Introduction
The utilization of surgical fusion for the treatment of disorders of the spine has been increasing dramatically in the past decades (1, 2). Despite this trend, a paucity of literature examining the issues surrounding the safety of this procedure remain. Existing data are limited by inclusion of small sample sizes, single institution experiences, and selected patient populations (3, 4, 5, 6). Further, few studies exist comparing the various surgical approaches to the spine and the outcomes associated with them (7, 8, 9). This data is important to identify patients at risk, allocate healthcare resources, adequately inform health care providers and patients of such risks and direct future research to improve perioperative outcomes. Therefore we sought to 1) examine demographics of patients undergoing primary anterior, posterior and anterior/posterior fusion of the non-cervical spine, 2) assess the perioperative incidence for morbidity and mortality and 2) determine independent risk factors for such outcome.
Materials and Methods
NIS annual data files were commercially obtained from the Hospital Cost and Utilization Project (HCUP). The NIS represents the largest all payer inpatient database in the United States and as part of the Hospital Cost and Utilization Project (HCUP) is sponsored by the Agency for Healthcare Research and Quality (AHRQ). In brief, the NIS contains information on inpatient discharges from approximately 8 million hospital admissions per year. Having grown since its inception in 1988 when it included data from 8 US states, the most recent data files represent a 20% stratified sample of approximately 1000 community hospitals in 38 states. The NIS provides weights that allow for nationally representative estimates. It includes over 100 clinical and non clinical data elements, such as diagnoses, procedures, admission and discharge status, patient demographics (e.g., gender, age, race, median income), payment source, length of stay, and hospital characteristics (e.g., size, location, teaching status). Detailed information on the NIS design can be found at www.hcup-us.ahrq.gov/nisoverview.jsp (10). As data used in this study are sufficiently de-identified, the use of this study was exempt from review by the institutional review board.
Study sample and analysis
Data collected for each year between 1998 and 2006 were read into a statistical software program (SAS version 9.1, SAS institute, Cary, NC), and analyzed. Discharges with a procedure code (ICD-9-CM) for primary anterior and posterior non-cervical spine fusion (8104-8108) were identified and included in the sample. Three procedure type groups were created: anterior spine fusion (ASF), posterior spine fusion (PSF), and anterior/posterior spine fusion (APSF). The prevalence of procedure sub-types and respective demographics (age, gender, race, disposition status, primary source of payment, distribution of procedures by hospital size, teaching status and location, and length of care) were evaluated. Frequencies of procedure-related complications were analyzed by determining cases that listed ICD-9-CM diagnosis codes specifying complications of surgical and medical care (ICD-9-CM 996.X to 999.X). In addition, we studied the prevalence of selected adverse diagnoses, including pulmonary embolism, venous thrombosis, respiratory insufficiency after trauma or surgery/Adult Respiratory Distress Syndrome (ARDS), and acute posthemorrhagic anemia, using the ICD-9-CM diagnosis code system. The indication for surgery was determined by the presence of ICD-9-CM diagnosis codes specifying degenerative disc disease (721.0-9, 722.0-9), spinal stenosis (724.0-09), scoliosis (737.0-acquired spondylolisthesis (738.4), trauma (800.0 – 899.9), and metastasis (198.3, 198.4, 198.5) as previously described (2,11,12).
Comorbidity profiles were analyzed by determining the prevalence of a number of disease states as defined in the Clinical Classification Software and provided in the NIS dataset (13). In order to determine overall comorbid burden, comorbidity indices were calculated as described by Charlson et al. (14) and adjusted for use with administrative data by Deyo et al. (15). Differences in in-hospital mortality between procedure sub-types were assessed. Subsequently, multivariate regression analysis was performed and odds ratios and 95% confidence intervals were calculated to determine independent predictors for in-hospital mortality.
Statistical Analysis
Significance of differences between procedure types were evaluated using a t-test for continuous, and chi-square test for categorical variables. A p-value of 0.05 was used to define significant differences. Continuous variables are presented as mean and standard error. Categorical variables are computed as percentages. For multivariate logistic regression analysis, control variables included in the model were: procedure type, age, gender, race, hospital size, location and teaching status, primary source of payment, indication for surgery and comorbidity index. Individual comorbidities were substituted for comorbidity index in order to determine the impact of specific comorbidities on mortality. A separate analysis was also conducted to identify the effect of peri-operative complications on mortality, while controlling for overall comorbidity burden (comorbidity index) and patient and health care system related demographics. For each individual predictor, odds ratio, 95% confidence interval and p-value were computed. All statistical analyses were performed using SAS version 9.1 (SAS Institutes, Cary, North Carolina). SAS procedures (e.g., SURVEYFREQ, and SURVEYLOGISTIC) were used in order to account for weighting, clustering and stratification in the NIS's complex survey design.
Results
Demographics
We identified a total of 261,356 admissions during which a primary spine fusion procedure was performed between 1998 and 2006. This represented a weighted national estimate of 1,273,228 hospitalizations. Of those 77.07% were PSF, 13.98% ASF, and 8.95% APSF. Patients undergoing ASF and APSF were on average significantly younger (44.8+/-0.08 and 44.22+/-0.11 years) then those undergoing PSF (52.12+/-0.04 years) (P<0.0001).
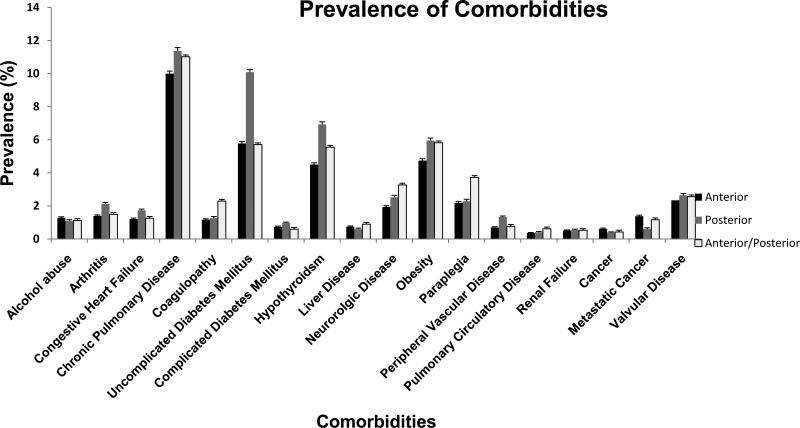
Table 1 contains information on patient and health care system related demographics. A significantly higher proportion of admissions undergoing spine fusions were female, and of white race. A higher proportion of admissions undergoing ASF and APSF were privately insured as compared to PSF, reflecting the lower average age of patients not qualifying for government services. Comparatively, more spine fusions were performed in urban centers and teaching institutions, especially APSF procedures. The majority of discharges were to the patients’ primary residence, however the proportion of non-routine discharges, including to skilled nursing facilities was higher for PSF and APSF patients. The average length of hospital stay was longest for APSF (7.63+/-0.06 days versus 5.65+/-0.04 days for ASF, and 5.15+/-0.01 days for PSF, P<0.0001). The prevalence of studied comorbidities for each procedure is shown in (Figure 1). Hypertension was the most commonly encountered disease recorded for either procedure type, affecting 21.44%+/-0.22 of ASF, 35.27%+/-0.11 of PSF and 23.27%+/-0.28 of APSF patients (P<0.0001).
Table 1.
Demographics of discharges after anterior, posterior, and anterior/posterior spine fusion.
| Demographics of Spine Surgery Discharges | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Spine Surgery Type | Anterior | Posterior | Anterior/Posterior | Total | P-Value | ||||
| N= (Unweighted (Weighted)) | 36224 | 177939 | 201885 | 981298 | 23247 | 113991 | 261356 | 1273228 | <0.0001 |
| % of total (SE) | 13.98 | 0.07 | 77.07 | 0.08 | 8.95 | 0.06 | 100 | 0 | |
| Variables | % | SE | % | SE | % | SE | % | SE | |
| Age groups (years) | <0.0001 | ||||||||
| 0-44 | 50.97 | 0.26 | 32.50 | 0.10 | 48.58 | 0.33 | 36.52 | 0.09 | |
| 45-64 | 39.21 | 0.26 | 39.70 | 0.11 | 41.18 | 0.32 | 39.77 | 0.10 | |
| 65-74 | 6.84 | 0.13 | 17.45 | 0.08 | 7.43 | 0.17 | 15.07 | 0.07 | |
| >75 | 2.98 | 0.09 | 10.35 | 0.07 | 2.81 | 0.11 | 8.65 | 0.06 | |
| Gender | <0.0001 | ||||||||
| Male | 45.97 | 0.26 | 44.43 | 0.11 | 46.07 | 0.33 | 44.79 | 0.10 | |
| Female | 54.03 | 0.26 | 55.57 | 0.11 | 53.93 | 0.33 | 55.21 | 0.10 | |
| Race | <0.0001 | ||||||||
| White | 83.71 | 0.22 | 83.97 | 0.10 | 80.65 | 0.30 | 83.63 | 0.08 | |
| Black | 6.35 | 0.15 | 6.71 | 0.07 | 5.99 | 0.18 | 6.59 | 0.06 | |
| Hispanic | 6.06 | 0.14 | 5.82 | 0.06 | 8.47 | 0.21 | 6.10 | 0.05 | |
| Other | 3.89 | 0.12 | 3.50 | 0.05 | 4.88 | 0.16 | 3.68 | 0.04 | |
| Insurance | <0.0001 | ||||||||
| Medicare | 13.83 | 0.18 | 30.02 | 0.10 | 13.74 | 0.23 | 26.31 | 0.09 | |
| Medicaid | 6.47 | 0.13 | 5.59 | 0.05 | 7.39 | 0.17 | 5.87 | 0.05 | |
| Private/ HMO | 56.75 | 0.26 | 48.88 | 0.11 | 57.77 | 0.33 | 50.77 | 0.10 | |
| Other | 22.96 | 0.22 | 15.51 | 0.08 | 21.10 | 0.27 | 17.05 | 0.07 | |
| Discharge Status | <0.0001 | ||||||||
| Routine | 79.10 | 0.21 | 69.63 | 0.10 | 70.49 | 0.30 | 71.03 | 0.09 | |
| Short Term Hospital | 0.57 | 0.04 | 0.53 | 0.02 | 0.71 | 0.06 | 0.55 | 0.01 | |
| Other transfers | 10.99 | 0.17 | 18.03 | 0.09 | 15.23 | 0.24 | 16.80 | 0.07 | |
| Home Health Care | 8.75 | 0.15 | 11.46 | 0.07 | 13.07 | 0.22 | 11.23 | 0.06 | |
| Against Medical Advice | 0.08 | 0.02 | 0.06 | 0.01 | 0.04 | 0.01 | 0.06 | 0.00 | |
| Died in Hospital | 0.51 | 0.04 | 0.26 | 0.01 | 0.44 | 0.04 | 0.31 | 0.01 | |
| Alive, Destination Unknown | 0.01 | 0.00 | 0.01 | 0.00 | 0.02 | 0.01 | 0.01 | 0.00 | |
| Hospital Size | <0.0001 | ||||||||
| Small | 11.69 | 0.15 | 10.82 | 0.04 | 16.13 | 0.22 | 11.42 | 0.01 | |
| Medium | 24.35 | 0.21 | 22.82 | 0.05 | 20.45 | 0.25 | 22.82 | 0.01 | |
| Large | 63.96 | 0.23 | 66.36 | 0.05 | 63.42 | 0.30 | 65.76 | 0.01 | |
| Hospital Location | <0.0001 | ||||||||
| Rural | 4.23 | 0.10 | 5.03 | 0.02 | 1.76 | 0.09 | 4.63 | 0.00 | |
| Urban | 95.77 | 0.10 | 94.97 | 0.02 | 98.24 | 0.09 | 95.37 | 0.00 | |
| Teaching Status | <0.0001 | ||||||||
| Non-teaching | 40.32 | 0.24 | 42.59 | 0.06 | 36.52 | 0.30 | 41.73 | 0.02 | |
| Teaching | 59.68 | 0.24 | 57.41 | 0.06 | 63.48 | 0.30 | 58.27 | 0.02 | |
SE= Standard Errors
Other transfer includes skilled nursing and intermediate care facility.
HMO=Health Maintenance Organization
Figure 1.
Depicted is the prevalence of studied comobidities by type of spine fusion. Error bars represent standard errors. P<0.0001 for all comorbidities between types of spine fusion.
The average comorbidity index among admissions for ASF and APSF (0.30+/-0.002 and 0.31+/-0.004) recipients was significantly lower compared to those for PSF (0.41+/-0.002), (P<0.0001). Table 2 details the incidence of various indications for spine fusion by surgical approach.
Table 2.
Incidence of various indications for spine fusion by procedure type.
| Indication for Spine Fusion by Procedure Type | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Anterior | Posterior | Anterior/Posterior | Total | P-Value | |||||
| Diagnosis | % | SE | % | SE | % | SE | % | SE | |
| Degenerative Disc Disease | 64.09 | 0.25 | 39.95 | 0.11 | 48.43 | 0.33 | 44.08 | 0.10 | <0.0001 |
| Spinal Stenosis | 2.30 | 0.08 | 9.64 | 0.07 | 2.15 | 0.10 | 7.95 | 0.05 | <0.0001 |
| Scoliosis | 5.92 | 0.12 | 6.18 | 0.05 | 12.42 | 0.22 | 6.70 | 0.05 | <0.0001 |
| Spondylolisthesis | 2.45 | 0.08 | 5.54 | 0.05 | 3.23 | 0.12 | 4.90 | 0.04 | <0.0001 |
| Trauma | 5.80 | 0.12 | 4.24 | 0.05 | 2.94 | 0.11 | 4.34 | 0.04 | <0.0001 |
| Metastasis | 1.98 | 0.07 | 0.78 | 0.02 | 1.58 | 0.08 | 1.02 | 0.02 | <0.0001 |
| Multiple Diagnoses | 10.29 | 0.16 | 28.14 | 0.10 | 21.78 | 0.27 | 25.07 | 0.09 | <0.0001 |
| Other | 7.13 | 0.14 | 5.48 | 0.05 | 7.45 | 0.17 | 5.89 | 0.05 | <0.0001 |
SE= Standard Errors
Outcomes
Complications categorized as procedure related were more frequent among APSF hospitalizations (23.81%+/-0.28) as compared to ASF (18.68%+/-0.21), and PSF (15.72%+/-0.08) patients, (P<0.0001). Table 3 shows the incidence of organ specific complications.
Table 3.
Incidence of procedure related complications (ICD 9-CM 996.X to 999.X) after spine fusion surgery.
| Procedure Related Complications After Spine Fusion | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Anterior | Posterior | Anterior/Posterior | Total | P-Value | |||||
| % | SE | % | SE | % | SE | % | SE | ||
| Device Related Complications | |||||||||
| Device Related | 5.37 | 0.12 | 3.52 | 0.04 | 6.01 | 0.16 | 4.00 | 0.04 | <0.0001 |
| Organ Specific Complications | |||||||||
| CNS | 0.35 | 0.03 | 1.02 | 0.02 | 0.76 | 0.06 | 0.90 | 0.02 | <0.0001 |
| Cardiac | 0.83 | 0.05 | 0.94 | 0.02 | 1.49 | 0.08 | 0.98 | 0.02 | <0.0001 |
| Peripheral Vascular | 0.27 | 0.03 | 0.08 | 0.01 | 0.32 | 0.04 | 0.13 | 0.01 | <0.0001 |
| Respiratory | 2.37 | 0.08 | 1.50 | 0.03 | 3.82 | 0.13 | 1.83 | 0.03 | <0.0001 |
| Gastrointestinal | 4.76 | 0.11 | 2.14 | 0.03 | 5.55 | 0.15 | 2.81 | 0.03 | <0.0001 |
| Genitourinary | 0.90 | 0.05 | 1.07 | 0.02 | 1.22 | 0.07 | 1.06 | 0.02 | <0.0001 |
| Other Complications of Procedure | |||||||||
| Shock | 0.08 | 0.01 | 0.08 | 0.01 | 0.17 | 0.03 | 0.09 | 0.01 | <0.0001 |
| Hematoma/Seroma | 1.46 | 0.06 | 1.55 | 0.03 | 2.66 | 0.11 | 1.64 | 0.03 | <0.0001 |
| Puncture Vessel/Nerve | 3.07 | 0.09 | 3.28 | 0.04 | 4.02 | 0.13 | 3.31 | 0.04 | <0.0001 |
| Wound Dehiscence | 0.23 | 0.03 | 0.19 | 0.01 | 0.53 | 0.05 | 0.23 | 0.01 | <0.0001 |
| Infection | 0.80 | 0.05 | 0.54 | 0.02 | 1.20 | 0.07 | 0.63 | 0.02 | <0.0001 |
| Other | 1.78 | 0.07 | 2.17 | 0.03 | 2.20 | 0.10 | 2.12 | 0.03 | <0.0001 |
| Medical Complication | 0.17 | 0.02 | 0.19 | 0.01 | 0.32 | 0.04 | 0.20 | 0.01 | <0.0001 |
CNS= Central Nervous System
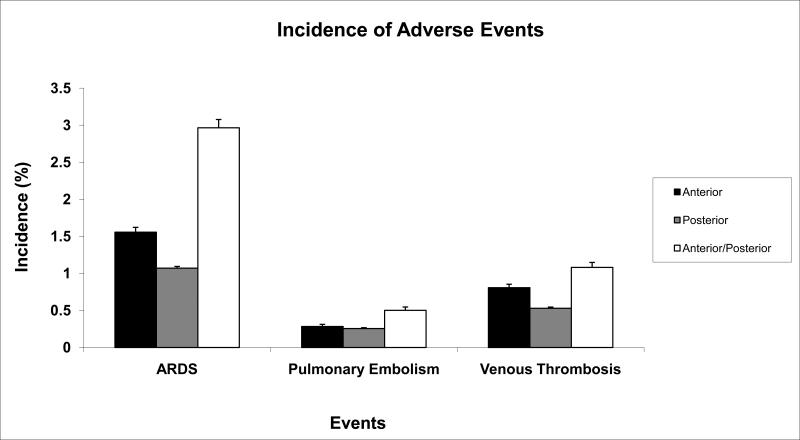
The incidence of pulmonary embolism, venous thrombosis, and ARDS was also increased among APSF patients (Figure 2). Acute posthemorrhagic anemia was coded at about double the rate among APSF (14.58%+/-0.23) and PSF (12.22%+/-0.07) patients compared to ASF procedures (6.85%+/-0.13), (P<0.0001)). This was reflected in the need for blood transfusions, which was highest in APSF (20.35%+/-0.27) and lowest in ASF patients (9.33%+/-0.15) (17.39%+/-0.08 for PSF), (P<0.0001). The incidence of procedure related complications by surgical site is shown in figure 3. Procedures involving the anterior thoracic approach had the highest rate of complications.
Figure 2.
The incidence of ARDS (Adult Respiratory Distress Syndrome), Pulmonary Embolism , and Venous Thrombosis is shown for the three types of spine fusion studied. P<0.0001 for all adverse events between types of spine fusion.
Figure 3.
Shown is the incidence of procedure related complications (ICD-9-CM 996.X to 999.X) for various surgical sites. P<0.0001
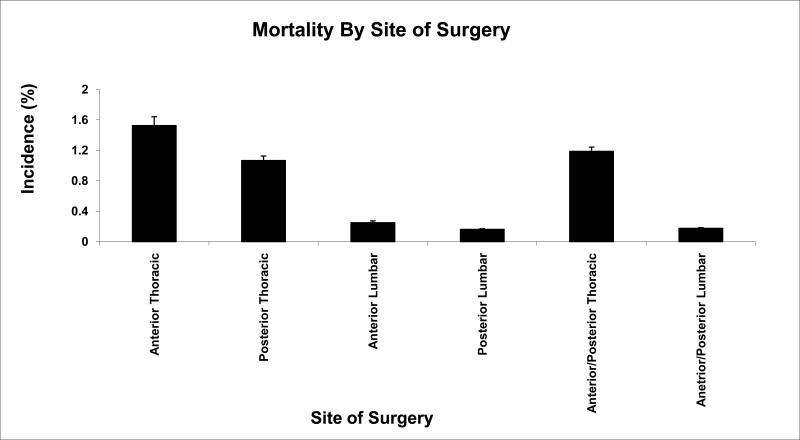
In-hospital mortality was significantly higher among ASF (0.51%+/-0.04) and APSF (0.44%+/- 0.04) compared to PSF recipients (0.26%+/-0.01), (P<0.0001). The thoracic approach was associated with the highest rates of a perioperative fatal event (Figure 4).
Figure 4.
Illustrated is the incidence of in-hospital mortality for various surgical sites. P=0.0001
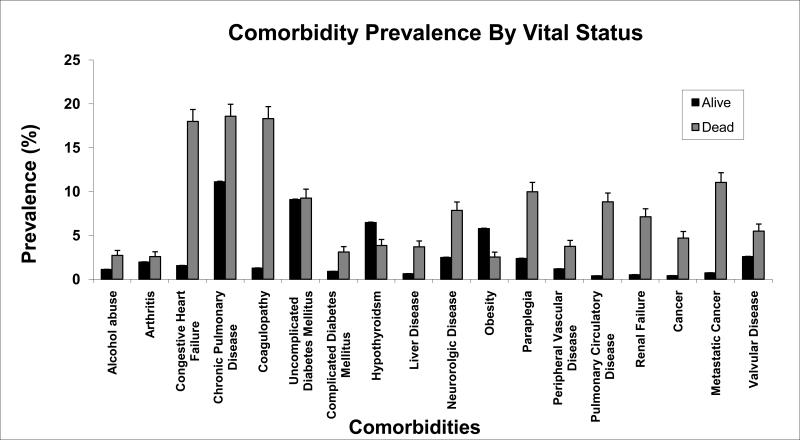
Table 4 details demographics of the patient population with a fatal outcome compared to non-fatalities. The average age among mortalities was 63.99 +/-0.60 years. Fatal events occurred in patients with a significantly higher average comorbidity index (0.82+/-0.04) compared to the overall patient spine surgical population (0.38+/-0.002), (P<0.0001). The prevalence of all studied comorbidities was generally higher among deaths when compared to patients that survived their spine fusion, except for hypothyroidsm and obesity (Figure 5). Electrolyte and fluid abnormalities were significantly more frequent among mortalities when compared to survivors (33.13%+/-1.66 vs. 6.19%+/-0.05, P<0.0001). Length of stay among mortalities was 19.14+/-0.76 days. Procedure related complications were also more frequent among fatalities (Table 5). The incidence of ARDS, pulmonary embolism and venous thromboembolism was increased in patients that died after surgery (22.50%+/-1.48 vs. 1.23%+/-0.02, 7.74%+/-0.94 vs. 0.26%+/-0.01, and 6.29%+/-0.85 vs. 0.60%+/-0.02, respectively, P<0.0001).
Table 4.
Demographics of hospitalizations with a non-fatal versus fatal outcome after spine fusion surgery.
| Demographics of Spine Fusion Discharges by Vital Status | |||||
|---|---|---|---|---|---|
| Vital Status | Alive | Dead | p-value | ||
| N= Unweighted (Weighted) | 259,807 | 1,265,815 | 806 | 3,990 | |
| % | SE | % | SE | ||
| Type of TKA | <0.0001 | ||||
| Anterior | 99.49 | 0.04 | 0.51 | 0.04 | |
| Posterior | 99.74 | 0.01 | 0.26 | 0.01 | |
| Anterior/Posterior | 99.56 | 0.04 | 0.44 | 0.04 | |
| Age groups (years) | <0.0001 | ||||
| 0-44 | 36.65 | 0.09 | 10.60 | 1.09 | |
| 45-64 | 39.80 | 0.10 | 31.08 | 1.64 | |
| 65-75 | 15.00 | 0.07 | 28.42 | 1.60 | |
| >75 | 8.56 | 0.06 | 29.90 | 1.62 | |
| Gender | <0.0001 | ||||
| Male | 44.79 | 0.10 | 56.42 | 1.75 | |
| Female | 55.21 | 0.10 | 43.58 | 1.75 | |
| Race | 0.06 | ||||
| White | 83.65 | 0.08 | 82.14 | 1.58 | |
| Black | 6.59 | 0.06 | 8.32 | 1.14 | |
| Hispanic | 6.07 | 0.05 | 5.61 | 0.94 | |
| Other | 3.68 | 0.04 | 3.93 | 0.81 | |
| Insurance | <0.0001 | ||||
| Medicare | 26.16 | 0.09 | 56.27 | 1.76 | |
| Medicaid | 5.87 | 0.05 | 7.19 | 0.92 | |
| Private/ HMO | 50.87 | 0.10 | 29.88 | 1.62 | |
| Other | 17.10 | 0.07 | 6.66 | 0.87 | |
| Hospital Size | <0.0001 | ||||
| Small | 11.44 | 0.01 | 5.69 | 0.79 | |
| Medium | 22.84 | 0.01 | 20.56 | 1.42 | |
| Large | 65.72 | 0.01 | 73.76 | 1.54 | |
| Hospital Location | 0.06 | ||||
| Rural | 4.65 | 0.00 | 2.82 | 0.60 | |
| Urban | 95.35 | 0.00 | 97.18 | 0.60 | |
| Teaching Status | 0.67 | ||||
| Non-teaching | 41.72 | 0.02 | 29.70 | 1.60 | |
| Teaching | 58.28 | 0.02 | 70.30 | 1.60 | |
SE= Standard Error
HMO=Health Maintenance Organization
Figure 5.
Shown is the prevalence of studied comorbidities among non-fatalities and fatalities after spine fusion surgery. P<0.0001 for all comorbidities, except uncomplicated diabetes mellitus (P= 0.7056).
Table 5.
Procedure related complications (ICD 9-CM 996.X to 999.X) after spine fusion surgery by vital status.
| Procedure Related Complications After Spine Fusion by Vital Status | |||||
|---|---|---|---|---|---|
| Vital Status | Alive | Dead | |||
| % | SE | % | SE | P-value | |
| Device Related Complications | |||||
| Device Related | 3.98 | 0.04 | 9.56 | 1.04 | <0.0001 |
| Organ Specific Complications | |||||
| CNS | 9.56 | 1.04 | 5.69 | 0.82 | <0.001 |
| Cardiac | 0.93 | 0.02 | 15.42 | 1.28 | <0.001 |
| Peripheral Vascular | 0.13 | 0.01 | 1.20 | 0.38 | <0.0001 |
| Respiratory | 1.80 | 0.03 | 7.89 | 0.95 | <0.0001 |
| Gastrointestinal | 2.80 | 0.03 | 5.21 | 0.79 | <0.0001 |
| Genitourinary | 1.06 | 0.02 | 2.32 | 0.54 | <0.0001 |
| Other Complications of Procedure | |||||
| Shock | 0.07 | 0.01 | 3.75 | 0.67 | <0.0001 |
| Hematoma/Seroma | 1.62 | 0.02 | 7.99 | 0.95 | <0.0001 |
| Puncture Vessel/Nerve | 3.30 | 0.04 | 5.19 | 0.78 | <0.0001 |
| Wound Dehiscence | 0.22 | 0.01 | 2.54 | 0.56 | <0.0001 |
| Infection | 0.62 | 0.02 | 6.39 | 0.87 | <0.0001 |
| Other | 2.12 | 0.03 | 1.48 | 0.42 | <0.0001 |
| Medical Complication | 0.20 | 0.01 | 0.40 | 0.23 | <0.0001 |
SE=Standard Error
CNS= Central Nervous System
Multivariate regression revealed a number of independent risk factors for mortality after spine fusions. When controlling for comorbidity severity, patient related factors that significantly increased the risk for perioperative mortality were male gender (OR 1.58 (1.37;1.84), (P<0.0001)), and increasing age. The age group between 65 and 74 years had a 2.4-fold increase (OR 2.36 (1.77; 3.14) (P<0.0001)) and the group >75 years at 4.5-fold increase (OR 4.53 (3.35; 6.13), (P<0.0001) in the risk for mortality when compared to those aged 45-65 years of age. Entries for ASF and APSF were associated with a significantly increased risk for mortality (OR 1.84(1.53; 2.22) (P<0.0001) and OR 1.91 (1.52; 2.39) (P<0.0001), respectively) compared to PSF. There was no difference in the risk for mortality between APSF and ASF procedures (P=0.3048). Patients of black race had a moderately increased risk for perioperative mortality compaared to their white counterparts (OR 1.44(1.06; 1.96), (P=0.0196)).
A number of comorbidities increased the risk of a fatal outcome (Table 6). Pulmonary circulatory disease was associated with the highest increase in the risk for perioperative mortality (OR 8.37 (5.95; 11.78), (P<0.0001). Each point increase in comorbidity index was associated with a 13%-increase of perioperative mortality risk (OR 1.13(1.04; 1.22), (P<0.0018).
Table 6.
Comorbidities as independent risk factors for in-hospital mortality after spine fusion surgery.
| Risk Factors for Peripoerative Mortality after Spine Fusion-Comorbidities | ||||
|---|---|---|---|---|
| Comorbidity | Odds Ratio | Lower −95%CI | Upper −95%CI | P-Value |
| Alcohol Abuse | 0.74 | 0.43 | 1.28 | 0.2849 |
| Arthritis | 1.05 | 0.67 | 1.65 | 0.8202 |
| Hypothyroidsm | 0.51 | 0.35 | 0.75 | 0.0007 |
| Chronic Lung Disease | 1.25 | 1.03 | 1.53 | 0.0260 |
| Congestive Heart Failure | 3.42 | 2.70 | 4.34 | <.0001 |
| Uncomplicated Diabetes Mellitus | 1.46 | 1.12 | 1.91 | 0.0051 |
| Complicated Diabetes Mellitus | 1.13 | 0.70 | 1.82 | 0.6179 |
| Liver Disease | 2.88 | 1.78 | 4.64 | <.0001 |
| Coagulopathy | 5.46 | 4.34 | 6.86 | <.0001 |
| Neurologic Disorders | 2.54 | 1.89 | 3.40 | <.0001 |
| Obesity | 0.69 | 0.44 | 1.10 | 0.1183 |
| Peripheral Vascular Disease | 1.58 | 1.03 | 2.43 | 0.0383 |
| Renal Disease | 3.43 | 2.38 | 4.96 | <.0001 |
| Pulmonary Circulatory Disease | 8.37 | 5.95 | 11.78 | <.0001 |
| Cardiac Valvular Disorders | 1.07 | 0.76 | 1.51 | 0.6959 |
| Electrolyte/Fluid Abnormalities | 2.48 | 2.07 | 2.97 | <.0001 |
| Metastatic Cancer | 1.79 | 1.05 | 3.05 | 0.0324 |
| Cancer | 1.68 | 0.98 | 2.87 | 0.0580 |
| Paraplegia | 1.62 | 1.23 | 2.13 | 0.0006 |
CI=Confidence Interval
When controlling for comorbidity severity, indication for surgery, and patient and health care system related demographics, a number of procedure related complications and adverse events were associated with an increased risk for perioperative mortality (Table 7). Among admissions with the highest risk for mortality were those complicated by cardiac and central nervous system events, ARDS and pulmonary embolism. Local complications such as infection, wound dehiscence and hematoma formation also increased the risk of death.
Table 7.
Complications as independent risk factors for in-hospital mortality after spine fusion surgery.
| Risk Factors for Peripoerative Mortality after Spine Fusion-Complications | ||||
|---|---|---|---|---|
| Comorbidity | Odds Ratio | Lower −95%CI | Upper −95%CI | P-Value |
| Posthemmorhagic Anemia | 1.22 | 0.97 | 1.54 | 0.0004 |
| ARDS | 5.85 | 4.65 | 7.37 | 0.0932 |
| Pulmonary Embolism | 8.17 | 5.34 | 12.50 | <.0001 |
| Thrombosis | 0.53 | 0.35 | 0.81 | <.0001 |
| Device Related | 1.22 | 0.92 | 1.63 | 0.0034 |
| CNS | 4.19 | 2.88 | 6.10 | 0.165 |
| Cardiac | 6.88 | 5.20 | 9.11 | <.0001 |
| Peripheral Vascular | 1.10 | 0.40 | 3.04 | <.0001 |
| Respiratory | 1.45 | 1.03 | 2.05 | 0.8586 |
| Gastrointestinal | 1.25 | 0.86 | 1.83 | 0.0333 |
| Genitourinary | 1.03 | 0.59 | 1.78 | 0.2467 |
| Shock | 8.18 | 4.27 | 15.65 | <.0001 |
| Hematoma/Seroma | 1.67 | 1.15 | 2.42 | 0.007 |
| Puncture Vessel/Nerve | 1.17 | 0.81 | 1.69 | 0.4012 |
| Wound Dehiscence | 1.94 | 1.02 | 3.66 | 0.0421 |
| Infection | 2.40 | 1.60 | 3.61 | <.0001 |
| Blood transfusion | 1.12 | 0.92 | 1.35 | 0.257 |
ARDS= Adult Respiratory Distress Syndrome
CI=Confidence Interval
CNS= Central Nervous System
When evaluating the impact of various indications for surgery on in-hospital mortality, adjusted risk was highest among those undergoing fusion for metastatic disease and trauma. Compared to degenerative indications for surgery the former were associated with an 18- and 14-fold increased risk for perioperative mortality (table 8).
Table 8.
Spine pathologies as independent risk factors for in-hospital mortality after spine fusion surgery. Odds ratios are comparative to the diagnosis of degenerative disc disease.
| Risk Factors for Peripoerative Mortality after Spine Fusion-Spine Pathology (Referent: Degenerative Disc Disease) | ||||
|---|---|---|---|---|
| Pathology | Odds Ratio | Lower −95%CI | Upper −95%CI | P-Value |
| Spinal Stenosis | 1.18 | 0.85 | 1.62 | 0.3256 |
| Scoliosis | 5.27 | 3.77 | 7.35 | <.0001 |
| Spondylolisthesis | 1.26 | 0.80 | 1.99 | 0.3198 |
| Trauma | 14.08 | 10.99 | 18.03 | <.0001 |
| Metastasis | 18.41 | 13.96 | 24.28 | <.0001 |
| Multiple Diagnoses | 0.82 | 0.63 | 1.07 | 0.1479 |
| Other | 6.85 | 5.37 | 8.73 | <.0001 |
CI= Confidence Interval
Discussion
In this study of nationally representative data collected for the NIS between the years of 1998 and 2006 we found an increased incidence of perioperative complications and adjusted risk of in-hospital mortality among hospital admissions undergoing APSF and ASF when compared to PSF procedures. The highest rates of fatal outcomes and complications were associated with procedures utilizing the anterior thoracic approach. Risk factors for in-hospital mortality included: male gender, advanced age, procedures indicated for metastatic disease and trauma as well as the presence of a number of comorbidities and perioperative complications.
In view of the increasing utilization of spine fusion procedures, these findings are of importance to the perioperative physician, in order to better assess the chance of morbidity and mortality, identify patients at risk and adequately inform patients of such risks before embarking on this procedure.
Procedures involving the anterior spine were associated with higher morbidity and mortality in our study, despite being performed in younger individuals with lower comorbidity burden. The risk of perioperative mortality was increased even when controlling for the indication for surgery. Complications associated with the anterior approach have long been recognized (16), but a paucity of comparative analysis addressing outcome in this patient population exists. The reason for the increased rate of complications is likely associated with the entry of the abdominal and thoracic cavity and the proximity of vital organs (16). This fact is supported by our finding of increased gastrointestinal and pulmonary complications among patients undergoing APSF and ASF compared to PSF procedures. The highest rate of morbidity and mortality was seen in APSF patients, which can be explained by longer surgical times, more blood loss and increased surgical complexity. Shen et al., without studying the specific approach, identified thoracic procedures to be associated with higher rates of complications and mortality compared to lumbar fusions (9), which is in concordance with our findings.
While the approach is often dictated by the individual patient's condition, newer access methods utilizing the retroperitoneal space, thus avoiding intra abdominal structures, and thoracoscopic exploration may be considered to reduce morbidity and mortality whenever feasible (17, 18, 19). Unfortunately, information on the utilization of these particular techniques is not discernable from the NIS data and their impact could therefore not be studied.
When studying patient demographics and their association with mortality, we found increased independent risk of a fatal event after spine fusion among men. Although this finding has been reported in the past in spine surgery patients (9, 20), little is known about the causality between gender and mortality risk.
We identified an increased incidence of morbidity and risk for mortality in patients with advanced age. Patients over the age of 75 made up almost one third of all mortalities, despite representing less than 9% of the spine surgical population in this study. Similarly, Li et al. was able to show that mortality increased in elderly patients after lumbar laminectomy compared to their younger counterparts. He further concluded that mortality was higher in the patient population over 85 years of age when comorbidities were present compared to otherwise healthy, elderly individuals (1.4% vs. 0.22%) (21). In our study of spine fusion patients, advanced age remained an independent predictor for mortality even when controlling for comorbidity burden. However, it must be mentioned that advanced age has not consistently been associated with increased mortality in the past (22, 23).
Increasing comorbidity burden and the presence of a number of diseases were associated with an increase in mortality risk in this and other studies (9, 20, 21). Pulmonary circulatory disease, congestive heart failure, renal disease and coagulopathies were associated with the highest increases of risk for perioperative mortality. While the latter comorbidities have been implicated as risk factors in the past (9), pulmonary circulatory disease as a risk factor has been less well documented. Patients with pulmonary hypertension and decreased right ventricular reserve may be less likely to deal with the consequences of pulmonary embolization of bone and marrow material during instrumentation, resulting in increases in pulmonary vascular resistance. Urban et al. was able to demonstrate an adverse pulmonary effect of perioperative events in the form of an increase in pulmonary vascular resistance in 15% (8/55) of patients undergoing anterior/posterior spine fusion, usually during or after posterior instrumentation (24). In a follow up study, the same author analyzed bronchoalveolar specimens and linked the presence of lipid laden macrophages to possible embolization of fat and debris entering the blood stream during the surgical procedure (25). This mechanism of lung injury is supported by echocardiographic studies, in which 80% of spine surgery patients experienced moderate to severe embolic events during instrumentation of the spine (26).
Perioperative complications were also associated with increases in the odds of a fatal event. Pulmonary embolism, perioperative shock, ARDS and cardiac complications were associated with the highest risk of mortality. All of these events had the highest incidence among APSF patients. While the mentioned findings are not surprising, it is noteworthy that local surgical complications including infection, wound dehiscence and hematoma/seroma formation also significantly increased the risk for mortality. The impact of wound complications, especially infections has been studied in the past and has been associated with increased morbidity and mortality (27). Our data confirm the importance of measures to reduce this complication and implement strategies to achieve this goal (28, 29).
This study is limited by a number of factors inherent to secondary data analysis of large administrative databases. As such, clinical information and that detailing the surgical procedure (i.e. type of anesthesia, amount of blood loss, length of surgery etc.) available in the NIS is limited and our analysis must be interpreted in this context. Although gathering data on the number of levels operated on may theoretically be possible through the use of the ICD-9-CM coding system, this information was missing in about two thirds of patient entries, thus making the inclusion of this variable in our analysis not feasible. Because of the nature of the NIS, only in-patient data are available and thus complications and events after discharge are not captured. Furthermore, readmissions cannot be discerned from this database. Thus, conclusions should be limited to the acute perioperative setting with the notion that mortality and complications are likely underestimated.
An additional limiting factor is the bias associated with the retrospective nature of our study. Nevertheless, because of the availability of data from a large, nationally representative sample, this type of analysis may provide a more accurate estimate of events surrounding primary non-cervical spine fusion procedures than various prospective studies that are limited in sample size and thus lack the ability to capture low-incidence outcomes.
In conclusion, using a nationally representative database we determined that APSF and ASF carried an increased adjusted risk of in-hospital mortality and greater incidence of in-hospital complications when compared to PSF procedures.
Until more data are available, careful selection of candidates for ASF and APSF and an in depth discussion about risks and alternatives with the patient cannot be overemphasized. Risk factors identified in this analysis may be used to gage the preoperative mortality risk for individual patients.
Acknowledgments
Financial disclosure: This study was performed with funds from the Hospital for Special Surgery Anesthesiology Young Investigator Award provided by the Department of Anesthesiology at the Hospital for Special Surgery (Stavros G. Memtsoudis) and Center for Education and Research in Therapeutics (CERTs) (AHRQ RFA-HS-05-14) and Clinical Translational Science Center (CTSC) (NIH UL1-RR024996) (Yan Ma). No conflicts of interest arise from any part of this study for any of the authors.
Footnotes
As data used in this study are sufficiently de-identified, the use of this study was exempt from review by the institutional review board.
References
- 1.Deyo RA, Gray DT, Kreuter W, et al. United States trends in lumbar fusion surgery for degenerative conditions. Spine. 2005;30:1441–5. doi: 10.1097/01.brs.0000166503.37969.8a. discussion 1446-7. [DOI] [PubMed] [Google Scholar]
- 2.Cowan JA, Jr, Dimick JB, Wainess R, et al. Changes in the utilization of spinal fusion in the United States. Neurosurgery. 2006;59:15–20. doi: 10.1227/01.NEU.0000219836.54861.CD. [DOI] [PubMed] [Google Scholar]
- 3.Hamdan AD, Malek JY, Schermerhorn ML, et al. Vascular injury during anterior exposure of the spine. J Vasc Surg. 2008;48:650–4. doi: 10.1016/j.jvs.2008.04.028. Epub 2008 Jun 30. [DOI] [PubMed] [Google Scholar]
- 4.Li G, Patil CG, Lad SP, Ho C, Tian W, Boakye M. Effects of age and comorbidities on complication rates and adverse outcomes after lumbar laminectomy in elderly patients. Spine. 2008;33:1250–5. doi: 10.1097/BRS.0b013e3181714a44. [DOI] [PubMed] [Google Scholar]
- 5.Cho KJ, Suk SI, Park SR, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine. 2007;32:2232–7. doi: 10.1097/BRS.0b013e31814b2d3c. [DOI] [PubMed] [Google Scholar]
- 6.Browne JA, Cook C, Pietrobon R, et al. Diabetes and early postoperative outcomes following lumbar fusion. Spine. 2007;32:2214–9. doi: 10.1097/BRS.0b013e31814b1bc0. [DOI] [PubMed] [Google Scholar]
- 7.Hee HT, Castro FP, Jr, Majd ME, et al. Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: analysis of complications and predictive factors. J Spinal Disord. 2001;14:533–40. doi: 10.1097/00002517-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Pradhan BB, Nassar JA, Delamarter RB, et al. Single-level lumbar spine fusion: a comparison of anterior and posterior approaches. J Spinal Disord Tech. 2002;15:355–61. doi: 10.1097/00024720-200210000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Shen Y, Silverstein JC, Roth S. In-hospital complications and mortality after elective spinal fusion surgery in the united states: a study of the nationwide inpatient sample from 2001 to 2005. J Neurosurg Anesthesiol. 2009;21:21–30. doi: 10.1097/ANA.0b013e31818b47e9. [DOI] [PubMed] [Google Scholar]
- 10.HCUP Databases. Healthcare Cost and Utilization Project (HCUP) July 2008 Agency for Healthcare Research and Quality. Rockville, MD: [February 12, 2009]. www.hcup-us.ahrq.gov/nisoverview.jsp. Last modified 7/11/08. [Google Scholar]
- 11.Patil CG, Patil TS, Lad SP, Boakye M. Complications and outcomes after spinal cord tumor resection in the United States from 1993 to 2002. Spinal Cord. 2008;46:375–9. doi: 10.1038/sj.sc.3102155. [DOI] [PubMed] [Google Scholar]
- 12.Patil CG, Lad SP, Santarelli J, Boakye M. National inpatient complications and outcomes after surgery for spinal metastasis from 1993-2002. Cancer. 2007;110:625–30. doi: 10.1002/cncr.22819. [DOI] [PubMed] [Google Scholar]
- 13.HCUP CCS. Healthcare Cost and Utilization Project (HCUP) May 2008 Agency for Healthcare Research and Quality. Rockville, MD: [February 12, 2009]. www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Last modified 5/12/08. [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 16.Ikard RW. Methods and complications of anterior exposure of the thoracic and lumbar spine. Arch Surg. 2006;141:1025–34. doi: 10.1001/archsurg.141.10.1025. [DOI] [PubMed] [Google Scholar]
- 17.Das K, Rawanduzy A, Couldwell WT. Posterolateral approach for decompression with anterior and posterior fusion: a less invasive surgical technique for stabilization of the thoracic spine. Case report. Neurosurg Focus. 1998;4:e3. doi: 10.3171/foc.1998.4.2.6. [DOI] [PubMed] [Google Scholar]
- 18.Amini A, Beisse R, Schmidt MH. Thoracoscopic spine surgery for decompression and stabilization of the anterolateral thoracolumbar spine. Neurosurg Focus. 2005;19:E4. [PubMed] [Google Scholar]
- 19.Börm W, Hübner F, Haffke T, et al. Approach-related complications of transthoracic spinal reconstruction procedures. Zentralbl Neurochir. 2004;65:1–6. doi: 10.1055/s-2004-44889. [DOI] [PubMed] [Google Scholar]
- 20.Oldridge NB, Yuan Z, Stoll JE, et al. Lumbar spine surgery and mortality among Medicare beneficiaries, 1986. Am J Public Health. 1994;84:1292–8. doi: 10.2105/ajph.84.8.1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li G, Patil CG, Lad SP, et al. Effects of age and comorbidities on complication rates and adverse outcomes after lumbar laminectomy in elderly patients. Spine. 2008;33:1250–5. doi: 10.1097/BRS.0b013e3181714a44. [DOI] [PubMed] [Google Scholar]
- 22.Cassinelli EH, Eubanks J, Vogt M, et al. Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis: an analysis of 166 patients. Spine. 2007;32:230–5. doi: 10.1097/01.brs.0000251918.19508.b3. [DOI] [PubMed] [Google Scholar]
- 23.Raffo CS, Lauerman WC. Predicting morbidity and mortality of lumbar spine arthrodesis in patients in their ninth decade. Spine. 2006;31:99–103. doi: 10.1097/01.brs.0000192678.25586.e5. [DOI] [PubMed] [Google Scholar]
- 24.Urban MK, Jules-Elysee KM, Beckman JB, et al. Pulmonary injury in patients undergoing complex spine surgery. Spine J. 2005;5:269–76. doi: 10.1016/j.spinee.2004.10.049. [DOI] [PubMed] [Google Scholar]
- 25.Urban MK, Urquhart B, Boachie-Adjei O. Evidence of lung injury during reconstructive surgery for adult spinal deformities with pulmonary artery pressure monitoring. Spine. 2001;26:387–90. doi: 10.1097/00007632-200102150-00015. [DOI] [PubMed] [Google Scholar]
- 26.Takahashi S, Kitagawa H, Ishii T. Intraoperative pulmonary embolism during spinal instrumentation surgery. A prospective study using transoesophageal echocardiography. J Bone Joint Surg Br. 2003;85:90–4. doi: 10.1302/0301-620x.85b1.13172. [DOI] [PubMed] [Google Scholar]
- 27.Kirkland KB, Briggs JP, Trivette SL, et al. The impact of surgical-site infections in the 1990s: Attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999;20:725–730. doi: 10.1086/501572. [DOI] [PubMed] [Google Scholar]
- 28.Olsen MA, Mayfield J, Lauryssen C, et al. Risk factors for surgical site infection in spinal surgery. J Neurosurg. 2003;98:149–155. [PubMed] [Google Scholar]
- 29.Maragakis LL, Cosgrove SE, Martinez EA, et al. Intraoperative fraction of inspired oxygen is a modifiable risk factor for surgical site infection after spinal surgery. Anesthesiology. 2009;110:556–62. doi: 10.1097/ALN.0b013e3181974be7. [DOI] [PubMed] [Google Scholar]