Abstract
Migration and embolization of the Amplatzer septal occluder (ASO) have been reported. However, there is only limited information on the methods of systematic retrieval of these devices. In this report, we describe the a case of a 4 year old girl who underwent closure of her atrial septal defect (ASD) using a 17 mm ASO. The device migrated in to the right atrium an anteroposterior plane 24 hours later with a resultant residual shunt. The device was successfully retrieved percutaneously and the ASD was closed using a 20 mm ASO.
Keywords: Atrial septal defect, bioptome, device embolization, goose neck snare
INTRODUCTION
Over the last few years, device closure of secundum ASD is being performed safely and effectively with high success rates in a selected group of patients. However, even in experienced hands, device embolization may occur as an uncommon yet serious complication. We describe a case of device migration which was treated successfully in the catheterization laboratory.
CASE REPORT
A four-year old girl, weighing 9 kg, presented with repeated lower respiratory tract infections and severe failure to thrive. Clinical examination revealed normal vital parameters with a 3/6 ejection systolic murmur in the pulmonary area. The splitting of the second heart sound was wide and fixed. The respiratory system examination was unremarkable. Her ECG revealed sinus a rhythm with QRS axis of +100 degrees. There was rsR' in lead V1. X-ray showed a cardiothoracic ratio of 55% with prominent pulmonary artery shadow. The lung fields were plethoric. Transthoracic echo (TTE) revealed a moderately large sized secundum ASD, measuring 15 mm, with adequate rims (> 5 mm) except the aortic rim which was almost absent. The ASD size was measured on 2D echo, without the use of color flow mapping. There was left superior vena cava (SVC) draining into the coronary sinus, which was dilated.
The child was taken for transcatheter closure under general anesthesia, with fluoroscopic and transesophageal echocardiographic (TEE) guidance. TEE confirmed the presence of a moderately large secundum ASD [Figure 1a] measuring 14 mm and having adequate rims all around, except the aortic rim, which was deficient. It was decided to close the defect using a 17 mm ASO (AGA Medical Corp., Plymouth, MN). The defect was not balloon-sized. The ASD was closed successfully using the routine technique of device closure.[1] The position of the device was found to be optimum and secured on TEE [Figure 1b] and fluoroscopy [Figure 2a and b] after the final release. Twenty-four hours later, prior to discharge, the child was subjected to a check TTE , as a part of a routine protocol. The device had moved from its previous position [Figure 1c] with a residual shunt seen superior and anterior to the device. This was confirmed on fluoroscopy [Figure 2c]. In view of the unstable position of the device with an evidence of a residual shunt, it was decided to attempt percutaneous retrieval.
Figure 1.
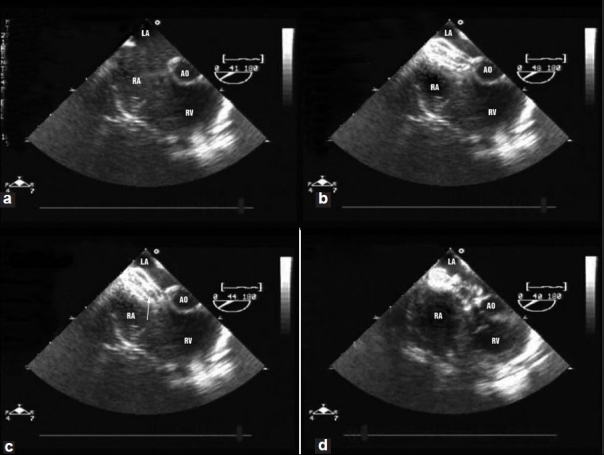
Transesophageal echo in the short axis view of the aorta (a) showing a large secundum atrial septal defect (b) Successful closure of the defect using 17 mm Amplatzer septal occluder (c) Migration of the device 24 hours later at the aortic end in the anteroposterior plane. The migrated device was successfully retrieved percutaneously, (d) Successful deployment of the 20 mm Amplatzer septal occluder
Figure 2.
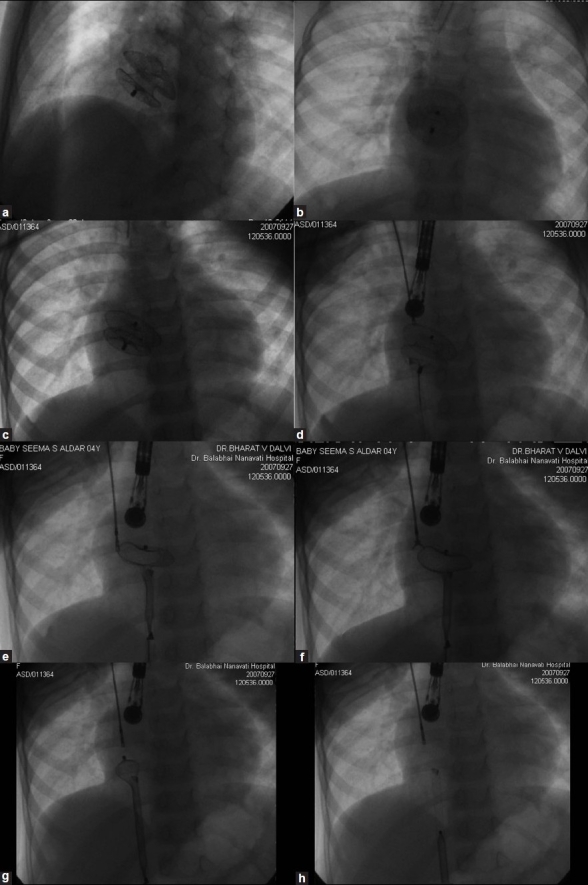
Fluroscopic images immediately after deployment, showing the normal position of the device (a) in left anterior oblique projection with cranial angulation and (b) posteroanterior projection. Fluroscopic image 24 hours later showing (c) migrated device (d) held by a bioptome from the right jugular vein and a snare from the right femoral vein (e) Right atrial disk being pulled into the 10F sheath, with left atrial disk still held by the bioptome. (f) Bioptome is opened to release the left atrial disk. (g) The left atrial disk being pulled into the sheath. (h) The entire device is slenderized and brought into the sheath
The procedure was done under general anesthesia. The right jugular vein was cannulated using a 5F hemaquit. A 10F straight long sheath, (Cook Medical Inc, Bloomington, IN), beveled at the distal end, was passed from the right femoral vein and Heparin 100 i.u/Kg was injected. Although the device was not free floating, a 5F bioptome (Cook Medical Inc., Bloomington, IN) introduced from the right jugular vein was used to stabilize the device [Figure 2d]. An Amplatz goose neck snare (eV3 Endovascular Inc., Plymouth, MN) with a 15 mm diameter was introduced from the right femoral vein via the 10F sheath through a 0.038” tracker catheter, provided with the snare itself, and the device was held by its screw located on the right atrial disk [Figure 2d]. Once the device was held at both the ends, the Amplatz goose neck snare was pulled with a constant pressure without any jerky movements. With a pull of gradually increasing intensity on the snare, accompanied by a gentle tension on the bioptome holding the LA disk, it was possible to slenderize the right atrial disk and retrieve it in the long sheath [Figure 2e]. At this juncture, the bioptome was opened and the left atrial disk was released [Figure 2f]. The entire device was subsequently pulled into the sheath [Figure 2g]. It was then decided to balloon size the defect and proceed with the device closure. Balloon sizing revealed the stretched balloon diameter of the ASD to be 20 mm. Hence, a 20 mm ASO was used and the device was successfully deployed [Figure 1d], using the balloon-assisted technique.[2] This technique is routinely used for closing all large ASDs in our laboratory. The child was discharged 24 hours later on aspirin (5 mg/kg/day) with the check echo showing an optimally placed ASO. On follow-up at six weeks, the device was stable with no residual shunt. The right ventricular volume had reduced significantly and the biventricular contractility was normal. The surrounding vital structures were functioning normally and there was no evidence of pericardial effusion or thrombus on the device.
DISCUSSION
The common causes of embolization are undersizing of the device, inadequacy of the rims of ASD, inadvertent improper deployment, overzealous 'Minnesota wiggle', excessive tension on the loading cable during release, and vigorous Valsalva maneuver.[3] In the present case, undersizing seems to be the most likely cause, as balloon sizing revealed the defect to be 20 mm. The other above-mentioned factors responsible for embolization were absent in this child. Additionally, the patient had left SVC with a dilated coronary sinus. It is possible that the dilated coronary sinus may have come in the way of adequate device anchoring. However, this purely remains a conjecture. We do not have a definite policy regarding sizing of the ASD. We mainly size the defect in those cases where the ASD is large, malaligned or has a very floppy rim. These criteria are subjective and the decision to size or not is made only after a thorough evaluation of the defect on TEE. This isolated incident has not prompted us to change our policy regarding balloon sizing of the defect.
The incidence of device embolization is reported to be about 0.5% in experienced hands, with successful percutaneous retrieval being reported in approximately 70% of the cases.[3] In the present case, the child remained asymptomatic despite embolization, which was detected incidentally.
Although, most of the embolized devices need to be retrieved, occasionally it may be possible to reposition them by pulling the right atrial disk into the right atrium with a snare.[4] In our case, the device had already migrated into the right atrium and therefore no attempt was made to reposition the device with a snare.
Stabilizing the device is crucial to retrieving it. Hence, we used a bioptome to hold on to the left atrial disk. This prevented the migration of the device and subsequently also helped in slenderizing it. Some authors have reported the use of a stiff guidewire, which is passed across the mesh of the device for stabilization.[4] We used a 10F long sheath to retrieve a 17 mm device. This was 2F bigger than the recommended sheath size for deployment. A bigger sheath allows more easy entry of the device into the sheath as compared to the one with the best fit.[3] The Cook sheath was used, as it was more stiff and therefore less likely to kink. The tip of the sheath was beveled so as to increase its surface area, which made it easier for the device to get into the sheath. The cut margin of the sheath was smoothened to make it as atraumatic as possible. This type of preshaping of the sheath has been recently reported as being useful for both deployment and retrieval.[5]
Once the device was stablized, the Amplatz gooseneck snare was used to hold the screw on the right atrial disk. Although, a bioptome or a crocodile clip could also be used to grip the screw, we were more familiar with the use of the gooseneck snare, and it appeared to hold the screw very firmly, especially at the time of bringing the device back into the sheath. The left atrial disk was released only when the entire right atrial disk and the waist of the device were inside the long sheath. Although this was our first retrieval, we feel that unless the device is held at both the ends, slenderizing it would be extremely difficult. This is because the screw on the right atrial disk can never be expected to perfectly align with the sheath. Thus, if one pulls only at one end, there is a chance that the screw might slip out of the snare or the delivery sheath might get kinked.
Although not applicable in this case, some of the other basic principles of percutaneous retrieval include, (i) protecting the device with a sheath rather than pulling it bare. This prevents injury to the valves, cardiac chambers and blood vessels, especially when retrieving large devices in smaller children, and (ii) not retrieving the devices from the ventricles across the atrioventricular valves. It is always safer to retrieve them from the aorta or the pulmonary artery.
In conclusion, although embolization of ASO is rare there is a finite incidence even in experienced hands. Therefore, all centers doing transcatheter closure of ASD using ASO should be prepared to undertake retrieval, ensuring availability of the hardware. The ASO can be safely retrieved by following certain principles, as has been documented in this case.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Masura J, Gavora P, Formanek A, Hijazi ZM. Transcatheter closure of secundum atrial septal defects using the new self-centering amplatzer septal occluder: Initial human experience. Cathet Cardiovasc Diagn. 1997;42:388–93. doi: 10.1002/(sici)1097-0304(199712)42:4<388::aid-ccd7>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 2.Dalvi BV, Pinto RJ, Gupta A. New technique for device closure of large atrial septal defects. Catheter Cardiovasc Interv. 2005;64:102–7. doi: 10.1002/ccd.20248. [DOI] [PubMed] [Google Scholar]
- 3.Levi DS, Moore JW. Embolization and retrieval of the Amplatzer septal occluder. Catheter Cardiovasc Interv. 2004;61:543–7. doi: 10.1002/ccd.20011. [DOI] [PubMed] [Google Scholar]
- 4.Peuster M, Boekenkamp R, Kaulitz R, Fink C, Hausdorf G. Transcatheter retrieval and repositioning of an Amplatzer device embolized into the left atrium. Catheter Cardiovasc Interv. 2000;51:297–300. doi: 10.1002/1522-726x(200011)51:3<297::aid-ccd11>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 5.Kutty S, Asnes JD, Srinath G, Preminger TJ, Prieto LR, Latson LA. Use of a straight, side-hole delivery sheath for improved delivery of Amplatzer ASD occluder. Catheter Cardiovasc Interv. 2007;69:15–20. doi: 10.1002/ccd.20953. [DOI] [PubMed] [Google Scholar]


