Abstract
Mindfulness training may disrupt the risk chain of stress-precipitated alcohol relapse. In 2008, 53 alcohol-dependent adults (mean age = 40.3) recruited from a therapeutic community located in the urban southeastern U.S. were randomized to mindfulness training or a support group. Most participants were male (79.2%), African American (60.4%), and earned < $20,000 annually (52.8%). Self-report measures, psychophysiological cue-reactivity, and alcohol attentional bias were analyzed via repeated measures ANOVA. 37 participants completed the interventions. Mindfulness training significantly reduced stress and thought suppression, increased physiological recovery from alcohol cues, and modulated alcohol attentional bias. Hence, mindfulness training appears to target key mechanisms implicated in alcohol dependence, and therefore may hold promise as an alternative treatment for stress-precipitated relapse among vulnerable members of society.
Keywords: mindfulness, alcohol dependence, stress, thought suppression, attentional bias, heart-rate variability, relapse, implicit cognition, addiction
Few social ills are as pernicious and persistent as alcohol dependence. Despite more than a century of intervention efforts, 28.4% of persons ever treated for alcohol problems remain dependent on alcohol and 19.1% continue to exhibit alcohol abuse or subclinical dependence symptoms in the past year (Dawson et al. 2005). Clearly, extant interventions are not effective for all alcohol misusers. Persons who drink to cope with stress have significantly higher rates of lifetime and current alcohol dependence symptoms than persons who drink for other reasons (Schroder & Perrine 2007), and stress is known to increase risk of relapse (Sinha 2007). Moreover, alcohol users have a comparatively high likelihood of experiencing serious life stressors: within the population of adult past-year drinkers, 72.5% reported experiencing at least one stressful life event in the past year, and 23.2% experienced 3 to 5 such stressors (Dawson, Grant, & Ruan 2005). The experience of stressful life events significantly predicts quantity and frequency of alcohol consumption; for example, drinkers who reported experiencing six or more stressful events in the past year consumed, on average, more than three times the amount of ethanol per day than did alcohol users who denied experiencing any such stressors (Dawson, Grant, & Ruan 2005). Congruent with such findings, an event-history analysis of 1786 young adults found that both distal and proximal exposure to stressful life events significantly predicted onset of alcohol dependence in a linear and additive fashion after controlling for socioeconomic status and history of psychiatric disorder, implicating a causal role for life stress in the etiology of the disorder (Lloyd & Turner 2008). Convergent evidence suggests that stress is a common precipitant of alcohol misuse and may play an important role in the pathogenesis of alcohol use disorders.
The central risk chain of stress-precipitated alcohol misuse, dependence, and relapse involves cognitive-affective mechanisms that may be explicated by an integrated biopsychosocial framework (for a review, see Garland, Boettiger, & Howard under review). In brief, stress appraisals coupled with deficits in coping resources result in psychophysiological reactivity, perseverative cognition, and negative affect, which in turn trigger automatized schemata to deploy sequences of maladaptive cognitive-behavioral processes that result in compulsive alcohol consumption in spite of often severe consequences for drinking.
Stress-activated engagement of alcohol use action schemata may result in implicit (i.e., unconscious) processing of salient stimuli, manifested as an involuntary attentional bias (AB) towards alcohol cues. Such alcohol approach bias is evident in visual probe tasks, in which heavy drinkers preferentially attend to alcohol cues, resulting in decreased reaction times (RTs) to probes replacing alcohol photographs presented for 500 and 2000 ms compared to probes replacing neutral photographs presented for the same duration (Field, Mogg, Zetteler, & Bradley 2004). Conversely, although alcohol dependent patients have been shown to exhibit an AB toward alcohol cues presented for 50 ms (Noel et al. 2006), they evidence AB away from alcohol cues presented for 500 ms (Stormark, Field, Hugdahl, & Horowitz 1997; Townshend & Duka 2007). Collectively, these findings suggest that alcohol dependent individuals in treatment, unlike their untreated counterparts, evince attentional disengagement from or avoidance of alcohol cues presented for longer stimulus durations (which allow for conscious mediation of attention), but continue to exhibit implicit appetitive attentional responses for short duration stimuli. Alcohol AB has been linked to subjective craving and alcohol consumption (Field & Eastwood 2005). Moreover, among persons who drink to cope with dysphoria, stress enhances alcohol AB and craving (Field & Powell 2007).
When attention is fixated on visual or olfactory alcohol cues, alcohol dependent individuals exhibit significant psychophysiological reactivity (Carter & Tiffany 1999). In turn, this alcohol cue-reactivity may lead to increased craving, which can trigger alcohol consumption as a means of reducing distress. Many persons recovering from alcohol use disorders attempt to suppress cravings, which, paradoxically, can serve to increase intrusive, automatic alcohol-related cognitions (Palfai, Monti, Colby, & Rohsenow 1997), dysphoria, and autonomic arousal (Wenzlaff & Wegner 2000). Indeed, among alcohol dependent persons, thought suppression is negatively correlated with vagally-mediated heart rate variability (Ingjaldsson, Laberg, & Thayer 2003), a putative index of emotion regulation and parasympathetic inhibition of stress reactions (Thayer & Lane 2000). As thoughts of drinking intensify and are coupled with psychobiological distress, the impulse to consume alcohol as a form of palliative coping may overcome depleted self-regulation strength (Muraven, Collins, & Nienhaus 2002; Muraven & Shmueli 2006) leading to relapse. The attempt to avoid distress or allay its impact through compulsive alcohol consumption results in negative reinforcement conditioning that may perpetuate this cycle by further sensitizing the brain to future stressful encounters via allostatic dysregulation of neuroendocrine systems (Koob 2003). Components of this risk chain may be especially malleable to targeted behavioral therapies.
Given that negative affect, autonomic arousal, automaticity, and attentional biases appear to be integral components of the risk chain for stress-precipitated alcohol misuse, dependence, and relapse, interventions targeting these mechanisms may hold promise for its treatment. One such intervention, mindfulness training, which originates from Buddhist traditions but has been co-opted by Western clinicians, has recently gained prominence in the psychological and medical literatures for its salutary effects on stress-related biobehavioral conditions (Baer & Krietemeyer 2006; Ludwig & Kabat-Zinn 2008). Mindfulness involves self-regulation of a metacognitive form of attention: a nonreactive, non-evaluative monitoring of moment-by-moment cognition, emotion, perception, and physiological state without fixation on thoughts of past or future (Garland 2007). A growing body of research suggests that mindfulness affects implicit cognition and attentional processes (e.g., Jha, Krompinger, & Baime 2007; Lutz, Slagter, Dunne, & Davidson 2008; Wenk-Sormaz 2005) as well as heart rate variability indices of parasympathetic regulation (Tang et al. 2009). This evidence, coupled with the knowledge that alcohol use disorders involve automaticity and attentional biases, suggests that mindfulness training may be an effective treatment for alcohol dependent persons coping with stress and dysphoria.
Mindfulness treatments may enhance clinical outcomes in substance-abusing populations. Using a nonrandomized pre-post comparison group design, Bowen et al. (2007) found that mindfulness training of incarcerated inmates reduced post-release substance use, substance-related problems, and psychiatric symptoms to a greater extent than standard chemical dependency services offered at the prison. Other pilot studies of mindfulness-based interventions with substance abusers have found significant reductions in distress, negative affect, stress-related biomarkers, and substance use (Marcus, Fine, & Kouzekanani 2001; Marcus et al. 2003; Zgierska et al. 2008). Despite this suggestive evidence that mindfulness interventions may ameliorate factors related to stress-precipitated alcohol misuse, future research should employ random assignment, as well as behavioral and psychophysiological indices of intervention-related change to overcome threats to validity and elucidate therapeutic mechanisms of action.
To that end, we conducted a pilot randomized controlled trial of a mindfulness intervention designed to disrupt cognitive, affective, and physiological risk mechanisms implicated in stress-precipitated relapse to alcohol consumption. A randomized, controlled design was used to compare the therapeutic effects of a mindfulness-oriented recovery enhancement (MORE) intervention to those of an evidence-based alcohol dependence support group (ASG) in a sample of low-income, primarily African American alcohol dependent adults recruited from a long-term, modified therapeutic community (TC).
We hypothesized that, relative to ASG, MORE would result in significantly greater decreases in perceived stress, impaired alcohol response inhibition, craving for alcohol, psychiatric symptoms, and thought suppression and significantly greater increases in mindfulness and in heart rate variability (HRV) recovery from stress-primed alcohol cues. Lastly, we hypothesized that mindfulness training would reduce alcohol AB, a presumed mechanism of change, by the intervention midpoint and prior to changes in clinical outcomes, such that, relative to ASG, MORE would result in significantly larger decreases in alcohol AB among participants with pre-treatment alcohol approach bias but not for those with baseline alcohol disengagement bias. This hypothesis was justified on the rationale that participants with pre-treatment alcohol disengagement bias entered our study with a pre-existing ability to disengage their attention from alcohol cues and would therefore exhibit a floor effect.
METHOD
Sample Characteristics
Participants were alcohol-dependent adults living in a TC serving persons with substance-use disorders. The TC serves approximately 600 individuals annually, 33% of whom are homeless prior to entering the program.
Potential participants met study inclusion criteria if they were ≥18 years old, met lifetime Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) alcohol dependence criteria, and had resided in the TC for ≥18 months. In this program, 18 months marks the time of transition to employment and residence outside of the TC, and thus represents a point of increased relapse risk. Persons with psychiatric symptoms (screened via the Brief Symptom Inventory; (Derogatis & Melisaratos 1983) were included in the study, as were those with comorbid substance use disorders.
Table 1 presents sample characteristics. Study participants (N = 53) had resided in the TC for a mean of 22.3 ± 3.7 months. A majority of participants were male (79.2%), African American (60.4%), and low-income (52.8% had earned < $20,000 in the year before entering the TC). Participants reported high rates of lifetime exposure to traumatic violence, moderate psychiatric symptomatology, and high levels of alcohol dependence severity: for example, the mean number of DSM-IV alcohol dependence criteria met by participants was 6.5 ± 1.0, and the mean number of standard alcoholic drinks consumed per day in the year before entering treatment was 19.0 ± 10.9. Approximately 81% of the sample reported daily use of at least one psychoactive drug in addition to alcohol before entering the TC, with cocaine the most frequently used drug (M = 17.1 ± 12.5 days used in the month before entering the TC). All participants reported continuous abstinence from psychoactive substance use during their residence in the TC, which ranged from 18 to 28 months. Reports of abstinence were corroborated by random urinalysis conducted at the TC, as well as through daily evaluation from program staff.
Table 1.
Pre-intervention Characteristics of MORE and ASG Intervention Groups, Total Study Participants and Program Completers*
| Variable | MORE (N=27) | ASG (N=26) | Total (N = 53) | Completers (N = 37) |
|---|---|---|---|---|
| Length of stay in residential program (M, SD) | 22.4 (2.6) | 22.2 (4.6) | 22.3 (3.7) | 22.05 (2.4) |
| Gender N (%) | ||||
| Male | 22 (81.5) | 20 (76.9) | 42 (79.2) | 28 (75.7) |
| Female | 5 (18.5) | 6 (23.1) | 11 (20.8) | 9 (24.3) |
| Race N (%) | ||||
| African American | 17 (62.9) | 15 (57.7) | 32 (60.4) | 24 (64.9) |
| Caucasian | 7 (25.9) | 11 (42.3) | 18 (34.0) | 12 (32.4) |
| Other | 3 (11.1) | 0 | 3 (5.6) | 1 (2.7) |
| Age (M, SD) | 39.9 (8.7) | 40.7 (10.2) | 40.3 (9.4) | 40.9 (9.5) |
| DSM-IV Dependence Criteria (M, SD) | 6.5 (0.9) | 6.6 (0.9) | 6.5 (1.0) | 6.4 (1.0) |
| Income before entering TC N (%) | ||||
| <$20,000 | 14 (51.9) | 14 (51.9) | 28 (52.8) | 21 (56.8) |
| $20,000–40,000 | 9 (33.3) | 8 (30.8) | 16 (32.1) | 11 (29.7) |
| $41,000–60,000 | 2 (7.4) | 3 (11.5) | 5 (9.4) | 3 (8.1) |
| $61,000–80,000 | 1 (3.7) | 0 | 1 (1.9) | 1 (2.7) |
| >$80,000 | 1 (3.7) | 1 (3.8) | 2 (3.8) | 1 (2.7) |
| Drinks per day prior to entering TC (M, SD) | 21.4 (11.9) | 16.6 (9.5) | 19.0 (10.9) | 18.7 (11.2) |
| AUDIT (M, SD) | 32.8 (6.0) | 31.8 (5.3) | 32.3 (5.6) | 32.08 (5.4) |
| DAST (M, SD) | 20.7 (5.1) | 21.2 (5.8) | 21.0 (5.4) | 20.4 (4.7) |
| Psychiatric symptoms: | ||||
| Depression | 4.9 (4.6) | 5.0 (4.4) | 4.9 (4.4) | 4.9 (4.9) |
| Anxiety | 5.8 (3.8) | 5.0 (4.3) | 5.4 (4.1) | 4.9 (4.2) |
| Hostility | 4.0 (3.6) | 4.3 (3.8) | 4.2 (3.6) | 3.9 (3.8) |
| Interpersonal sensitivity | 4.4 (3.8) | 3.9 (3.4) | 4.2 (3.6) | 4.2 (3.9) |
| Trauma: | ||||
| # of times seen someone killed in person | 3.0 (3.2) | 2.7 (2.7) | 2.9 (2.9) | 2.9 (2.9) |
| # of times hurt or in danger of being killed | 6.0 (11.4) | 6.7 (12.3) | 6.4 (11.7) | 6.4 (11.7) |
| # of times hit by someone with intent to hurt | 7.3 (6.9) | 9.1 (11.4) | 8.1 (9.3) | 8.1 (9.3) |
| # of times mugged | 2.4 (2.9) | 1.5 (1.5) | 2.0 (2.3) | 2.0 (2.3) |
| # of times attacked by a weapon or by someone with intent to kill | 2.5 (2.2) | 2.3 (1.7) | 2.4 (2.0) | 2.4 (2.0) |
All of the variables listed above were analyzed with one-way ANOVAs and chi-square tests. No significant baseline differences between treatment groups or completers and non-completers were found.
Intervention Groups
MORE
The ten-session, manualized MORE intervention was adapted as a treatment for alcohol dependence from Mindfulness-Based Cognitive Therapy, an empirically-supported, mindfulness intervention designed to prevent depression relapse (Segal, Williams, & Teasdale 2002). MORE involves mindful breathing and walking meditations, as well as experiential exercises relating general mindfulness principles to addiction-specific issues such as relapse triggers, craving, thought suppression, stress, and unconscious substance use behaviors. A Master’s level social worker (MSW) with experience in mindfulness meditation who was trained in cognitive-behavioral treatments for substance dependence delivered the MORE intervention.
ASG
To control for time, attention, credibility, and group process, the ten-session ASG condition consisted of MSW-led social support groups derived from the active, evidence-based treatment condition outlined in the Matrix Model intensive outpatient treatment manual (Rawson & McCann 2006). The addictions treatment training of each MSW was comparable. Wherever possible, ASG topics were selected to roughly match corresponding themes of the MORE intervention. ASG participants were guided to disclose feelings and thoughts about group topics, as well as to provide advice and emotional support for their peers. Although the Master’s-level social worker facilitated discussion using client-centered counseling skills (Rogers 2003), no prescriptions for change were given.
For fifteen minutes a day, MORE participants were asked to practice mindfulness exercises while ASG participants were asked to journal for 15 minutes per day on support group topics. A brief session by session description of the study treatment groups is detailed in Table 2.
Table 2.
Session-Specific Description of MORE1 and ASG Interventions
| Session | MORE | ASG |
|---|---|---|
| 1 | Discussion of mindfulness and automatic drinking; mindfulness of craving; mindful breathing and body scan | Discussion of triggers for alcohol dependence relapse |
| 2 | Discussion of cognitive reappraisal; practice of mindful decentering and mindful breathing | Discussion of justifications for relapse and using alcohol to mask one’s emotions |
| 3 | Discussion of attentional re-orienting as means of coping with negative emotions and craving; mindful breathing; mindfulness of perceptions & sensations | Discussion of how participants cope with emotions of anger and sadness |
| 4 | Discussion of craving; practice of “urge surfing,” mindfulness of craving, and contemplation of negative consequences of drinking; imaginal alcohol cue-exposure; mindful breathing practice | Discussion of how participants cope with craving and managing compulsive behavior |
| 5 | Discussion of the relationship of the stress response to craving; imaginal stress exposure; mindful breathing | Discussion of stress and methods participants use to relax without alcohol |
| 6 | Discussion of thought suppression, aversion, and attachment; exercise in the futility of thought suppression; mindful breathing and acceptance | Discussion of the attempt to maintain control and loss of control |
| 7 | Discussion of the deleterious effects of alcohol on the body; mindful interoceptive awareness; mindful walking | Discussion of physical health promotion and ways to recreate without alcohol |
| 8 | Discussion of relational triggers for relapse; mindful communication; compassion meditation | Discussion of codependence relationships and the challenge of forming friendships without alcohol |
| 9 | Discussion of interdependence, meaning, and spirituality; meditation on interdependence; mindful breathing | Discussion of spirituality |
| 10 | Review; discussion of how to maintain mindfulness practice; development of mindful relapse prevention plan; imaginal rehearsal of mindful relapse prevention; mindful breathing | Reflection on the support group experience; discussion of the recovery process |
MORE is adapted from Mindfulness-based Cognitive Therapy for Depression [29] and tailored to apply mindfulness principles to addiction-related topics.
Design and Procedure
All study procedures were approved by the University of North Carolina – Chapel Hill Institutional Review Board. Participants were recruited when they had resided at least 18 months at the TC through an informational presentation about the study made at the TC, as well as through flyers and direct referrals from TC staff. Screening procedures included administration of the Alcohol Use Disorders Identification Test (AUDIT) and a semi-structured diagnostic interview conducted by a MSW to ensure that all participants met lifetime DSM-IV criteria for alcohol dependence. Participants were excluded if they scored < 16 on the AUDIT, or if they endorsed screening questions indicating active psychosis (Degenhardt, Hall, Korten, & Jablensky 2005) or suicidality. Upon enrollment, participants were randomly assigned to either MORE or ASG. No participants refused randomization. Participants received $25 for completion of each assessment and $5 for attending each intervention session, with a possible bonus of $25 for perfect attendance of all assessments and sessions; total maximum: $175.
Measures
Study participants completed standardized psychosocial instruments, a psychophysiological cue-reactivity protocol, and a computer-based measurement of alcohol AB before and after 10 weeks of intervention; the alcohol AB assessment was also administered at the intervention midpoint (5 weeks). Psychosocial instruments were verbally administered in interviews conducted by a research assistant who was blind to group assignment. All measures were administered in the same order across participants in a single session. Cronbach’s alpha (α) is reported as an index of the internal consistency of each psychometric instrument in the present sample.
Intervention credibility
Perceived credibility of the MORE and ASG interventions as treatments for alcohol dependence was assessed after session two using a scale (α = .83) based on the Attitudes Towards Treatment measure (Borkovec & Nau 1972) which assesses patients’ expectations of benefit once treatment has been explained. The scale has been found to distinguish between standard psychotherapy approaches and illogical placebo treatments, is predictive of clinical improvement, and relatively independent of symptom severity (Borkovec & Nau 1972).
Mindfulness
The Five Facet Mindfulness Questionnaire (FFMQ, α = .81), comprised of 39 Likert-type items, was used to measure self-reported mindfulness. The FFMQ yields a total score and scores for five internally consistent mindfulness factors each with their own convergent and predictive validity: nonreactivity to inner experience (tapped by items such as “I watch my feelings without getting lost in them”), observing and attending to experience (“I pay attention to sensations, such as the wind in my hair or the sun on my face”), describing and discriminating emotional experiences (“I’m good at finding words to describe my feelings”), nonjudging of experience (“I tell myself I shouldn’t be feeling the way that I am feeling”), and acting with awareness (“I find myself doing things without paying attention”) (Baer, Smith, Hopkins, Krietemeyer, & Toney 2006).
Psychosocial factors related to alcohol-dependence
The Brief Symptom Inventory (BSI, α = .96) was use to measure to what degree participants were currently distressed by psychiatric symptoms (Derogatis & Melisaratos 1983) on 5-point scale (0 = not at all, 4 = extremely). The 53 items include symptoms such as “Feeling fearful” and “Feelings of guilt.” Subjective alcohol craving frequency and intensity was assessed with the Penn Alcohol Craving Scale (PACS, α = .91) (Flannery et al. 2001). Self-reported ability to inhibit the urge to use alcohol was assessed with the Impaired Alcohol Response Inhibition Scale (IRISA, α = .79) (Guardia, Trujols, Burguete, Luquero, & Cardus 2007). Participants indicate on a 4-point scale with 14 items how often over the past week they would agree with statements including “When I have decided not to drink, I find it easy not to” and “If I thought about the possibility of drinking I think I could have resisted.” The 10-item Perceived Stress Scale (PSS-10, α = .85) was used to assess on a 5-point scale how often (0 = never, 4 = very often) in the past month participants found their lives unpredictable, uncontrollable, and overwhelming (Cohen, Kamarck, & Mermelstein 1983), and includes items like “How often have you felt nervous and ‘stressed’?” and “How often have you felt that you were on top of things?”. Chronic thought suppression, the maladaptive and counterproductive tendency to avoid or repress undesirable cognitions and emotions, was assessed with the White Bear Suppression Inventory (WBSI, α = .84) (Wegner & Zanakos 1994). Participants indicate agreement on a 5-point scale with 15 items, including “I always try to put problems out of mind” and “I often do things to distract myself from my thoughts.”
Psychophysiological cue-reactivity
Due to our interest in the effects of stress on alcohol dependence, a cue-reactivity protocol was used to measure autonomic reactivity to and recovery from stress-primed alcohol cues. First, electrocardiogram (ECG) sensors were attached to participants’ right and left pectoral muscles. ECG was sampled at 500 Hz and recorded continuously throughout the protocol on a Biopac MP150 data acquisition system (Biopac Systems, Goleta, CA). Once electrodes were attached, participants were asked to rate their current level of distress on a 10-point visual analogue scale (VAS) (0 = not at all, 9 = extremely). Next, participants were instructed to remain motionless, silent, and “not think about anything in particular” for a 5-minute baseline. After this baseline period, participants again rated their current distress to assess whether any initial reactivity elicited by the unfamiliar experimental context had stabilized after the 5-minute rest period. Next, 30 aversive photographs from the International Affective Picture System (IAPS) were serially presented on a 15” laptop screen for 10 seconds each (total duration: 5 min). Participants were asked to fixate on the image stream while holding as still as possible. After this presentation, participants again rated their current level of distress. Next, 30 photographs of beer, wine, and distilled liquor (12 of which included individuals drinking or preparing to drink alcohol) were serially presented for 10 seconds each (total duration: 5 min), and participants were again instructed to keep still and fixate on the image stream. At the end of the alcohol cue exposure period, participants were asked to rate their current level of distress. Lastly, participants were instructed, “Remaining silent and keeping your body still, use whatever methods you have learned to cope with or reduce your craving” for a 5-minute recovery period, after which they again rated their current level of distress. A single qualitative question, “What methods did you use to cope?”, identified coping strategies used.
R-R intervals were detected in the ECG data using automated routines in Nevrokard aHRV software (Medistar, Stegne, Ljubljana, Slovenia). The R-wave file was then visually inspected to correct misidentified or omitted R-waves. Kubios 2.0 (Biosignal Analysis and Medical Imaging Group, University of Finland) was used for time-domain analysis of R-R intervals. The square root of the mean squared differences between successive R-R intervals (RMSSD) was selected as our estimate of vagally mediated HRV. The present analysis focused on a particular planned contrast: HRV recovery, that is, changes in HRV between alcohol cue exposure and the recovery period.
Alcohol attentional bias
A modified dot probe task (MacLeod, Mathews, & Tata 1986) created in E-Prime 1.2 (PST Inc., Pittsburgh, PA) and presented on an IBM T60 laptop with a 15” screen was used to measure alcohol AB (for methodological details, see Garland, Boettiger, Gaylord, West Chanon, & Howard under review). In brief, for each trial, two grayscale images appeared, one on each side of a fixation cross (+); one image was neutral in content, the other was alcohol-related. Each pair of images was presented for either 200 ms or 2000 ms. Left/right position of the alcohol images and presentation duration were both randomized and counterbalanced across 20 practice trials and 160 trials. Following a 50 ms inter-stimulus interval (ISI), a target (two dots) replaced one of the images and a distracter probe (one dot) replaced the other image; probes appeared for 100ms. Participants were instructed to fixate on the cross between the images and indicate the location of the target by responding with a left or right button press on a keypad. Target probes pseudorandomly replaced alcohol and neutral images with equal frequency.
Alcohol stimuli included 13 photographs of alcoholic drinks, and 7 photos of persons drinking alcohol. Neutral stimuli included 13 photos of kitchen items and 7 photos of persons in kitchen scenes. Stimulus sets were analyzed with respect to their spatial frequency content to ensure that they did not differ in terms of basic visual properties, which could elicit reflexive attentional capture irrespective of image content. On measures of both the spectral peak (Neutral: 0.0180, Alcohol: 0.0176, t(38)=0.383, p=0.704) and spectral width (Neutral: 59.20, Alcohol: 59.29, t(38)=−0.027, p=0.979), the two stimulus sets were not significantly different.
Data analysis
Data were examined for outliers and to ensure they met distributional assumptions for normality. All outcome variables were approximately normally distributed, save for heart rate variability data (RMSSD) which was skewed and therefore log-transformed (log10). Bivariate correlations, t-tests, chi-square tests, and repeated-measures analyses of variance (ANOVA) as implemented in SPSS 17.0 were used to test hypotheses, compare group differences at baseline and over time, and explore individual differences in the change process. When necessary, Greenhouse-Geisser corrections were used to address violations of sphericity.
For AB data, trials with extreme RTs (>3 SD above the individual mean) were discarded as outliers (mean = 2.5±1.5 per participant); error trials were also discarded (mean = 4.9±.08). For each participant, AB scores were calculated by subtracting their mean RT to probes replacing alcohol photos from their mean RT to probes replacing neutral photos, such that positive bias scores indicate an AB toward visual alcohol cues.
RESULTS
Pre-intervention Group Differences
There were no significant pre-intervention differences between MORE and ASG participants on age, gender, race, income, number of months residing in the TC, alcohol dependence criteria, AUDIT, DAST, exposure to traumatic violence, craving, impaired alcohol response inhibition, psychiatric symptoms, mindfulness, thought suppression, or alcohol attentional bias (Table 1). Similarly, there were no significant differences between MORE and ASG participants in HRV responses during the pre-intervention cue-reactivity protocol. The only difference approaching statistical significance (p = .094) was for number of drinks/day, such that participants randomized to MORE had marginally higher levels of alcohol consumption before entering the TC than those randomized to ASG. Similarly, there were no significant differences between intervention completers and drop outs on any of the variables listed above. In addition, there was no significant difference between MORE and ASG participants in intervention credibility ratings (mean = 39.4±6.4, and 40.6± 4.7, respectively; F(1, 41) = .497, p = .485).
Intervention Compliance and Attrition
Approximately 69% (N = 37) of the total enrolled sample (N = 53) completed post-intervention assessments, with 18 participants completing the MORE intervention and 19 completing the ASG intervention; attrition did not significantly differ between groups. Similarly, the groups did not differ in attendance; MORE participants completed 8.0 ± 2.1 sessions, whereas ASG participants completed 7.3 ± 3.5 sessions.
Outcomes
Table 3 summarizes changes in clinical and attentional variables over the course of both the MORE and ASG interventions.
Table 3.
Intervention effects on Clinical and Attentional Variables
| Variables | Means | F-test | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | df | F | ηρ2 | p | |||
| Perceived stress | Time | 1 | 18.11 | .34 | <.001 | |||
| MORE (n=18) | 15.6 (4.7) | 10.8 (5.3) | Group X Time | 1 | 5.06 | .13 | .03 | |
| ASG (n=19) | 16.0 (7.6) | 14.5 (5.8) | ||||||
| Thought suppression | Time | 1 | .11 | .00 | .74 | |||
| MORE (n=18) | 53.6 (8.7) | 50.1 (7.9) | Group X Time | 1 | 4.26 | .11 | .04 | |
| ASG (n=19) | 50.9 (11.2) | 53.5 (9.4) | ||||||
| Mindfulness | Time | 1 | .98 | .02 | .33 | |||
| MORE (n=17) | 108.3 (12.3) | 109.8 (14.6) | Group X Time | 1 | .05 | .002 | .81 | |
| ASG (n=19) | 115.9 (15.1) | 118.3 (17.9) | ||||||
| Craving | Time | 1 | 1.36 | .04 | .25 | |||
| MORE (n=18) | 4.7 (5.5) | 4.6 (5.3) | Group X Time | 1 | 1.05 | .03 | .31 | |
| ASG (n=19) | 4.9 (4.4) | 3.2 (3.6) | ||||||
| Impaired alcohol response inhibition | Time | 1 | 3.43 | .07 | .09 | |||
| MORE (n=18) | 7.8 (5.5) | 4.9 (4.9) | Group X Time | 1 | .88 | .03 | .35 | |
| ASG (n=18) | 6.2 (4.9) | 5.3 (4.2) | ||||||
| Global psychiatric symptoms | Time | 1 | 10.83 | .24 | .002 | |||
| MORE (n=18) | 42.7 (36.4) | 19.6 (12.5) | Group X Time | 1 | .50 | .01 | .48 | |
| ASG (n=19) | 46.7 (33.0) | 31.8 (21.4) | ||||||
| Pre | Mid | Post | df | F | η | p | ||
| 200ms approach AB | Time | 1 | 1.76 | .10 | .20 | |||
| MORE (n=9) | 7.2 (6.9) | 10.7 (13.9) | 2.9 (21.9) | Group X Time | 2 | 4.76 | .23 | .03 |
| ASG (n=9) | 13.5 (8.2) | −9.0 (19.9) | 17.6 (17.2) | |||||
| 2000ms approach AB | Time | 1 | 4.54 | .27 | .02 | |||
| MORE (n=7) | 12.6 (12.1) | 3.6 (23.7) | 2.3 (21.9) | Group X Time | 1 | 1.07 | .08 | .36 |
| ASG (n=7) | 12.9 (9.1) | −12.8 (10.9) | 1.7 (10.4) | |||||
Intervention effects on self-report measures
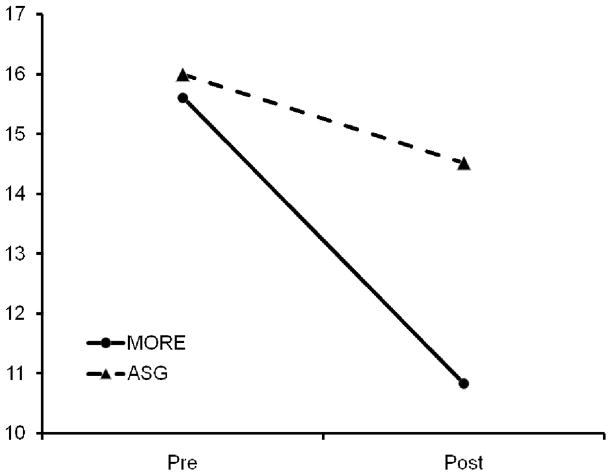
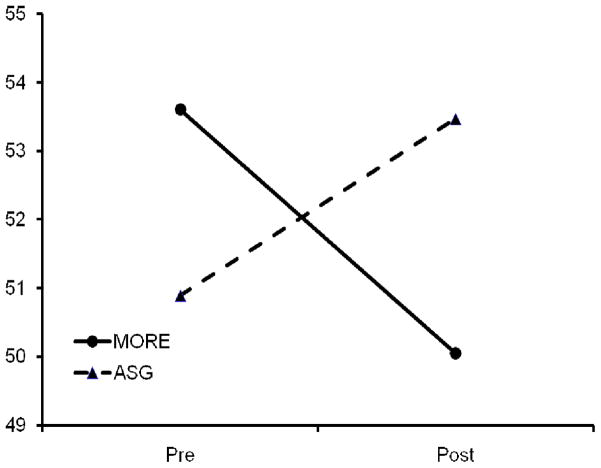
Both MORE and ASG led to significant reductions in perceived stress over time, F(1, 35) = 18.11, p < .001, ηρ2 = .34. Moreover, there was a significant intervention × time interaction on perceived stress, F(1, 35) = 5.06, p = .03, ηρ2 = .13, such that MORE led to significantly larger decreases in perceived stress over a 10-week period than did ASG (Figure 1). Although there were no main effects of time on thought suppression, there was a significant intervention × time interaction on thought suppression, F(1, 35) = 4.26, p = .04, ηρ2 = .11, such that MORE led to significant decreases in thought suppression over a-10 week period, whereas an ASG led to increased thought suppression (Figure 2). Conversely, while there was a significant decrease in psychiatric symptoms over time, F(1, 35) = 10.83, p = .002, ηρ2 = .24, there was no significant intervention × time interaction on psychiatric symptoms. With regard to self-reported mindfulness, there were neither main effects nor an intervention × time interaction effect on changes in FFMQ scores, including subscales. Similarly, there was an absence of both main and interaction effects on craving and impaired alcohol response inhibition, suggesting that both interventions had negligible effects on alcohol urges and neither reduced craving more than the other.
Figure 1.
Intervention group differences in perceived stress at baseline and 10-weeks post-intervention
Figure 2.
Intervention group differences in thought suppression at baseline and 10-weeks post-intervention.
Intervention effects on alcohol attentional bias
Despite the fact that pre-intervention 2000 and 200 ms AB data were both approximately normally distributed (Kolmogorov-Smirnov tests p’s = .97 and .26, respectively), approximately one-half of participants exhibited 2000 and 200 ms AB towards probes replacing alcohol photos while the other half exhibited AB towards probes replacing neutral photos. Given that AB towards alcohol cues is theorized to represent appetitive conditioning (Field & Cox 2008) while AB away from alcohol cues is thought to represent disengagement from or avoidance of the substance (Townshend & Duka, 2007), we analyzed data from participants with these two apparently distinct types of AB separately. Thus, for each presentation duration (2000 ms and 200 ms) we divided participants into two groups: those with an AB > 0, i.e., the 200 ms (N = 18) and 2000 ms (N = 16) alcohol approach groups, and those with an AB < 0, i.e., the 200 ms (N = 19) and 2000 ms (N = 21) alcohol disengagement groups.
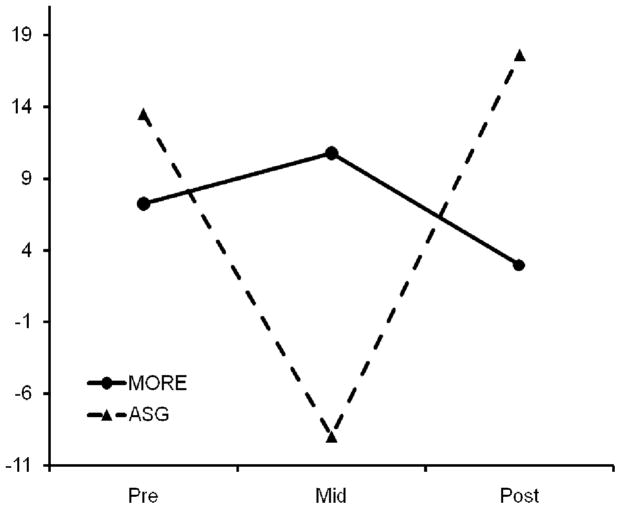
Among the 200ms alcohol approach bias group, there was a significant intervention × time interaction on 200 ms AB, F(2, 32) = 4.76, p = .03, ηρ2 = .23 (Figure 3). Within-subjects contrasts revealed a significant quadratic form to the intervention × time interaction, F(1, 16) = 8.09, p = .01. For the 2000ms alcohol approach bias group, 2000 ms AB significantly decreased over the course of both interventions, F(2, 12) = 4.54, p = .02, and there was no significant intervention × time effect.
Figure 3.
Intervention group differences in 200 ms AB at baseline, 5-week intervention midpoint, and 10-weeks post-intervention for participants with alcohol approach attentional bias.
Intervention effects on heart rate variability responses to stress-primed alcohol cues
Due to hardware problems during physiological recording, complete post-intervention HRV data was available for 18 MORE and 16 ASG participants. To examine the effects of the intervention on HRV responses to alcohol cue-exposure following experimental stress-induction, we controlled for severity of alcohol dependence by including the number of drinks consumed a day prior to entering the TC as a covariate. Because tonic levels of perceived stress are known influence HRV, we also covaried post-intervention perceived stress to examine intervention effects on HRV responses to the experimental alcohol cue-reactivity paradigm. Although the overall F-test for the intervention × experimental condition (baseline, stress exposure, alcohol exposure, recovery) interaction was nonsignificant, there was a significant intervention × condition interaction on the planned contrast between alcohol cue exposure and the recovery period, F(1,30) = 5.30, p = .03, ηρ2 = .15, indicating that the pattern of HRV from alcohol cue exposure to recovery varied as a function of intervention (See Figure 4). MORE participants had higher HRV during alcohol cue exposure which then decreased during the recovery period, whereas ASG participants had lower HRV during alcohol cue exposure which then increased during the recovery period. No such significant intervention × condition effect on HRV was found during the baseline assessment after covarying for severity of alcohol dependence and pre-intervention perceived stress, lending support to the interpretation that the observed post-intervention between-groups differences in HRV recovery were the result of the MORE and ASG interventions.
Figure 4.
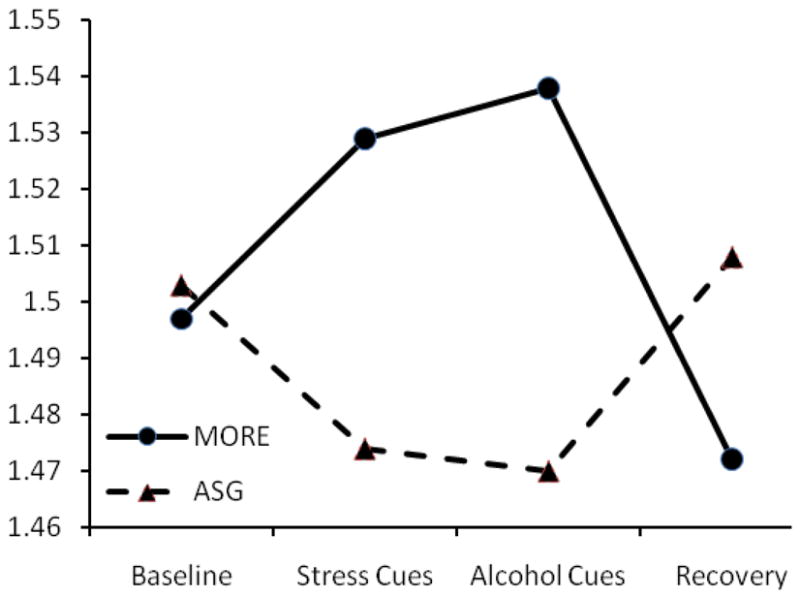
Intervention group differences in post-treatment HRV (RMSSD, log10)* during stress-primed alcohol cue-reactivity protocol.
* This figure depicts mean RMSSD, log10, across experimental conditions after covarying prior level of alcohol consumption and post-treatment perceived stress
Qualitative inquiry indicated that during the post-intervention cue-reactivity protocol, all MORE participants practiced mindfulness meditation during the recovery period while the most common strategies used by ASG participants included cognitive reappraisal (e.g., focus on the negative consequences of drinking and the positive benefits of sobriety) as well as suppression (e.g., tried to think about something else). With regard to subjective distress during the cue-reactivity protocol, after controlling for prior level of alcohol consumption and tonic post-intervention perceived stress, MORE participants had significantly larger reductions in distress from alcohol cue-exposure to the recovery period than did ASG participants, F(1,32) = 4.94, p = .03, ηρ2 = .13.
Individual difference variables and changes in stress and addiction-related factors
To determine whether improvements in self-reported ability to inhibit alcohol responses were associated with individual differences in baseline stress, changes in impaired alcohol response inhibition (as measured by the IRISA) were correlated with pre-intervention perceived stress. Among MORE participants, the greatest improvements in self-reported ability to inhibit alcohol responses were found among those with highest pre-intervention levels of perceived stress, r = .52, p = .03. Among ASG participants, these variables were not significantly correlated, indicating that the relationship between pre-treatment stress and improved ability to inhibit alcohol responses may be attributable to the MORE intervention. Thus, it appears that MORE is most effective at inhibiting the appetitive alcohol responses of persons who experience high levels of stress at baseline, i.e. persons who may be more likely to drink as a means of coping with stress.
Importantly, among MORE participants, changes in thought suppression were correlated with changes in AB200 (r = .49, p = .042), changes in impaired alcohol response inhibition (r = .48, p = .045), and changes in post-intervention HRV recovery, (r = .49, p = .045). MORE participants who experienced greater decreases in thought suppression over the course of intervention also evidenced greater decreases in AB200 and impaired alcohol response inhibition while evincing the greater HRV recovery. However, among ASG participants, there was no significant correlation between these variables. In contrast, across the entire sample of persons who completed either intervention, decreases in stress were positively correlated with decreases in impaired alcohol response inhibition (r = .33, p = .046).
DISCUSSION
The present results suggest that mindfulness training may affect cognitive, affective, and physiological risk mechanisms implicated in relapse to alcohol dependence. Mindfulness training appeared to reduce stress and alcohol thought suppression to a significantly greater extent than did an evidence-based active control intervention. Notably, mindfulness training seems to decrease AB towards brief (200ms) visual alcohol cues, an implicit cognitive process linked with alcohol dependence, and increase HRV recovery from alcohol cues following stress induction. In addition, MORE appears to be a feasible intervention to prevent stress-precipitated alcohol relapse, based on the high perceived treatment credibility and program adherence, and the absence of significant differences in attrition from an ASG, the current standard of care.
Mindfulness training reduces stress and thought suppression
Among recovering alcohol-dependent individuals, mindfulness training appears to be a potentially effective stress reduction technique. MORE reduced perceived stress to a greater extent than did ASG, which is noteworthy given that social support reduces stress reactivity and buffers deleterious effects of stressful life events (Christenfeld & Gerin 2000). The stress reduction effects of mindfulness training among nonclinical populations are well known in the literature (Grossman, Niemann, Schmidt, & Walach 2004), but it is notable that significant effects were obtained in a sample of clinically-disordered, alcohol-dependent adults with extensive trauma histories who may be more vulnerable to stress-precipitated relapse due to allostatic dysregulation of neural stress circuitry (Valdez & Koob 2004).
Like stress, thought suppression significantly decreased over the course of ten weeks of mindfulness training. In turn, decreases in thought suppression among MORE participants were significantly correlated with decreases in impaired alcohol response inhibition, raising the possibility that participants who improved their ability to regulate drinking urges may have done so via reductions in thought suppression. Alternatively, MORE participants who experienced attenuated drinking urges may have had less need to engage in thought suppression. Our finding that mindfulness training reduced thought suppression partially replicates results reported by Bowen et al. (2007) within the context of our randomized controlled design, although limitations of statistical power in the present study preclude replication of their tests for mediation. Thought suppression appears to play a substantial role in psychopathology (Purdon, 1999), by increasing the rate, intensity, and accessibility of the very thoughts and moods it is directed against (Wegner, Schneider, Carter, & White 1987), as well as intensifying sympathetic nervous system activity (Gross 2002; Gross & Levenson 1993; Wenzlaff & Wegner 2000). In the context of alcohol dependence, thought suppression seems to enhance the conscious awareness of alcohol-related cognitions and affective reactions. MORE, with its emphasis on nonjudgmental, metacognitive awareness of present-moment experience, appeared to counter this deleterious cognitive strategy and therefore may have prevented post-suppression rebound effects from exacerbating negative affect and intrusive alcohol-related cognitions that can promote relapse. Conversely, participants in the alcohol-dependence support group may have professed invulnerability to alcohol urges for the purposes of social conformity and maintaining an appearance of competence, thereby leading to the increased thought suppression observed in the ASG data.
Contrary to our hypotheses, MORE did not significantly increase self-reported mindfulness, nor did it result in significant decrements in craving. This counterintuitive finding may be explained by the nature of the participants and by the mindfulness training itself. Prior to mindfulness training, the alcohol-dependent individuals sampled in this study may have overestimated their level of mindfulness due to their lack of understanding of the construct and their general lack of self-awareness, which was one of the intended targets of mindfulness training itself. After ten weeks of mindfulness practice reflecting on their own internal experience, MORE participants may have had a greater sense of the meaning of the FFMQ questions, and having encountered numerous challenges in their attempts to embody the principles of nonreactivity, nonjudgment, acting with awareness, etc., may have been able to more accurately appraise their level of mindfulness. Similarly, the alcohol-dependent study participants residing in a therapeutic community where access and exposure to alcohol was limited may have lacked awareness of the extent to which they continued to have drinking urges, leading to an underreporting of craving at baseline. This lack of awareness of alcohol reactivity that has been shown to be predictive of future relapse (Rohsenow et al. 1994). Because MORE was partly designed to increase consciousness of craving and decrease urge suppression, ten weeks of the intervention may have heightened awareness of latent alcohol urges, thus resulting in an apparent lack of change in craving over time. Of course, such interpretations are speculative, and a number of alternative interpretations are possible, such as inaccurate reporting due to social desirability bias, ceiling/floor effects due to previous participation in a therapeutic community, and the possibility of true null effects of MORE on mindfulness and craving.
In contrast to the null effects on craving, both interventions led to statistically significant reductions in psychiatric symptoms. The fact that ASG exerted a treatment effect comparable to that of MORE indicates that the control condition used in this study was therapeutically active. Moreover, this finding confirms those of Bowen et al. (2006) that mindfulness training decreases psychiatric symptoms among substance abusers. However, given that no significant differences were found between intervention conditions, it cannot be ruled out that the reductions in psychiatric symptoms observed were due to placebo effects, the passage of time, or other elements of the TC.
Mindfulness training augments psychophysiological recovery from alcohol cues
MORE and ASG had differential effects on HRV during a stress-primed alcohol cue-reactivity paradigm. Although there were no significant differences at baseline, after 10 weeks of intervention, MORE participants, relative to ASG participants, exhibited high HRV during alcohol cue exposure which then decreased as they practiced mindfulness meditation during the recovery period. Given that greater HRV has been linked to greater prefrontal inhibition of stress-induced sympathetic nervous system activation during emotion regulation tasks (Thayer & Lane 2009), the pattern observed among MORE participants may be interpreted as evidence of engagement of emotion regulation processes during alcohol cue exposure followed by disengagement of cognitive resources from alcohol-related cognitions and cravings during the recovery period. This interpretation is consistent with conceptualizations of mindfulness as involving a “letting go” of distressing mental content (Baer & Krietemeyer 2006). However, lower HRV may also be related the rhythmic pacing of the breath that may stem from novice meditation techniques of breath focus and counting (Peressutti, Martin-Gonzalez, J, & Mesa 2009). These techniques may work as a rhythmic stimulus that entrains the breath and reduces overall HRV. Alternatively, lower HRV during recovery may indicate reduced parasympathetic efference associated with focused, concentrated attention on the breath. While highly experienced meditators may show increased HRV during mindfulness practice, novice meditators, for whom meditation on the breath is cognitively demanding, exhibit decreased HRV during meditation practice (Peressutti et al., 2009). Heightened cognitive load has been shown to suppressed HRV during working memory and sustained attention tasks (Hansen, Johnsen, & Thayer, 2003). Thayer and Lane’s (2000) assert that “appropriate short-term suppression of HRV” during attentional engagement is critical for self-regulation (p. 207).
Other converging evidence supports these interpretations. Indeed, the neurovisceral integration model (Thayer & Lane 2000) posits that as central autonomic network activity increases, HRV increases. Thus, HRV should increase proportionally to the intensity of conscious processing of emotion and emotion regulation. Indeed, relative to ASG participants, MORE participants had higher post-intervention HRV during stress and alcohol cue exposure (despite having lower pre-intervention levels of HRV), perhaps indicating the marshalling of greater cognitive control in service of regulating negative emotions triggered by aversive images and cravings elicited by alcohol cues. Such HRV effects have been found to result from the control of urges: high self-regulation efforts to resist temptation result in increased HRV (Segerstrom & Nes 2007), and alcoholics who report a greater ability to regulate alcohol urges experience increased HRV when exposed to alcohol cues relative to those who report less ability to regulate alcohol-use compulsions (Ingjaldsson et al. 2003).
In contrast, the post-intervention ASG group evidenced phasic suppression of HRV during stress and alcohol cue exposure, a pattern that seems to indicate disruption of homeostasis, anxiety, and stress reactivity (Thayer & Lane 2000). Subsequently, ASG participants increased HRV during the recovery period when they were engaged in emotion regulation strategies such as reappraisal and suppression. These strategies may have required a high level of PFC activation, thus leading to the increased HRV observed among ASG participants during the recovery period, an interpretation supported by research showing increased HRV during reappraisal and suppression (Butler, Wilhelm, & Gross 2006).
Hypothetically, this pattern of cardiac response may indicate the superior efficiency of mindfulness as an emotion regulation strategy relative to reappraisal, distraction, and suppression strategies, an inference supported by our self-report data that show that MORE led to greater reductions in subjective distress from alcohol cue-exposure to recovery. Concomitantly, for those participants trained in mindfulness, larger pre-post reductions in thought suppression were correlated with greater post-intervention HRV recovery from alcohol cue exposure. We speculate that those MORE participants who most successfully learned to employ mindfulness to cope with alcohol-related cognitions and craving instead of suppression were able to disengage from those mental phenomena more efficiently, as reflected by increased HRV recovery. In contrast, alcohol dependent persons who continued to use thought suppression as a strategy may have remained fixated on alcohol-related cognitions and cues due to the post-suppression rebound effect, resulting in less HRV recovery which may be reflective of continued ruminative engagement (Key, Campbell, Bacon, & Gerin 2008).
Mindfulness training modulates implicit alcohol attentional bias
Intervention effects on 200 ms alcohol AB may also index degree of disengagement from alcohol-related cognitions. Given that mindfulness training has been shown to impact attentional orienting and alerting processes (Jha et al. 2007), we hypothesized that MORE would impact 200ms AB in persons with alcohol approach biases at baseline. Although this hypothesis was supported by the data, we expected a simple decreasing linear change trajectory and not the apparently u-shaped, quadratic pattern observed. What could account for the pattern of results seen in the AB data? During the first five weeks of the MORE intervention, participants were encouraged to decenter from their cognitive-emotional experience and become aware of whatever thoughts and feelings arose during the meditation sessions. Several mindfulness exercises involved imaginal alcohol exposure in order to teach methods to deal mindfully with craving. During these exercises, participants were encouraged to imagine having strong alcohol cravings and to notice the resultant physiological and affective reactivity. In addition, participants were asked to log daily experiences of craving and to carefully attend to the psychophysiological concomitants of the craving experience. Participation in these exercises may have activated alcohol use action schema, triggering implicit positive alcohol expectancies through the imagination of conditioned, hedonic stimuli, resulting in the deployment of a conditioned attentional response, i.e. increases in the 200 ms AB. As the mindfulness participants became more proficient at self-regulating attention and developing metacognitive awareness of automatic response patterns, this effect may have been attenuated by the post-intervention time point.
Conversely, by five weeks into the alcohol support group intervention, participants may have felt considerable pressure to conform to the culture of the group, which emphasized an abstinence-only attitude toward recovery from alcohol dependence. Group culture focused on the negative consequences of drinking, and the climate of the group was such that verbal pronouncements of one’s ability to resist the temptation to drink were reinforced via social influence, social norms, and/or social control. These discussions may have activated negative implicit alcohol expectancies and therefore attenuated the 200 ms AB. However, post-intervention, when the social support group was officially disbanded at the end of the 10-week intervention, the influence and norms afforded by the group culture were no longer in place. Without this social control element, appetitive tendencies towards alcohol may have been unchecked, and given the lack of skill acquisition in the support group, participants may have had no means of coping with implicit cognitive biases towards alcohol.
To determine the clinical significance of the small yet statistically significant change in 200 ms AB over time among MORE participants, post-intervention craving was regressed onto pre-post change in 200 ms AB for MORE participants with alcohol approach biases (N = 9). Pre-post change in 200 ms AB significantly predicted post-intervention craving, β = .79, p = .01, R-squared = .62. The finding that decreases in 200 ms AB over the course of mindfulness intervention predicted higher craving at the end of the intervention is counterintuitive. This seemingly paradoxical finding may be understood in light of Tiffany’s Cognitive Processing Model of Addiction (1990), which posits that conscious craving results from inhibition of automatized alcohol use action schema. The 200 ms AB has been considered an automatic, unconscious bias in initial attentional orienting towards alcohol-related stimuli (Field & Cox 2008). Stimuli presented for 200 ms are too fast for conscious deployment of attention; therefore, initial orienting to such stimuli may be driven by implicit appetitive processes that can detect and operate on nonconscious stimuli. According to Tiffany’s theory, when alcohol use action schemas operate in an unobstructed fashion, there is an absence of craving; however, interruption of automatic, appetitive cognitive-behavioral responses promotes craving.
Training in mindfulness meditation may lead to disruption of maladaptive, automatized cognitive-behavioral reactions. Deikman (1966) conceptualized the effect of meditation as a form of “deautomatization,” that is, an undoing of automatization whereby unconscious, habitual patterns of perception and motor behavior are reinvested with attention. It is plausible that during the course of the MORE intervention, automatized alcohol use action schema were deautomatized through formal and informal mindfulness practices, which involve the intentional and conscious direction of attention to cognitions, emotions, physiology, and behavior. Given that such conscious attentional processing disrupts automatic processing (Lieberman, 2003), mindfulness training may have interrupted alcohol use action schema, which Tiffany’s (1990) theory would predict to result in an increase in conscious craving. This prediction appears to have been borne out in the present data linking decreased automatic alcohol attentional bias to increased craving. This finding also is sensible in the context of the findings of Rohsenow and colleagues (1994), who found that that greater awareness of physiological reactivity during alcohol cue exposure predicted drinking among alcohol dependent men thrre months post-intervention while urge to drink was not a significant predictor of future drinking behavior. Increased awareness of craving-related reactivity may indicate that automatic addictive patterns have been disrupted, which may allow for the strategic deployment of self-regulatory mechanisms, eventuating in decreased drinking over time.
The identified effects of MORE on thought suppression also support a deautomatization interpretation of the correlation between mindfulness-induced reductions in 200 ms AB and higher post-intervention craving, and notably, among MORE participants, reductions in thought suppression were significantly correlated with decreases in 200 ms AB. Over time, mindfulness training may reduce to reduce the tendency to suppress one’s thoughts and feelings, thereby allowing cravings that had been previously suppressed to surface to consciousness. In so doing, automatic appetitive schema (indexed by 200 ms AB) which may have been operating unchecked by controlled cognitive processing during active suppression may become accessible to explicit cognitive control. Thus, as thought suppression decreases, controlled cognitive processing can be more effectively deployed to inhibit and counter appetitive responding (as evidenced by the significant correlation between decreases in thought suppression and decreases in impaired alcohol response inhibition), resulting in decreased attentional capture by alcohol cues coupled with the conscious experience of craving as alcohol use action schema are disrupted. Through mindfulness, alcohol urges can be attended to in a nonreactive, nonjudgmental fashion, obviating the need for suppression. In so doing, cravings may extinguish over time, instead of intensifying as a result of suppression attempts.
Alternatively, the counterintuitive relationship between decreased 200 ms AB and increased craving may be explained by the methodological issues that plague self-report measures of craving, such as lack of consensus on the operationalization of the construct, the temporal scope of the craving measurement, and inconsistency between psychological and physiological indices of craving (Monti, Rohsenow, & Hutchison 2000; Tiffany, Carter, & Singleton 2000). If awareness of craving increased after ten weeks of mindfulness training, differences in pre-post craving scores may be biased, leading to spurious correlations between change in craving and 200 ms AB. In contrast, performance on a dot probe task with alcohol stimuli presented for 200 ms latencies may be a more valid indicator of appetitive tendencies towards alcohol than self-reports of craving.
Limitations
The primary limitation of this study is its small sample size, which limits statistical power and generalizability of the findings. Generalizability of study findings may also be limited by the sample selection and the absence of random sampling - participants who had resided for at least 18 months in a TC self-selected into the study, and thus had been exposed to a therapeutic milieu for an unusually long length of time relative to a 28-day residential or intensive outpatient treatment format. Due to the probable high motivation and competence of participants who had successfully maintained sobriety for over 18 months while residing in the TC, MORE and ASG may have had greater salutary effects in this sample than in persons with less commitment or ability to change. Conversely, because persons who could not maintain sobriety for a substantial length of time (i.e., those who were most severely impaired or dependent) were not included in this study, intervention effects may have been underestimated for individuals who might have shown the greatest benefit from MORE or ASG. Another substantial limitation was that self-report measures were administered during face-to-face interviews, which may have led to social desirability bias in self-reported outcomes. Our interpretations of HRV data may be confounded because we were unable to control for the effects of respiration (Grossman & Taylor 2007), although there is ample debate in the literature regarding the need for such corrections (e.g., Denver, Reed, & Porges 2007). Given the presence of counterintuitive findings, this study needs to be replicated with a larger and more broadly representative sample, and additional research is needed to explore the clinical significance of the effect of mindfulness training on stress, thought suppression, HRV, and alcohol attentional bias. To that end, we are collecting follow-up data and will examine how intervention-related changes in these cognitive, affective, and physiological variables predict alcohol relapse.
By a three-month, post-intervention follow-up, few participants from either treatment group had relapsed. However, anecdotal reports suggested that mindfulness training was perceived to be useful for preventing stress-precipitated relapse. For example, one MORE participant who was transitioning out of the TC and had obtained employment at a restaurant that served alcohol reported that her practice of mindfulness helped her to cope with cravings when stressed on the job. During a follow-up interview, this participant stated,
“I had to practice it [mindfulness] every day, when I went out looking for a job, and being rejected, because of my not working in two years, using the techniques that were being taught to me, in my everyday life. Yeah, I use it every day… I work at Red Lobster, where they do serve alcohol, and it [mindfulness] played a very big part when I had to deal with some customers that were drinking. And, it played a big part in helping me get through it. I had to go outside and breathe. Well, by me using it every day, breathing, taking time to sit down and think about what I’m going to do before I react, not reacting on impulse. I was very self-destructive, and if something got in my way, I would hide behind the alcohol and the drugs to get past it, and so now instead of doing that, I take whatever time I need to sit down and collect my thoughts, and not stay in my head about nothing.”
Although event-history analyses are needed to determine whether MORE affects the rate and timing of relapse, such clinical anecdotes indicate that mindfulness training may reduce the occurrence of relapse in high risk situations.
Conclusion
In sum, the unwitting attempts of recovering alcohol dependent persons to suppress appetitive cognitive-emotional reactions towards alcohol may obscure these responses from consciousness only to perpetuate and intensify them within the cognitive unconscious. In the domain of unconscious mental life, automatic processes run smoothly and efficiently uninhibited by volitional control (Kihlstrom 1987). Hence, by shunting appetitive reactions into the unconscious, the alcohol dependent individual may increase the very appetitive response towards alcohol he or she is trying to suppress and exacerbate psychophysiological reactivity to alcohol cues. Mindfulness training may serve to undo this process, making unconscious responses conscious. Thus, practice of mindfulness may promote the recovery of alcohol dependent persons through: a) deautomatization of alcohol use action schema, resulting in diminished attentional bias towards subliminal alcohol cues and increased craving as a result of disrupted automaticity; and b) decreased thought suppression resulting in increased awareness of alcohol urges over time, increased HRV recovery from alcohol cue-exposure, and improved ability to inhibit appetitive responses.
Accordingly, mindfulness training may be a tractable means of promoting enduring behavior change. Although brief motivational interventions may be highly effective at impelling the desire towards sobriety, participants of such motivational enhancement therapies remain prone to eventual relapse; indeed, relapse is often a part of the recovery process. As such, interventions that consolidate short-term treatment gains into broader lifestyle change are of major significance to the addictions treatment field. During the gradual practice of mindfulness, one learns to work with negative emotions in a metacognitive context, resulting in nonreactivity to difficult mental contents and improved self-regulation in the face of stressors. The developmental process of cultivating and embedding mindfulness principles into all aspects of one’s life may solidify gains made in prior treatment and provide an effective, long-term approach to coping with stress-precipitated relapse.
Despite evidence suggesting that stress appraisal and attentional biases are key components of alcohol dependence, the form of addictions treatment most available to poor and marginalized persons, social support groups, does not target these pathogenic mechanisms directly. In contrast, practice of mindfulness may attenuate stress reactivity and thought suppression while disrupting addictive automaticity, resulting in increased awareness of craving and greater ability to cope with and recover from alcohol urges in stressful contexts. Hence, mindfulness training may hold promise as an alternative, targeted treatment for stress-precipitated alcohol dependence among vulnerable members of society.
Contributor Information
Eric L. Garland, Florida State University, College of Social Work.
Susan A. Gaylord, University of North Carolina – Chapel Hill, School of Medicine, Department of Physical Medicine & Rehabilitation - Program on Integrative Medicine
Charlotte A. Boettiger, University of North Carolina – Chapel Hill, Department of Psychology, Biomedical Research Imaging Center, Bowles Center for Alcohol Studies, Curriculum in Neurobiology.
Matthew O. Howard, University of North Carolina – Chapel Hill, School of Social Work
References
- Baer RA, Krietemeyer J. Overview of mindfulness- and acceptance-based treatment approaches. In: Baer RA, editor. Mindfulness-based treatment approaches: Clinician’s guide to evidence base and applications. Boston, MA: Elsevier; 2006. pp. 1–27. [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Borkovec T, Nau S. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry. 1972;3(4):257–260. [Google Scholar]
- Bowen S, Witkiewitz K, Dillworth TM, Marlatt GA. The role of thought suppression in the relationship between mindfulness meditation and alcohol use. Addict Behav. 2007 doi: 10.1016/j.addbeh.2007.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler EA, Wilhelm FH, Gross JJ. Respiratory sinus arrhythmia, emotion, and emotion regulation during social interaction. Psychophysiology. 2006;43(6):612–622. doi: 10.1111/j.1469-8986.2006.00467.x. [DOI] [PubMed] [Google Scholar]
- Carter BL, Tiffany ST. Meta-analysis of cue-reactivity in addiction research. Addiction. 1999;94(3):327–340. [PubMed] [Google Scholar]
- Christenfeld N, Gerin W. Social support and cardiovascular reactivity. Biomedicine and Pharmacotherapy. 2000;54(5):251–257. doi: 10.1016/S0753-3322(00)80067-0. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health, Society, and Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100(3):281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Korten A, Jablensky A. Use of a brief screening instrument for psychosis: Results of an ROC analysis. New South Wales, Australia: National Drug and Alcohol Research Centre (NDARC); 2005. Technical Report No. 210. [Google Scholar]
- Deikman AJ. Deautomatization and the mystic experience. Psychiatry. 1966;29:324–388. doi: 10.1080/00332747.1966.11023476. [DOI] [PubMed] [Google Scholar]
- Denver JW, Reed SF, Porges SW. Methodological issues in the quantification of respiratory sinus arrhythmia. Biological Psychology. 2007;74(2):286–294. doi: 10.1016/j.biopsycho.2005.09.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological Medicine. 1983;13(3):595–605. [PubMed] [Google Scholar]
- Field M, Cox WM. Attentional bias in addictive behaviors: a review of its development, causes, and consequences. Drug and Alcohol Dependence. 2008;97(1–2):1–20. doi: 10.1016/j.drugalcdep.2008.03.030. [DOI] [PubMed] [Google Scholar]
- Field M, Eastwood B. Experimental manipulation of attentional bias increases the motivation to drink alcohol. Psychopharmacology (Berl) 2005;183(3):350–357. doi: 10.1007/s00213-005-0202-5. [DOI] [PubMed] [Google Scholar]
- Field M, Mogg K, Zetteler J, Bradley BP. Attentional biases for alcohol cues in heavy and light social drinkers: the roles of initial orienting and maintained attention. Psychopharmacology (Berl) 2004;176(1):88–93. doi: 10.1007/s00213-004-1855-1. [DOI] [PubMed] [Google Scholar]
- Field M, Powell H. Stress increases attentional bias for alcohol cues in social drinkers who drink to cope. Alcohol and Alcoholism. 2007;42(6):560–566. doi: 10.1093/alcalc/agm064. [DOI] [PubMed] [Google Scholar]
- Flannery BA, Roberts AJ, Cooney N, Swift RM, Anton RF, Rohsenow DJ. The role of craving in alcohol use, dependence, and treatment. Alcoholism: Clinical and Experimental Research. 2001;25(2):299–308. [PubMed] [Google Scholar]
- Garland EL. The meaning of mindfulness: A second-order cybernetics of stress, metacognition, and coping. Complementary Health Practice Review. 2007;12(1):15–30. [Google Scholar]
- Garland EL, Boettiger CA, Howard MO. Targeting cognitive-affective risk mechanisms in stress-precipitated alcohol dependence: An integrated, biopsychosocial model. doi: 10.1016/j.mehy.2011.02.014. (Under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Boettiger CA, Gaylord SA, West Chanon VM, Howard MO. Mindfulness is inversely associated with alcohol attentional bias among recovering alcohol-dependent adults. doi: 10.1007/s10608-011-9378-7. (Under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ. Emotion regulation: affective, cognitive, and social consequences. Psychophysiology. 2002;39(3):281–291. doi: 10.1017/s0048577201393198. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Levenson RW. Emotional suppression: physiology, self-report, and expressive behavior. Journal of Personality and Social Psychology. 1993;64(6):970–986. doi: 10.1037//0022-3514.64.6.970. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. Journal of Psychosomatic Research. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Grossman P, Taylor EW. Toward understanding respiratory sinus arrhythmia: relations to cardiac vagal tone, evolution and biobehavioral functions. Biological Psychology. 2007;74(2):263–285. doi: 10.1016/j.biopsycho.2005.11.014. [DOI] [PubMed] [Google Scholar]
- Guardia J, Trujols J, Burguete T, Luquero E, Cardus M. Impaired response inhibition scale for alcoholism (IRISA): development and psychometric properties of a new scale for abstinence-oriented treatment of alcoholism. Alcoholism: Clinical and Experimental Research. 2007;31(2):269–275. doi: 10.1111/j.1530-0277.2006.00314.x. [DOI] [PubMed] [Google Scholar]
- Hansen AL, Johnsen BH, Thayer JF. Vagal influence on working memory and attention. International Journal of Psychophysiology. 2003;48(3):263–274. doi: 10.1016/s0167-8760(03)00073-4. [DOI] [PubMed] [Google Scholar]
- Ingjaldsson JT, Laberg JC, Thayer JF. Reduced heart rate variability in chronic alcohol abuse: relationship with negative mood, chronic thought suppression, and compulsive drinking. Biological Psychiatry. 2003;54(12):1427–1436. doi: 10.1016/s0006-3223(02)01926-1. [DOI] [PubMed] [Google Scholar]
- Jha A, Krompinger J, Baime M. Mindfulness training modifies subsystems of attention. Cognitive, Affective, and Behavioral Neuroscience. 2007;7(2):109–119. doi: 10.3758/cabn.7.2.109. [DOI] [PubMed] [Google Scholar]
- Key BL, Campbell TS, Bacon SL, Gerin W. The influence of trait and state rumination on cardiovascular recovery from a negative emotional stressor. Journal of Behavior Medicine. 2008;31(3):237–248. doi: 10.1007/s10865-008-9152-9. [DOI] [PubMed] [Google Scholar]
- Kihlstrom JF. The cognitive unconscious. Science. 1987;237(4821):1445–1452. doi: 10.1126/science.3629249. [DOI] [PubMed] [Google Scholar]
- Koob GF. Alcoholism: allostasis and beyond. Alcoholism: Clinical and Experimental Research. 2003;27(2):232–243. doi: 10.1097/01.ALC.0000057122.36127.C2. [DOI] [PubMed] [Google Scholar]
- Lieberman MD. Reflective and reflexive judgment processes: A social cognitive neuroscience approach. In: Forgas JP, Williams K, Hippel WV, editors. Social judgments: Implicit and explicit processes. New York: Cambridge University Press; 2003. pp. 44–67. [Google Scholar]
- Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300(11):1350–1352. doi: 10.1001/jama.300.11.1350. [DOI] [PubMed] [Google Scholar]
- Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends in Cognitive Sciences. 2008;12(4):163–169. doi: 10.1016/j.tics.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLeod C, Mathews A, Tata P. Attentional biases in emotional disorders. Journal of Abnormal Psychology. 1986;95:15–20. doi: 10.1037//0021-843x.95.1.15. [DOI] [PubMed] [Google Scholar]
- Marcus MT, Fine M, Kouzekanani K. Mindfulness-based meditation in a therapeutic community. Journal of Substance Use. 2001;5:303–311. [Google Scholar]
- Marcus MT, Fine M, Moeller G, Khan MM, Pitts K, Swank PR, et al. Change in stress levels following mindfulness-based stress reduction in a therapeutic community. Addictive Disorders and their Treatment. 2003;2:63–68. [Google Scholar]
- Monti PM, Rohsenow DJ, Hutchison KE. Toward bridging the gap between biological, psychobiological and psychosocial models of alcohol craving. Addiction, 95 Supplement. 2000;2:S229–236. doi: 10.1080/09652140050111799. [DOI] [PubMed] [Google Scholar]
- Muraven M, Collins RL, Nienhaus K. Self-control and alcohol restraint: an initial application of the self-control strength model. Psychology of Addictive Behaviors. 2002;16(2):113–120. doi: 10.1037//0893-164x.16.2.113. [DOI] [PubMed] [Google Scholar]
- Muraven M, Shmueli D. The self-control costs of fighting the temptation to drink. Psychology of Addictive Behaviors. 2006;20(2):154–160. doi: 10.1037/0893-164X.20.2.154. [DOI] [PubMed] [Google Scholar]
- Noel X, Colmant M, Van Der Linden M, Bechara A, Bullens Q, Hanak C, et al. Time course of attention for alcohol cues in abstinent alcoholic patients: the role of initial orienting. Alcoholism: Clinical and Experimental Research. 2006;30(11):1871–1877. doi: 10.1111/j.1530-0277.2006.00224.x. [DOI] [PubMed] [Google Scholar]
- Palfai TP, Monti PM, Colby SM, Rohsenow DJ. Effects of suppressing the urge to drink on the accessibility of alcohol outcome expectancies. Behaviour Research and Therapy. 1997;35(1):59–65. doi: 10.1016/s0005-7967(96)00079-4. [DOI] [PubMed] [Google Scholar]
- Peressutti C, Martin-Gonzalez JMJMG-M, Mesa D. Heart rate dynamics in different levels of Zen meditation. International Journal of Cardiology. 2009 doi: 10.1016/j.ijcard.2009.06.058. [DOI] [PubMed] [Google Scholar]
- Purdon C. Thought suppression and psychopathology. Behaviour Research and Therapy. 1999;37(11):1029–1054. doi: 10.1016/s0005-7967(98)00200-9. [DOI] [PubMed] [Google Scholar]
- Rawson R, McCann MJ. C. f. S. A. Treatment. DHHS Publication No. (SMA) 06–4152. 2006. Counselor’s Treatment Manual: Matrix Intensive Outpatient Treatment for People With Stimulant Use Disorders. [Google Scholar]
- Rogers C. Client-centered therapy: Its current practice, implications, and theory. New York: Constable; 2003. [Google Scholar]
- Rohsenow DJ, Monti PM, Rubonis AV, Sirota AD, Niaura RS, Colby SM, et al. Cue reactivity as a predictor of drinking among male alcoholics. Journal of Consulting and Clinical Psychology. 1994;62(3):620–626. doi: 10.1037//0022-006x.62.3.620. [DOI] [PubMed] [Google Scholar]
- Schroder KE, Perrine MW. Covariations of emotional states and alcohol consumption: evidence from 2 years of daily data collection. Soc Sci Med. 2007;65(12):2588–2602. doi: 10.1016/j.socscimed.2007.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal Z, Williams JM, Teasdale JD. Mindfulness-based cognitive therapy for depression. New York: The Guilford Press; 2002. [Google Scholar]
- Segerstrom SC, Nes LS. Heart rate variability reflects self-regulatory strength, effort, and fatigue. Psychological Science. 2007;18(3):275–281. doi: 10.1111/j.1467-9280.2007.01888.x. [DOI] [PubMed] [Google Scholar]
- Sinha R. The role of stress in addiction relapse. Current Psychiatry Reports. 2007;9(5):388–395. doi: 10.1007/s11920-007-0050-6. [DOI] [PubMed] [Google Scholar]
- Stormark KM, Field NP, Hugdahl K, Horowitz M. Selective processing of visual alcohol cues in abstinent alcoholics: an approach-avoidance conflict? Addictive Behaviors. 1997;22(4):509–519. doi: 10.1016/s0306-4603(96)00051-2. [DOI] [PubMed] [Google Scholar]
- Tang YY, Ma Y, Fan Y, Feng H, Wang J, Feng S, et al. Central and autonomic nervous system interaction is altered by short-term meditation. Proceedings of the National Academy of Sciences U S A. 2009;106(22):8865–8870. doi: 10.1073/pnas.0904031106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders. 2000;61(3):201–216. doi: 10.1016/s0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Lane RD. Claude Bernard and the heart-brain connection: further elaboration of a model of neurovisceral integration. Neuroscience and Biobehavioral Reviews. 2009;33(2):81–88. doi: 10.1016/j.neubiorev.2008.08.004. [DOI] [PubMed] [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychological Review. 1990;97(2):147–168. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- Tiffany ST, Carter BL, Singleton EG. Challenges in the manipulation, assessment and interpretation of craving relevant variables. Addiction, 95 Supplement. 2000;2:S177–187. doi: 10.1080/09652140050111753. [DOI] [PubMed] [Google Scholar]
- Townshend JM, Duka T. Avoidance of alcohol-related stimuli in alcohol-dependent inpatients. Alcoholism: Clinical and Experimental Research. 2007;31(8):1349–1357. doi: 10.1111/j.1530-0277.2007.00429.x. [DOI] [PubMed] [Google Scholar]
- Wegner DM, Schneider DJ, Carter SR, 3rd, White TL. Paradoxical effects of thought suppression. Journal of Personality and Social Psychology. 1987;53(1):5–13. doi: 10.1037//0022-3514.53.1.5. [DOI] [PubMed] [Google Scholar]
- Wegner DM, Zanakos S. Chronic thought suppression. Journal of Personality. 1994;62(4):616–640. doi: 10.1111/j.1467-6494.1994.tb00311.x. [DOI] [PubMed] [Google Scholar]
- Wenk-Sormaz H. Meditation can reduce habitual responding. Alternative Therapies: Health and Medicine. 2005;11(2):42–58. [PubMed] [Google Scholar]
- Wenzlaff RM, Wegner DM. Thought suppression. Annual Review of Psychology. 2000;51:59–91. doi: 10.1146/annurev.psych.51.1.59. [DOI] [PubMed] [Google Scholar]
- Valdez GR, Koob GF. Allostasis and dysregulation of corticotropin-releasing factor and neuropeptide Y systems: implications for the development of alcoholism. Pharmacology, Biochemistry, and Behavior. 2004;79(4):671–689. doi: 10.1016/j.pbb.2004.09.020. [DOI] [PubMed] [Google Scholar]
- Zgierska A, Rabago D, Zuelsdorff M, Coe C, Miller M, Fleming M. Mindfulness meditation for alcohol relapse prevention: A feasibility pilot study. Journal of Addiction Medicine. 2008;2(3):165–173. doi: 10.1097/ADM.0b013e31816f8546. [DOI] [PMC free article] [PubMed] [Google Scholar]