Abstract
Purpose:
To describe a case of choroidal neovascularization (CNV) in a female diagnosed with Beals–Hecht syndrome.
Methods:
A retrospective, interventional case is described in a 26-year-old female complaining of metamorphopsia and visual loss in her left eye (counting fingers). The fluorescein angiogram and the optical coherence tomography supported the diagnosis of CNV. Intravitreal ranibizumab was administered.
Results:
After the third intravitreal ranibizumab, her visual acuity improved to 0.8 and the morphology of the macular area was restored.
Conclusions:
To our knowledge this is the first report of CNV in Beals–Hecht syndrome treated with ranibizumab. Self-monitoring by periodically performing Amsler grid test is strongly recommended in these patients in order to achieve an early diagnosis of eventual CNV and avoid visual acuity loss.
Keywords: Beals–Hecht syndrome, connective tissue disease, choroidal neovascularization, ranibizumab
Introduction
Beals–Hecht syndrome is an autosomal dominantly inherited connective tissue disorder caused by a mutation in the fibrillin-2 gene (FBN2) in 5q23.1 Although the clinical features can be similar to Marfan syndrome, multiple joint contractures and crumpled ears in the absence of significant aortic root dilatation are characteristic of Beals syndrome and rarely found in Marfan syndrome.2 General ocular complications are estimated to be present in 20% of patients with Beals syndrome or congenital contractural arachnodactyly (CCA).3 Whereas ectopia lentis is very rare in Beals Syndrome, the typical ophthalmic features include blue sclera, axial myopia, cataract, lens coloboma, cilliary body hyoplasia, and glaucoma.3
Case report
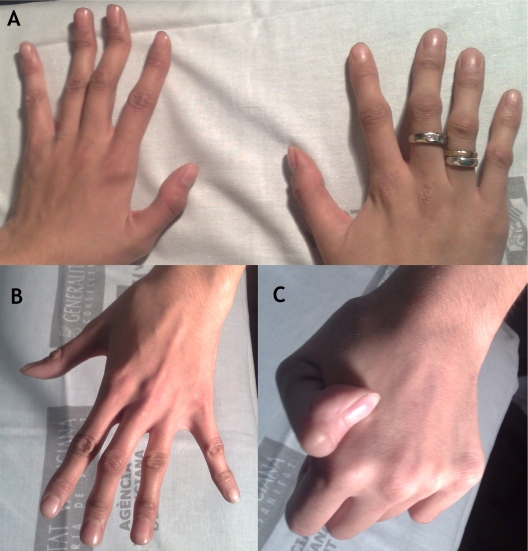
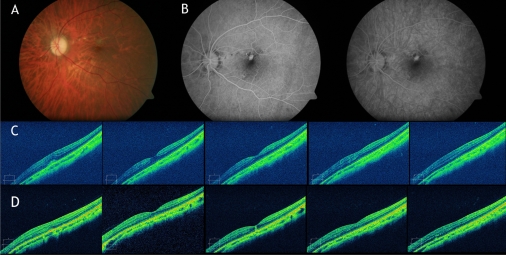
We describe a case of a 27-year-old woman who attended our Emergency Department complaining of sudden metamorphopsia and visual acuity (VA) loss in her left eye (LE). She referred a similar episode 4 years before presentation resulting in visual loss in her right eye (RE). Best-corrected visual acuity (BCVA) measured 0.16 RE and 0.4 LE. Systemic examination showed marfanoid habit, scoliosis, crumpled ears, and CCA (Figure 1). The patient had been recently diagnosed with Beals–Hecht syndrome after genetic testing. Ocular findings included axial myopia (axial length: 27,76 mm RE and 27,94 mm LE), blue sclera, and fundus examination showed a disciform-like scar RE and a juxtafoveal fibrovascular proliferation LE. Fluorescein angiography confirmed the presence of a predominantly classic choroidal neovascular membrane (CNV) LE, which induced intraretinal edema with foveal pit loss in the spectral-domain optical coherence tomography (Cirrus High-Definition OCT, Carl Zeiss Meditec, Dublin, CA, USA) images (Figure 2). With the formal diagnosis of a disciform maculopathy RE as described in Ehlers–Danlos disease,4 and CNV LE, the patient received three monthly intravitreal injections of ranibizumab (Lucentis, Genentech, South San Francisco, CA, USA). One month after the third injection the BCVA measured 0.8 LE and the OCT showed complete resolution of the retinal edema and normalization of the foveal anatomy (Figure 2). This outcome remained stable through an 8-months follow-up without further intravitreal retreatments.
Figure 1.
(A–C) Typical contractural aracnodactylia in Beals syndrome (A, B) and joint hypermobility (C).
Figure 2.
Fundus examination. A) Retinography showing disciform-like scar RE and juxtafoveal fibrovascular proliferation LE. B) Angiogram showing predominantly classic choroidal neovascular membrane (CNV). C) Spectral-domain optical coherence tomography (SD-OCT) images showing the subretinal choroidal neovascular membrane inducing loss of foveal anatomy. D) SD-OCT images showing complete resolution of the retinal edema and normalization of the foveal anatomy after three monthly intravitreal ranibizumab injections.
Discussion
To our knowledge this is the f irst report of CNV in Beals–Hecht syndrome treated with ranibizumab. Why this case is more likely to be due to the collagen disease rather than to axial myopia? On the one hand, the appearance of the RE disciform scar is unusual for myopic CNV, but it has been described in the context of Ehlers–Danlos disease, caused by collagen disorder;4 on the other hand, LE did not show a significant myopic choroidopathy and in addition lacquer crack lesions were only evidence between inferior vascular arcades but not within the posterior pole.
Ranibizumab has been widely used for myopic CNV with very good results, with fewer retreatments needed as compared to CNV due to age-related macular degeneration.5,6 In the case we report, the clinical and morphological response to intravitreal ranibizumab was excellent resulting in long-term normalization of the foveal contour and improvement in visual acuity.
From our point of view, as far as onset of metamorphopsia may be an initial symptom of CNV, self-monitoring by periodically performing Amsler grid test is strongly recommended in these patients in order to achieve an early diagnosis and avoid VA loss.
Footnotes
Disclosure
No conflicts of interest were declared in relation to this paper.
References
- 1.Robinson PN, Godfrey M. The molecular genetics of Marfan syndrome and related microfibrillopathies. J Med Genet. 2000;37:9–25. doi: 10.1136/jmg.37.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tunçbilek E, Alanay Y. Congenital contractural arachnodactyly (Beals syndrome) Orphanet J Rare Dis. 2006;1:20. doi: 10.1186/1750-1172-1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Takaesu-Miyagu S, Sakai H, Shiroma T, et al. Ocular findings of Beals syndrome. Jpn J Ophthalmol. 2004;48:470–474. doi: 10.1007/s10384-004-0106-7. [DOI] [PubMed] [Google Scholar]
- 4.Mishra RK, Goel IB. Disciform macular degeneration associated with Ehlers-Danlos Syndrome. (Cutis Hyperelastica) J All India Ophthalmol Soc. 1963;11:87–95. [PubMed] [Google Scholar]
- 5.Lalloum F, Souied EH, Bastuji-Garin S, et al. Intravitreal ranibizumab for choroidal neovascularization complicating pathologic myopia. Retina. 2010;30:399–406. doi: 10.1097/IAE.0b013e3181bcef24. [DOI] [PubMed] [Google Scholar]
- 6.Konstantinidis L, Mantel I, Pournaras JA, et al. Intravitreal ranibizumab (Lucentis) for the treatment of myopic choroidal neovascularization. Graefes Arch Clin Exp Ophthalmol. 2009;247:311–318. doi: 10.1007/s00417-008-0995-0. [DOI] [PubMed] [Google Scholar]