Abstract
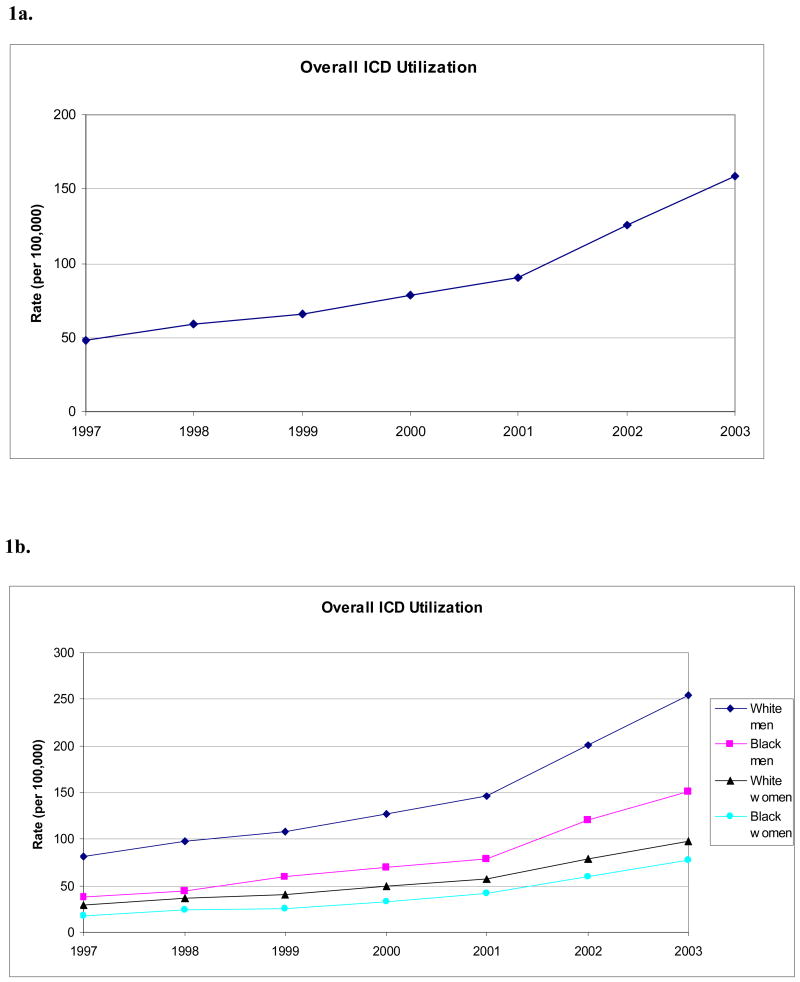
Differences in the use of implantable cardioverter-defibrillators (ICDs) have been reported, but the extent to which they have widened after the publication of major clinical trials supporting their use is unclear. Using data on Medicare beneficiaries, we determined annual age-standardized population-based utilization rates of ICDs for white men, black men, white women, and black women from 1997 to 2003. During the study period, overall use of ICDs increased most for white men (81.7 to 254.7 procedures per 100,000 from 1997 to 2003) and black men (38.0 to 151.7 procedures per 100,000), with white women (28.9 to 98.4 procedures per 100,000) and black women (18.2 to 77.3 procedures per 100,000) showing smaller increases in comparison. After adjustment with multivariable regression models, differences in utilization rates between whites and men widened compared to blacks and women between 1997 and 2003, a period when indications for ICD therapy have expanded.
Background
Clinical indications for implantable cardioverter-defibrillators (ICDs) have expanded rapidly in the past decade. Randomized clinical trials have found that ICDs reduce mortality in patients with documented ventricular arrhythmias and in those with left ventricular dysfunction who are at high-risk for sudden cardiac death.1-6 In addition, ICDs have also demonstrated improvements in clinical outcomes in real-world populations,7, 8 suggesting favorable cost-effectiveness ratios when compared with standard medical therapy.9, 10 Despite these findings, there is some evidence that ICDs remain under-utilized among eligible patients due to their high upfront costs and limited resources.11
Prior studies have documented racial and gender differences in the use of medical and surgical procedures, including ICDs.12-15 Most of these reports suggest under-use and disparities in care for vulnerable populations, including blacks and women, when compared with whites and men.16-19 What remains unclear, however, is the extent to which these differences have been exacerbated by expanding indications for procedures whose optimal roles in care are still evolving. If newer procedures disseminate more slowly among blacks and women, it would argue for the development of specific strategies for ensuring that emerging and innovative evidence is appropriately translated to vulnerable populations.
Accordingly, we examined changes in racial and gender differences in population-based rates of utilization for ICDs among Medicare beneficiaries between 1997 and 2003, a time frame that encompassed the publication of several landmark randomized clinical trials supporting their use. Examining the use of ICDs in Medicare beneficiaries over this time period represents an ideal opportunity to evaluate how expanding indications for newer procedures may affect racial and gender differences in utilization given that the majority of recipients of ICDs in the U.S. are 65 years or older, which allows for near complete capture of their utilization within this national data source.
Methods
Data Sources and Study Population
For these analyses, Medicare Provider and Analysis Review (MEDPAR) Part A, Denominator, and Provider-of-Service (POS) files from 1997 through 2003 were obtained from the Centers for Medicare & Medicaid Services (CMS). Part A files include data on acute-care hospitalizations. Denominator files contain data on eligible Medicare beneficiaries for that year, including demographic and enrollment information. POS files contain data on hospital providers, including facility characteristics and Zip code locations. Data on all Medicare beneficiaries age 65 years or older enrolled in fee-for-service programs within the U.S. were included. To be consistent with prior literature on racial differences in the Medicare population, we excluded the non-black, non-white population (9.6% of the overall study population). After these exclusions, the average study cohort size annually was 26.6 million enrollees, of which 25.3 million (95%) had both Part A and Part B coverage. No substantial changes in the distribution of the population by race or gender were seen during this study period.
We used the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedural codes to identify patients undergoing ICD implantation with or without pacemaker capability (ICD-9-CM procedure codes 37.94-37.96) from 1997 to 2003. For the purposes of a secondary analysis, we also categorized ICD implantation as being performed for primary or secondary prevention. We considered an ICD to be placed for secondary prevention if a patient had an inpatient hospitalization for ventricular arrhythmia (ICD-9 diagnosis codes 427.1 and 427.41) or cardiac arrest (ICD-9 diagnosis code 427.5) within the prior year and did not have a concurrent myocardial infarction (ICD-9 diagnosis code 410.x) during the index arrhythmic event. ICDs that did not meet criteria for secondary prevention were categorized as being performed for primary prevention.
To contrast differences in utilization rates of ICDs with general trends in racial and gender differences in procedural utilization during this time period, we also analyzed data on patients undergoing pacemaker implantation (ICD-9-CM procedure codes 00.50, 00.53, 37.70-37.72, and 37.80-37.83) including single and dual-chamber devices. These patients represent an ideal comparison group for several reasons. First, unlike with ICDs, no randomized clinical trials were published during this time period that would have rapidly expanded indications for these devices. Moreover, pacemaker implantation is frequently performed by physicians also responsible for placing an ICD, thereby representing a reasonable proxy for temporal changes in access to these procedures. The Institutional Review Board of the University of Michigan and the Centers for Medicare and Medicaid Services (CMS) approved this protocol prior to its initiation.
Statistical Analyses
We calculated population-based rates of utilization for ICDs and pacemakers in white men, black men, white women, and black women between 1997 and 2003 in the United States. The numerator for these rates was the total number of patients in each racial and gender category that underwent the procedure in that calendar year. The denominator for these rates was the total number of eligible Medicare beneficiaries in each racial and gender category enrolled in the mid-point of that calendar year. All rates were adjusted for differences in age (65 to 69 years, 70 to 74 years, 75 to 79 years, 80 to 84 years, and 85 years and over) across years using direct standardization techniques with the total beneficiary population for the entire study period as the standard population.20 Rates for ICDs used in secondary prevention were further adjusted for annual rates of qualifying ventricular arrhythmias and cardiac arrest, with rates among white men in each age stratum as the referent.
We visually examined trends in ICD use between 1997 and 2003, and qualitatively assessed whether racial and gender differences increased, decreased or remained the same over time. To test for statistically significant changes in racial and gender differences over time, we constructed a series of linear regression models with white men as the primary reference group. Differences in population-based rates between white men and the other 3 racial and gender categories were the dependent variables in these separate models, with year (i.e., independent variable) included as a continuous variable. As a result, the regression coefficient for the variable year in the models represented mean annual increases or decreases from baseline differences in utilization. We also evaluated quadratic and cubic values of the variable year in our regression models but did not find that the inclusion of these exponential terms changed our results (results not reported). In addition, we separately compared rates for black men with black women and white women with black women.
In a secondary analysis, we determined population-based rates of utilization for ICDs separately among patients identified as undergoing placement for primary and secondary prevention. We constructed similar linear regression models to those described above. For all analyses, the null hypothesis was evaluated at a two-sided significance level of 0.05. All analyses were performed with SAS 9.1 (SAS Institute, Cary, NC).
Results
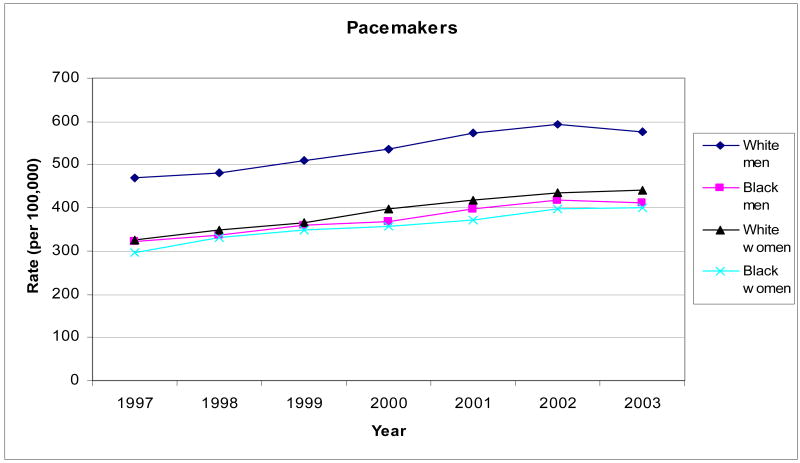
From 1997 through 2003, age-standardized, population-based rates of ICD use in the Medicare population increased from 48.3 procedures per 100,000 to 158.9 procedures per 100,000. This increase did not occur linearly: rates increased by 10.5 procedures per 100,000 per year from 1997 to 2001 and then increased by 29.3 procedures per 100,000 per year from 2001 to 2003 (Figure 1). In contrast, age-standardized, population-based rates of utilization for pacemakers in the Medicare population showed a more gradual increase from 372.6 procedures per 100,000 in 1997 to 495.2 procedures per 100,000 in 2003, an average increase of 5% per year (Figure 2).
Figure 1. Age-Adjusted National Rates of Overall Defibrillator Implantation (1a) and By Race and Gender Groups (1b) Among Medicare Enrollees, 1997 through 2003.
Figure 2. Age-Adjusted National Rates of Pacemaker Implantation Among Medicare Enrollees, 1997 through 2003.
Population-Based Utilization By Race and Gender
During the study period, overall rates of ICD use increased most for white men (81.7 procedures per 100,000 in 1997 to 254.7 procedures per 100,000 in 2003) and black men (38.0 to 151.7 procedures per 100,000), with white women (28.9 to 98.4 procedures per 100,000) and black women (18.2 to 77.3 procedures per 100,000) showing smaller increases in comparison (Table 1; Figure 1). Compared with white men, a significant widening of existing differences in utilization rates were seen from 1997 to 2003 across the other 3 racial and gender categories (Table 2). The difference in utilization rates for white men as compared with black men widened on average by +9.0 procedures per 100,000 per year over the study period or a relative increase of 21% annually (p=0.002).
Table I. Rates of ICD Procedures in Medicare Enrollees, 1997 and 2003*.
| 1997 | 2003 | Change | |
|---|---|---|---|
| OVERALL | |||
| White Men | 81.7 | 254.7 | 173.0 |
| Black Men | 38.0 | 151.7 | 113.7 |
| White Women | 28.9 | 98.4 | 69.5 |
| Black Women | 18.2 | 77.3 | 59.1 |
| PRIMARY PREVENTION | |||
| White Men | 10.4 | 56.9 | 46.5 |
| Black Men | 5.5 | 34.3 | 28.8 |
| White Women | 1.9 | 12.4 | 10.5 |
| Black Women | 1.2 | 13.7 | 12.5 |
| SECONDARY PREVENTION | |||
| White Men | 71.3 | 197.8 | 126.5 |
| Black Men | 32.5 | 117.4 | 84.9 |
| White Women | 27.0 | 86.0 | 59.0 |
| Black Women | 17.0 | 63.6 | 46.6 |
Rates are per 100,000 enrollees.
Table II. Widening of Baseline Differences in ICD Utilization Between Racial and Gender Subgroups.
| OVERALL ICDs | Baseline Utilization Difference * | Annual Change from Baseline Gap** |
|---|---|---|
| White Men | Reference | Reference |
| Black Men | 43.7 | 9.0 (21%) † |
| White Women | 52.8 | 16.3 (31%) † |
| Black Women | 63.5 | 17.8 (28%) † |
| White Women | Reference | Reference |
| Black Women | 10.7 | 1.6 (15%) † |
| Black Men | Reference | Reference |
| Black Women | 19.8 | 8.8 (44%) † |
| PRIMARY PREVENTION | Baseline Utilization Difference* | Annual Change from Baseline Gap** |
| White Men | Reference | Reference |
| Black Men | 4.9 | 2.2 (45%)† |
| White Women | 8.5 | 4.7 (55%) † |
| Black Women | 9.2 | 4.5 (49%) † |
| White Women | Reference | Reference |
| Black Women | 0.7 | -0.3 (-43%)† |
| Black Men | Reference | Reference |
| Black Women | 4.3 | 2.2 (51%)† |
| SECONDARY PREVENTION | Baseline Utilization Difference* | Annual Change from Baseline Gap** |
| White Men | Reference | Reference |
| Black Men | 38.8 | 6.8 (18%) † |
| White Women | 44.3 | 11.5 (26%) † |
| Black Women | 54.3 | 13.4 (25%) † |
| White Women | Reference | Reference |
| Black Women | 10.0 | 1.8 (18%) † |
| Black Men | Reference | Reference |
| Black Women | 15.5 | 6.6 (43%) † |
Rates are per 100,000
Rates represent the annual absolute (and relative, in %) change per 100,000 from the baseline difference in ICD utilization between the compared groups.
P for trend <0.05 in linear regression models.
Similar but more pronounced effects were seen when white men were compared with white women (difference, +16.3 procedures per 100,000 per year or a relative increase of 31% annually; p=0.002) and black women (difference, +17.8 procedures per 100,000 per year or a relative increase of 28% annually; p=0.001). Moreover, the existing difference in utilization rates for black men as compared with black women widened on average by +8.8 procedures per 100,000 per year or a relative increase of 44% annually (p=0.001) whereas the difference for white women as compared with black women widened by +1.6 procedures per 100,000 per year or a relative increase of 15% annually (p=0.001).
No significant widening or narrowing in differences for pacemaker utilization were noted among the 4 race and gender categories throughout the study period, with each group achieving similar absolute utilization rate gains over time (Figure 2).
Population-Based Utilization By Indication
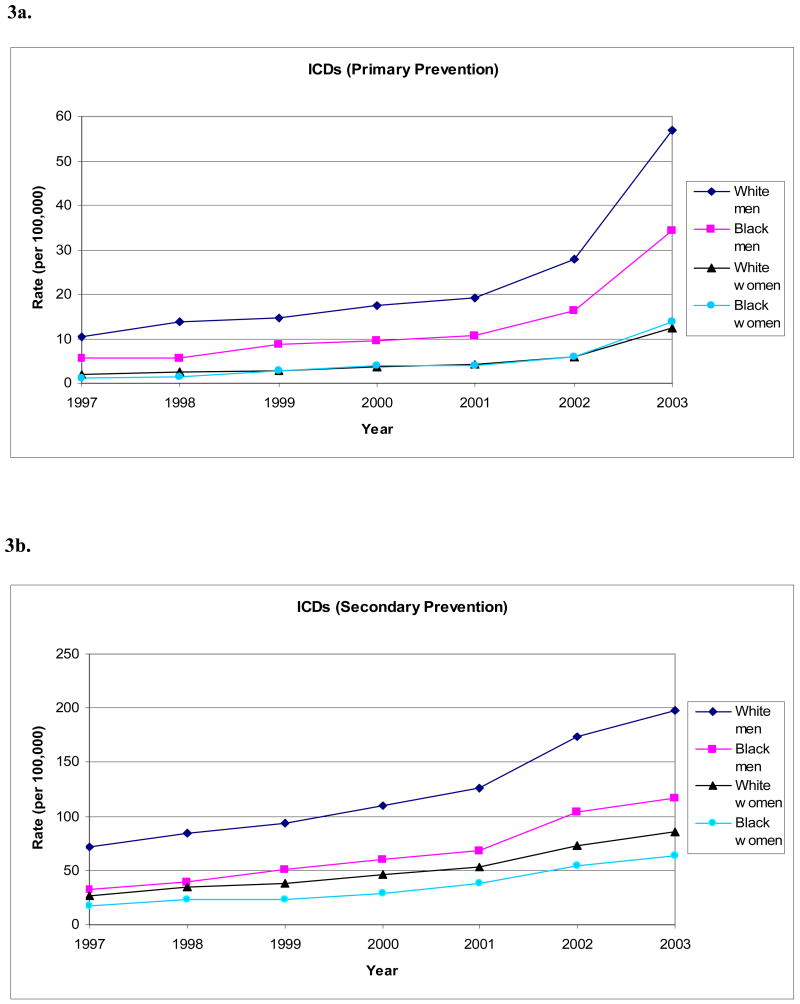
For ICDs implanted for primary prevention, rates of utilization over time increased most for white men (10.4 procedures per 100,000 in 1997 to 56.9 procedures per 100,000 in 2003) and black men (5.5 to 34.3 procedures per 100,000), with women showing smaller increases (Table 1; Figure 3). In addition, the rate of increase was linear from 1997 to 2001 for all 4 groups but then rose sharply in 2002, coincident with the publication of the Second Multicenter Automated Defibrillator Implantation Trial (MADIT-II). Existing differences in rates of ICD use widened between white men and the other 3 racial and gender categories during the study period (Table 2).
Figure 3. Age-Adjusted National Rates of Defibrillator Implantation for Primary Prevention (1a) and Secondary Prevention (1b) Among Medicare Enrollees, 1997 through 2003.
Similar trends were generally noted for ICDs implanted for secondary prevention. Rates of utilization over time increased most for white men (71.3 to 197.8 procedures per 100,000) and black men (32.5 to 117.4 procedures per 100,000), with women showing smaller increases (Table 1; Figure 3). In contrast to rates associated with primary prevention, changes over time were, in large part, linear for all 4 groups. Still, a significant widening in the existing differences in ICD utilization rates were seen across each race and gender category when compared with white men during this time period (Table 2).
Discussion
We found that rates of ICD use not only differed by race and gender, but that such differences widened from 1997 to 2003, a time period that was characterized by the publication of several landmark randomized clinical trials related to their use. The widening was most notable for ICDs implanted for primary prevention and grew most markedly after publication of the MADIT-II trial in 2002 when indications and reimbursement for primary prevention were expanded. In contrast, we found no increases in the existing differences of pacemaker use during this time period. Our findings highlight that there is a potential for disparities in the utilization of newer procedures like ICDs to widen among vulnerable populations as indications for their use expand.
Although prior studies have shown that blacks are less likely to receive an ICD for secondary prevention11, 17, 21, 22, no prior reports have examined whether differences in use have widened or narrowed over time. In addition, earlier studies focused on relative differences in the use of ICDs.11, 17, 21, 22 In contrast, we examined absolute differences in rates of utilization. Absolute differences provide a better measure of the total number of at-risk Medicare beneficiaries who may benefit from the narrowing or elimination of racial or gender differences in procedural utilization. This is because trends in absolute differences have a consistent interpretation, regardless of whether the primary outcome is receipt or non-receipt of therapy.15 For instance, if adherence to an effective medication increases from 2 percent to 80 percent among whites but only from 1 percent to 60 percent among blacks, this would represent a significant 19 percent absolute increase in adherence but a paradoxical relative decrease (from 2.0 to 1.3). Conversely, if non-adherence was the outcome measured instead of adherence, the absolute difference (in this case, decrease in non-adherence) would remain at 19 percent and there would instead be a relative decrease in non-adherence from 1.0 to 0.5. Therefore, from a policy perspective, absolute differences provide a more informative and consistent assessment of disparities in resource utilization across populations. In this study, we found that although rates of utilization for ICDs increased over time for blacks and women, these increases did not reduce baseline racial and gender gaps because the corresponding rates for whites and men increased even faster. Prior research evaluating absolute differences in the use of medical therapies have similarly argued that this approach may provide a more useful benchmark for policy-makers interested in addressing racial and gender disparities15 and therefore highlights the need to examine both relative and absolute differences in the utilization of effective therapies.
The reasons for observed racial and gender differences in utilization rates of effective therapies likely reflect complex interactions between patients, providers, healthcare markets, and geographic factors. It is possible that differences may be attributable to the “overuse” of ICDs in whites and men. It may also be that “underuse” in blacks and women is largely responsible for these differences.16, 18, 19 Our analysis is unfortunately unable to differentiate between these 2 possibilities. Prior evidence does suggest that patient preferences and cultural norms for particular therapies can be a significant determinant for procedural utilization and may be partly responsible for these differences across various racial and ethnic groups.23 There may also be differences in the intensity and frequency with which physicians engage patients in the decision-making process, which may influence patient acceptance of ICD therapy. Although a patient's ability to pay may affect whether therapy is offered by a physician, this is unlikely to be an explanation for our observed racial differences, as our study population was an insured Medicare population where the vast majority (95%) had both Part A and Part B coverage. Lastly, geographic variation in access to care may affect which patient subgroups will likely receive state-of-the-art therapies, although one would not expect geography to have a significant impact on gender differences in utilization. The fact that we also demonstrated no significant change in differences in utilization rates for pacemakers during the study period suggests access to care may be less likely to explain our results.
Although racial differences in utilization of invasive treatments have been documented widely throughout the cardiovascular literature, gender differences in their use have been less well studied. Because we did not have patient-level data on rates of ischemic heart disease and left ventricular dysfunction in the population, and because men have higher rates of ischemic heart disease than age-matched women, differences in disease severity and clinical indications certainly explain a portion of the gender differences observed in the use of ICDs for primary prevention. However, significant gender differences and widening of such differences were similarly observed in the utilization of ICDs for secondary prevention, even after controlling for population-based rates of incident qualifying ventricular arrhythmias for an ICD. Therefore, further studies are needed to determine factors related to underuse of ICDs in women.
An important aspect of our study was the separation of patients into those undergoing ICD placement for primary and secondary prevention. At the beginning of our study period, clinical trials such as the Amiodarone Versus Implantable Defibrillator (AVID) trial established the mortality benefit of ICDs in secondary prevention for patients with documented ventricular arrhythmias.5 Rates of ICD use for secondary prevention therefore increased for each racial and gender group annually during our study period, although disproportionately so for whites and men. This accounted for the widening of existing differences noted over time in this population. In contrast, the use of ICDs for primary prevention was limited until 2002 and overall population-based rates of utilization remained low. After the publication of the MADIT-II trial, however, use of ICDs rose in this population also with a similar widening in existing differences across racial and gender categories.
As the Institute of Medicine and healthcare policy-makers focus on eliminating or narrowing racial and gender disparities in healthcare outcomes, it is important to recognize that appropriately translating findings from emerging and innovative therapies to vulnerable populations remains a real challenge. Our study supports the hypothesis that the benefits of expanding indications for evolving technologies, like ICDs, are not equitably distributed among blacks and women. Although there has been concerted effort to improve recruitment of these patients in contemporary clinical trials, future studies may be needed to identify strategies for ensuring that this evidence is evenly disseminated.
Our study should be interpreted in the context of the following limitations. We did not assess ICD utilization in patients under 65 years of age. Because the majority of ICD recipients are Medicare eligible, it is unlikely that inclusion of these patients would have significantly affected our results. We also did not have clinical information on left ventricular ejection fraction or the precise indication for receiving an ICD. As a result, our estimates of utilization rates for primary and secondary prevention, which were secondary analyses in this study, may contain misclassification bias and should be interpreted with these considerations in mind. Moreover, differential indications may explain some of the observed differences in our study, although it is unlikely that the prevalence of the underlying indications for ICDs in different racial and gender groups would have changed over our period of observation. Therefore, widening differences in the rates of procedure use over time suggest there is differential penetration of new knowledge or differential intensity of recommendation of ICD therapy to disadvantaged populations, including black patients and women. As mentioned previously, our study is unable to establish what the “right” utilization rate for ICDs should be. Therefore, we are unable to know whether observed differences were due to overuse, underuse, or both. Regardless, differences in utilization rates across race and gender are important considerations for policy-makers.
Conclusion
We found that baseline rates of ICD utilization differed by race and gender, and that these differences widened from 1997 to 2003 as the indications for these procedures expanded. Our study raises questions about the potential for disparities in newer procedures to worsen as the benefits of landmark randomized clinical trials are translated into routine clinical practice. Accordingly, more research into the dissemination of new knowledge into practice is needed if the Institute of Medicine's goal for a more equitable healthcare system is to be realized.
Acknowledgments
Funding Sources
Dr. Chan completed part of this work while supported by an NIH Cardiovascular Multidisciplinary Research Training Grant and by the Ruth L. Kirchstein Research Service Award. Dr. Nallamothu completed part of this work while supported as a clinical scholar under a K12 grant from the National Institutes of Health (RR017607-01). Neither funding agency had any involvement in the design, collection, management, or analysis of the study or in manuscript preparation.
Footnotes
Financial Disclosures:
Dr. Paul Chan None
Dr. John Birkmeyer None
Dr. Harlan Krumholz None
Dr. John Spertus None
Dr. Brahmajee Nallamothu None
Disclaimer: The content of this publication does not necessarily reflect the views or policies of the Centers for Medicare and Medicaid Services, the Department of Health and Human Services or the Department of Veterans Affairs, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. The authors assume full responsibility for the accuracy and completeness of the ideas presented.
References
- 1.Moss AJ, Hall WJ, Cannom DS, et al. Improved Survival with an Implanted Defibrillator in Patients with Coronary Disease at High Risk for Ventricular Arrhythmia. N Engl J Med. 1996;335:1933–1940. doi: 10.1056/NEJM199612263352601. [DOI] [PubMed] [Google Scholar]
- 2.Moss AJ, Z W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction. 2002:870–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 3.Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 4.Buxton AE, Lee KL, Fisher JD, et al. A Randomized Study of the Prevention of Sudden Death in Patients with Coronary Artery Disease. N Engl J Med. 1999;341:1882–1890. doi: 10.1056/NEJM199912163412503. [DOI] [PubMed] [Google Scholar]
- 5.A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. N Engl J Med. 1997;337:1576–1583. doi: 10.1056/NEJM199711273372202. [DOI] [PubMed] [Google Scholar]
- 6.Connolly SJ, Gent M, Roberts RS, et al. Canadian implantable defibrillator study (CIDS) : a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation. 2000;101:1297–1302. doi: 10.1161/01.cir.101.11.1297. [DOI] [PubMed] [Google Scholar]
- 7.Chan PS, Chow T, Kereiakes D, et al. Effectiveness of implantable cardioverter-defibrillators in patients with ischemic heart disease and left ventricular dysfunction. Arch Intern Med. 2006;166:2228–2233. doi: 10.1001/archinte.166.20.2228. [DOI] [PubMed] [Google Scholar]
- 8.Chan PS, Hayward RA. Mortality reduction by implantable cardioverter-defibrillators in high-risk patients with heart failure, ischemic heart disease, and new-onset ventricular arrhythmia: an effectiveness study. J Am Coll Cardiol. 2005;45:1474–1481. doi: 10.1016/j.jacc.2005.01.031. [DOI] [PubMed] [Google Scholar]
- 9.Sanders GD, Hlatky MA, Owens DK. Cost-effectiveness of implantable cardioverter-defibrillators. N Engl J Med. 2005;353:1471–1480. doi: 10.1056/NEJMsa051989. [DOI] [PubMed] [Google Scholar]
- 10.Al-Khatib SM, Anstrom KJ, Eisenstein EL, et al. Clinical and economic implications of the multicenter automatic defibrillator implantation trial-II. Ann Intern Med. 2005;142:593–600. doi: 10.7326/0003-4819-142-8-200504190-00007. [DOI] [PubMed] [Google Scholar]
- 11.Voigt A, Ezzeddine R, Barrington W, et al. Utilization of implantable cardioverter-defibrillators in survivors of cardiac arrest in the United States from 1996 to 2001. J Am Coll Cardiol. 2004;44:855–858. doi: 10.1016/j.jacc.2004.05.053. [DOI] [PubMed] [Google Scholar]
- 12.Escarce JJ, Epstein KR, Colby DC, et al. Racial differences in the elderly's use of medical procedures and diagnostic tests. Am J Public Health. 1993;83:948–954. doi: 10.2105/ajph.83.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vaccarino V, Rathore SS, Wenger NK, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–682. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kressin NR, Petersen LA. Racial differences in the use of invasive cardiovascular procedures: review of the literature and prescription for future research. Ann Intern Med. 2001;135:352–366. doi: 10.7326/0003-4819-135-5-200109040-00012. [DOI] [PubMed] [Google Scholar]
- 15.Jha AK, Fisher ES, Li Z, et al. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353:683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 16.Schneider EC, Leape LL, Weissman JS, et al. Racial differences in cardiac revascularization rates: does “overuse” explain higher rates among white patients? Ann Intern Med. 2001;135:328–337. doi: 10.7326/0003-4819-135-5-200109040-00009. [DOI] [PubMed] [Google Scholar]
- 17.Gauri AJ, Davis A, Hong T, et al. Disparities in the use of primary prevention and defibrillator therapy among blacks and women. Am J Med. 2006;119:e17–21. doi: 10.1016/j.amjmed.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 18.Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation--clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343:1537–1544. doi: 10.1056/NEJM200011233432106. 1532 p preceding 1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Canto JG, Allison JJ, Kiefe CI, et al. Relation of race and sex to the use of reperfusion therapy in Medicare beneficiaries with acute myocardial infarction. N Engl J Med. 2000;342:1094–1100. doi: 10.1056/NEJM200004133421505. [DOI] [PubMed] [Google Scholar]
- 20.Rothman K, Greenland S. Modern Epidemiology. 2nd. Philadelphia, PA: Lippincott-Raven Publishers; 1998. pp. 260–262. [Google Scholar]
- 21.Groeneveld PW, Heidenreich PA, Garber AM. Trends in implantable cardioverter-defibrillator racial disparity: the importance of geography. J Am Coll Cardiol. 2005;45:72–78. doi: 10.1016/j.jacc.2004.07.061. [DOI] [PubMed] [Google Scholar]
- 22.Hernandez AF, Fonarow GC, Liang L, et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. Jama. 2007;298:1525–1532. doi: 10.1001/jama.298.13.1525. [DOI] [PubMed] [Google Scholar]
- 23.Rathore SS, Krumholz HM. Differences, disparities, and biases: clarifying racial variations in health care use. Ann Intern Med. 2004;141:635–638. doi: 10.7326/0003-4819-141-8-200410190-00011. [DOI] [PubMed] [Google Scholar]