(6 supp):98–107 [DOI] [PubMed] [Google Scholar]
- 2.Dryfoos JG. Schools as places for health, mental health, and social services. Teach Coll Rec. 1993;94(3):540–567 [Google Scholar]
- 3.Kaplan DW, Brindis C, Naylor KE, Phibbs SL, Ahlstrand KR, Melinkovich P. Elementary school-based health center use. Pediatrics. 1998;101(6):E12. [DOI] [PubMed] [Google Scholar]
- 4.Juszczak L, Schlitt J, Moore A. School-Based Health Centers: National Census School Year 2004–05. Washington, DC: National Assembly on School-Based Health Care; 2007 [Google Scholar]
- 5.Friedrich M. 25 years of school-based health centers. JAMA. 1999;281(9):781–782 [DOI] [PubMed] [Google Scholar]
- 6.Armbruster P, Gerstein SH, Fallon T. Bridging the gap between service need and service utilization: a school-based mental health program. Community Ment Health J. 1997;33(3):199–211 [DOI] [PubMed] [Google Scholar]
- 7.Dryfoos JG. Safe Passage: Making It Through Adolescence in a Risky Society: What Parents, Schools, and Communities Can Do. New York, NY: Oxford University Press; 1998 [Google Scholar]
- 8.Santelli J, Kouzis A, Newcomer S. School-based health centers and adolescent use of primary care and hospital care. J Adolesc Health. 1996;19(4):267–275 [DOI] [PubMed] [Google Scholar]
- 9.Tyack D. Health and social services in public schools: historical perspectives. Future Child. 1992;2(1):19–31 [Google Scholar]
- 10.Davies AR, Ware JE. Measuring Health Perceptions in the Health Insurance Experiment. Santa Monica, CA: Rand; 1981 [Google Scholar]
- 11.Mossey JM, Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am J Public Health. 1982;72(8):800–808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Idler EL, Angel RJ. Self-rated health and mortality in the NHANES-I epidemiologic follow-up study. Am J Public Health. 1990;80(4):446–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Warren R. Wealth and Health, Health and Wealth. Toronto, Canada: Queen's Printer for Ontario; 1994 [Google Scholar]
- 14.Venus PJ, Levin R, Rector TS. Women's perceptions of Medicaid managed care. Womens Health Issues. 1999;9(2):81–92 [DOI] [PubMed] [Google Scholar]
- 15.Bierman AS, Steiner C, Friedman B, Fillmore CM, Clancy C. Epidemiology of preventable hospitalizations in the United States: measuring socioeconomic inequalities in health, access, and quality. Am J Epidemiol. 1999;149(11 Supp):1779921963 [Google Scholar]
- 16.Fylkesnes K, Førde OH. The Tromsø Study: predictors of self-evaluated health—has society adopted the expanded health concept? Soc Sci Med. 1991;32(2):141–146 [DOI] [PubMed] [Google Scholar]
- 17.Sprenkle MD, Niewoehner DE, Nelson DB, Nichol KL. The Veterans Short Form 36 questionnaire is predictive of mortality and health-care utilization in a population of veterans with a self-reported diagnosis of asthma or COPD. Chest. 2004;126(1):81–89 [DOI] [PubMed] [Google Scholar]
- 18.Vingilis E, Wade TJ, Seeley J. Predictors of adolescent health care utilization. J Adolesc. 2007;30(5):773–800 [DOI] [PubMed] [Google Scholar]
- 19.Seid M, Varni JW, Segall D, Kurtin PS. Health-related quality of life as a predictor of pediatric healthcare costs: a two-year prospective cohort analysis. Health Qual Life Outcomes. 2004;2(48):1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wade TJ, Mansour ME, Guo JJ, Huentelman T, Line K, Keller KN. Access and utilization patterns of school-based health centers at urban and rural elementary and middle schools. Public Health Rep. 2008;123(6):739–750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wade TJ, Mansour ME, Line K, Huentelman T, Keller KN. Improvements in health-related quality of life among school-based health center users in elementary and middle school. Ambul Pediatr. 2008;8(4):241–249 [DOI] [PubMed] [Google Scholar]
- 22.Wade TJ, Line K, Huentelman T. School-Based Health Centers (SBHC) Evaluation Project Final Report. Cincinnati, OH: Health Foundation of Greater Cincinnati; 2004 [Google Scholar]
- 23.Guo JJ, Jang R, Keller KN, McCracken AL, Pan W, Cluxton RJ. Evaluation of Health Outcomes and Costs Among Medicaid Recipients Enrolled in School-Based Health Centers. Cincinnati, OH: Health Foundation of Greater Cincinnati; 2004 [Google Scholar]
- 24.Guo JJ, Jang R, Keller KN, McCracken AL, Pan W, Cluxton RJ. Impact of school-based health centers on children with asthma. J Adolesc Health. 2005;37(4):266–274 [DOI] [PubMed] [Google Scholar]
- 25.Guo JJ, Wade TJ, Keller KN. Impact of school-based health care centers on students with mental health problems. Public Health Rep. 2008;123(6):768–780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.International Classification of Diseases, Ninth Revision, Clinical Modification Hyattsville, MD: National Center for Health Statistics; 1980. DHHS publication PHS 80-1260 [Google Scholar]
- 27.Drummond MF, O'Brien B, Stoddart GL, Torrance GW. Cost Analysis. In: Methods for the Economic Evaluation of Health Care Programs. 2nd ed.New York, NY: Oxford University Press, 1999:52–96 [Google Scholar]
- 28.Bureau of Labor Statistics Consumer Price Index for all Urban Consumers 1997, 1998, 1999, 2000, 2001, 2002. Washington, DC: US Dept of Labor; 2003 [Google Scholar]
- 29.Bureau of Labor Statistics Medical Care Inflation Continues to Rise. Washington, DC: US Dept of Labor; 2001 [Google Scholar]
- 30.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39(8):800–812 [DOI] [PubMed] [Google Scholar]
- 31.Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3(6):329–341 [DOI] [PubMed] [Google Scholar]
- 32.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the Pediatric Quality of Life Inventory. Med Care. 1999;37(2):126–139 [DOI] [PubMed] [Google Scholar]
- 33.SAS Institute Inc Base SAS 9.1 Procedures Guide. Cary, NC: SAS Institute Inc; 2004 [Google Scholar]
- 34.Forrest CB, Simpson L, Clancy C. Child health service research. Challenges and opportunities. JAMA. 1997;277(22):1787–1793 [PubMed] [Google Scholar]
- 35.Homer CJ, Kleinman LC, Goldman DA. Improving the quality of care for children in health systems. Health Serv Res. 1998;33(4 Pt 2):1091–1109 [PMC free article] [PubMed] [Google Scholar]
- 36.Idler EL, Russell LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I epidemiologic follow-up study, 1992. Am J Epidemiol. 2000;152(9):874–883 [DOI] [PubMed] [Google Scholar]
- 37.Mechanic D, Hansell S. Adolescent competence, psychosocial well-being, and self-addressed physical health. J Health Soc Behav. 1987;28(4):364–374 [PubMed] [Google Scholar]
- 38.Vingilis E, Wade TJ, Adlaf E. What factors predict student self-rated physical health? J Adolesc. 1998(1);21:83–97 [DOI] [PubMed] [Google Scholar]
- 39.Wade TJ, Pevalin DJ, Vingilis E. Revisiting student self-rated physical health. J Adolesc. 2000;23(6):785–791 [DOI] [PubMed] [Google Scholar]
- 40.McCord MT, Klein JD, Foy JM, Fothergill K. School-based clinic use and school performance. J Adolesc Health. 1993;14(2):91–98 [DOI] [PubMed] [Google Scholar]
- 41.Anglin TM, Naylor KE, Kaplan DW. Comprehensive school-based health care: high school students’ use of medical, mental health, and substance abuse services. Pediatrics. 1996;97(3):318–330 [PubMed] [Google Scholar]
- 42.Kisker EE, Brown RS. Do school-based health centers improve adolescents’ access to health care, health status, and risk-taking behavior? J Adolesc Health. 1996;18(5):335–343 [DOI] [PubMed] [Google Scholar]