Abstract
Catatonia in the setting of a mood disorder, an organic process, or a psychotic disorder presents significant risk to the patient’s well-being, as well as an additional barrier to treating the underlying disorder. The signs and symptoms of catatonia interfere severely with essential activities of daily living; they also at times compromise the ability of caregivers to evaluate and treat the patient’s primary disorder driving the catatonia. This interference often leads to medical emergencies, such as marked dehydration and pressure ulcers. Another life-threatening complication of the immobility commonly seen in catatonic patients is the development of deep vein thromboses (DVT) and pulmonary emboli. As with all patients, it is critical to provide preventative measures where possible to minimize risk of complications. Routine anticoagulation perhaps deserves more consideration in the case of catatonia, such as the one presented in this case report.
Keywords: catatonia, anticoagulation therapy, pulmonary embolism, immobility, major depressive disorder
Introduction
In this report, we discuss the case of a woman with major depressive disorder with catatonic features, who due to medication nonadherence and a slow recovery, developed pulmonary emboli. We believe this is the first detailed discussion of catatonia associated with depression that progressed to this deadly complication. This case examines the need to aggressively treat catatonic patients who are refractory to initial treatment. We also review signs, symptoms, and risk factors of embolism and discuss embolism prophylaxis and subsequent management.
Case Presentation
Ms. K was a 34-year-old African American woman admitted to the state psychiatric hospital with a past medical history of major depressive disorder with psychotic features and nonadherence with medications. The patient had been hospitalized over 10 times in the past two years for major depressive episodes. At baseline, Ms. K was a high functioning individual who held a good job and home-schooled her children. Most recently, the patient’s husband actively sought out psychiatric care for Ms. K when she would not eat, drink, complete activities of daily living (bathing), and was completely unresponsive for the duration of three days.
Upon this presentation (Day 1), Ms. K was healthy and alert, but essentially mute, answering questions by nodding her head a fraction of the time. The mental status exam was positive for mutism with minimal eye contact and movement. Mood, thought process, thought content, perception, orientation, memory, and judgment were all unable to be assessed. Her affect was dysphoric, flat, and non-labile. Her insight was judged to be poor due to her repeated nonadherence to treatment and subsequent hospitalizations. Her intellectual functioning was judged to be average to above average based on her academic achievements. The patient significantly minimized her illness.
Ms. K had a normal physical exam on Day 1 and her EKG showed sinus tachycardia at 107 beats per minute, with nonspecific T-wave changes; however, the patient was not in acute distress and did not complain of any chest pain or shortness of breath. Oxygen saturation was 100 percent. Her labs from Day 28 revealed a normal basic metabolic panel, CBC, CPK, RPR, thyroid function tests, liver function tests, serum hCG, B12 and folic acid levels with the following exceptions: low potassium at 3.1mEq/L, chloride high at 111mEq/L, high glucose at 129mg/dL, low WBC count at 3.7 x 103 per µL, and a B12 level over 2000pg/mL. An magnetic resonance imaging (MRI) of the brain was unremarkable. Ms. K was started on escitalopram 20mg q.a.m. and lorazepam 2mg q.i.d. Electro convulsive therapy (ECT) was discussed, but the patient refused. Collateral history revealed that risperidone 2mg b.i.d. was effective for past depressive episodes; therefore, it was added after minimal response from the previous medications. As the catatonic features began to subside, this patient’s affect remained blunted and dysphoric; therefore, duloxetine 30mg b.i.d. was added. The patient slowly responded to treatment and was discharged on Day 40.
On Day 48, the patient was readmitted to the state hospital with similar catatonic features precipitated by medication nonadherence after initial discharge. Ms K. believed that she no longer had a mental illness, and that the lorazepam would just prevent her from continuing her daily activities effectively. Physical exam was noncontributory, but her oxygen saturation was 93 percent as opposed to 100 percent on Day 1. Ms. K’s catatonia continued to impair her movement and functioning, and was so severe that she refused food and medications. On Day 49, she was taken to a community hospital emergency room for severe dehydration and was given intravenous fluids over several hours. The patient was returned to the state mental facility on the same day where her previous medication regiment was reinstated. At this point, Ms. K began to have labored breathing with an increased respiratory rate, and her pulse oximetry now read approximately 80 percent. She was immediately taken back to the same emergency department for acute evaluation. There, her EKG showed inverted T-waves, and a spiral computed tomography (CT) scan demonstrated bilateral pulmonary emboli. She was started on intravenous heparin and was later switched to warfarin sodium with an international normalized ratio (INR) goal of 2.5 to 3.0. She continued to take her psychotropic medications while in the community hospital.
On Day 65, Ms. K was released back to the state mental hospital. Having been on her medications for just over two weeks, she began to show gradual resolution of her major depressive disorder with catatonic features. Initially, she was able to express herself verbally, and later her movements became more fluid. Her affect brightened, and she began to participate in treatment groups and social activities on the ward. The family of the patient was educated on the importance of adherence. Ms. K was scheduled for follow-up appointments at an outpatient clinic to include case management, and discharged home.
Diagnostic and Associated Features
The term catatonia is used in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Revision (DSM-IV) as a subtype and a specifier. Catatonia as a subtype of schizophrenia is often discussed in literature, but this condition is most often seen in the psychiatric population as a specifier to affective disorders. Acute catatonia has a prevalence in an inpatient psychiatric population of 7 to 15 percent.1 The catatonic patient probably frequently goes unrecognized due to the unfounded belief that catatonia is diminishing in developed countries.2
The diagnosis of catatonia is largely based on patient interview, observation, collateral history, mental status examination, and physical examination, with special emphasis on neurological findings. Recognition of the wide-ranging signs and symptoms of catatonia is essential to successful diagnosis (Table 1).3 The patient in the case presented in the article had motoric immobility evidenced as a stupor, as well as extreme negativism and mutism. Coupled with the patient’s long history of depression, the diagnosis of major depressive disorder with catatonic features was made after medical causes of acute catatonia were ruled out.
Table 1.
DSM-IV-TR criteria for catatonia as a mood specifier
| SPECIFY IF: |
| With catatonic features (can be applied to the current or most recent major depressive episode, manic episode, or mixed episode in major depressive disorder, bipolar I disorder, or bipolar II disorder) |
THE CLINICAL PICTURE IS DOMINATED BY AT LEAST TWO OF THE FOLLOWING:
|
As the syndrome of catatonia stretches across psychiatric and medical disorders, the laboratory work-up to correctly diagnosis it is primarily focused on picking up underlying medical or neurologic disorders that may be causing the catatonic presentation. Non-psychiatric conditions that may induce catatonia include metabolic derangements, drug intoxication and withdrawal, seizure disorders, thalamic lesions, parietal and frontal lobe disease, general paresis, Parkinsonism, endocrinopathies, viral infections, including HIV and typhoid fever, heatstroke, and various autoimmune diseases.
In our case, neuroleptic malignant syndrome (NMS) and lethal catatonia were excluded, as the patient had no fever or elevated CPK. A psychiatrist must always rule out the lethal form of catatonia, which leads to mortality in 44 percent of cases.4 However, the term acute non-lethal catatonia is a misnomer, as the condition can lead to deadly complications.
General Treatment of Catatonia
The mainstay of treatment of catatonic patients has for decades remained a selection of somatic treatments. Benzodiazepines, particularly lorazepam, barbiturates, and electroconvulsive therapy (ECT) are the most efficacious therapies available to patients. Bush and colleagues demonstrated that 76 percent of acutely catatonic patients were responsive to 4 to 8mg of lorazepam per day; the remaining patients were successfully treated with ECT.5 ECT is well known to be efficacious in mania, depression, and catatonia. Hawkins, et al., revealed ECT to have an 85-percent response rate in catatonic patients, and proposed that this therapy should be used when rapid resolution of symptoms is necessary.6 Due to the lack of ECT availability in many state facilities, stigma surrounding the procedure, and difficulty with informed consent in an acute inpatient setting, this procedure is rarely preformed when most needed. Our patient refused transportation to receive ECT at a community hospital on several occasions.
None of these particular somatic treatments are efficacious for schizophrenia itself, and catatonia resulting from schizophrenia may be somewhat less responsive to these interventions than is catatonia from other etiologies.7 Currently, the use of antipsychotics is controversial in the treatment of catatonia. First-generation neuroleptics may worsen all forms of catatonia. Case reports and retrospective studies reveal that second-generation antipsychotics, including risperidone, may be of benefit in the acute non-lethal form of catatonia.9 Perhaps the addition of risperidone in the case of our patient helped resolve her catatonia along with her severe depression.
Infrequent case reports describe attempts to help catatonic patients with other medications and treatments, including amantidine, bromocriptine, dantrolene, zolpidem, lithium, carbamazepine, and transcranial magnetic stimulation (TMS). Evidence for efficacy of these modalities falls short of the literature accumulated for lorazepam. The benzodiazepines treat the specific syndrome of catatonia, without amelioration of the underlying disorder, which was in this case major depression. When the catatonia resolved, our patient remained depressed. Experts believe this is further evidence that the pathophysiology of catatonia is distinct from that of any specific psychiatric disorder.7
It is essential to employ these treatments directed at the catatonic syndrome itself quickly after diagnosis, especially if the patient is not eating, drinking, or moving spontaneously. Without resolution of these severe impairments, delivering other treatments, such as antidepressants, will be severely hindered as there are very limited choices for parenteral routes of administration. Often intramuscular or intravenous lorazepam must be given on an emergency basis in order to break the catatonia sufficiently to allow for further treatment options, as well as for diagnostic interviews and informed consent discussions. The syndrome may take hours to several days to resolve, and treatment may need to continue for months to prevent relapse.
Lethal Complications of Catatonia
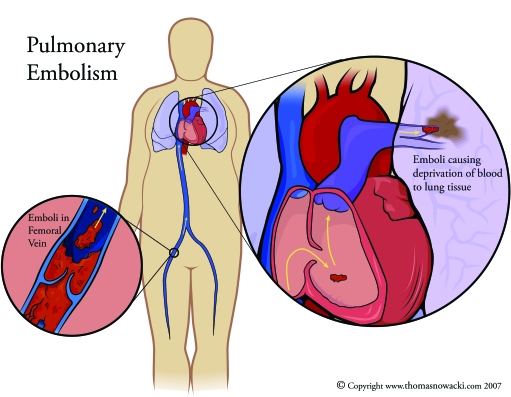
Profound negativism, immobility, and refusal to take in fluids predisposes patients to malnutrition, dehydration, rhabdomyolysis, aspiration pneumonia, obstructive nephropathy, azotemia, deep vein thrombosis (DVT), and ultimately pulmonary embolizm (PE).9,10 Autopsies of catatonic patients revealed a seven-percent mortality by PE.11 Virchow’s triad of venous stasis, endothelial damage, and hypercoagulabilty are the classic risk factors for DVT. The thrombosis can then dislodge and lead to an embolism (Figure 1).13 McCall and colleagues revealed that fatal embolisms associated with catatonia occurred after two weeks or more of continuous catatonic symptoms. The time may account for the DVT formation, and embolism may occur upon symptom resolution and subsequent ambulation.14 Catatonia that does not respond to oral medications in the first few days must be treated as an emergent situation. Rapid resolution was needed in this particular case, and ECT probably would have been tremendously helpful in breaking both the depression and the catatonia.
Figure 1.
Progression of a PE (Copyright permission obtained from www.thomasnowacki.com)
Just as a patient who remains motionless for long periods of time on an airplane is at risk for a PE, so is a catatonic patient who has remained motionless for many days.15 A second risk factor our patient faced was dehydration due to lack of fluid intake. Also, patients with depression, like Ms. K, may be at further risk due to lower platelet serotonin uptake.16 Depression leads to a 41-percent greater platelet activation with higher procoagulant properties.17
Prophylactic Treatments in Catatonic Patients
DVT and PE may be less readily considered complications of the immobility inherent in catatonia than are the more immediate concerns for dehydration and decreased urine output. The physician must conduct frequent physical exams to evaluate for these and other complications, as the patient’s ability to report symptoms will be seriously impaired. As in the case presented, a patient in a severe catatonic state that involves mutism and negativism will likely be unable to communicate leg pain from a DVT, as well as any other medical complaints he or she may have.12 A psychiatrist should be aware of the signs of DVT, such as posterior calf pain, swelling, and warmth, as well as a less reliable positive Homan’s sign (increased resistance or pain with dorsiflexion of the foot). Diagnosis of DVT is made using a Doppler ultrasound of the lower extremity. Ms K developed the most common symptom of PE, dyspnea; as well as the most common sign, tachypnea.18 Diagnosis of a PE is made by a ventilation-perfusion (V-Q) scan, or a spiral CT of the chest as was done in our patient. D-dimer assays are sensitive but not specific in diagnosing PE and are a good initial investigation; however, we did not have immediate access to such a test.19
Much has been published on the prophylactic treatments for hypercoagulability available while patients are hospitalized, based on stratified risk. Various formulations of heparin are used in treatment and prevention of DVT and PE. Heparin works as an anticoagulant by binding to antithrombin III, producing a change that allows anti-thrombin III to more rapidly inhibit thrombin. Unfractionated heparin carries a risk of bleeding by elevating partial thromboplastin time (PTT). Also, heparin-induced thrombocytopenia (HIT) may occur in as many as 10 to 20 percent of treated patients.20 The low cost is also offset by the daily blood draws and lab work necessary to assess platelet count and PTT. Side effects are significantly lessened with the low molecular weight preparations, such as enoxaparin. Platelet counts may be evaluated every 5 to 10 days due to the decreased risk of HIT, and PTT does not need to be followed. Contraindications to heparin use include active bleeding, liver disease with elevated PTT at baseline, malignant hypertension, and suspected HIT.20
Vitamin K antagonists, such as warfarin, are not favored for prophylaxis due to their complex management and delayed onset of action.21 Instead, warfarin is used as secondary therapy after a patient has sustained a PE. In this case, Ms. K was sent back to the psychiatric hospital on warfarin; therefore, interactions with psychotropics had to be considered in order to maintain an INR of 2.5 to 3.0. For example, fluoxetine and fluvoxamine have been shown to increase INR, while carbamazepine has been shown to decrease INR.22
Other nonpharmacologic prophylactic options include placement of elastic stockings, devices for intermittent pneumatic compression, and ambulation or exercises, which all work to prevent stasis by helping muscles push the blood pooling in lower extremity veins back toward the heart. In addition, combining one of these interventions with heparin may be more effective than using either method alone.21 It is important to consider in the risk-benefit analysis that each of these prophylactic modalities pose special risks on an acute psychiatric unit: decreased clotting may become a factor if physically aggressive patients are also treated on the unit, and pneumatic devices with cords as well as elastic stockings may provide means for self-harm behaviors or suicide. Range of motion exercises can be attempted to lessen the immobility, but catatonic symptoms, such as negativism and waxy flexibility, may hinder this.
Considering the above risks, prophylaxis through once daily subcutaneous enoxaparin 40mg is justified in an immobile catatonic patient who is not responding to medications within the first few days of treatment, especially when other risk factors for PE are present (Table 2). 21 A medicine consult is advised if a psychiatrist recognizes the risk factors, but does not feel comfortable using anticoagulants. Also, the treating team must consider the need to transfer the patient to a medical facility or unit.
Table 2.
Risk factors for pulmonary embolism
| PULMONARY EMBOLISM RISK FACTORS | |
|---|---|
| RISK FACTOR | EXPLANATION |
| Inactivity and/or prolonged bed rest | Increases venous stasis |
| Previous PE or DVT | A personal history or immediate family history of clotting are at risks |
| Surgical procedures | Abdominal, hip or knee replacement, or obstetric/gynecological procedures are higher risk |
| Medical and genetic conditions | Cancer, chemotherapy, menopausal women on tamoxifen or raloxifene, hypertension, cardiovascular disease (esp. acute exacerbation of CHF), pulmonary disease (esp. acute exacerbation of COPD), factor V Leiden, and antiphospholipid antibody |
| Overweight BMI | Overweight people produce more leptin, predisposing them to clot formation |
| Pacemakers or venous catheters | Clots can form on these foreign bodies |
| Pregnancy and childbirth | Aside from increased rates of bed rest and venous stasis, pregnancy is a hypercoagulable state |
| Birth control pills | Clotting factors in blood increase in response to estrogen in these medications |
| Smoking | Increased risk of thrombosis |
| Dehydration | An acquired risk factor for thrombosis |
| Increasing age | Unmodifiable risk for thrombosis |
Conclusion
The case presented reveals the devastating complications of a major depressive episode with catatonic features, particularly PE. Special attention must be paid to a patient who remains refractory to benzodiazepines, especially when the motionless catatonic features persist for days. Symptoms lasting longer than 72 hours may require ECT, among other immediate interventions.14 A psychiatrist must never abandon the medical training necessary to recognize the signs and symptoms of general medical conditions that contribute to or arise from Axis I disorders. Physicians with proper knowledge can aggressively treat and prevent potentially lethal complications and side effects. Furthermore, such prophylaxis can be applied to all psychiatric patients with significant thromboembolic risk factors.
References
- 1.Fink M, Taylor MA. Catatonia: Subtype or syndrome in DSM (Editorial) Am J Psychiatry. 2006;163(11):1875–6. doi: 10.1176/ajp.2006.163.11.1875. [DOI] [PubMed] [Google Scholar]
- 2.Chalasani P, Healy D, Morriss R. Presentation and frequency of catatonia in new admissions to two acute psychiatric admission units in India and Wales. Psycholog Med. 2005;35:1667–75. doi: 10.1017/S0033291705005453. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Revision, Text Revision. Washington, DC: American Psychiatric Press, Inc.; 2000. [Google Scholar]
- 4.Rosebush P, Hildebrand A, Furlong B, et al. Catatonic syndrome in a general psychiatric population: Frequency, clinical presentation, and response to lorazepam. J Clin Psychiatry. 1990;51:357–62. [PubMed] [Google Scholar]
- 5.Bush G, Fink M, Petrides G, et al. Catatonia. II. Treatment with lorazepam and electroconvulsive therapy. Acta Psychiatr Scand. 1996;93:137–43. doi: 10.1111/j.1600-0447.1996.tb09815.x. [DOI] [PubMed] [Google Scholar]
- 6.Hawkins JM, Archer KJ, Strakowski SM, Keck PE. Somatic treatment of catatonia. Int J Psychiatry Med. 1995;25(4):345–69. doi: 10.2190/X0FF-VU7G-QQP7-L5V7. [DOI] [PubMed] [Google Scholar]
- 7.Ungvari GS, Kau LS, Wai-Kwong T, Shing NF. The pharmacological treatment of catatonia: an overview. Eur Arch Psychiatry Clin Neurosci. 2001;251(Suppl. 1):31–4. doi: 10.1007/pl00014198. [DOI] [PubMed] [Google Scholar]
- 8.Van Den Eede F, Van Hecke J, Van Dalfson A, et al. The use of atypical antipsychotics in the treatment of catatonia. Eur Psychiatr. 2005;20(5–6):422–9. doi: 10.1016/j.eurpsy.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Carroll BT. Catatonia on the consultation-liaison service. Psychosomatics. 1992;32:310–15. doi: 10.1016/S0033-3182(92)71970-7. [DOI] [PubMed] [Google Scholar]
- 10.Carroll BT. Complications of catatonia (letter) J Clin Psychiatry. 1996;57:95. [PubMed] [Google Scholar]
- 11.Hussar AE. Leading causes of death in institutionalized chronic schizophrenic patients: A study of 1,275 autopsy protocols. J Nerv Ment Dis. 1966;142(1):45–57. doi: 10.1097/00005053-196601000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Lachner C, Sandson NB. Medical complications of catatonia: A case of catatonia-induced deep venous thrombosis. Psychosomatics. 2003;44:512–14. doi: 10.1176/appi.psy.44.6.512. [DOI] [PubMed] [Google Scholar]
- 13.Carson JL, Kelley MA, Duff A, et al. The clinical course of pulmonary embolism. N Engl J Med. 1992;326:1240–5. doi: 10.1056/NEJM199205073261902. [DOI] [PubMed] [Google Scholar]
- 14.McCall WV, Mann SC, Shelp FE, Caroff SN. Fatal pulmonary embolism in the catatonic syndrome: Two case reports and a literature review. J Clin Psychiatry. 1995;56:21–5. [PubMed] [Google Scholar]
- 15.Bagshaw M. Traveller's thrombosis: A review of deep vein thrombosis associated with travel. Aviat Space Environ Med. 2001;72(9):848–51. [PubMed] [Google Scholar]
- 16.Tuomisto J, Tukiainen E. Decreased uptake of 5-hydroxytryptamine in blood platelets from depressed patients. Nature. 1976;262:596–8. doi: 10.1038/262596a0. [DOI] [PubMed] [Google Scholar]
- 17.Musselman DL, Tomer A, Manatunga AK, et al. Exaggerated platelet reactivity in major depression. Am J Psychiatry. 1996;153:1313–17. doi: 10.1176/ajp.153.10.1313. [DOI] [PubMed] [Google Scholar]
- 18.Golghaber S, Pulmonary embolism. Harrison's Principles of Internal Medicine. In: Fauci A, Braunwald E, Isselbacher K, editors. 15th. New York, NY: McGraw-Hill; 2001. pp. 1508–13. [Google Scholar]
- 19.Dixon AK, Coulden RA, Peters AM. The noninvasive diagnosis of pulmonary embolus. Br Med J. 2001;323:412–13. doi: 10.1136/bmj.323.7310.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DiPiro JT, Talbert RL, Yee GC, et al. Columbus, OH: McGraw-Hill Companies, Inc.; 2005. Pharmacotherapy: A pathophysiologic approach. [Google Scholar]
- 21.Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism. The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(Suppl 3):338S–400S. doi: 10.1378/chest.126.3_suppl.338S. [DOI] [PubMed] [Google Scholar]
- 22.Sayal K, Duncan D, McConnell H, Taylor D. Psychotropic interactions with warfarin. Acta Psychiatrica Scandinavica. 2000;102:250–5. doi: 10.1034/j.1600-0447.2000.102004250.x. [DOI] [PubMed] [Google Scholar]