Abstract
The nuclear transcription factor Peroxisome Proliferator-Activated Receptor (PPAR) γ plays a central role in normal lung development. However, the effects of modulating PPARγ expression by exogenously administered PPARγ agonists on lung development and basic blood biochemical and metabolic profiles in a developing animal are not known. To determine these effects, newborn Sprague-Dawley rat pups were administered either diluent or rosiglitazone (RGZ), a potent PPARγ agonist, for either 1 or 7 days. Then the pups were sacrificed and the lungs were examined for specific markers of alveolar epithelial, mesenchymal, and vascular maturation, and lung morphometry. The effect of RGZ on a limited number of blood biochemical and metabolic parameters was also determined. Overall, systemically administered RGZ significantly enhanced lung maturation without affecting serum electrolytes, blood glucose, blood gases, plasma cholesterol, triglycerides, and serum cardiac troponin levels. The lung maturation effect of PPARγ agonists was also confirmed by another PPARγ agonist, the naturally occurring PPARγ ligand prostaglandin J2. We conclude that systemically administered RGZ significantly enhances lung maturation without significantly affecting the acute blood biochemical and metabolic profiles, providing rationale for further studying PPARγ agonists for enhancing lung maturation, and for promoting lung injury/repair in neonates.
Keywords: Bronchopulmonary Dysplasia, Chronic Lung Injury, Lung maturity, PPARγ, Rosiglitazone
Introduction
Peroxisome Proliferator-Activated Receptor (PPAR) γ, a member of the retinoid X-receptor heterodimer family of the retinoid/steroid/thyroid hormone superfamily of ligand-activated nuclear receptors, plays a central role in lipid storage and metabolism in various organs, including the lung (1,2). Recently, it has been demonstrated to play a central role in normal lung development by stimulating the alveolar epithelial-mesenchymal paracrine signaling that is critical for normal lung development (3,4). However, the effect of manipulating PPARγ expression by exogenously administered PPARγ agonists on lung development in a developing animal is not known. This is important since steroid administration, the contemporary standard intervention to enhance fetal lung maturation, has significant limitations. For example, this therapy, is effective in only 50–70% of infants, is sex-specific, has a delayed onset of action, and with repeated use, it may result in significant somatic growth restriction and neurodevelopmental handicaps (5–8). Similarly, all-trans retinoic acid, another agent that is known to promote alveolarization in both neonatal and adult animal models, is also known to exhibit well-documented teratogenic effects, its effects are species specific, and it does not result in improved pulmonary function (9,10). In view of the limited options for agents that can be used to stimulate lung maturation, alternate strategies for accelerating fetal lung maturation that are uniformly effective and safe are needed.
In the present work, using a neonatal rat model for lung development, we sought to examine the effects of the systemically administered PPARγ agonists rosiglitazone (RGZ) and Prostaglandin J2 (PGJ2) for up to 7 days on selected markers of lung differentiation, and to determine whether this intervention affects the basic blood biochemical and metabolic profiles of the treated animal. We hypothesized that PPARγ agonists given systemically would enhance lung maturation without significantly altering basic blood biochemical and metabolic profiles. Therefore, following systemic PPARγ agonist administration, lung maturation was assessed by examining the expression of key alveolar epithelial and mesenchymal molecular markers that are the hallmarks of lung maturation in the developing lung, including the expressions of surfactant proteins B and C, choline incorporation into saturated phosphatidylcholine, triolein uptake by the lung, and by lung morphometry. The effects of systemically administered RGZ on basic blood biochemical and metabolic profiles was assessed by measuring serum electrolytes, blood gases, blood glucose, cardiac troponin, and plasma cholesterol and triglycerides.
Methods
Animal protocol
Pathogen-free, timed (time e0=day of mating), first-time pregnant Sprague Dawley rats (200–220g) were obtained from Charles River (Holister, CA) at day 16 of gestation and were allowed to acclimatize in humidity- and temperature-controlled rooms on a 12:12-hour-light:dark cycle, and were allowed food and water ad libitum. On d22 of pregnancy, dams were allowed to deliver spontaneously. Newborn pups receiving RGZ were divided into the following 6 groups-control, RGZ 0.1 mg/kg, 0.3 mg/kg, 1 mg/kg, 3 mg/kg, or 8 mg/kg groups. The diluent (saline) or RGZ (Cayman Chemicals, Ann Arbor, MI) was administered intraperitoneally (i.p.) with a microsyringe in 100 μl volumes once daily for either 1 or 7 days. The first dose of RGZ was administered as soon as possible after delivery, and in no case was the interval between the administration of the first dose and sacrifice at 24 hours less than 22 hours. To demonstrate that the effects of PPARγ agonists on lung maturation are not RGZ-specific, some animals received the PPARγ agonist PGJ2 at 0.1 mg/kg, 0.3 mg/kg, 1 mg/kg, or 10% dimethyl suphoxide (vehicle-treated controls) in 100 μl volumes administered i.p. once daily for 7 days. At the end of each experimental period, the pups were sacrificed using 0.1 ml euthasol per pup. The lungs were collected and processed either immediately for [3H]choline incorporation and [3H]triolein uptake, or flash-frozen for later Western hybridization for the markers of lung maturation. Tissue was also processed for lung morphometry and lamellar body staining as described below. To determine the effects of systemically administered RGZ on PPARγ and its down-stream target Adipocyte Differentiation Related Protein (ADRP), expression in selected extra-pulmonary tissues, peritoneal fat, liver, and kidneys were flash-frozen from the sacrificed animals. Blood was collected by cardiac puncture from each pup and either processed immediately for blood gases, electrolytes, and glucose analysis, or frozen at −80°C for later determination of blood cholesterol, triglyceride, and cardiac troponin levels. A total of 20 pups were used for each condition (2–3/litter). All animal procedures were performed following the guidelines of the National Institutes of Health for the care and use of laboratory animals, and approved by the Los Angeles Biomedical Research Institute, Animal Care and Use Committee.
Western blot analysis
Western analysis was performed as described previously (11). The specific primary antibodies used included PPARγ (1:2,000, Alexis Biochemicals, San Diego, CA), Surfactant Protein-B (SP-B) and SP-C (1:2,000 for each, Chemicon, Temecula, CA), cholinephosphate cytidylyltransferase-α (CCT-α) (1:2,000, a gift from Dr. Mallampalli, University of Iowa, Iowa), PTHrP receptor (1:100, Upstate, Temecula, CA), ADRP (1:3,000, a gift from Dr. Constantine Londos, NIDDK); VEGF, and FLK-1 (1:350 for each, Santa Cruz, Biotechnology, San Diego, CA). The blots were subsequently stripped and reprobed with antiGAPDH antibody (1:10,000, Chemicon, Temecula, CA), and specific protein values were normalized to GAPDH.
Lung Morphology
Rat lung was inflated in situ with 4% paraformaldehyde in phosphate buffer at a standard inflation pressure of 5 cm of H20, and was fixed as described previously (11). An investigator unaware of the treatment groups performed lung morphometry, which was objectively assessed by determining the radial alveolar count (RAC) and mean linear intercept (MLI) methods on H & E stained sections. Fifty randomly selected, non-overlapping fields from sections obtained from 12 blocks from each treatment group were included for measurement. Briefly, radial alveolar counts were performed by identifying respiratory bronchioles, as described by Randell et al (12). The MLI, which represents the average alveolar diameter, was analyzed with Image-Pro plus image-analysis software (Zeiss, Germany). Slides were examined at 100-fold magnification and at least two sections from each pup were used and a minimum of six animals from each group were analyzed.
Lamellar Body Staining
P180 lamellar body protein expression was assessed by immunofluorescence staining. Briefly, 8μm cryosections were incubated with lamellar body monoclonal antibody (1:500 dilution, COVANCE, Berkeley, CA) at room temperature for 1 hour and then the secondary antibody goat anti-mouse Rhodamine IgG (1:200 dilution, Santa Cruz, CA) was applied to the sections for another 30 minutes. The sections were washed with phosphate buffered saline and then mounted with Vectashield mounting medium with DAPI for visualization under a fluorescence microscope.
Triglyceride uptake and Choline Incorporation into Saturated Phosphotidylcholine Assays
Triglyceride uptake and incorporation of [methyl-3H]-choline chloride (NEN Dupont) into saturated phosphatidylcholine in cultured lung explants was determined as described previously (12).
Blood Gas, Glucose, and Serum Electrolytes Assays
These parameters were assayed, using I-Stat (Abbott Laboratories, Abbott Park, Illinois), cartridge EC8+, according to the manufacturer’s protocol.
Plasma Cholesterol and Triglyceride Determination
These were measured by enzymatic methods, using the RAICHEM kit (Hemagen Diagnostics, San Diego, CA), following the manufacturer’s protocol.
Measurement of Serum Cardiac Troponin I Levels
Serum cardiac troponin I levels were determined by a rat cardiac Tn-I ELISA kit as per the manufacturer’s protocol (Cat. # 2010-2-HS, Life Diagnostics Inc., West Chester, PA). The detection limit of this assay is 0.156 ng/ml.
Statistical Analysis
ANOVA was used to statistically analyze the experimental data. p ≤ 0.05 was considered to indicate statistically significant differences between the experimental groups.
Results
A. Effect of RGZ on alveolar epithelial differentiation
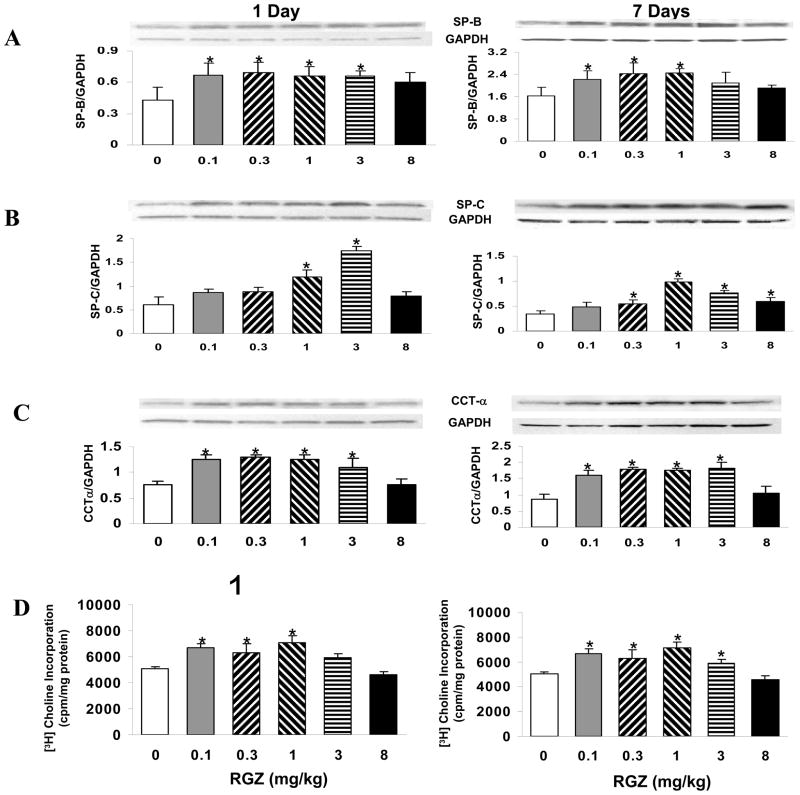
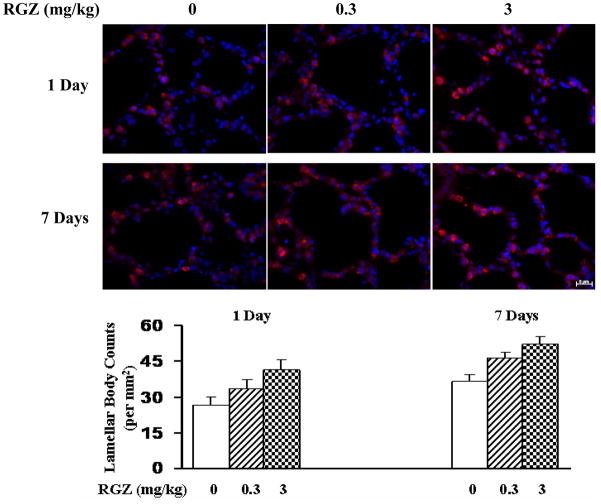
Since pulmonary surfactant is a key marker of lung epithelial differentiation, we examined the effect of RGZ administration on surfactant protein and phospholipid synthesis. Compared to the controls, RGZ administration increased SP-B and SP-C expression on both days 1 and 7 (*=p<0.05, RGZ vs. control; Fig. 1A and 1B), with greater effects at 0.3 and 1 mg/kg for SP-B, and at 1 and 3 mg/kg for SP-C expression. Similarly, following RGZ administration, the expression of CCT-α, the rate-limiting enzyme in surfactant phospholipids synthesis, increased significantly on both days 1 and 7 at all doses of RGZ examined except at the 8 mg/kg dose (*=p<0.05, RGZ vs. control; Fig. 1C). This effect was also mirrored by significantly increased [3H]choline incorporation into saturated phosphatidylcholine, a functional marker for surfactant phospholipids synthesis, and hence that of CCT-α enzyme activity (*p<0.05, RGZ vs. control; Fig. 1D). Increased alveolar epithelial differentiation by RGZ treatment is also reflected by the increased lamellar body staining at both days 1 and 7, as determined by specific labeling for p180 lamellar body, a specific marker for alveolar epithelial type II cells (*p<0.05, RGZ vs. control; Fig. 2).
Fig. 1. Effect of rosiglitazone on surfactant protein and phospholipid synthesis.
The newborn rat pups were administered either diluent or RGZ in graded doses in 100μl volume once daily i.p. for either 1 or 7 days. Compared to the controls, RGZ administration increased surfactant protein B and C expression at both days 1 and 7 (Fig. 1A and 1B) with greater effects at 0.3 and 1 mg/kg for SP-B, and at 1 and 3 mg/kg for SP-C expression. Furthermore, compared to the controls, RGZ administration increased cholinephosphate cytidylyltransferase-α expression significantly at both days 1 and 7 at all doses of RGZ examined except at the 8 mg/kg dose (Fig. 1C). Representative Western blots from the whole lung lysates and the corresponding density histograms are shown (n=5, mean ± SD, *p<0.05, RGZ vs. control,). RGZ treatment resulted in significantly increased [3H]choline incorporation into saturated phosphatidylcholine (Fig. 1D) (n=6, mean ± SD, *p<0.05, RGZ vs. control).
Fig. 2. Effect of rosiglitazone on lamellar body number.
The newborn rat pups were administered either diluent or RGZ in 100μl volume once daily i.p. for either 1 or 7 days. With RGZ treatment, there was significantly increased lamellar body staining at both days 1 and 7 as determined by specific labeling for the lamellar body marker p180. Representative cryostat sections of fixed lung tissue labeled with p180 lamellar body (red staining) are shown. DAPI was used for counterstaining (n=5, mean ± SD, *p<0.05 vs. control). Magnification 40x.
B. Effect of RGZ on alveolar mesenchymal differentiation
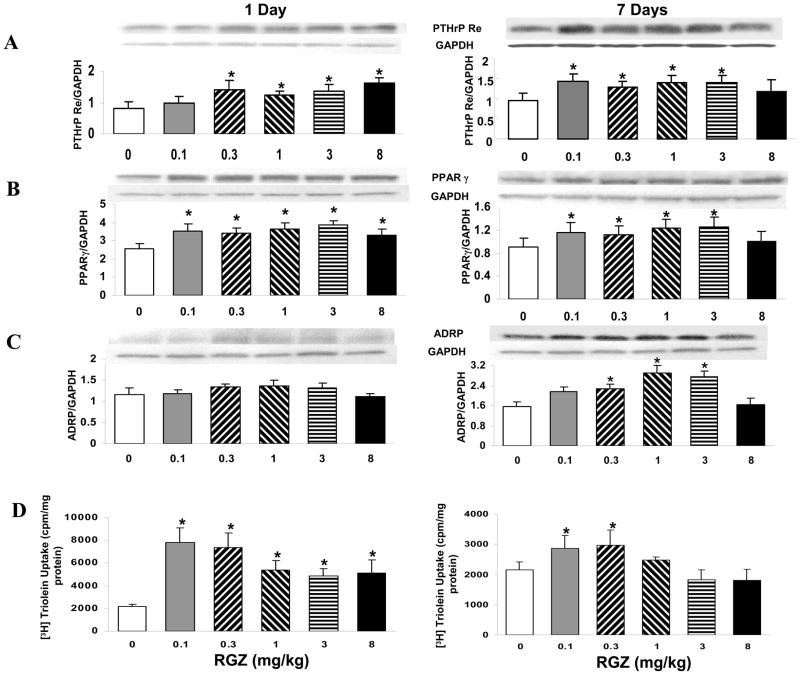
Since we have previously shown that PTHrP/PPARγ signaling is centrally involved in determining alveolar mesenchymal differentiation, we next examined the effect of RGZ administration on PTHrP receptor, PPARγ, and ADRP expression, key markers of alveolar mesenchymal differentiation. Compared to controls, with RGZ administration there was an overall significantly increased expression of PTHrP receptor (Fig. 3A), PPARγ (Fig. 3B), and ADRP (Fig. 3C) at both days 1 and 7 (*=p<0.05, RGZ vs. control). Similarly, with RGZ treatment, triolein uptake, a functional marker of alveolar mesenchymal differentiation, increased significantly, consistent with the increased PTHrP receptor, PPARγ, and ADRP expression at both days 1 and 7 (*p<0.05, RGZ vs. control; Fig. 3D).
Fig. 3. Effect of rosiglitazone on pro-homeostatic mesenchymal markers PTHrP receptor, PPARγ, and ADRP expression and triolein uptake.
The newborn rat pups were administered either diluent or RGZ in graded doses in 100μl volume once daily i.p. for either 1 or 7 days. Compared to controls, with RGZ administration there was an overall significantly increased expression of PTHrP receptor (Fig. 3A), PPARγ (Fig. 3B), and ADRP (Fig. 3C) at both days 1 and 7. Representative Western blots from the whole lung lysates and the corresponding density histograms are shown (n=5, mean ± SD, *p<0.05, RGZ vs. control). Furthermore, RGZ treatment significantly increased triolein uptake at both days 1 and 7 (Fig. 3D, n=6, mean ± SD, *p<0.05, RGZ vs. control).
C. Effect of RGZ on lung morphometry
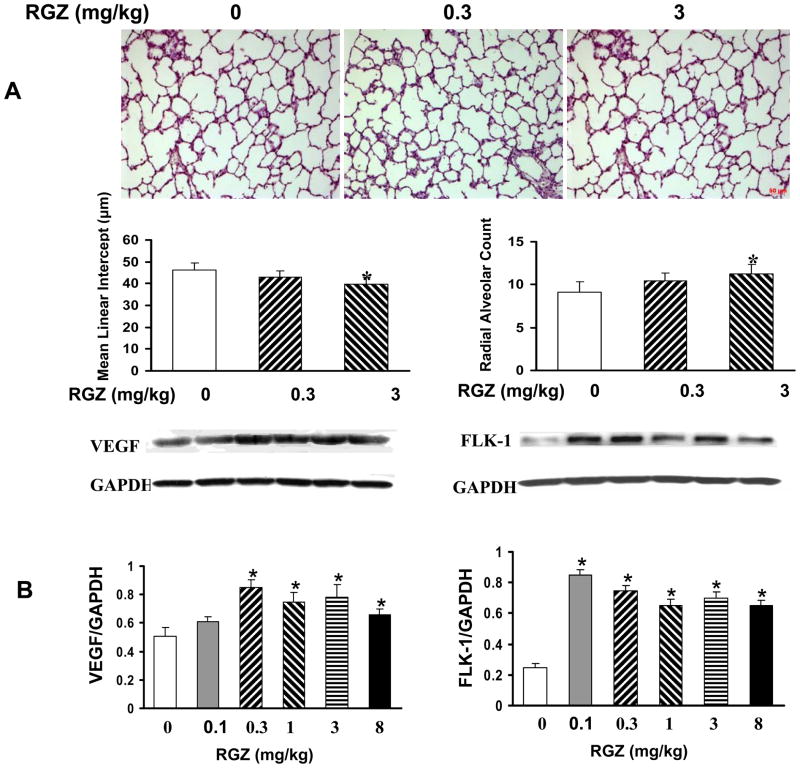
Histologic examination of lungs obtained from control and experimental animals showed enhancement of alveolarization in both the 0.3 mg/kg and 3 mg/kg RGZ treatment for 7 days groups (Fig. 4A), without any significant changes in alveolarization in the 8 mg/kg RGZ treatment group (data not shown) [mean alveolar counts; 9.1 ± 1.2 vs. 10.4 ± 1 vs. 11.3 ± 1.1, control vs. RGZ at 0.3 mg/kg or 3 mg/kg, respectively, *=p < 0.05); mean linear intercepts, 46.4 ± 2.9 vs. 42.8 ± 3.2 vs. 39.6 ± 3.4, control vs. RGZ at 0.3 mg/kg or 3 mg/kg, respectively, *=p < 0.05)]. Since enhanced alveolarization must be accompanied by increased vascularization, we next probed for the expression of VEGF and its receptor FLK-1 in RGZ-treated animals. VEGF is a critical mediator of normal lung vascularization during development and is essential for the establishment of normal lung architecture (13). As predicted, with RGZ treatment, expression of both VEGF and FLK-1 increased significantly (*=p<0.05, RGZ vs. control; Fig. 4B).
Fig. 4. Effect of rosiglitazone on lung morphometry.
The newborn rat pups were administered either diluent or RGZ in 100μl volume once daily i.p. for 7 days (). RGZ treatment resulted in a significant increase in alveolarization in the RGZ 3 mg/kg treatment group, with a trend toward an increase in the RGZ 0.3 mg/kg treatment group [mean alveolar counts : control vs. RGZ, 0.3 mg/kg, 3 mg/kg,, 9.1 ± 1.2 vs. 10.4 ± 1,11.3 ± 1.1, respectively, ,*=p < 0.05) ; mean linear intercepts: control vs. RGZ, 0.3 mg/kg, 3 mg/kg, 46.4 ± 2.9 vs. 42.8 ± 3.2,39.6 ± 3.4, respectively, Fig. 4A, n=6, *p<0.05, RGZ vs. control)]. Representative H & E stained lung sections and the corresponding histograms are shown; Magnification 10x. Furthermore, compared to controls, RGZ administration increased VEGF and FLK-1 expression significantly. Representative Western blots from the whole lung lysates and the corresponding density histograms are shown (Fig. 4B, n=5, mean ± SD, *p<0.05, RGZ vs. control).
D. Effect of RGZ on blood gas and serum electrolyte profile
There was no significant effect of RGZ on blood gas analyses (pH, PaCO2, and PaO2, Table 1) and serum electrolytes (serum potassium, sodium, and ionized calcium, Table 2) on either day 1 or day 7 at all doses of RGZ examined.
Table 1.
Blood gas measurements in 1 day and 7 days rosiglitazone treatment
| Rosiglitazone (mg/kg) | pH | Pco2 (mmHg) | Po2 (mmHg) | |||
|---|---|---|---|---|---|---|
| 1 Day | 7 Days | 1 Day | 7 Days | 1 Day | 7 Days | |
| 0 | 7.40 ± 0.02 | 7.47 ± 0.06 | 44.8 ± 9.36 | 46.3 ± 3.51 | 38.8 ± 8.3 | 43.7 ± 2.08 |
| 0.1 | 7.42 ± 0.01 | 7.43 ± 0.04 | 42.3 ± 2.53 | 45.0 ± 9.85 | 45.7 ± 5.85 | 32.0 ± 3.61 |
| 0.3 | 7.41 ± 0.04 | 7.50 ± 0.08 | 45.8 ± 6.03 | 46.7 ± 8.08 | 43.0 ± 5.13 | 33.2 ± 5.17 |
| 1 | 7.35 ± 0.04 | 7.48 ± 0.07 | 42.8 ± 7.79 | 45.7 ± 2.89 | 46.7 ± 5.13 | 29.3 ± 2.22 |
| 3 | 7.40 ± 0.02 | 7.40 ± 0.02 | 54.3 ± 3.05 | 46.7 ± 6.03 | 44.3 ± 3.78 | 36.0 ± 9.64 |
| 8 | 7.44 ± 0.03 | 7.45 ± 0.04 | 48.3 ± 2.08 | 47.0 ± 5.57 | 47.0 ± 2.65 | 30.0 ± 2.0 |
Values are mean ± SD, n=20 pups
Table 2.
Blood electrolyte measurements in 1 day and 7 days rosiglitazone treatment
| Rosiglitazone (mg/kg) | K+ (mEq/L) | Na+ (mEq/L) | Ca2+ (mEq/L) | |||
|---|---|---|---|---|---|---|
| 1 Day | 7 Days | 1 Day | 7 Days | 1 Day | 7 Days | |
| 0 | 4.85 ± 0.18 | 4.85 ± 0.69 | 137.5 ± 5.3 | 127.3 ± 2.3 | 1.33 ± 0.04 | 1.49 ± 0.06 |
| 0.1 | 5.18 ± 0.09 | 5.08 ± 0.56 | 132.3 ± 1.2 | 126.8 ± 2.4 | 1.38 ± 0.02 | 1.42 ± 0.11 |
| 0.3 | 4.39 ± 0.32 | 4.97 ± 0.77 | 133.8 ± 4.5 | 125.8 ± 2.4 | 1.38 ± 0.08 | 1.46 ± 0.07 |
| 1 | 4.83 ± 0.63 | 4.73 ± 0.66 | 133.5 ± 3.3 | 127.5 ± 6.2 | 1.40 ± 0.09 | 1.42 ± 0.07 |
| 3 | 4.22 ± 0.10 | 4.53 ± 0.49 | 138.7 ± 5.1 | 128.8 ± 1.9 | 1.43 ± 0.04 | 1.47 ± 0.12 |
| 8 | 4.99 ± 1.11 | 4.39 ± 0.58 | 137.7 ± 3.1 | 129.0 ± 1.7 | 1.33 ± 0.05 | 1.41 ± 0.05 |
Values are mean ± SD, n=20 pups
E. Effect of RGZ on blood glucose, cholesterol, triglyceride, and cardiac troponin levels (Table 3)
Table 3.
Blood glucose and serum lipid measurements in 1 day and 7 days rosiglitazone treatment
| Rosiglitazone (mg/kg) | Glucose (mg%) | Cholesterol (mg/dl) | Triglyceride (mg/dl) | |||
|---|---|---|---|---|---|---|
| 1 Day | 7 Days | 1 Day | 7 Days | 1 Day | 7 Days | |
| 0 | 85.3 ± 8.9 | 126.7 ± 2.9 | 115.9 ± 4.5 | 147.0 ± 20.5 | 132.5 ± 8.4 | 134.9 ± 5.8 |
| 0.1 | 91.8 ± 5.1 | 124.7 ± 3.8 | 106.5 ± 10.9 | 130.6 ± 13.7 | 118.7 ± 9.2 | 118.7 ± 23.2 |
| 0.3 | 98.8 ± 5.6 | 128.0 ± 5.3 | 108.7 ± 5.3 | 143.6 ± 22.7 | 132.3 ± 10.8 | 113.1 ± 8.9 |
| 1 | 87.2 ± 8.6 | 131.0 ± 5.3 | 105.5 ± 3.2 | 136.7 ± 26.7 | 130.1 ± 7.5 | 135.2 ± 10.3 |
| 3 | 93.0 ± 7.5 | 136.3 ± 11.7 | 105.9 ± 6.8 | 142.9 ± 7.33 | 130.8 ± 7.5 | 111.8 ± 7.0 |
| 8 | 83.0 ± 4.6 | 84.0 ± 14.9 | 105.9 ± 9.7 | 139.0 ± 17.4 | 131.3 ± 9.5 | 120.3 ± 12.2 |
Values are mean ± SD, n=20 pups
Since in the adult RGZ is used as a potent antidiabetic agent, we determined its effect on blood glucose levels. There was no significant effect on blood glucose at either day 1 or day 7, for all of the doses of RGZ examined except for the highest dose used, i.e., 8 mg/kg for 7 days, which resulted in statistically significantly lower glucose values compared to controls (84 ± 15 vs. 127 ± 3 (mean ± SD), (*p<0.05, RGZ vs. control). Lastly, troponin I levels were undetectable in both- the 7 day control and RGZ treated groups.
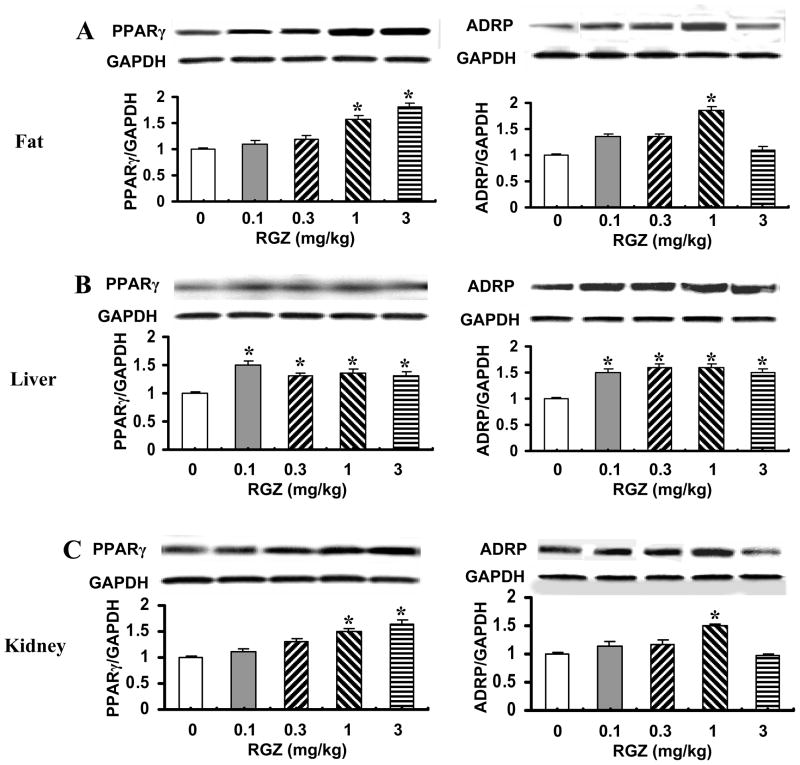
F. Effect of RGZ on PPARγ and ADRP expression in peritoneal fat, liver, and kidney
Since the PPARγ gene is expressed in a wide range of tissues, we next surveyed the effect of systemically administered RGZ on PPARγ and ADRP expression in a few selected extra-pulmonary PPARγ-expressing tissues such as the peritoneal fat (Fig. 5A), liver (Fig. 5B), and kidney (Fig. 5C). In general, 7 day systemic administration of RGZ increased PPARγ and ADRP expression in all extra-pulmonary PPARγ-expressing tissues examined (*=p<0.05 vs. controls; Fig. 5).
Fig. 5. Effect of rosiglitazone on PPARγ and ADRP expression in peritoneal fat, liver, and kidney.
The newborn rat pups were administered either diluent or RGZ in graded doses in 100μl volume once daily i.p. for 7 days and then PPARγ and ADRP expression was examined in the whole tissue lysates of peritoneal fat (A), liver (B), and kidney (C). In general, 7 day systemic administration of RGZ increased PPARγ and ADPR expression in all of the extra-pulmonary tissues examined. Representative Western blots from the whole tissue lysates and the corresponding density histograms are shown (Fig. 5, n=5, mean ± SD, *p<0.05, RGZ vs. control).
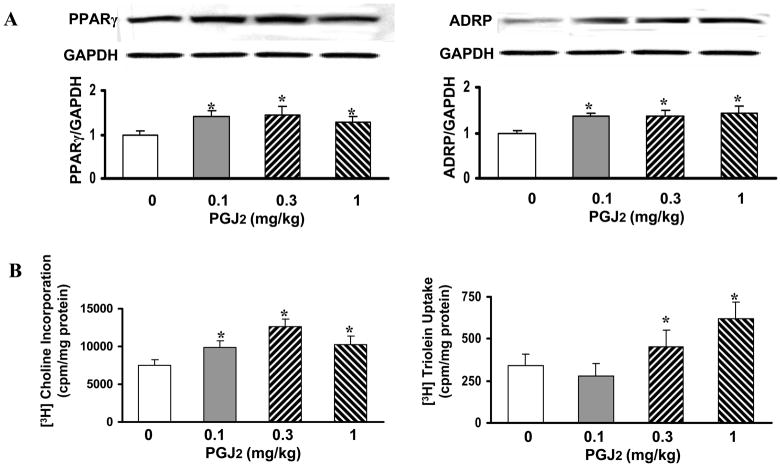
G. Effect of PGJ2 on alveolar differentiation
To determine that the effects of the PPARγ agonist RGZ observed by us for neonatal rat lung maturation are not RGZ specific, in a series of experiments, we treated neonatal pups with another PPARγ agonist PGJ2 (0.1–1 mg/kg) for 7 days and examined the expression of PPARγ and its down-stream target ADRP. Compared to controls, expression of both PPARγ and ADRP increased significantly with all 3 doses of PGJ2 examined (*=p<0.05, PGJ2 vs. control; Fig. 6A). Similar to RGZ’s effects on functional markers of lung maturation, i.e., [3H]choline incorporation and [3H]triolein uptake, by the lung explants of treated animals, in general, [3H]choline incorporation and [3H]triolein uptake by the lungs of PGJ2-treated animals also significantly increased (*=p<0.05, PGJ2 vs. control; Fig. 6B).
Fig. 6. Effect of PGJ2 on alveolar differentiation.
The newborn rat pups were administered either diluent or PGJ2 (0.1–1 mg/kg) for 7 days and then PPARγ and ADRP expression were examined. Compared to controls, expression of both PPARγ and ADRP increased significantly with all 3 doses of PGJ2 examined (*=p<0.05, PGJ2 vs. control; A). Similarly, [3H]choline incorporation and [3H]triolein uptake by the lungs of PGJ2-treated animals also increased significantly (Fig. 6, n=6, mean ± SD, *=p<0.05, PGJ2 vs. control; B).
Discussion
Since pulmonary immaturity is the principal contributor to the premature infant’s significantly increased risk for morbidity and mortality, attempts to advance lung maturity have been a major research focus for decades. This has led to the widespread use of antenatal steroids, which result in significantly enhanced lung maturity, with the resultant significant decrease in morbidity and mortality associated with prematurity (5). However, in contrast to the beneficial effects of antenatal steroids, there is no intervention that has been shown to consistently enhance pulmonary maturity postnatally (14–16). In fact, daily administration of dexamethasone to newborn rats from postnatal day 4 to 13 irreversibly impairs saccule septation (14), which persists at least until postnatal day 60 (15). Furthermore, significant concerns over the adverse effects of postnatal steroids on infants’ neurodevelopment preclude their routine use during the postnatal period (16).
In this study, we show that the PPARγ agonist RGZ, given daily systemically to Sprague Dawley rat pups, results in significantly enhanced pulmonary maturity, as evidenced by increased expression of surfactant proteins B and C, and increased surfactant phospholipids synthesis, the markers of pulmonary epithelial differentiation, at both days 1 and 7. This was accompanied by the significantly increased expression of PTHrP receptor, PPARγ, ADRP, and increased triolein uptake, key markers of lung mesenchymal differentiation, at both days 1 and 7. At day 7, there was evidence for increased alveolarization, as supported by increased radial alveolar count and decreased mean linear intercept, which was also accompanied by increased lung vascularization, as evidenced by increased expression of VEGF (and its receptor), the key regulator of lung vascularization during development. Furthermore, as expected, the effects of RGZ were not lung-specific since there was also increased expression of PPARγ and ADRP in all of the PPARγ-expressing extra-pulmonary tissues examined. However, there were no significant effects of RGZ on blood gases, serum electrolytes, blood glucose, cholesterol, or triglyceride levels, except at the highest dose used, i.e., 8 mg/kg, which resulted in statistically significantly lower blood glucose values, suggesting that systemically administered RGZ significantly enhanced lung maturation without significantly affecting basic blood biochemical and metabolic profiles. Based on these findings, we speculate that PPARγ agonists may be therapeutically effective agents for enhancing lung maturation and promoting lung injury repair in neonates.
In humans, PPARγ is highly expressed in adipose tissue, and serves as an important transcriptional regulator of genes involved in glucose and lipid metabolism, cell proliferation, and control of inflammation (17). Expression and activation of PPARγ is sufficient to trigger the adipocyte differentiation cascade and to confer a lipid-storing phenotype on mesenchymal cells in culture (18). In the developing lung, PPARγ expression has been clearly documented in lipid-laden lung alveolar interstitial fibroblasts (~lipofibroblasts) as well as in alveolar type II (ATII) cells (3,4,19). Although there are only limited data on PPARγ’s role in the alveolar epithelium, there is extensive information on its role in the lung mesenchyme (2,4,20,21). Pulmonary lipofibroblasts express PPARγ, as well as other genes involved in lipid metabolism, e.g., genes involved in the hydrolysis of triglycerides at the plasma membrane, in the transport of fatty acids across the plasma membrane, as well as ADRP, which is necessary for uptake, storage and exocytosis of lipid droplets (2,19). PPARγ expression in alveolar adepithelial lipofibroblasts has been shown to promote alveolar development and homeostasis via the PTHrP-PPARγ alveolar epithelial-mesenchymal paracrine signaling pathway (2,19,20,22). PPARγ’s epithelial expression is also critical in lung development, as indicated by the fact that airway epithelial cell PPARγ-deficient mice show persistent abnormalities in postnatal lung maturation, evidenced by enlarged airspaces and the accompanying alterations in lung physiology and whole lung extracellular matrix gene expression pattern (4). In addition to PPARγ’s previously highlighted role in lung alveolar epithelial-mesenchymal interactions, the data presented here for the first time also suggest its role in the pulmonary vasculature during lung development. This possibly provides an integrated mechanistic basis for enhanced lung development following exogenous systemic PPARγ agonist administration, i.e., coordinated stimulation of the epithelial, mesenchymal, and vascular compartments of the developing lung.
Although a variety of structurally distinct molecules have been shown to bind and activate PPARγ, due to extensive clinical experience with the synthetic thiazolidinedione compound RGZ, we chose to use RGZ in this study (21). The dose range of RGZ chosen in this study was based upon our previous work and that of others (23–26). The fact that lung maturation was stimulated by not only RGZ, but also by the naturally occurring PPARγ agonist PGJ2 suggests that this effect is not ligand-specific and is likely mediated by PPAR-γ-dependent rather than PPAR-independent activities of PPAR agonists. Since activation of PPARγ also regulates the transcription of insulin-responsive genes involved in the control of glucose production, transport, and utilization, we also examined whether the use of RGZ would affect blood glucose in normal rat pups. It was reassuring to note that daily RGZ administration to neonatal pups for up to 7 days did not result in hypoglycemia. In addition, since PPARγ-responsive genes also participate in the regulation of lipid metabolism, and have been shown to affect plasma lipid profiles when used long-term in adults (27), we examined the effect of RGZ administration for 7 days to neonatal rat pups on blood cholesterol and total triglyceride levels, but did not find any significant effect on these parameters. Furthermore, since RGZ has been shown to exacerbate and/or lead to cardiac failure (28), we examined its effect on plasma cardiac troponin levels and found undetectable troponin I levels in both control and 7 day RGZ-treated pups. Although it is reassuring to note that cardiac troponin I levels were below the detection limit of the kit we used, it can not be concluded with certainty that RGZ administration did not affect cardiac troponin I levels at all. Lastly, it was also reassuring to note that systemic administration of RGZ for 7 days did not affect neonatal rat pup blood gases and serum electrolytes significantly.
It is important to note that since safety and efficacy of PPARγ agonists such as RGZ has not been tested in the neonatal/pediatric population, their clinical use can not be recommended at present. However, the work presented here provides proof-of-principle for their efficacy in promoting lung maturation. Furthermore, although it is reassuring to note that acute blood parameters examined here were not affected by up to 7 days of treatment with RGZ, more rigorous testing, including its long-term effects need to be evaluated before its use in the human infant can be considered. On the whole, our data provide a strong case for further exploring the use of PPARγ agonists for the purposes of enhancing lung maturation and for possibly promoting lung injury/repair.
Acknowledgments
This study was supported by grants from the NIH (HL075405 and HL55268) and the TRDRP (14RT-0073 and 15IT-0250).
Abbreviations
- ADRP
Adipocyte Differentiation-Related Protein
- ATII
Alveolar Type 2
- PPARγ
Peroxisome Proliferator-Activated Receptor Gamma
- PGJ2
Prostaglandin J2
- PTHrP
Parathyroid Hormone-related Protein
- RGZ
Rosiglitazone
- SP
Surfactant Protein
- VEGF
Vascular Endothelial Growth Factor
References
- 1.Tontonoz P, Hu E, Spiegelman BM. Regulation of adipocyte gene expression and differentiation by peroxisome proliferator activated receptor gamma. Curr Opin Genet Dev. 1995;5:571–576. doi: 10.1016/0959-437x(95)80025-5. [DOI] [PubMed] [Google Scholar]
- 2.Chen H, Jackson S, Doro M, McGowan S. Perinatal expression of genes that may participate in lipid metabolism by lipid-laden lung fibroblasts. J Lipid Res. 1998;39:2483–2492. [PubMed] [Google Scholar]
- 3.Torday JS, Torres E, Rehan VK. The role of fibroblast transdifferentiation in lung epithelial cell proliferation, differentiation, and repair in vitro. Pediatr Pathol Mol Med. 2003;22:189–207. doi: 10.1080/pdp.22.3.189.207. [DOI] [PubMed] [Google Scholar]
- 4.Simon DM, Arikan MC, Srisuma S, Bhattacharya S, Tsai LW, Ingenito EP, Gonzalez F, Shapiro SD, Mariani TJ. Epithelial cell PPAR[gamma] contributes to normal lung maturation. FASEB J. 2006;20:1507–1509. doi: 10.1096/fj.05-5410fje. [DOI] [PubMed] [Google Scholar]
- 5.NIH Consensus Development Panel on the Effect of Corticosteroids for Fetal Maturation on Perinatal Outcomes. Effect of corticosteroids for fetal maturation on perinatal outcomes. JAMA. 1995;273:413–418. doi: 10.1001/jama.1995.03520290065031. [DOI] [PubMed] [Google Scholar]
- 6.Wapner RJ, Sorokin Y, Mele L, Johnson F, Dudley DJ, Spong CY, et al. Long-term outcomes after repeat doses of antenatal corticosteroids. N Engl J Med. 2007;357:1190–1198. doi: 10.1056/NEJMoa071453. [DOI] [PubMed] [Google Scholar]
- 7.Ballard PL, Ballard RA, Granberg JP, Sniderman S, Gluckman PD, Kaplan SL, Grumbach MM. Fetal sex and prenatal betamethasone therapy. J Pediatr. 1980;97:451–454. doi: 10.1016/s0022-3476(80)80204-6. [DOI] [PubMed] [Google Scholar]
- 8.Nielson HC, Torday JS. Sex differences in fetal lung development: Biology, Etiology, and Evolutionary Significance. In: Mendelson CR, editor. Endocrinology of the Lung-Development and Surfactant Synthesis. Humana Press; Totowa, New Jersey: 2000. pp. 141–159. [Google Scholar]
- 9.Willet KE, Jobe AH, Ikegami M, Newnham J, Sly PD. Antenatal retinioic acid does not alter alveolization or postnatal lung function in preterm sheep. Eur Respir. 2000;J16:101–107. doi: 10.1034/j.1399-3003.2000.16a18.x. [DOI] [PubMed] [Google Scholar]
- 10.Srinivasan G, Bruce EN, Houtz PK, Bruce MC. Dexamethasone-induced changes in lung function are not prevented by concomitant treatment with retinoic acid. Am J Physiol Lung Cell Mol Physiol. 2002;283:L275–287. doi: 10.1152/ajplung.00423.2001. [DOI] [PubMed] [Google Scholar]
- 11.Rehan VK, Wang Y, Sugano S, Santos J, Patel S, Sakurai R, Boros LG, Lee WP, Torday JS. In utero nicotine exposure alters fetal rat lung alveolar type II cell proliferation, differentiation, and metabolism. Am J Physiol Lung Cell Mol Physiol. 2007;292:L323–333. doi: 10.1152/ajplung.00071.2006. [DOI] [PubMed] [Google Scholar]
- 12.Randell SH, Mercer RR, Young SL. Postnatal growth of pulmonary acini and alveoli in normal and oxygen-exposed rats studied by serial section reconstructions. Am J Anat. 1989;186:55–68. doi: 10.1002/aja.1001860105. [DOI] [PubMed] [Google Scholar]
- 13.Carmeliet P, Ferreira V, Breier G, Pollefeyt S, Kieckens L, Gertsenstein M, et al. Abnormal blood vessel development and lethality in embryos lacking a single VEGF allele. Nature. 1996;380:435–439. doi: 10.1038/380435a0. [DOI] [PubMed] [Google Scholar]
- 14.Massaro D, Massaro GD. Dexamethasone accelerates postnatal alveolar wall thinning and alters wall composition. Am J Physiol. 1986;251:R218–224. doi: 10.1152/ajpregu.1986.251.2.R218. [DOI] [PubMed] [Google Scholar]
- 15.Massaro D, Teich N, Maxwell S, Massaro GD, Whitney P. Postnatal development of alveoli. Regulation and evidence for a critical period in rats. J Clin Invest. 1985;76:1297–1305. doi: 10.1172/JCI112103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cerny L, Torday JS, Rehan VK. Prevention and treatment of bronchopulmonary dysplasia: contemporary status and future outlook. Lung. 2008;186:75–89. doi: 10.1007/s00408-007-9069-z. [DOI] [PubMed] [Google Scholar]
- 17.Heikkinen S, Auwerx J, Argmann CA. PPARgamma in human and mouse physiology. Biochem Biophys Acta. 2007;1771:999–1013. doi: 10.1016/j.bbalip.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tontonoz P, Hu E, Spiegelman BM. Regulation of adipocyte gene expression and differentiation by peroxisome proliferator activated receptor gamma. Curr Opin Genet Dev. 1995;5:571–576. doi: 10.1016/0959-437x(95)80025-5. [DOI] [PubMed] [Google Scholar]
- 19.Rehan VK, Sugano S, Wang Y, Santos J, Romero S, Dasgupta C, Keane MP, Stahlman MT, Torday JS. Evidence for the presence of lipofibroblasts in human lung. Exp Lung Res. 2006;32:379–393. doi: 10.1080/01902140600880257. [DOI] [PubMed] [Google Scholar]
- 20.Torday JS, Rehan VK. Developmental cell/molecular biologic approach to the etiology and treatment of bronchopulmonary dysplasia. Pediatr Res. 2007;62:2–7. doi: 10.1203/PDR.0b013e31806772a1. [DOI] [PubMed] [Google Scholar]
- 21.Standiford TJ, Keshamouni VG, Reddy RC. Peroxisome proliferator-activated receptor-{gamma} as a regulator of lung inflammation and repair. Proc Am Thorac Soc. 2005;2:226–231. doi: 10.1513/pats.200501-010AC. [DOI] [PubMed] [Google Scholar]
- 22.Torday JS, Rehan VK. Stretch-stimulated surfactant synthesis is coordinated by the paracrine actions of PTHrP and leptin. Am J Physiol Lung Cell Mol Physiol. 2002;283:L130–135. doi: 10.1152/ajplung.00380.2001. [DOI] [PubMed] [Google Scholar]
- 23.Liu D, Zeng BX, Zhang SH, Yao SL. Rosiglitazone, an agonist of peroxisome proliferator-activated receptor gamma, reduces pulmonary inflammatory response in a rat model of endotoxemia. Inflamm Res. 2005;54:464–470. doi: 10.1007/s00011-005-1379-0. [DOI] [PubMed] [Google Scholar]
- 24.Rehan VK, Wang Y, Patel S, Santos J, Torday JS. Rosiglitazone, a peroxisome proliferator-activated receptor-gamma agonist, prevents hyperoxia-induced neonatal rat lung injury in vivo. Pediatr Pulmonol. 2006;41:558–569. doi: 10.1002/ppul.20407. [DOI] [PubMed] [Google Scholar]
- 25.Wayman NS, Hattori Y, McDonald MC, Mota-Filipe H, Cuzzocrea S, Pisano B, Chatterjee PK, Thiemermann C. Ligands of the peroxisome proliferator-activated receptors (PPAR-gamma and PPAR-alpha) reduce myocardial infarct size. FASEB J. 2002;16:1027–1040. doi: 10.1096/fj.01-0793com. [DOI] [PubMed] [Google Scholar]
- 26.Genovese T, Cuzzocrea S, Di Paola R, Mazzon E, Mastruzzo C, Catalano P, Sortino M, Crimi N, Caputi AP, Thiemermann C, Vancheri C. Effect of rosiglitazone and 15-deoxy-Delta12,14-prostaglandin J2 on bleomycin-induced lung injury. Eur Respir J. 2005;25:225–234. doi: 10.1183/09031936.05.00049704. [DOI] [PubMed] [Google Scholar]
- 27.Khan MA, St Peter JV, Xue JL. A prospective, randomized comparison of the metabolic effects of pioglitazone or rosiglitazone in patients with type 2 diabetes who were previously treated with troglitazone. Diabetes Care. 2002;25:708–711. doi: 10.2337/diacare.25.4.708. [DOI] [PubMed] [Google Scholar]
- 28.Home PD, Pocock SJ, Beck-Nielsen H, Gomis R, Hanefeld M, Jones NP, Komajda M, McMurray JJ. Rosiglitazone evaluated for cardiovascular outcomes--an interim analysis. N Engl J Med. 2007;357:28–38. doi: 10.1056/NEJMoa073394. [DOI] [PubMed] [Google Scholar]