Abstract
Objectives. We assessed attitudes and beliefs about smoke-free laws, compliance, and secondhand smoke exposure before and after implementation of a comprehensive smoke-free law in Mexico City.
Methods. Trends and odds of change in attitudes and beliefs were analyzed across 3 representative surveys of Mexico City inhabitants: before implementation of the policy (n = 800), 4 months after implementation (n = 961), and 8 months after implementation (n = 761).
Results. Results indicated high and increasing support for 100% smoke-free policies, although support did not increase for smoke-free bars. Agreement that such policies improved health and reinforced rights was high before policy implementation and increased thereafter. Social unacceptability of smoking increased substantially, although 25% of nonsmokers and 50% of smokers agreed with smokers' rights to smoke in public places at the final survey wave. Secondhand smoke exposure declined generally as well as in venues covered by the law, although compliance was incomplete, especially in bars.
Conclusions. Comprehensive smoke-free legislation in Mexico City has been relatively successful, with changes in perceptions and behavior consistent with those revealed by studies conducted in high-income countries. Normative changes may prime populations for additional tobacco control interventions.
Smoke-free policies can reduce involuntary exposure to toxic secondhand tobacco smoke (SHS), reduce tobacco consumption and promote quitting,1,2 and shift social norms against smoking.3–5 These policies are fundamental to the World Health Organization's Framework Convention on Tobacco Control, an international treaty that promotes best-practices tobacco control policies across the world.6
Evidence of successful implementation of smoke-free policies generally comes from high-income countries. Low- and middle-income countries increasingly bear the burden of tobacco use,7 however, and these countries may face particular challenges in implementing smoke-free policies, including greater social acceptability of tobacco use, shorter histories of programs and policies to combat tobacco-related dangers, and greater tolerance of law breaking.8–10 There is a need for research that will help identify effective strategies for promoting and implementing smoke-free policies in low- and middle-income countries.
Studies in high-income countries generally indicate that popular support for laws that ban smoking in public places and workplaces is strong and increases after such laws are passed.11–15 Weaker laws that allow smoking in some workplaces can leave policy support unchanged.16 Policy-associated increases in support have been shown across populations that include smokers11,13,14,17,18 and bar owners and staff.19,20 Beliefs about rights to work in smoke-free environments11 and the health benefits of these environments21 have also been shown to increase with policy implementation. Support for banning smoking in all workplaces appears high in Latin American countries,22 but responses to smoke-free policies are less well known. In Uruguay, the first country in the Americas to prohibit smoking in all workplaces, including restaurants and bars,23 support before the law was unknown. However, the level of support was high among both the general population22 and smokers24 after the law's implementation.
Compliance with smoke-free laws in high-income countries has been good, particularly when laws apply across all workplaces, including restaurants and bars, and involve media campaigns. Self-reported declines in exposure in regulated venues11,17,25 are consistent with findings from observational studies,11,26 biomarkers of exposure,11,25,27 and air quality assessments.11,12
Approximately 26% of Mexican adults residing in urban areas smoke.8 Most Mexicans recognize the harms of SHS and support smoke-free policies.9,24,28,29 According to an opinion poll conducted before the August 2007 passage of a smoke-free law in Mexico City, about 80% of both Mexico City inhabitants and Mexicans in general supported prohibiting smoking in enclosed public places and workplaces.28 In 2006, 60% of smokers reported that their workplace had a smoking ban, with Mexico City smokers reporting the lowest percentage of workplace bans at 37%.24
Mexico City's smoke-free workplace law30–32 initially allowed for designated smoking areas that were ventilated and physically separate.22,33 Concerns about the inequity of this law for small business owners who could not afford to build designated smoking areas led the hospitality industry to support a comprehensive smoke-free law31,32 that prohibited smoking inside all enclosed public places and workplaces, including public transport, restaurants, and bars. This law entered into force on April 3, 2008.
Media coverage of the law was similar to that in high-income countries, pitting arguments about the government's obligation to protect citizens from SHS dangers against arguments about discrimination toward smokers and the “slippery slope” of regulating behavior4,32,34 (J. F. Thrasher et al., unpublished data, 2010). Most print media coverage was either positive or neutral, with much less coverage pitched against tobacco control policies.34
In the month before and after the law came into effect, the Mexico City Ministry of Health and nongovernmental organizations disseminated print materials and aired radio spots describing the dangers of SHS and the benefits of the law.30 Community health promoters informed businesses about the law. From September through December 2008, a television, radio, print, and billboard campaign emphasized the law's benefits.35 We assessed, among Mexico City inhabitants, the prevalence of and increases in support, beliefs, norms, and compliance around the smoke-free law, as well as decreases in SHS exposure.
METHODS
Data from 2 representative, population-based samples of Mexico City inhabitants were analyzed. The first sample of 800 participants was surveyed during the 2 weeks (March 21 to April 2, 2008) immediately before the law entered into force. With a sampling frame of all Mexico City inhabitants, a multistage sampling procedure was followed to randomly select 5 adult women and 5 adult men in each selected block group. The American Association of Public Opinion Research (AAPOR) response rate among households that were approached was 41.8% (see AAPOR calculation 1), with a cooperation rate among eligible participants of 69.6% (AAPOR calculation 1).36
In August 2008, a second survey of Mexico City inhabitants aimed to evaluate a smoke-free media campaign (J. F. Thrasher et al., unpublished data, 2010). A similar multistage sampling procedure was followed, with random selection of 5 adults from each selected block group and oversampling of block groups inhabited by the campaign's target population. The AAPOR household response rate was 62.2% (AAPOR calculation 1), with a cooperation rate among eligible participants of 75.5% (AAPOR calculation 1).36 The higher response rate in this second sample may reflect the monthlong data collection period, as opposed to the 2-week period in the first survey. From November 16 to December 15, 2008, participants from the second sample were reinterviewed.
Measures
Smoke-free policy support, beliefs, and norms.
Items were the same in each survey, except where otherwise indicated. Support for smoke-free venues was assessed through standard items focusing on the extent to which participants agreed with prohibiting smoking in different venues (i.e., restaurants and cafes; bars, cantinas, and discos; workplaces; hotels; all enclosed workplaces and public places). Two items focused on the perceived health benefits of smoke-free places: “Smoke-free laws improve the health of your family” and “Smoke-free laws improve the health of people like you.” For these items, the prelaw survey specified “will improve” or “will benefit” to assess expectations after the law's entry into force.
Items on perceived rights addressed smokers' rights (i.e., “Smokers have a right to smoke in smoke-free areas,” “If someone does not want to breathe cigarette smoke, then they should go somewhere else”) as well as those for patrons and workers (i.e., “Workers have a right to work without having to breathe tobacco smoke,” “Customers in enclosed public places have a right to breathe smoke-free air”). The social acceptability of smoking was assessed with 3 items (i.e., “People who are important to you think you should not smoke,” “Mexican society disapproves of smoking,” “Smokers are more and more marginalized”). Likert-scale response options ranged from “strongly agree” to “strongly disagree”; however, the 5 response options in the prelaw survey included a neutral option, whereas the 4-point response scale used in the subsequent survey did not. All responses were dichotomized to reflect agreement (1) versus disagreement or a neutral response (0).
Compliance and exposure to secondhand smoke.
Compliance was assessed with questions used in other studies.37 Participants who worked in enclosed areas were asked how often people had smoked inside in the previous 30 days (never, once, a few times, a lot, always), with categories recoded to never (0) versus once or more (1). Participants who had been to certain public venues (i.e., restaurants or cafes, informal eateries or fondas, bars or discos) in the previous 30 days were asked whether anyone smoked inside those venues in their most recent visit there. Participants also estimated their overall frequency of SHS exposure from other people's cigarettes in the preceding month (none, 1–3 times, not daily but once or more a week, daily). To assess change over time, we recoded this variable to no exposure (1) versus any exposure (0) and to daily exposure (1) versus less than daily exposure (0).
Sociodemographic characteristics and smoking behavior.
Standard questions were used to assess sociodemographic characteristics, and participants were classified as current smokers if they reported having smoked at least one cigarette in the preceding month.
Analysis
Stata version 10.0 (StataCorp LP, College Station, TX) was used in analyzing the data. We used an unweighted t test, crude odds ratios (ORs), and ordinal regression in pairwise group comparisons of sample characteristics across the 3 surveys, as well as attrition analyses associated with the 2 postlaw surveys. All other analyses adjusted for the sampling design and sampling weights, which included weighting of the sample to be representative of the income and gender distribution of adult inhabitants of Mexico City.
For each survey period, we estimated the prevalence of support, beliefs, and norms around the smoke-free policy, as well as of compliance across venues and overall SHS exposure. The prevalence of and changes in these factors were estimated for the entire sample and separately for smokers and nonsmokers. To assess changes in key indicators across survey periods, we pooled data across the 3 waves while adjusting for the dependence between repeated individual observations across the 2 postlaw survey assessments.
Logistic regression models were estimated for each indicator of interest; survey wave was entered as a continuous variable to test for linear trends over time, with simultaneous estimation of odds ratios comparing each postimplementation survey with the preimplementation survey. These models were estimated both without and with adjustment for sociodemographic characteristics, smoking status, and exposure to the law.
RESULTS
Relative to the members of the prelaw sample (n = 800), members of the first postlaw sample (postlaw sample 1; n = 961) and second postlaw follow-up sample (postlaw sample 2; n = 786) were older on average, were more likely to be female, had slightly higher educational achievement, were less likely to smoke, and were less likely to have eaten in an informal eatery in the preceding month (Table 1). Eighty-two percent of people who participated in the first postlaw survey were successfully followed up. Attrition analyses indicated that those who were not successfully followed up were more likely to be younger, to have higher educational achievement, to have smoked in the previous month, and to work indoors.
TABLE 1.
Sample Characteristics: Mexico City Inhabitants, 2008
| Characteristic | Prelaw Sample (n = 800) | Postlaw Sample 1 (n = 961) | Postlaw Sample 2 (n = 786) | Not Followed From First to Second Postlaw Survey (n = 175) |
| Mean age,abc y | 41.6 | 44.7 | 45.4 | 41.7 |
| Female,ab % | 50 | 65 | 66 | 60 |
| Education,abd % | ||||
| Elementary or secondary | 28 | 25 | 26 | 23 |
| Secondary | 29 | 19 | 20 | 15 |
| Technical schoole | 10 | 11 | 11 | 7 |
| High school | 19 | 27 | 26 | 32 |
| University or more | 12 | 18 | 17 | 23 |
| Monthly household income (Mexican pesos),d % | ||||
| 0–1500 | 12 | 10 | 11 | 6 |
| 1501–3000 | 25 | 26 | 26 | 25 |
| 3001–5000 | 26 | 32 | 33 | 28 |
| 5001–8000 | 16 | 19 | 18 | 24 |
| ≥8001 | 21 | 13 | 12 | 17 |
| Current smoker,bfg % | 31 | 24 | 22 | 31 |
| Exposure, % | ||||
| Work indoorsg | 33 | 29 | 26 | 41 |
| Visited restaurant or cafe in past month | 43 | 44 | 44 | 42 |
| Visited informal eatery in past monthab | 35 | 27 | 26 | 27 |
| Visited bar or cantina in past month | 17 | 16 | 15 | 18 |
Note. The smoke-free law went into effect on April 3, 2008. Prelaw survey data were collected from March 21 to April 2, 2008; data for the first postlaw survey were collected in August 2008; and data for the second postlaw survey were collected from November 16 to December 15, 2008.
Difference between prelaw sample and postlaw sample 1 significant at P < .001.
Difference between prelaw sample and postlaw sample 2 significant at P < .001.
Difference between postlaw sample 1 without follow-up and postlaw sample 2 significant at P < .01.
Difference between postlaw sample 1 without follow-up and postlaw sample 2 significant at P < .05.
Vocational or trade school that usually is an alternative to high school.
Difference between prelaw sample and postlaw sample 1 significant at P < .01.
Difference between postlaw sample 1 without follow-up and postlaw sample 2 significant at P < .001.
The crude odds ratios for smoking prevalence decreased across the survey waves (prelaw sample vs postlaw sample 1: OR = 0.61; 95% confidence interval [CI] = 0.45, 0.82; prelaw sample vs postlaw sample 2: OR = 0.59; 95% CI = 0.41, 0.84). However, these odds ratios became nonsignificant in models that adjusted for sociodemographic characteristics (prelaw sample vs postlaw sample 1: adjusted OR [AOR] = 0.75; 95% CI = 0.53, 1.05; prelaw sample vs postlaw sample 2: AOR = 0.82; 95% CI = 0.56, 1.20).
Smoke-Free Policy Support, Beliefs, and Norms
In all 3 surveys, the majority of Mexico City inhabitants, whether smokers or nonsmokers, agreed with prohibiting smoking across venues (Table 2). Levels of agreement were lowest for bars and highest for workplaces at each assessment. Similarly high proportions of participants agreed that the law would improve health and that customers and workers had a right to clean air. The percentages of participants in agreement with the right of smokers to smoke inside were lower but nonetheless noteworthy among nonsmokers (23% in the prelaw sample, 27% in postlaw sample 2) and smokers (38% in the prelaw sample, 54% in postlaw sample 2) alike. Similar percentages were observed among nonsmokers (43% in the prelaw sample, 33% in postlaw sample 2) and smokers (50% in the prelaw sample, 40% in postlaw sample 2) in assessments of agreement with smokers' right to stay where they are when someone else is bothered by their smoke.
TABLE 2.
Prelaw and Postlaw Indicators of Support for and Perceived Benefits of Mexico City's Smoke-Free Law: 2008
| Postlaw Sample 1 |
||||||
| Indicator | Prelaw Sample Agreement, % (SE) | Entire Sample Agreement, % (SE) | Followed-Up Subsample Agreement, % (SE) | Postlaw Sample 2 Agreement, % (SE) | Unadjusted P for Trend | AdjustedaP for Trend |
| General population | ||||||
| Support for prohibiting smoking inside of: | ||||||
| Restaurants and cafes | 80 (1.6) | 84 (2.3) | 83 (2.7) | 93 (1.1) | <.001 | .001 |
| Bars, cantinas, and discos | 61 (1.9) | 67 (2.5) | 65 (2.8) | 71 (2.7) | .004 | .547 |
| Workplaces | 88 (1.2) | 95 (1.1) | 95 (1.3) | 97 (0.7) | <.001 | <.001 |
| Hotels | 69 (1.8) | 74 (2.2) | 75 (2.3) | 82 (2.0) | <.001 | .047 |
| All enclosed workplaces, including restaurants and bars | 78 (1.6) | 80 (2.4) | 79 (2.8) | 88 (1.5) | <.001 | .091 |
| Smoke-free laws improve: | ||||||
| Health of people like you | 89 (1.2) | 95 (1.1) | 95 (1.2) | 97 (0.6) | <.001 | <.001 |
| Health of your family | 91 (1.1) | 96 (0.9) | 96 (1.1) | 98 (0.7) | <.001 | <.001 |
| Perceived rights of: | ||||||
| Workers to work in smoke-free environments | 91 (1.1) | 97 (0.8) | 96 (0.9) | 98 (0.6) | <.001 | <.001 |
| Customers to breathe smoke-free air in enclosed public places | 87 (1.2) | 96 (1.0) | 97 (0.9) | 98 (0.7) | <.001 | <.001 |
| Smokers to smoke inside enclosed public places | 28 (1.6) | 37 (2.8) | 38 (3.0) | 33 (2.5) | .002 | <.001 |
| Smokers to stay where they are when their smoke bothers someone | 45 (1.9) | 35 (2.5) | 34 (2.6) | 35 (2.7) | <.001 | .013 |
| Social acceptability of smoking | ||||||
| People who are important to you think you should not smoke | 86 (1.2) | 92 (1.3) | 93 (1.4) | 94 (1.1) | <.001 | <.001 |
| Mexican society disapproves of smoking | 50 (1.9) | 60 (2.7) | 62 (2.8) | 66 (2.7) | <.001 | <.001 |
| Smokers are increasingly marginalized | 44 (1.9) | 52 (2.7) | 55 (2.8) | 61 (2.8) | <.001 | <.001 |
| Exposure in regulated venues | ||||||
| At work in past monthb | 45 (3.4) | 38 (5.0) | 35 (5.5) | 15 (3.0) | <.001 | <.001 |
| Most recent visit to restaurant or cafec | 57 (3.0) | 17 (3.0) | 22 (3.3) | 11 (3.0) | <.001 | <.001 |
| Most recent visit to informal eateryc | 39 (3.2) | 15 (3.0) | 20 (4.3) | 6 (2.0) | <.001 | <.001 |
| Most recent visit to bar or cantinac | 83 (3.2) | 40 (6.0) | 41 (7.0) | 28 (5.0) | <.001 | <.001 |
| Nonsmokers | ||||||
| Support for prohibiting smoking inside of: | ||||||
| Restaurants and cafes | 85 (1.7) | 88 (2.6) | 87 (3.0) | 97 (0.8) | <.001 | .003 |
| Bars, cantinas, and discos | 68 (2.2) | 73 (2.8) | 71 (3.1) | 79 (3.0) | .005 | .261 |
| Workplaces | 91 (1.3) | 97 (1.1) | 97 (1.3) | 99 (0.6) | <.001 | <.001 |
| Hotels | 76 (1.9) | 80 (2.3) | 80 (2.4) | 88 (2.0) | <.001 | .029 |
| All enclosed workplaces, including restaurants and bars | 85 (1.7) | 83 (2.9) | 82 (3.3) | 93 (1.3) | .001 | .065 |
| Smoke-free laws improve: | ||||||
| Health of people like you | 93 (1.1) | 98 (0.6) | 98 (0.7) | 99 (0.2) | <.001 | <.001 |
| Health of your family | 93 (1.1) | 98 (0.6) | 98 (0.7) | 99 (0.6) | <.001 | <.001 |
| Perceived rights of: | ||||||
| Workers to work in smoke-free environments | 94 (1.0) | 97 (0.7) | 97 (0.8) | 99 (0.2) | <.001 | <.001 |
| Customers to breathe smoke-free air in enclosed public places | 91 (1.3) | 97 (1.0) | 97 (1.0) | 99 (0.5) | <.001 | <.001 |
| Smokers to smoke inside enclosed public places | 23 (1.9) | 36 (3.3) | 37 (3.4) | 27 (2.5) | .004 | <.001 |
| Smokers to stay where they are when their smoke bothers someone | 43 (2.3) | 35 (2.8) | 35 (3.0) | 33 (3.0) | .014 | .068 |
| Social acceptability of smoking | ||||||
| People who are important to you think you should not smoke | 89 (1.4) | 94 (1.3) | 94 (1.3) | 96 (1.0) | <.001 | <.001 |
| Mexican society disapproves of smoking | 53 (2.3) | 62 (3.2) | 63 (3.2) | 67 (3.0) | .001 | <.001 |
| Smokers are increasingly marginalized | 47 (2.3) | 54 (3.2) | 56 (3.2) | 60 (3.1) | <.001 | .003 |
| Exposure in regulated venues | ||||||
| At work in past monthb | 41 (4.3) | 30 (5.6) | 28 (5.8) | 14 (3.5) | <.001 | .024 |
| Most recent visit to restaurant or cafec | 57 (3.6) | 18 (3.2) | 22 (3.9) | 15 (3.3) | <.001 | <.001 |
| Most recent visit to informal eateryc | 39 (4.0) | 15 (3.7) | 21 (4.8) | 10 (2.6) | <.001 | <.001 |
| Most recent visit to bar or cantinac | 84 (4.5) | 44 (8.7) | 48 (9.9) | 41 (6.0) | <.001 | <.001 |
| Smokers | ||||||
| Support for prohibiting smoking inside of: | ||||||
| Restaurants and cafes | 69 (3.2) | 69 (5.3) | 68 (6.1) | 79 (4.1) | .08 | .127 |
| Bars, cantinas, and discos | 45 (3.4) | 46 (5.3) | 41 (6.0) | 41 (6.2) | .449 | .22 |
| Workplaces | 80 (2.7) | 87 (3.3) | 86 (4.2) | 91 (2.6) | .004 | .024 |
| Hotels | 52 (3.4) | 54 (5.4) | 55 (6.2) | 60 (5.8) | .301 | .658 |
| All enclosed workplaces, including restaurants and bars | 64 (3.5) | 67 (4.7) | 65 (5.7) | 70 (4.9) | .389 | .868 |
| Smoke-free laws improve: | ||||||
| Health of people like you | 80 (2.9) | 85 (4.1) | 81 (5.2) | 89 (2.7) | .1 | .245 |
| Health of your family | 87 (2.5) | 89 (3.5) | 87 (4.5) | 94 (2.3) | .201 | .198 |
| Perceived rights of: | ||||||
| Workers to work in smoke-free environments | 82 (2.6) | 94 (2.2) | 94 (2.7) | 92 (2.6) | .011 | .01 |
| Customers to breathe smoke-free air in enclosed public places | 79 (2.7) | 94 (3.0) | 97 (1.6) | 95 (2.0) | <.001 | <.001 |
| Smokers to smoke inside enclosed public places | 38 (3.2) | 40 (5.0) | 43 (6.1) | 54 (6.1) | .013 | <.001 |
| Smokers to stay where they are when their smoke bothers someone | 50 (3.4) | 38 (5.2) | 32 (5.7) | 40 (5.9) | .055 | .141 |
| Social acceptability of smoking | ||||||
| People who are important to you think you should not smoke | 83 (2.4) | 86 (3.5) | 85 (4.4) | 86 (3.5) | .225 | .103 |
| Mexican society disapproves of smoking | 43 (3.4) | 56 (5.2) | 57 (6.2) | 65 (5.8) | .002 | .012 |
| Smokers are increasingly marginalized | 38 (3.3) | 45 (5.0) | 48 (6.0) | 63 (5.7) | <.001 | .019 |
| Exposure in regulated venues | ||||||
| At work in past monthb | 52 (5.5) | 52 (7.6) | 54 (8.5) | 19 (4.3) | .014 | .024 |
| Most recent visit to restaurant or cafec | 57 (5.1) | 16 (5.5) | 20 (6.8) | 23 (1.0) | .011 | .005 |
| Most recent visit to informal eateryc | 39 (5.2) | 16 (7.7) | 19 (9.7) | 18 (2.5) | <.001 | .002 |
| Most recent visit to bar or cantinac | 83 (4.2) | 35 (9.1) | 31 (6.5) | 25 (4.5) | <.001 | <.001 |
Note. OR = odds ratio; CI = confidence interval. The smoke-free law went into effect on April 3, 2008. Prelaw survey data were collected from March 21 to April 2, 2008; data for the first postlaw survey were collected in August 2008; and data for the second postlaw survey were collected from November 16 to December 15, 2008.
Models adjusted for age, gender, education, income, and smoking status (except in the analyses stratified by smoking status), as well as for work in enclosed places and having visited a restaurant or cafe, informal eatery, bar, or cantina in the past month for non-exposure-related outcomes.
Among those who work in enclosed places.
Among those who had visited these venues in the past month.
Logistic models involved omnibus assessments of linear change across all 3 survey waves as well as simultaneous estimation of unadjusted odds ratios indicating changes in percentage of agreement with key indicators. Prelaw-to-postlaw increases among the general population and among nonsmokers, in particular, were statistically significant across almost all indicators of support, beliefs, and norms in favor of the law (Tables 2 and 3). Although indicators in favor of the law generally increased among smokers, these trends did not reach statistical significance for smoke-free policy support in any venue except workplaces or for the perceived health benefits of smoke-free places.
TABLE 3.
Prelaw to Postlaw Changes in Mexico City Inhabitants' Reported Support, Beliefs, Norms, and Compliance: 2008
| Prelaw Sample vs Postlaw Sample 1 |
Prelaw Sample vs Postlaw Sample 2 |
Postlaw Sample 1 vs Postlaw Sample 2, Adjusted ORa(95% CI) | |||
| Outcome of Interest | Crude OR (95% CI) | Adjusted ORa(95% CI) | Crude OR (95% CI) | Adjusted ORa(95% CI) | |
| General population | |||||
| Support for prohibiting smoking inside of: | |||||
| Restaurants and cafes | 1.29 (0.88, 1.88) | 0.87 (0.55, 1.38) | 3.22*** (2.24, 4.62) | 2.50*** (1.62, 3.87) | 2.50*** (1.57, 3.98) |
| Bars, cantinas, and discos | 1.28 (0.98, 1.67) | 0.86 (0.62, 1.18) | 1.54** (1.14, 2.07) | 1.21 (0.81, 1.79) | 1.20 (0.89, 1.63) |
| Workplaces | 2.77*** (1.70, 4.53) | 2.19* (1.19, 4.02) | 5.08*** (2.92, 8.83) | 4.44*** (2.44, 8.07) | 1.83 (0.94, 3.56) |
| Hotels | 1.30 (0.99, 1.70) | 0.93 (0.57, 1.24) | 2.05*** (1.59, 2.71) | 1.57* (1.1, 2.3) | 1.58** (1.17, 2.14) |
| All enclosed workplaces, including restaurants and bars | 1.09 (0.78, 1.53) | 0.75 (0.49, 1.14) | 2.11*** (1.52, 2.93) | 1.63** (1.11, 2.39) | 1.93*** (1.29, 2.87) |
| Smoke-free laws improve: | |||||
| Health of people like you | 2.31** (1.37, 3.90) | 3.14*** (1.35, 5.86) | 3.89*** (2.37, 6.38) | 3.31*** (1.9, 5.80) | 1.69 (0.92, 3.09) |
| Health of your family | 2.33** (1.36, 3.98) | 3.07*** (1.35, 5.51) | 4.40*** (2.23, 8.68) | 5.48*** (2.72, 11.49) | 1.89 (0.93, 3.86) |
| Perceived rights of: | |||||
| Workers to work in smoke-free environments | 3.15*** (1.90, 5.21) | 2.30** (1.30, 4.03) | 5.20*** (2.77, 9.75) | 4.03*** (2.0, 8.10) | 1.65 (0.93, 2.93) |
| Customers to breathe smoke-free air in enclosed public places | 3.73*** (2.16, 6.43) | 5.02*** (2.79, 9.04) | 7.54*** (4.16, 13.70) | 6.61*** (3.36, 12.90) | 2.02 (0.94, 4.35) |
| Smokers to smoke inside enclosed public places | 1.71*** (1.29, 2.27) | 2.17*** (1.55, 3.02) | 1.39* (1.06, 1.86) | 1.94*** (1.41, 2.66) | 0.81 (0.59, 1.12) |
| Smokers to stay where they are when their smoke bothers someone | 0.68** (0.53, 0.89) | 0.66** (0.48, 0.89) | 0.67** (0.51, 0.88) | 0.71* (0.51, 0.97) | 0.98 (0.71, 1.34) |
| Social acceptability of smoking | |||||
| People important to you think you should not smoke | 1.94** (1.30, 2.90) | 2.37*** (1.48, 3.79) | 2.41*** (1.61, 3.62) | 2.22*** (1.41, 3.51) | 1.34 (0.95, 1.88) |
| Mexican society disapproves of smoking | 1.54** (1.18, 2.00) | 1.44* (1.06, 1.94) | 2.05*** (1.55, 2.71) | 1.97*** (1.41, 2.74) | 1.34 (0.95, 1.88) |
| Smokers are increasingly marginalized | 1.35* (1.05, 1.74) | 1.27 (0.95, 1.69) | 1.98*** (1.51, 2.60) | 1.84*** (1.35, 2.51) | 1.47* (1.11, 1.95) |
| Exposure in regulated venues | |||||
| At work in past monthb | 0.77 (0.47, 1.27) | 0.68 (0.38, 1.20) | 0.22*** (0.17, 0.40) | 0.32*** (0.17, 0.6) | 0.28*** (0.14, 0.54) |
| Most recent visit to restaurant or cafec | 0.16*** (0.10, 0.25) | 0.18*** (0.11, 0.32) | 0.10*** (0.05, 0.21) | 0.11*** (0.05, 0.24) | 0.62 (0.28, 1.39) |
| Most recent visit to informal eateryc | 0.28*** (0.16, 0.49) | 0.28*** (0.14, 0.55) | 0.11*** (0.06, 0.19) | 0.10*** (0.05, 0.21) | 0.38** (0.18, 0.78) |
| Most recent visit to bar or cantinac | 0.17*** (0.09, 0.32) | 0.10*** (0.04, 0.2) | 0.10*** (0.05, 0.21) | 0.06*** (0.02, 0.18) | 0.59 (0.25, 1.37) |
| Nonsmokers | |||||
| Support for prohibiting smoking inside of: | |||||
| Restaurants and cafes | 1.23 (0.72, 2.09) | 0.83 (0.44, 1.56) | 4.90*** (2.81, 8.55) | 4.07*** (1.99, 8.29) | 5.39*** (2.27, 12.78) |
| Bars, cantinas, and discos | 1.23 (0.88, 2.62) | 0.91 (0.62, 1.35) | 1.77** (1.19, 2.62) | 1.40 (0.86, 2.29) | 2.06** (1.32, 3.20) |
| Workplaces | 3.36*** (1.56, 7.24) | 2.72* (1.02, 7.23) | 8.39*** (3.00, 23.47) | 10.30*** (3.67, 28.85) | 4.50* (1.23, 16.42) |
| Hotels | 1.21 (0.86, 1.70) | 0.94 (0.61, 1.40) | 2.24*** (1.49, 3.36) | 1.87* (1.15, 3.05) | 2.56*** (1.76, 4.64) |
| All enclosed workplaces, including restaurants and bars | 0.92 (0.58, 1.47) | 0.68 (0.40, 1.18) | 2.55c (1.59, 4.11) | 2.08** (1.20, 3.63) | 4.12*** (2.61, 10.03) |
| Smoke-free laws improve: | |||||
| Health of people like you | 4.11*** (1.81, 9.32) | 7.12*** (2.48, 20.48) | 12.60*** (5.19, 30.56) | 11.78*** (4.43, 31.23) | 5.05** (1.74, 14.72) |
| Health of your family | 3.94*** (1.97, 7.87) | 5.73*** (2.32, 14.15) | 8.54*** (2.40, 30.41) | 23.70*** (8.25, 68.06) | 2.68 (0.63, 11.47) |
| Perceived rights of: | |||||
| Workers to work in smoke-free environments | 2.39** (1.23, 4.62) | 1.74 (0.84, 3.55) | 12.84*** (4.67, 35.31) | 8.76*** (3.0, 25.34) | 8.33*** (2.65, 26.17) |
| Customers to breathe smoke-free air in enclosed public places | 2.83*** (1.51, 5.30) | 2.99*** (1.51, 5.92) | 8.33*** (3.60, 19.27) | 7.55*** (2.90, 19.60) | 4.06** (1.40, 11.79) |
| Smokers to smoke inside enclosed public places | 2.13*** (1.50, 3.02) | 2.43*** (1.62, 3.63) | 1.36 (0.98, 1.87) | 1.77** (1.22, 2.57) | 0.51** (0.30, 0.85) |
| Smokers to stay where they are when their smoke bothers someone | 0.73* (0.54, 0.99) | 0.77 (0.53, 1.12) | 0.70* (0.51, 0.96) | 0.72 (0.48, 1.05) | 1.01 (0.64, 1.60) |
| Social acceptability of smoking | |||||
| People important to you think you should not smoke | 2.14** (1.28, 3.59) | 2.80** (1.45, 5.40) | 3.03*** (1.80, 5.11) | 2.78*** (1.54, 5.00) | 1.25 (0.63, 2.47) |
| Mexican society disapproves of smoking | 1.48* (1.08, 2.03) | 1.39 (0.97, 1.96) | 1.92*** (1.39, 2.65) | 1.91** (1.29, 2.80) | 1.45 (0.89, 2.38) |
| Smokers are increasingly marginalized | 1.40 (0.98, 1.81) | 1.35 (0.95, 1.91) | 1.79*** (1.31, 2.44) | 1.75** (1.22, 2.52) | 1.27 (0.84, 1.92) |
| Exposure in regulated venues | |||||
| At work in past monthb | 0.63 (0.34, 1.18) | 0.50 (0.23, 1.05) | 0.25*** (0.12, 0.55) | 0.41* (0.18, 0.96) | 0.45 (0.18, 1.13) |
| Most recent visit to restaurant or cafec | 0.16*** (0.10, 0.27) | 0.17*** (0.09, 0.34) | 0.07*** (0.04, 0.14) | 0.07*** (0.03, 0.15) | 0.44* (0.19, 0.99) |
| Most recent visit to informal eateryc | 0.26*** (0.13, 0.50) | 0.25*** (0.11, 0.54) | 0.09*** (0.04, 0.21) | 0.07*** (0.02, 0.19) | 0.39 (0.13, 1.13) |
| Most recent visit to bar or cantinac | 0.17*** (0.65, 0.45) | 0.13** (0.03, 0.59) | 0.10*** (0.04, 0.28) | 0.07*** (0.02, 0.29) | 0.76 (0.21, 2.75) |
| Smokers | |||||
| Support for prohibiting smoking inside of: | |||||
| Restaurants and cafes | 1.04 (0.62, 1.81) | 1.06 (0.52, 2.15) | 1.71* (1.01, 2.91) | 1.67 (0.92, 3.02) | 1.65 (0.81, 3.34) |
| Bars, cantinas, and discos | 1.01 (0.61, 1.66) | 0.72 (0.40, 1.30) | 0.78 (0.45, 1.38) | 0.70 (0.36, 1.37) | 0.77 (0.38, 1.60) |
| Workplaces | 1.80 (0.93, 3.46) | 1.81 (0.77, 4.26) | 2.63** (1.31, 5.28) | 2.54* (1.10, 5.88) | 1.47 (0.66, 3.27) |
| Hotels | 1.08 (0.65, 1.77) | 0.96 (0.53, 1.76) | 1.36 (0.79, 2.30) | 1.19 (0.66, 2.14) | 1.26 (0.70, 2.25) |
| All enclosed workplaces, including restaurants and bars | 1.13 (0.69, 1.84) | 0.97 (0.55, 1.71) | 1.26 (0.74, 2.15) | 1.07 (0.61, 1.89) | 1.12 (0.67, 1.87) |
| Smoke-free laws improve: | |||||
| Health of people like you | 1.22 (0.6, 2.44) | 1.86 (0.77, 4.44) | 1.75 (0.93, 3.30) | 1.44 (0.67, 3.01) | 1.44 (0.61, 3.40) |
| Health of your family | 1.06 (0.47, 2.41) | 1.57 (0.62, 3.99) | 1.86 (0.80, 4.36) | 1.84 (0.66, 5.12) | 1.75 (0.61, 5.03) |
| Perceived rights of: | |||||
| Workers to work in smoke-free environments | 3.42** (1.48, 7.91) | 3.34* (1.23, 9.09) | 2.62* (1.16, 5.89) | 3.26* (1.25, 8.52) | 0.77 (0.40, 1.46) |
| Customers to breathe smoke-free air in enclosed public places | 4.67** (1.53, 14.29) | 19.34*** (5.30, 70.59) | 5.50*** (2.54, 11.91) | 7.81*** (2.82, 21.64) | 1.18 (0.31, 4.49) |
| Smokers to smoke inside enclosed public places | 1.22 (0.77, 1.94) | 1.62 (0.89, 2.94) | 2.11** (1.24, 3.58) | 3.08*** (1.65, 5.74) | 1.73** (1.02, 2.92) |
| Smokers to stay where they are when their smoke bothers someone | 0.61* (0.37, 1.00) | 0.41** (0.22, 0.76) | 0.66 (0.39, 1.11) | 0.79 (0.44, 1.42) | 1.09 (0.58, 2.04) |
| Social acceptability of smoking | |||||
| People important to you think you should not smoke | 1.38 (0.72, 2.64) | 2.15* (1.09, 4.24) | 1.40 (0.73, 2.66) | 1.62 (0.79, 3.35) | 1.01 (0.42, 2.45) |
| Mexican society disapproves of smoking | 1.58 (1.00, 2.49) | 1.64 (0.97, 2.77) | 2.34** (1.34, 4.09) | 2.18* (1.15, 4.13) | 1.48 (0.80, 2.77) |
| Smokers are increasingly marginalized | 1.25 (0.78, 1.99) | 1.08 (0.62, 1.85) | 2.59*** (1.51, 4.44) | 2.17** (1.21, 3.90) | 2.08* (1.09, 3.98) |
| Exposure in regulated venues | |||||
| At work in past monthb | 1.14 (0.65, 1.99) | 0.84 (0.44, 1.59) | 0.17*** (0.08, 0.38) | 0.15*** (0.06, 0.39) | 0.15*** (0.07, 0.34) |
| Most recent visit to restaurant or cafec | 0.15*** (0.08, 0.28) | 0.28*** (0.11, 0.49) | 0.21* (0.05, 0.85) | 0.21** (0.07, 0.65) | 1.39 (0.32, 6.06) |
| Most recent visit to informal eateryc | 0.33* (0.11, 0.97) | 0.31 (0.08, 1.19) | 0.13*** (0.06, 0.28) | 0.13*** (0.04, 0.43) | 0.41 (0.12, 1.41) |
| Most recent visit to bar or cantinac | 0.15*** (0.09, 0.27) | 0.03*** (0.01, 0.06) | 0.08*** (0.03, 0.17) | 0.02*** (0.01, 0.05) | 0.50 (0.22, 1.12) |
Note. OR = odds ratio; CI = confidence interval. The smoke-free law went into effect on April 3, 2008. Prelaw survey data were collected from March 21 to April 2, 2008; data for the first postlaw survey were collected in August 2008; and data for the second postlaw survey were collected from November 16 to December 15, 2008.
Adjusted for age, gender, education, income, smoking status, work in enclosed places, and having visited a restaurant or cafe, informal eatery, bar, or cantina in the past month.
Among those who work in enclosed places.
Among those who had visited these venues in the past month.
*P < .05; **P < .01; ***P < .001.
Adjusted odds ratios and linear trends were also estimated to assess changes over time after control for sociodemographics, current smoking status, and exposure to the law. In the general population and among the subpopulation of nonsmokers, the statistical significance of the bivariate results was generally maintained across indicators of support, beliefs, and norms. The only change to a nonsignificant result in the trend analyses was found for models of support for smoke-free bars and for all workplaces, including restaurants and bars. However, statistically significant increases in crude and adjusted odds of support for all workplaces being smoke free were found when the second postlaw survey was compared with the previous surveys, suggesting a nonlinear change over time. Among smokers, the statistical significance of results for linear trends and odds ratios was consistent across adjusted and unadjusted models.
Smoke-Free Policy Compliance and Secondhand Smoke Exposure
Participants who reported working in enclosed areas were asked whether someone had smoked in the interior areas of their workplace in the previous month. In both the general population and among smokers, the decrease over time was statistically significant in unadjusted as well as adjusted analyses; among nonsmokers, however, this decrease was significant only in unadjusted analyses (Table 3). Participants who had visited any of 3 types of venues (restaurants or cafes; fondas; and bars, cantinas, or discos) in the preceding month were asked whether anyone had smoked inside during their most recent visit. Crude and adjusted trends over time, as well as odds ratios comparing the prelaw assessment with each of the 2 postlaw assessments, indicated statistically significant decreases in SHS exposure across all venues (Table 3).
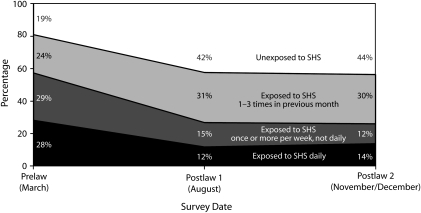
We also estimated overall frequency of exposure to smoke from another person's cigarette in the preceding month (Figure 1). The percentage of participants who reported no exposure in the previous month increased from 19% to 44%. The bivariate and multivariate adjusted odds ratios for lack of exposure to SHS in the preceding month increased from the prelaw survey to the first postlaw survey (OR = 3.28; 95% CI = 2.16, 4.99; AOR = 3.25; 95% CI = 1.95, 5.40) and to the second postlaw survey (OR = 3.45; 95% CI = 2.18, 5.45; AOR = 2.82; 95% CI = 1.63, 4.87).
FIGURE 1.
Self-reported overall exposure to secondhand smoke (SHS) among Mexico City inhabitants, before and after implementation of a comprehensive smoke-free policy: 2008.
Note. The smoke-free law entered into force on April 3, 2008.
Over the survey period, the percentage of participants exposed daily to SHS decreased by half (from 28% to 14%). The bivariate and adjusted odds ratios for daily exposure were significantly lower in both the first postlaw survey (OR = 0.35; 95% CI = 0.24, 0.52; AOR = 0.38; 95% CI = 0.24, 0.60) and the second postlaw survey (OR = 0.43; 95% CI = 0.27, 0.68; AOR = 0.50; 95% CI = 0.31, 0.81) than during the prelaw period. Self-reported SHS exposure did not significantly change between the postlaw surveys.
DISCUSSION
The results of our study are generally consistent with results of studies focusing on smoke-free policies in high-income countries. Similar to populations in other jurisdictions,11–15,22 a majority of Mexico City inhabitants supported prohibiting smoking within all venues queried, and this support generally increased after the law came into effect. The lowest level of support was for smoke-free bars, the venue for which noncompliance was highest and the only venue without a statistically significant increase in support, except among nonsmokers.
Other studies of bar patrons, owners, and workers have concluded that their perception of these policies grew more favorable over time.19,20 Such findings may translate to Mexico City over a longer period of time than our study encompassed; however, pockets of resistance against the law may nonetheless grow, as indicated by smokers' growing sentiment that smokers have a right to smoke inside enclosed public places; this sentiment characterized 54% of smokers and 27% of nonsmokers at the most recent assessment.
The global economic crises after the law's implementation revitalized media (and likely tobacco industry sponsored) scaremongering about hospitality industry losses caused by the law (J. F. Thrasher et al., unpublished data, 2010). Scientific studies designed to dispel such concerns with meaningful local-level data inevitably lag behind the expression of these concerns. The importance of conducting and communicating results from economic studies may continue to prove critical across jurisdictions implementing smoke-free policies, especially during periods of economic crisis.
Other beliefs and perceived norms examined in this study are likely to bolster the success of the Mexico City smoke-free law. For example, a large majority of participants expressed beliefs in favor of workers' and customers' rights to breathe clean air (91% in the prelaw survey and 98% in the postlaw survey 2) and the health benefits that smoke-free areas confer on their families (91% in the prelaw survey and 98% in postlaw survey 2) and people similar to them (89% in the prelaw survey and 97% in postlaw survey 2). Similarly high percentages have been reported among New Zealanders.11
No smoke-free policy evaluation of which we are aware has assessed the perceived rights of smokers. Our results suggest an opposing tendency to agree with smokers' rights to smoke inside of public places among approximately one third of the population. Hence, in spite of favorable perceptions of smoke-free laws, a substantial proportion of the population appears conflicted. Some Mexican media have promoted the perspective of smokers' rights (J. F. Thrasher et al., unpublished data, 2010), which, in combination with the law's implementation, may also account for the relatively abrupt shift in the perceived social acceptability of smoking revealed in this study. The percentage of people who agreed that Mexican society disapproved of smoking jumped by 32% (from 50% to 66%) over the 8-month period that our surveys covered, with a 38% rise (from 44% to 61%) among those who agreed that smokers were increasingly marginalized.
Such normative shifts are one of the reasons why the World Health Organization has highlighted the importance of smoke-free policies in laying the foundation for future tobacco control policies and programs. Reactions centering on violation of smokers' rights may nevertheless dissipate over time, as other studies have concluded.
Self-reported compliance with the law appeared reasonably good but not complete. The perception that the law applied to public workplaces such as restaurants and bars but not to private workplaces may explain the lack of compliance found in the first postlaw survey (37%), although this percentage had dropped significantly by the final survey (15%). Lack of compliance reported by participants during their most recent visit to a bar was highest at the second follow-up survey (37%), with less (but still prevalent) noncompliance in restaurants (17%) and informal eateries (12%). Higher rates of compliance have been found in studies in high-income countries that rely on self-reported data17,38; however, these studies have been conducted among smokers, who may be more likely to overreport compliance than nonsmokers. In spite of possible biases in our estimates of compliance, overall decreases in reported levels of SHS exposure are notable and likely to improve health outcomes.
We found no statistically significant reduction in the prevalence of smoking over the survey period, a result that differs from other studies that have shown a reduction in consumption but have had more power to detect such changes.12,17 The slightly different sampling procedures in each survey may have led to different participation rates among smokers. The prelaw survey quota sampling ensured that 50% of the sample was female. The second sample included more women (66%), which may have resulted in lower rates of participation among smokers because the smoking prevalence among urban Mexican women is less than half that of men.
Opinion poll survey data collected in Mexico City in 2008 and 2009 suggested that the prevalence of smoking was stable over this period.39 Although lower rates of participation among smokers in the postlaw period could have biased our results, our stratified analyses show important changes among smokers and nonsmokers alike. The increasing social unacceptability of smoking revealed in our study may ultimately translate into reduced consumption, but perhaps over the long term.40
Limitations
Conclusions about the causal impact of Mexico City's smoke-free law should be tempered by a few observations. Although our response rates were reasonable, survey participants may have differed from those who did not take part, and varying response rates and sample composition across the surveys may have biased comparisons in unpredictable ways. However, for the most part, bivariate and multivariate adjusted models produced similar point estimates and maintained statistical significance, suggesting that differences across the samples may not have been biased. Missing values for the 16% of participants who were lost to follow-up were not imputed because attrition was not random. However, analyses of the cohort that was successfully followed up controlled for unmeasured individual-level characteristics that may have otherwise confounded our results.
Measurement may have introduced some biases. In particular, the lack of a neutral response option for some of the attitude measures in our postlaw surveys may have biased our results in favor of finding the desired effects, because we assumed that neutral responders were not disposed to favor the law. However, we also found statistically significant normative and attitudinal change across the 2 postlaw surveys that had no neutral option, which suggests that instrumentation bias does not account for our findings.
Some measures, particularly the compliance measures, may have suffered from self-report biases. Other studies have shown that self-reports are consistent with conclusions from environmental monitoring and biomarker studies.11,25 Our results on compliance are also consistent with results from an airborne nicotine monitoring study, conducted after the law's passage, that revealed lower levels of SHS in restaurants and bars in Mexico City than in other cities.41 Analyses of cohorts of smokers from 2007 until the end of 2008 were conducted to help rule out the possibility of secular trends accounting for the observed results; these analyses showed decreases in self-reported SHS exposure in bars and restaurants, as well as increases in support for smoke-free policies in those venues, both of which were greater among smokers in Mexico City than among smokers in other Mexican cities.42
Conclusions
Consistent with studies conducted in high-income countries, we found that the Mexico City law prohibiting smoking across workplaces, including restaurants and bars, has built upon and increased beliefs and norms in favor of such policies and perhaps has laid the foundation for other interventions that build on smoking “denormalization.” The law's implementation was accompanied by a significant drop in overall toxic SHS exposure. Other Mexican cities, as well as other low- and middle-income countries, may look to the success of Mexico City as an example. Nevertheless, governmental officials and civil society advocates should continue to address compliance problems so that the benefits of smoke-free policies are further entrenched into the social fabric of one of the largest cities in the world.
Acknowledgments
This article is based on data collected with funding from a Roswell Park Cancer Institute grant through the Flight Attendant Medical Research Institute and with a grant from the Bloomberg Initiative to Reduce Tobacco Use through the World Lung Foundation and the International Union against Tuberculosis and Lung Disease. Analyses were supported in part by the Mexican National Council on Science and Technology (Convocatoria Salud 2007-C01-70032) and an unrestricted grant from Johnson & Johnson.
Human Participant Protection
This study was approved by the institutional review board of the Mexican National Institute of Public Health. Participants provided written informed consent.
References
- 1.Brownson RC, Hopkins DP, Wakefield M. Effects of smoking restrictions in the workplace. Annu Rev Public Health. 2002;23:333–348 [DOI] [PubMed] [Google Scholar]
- 2.Fichtenberg CM, Glantz SA. Effect of smoke-free policies on smoking behavior: a systematic review. BMJ. 2002;325(7357):188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wasserman J, Manning WG, Newhouse JP, Winkler JD. The effects of excise taxes and regulations on cigarette smoking. J Health Econ. 1991;10(1):43–64 [DOI] [PubMed] [Google Scholar]
- 4.Jacobson PD, Zapawa LM. Clean indoor air restrictions. : Rabin RL, Sugarman SD, Regulating Tobacco. New York, NY: Oxford University Press; 2001:207–244 [Google Scholar]
- 5.Hamilton WL, Biener L, Brennan RT. Do local tobacco regulations influence perceived smoking norms? Evidence from adult and youth surveys in Massachusetts. Health Educ Res. 2008;23(4):709–722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Framework Convention on Tobacco Control. Geneva, Switzerland: World Health Organization; 2003 [Google Scholar]
- 7.Mathers C, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thrasher JF, Reynales-Shigematsu L, Baezconde-Garbanati L, et al. Promoting the effective translation of the Framework Convention on Tobacco Control: a case study of challenges and opportunities for strategic communications in Mexico. Eval Health Prof. 2008;31(2):145–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thrasher JF, Besley JC, González W. Perceived justice and popular support for public health laws: a case study around comprehensive smoke-free legislation in Mexico City. Soc Sci Med. 2010;70(5):787–793 [DOI] [PubMed] [Google Scholar]
- 10.Sussman S, Pokhrel P, Black D, et al. Tobacco control in developing countries: Tanzania, Nepal, China, and Thailand as examples. Nicotine Tob Res. 2007;9(3):S447–S457 [DOI] [PubMed] [Google Scholar]
- 11.Edwards R, Thomson G, Wilson N, et al. After the smoke has cleared: evaluation of the impact of a new national smoke-free law in New Zealand. Tob Control. 2008;17(1):1–10 [DOI] [PubMed] [Google Scholar]
- 12.Gorini G, Chellini E, Galeone D. What happened in Italy? A brief summary of studies conducted in Italy to evaluate the impact of the smoking ban. Ann Oncol. 2007;18(10):1620–1622 [DOI] [PubMed] [Google Scholar]
- 13.Tang H, Cowling D, Lloyd J, et al. Changes of attitudes and patronage behaviors in response to a smoke-free law. Am J Public Health. 2003;93(4):611–617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Friis RH, Safer AM. Analysis of responses of Long Beach, California residents to the smoke-free bars law. Public Health. 2005;119(12):1116–1121 [DOI] [PubMed] [Google Scholar]
- 15.Rayens M, Hahn E, Langley R, Hedgecock S, Butler K, Greathouse-Maggio L. Public opinion and smoke-free laws. Policy Polit Nurs Pract. 2007;8(4):262–270 [DOI] [PubMed] [Google Scholar]
- 16.Biener L, Garrett C, Skeer M, Siegel M, Connolly G. The effects on smokers of Boston's smoke-free bar ordinance: a longitudinal analysis of changes in compliance, patronage, policy support and smoking at home. J Public Health Manag Pract. 2007;13(6):630–636 [DOI] [PubMed] [Google Scholar]
- 17.Fong GT, Hyland A, Borland R, Hammond D, Hastings G, McNeil AD, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK Survey. Tob Control. 2006;15(suppl 3):iii51–iii58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyland A, Higbee C, Borland R, et al. Attitudes and beliefs about secondhand smoke and smoke-free policies in four countries: findings from the International Tobacco Control Four Country Survey. Nicotine Tob Res. 2009;11(6):642–649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hilton S, Semple S, Miller B, et al. Expectations and changing attitudes of bar workers before and after the implementation of smoke-free legislation in Scotland. BMC Public Health. 2007;7(206):1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tang H, Cowling DW, Stevens CM, Lloyd JC. Changes of knowledge, attitudes, beliefs, and preference of bar owner and staff in response to a smoke-free bar law. Tob Control. 2004;13(1):87–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pursell L, Allwright S, O'Donovan D, et al. Before and after study of bar workers' perceptions of the impact of smoke-free workplace legislation in the Republic of Ireland. BMC Public Health. 2007;7(147):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sebrié EM, Schoj V, Glantz SA. Smoke free environments in Latin America: on the road to real change? Prev Control. 2008;3(1):21–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thrasher JF, Chaloupka F, Hammond D, et al. Evaluación de las políticas contra el tabaquismo en países latinoamericanos en la era del Convenio Marco para el Control del Tabaco. Salud Publica Mex. 2006;48(suppl 1):S155–S166 [DOI] [PubMed] [Google Scholar]
- 24.Thrasher JF, Boado M, Sebrié EM, Bianco E. Smoke-free policies and the social acceptability of smoking in Uruguay and Mexico: findings from the International Tobacco Control Policy Evaluation (ITC) Project. Nicotine Tob Res. 2009;11(6):591–599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haw SJ, Gruer L. Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: national cross-sectional survey. BMJ. 2007;335(7619):549–552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Skeer M, Land ML, Cheng DM, Siegel MB. Smoking in Boston bars before and after a 100% smoke-free regulation: an assessment of early compliance. J Public Health Manag Pract. 2004;10(6):501–507 [DOI] [PubMed] [Google Scholar]
- 27.Akhtar P, Currie D, Currie C, Haw S. Changes in Child Exposure to Environmental Tobacco Smoke (CHETS) study after implementation of smoke-free legislation in Scotland: National cross-sectional survey. BMJ. 2007;335(7619):545–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abundis F. La ley general de control del tabaco y la opinión pública. Salud Publica Mex. 2008;50(suppl 3):S366–S371 [DOI] [PubMed] [Google Scholar]
- 29.Thrasher JF, Bentley ME. The meanings and context of smoking among Mexican university students. Public Health Rep. 2006;121(5):578–585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.González-Roldan JF. Abogacía para el control del tabaco en México: retos y recomendaciones. Salud Publica Mex. 2008;50(suppl 3):S391–S400 [DOI] [PubMed] [Google Scholar]
- 31.Mondragón M. Prohibición de fumar en lugares públicos y mercantiles: retos para implementar la ley en el Distrito Federal. Salud Publica Mex. 2008;50(suppl 3):S401–S404 [DOI] [PubMed] [Google Scholar]
- 32.Expacios Guillermo-Tenorio X. 100% libres de humo: una realidad del Distrito Federal. Salud Publica Mex. 2008;50(suppl 3):S384–S390 [DOI] [PubMed] [Google Scholar]
- 33.Sebrié EM, Glantz SA. “Accommodating” smoke-free policies: tobacco industry's Courtesy of Choice programme in Latin America. Tob Control. 2007;16(5):e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Llaguno-Aguilar SE, Dorantes-Alonso AC, Thrasher JF, Villalobos V, Besley JC. Análisis de la cobertura del tema de tabaco en medios impresos mexicanos. Salud Publica Mex. 2008;50(suppl 3):S348–S354 [DOI] [PubMed] [Google Scholar]
- 35.Villalobos V, Ortiz-Ramirez O, Thrasher JF, Arillo-Santillán E, Pérez-Hernández R, Cedillo C, González W. Mercadotecnia social para promover políticas públicas de salud: el desarrollo de una campaña para promover la norma social de no fumar en restaurantes y bares del Distrito Federal, México. Salud Publica Mex. In press [PubMed] [Google Scholar]
- 36.Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 3rd ed.Lenexa, KS: American Association for Public Opinion Research; 2004 [Google Scholar]
- 37.Methods for Evaluating Tobacco Control Policies. Vol. 12 Lyon, France: International Agency for Research on Cancer; 2009 [Google Scholar]
- 38.Hyland A, Hassan LM, Higbee C, et al. The impact of smokefree legislation in Scotland: results from the Scottish ITC: Scotland/UK longitudinal surveys. Eur J Public Health. 2009;19(2):198–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Encuesta Nacional de Opinión Pública: Espacios Libres de Humo de Tabaco. Juárez, Mexico: Consejo Nacional contra Tabaquismo; 2009 [Google Scholar]
- 40.Alamar B, Glantz SA. Effect of increased social unacceptability of cigarette smoking on reduction in cigarette consumption. Am J Public Health. 2006;96(8):1359–1363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barrientos-Gutiérrez T, Reynales Shigematsu L-M, Lazcano-Ponce E. Lugares 100% Libres de Humo de Tabaco: Exposición a Humo de Tabaco y Efectos a la Salud en Bares y Restaurantes de México. Cuernavaca, Mexico: Instituto Nacional de Salud Pública; 2009 [Google Scholar]
- 42.Thrasher J, Swayampakala K, Villalobos V, Arillo-Santillán E, Walseman K, Bottai M. Differential impact of local and federal smoke-free legislation in Mexico: a longitudinal study of campaign exposure, support for smoke-free policies and secondhand tobacco smoke exposure among adult smokers. Salud Publica Mex. In press [DOI] [PMC free article] [PubMed] [Google Scholar]