Abstract
AIM: To investigate the association of colorectal adenomas with both Helicobacter pylori (H. pylori) infection and metabolic syndrome.
METHODS: Using a cross-sectional hospital-based study, we analyzed physical examination data from 9311 healthy subjects with overnight physical examinations performed between January 2004 and December 2006. Examined data included gender, age, life style, anthropometric measurements, blood pressure, biochemical and hematological studies, H. pylori infection detected by esophagogastroduodenoscopy and biopsy urease tests, and colorectal adenomas detected with a complete total colonoscopy.
RESULTS: The prevalence values for H. pylori infection, metabolic syndrome, and colorectal adenoma were 39.2%, 18.7%, and 20.7%, respectively. Colorectal adenoma risk factors included male gender [odd ratio (OR): 2.005, 95% confidence interval (CI): 1.740-2.310, P < 0.001], advanced age (OR: 1.046, 95% CI: 1.040-1.052, P < 0.001), smoking (OR: 1.377, 95% CI: 1.146-1.654, P = 0.001), increased body fat (OR: 1.016, 95% CI: 1.007-1.026, P = 0.001), higher white blood cell count (OR: 1.038, 95% CI: 1.005-1.073, P = 0.025), H. pylori infection (OR: 1.366, 95% CI: 1.230-1.517, P < 0.001), and metabolic syndrome (OR: 1.408, 95% CI: 1.231-1.610, P < 0.001). In addition, concomitant H. pylori infection with metabolic syndrome further increased the probability of colorectal adenomas.
CONCLUSION: Our study revealed H. pylori infection with concomitant metabolic syndrome might further increase the risk of colorectal adenomas.
Keywords: Biopsy urease test, Colorectal adenoma, Colorectal cancer, Helicobacter pylori, Metabolic syndrome
INTRODUCTION
Colorectal cancer is an extremely common malignancy and one of the leading causes of cancer mortality worldwide. Colorectal adenoma is the premalignant lesion in colorectal cancer and develops into colorectal carcinoma through the adenoma-to-carcinoma sequence[1]. The direct etiology of colorectal neoplasms is still unknown. However, previous epidemiological studies have identified family history, dietary factors, smoking, sedentary lifestyles, and alcohol consumption as potential contributors to colorectal neoplasm development[2]. Identification of the etiology of colorectal neoplasms might assist in the development of strategies targeted toward its prevention.
Helicobacter pylori (H. pylori) is a human pathogen that infects the gastric mucosa and causes inflammatory process that culminate in chronic gastritis, peptic ulceration, gastric lymphoma of mucosa-associated lymphoid tissue, and adenocarcinoma[3]. H. pylori is a gram-negative microaerophilic bacillus, and has been classified by the International Agency for Research on Cancer as a class I human carcinogen since 1994[4]. The role of H. pylori in colorectal carcinogenesis has been epidemiologically examined in recent decades; however, the association has remained inconclusive. Several studies have identified an association between H. pylori infection and colorectal neoplasms[5-9], while others have identified a negative association between the two[10-12]. Methodological issues might account for some of the inconsistent results, including the IgG serum antibody test and incomplete colonoscopic examinations for diagnosis.
Metabolic syndrome is a clinical cluster of metabolic abnormalities. It is also referred to as insulin resistance syndrome, and is diagnosed by criteria corresponding to the modified National Cholesterol Education Program (NCEP) criteria[13]. Diagnosis is fulfilled by the presence of any three of the following conditions: higher waist circumference (≥ 90 cm in men and ≥ 80 cm in women), elevated triglycerides (≥ 150 mg/dL), lower high density lipoprotein cholesterol (< 40 mg/dL in men and < 50 mg/dL in women), elevated blood pressure (systolic blood pressure ≥ 130 mmHg or diastolic blood pressure ≥ 85 mmHg), and elevated fasting glucose (≥ 100 mg/dL). This syndrome might be a risk factor for type 2 diabetes and cardiovascular disease[14,15]. In recent years, metabolic syndrome has also been associated with an increased risk of colorectal adenoma. However, there is very limited medical literature examining the relationship between colorectal adenoma and metabolic syndrome[16-18]. Additional information on the correlation between metabolic syndrome and colorectal neoplasms could result in the recommendation for screening of colorectal neoplasms in the patient with metabolic syndrome.
Using a cross-sectional hospital-based study, we investigated the association of colorectal adenoma with both H. pylori infection and metabolic syndrome. Further, the probability of colorectal adenoma in patients with both H. pylori infection and metabolic syndrome was evaluated.
MATERIALS AND METHODS
A total of 11 787 asymptomatic subjects were admitted to the general physical examination department of the Buddhist Dalin Tzu-Chi General Hospital for general check-ups (two-day health examination) between January 2004 and December 2006. Excluding 2476 subjects aged below 40 years, a final total of 9311 study participants (3906 males and 5405 females) were enrolled in the study. The demographic data included age, gender, medical past history, and lifestyle. Clinical data included blood pressure, fasting plasma sugar, plasma lipids levels (total cholesterol, high density lipoprotein cholesterol, low density lipoprotein cholesterol, and triglycerides), and hematological variables. Anthropometric measurements including height (meters), weight (kilograms), and body fat (percent; Body Composition Analyzer TBF-410, Tanita, Japan) were also examined.
Metabolic syndrome was diagnosed with the modified NCEP criteria. H. pylori infection was detected by the biopsy urease test (CLO test, Pronto Dry, Gastrex, Poland) using standard video esophagogastroduodenoscopy (EGD) with gastrofibroscopes (GIFXP-240, GIFQ260, Olympus Optical, Tokyo Japan). A specimen for biopsy urease testing of each subject was taken from the gastric antrum using biopsy forceps and assessed within 60 min. The agar color of the biopsy urease testing turned from yellow to red when the biopsy specimen was infected with H. pylori, which contained intracytoplasmic urease. Colorectal adenomas were identified by complete total colonoscopy using standard video colonoscopes (CF 240I, Olympus Optical, Tokyo, Japan) by single- and double-handed methods under intravenous 1% Propofol (Fresenius Kabi, Austria). This study was performed under the approval of our hospital Institutional Review Board.
Statistical analysis
Data for continuous variables were expressed as mean ± SD. The t test was applied for continuous variables when the data fitted a Gaussian distribution. If the continuous data did not fit the Gaussian distribution, the Wilcoxon rank sum test was applied. Categorical variables were tested with the χ2 test. Stepwise logistic regression analysis was conducted for significant variable selection. Basic model-fitting techniques for regression analysis were applied to assure the quality of analysis results, including variable selection, goodness-of-fit assessment, and regression diagnostics. Statistical significance was established for two-sided P values < 0.05. All statistical analyses were performed with the SAS® software, version 9.1.3 (SAS Institute Inc., Cary, NC, USA) and R 2.6.2 (R Development Core Team, R Foundation for Statistical Computing, 2008, Vienna, Austria).
RESULTS
The median ages of the study participants were 54 years in males and 52 years in females. All subjects went through complete EGD examination, and 2.8% of participants had incomplete colonoscopy examination. The raw prevalence rates of H. pylori infection, metabolic syndrome, and colorectal adenoma were 39.2%, 18.7% and 20.7%, respectively. A total of 1923 adenomas, including 1691 tubular adenoma, 208 tubulovillous adenomas, and 24 serrated adenomas, were detected. Males were significantly older (P < 0.001), were more likely to smoke (P < 0.001), drink alcohol (P < 0.001), have heavier body weight (P < 0.001), lesser body fat (P < 0.001), and higher systolic and diastolic blood pressure values (P < 0.001). Males additionally had a higher proportion of hypertension (P < 0.001), diabetes (P < 0.001), higher fasting blood glucose levels (P < 0.001), higher white blood cell (WBC) counts (P < 0.001), lower lymphocyte percentages (P < 0.001), and a higher prevalence of colorectal adenoma (P < 0.001). There were no significant differences in total plasma cholesterol levels (P = 0.448), metabolic syndrome frequency (P = 0.154), and H. pylori infection frequency (P = 0.096) between males and females (Table 1).
Table 1.
Baseline characteristics of the study subjects
| Variable | Male | Female | P |
| n | 3906 | 5405 | |
| Age (yr) | 54 (48, 61) | 52 (47, 59) | < 0.001 |
| Smoke, n (%) | 884 (22.6) | 49 (0.9) | < 0.001 |
| Alcohol, n (%) | 876 (22.4) | 119 (2.2) | < 0.001 |
| Body weight (kg) | 67.6 (61.8, 74.2) | 56.0 (51.3, 61.7) | < 0.001 |
| Body fat (%) | 22.7 (19.4, 26.1) | 30.6 (26.8, 34.9) | < 0.001 |
| Systolic BP (mmHg) | 128 (116, 141) | 122 (111, 138) | < 0.001 |
| Diastolic BP (mmHg) | 81 (73, 88) | 74 (66, 82) | < 0.001 |
| Hypertension, n (%) | 1518 (38.9) | 1575 (29.1) | < 0.001 |
| Diabetes, n (%) | 317 (8.1) | 330 (6.1) | < 0.001 |
| Glucose AC (mg/dL) | 90 (84, 97) | 88 (83, 95) | < 0.001 |
| TCH (mg/dL) | 191 (168, 215) | 190 (169, 215) | 0.448 |
| WBC (× 103/μL) | 6.31 (5.38, 7.42) | 5.90 (5.02, 6.97) | < 0.001 |
| Lymphocyte (%) | 32.2 (27.0, 37.4) | 33.9 (28.7, 39.2) | < 0.001 |
| MS, n (%) | 755 (19.3) | 982 (18.2) | 0.154 |
| H. pylori, n (%) | 1571 (40.2) | 2083 (38.5) | 0.096 |
| Adenoma, n (%) | 1053 (27.0) | 870 (16.1) | < 0.001 |
n: Subject number; BP: Blood pressure; TCH: Total plasma cholesterol; WBC: White blood cell; H. pylori: Helicobacter pylori; MS: Metabolic syndrome.
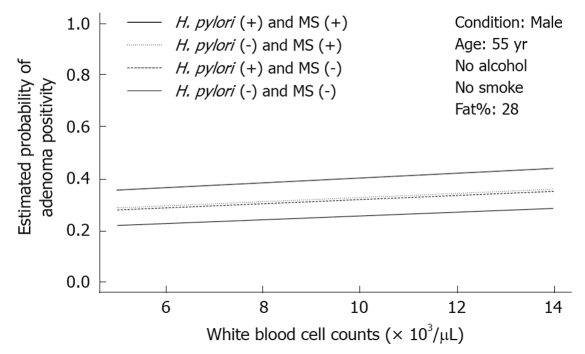
Multivariate logistic regression analysis revealed that male gender (OR: 2.005; 95% confidence interval (CI), 1.740-2.310, P < 0.001), advanced age (OR: 1.046, 95% CI: 1.040-1.052, P < 0.001), smoking (OR: 1.377, 95% CI: 1.146-1.654, P = 0.001), increased body fat (OR: 1.016, 95% CI: 1.007-1.026, P = 0.001), higher white blood cell (WBC) count (OR: 1.038, 95% CI: 1.005-1.073, P = 0.025), H. pylori infection (OR: 1.366, 95% CI: 1.230-1.517, P < 0.001), and metabolic syndrome (OR: 1.408, 95% CI: 1.231-1.610, P < 0.001) were associated risk factors for colorectal adenoma. Alcohol consumption (OR: 0.990, 95% CI: 0.826-1.187, P = 0.915) was not a risk factor for colorectal adenoma (Table 2). Under analysis with a conditional effect plot, colorectal adenoma risk was positively associated with WBC count among paired groups of positive and negative H. pylori-infected patients and paired groups of positive and negative metabolic syndrome patients (Figure 1).
Table 2.
Multivariate logistic regression analysis of the risk factors for colorectal adenomas
| Variable | β | SE | P | OR | 95% CI |
| Intercept | -5.031 | 0.253 | < 0.001 | - | - |
| Gender (M vs F) | 0.696 | 0.072 | < 0.001 | 2.005 | 1.740-2.310 |
| Age (per year) | 0.045 | 0.003 | < 0.001 | 1.046 | 1.040-1.052 |
| Smoke (yes vs no) | 0.320 | 0.094 | 0.001 | 1.377 | 1.146-1.654 |
| Alcohol (yes vs no) | -0.010 | 0.093 | 0.915 | 0.990 | 0.826-1.187 |
| Body fat (%) | 0.016 | 0.005 | 0.001 | 1.016 | 1.007-1.026 |
| WBC (per 103/μL) | 0.038 | 0.017 | 0.025 | 1.038 | 1.005-1.073 |
| H. pylori (yes vs no) | 0.312 | 0.054 | < 0.001 | 1.366 | 1.230-1.517 |
| MS (yes vs no) | 0.342 | 0.068 | < 0.001 | 1.408 | 1.231-1.610 |
WBC: White blood cell; H. pylori: Helicobacter pylori; MS: Metabolic syndrome; OR: Odd ratio; CI: Confidence interval.
Figure 1.
Conditional effect plot of Helicobacter pylori infection status and metabolic syndrome on the probability of adenoma positivity. The conditions were designed as non-smoking males at 55 years old and 28% body fat with the pair of both Helicobacter pylori (H. pylori) positivity and metabolic syndrome (MS) positivity vs another three pairs.
DISCUSSION
The results of our study supported the association of H. pylori infection with colorectal adenomas and were consistent with previous reports that metabolic syndrome might increase colorectal adenoma risk. It also showed that individuals with concomitant metabolic syndrome and H. pylori infection might have a further increased risk of colorectal adenomas.
The inconclusive results of previous studies concerning the relationship between H. pylori infection and colorectal neoplasm might have been due to sample bias, small sample size, inadequate consideration of potential confounding variables, and a varying frequency of cag A+ strains in the study populations[19,20]. In addition, incomplete colonoscopic studies and evaluation of H. pylori infection with the IgG serum test (which cannot represent real-time H. pylori infection) might also have contributed to the inconsistent results. The advantages of our study include large sample size, detection of H. pylori infection with the EGD and biopsy CLO test, and complete colonoscopy to the distal terminal ileum after good bowel preparation in 97.2% of the cases. Furthermore, patient lifestyle habits including smoking and alcohol consumption, gender, and age were also evaluated in this study. These factors might minimize potential variables during the data analysis.
However, there were also some limitations in our study. Patients in the study were selected from a population who sought routine physical examinations at our institute, and their psychosocial behaviors and lifestyle habits might differ from those in the general population, resulting in a confounding bias that could be ignored in the data analysis. Although H. pylori infection can be more accurately detected by biopsy CLO test than by the serum IgG method logically, in rare instances antral biopsies with CLO tests might not be representative of all gastric states of H. pylori infection. In addition, past historical data of diagnosis and treatment of H. pylori infection were not included in the analysis, although the enrolled cases were clinically asymptomatic. Additionally, blood insulin, gastrin levels, and proinflammatory cytokines were not measured. The study design also did not allow the identification of the pathologic mechanisms underlying the association of colorectal adenoma with metabolic syndrome and H. pylori infection.
The pathogenic mechanisms by which H. pylori exerts its malignant potential in the induction of colorectal neoplasms are not completely understood. A few studies have revealed that fecal shedding of viable H. pylori and its antigen occurs under certain circumstances[21,22], suggesting that H. pylori moves through the intestinal tract in direct contact with colonic mucosa, and could therefore locally activate colonic carcinogenesis. H. pylori was recently detected within colorectal carcinoma tissues[23]. The role of H. pylori-specific affinity for colorectal neoplasms requires further investigation. The presence of H. pylori might alter normal gastrointestinal flora as a consequence of progressive chronic gastritis with glandular atrophy and decreased acid production. This could further influence colorectal carcinogenesis. Persistent H. pylori exposure induces hypergastrinemia, which is a putative trophic factor for the large bowel mucosa. Cell proliferation and gastrin-induced genomic instability can increase the risk of DNA replication error and play a role in the development of colorectal neoplasms[24]. H. pylori infection might also result in direct damage to the colorectal mucosa or indirect damage to the epithelium through inflammatory responses. Contact between a repairing epithelium and endogenous or dietary carcinogens within the gut might transform the colorectal mucosa[25]. The CagA protein is the product of the cytotoxin-associated gene and is produced by cagA+ strains of H. pylori. It might locally activate colonic carcinogenesis through the induction of cytokine expression, including cytokines such as interleukin (IL)-8, which is associated with colorectal cancer[26]. In summary, H. pylori might result in local and distant interactions with colorectal mucosa and contribute to the pathogenesis of malignant transformation. However, further mechanistic studies are required.
Metabolic syndrome and its association with colorectal adenomas have been the subjects of recent study, and the pathogenic mechanisms for this potential association are still unclear. Insulin (a core contributor to metabolic syndrome) has been demonstrated to promote colorectal carcinogenesis in animal studies for more than 10 years[27,28]. It is postulated that insulin might exert proliferative effects on colonic tumor cells directly or indirectly via the insulin-like growth factor pathway[29]. Furthermore, increased production of proinflammatory cytokines and decreased production of anti-inflammatory adiponectin in adipocytes might be related to adenoma growth[30]. In addition, hypertriglyceridemia (a component of metabolic syndrome) might be involved in colorectal neoplasm pathogenesis. Triglycerides act as potent energy sources for cancer cell growth[31], and elevated serum triglyceride levels have been associated with increased synthesis of bile acids, which could promote large bowel carcinogenesis, as demonstrated in experimental studies[32]. Metabolic syndrome is associated with chronic inflammation, which might explain its possible association with colorectal adenoma. Adipose tissue and circulating levels of inflammatory cytokines [including tumor necrosis factor (TNF)-α and IL-6] are increased in obese and diabetic patients, and can induce several metabolic derangements characteristic of metabolic syndrome[33,34]. IL-6-induced C-reactive protein (CRP) could predict colon cancer occurrence; meanwhile, an elevated CRP level is a consistent feature of metabolic syndrome[35]. The findings indicate that chronic inflammation might be associated with colorectal carcinogenesis. In short, these evidence-base data suggest that metabolic syndrome might be a risk factor for colorectal neoplasm development.
In this study, concomitant with H. pylori infection and metabolic syndrome might further increase the risk of developing colorectal adenoma. The concomitant effect of metabolic syndrome and H. pylori might occur secondary to common inflammatory pathways of colorectal pathological mechanisms associated with metabolic syndrome and H. pylori infection. The inflammation-related factors of metabolic syndrome include IL-6, TNF-α, fibrinogen, and cyclooxygenase-2. The inflammation-related factors of H. pylori including IL-8, TNF-α, and the Cag A, Vac A, and babA2 proteins might display similar inflammatory effects attributable to the common inflammatory pathway. White blood cell counts are a risk factor of colorectal adenoma in the multivariate logistic regression analysis and might support this hypothesis of the involvement of the common inflammatory pathway. However, further investigations on the pathogenesis of this concomitant effect are necessary. Clinically, our results suggested that both H. pylori infection and metabolic syndrome should both be evaluated for the prevention of colorectal adenomas and carcinomas.
Studies have revealed that moderate alcohol consumption is related to increased insulin-sensitivity[36], while smoking exerted the opposite effect[37]. Other studies have suggested that both alcohol use and cigarette smoking were associated with increased risk of colorectal adenoma[38,39]. Cigarette smoking was related to colorectal adenomas in this study, although alcohol consumption was not. To clarify the association between alcohol consumption and colorectal adenoma, further studies are necessary.
In conclusion, this cross-sectional hospital-based study revealed a direct association of colorectal adenoma with H. pylori infection and metabolic syndrome. Furthermore, H. pylori infection concomitant with metabolic syndrome might further increase the risk of colorectal adenoma. These results suggest that both H. pylori infection and metabolic syndrome should be considered important entities with regards to the prevention of colorectal adenoma and carcinoma. This is particularly important when a patient clinically presents with concomitant H. pylori infection and metabolic syndrome. The combined effects of metabolic syndrome and H. pylori infection should be further clarified.
COMMENTS
Background
Colorectal cancer is one of the leading causes of cancer mortality worldwide. Colorectal adenoma is the premalignant lesion in colorectal cancer. Identification of the etiology of colorectal neoplasms might assist in the development of strategies targeted toward its prevention. Previous epidemiological studies have identified family history, dietary factors, smoking, sedentary lifestyles, and alcohol consumption as potential contributors to colorectal neoplasm development. Recently, reports revealed that Helicobacter pylori (H. pylori) infection is associated with colorectal neoplasm, and a few reports disclosed that metabolic syndrome was also associated with an increased risk of colorectal adenoma. Based on these findings, the probability of colorectal adenoma in patients with both H. pylori infection and metabolic syndrome was further evaluated.
Research frontiers
Colorectal cancer is an extremely common malignancy, however, the direct etiology of colorectal neoplasm is still unknown. Epidemiologically, identification of the etiology of colorectal neoplasm might assist in development of strategies targeted toward its prevention. During latest decade, H. pylori infection and metabolic syndrome, respectively, were identified to be associated with colorectal neoplasms and hypotheses were provided to explain the mechanisms of their relationships. However, until now, there was no study focusing on whether concomitant H. pylori infection with metabolic syndrome in a patient will increase his or her risk of colorectal adenoma.
Innovations and breakthroughs
This study supported the association of colorectal adenoma individually with H. pylori infection and metabolic syndrome. Furthermore, H. pylori infection concomitant with metabolic syndrome might further increase the risk of colorectal adenoma.
Applications
These results suggest that both H. pylori infection and metabolic syndrome should be considered important entities with regards to the prevention of colorectal adenoma and carcinoma. This is particularly important when a patient clinically presents with concomitant H. pylori infection and metabolic syndrome; the increased risk of developing colorectal adenomas should be more seriously considered for preventive purpose.
Peer review
This paper reports an important study that assesses the rate of metabolic syndrome, H. pylori, and colonic adenomas in a large population of asymptomatic individuals. The significances of these findings are discussed in relation to previous studies, and hypothesis to explain the findings are reviewed. Strengths of the study include the size of the sample, high completion rate of colonoscopy, and the use of well-established diagnostic criteria for metabolic syndrome in this population. Limitations are acknowledged by the authors and include the single centre nature of the study, select patient population, and possible false negative results of HP testing.
Acknowledgments
The authors greatly appreciate the financial and technical support of Dalin Tzu Chi General Hospital, and the help of the President of the School of Medicine of Japan Jichi Medical University, Professor Fumimaro Takaku, who kindly revised the manuscript.
Footnotes
Supported by Buddhist Dalin Tzu Chi General Hospital
Peer reviewer: Dr. Charles B Ferguson, MRCP, Department of Gastroenterology, Belfast City Hospital, 51 Lisburn Road, Belfast, BT9 7AB, United Kingdom
S- Editor Wang YR L- Editor Stewart GJ E- Editor Lin YP
References
- 1.Fearon ER, Vogelstein B. A genetic model for colorectal tumorigenesis. Cell. 1990;61:759–767. doi: 10.1016/0092-8674(90)90186-i. [DOI] [PubMed] [Google Scholar]
- 2.Giovannucci E. Modifiable risk factors for colon cancer. Gastroenterol Clin North Am. 2002;31:925–943. doi: 10.1016/s0889-8553(02)00057-2. [DOI] [PubMed] [Google Scholar]
- 3.Rothenbacher D, Brenner H. Burden of Helicobacter pylori and H. pylori-related diseases in developed countries: recent developments and future implications. Microbes Infect. 2003;5:693–703. doi: 10.1016/s1286-4579(03)00111-4. [DOI] [PubMed] [Google Scholar]
- 4.Infection with Helicobacter pylori. In: World Health Organization. IARC monographs on the evaluation of carcinogenic risks to humans. Vol. 61. Schistosomes, liver flukes and Helicobacter pylori. Lyon, France: International Agency for Research on Cancer; 1994. pp. 177–240. [PMC free article] [PubMed] [Google Scholar]
- 5.Meucci G, Tatarella M, Vecchi M, Ranzi ML, Biguzzi E, Beccari G, Clerici E, de Franchis R. High prevalence of Helicobacter pylori infection in patients with colonic adenomas and carcinomas. J Clin Gastroenterol. 1997;25:605–607. doi: 10.1097/00004836-199712000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Breuer-Katschinski B, Nemes K, Marr A, Rump B, Leiendecker B, Breuer N, Goebell H. Helicobacter pylori and the risk of colonic adenomas. Colorectal Adenoma Study Group. Digestion. 1999;60:210–215. doi: 10.1159/000007661. [DOI] [PubMed] [Google Scholar]
- 7.Mizuno S, Morita Y, Inui T, Asakawa A, Ueno N, Ando T, Kato H, Uchida M, Yoshikawa T, Inui A. Helicobacter pylori infection is associated with colon adenomatous polyps detected by high-resolution colonoscopy. Int J Cancer. 2005;117:1058–1059. doi: 10.1002/ijc.21280. [DOI] [PubMed] [Google Scholar]
- 8.Fujimori S, Kishida T, Kobayashi T, Sekita Y, Seo T, Nagata K, Tatsuguchi A, Gudis K, Yokoi K, Tanaka N, et al. Helicobacter pylori infection increases the risk of colorectal adenoma and adenocarcinoma, especially in women. J Gastroenterol. 2005;40:887–893. doi: 10.1007/s00535-005-1649-1. [DOI] [PubMed] [Google Scholar]
- 9.Zumkeller N, Brenner H, Zwahlen M, Rothenbacher D. Helicobacter pylori infection and colorectal cancer risk: a meta-analysis. Helicobacter. 2006;11:75–80. doi: 10.1111/j.1523-5378.2006.00381.x. [DOI] [PubMed] [Google Scholar]
- 10.Siddheshwar RK, Muhammad KB, Gray JC, Kelly SB. Seroprevalence of Helicobacter pylori in patients with colorectal polyps and colorectal carcinoma. Am J Gastroenterol. 2001;96:84–88. doi: 10.1111/j.1572-0241.2001.03355.x. [DOI] [PubMed] [Google Scholar]
- 11.Limburg PJ, Stolzenberg-Solomon RZ, Colbert LH, Perez-Perez GI, Blaser MJ, Taylor PR, Virtamo J, Albanes D. Helicobacter pylori seropositivity and colorectal cancer risk: a prospective study of male smokers. Cancer Epidemiol Biomarkers Prev. 2002;11:1095–1099. [PubMed] [Google Scholar]
- 12.Grahn N, Hmani-Aifa M, Fransén K, Söderkvist P, Monstein HJ. Molecular identification of Helicobacter DNA present in human colorectal adenocarcinomas by 16S rDNA PCR amplification and pyrosequencing analysis. J Med Microbiol. 2005;54:1031–1035. doi: 10.1099/jmm.0.46122-0. [DOI] [PubMed] [Google Scholar]
- 13.Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004;27:1182–1186. doi: 10.2337/diacare.27.5.1182. [DOI] [PubMed] [Google Scholar]
- 14.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414–1431. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 15.Haslam DW, James WP. Obesity. Lancet. 2005;366:1197–1209. doi: 10.1016/S0140-6736(05)67483-1. [DOI] [PubMed] [Google Scholar]
- 16.Morita T, Tabata S, Mineshita M, Mizoue T, Moore MA, Kono S. The metabolic syndrome is associated with increased risk of colorectal adenoma development: the Self-Defense Forces health study. Asian Pac J Cancer Prev. 2005;6:485–489. [PubMed] [Google Scholar]
- 17.Wang YY, Lin SY, Lai WA, Liu PH, Sheu WH. Association between adenomas of rectosigmoid colon and metabolic syndrome features in a Chinese population. J Gastroenterol Hepatol. 2005;20:1410–1415. doi: 10.1111/j.1440-1746.2005.03971.x. [DOI] [PubMed] [Google Scholar]
- 18.Kim JH, Lim YJ, Kim YH, Sung IK, Shim SG, Oh SO, Park SS, Yang S, Son HJ, Rhee PL, et al. Is metabolic syndrome a risk factor for colorectal adenoma? Cancer Epidemiol Biomarkers Prev. 2007;16:1543–1546. doi: 10.1158/1055-9965.EPI-07-0199. [DOI] [PubMed] [Google Scholar]
- 19.Shmuely H, Passaro D, Figer A, Niv Y, Pitlik S, Samra Z, Koren R, Yahav J. Relationship between Helicobacter pylori CagA status and colorectal cancer. Am J Gastroenterol. 2001;96:3406–3410. doi: 10.1111/j.1572-0241.2001.05342.x. [DOI] [PubMed] [Google Scholar]
- 20.Takeda H, Asaka M. Helicobacter pylori and colorectal neoplasm: a mysterious link? J Gastroenterol. 2005;40:919–920. doi: 10.1007/s00535-005-1696-7. [DOI] [PubMed] [Google Scholar]
- 21.Thomas JE, Gibson GR, Darboe MK, Dale A, Weaver LT. Isolation of Helicobacter pylori from human faeces. Lancet. 1992;340:1194–1195. doi: 10.1016/0140-6736(92)92894-l. [DOI] [PubMed] [Google Scholar]
- 22.Parsonnet J, Shmuely H, Haggerty T. Fecal and oral shedding of Helicobacter pylori from healthy infected adults. JAMA. 1999;282:2240–2245. doi: 10.1001/jama.282.23.2240. [DOI] [PubMed] [Google Scholar]
- 23.Jones M, Helliwell P, Pritchard C, Tharakan J, Mathew J. Helicobacter pylori in colorectal neoplasms: is there an aetiological relationship? World J Surg Oncol. 2007;5:51. doi: 10.1186/1477-7819-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ames BN, Gold LS. Too many rodent carcinogens: mitogenesis increases mutagenesis. Science. 1990;249:970–971. doi: 10.1126/science.2136249. [DOI] [PubMed] [Google Scholar]
- 25.Parsonnet J. Bacterial infection as a cause of cancer. Environ Health Perspect. 1995;103 Suppl 8:263–268. doi: 10.1289/ehp.95103s8263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brew R, Erikson JS, West DC, Kinsella AR, Slavin J, Christmas SE. Interleukin-8 as an autocrine growth factor for human colon carcinoma cells in vitro. Cytokine. 2000;12:78–85. doi: 10.1006/cyto.1999.0518. [DOI] [PubMed] [Google Scholar]
- 27.Tran TT, Medline A, Bruce WR. Insulin promotion of colon tumors in rats. Cancer Epidemiol Biomarkers Prev. 1996;5:1013–1015. [PubMed] [Google Scholar]
- 28.Corpet DE, Jacquinet C, Peiffer G, Taché S. Insulin injections promote the growth of aberrant crypt foci in the colon of rats. Nutr Cancer. 1997;27:316–320. doi: 10.1080/01635589709514543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yu H, Rohan T. Role of the insulin-like growth factor family in cancer development and progression. J Natl Cancer Inst. 2000;92:1472–1489. doi: 10.1093/jnci/92.18.1472. [DOI] [PubMed] [Google Scholar]
- 30.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 31.Moller DE, Flier JS. Insulin resistance--mechanisms, syndromes, and implications. N Engl J Med. 1991;325:938–948. doi: 10.1056/NEJM199109263251307. [DOI] [PubMed] [Google Scholar]
- 32.Hill MJ. Bile flow and colon cancer. Mutat Res. 1990;238:313–320. doi: 10.1016/0165-1110(90)90023-5. [DOI] [PubMed] [Google Scholar]
- 33.Katsuki A, Sumida Y, Murashima S, Murata K, Takarada Y, Ito K, Fujii M, Tsuchihashi K, Goto H, Nakatani K, et al. Serum levels of tumor necrosis factor-alpha are increased in obese patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab. 1998;83:859–862. doi: 10.1210/jcem.83.3.4618. [DOI] [PubMed] [Google Scholar]
- 34.Kern PA, Ranganathan S, Li C, Wood L, Ranganathan G. Adipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistance. Am J Physiol Endocrinol Metab. 2001;280:E745–E751. doi: 10.1152/ajpendo.2001.280.5.E745. [DOI] [PubMed] [Google Scholar]
- 35.Erlinger TP, Platz EA, Rifai N, Helzlsouer KJ. C-reactive protein and the risk of incident colorectal cancer. JAMA. 2004;291:585–590. doi: 10.1001/jama.291.5.585. [DOI] [PubMed] [Google Scholar]
- 36.Davies MJ, Baer DJ, Judd JT, Brown ED, Campbell WS, Taylor PR. Effects of moderate alcohol intake on fasting insulin and glucose concentrations and insulin sensitivity in postmenopausal women: a randomized controlled trial. JAMA. 2002;287:2559–2562. doi: 10.1001/jama.287.19.2559. [DOI] [PubMed] [Google Scholar]
- 37.Facchini FS, Hollenbeck CB, Jeppesen J, Chen YD, Reaven GM. Insulin resistance and cigarette smoking. Lancet. 1992;339:1128–1130. doi: 10.1016/0140-6736(92)90730-q. [DOI] [PubMed] [Google Scholar]
- 38.Giovannucci E, Martínez ME. Tobacco, colorectal cancer, and adenomas: a review of the evidence. J Natl Cancer Inst. 1996;88:1717–1730. doi: 10.1093/jnci/88.23.1717. [DOI] [PubMed] [Google Scholar]
- 39.Toyomura K, Yamaguchi K, Kawamoto H, Tabata S, Shimizu E, Mineshita M, Ogawa S, Lee KY, Kono S. Relation of cigarette smoking and alcohol use to colorectal adenomas by subsite: the self-defense forces health study. Cancer Sci. 2004;95:72–76. doi: 10.1111/j.1349-7006.2004.tb03173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]