Abstract
The equivalency of behavioral interventions has led to the consideration of whether patient related factors influence clinical trial outcomes. The primary purpose of this secondary analysis was to determine if treatment preference and patient expectation were predictors of trial outcomes and if selected patient satisfaction items were appropriate as outcome measures. Perceived effectiveness, treatment preference and patient expectation were assessed before random assignment, and patient satisfaction was assessed 6-months later. Patient preference was associated with perceived effectiveness for those with no treatment preference and those preferring graded exposure. Higher patient expectation was associated with higher perceived effectiveness ratings for all treatments in the clinical trial. Patients with no strong treatment preferences had larger 6-month improvements in pain intensity and disability, while patients with higher expectations had lower disability at baseline, 4-weeks, and 6-months. Patient satisfaction rates did not differ based on treatment received. Patient satisfaction was highest with treatment delivery, and much lower with treatment effect. Patient satisfaction was uniformly associated with expectations being met, but only satisfaction with treatment effect was associated with lower pain and disability scores. These data support assessment of treatment preference and patient expectation as predictors and patient satisfaction as an outcome measure in LBP clinical trials.
Introduction
Conservative interventions often have equivalent effects for patients with low back pain (LBP). Specific to the purposes of the current study, individual clinical trials have highlighted the effectiveness of behavioral interventions for LBP, 12,18,21,22,29,30,36,43 but there are also numerous null trials for behavioral interventions.19,38,42 Reviews for behavioral interventions reflect this ambiguity, with a Cochrane review for chronic LBP indicating no additional benefit from behavioral treatment in comparison to exercise or other usual treatments.39 In contrast, a clinical practice guideline from the American College of Physicians and American Pain Society includes cognitive and behavioral therapies as a recommended treatment for chronic LBP.3 The equivalency of behavioral interventions for LBP has led to the consideration of whether patient related factors influence clinical trial outcomes.
Preference and expectation are factors that have been explored for their influence on outcomes in LBP clinical trials. Preference could potentially influence outcome by preventing individuals with strong treatment preferences from ever enrolling in trials or by having individuals receive unmatched treatment after randomization.11,45,46 A working hypothesis for those enrolled in trials is that receiving unmatched treatment has a greater probability of experiencing worse outcomes in comparison to those receiving matched treatment.11,45,46 Expectation refers to the beliefs the patient has regarding the potential benefit of the treatment and can be measured in either general terms of outcome or as it relates to a specific intervention.40 The importance of expectation for LBP clinical trials has been highlighted as higher pre-treatment expectations were predictive of improved outcomes in previous pain studies.32,23,26,27,4,37,28
Preference and expectation are predictors of interest, while patient satisfaction has been highlighted as an important outcome measure for clinical trials of LBP. Assessment of satisfaction provides patient perspective on the treatment episode as a compliment to traditional outcome measures (e.g. pain intensity and disability). Previous studies suggest patient satisfaction is a multidimensional construct, consisting of satisfaction related to treatment delivery and satisfaction related to treatment effects.2,16,13,20 Interestingly, previous studies suggest that satisfaction with treatment delivery is frequently quite high, while satisfaction with treatment effects is lower.13,20,7,33,49 Therefore, it may be important to separately assess satisfaction with treatment delivery and treatment effects when determining clinical outcomes.
The current study is a secondary analysis of preference, expectation, and satisfaction for individuals participating in a randomized trial of behavioral physical therapy interventions for acute and sub-acute LBP.14 Treatment preference and patient expectation were assessed at baseline and used as predictors. We hypothesized that patients with matched treatment preference (i.e. randomly assigned to their preferred treatment) would have a) higher perceived effectiveness ratings for their preferred treatment and b) better pain and disability outcomes in comparison to those with unmatched treatment preference. We further hypothesized that patients with higher treatment expectations (i.e. expecting greater symptom relief) would have a) higher perceived effectiveness ratings for all treatments and b) better pain and disability outcomes in comparison to those with lower general treatment expectation. Satisfaction was assessed at 6-month follow-up and was used as an outcome measure. We determined if satisfaction rates differed based on a) type of treatment received in the trial and b) whether the focus was on treatment delivery or treatment effect. We hypothesized that similar satisfaction rates would be observed for each treatment group and that patients would rate satisfaction with treatment delivery higher than treatment effect. We also determined what factors differentiated between satisfied and unsatisfied individuals. From our previous work, we hypothesized that satisfaction with treatment delivery would be associated with expectation being met, while satisfaction with treatment effect would be associated with expectation being met and lower pain and disability scores13
Materials and Methods
Overview
This study was a planned secondary analysis of a randomized trial comparing physical therapy to physical therapy supplemented with graded activity or graded exposure for patients with acute and sub-acute LBP.14 The study was conducted at the University of Florida and affiliated outpatient physical therapy clinics. The study was approved by the University of Florida Institutional Review Board, and all subjects provided informed consent before participating in this study.
Subjects
Inclusion and exclusion criteria were based on guidelines from the Quebec Task Force on Spinal Disorders (QTFSD).41 For purposes of this study acute and sub-acute LBP were operationally defined as reporting current symptoms for 1 – 24 weeks and chronic LBP was defined as reporting current symptoms for greater than 24 weeks. Consecutive patients seeking treatment for LBP at University of Florida affiliated clinics were recruited and screened for eligibility. Inclusion criteria were patients aged between 15 and 60 with acute/sub-acute LBP with or without radiating symptoms. Patients had to have the ability to read and speak English because of the number of questionnaires. Exclusion criteria were patients with chronic LBP, signs of nerve root compression, lumbar spinal stenosis, and post-operative lumbar spine surgery. Patients were also excluded for pregnancy, osteoporosis, and spinal disorders related to metastatic disease, visceral disease, or fracture.
Intervention
Patients that met the eligibility criteria provided informed consent and were then treated for 4-weeks by licensed physical therapists according to their random assignment of physical therapy alone, physical therapy with graded activity, or physical therapy with graded exposure. Patients were re-assessed by a blinded evaluator 4-weeks after randomization and completed mail follow up for self-report questionnaires at 6-months. The primary analysis of the trial indicated no differences at 4-weeks or 6-months for the primary outcome measures.14 Therefore, patients were analyzed as a single cohort for this study, unless otherwise indicated.
Measures
Perceived effectiveness
Patient rating of perceived effectiveness for each treatment was obtained using a numerical rating scale (NRS) ranging from “0” (not at all effective) to “100” (most effective possible). Patients separately rated the effectiveness of physical therapy, physical therapy with graded activity, and physical therapy with graded exposure prior to random assignment.
Treatment preference
Preference was assessed categorically by having the patient indicate which treatment they would prefer if given the choice.11,45,46 Patients were also given the option of selecting “no strong preference for any treatment”. Preference selection was made before treatment randomization, resulting in 3 possible categories after randomization had occurred – matched treatment preference, unmatched treatment preference, and no treatment preference. These 3 categories were used as variables in the subsequent data analysis.
Patient expectation
Patient expectation of complete symptom relief was rated using 2 selected individual items from a LBP outcome assessment tool.5 At baseline patients rated their expectations for complete symptom relief (1 – “Not at all likely” to 5 – “Extremely likely”). Patients indicating symptom relief was “extremely likely” or “very likely” were categorized in the higher expectation group, while all other responses were categorized in the lower expectation group. At 6-months patients rated whether their expectations for symptom relief had been met (1 – “Definitely not” to 5 – “Definitely yes”).
Patient satisfaction
At 6-months patient satisfaction was assessed via patient response to 3 items from the aforementioned LBP outcome assessment tool.5 The first item was “Would you have the same physical therapy treatment again if you had the same condition?” (1 – “Definitely not” to 5 – “Definitely yes”). The second item was “How would you rate the overall results of your physical therapy treatment for your back or leg pain?” (1 – “Terrible” to 6 – “Excellent”). The third item was “If you had to spend the rest of your life with the symptoms you have right now, how would you feel about it?” (1 –“Very dissatisfied” to 5 – “Very satisfied”). Patients indicating 6-month satisfaction higher than the neutral rating were categorized as “satisfied” while those rating neutral or lower were categorized as “unsatisfied.” Our previous work has indicated that the first 2 items were indicative of satisfaction with treatment delivery, while the third item was indicative of satisfaction with treatment effect.13
Pain intensity
Patients rated their pain intensity using an NRS ranging from “0” (no pain) to “10” (worst pain imaginable).24 Patients rated pain intensity over 3 conditions, the present pain intensity, the worst pain intensity over the past 24 hours, and the best pain intensity over the past 24 hours. These 3 ratings were summed and divided by 3 (arithmetic mean) for use in data analyses.25
Disability
Disability was assessed with the Oswestry Disability Questionnaire (ODQ), which has been recommended as appropriate outcome measure for self-report of disability.8,9 The ODQ has 10 items that assess how LBP affects common daily activities, for example sitting, standing, and lifting. The ODQ has a range of 0 (no disability due to back pain) to 100 (completely disabled due to back pain), so higher scores indicate higher disability from LBP.
Data Analysis
Descriptive analyses were generated and reported in the appropriate metric for continuous and categorical variables. The analyses for comparing baseline effectiveness ratings based on treatment preference category and expectation ratings involved separate repeated measures ANOVA models. These models had treatment preference or patient expectation as the between group factor, type of treatment as the within subjects factor, and perceived effectiveness ratings as the dependent variable. The analysis for the influence of treatment preference category and patient expectation ratings on pain intensity and disability also involved separate repeated measures ANOVA models. These models had treatment preference category or patient expectation rating as the between group factor, time (baseline, 4-week, and 6-months) as the within subjects factor, and pain intensity or disability scores as the dependent variable. Satisfaction at 6-months based on treatment received was investigated with chi-square analyses. Individuals satisfied at 6-months were compared to unsatisfied individuals by independent t-test on pain intensity, disability, and whether treatment expectations had been met.
Results
Descriptive statistics for this sample are reported in Table 1. Baseline data was used for the effectiveness rating analyses (n = 105), while the subsequent analyses were limited to those subjects providing complete 6-month data (n = 72). There were no statistical differences between those providing 6-month data and those not for age, sex, baseline pain intensity ratings, and baseline disability scores (Table 1). Specific to the purposes of this paper, there were also no baseline differences for perceived effectiveness ratings, treatment preference, or patient expectation for those providing 6-month data and those not (Table 1).
Table 1.
Baseline Characteristics for Subjects Included in this Analysis
| Variable | Total Sample (n = 105) |
6-Month Data (n = 72) |
No 6-Month Data (n = 33) |
p-value |
|---|---|---|---|---|
| Age* | 37.2 (14.5) | 38.6 (14.8) | 34.1 (13.4) | 0.136 |
| Sex^ (# of female subjects) |
69 | 50 | 19 | 0.172 |
| Prior history of LBP^ (# with prior history) |
66 | 46 | 20 | 0.353 |
| Leg pain with LBP^ (# with leg pain) |
46 | 30 | 16 | 0.876 |
| Duration of LBP^ (# of weeks present episode) |
7.5 (6.1) | 7.1 (6.1) | 8.3 (6.2) | 0.323 |
| Pain intensity (0 – 10 NRS) |
4.7 (2.1) | 4.7 (2.1) | 4.8 (2.0) | 0.710 |
| Disability (0 – 100 ODQ score) |
29.5 (16.2) | 29.3 (15.1) | 29.9 (18.4) | 0.835 |
| Perceived Effectiveness | ||||
| Physical therapy only (0 – 100 NRS) |
83.5 (16.6) | 83.3 (17.6) | 84.0 (14.1) | 0.840 |
| Graded activity (0 – 100 NRS) |
85.7 (16.0) | 84.5 (17.2) | 88.5 (12.8) | 0.252 |
| Graded exposure (0 – 100 NRS) |
79.4 (20.8) | 78.8 (21.0) | 81.3 (20.4) | 0.593 |
| Treatment Preference* | 0.461 | |||
| Physical therapy only | 18 | 10 | 8 | |
| Graded activity | 39 | 28 | 11 | |
| Graded exposure | 7 | 1 | 6 | |
| No preference | 39 | 26 | 13 | |
| Patient Expectation | 0.532 | |||
| High expectation | 82 | 55 | 27 | |
| Low expectation | 23 | 17 | 6 |
All values are reported as mean (standard deviation) or number
P-values are comparison of those providing 6-month follow-up and those not providing 6-month follow-up (t-tests for continuous data and chi-square for categorical data)
LBP = low back pain, NRS = numeric rating scale, ODQ = Oswestry Disability Questionnaire
2 with missing data
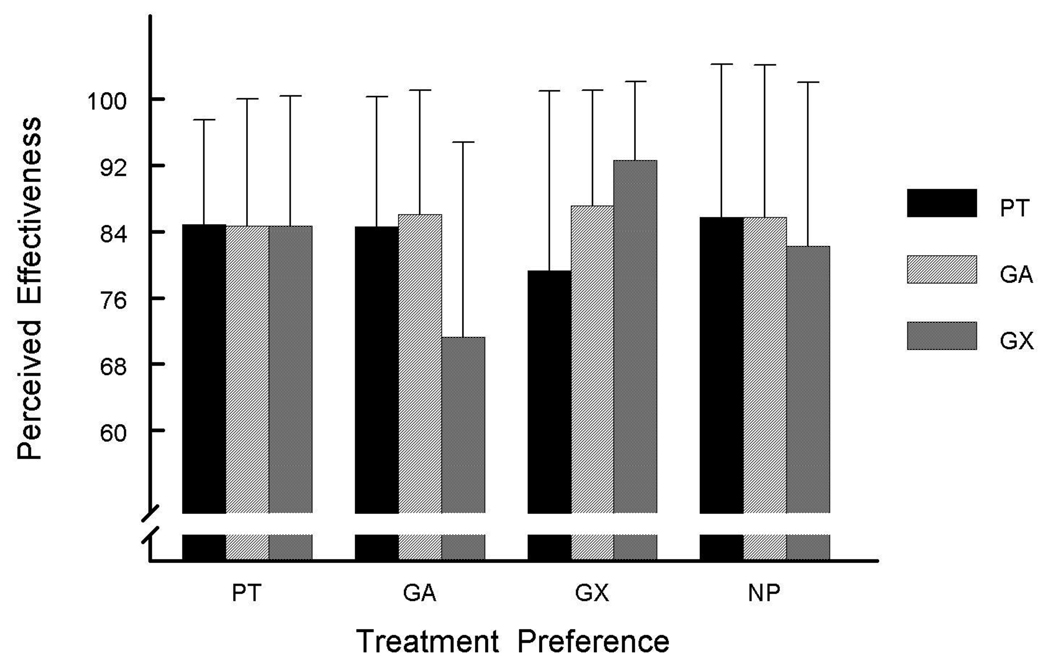
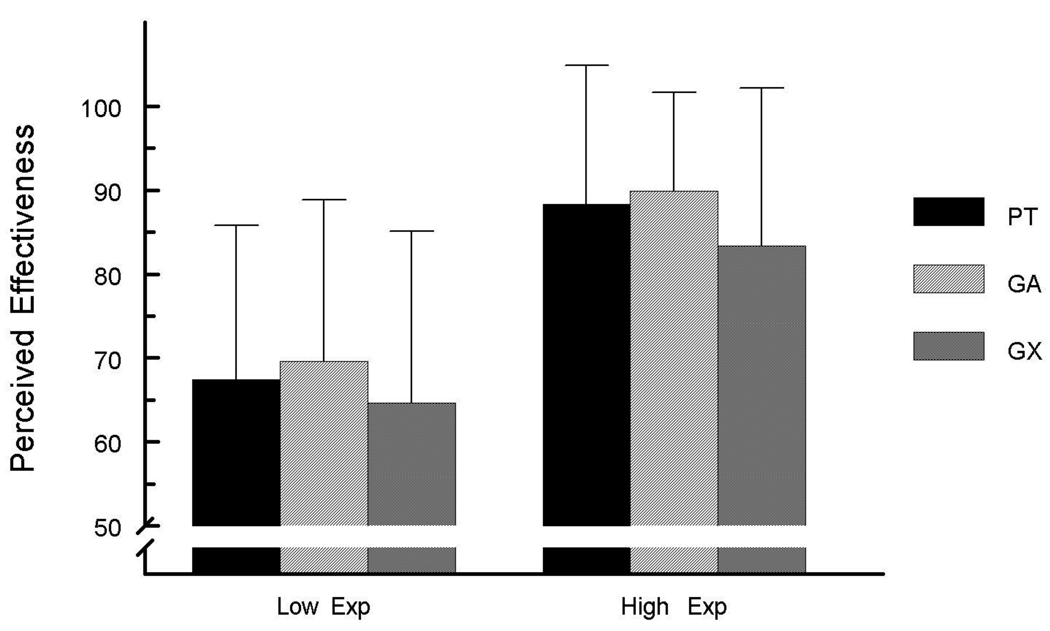
Perceived effectiveness
There was a group × type of treatment interaction for perceived effectiveness ratings (F6,178 = 4.6, p < 0.01) in the treatment preference model (Figure 1). The nature of the interaction was that patients indicating preference for physical therapy alone or no treatment strong preference had statistically similar effectiveness ratings across the 3 treatment options. Patients indicating preference for graded activity had similar perceived effectiveness ratings for physical therapy alone and graded activity, with significantly lower effectiveness ratings for graded exposure. Patients indicating preference for graded exposure had highest effectiveness ratings for graded exposure, with lower ratings for graded activity and physical therapy alone. There was no group × type of treatment interaction for perceived effectiveness ratings (F2, 186 = 0.1, p = 0.91) in the patient expectation model (Figure 2). However, there was a significant between group main effect (F1, 93 = 38.7, p < 0.01) indicating higher patient expectation was related with higher perceived effectiveness ratings for all treatment categories.
Figure 1. Perceived Effectiveness Ratings Based on Treatment Preference.
Figure Key
Y-axis indicates perceived effectiveness rating of treatment (0 – 100)
PT = physical therapy, GA = physical therapy with graded activity, GX = physical therapy with graded exposure, and NP = no strong treatment preference
Error bars = 1 standard deviation
Figure 2. Perceived Effectiveness Ratings Based on Patient Expectation.
Figure Key
Y-axis indicates perceived effectiveness rating of treatment (0 – 100)
Low Exp = low expectation of symptom relief, High Exp = high expectation of symptom relief, PT = physical therapy, GA = physical therapy with graded activity, GX = physical therapy with graded exposure, and NP = no strong treatment preference
Error bars = 1 standard deviation
Treatment preference
There were group × time interactions for the treatment preference models for pain intensity (F4,134 = 3.2, p = 0.02) and disability (F4,134 = 3.6, p < 0.01). The nature of the interaction was such that patients with no treatment preference had the largest 6-month improvements for pain intensity and disability scores. In contrast, patients with matched and unmatched treatment preference had similar 4-week and 6-month improvements for pain intensity and disability scores (Table 2).
Table 2.
Treatment Preference and Patient Expectation Influence on Pain Intensity and Disability
| Outcome Measure |
Preference Group |
Baseline | 4-Weeks | 6-Months | 6-Month Change |
|---|---|---|---|---|---|
| NRS# (0 – 10) |
Unmatched (n = 32) |
4.2 (2.1) | 2.1 (1.8) | 2.0 (1.9) | 2.3 (1.9) |
| Matched (n = 14) |
4.1 (2.0) | 1.9 (1.9) | 1.7 (1.9) | 2.6 (2.2) | |
| No Strong (n = 26) |
5.3 (2.1) | 2.1 (1.9) | 1.1 (1.7) | 4.2 (2.2)* | |
| ODQ# (0 – 100) |
Unmatched (n = 32) |
26.7 (12.0) | 17.4 (13.2) | 13.1 (13.2) | 13.3 (9.0) |
| Matched (n = 14) |
27.1 (12.8) | 13.7 (11.3) | 15.5 (13.5) | 11.7 (13.2) | |
| No Strong (n = 26) |
32.7 (18.3) | 13.5 (13.0) | 8.3 (10.5) | 24.4 (19.0)* | |
|
Outcome Measure |
Expectation Group |
Baseline | 4-Weeks | 6-Months |
6-Month Change |
| NRS (0 – 10) |
Low (n = 17) |
4.7 (2.1) | 2.3 (1.9) | 1.9 (1.6) | 2.8 (2.5) |
| High (n = 55) |
4.6 (2.1) | 2.0 (1.8) | 1.5 (1.8) | 3.1 (2.2) | |
| ODQ^ (0 – 100) |
Low (n = 17) |
33.9 (19.3) | 21.5 (15.0) | 15.9 (12.0) | 18.0 (20.1) |
| High (n = 55) |
27.4 (12.9) | 13.2 (11.4) | 10.4 (12.4) | 16.7 (13.2) | |
All values reported as mean (standard deviation) for completers of trial only
NRS - Numerical Rating Scale for pain intensity, ODQ - Oswestry Disability Questionnaire
Statistically significant interaction for 6-month improvement (p < 0.05)
Statistically significant between group effect (p < 0.05)
Larger 6-month improvement (p < 0.05)
Patient expectation
There were no group × time interactions for the patient expectation models for pain intensity (F2,136 =0.1, p = 0.92) and disability (F2,136 = 0.3, p = 0.77). For pain intensity there was a large main effect for 6-month improvement in pain intensity (F2,136 = 53.7, p < 0.01) with no group difference based on higher or lower expectation ratings (F1,68 = 0.5, p = 0.49). For disability there was a large main effect for 6-month improvement in disability (F2,136 = 42.2, p < 0.01). There was also a main effect for higher and lower expectation ratings (F1,68 = 5.5, p = 0.02). Patients with higher treatment expectations had lower disability scores at baseline, 4-weeks, and 6-months (Table 2).
Patient satisfaction
The treatment delivery items resulted in higher satisfaction ratings, with 90.3% indicating they would select the same treatment again and 87.5% indicating satisfaction with overall treatment results. In contrast, the treatment effect item was associated with a lower satisfaction rate, with only 45.8% indicating satisfaction with current symptoms for rest of life. Furthermore, patient satisfaction rates did not differ based on treatment received (Table 3). All treatment groups reported high satisfaction on the treatment delivery items (86% – 96%), while simultaneously reporting lower satisfaction on the treatment effect item (36% – 50%). Patients satisfied with treatment delivery were more likely to have had expectations met (p < 0.05), but had similar levels of 6-month pain intensity and disability scores (p > 0.05). In contrast, patients satisfied with the treatment effect were more likely to have had expectations met and also reported lower 6-month pain intensity and disability scores (p < 0.05).
Table 3.
6-Month Satisfaction Rates for Patients Participating in Behavioral Physical Therapy Interventions Clinical Trial
| Physical Therapy |
Physical Therapy with Graded activity |
Physical Therapy with Graded Exposure |
p-value | |
|---|---|---|---|---|
| Follow-up completed | 26 (77%) | 22 (63%) | 24 (73%) | .439 |
| Would select same treatment again^ |
24 (92%) | 20 (91%) | 21 (88%) | .842 |
| Overall rating of positive treatment effect^ |
23 (89%) | 19 (86%) | 21 (88%) | .976 |
| Satisfied with symptoms if present rest of life* |
13 (50%) | 8 (36%) | 12 (50%) | .564 |
Significance across treatment groups tested with chi-square test
Response related to satisfaction with treatment delivery
Response related to satisfaction with treatment effect
Discussion
This study was a planned secondary analysis of a clinical trial for physical therapy supplemented with behavioral interventions for acute and sub-acute LBP.14 Preference and expectation have been previously cited as potentially important influences for LBP clinical trials.26,17,37,10 The current study adds to the existing literature by investigating these factors in a clinical trial of physical therapy supplemented with behavioral interventions. These data support the continued assessment of treatment preference and patient expectation in LBP clinical trials, and provide additional information on how these factors potentially influence treatment outcomes.
Although this study was primarily clinically oriented, there are some theoretical implications to consider from these data. Previous attention has focused on treatment preference or patient expectations, without much attention on why these decisions were made. We obtained concurrent perceived effectiveness ratings for trial treatments and used these ratings to investigate our theoretical assumption that preference and expectation decisions would largely be determined by perceived effectiveness ratings. That is, we expected patients to give higher perceived effectiveness ratings to treatments they preferred. We also expected perceived effectiveness ratings to be associated with treatment expectations.
These data partially supported our theoretical assumptions and provided novel information on why treatment preference and patient expectation decisions are made. First, it should not be assumed that patient preference is predominantly determined by the perceived effectiveness of treatments. In this trial we observed that preference decisions varied based on treatment options, and in some cases the preferred treatment was not associated with the highest perceived effectiveness ratings (i.e. physical therapy alone or supplemented with graded activity). Second, the pattern for patient expectation and perceived effectiveness was more predictable. In this trial we observed individuals with higher expectations had higher perceived effectiveness, regardless of the treatment.
Collectively these results support a theoretical model in which patient expectation has a stronger link with perceived effectiveness, in comparison to treatment preference. While these findings are interesting, there are some other factors to consider when interpreting the perceived effectiveness ratings. In this sample of individuals with acute and subacute LBP even those with low treatment expectations had fairly high perceived effectiveness ratings (Figure 2), suggesting this cohort perceived all potential treatment options to have some merit. Also, we did not collect information on other potentially important variables that would factor into preference and expectation ratings, such as familiarity with treatment, prior treatment experiences, and perceptions of health care providers. Future research in this area will include more complex theoretical models to determine predictors of treatment preference and patient expectation.
Our data suggested that treatment preference and patient expectation have the potential to influence outcomes for clinical trials of physical therapy supplemented with behavioral interventions. For treatment preference we observed a different relationship than what has been previously hypothesized.45,46,11 and what we hypothesized for this analysis. The largest pain intensity and disability improvements were associated with those having no strong treatment preference. This provides a preliminary indication that individuals without pre-set impressions of behavioral treatments may experience a better response in comparison to those with definite preferences. Other studies have provided mixed support that random assignment to a preferred treatment results in better LBP clinical trial outcomes.26,10,35 One trial found that patients preferring massage or acupuncture did better when randomly assigned to receive those treatments.26 In contrast, another trial reported patient preference did not influence pain intensity and disability outcomes for those receiving an education and exercise program.35 A trial that randomly assigned patients to usual care or choice of complementary or alternative treatments reported no difference on clinical outcomes of pain and disability.10 Converging evidence comes from a clinical trial of treatments for patients with whiplash associated disorder which reported no improved pain and disability outcomes when patients were randomly assigned to preferred their preferred treatment.44
Direct comparisons from the current analysis to the previously cited studies are difficult because of methodological differences in preference options. For example, it was not an option to allow individuals to select a “no strong treatment preference” category in some studies10,35 while our data suggest that no preference may be an important issue to consider. Another important methodological difference in the current analysis was the use of behavioral interventions, while other studies used an education and exercise program35 or complementary and alternative therapies.26,10 The previously cited studies and this current analysis differ substantially in important areas, but they do provide empirical evidence that supports26 and refutes35,10 the prevailing hypothesis that receiving treatment matched to preference enhances outcomes. Therefore the influence of treatment preference may be more complex than originally thought and more studies are necessary to further define its effect on clinical outcomes. Our data suggest continued investigation of individuals stating no strong treatment preference may be warranted for behavioral interventions.
In our data higher patient expectation was associated with lower disability, but not with lower pain intensity scores. Specifically, patient expectation had a main effect on disability as no interaction effect was observed. Patients with higher expectations had lower baseline, 4-week, and 6-month disability scores in comparison to those with lower expectations. The absolute improvement in disability scores was similar between higher and lower patient expectation groups.. These findings are in contrast to a secondary analysis from Myers et al37 which indicated that individuals with higher expectations had larger improvements in disability. These data provide another example of how patient expectation can potentially be associated with clinical trial outcomes. This relationship of patient expectation and disability level is consistent with experimental and neuroimaging data indicating a feedback loop operates to reinforce interpretations of repeated sensory experiences to fit expectations.47 In this theoretical model patients’ interpretation of each sensory experience is consistent with pre-treatment expectations, with increasing effect from each subsequent experience.
Patient satisfaction is a patient outcome of interest1,15,13,20 and these analyses supported our proposed hypotheses. The 6-month satisfaction rates did not differ based on treatment received for any of the satisfaction items. These rates were very high for the 2 treatment delivery items (88% and 90%), while much lower rate for the treatment effect item (46%). This discordant relationship in satisfaction ratings has been reported in previous pain studies.13,20,6,34,48 The data in this analysis provide additional evidence that, paradoxically, individuals can report satisfaction with treatment delivery while simultaneously reporting low satisfaction with treatment effects. Exploration of differences in the patient satisfaction ratings supported observations from our previous study using these same 3 satisfaction items in a previous LBP clinical trial.13 Patient satisfaction with treatment delivery and effect were both strongly associated with treatment expectations being met at 6-months. However, only satisfaction with treatment effect was associated with lower 6-month pain intensity and disability. These data provide evidence that comprehensive assessment of patient satisfaction should distinguish treatment delivery and effect especially if the goal is to link patient satisfaction to the resolution of symptoms. Satisfaction with treatment delivery may only be capable of discerning whether patient expectations were met while satisfaction with treatment effect was additionally associated with lower pain intensity and disability levels.
This study has several limitations that should be considered when interpreting these results. First, we focused only on perceived effectiveness ratings because we thought it the most proximal reason for individuals to make treatment preference and expectation decisions. It is very likely that these decisions are influenced by other factors that were not accounted for in our analysis. For example, a recent study in a surgical cohort indicated preference for surgery was not related to gender or race, but was related to age, education level, pain levels, and duration of symptoms.31 Second, this study focused on pain intensity and disability and we did not include subsequent healthcare utilization. This means we could not investigate if patient satisfaction was related to continued healthcare use, as has been previously hypothesized.40 Other limitations include that there were low numbers of subjects that indicated preference for physical therapy with graded exposure in comparison to the other treatments and that our patient expectation measure was of general expectations, not those specific to the treatment being received. Also, our measure of expectation allowed for only high and low expectations to be determined and this scaling did not match our disability and pain outcome measures. Future studies should attempt to use similar scaling for expectation and outcome measures. Last, this study was a secondary analysis of a clinical trial and although these were a priori analyses, they were not the primary focus of the original study.
Conclusion
These data support assessment of treatment preference and patient expectation as predictors and patient satisfaction as an outcome measure in LBP clinical trials. Patient expectation was strongly associated with perceived effectiveness ratings while treatment preference was not. Patients without a strong treatment preference had larger improvements in 6-month pain intensity and disability outcomes, in comparison to those receiving matched or unmatched treatment. Patients with higher treatment expectations had lower disability scores during baseline, 4-week, and 6-month assessments. 6-month satisfaction rates did not differ based on treatment received and higher rates were associated with treatment delivery items. Only the satisfaction with treatment effect item was associated with lower 6-month pain intensity and disability scores, indicating a need to separately assess treatment delivery and effect.
Perspective.
These data indicate treatment preference potentially impacts rate of improvement for patients with low back pain. Patient expectation did not impact rate of improvement, but those with higher expectations had lower pain and disability scores throughout the trial. Optimal assessment of patient satisfaction should include items that separately consider treatment delivery and effect.
Acknowledgments
SZG (PI) and MER were supported by NIH-NIAMS Grant AR051128 while preparing this manuscript.
Michael Borut, Melissa Cere, Anthony Cere, Michael Hodges, Dalton Reed, Carolina Valencia, and Giorgio Zeppieri, Jr. assisted with recruitment and data collection.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflict of interests to report.
Contributor Information
Steven Z. George, Associate Professor and Assistant Department Chair, Department of Physical Therapy, Center for Pain Research and Behavioral Health, University of Florida, Gainesville FL (USA).
Michael E. Robinson, Professor, Department of Clinical and Health Psychology, Center for Pain Research and Behavioral Health, University of Florida, Gainesville, FL (USA).
Reference List
- 1.Beattie PF, Pinto MB, Nelson MK, Nelson R. Patient satisfaction with outpatient physical therapy: instrument validation. Phys.Ther. 2002;82:557–565. [PubMed] [Google Scholar]
- 2.Beattie PF, Pinto MB, Nelson MK, Nelson R. Patient satisfaction with outpatient physical therapy: instrument validation. Phys.Ther. 2002;82:557–565. [PubMed] [Google Scholar]
- 3.Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, Owens DK. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann.Intern.Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 4.Cole DC, Mondloch MV, Hogg-Johnson S. Listening to injured workers: how recovery expectations predict outcomes--a prospective study. CMAJ. 2002;166:749–754. [PMC free article] [PubMed] [Google Scholar]
- 5.Daltroy LH, Cats-Baril WL, Katz JN, Fossel AH, Liang MH. The North American spine society lumbar spine outcome assessment Instrument: reliability and validity tests. Spine. 1996;21:741–749. doi: 10.1097/00007632-199603150-00017. [DOI] [PubMed] [Google Scholar]
- 6.Dawson R, Spross JA, Jablonski ES, Hoyer DR, Sellers DE, Solomon MZ. Probing the paradox of patients' satisfaction with inadequate pain management. J.Pain Symptom.Manage. 2002;23:211–220. doi: 10.1016/s0885-3924(01)00399-2. [DOI] [PubMed] [Google Scholar]
- 7.Dawson R, Spross JA, Jablonski ES, Hoyer DR, Sellers DE, Solomon MZ. Probing the paradox of patients' satisfaction with inadequate pain management. J.Pain Symptom.Manage. 2002;23:211–220. doi: 10.1016/s0885-3924(01)00399-2. [DOI] [PubMed] [Google Scholar]
- 8.Deyo RA, Battie M, Beurskens AJ, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Von Korff M, Waddell G. Outcome measures for low back pain research. A proposal for standardized use. Spine. 1998;23:2003–2013. doi: 10.1097/00007632-199809150-00018. [DOI] [PubMed] [Google Scholar]
- 9.Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, Haythornthwaite JA, Jensen MP, Kerns RD, Ader DN, Brandenburg N, Burke LB, Cella D, Chandler J, Cowan P, Dimitrova R, Dionne R, Hertz S, Jadad AR, Katz NP, Kehlet H, Kramer LD, Manning DC, McCormick C, McDermott MP, McQuay HJ, Patel S, Porter L, Quessy S, Rappaport BA, Rauschkolb C, Revicki DA, Rothman M, Schmader KE, Stacey BR, Stauffer JW, von ST, White RE, Witter J, Zavisic S. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J.Pain. 2008;9:105–121. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Eisenberg DM, Post DE, Davis RB, Connelly MT, Legedza AT, Hrbek AL, Prosser LA, Buring JE, Inui TS, Cherkin DC. Addition of choice of complementary therapies to usual care for acute low back pain: a randomized controlled trial. Spine (Phila Pa 1976) 2007;32:151–158. doi: 10.1097/01.brs.0000252697.07214.65. [DOI] [PubMed] [Google Scholar]
- 11.Fairhurst K, Dowrick C. Problems with recruitment in a randomized controlled trial of counselling in general practice: causes and implications. J.Health Serv.Res.Policy. 1996;1:77–80. doi: 10.1177/135581969600100205. [DOI] [PubMed] [Google Scholar]
- 12.George SZ, Fritz JM, Bialosky JE, Donald DA. The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine. 2003;28:2551–2560. doi: 10.1097/01.BRS.0000096677.84605.A2. [DOI] [PubMed] [Google Scholar]
- 13.George SZ, Hirsh AT. Distinguishing patient satisfaction with treatment delivery from treatment effect: a preliminary investigation of patient satisfaction with symptoms after physical therapy treatment of low back pain. Arch.Phys Med.Rehabil. 2005;86:1338–1344. doi: 10.1016/j.apmr.2004.11.037. [DOI] [PubMed] [Google Scholar]
- 14.George SZ, Zeppieri G, Jr, Cere AL, Cere MR, Borut MS, Hodges MJ, Reed DM, Valencia C, Robinson ME. A randomized trial of behavioral physical therapy interventions for acute and sub-acute low back pain ( NCT00373867) Pain. 2008;140:145–157. doi: 10.1016/j.pain.2008.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldstein MS, Elliott SD, Guccione AA. The development of an instrument to measure satisfaction with physical therapy. Phys.Ther. 2000;80:853–863. [PubMed] [Google Scholar]
- 16.Goldstein MS, Elliott SD, Guccione AA. The development of an instrument to measure satisfaction with physical therapy. Phys.Ther. 2000;80:853–863. [PubMed] [Google Scholar]
- 17.Goldstein MS, Morgenstern H, Hurwitz EL, Yu F. The impact of treatment confidence on pain and related disability among patients with low-back pain: results from the University of California, Los Angeles, low-back pain study. Spine J. 2002;2:391–399. doi: 10.1016/s1529-9430(02)00414-x. [DOI] [PubMed] [Google Scholar]
- 18.Hagen EM, Eriksen HR, Ursin H. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain? Spine. 2000;25:1973–1976. doi: 10.1097/00007632-200008010-00017. [DOI] [PubMed] [Google Scholar]
- 19.Hay EM, Mullis R, Lewis M, Vohora K, Main CJ, Watson P, Dziedzic KS, Sim J, Minns LC, Croft PR. Comparison of physical treatments versus a brief pain-management programme for back pain in primary care: a randomised clinical trial in physiotherapy practice. Lancet. 2005;365:2024–2030. doi: 10.1016/S0140-6736(05)66696-2. [DOI] [PubMed] [Google Scholar]
- 20.Hirsh AT, Atchison JW, Berger JJ, Waxenberg LB, Lafayette-Lucey A, Bulcourf BB, Robinson ME. Patient satisfaction with treatment for chronic pain: predictors and relationship to compliance. Clin.J.Pain. 2005;21:302–310. doi: 10.1097/01.ajp.0000113057.92184.90. [DOI] [PubMed] [Google Scholar]
- 21.Indahl A, Haldorsen EH, Holm S, Reikeras O, Ursin H. Five-year follow-up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine. 1998;23:2625–2630. doi: 10.1097/00007632-199812010-00018. [DOI] [PubMed] [Google Scholar]
- 22.Indahl A, Velund L, Reikeraas O. Good prognosis for low back pain when left untampered. A randomized clinical trial. Spine. 1995;20:473–477. doi: 10.1097/00007632-199502001-00011. [DOI] [PubMed] [Google Scholar]
- 23.Iversen MD, Daltroy LH, Fossel AH, Katz JN. The prognostic importance of patient pre-operative expectations of surgery for lumbar spinal stenosis. Patient.Educ.Couns. 1998;34:169–178. doi: 10.1016/s0738-3991(97)00109-2. [DOI] [PubMed] [Google Scholar]
- 24.Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83:157–162. doi: 10.1016/s0304-3959(99)00101-3. [DOI] [PubMed] [Google Scholar]
- 25.Jensen MP, Turner LR, Turner JA, Romano JM. The use of multiple-item scales for pain intensity measurement in chronic pain patients. Pain. 1996;67:35–40. doi: 10.1016/0304-3959(96)03078-3. [DOI] [PubMed] [Google Scholar]
- 26.Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine (Phila Pa 1976) 2001;26:1418–1424. doi: 10.1097/00007632-200107010-00005. [DOI] [PubMed] [Google Scholar]
- 27.Kapoor S, Shaw WS, Pransky G, Patterson W. Initial patient and clinician expectations of return to work after acute onset of work-related low back pain. J.Occup.Environ.Med. 2006;48:1173–1180. doi: 10.1097/01.jom.0000243401.22301.5e. [DOI] [PubMed] [Google Scholar]
- 28.Linde K, Witt CM, Streng A, Weidenhammer W, Wagenpfeil S, Brinkhaus B, Willich SN, Melchart D. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007;128:264–271. doi: 10.1016/j.pain.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Lindstrom I, Ohlund C, Eek C, Wallin L, Peterson LE, Fordyce WE, Nachemson AL. The effect of graded activity on patients with subacute low back pain: a randomized prospective clinical study with an operant-conditioning behavioral approach. Phys Ther. 1992;72:279–290. doi: 10.1093/ptj/72.4.279. [DOI] [PubMed] [Google Scholar]
- 30.Linton SJ, Boersma K, Jansson M, Svard L, Botvalde M. The effects of cognitive-behavioral and physical therapy preventive interventions on pain-related sick leave: a randomized controlled trial. Clin.J.Pain. 2005;21:109–119. doi: 10.1097/00002508-200503000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Lurie JD, Berven SH, Gibson-Chambers J, Tosteson T, Tosteson A, Hu SS, Weinstein JN. Patient preferences and expectations for care: determinants in patients with lumbar intervertebral disc herniation. Spine (Phila Pa 1976) 2008;33:2663–2668. doi: 10.1097/BRS.0b013e31818cb0db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lutz GK, Butzlaff ME, Atlas SJ, Keller RB, Singer DE, Deyo RA. The relation between expectations and outcomes in surgery for sciatica. J.Gen.Intern.Med. 1999;14:740–744. doi: 10.1046/j.1525-1497.1999.10417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCracken LM, Klock PA, Mingay DJ, Asbury JK, Sinclair DM. Assessment of satisfaction with treatment for chronic pain. J.Pain Symptom.Manage. 1997;14:292–299. doi: 10.1016/s0885-3924(97)00225-x. [DOI] [PubMed] [Google Scholar]
- 34.McCracken LM, Klock PA, Mingay DJ, Asbury JK, Sinclair DM. Assessment of satisfaction with treatment for chronic pain. J.Pain Symptom.Manage. 1997;14:292–299. doi: 10.1016/s0885-3924(97)00225-x. [DOI] [PubMed] [Google Scholar]
- 35.Moffett JK, Torgerson D, Bell-Syer S, Jackson D, Llewlyn-Phillips H, Farrin A, Barber J. Randomised controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences. BMJ. 1999;319:279–283. doi: 10.1136/bmj.319.7205.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Molde HE, Grasdal A, Eriksen HR. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain: a 3-year follow-up study. Spine. 2003;28:2309–2315. doi: 10.1097/01.BRS.0000085817.33211.3F. [DOI] [PubMed] [Google Scholar]
- 37.Myers SS, Phillips RS, Davis RB, Cherkin DC, Legedza A, Kaptchuk TJ, Hrbek A, Buring JE, Post D, Connelly MT, Eisenberg DM. Patient expectations as predictors of outcome in patients with acute low back pain. J.Gen.Intern.Med. 2008;23:148–153. doi: 10.1007/s11606-007-0460-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ostelo RW, de Vet HC, Vlaeyen JW, Kerckhoffs MR, Berfelo WM, Wolters PM, van den Brandt PA. Behavioral graded activity following first-time lumbar disc surgery: 1-year results of a randomized clinical trial. Spine. 2003;28:1757–1765. doi: 10.1097/01.brs.0000083317.62258.e6. [DOI] [PubMed] [Google Scholar]
- 39.Ostelo RW, van Tulder MW, Vlaeyen JW, Linton SJ, Morley SJ, Assendelft WJ. Behavioural treatment for chronic low-back pain. Cochrane.Database.Syst.Rev. 2005 doi: 10.1002/14651858.CD002014.pub2. CD002014. [DOI] [PubMed] [Google Scholar]
- 40.Robinson ME, Brown JL, George SZ, Edwards PS, Atchison JW, Hirsh AT, Waxenberg LB, Wittmer V, Fillingim RB. Multidimensional success criteria and expectations for treatment of chronic pain: the patient perspective. Pain Med. 2005;6:336–345. doi: 10.1111/j.1526-4637.2005.00059.x. [DOI] [PubMed] [Google Scholar]
- 41.Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine. 1987;12:S1–S59. [PubMed] [Google Scholar]
- 42.Smeets RJ, Vlaeyen JW, Hidding A, Kester AD, van der Heijden GJ, van Geel AC, Knottnerus JA. Active rehabilitation for chronic low back pain: Cognitive-behavioral, physical, or both? First direct post-treatment results from a randomized controlled trial [ISRCTN22714229] BMC.Musculoskelet.Disord. 2006;7:5. doi: 10.1186/1471-2474-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Staal JB, Hlobil H, Twisk JW, Smid T, Koke AJ, van Mechelen W. Graded activity for low back pain in occupational health care: a randomized, controlled trial. Ann.Intern.Med. 2004;140:77–84. doi: 10.7326/0003-4819-140-2-200401200-00007. [DOI] [PubMed] [Google Scholar]
- 44.Stewart MJ, Maher CG, Refshauge KM, Herbert RD, Nicholas MK. Patient and clinician treatment preferences do not moderate the effect of exercise treatment in chronic whiplash-associated disorders. Eur.J.Pain. 2008;12:879–885. doi: 10.1016/j.ejpain.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 45.Torgerson DJ, Klaber-Moffett J, Russell IT. Patient preferences in randomised trials: threat or opportunity? J.Health Serv.Res.Policy. 1996;1:194–197. doi: 10.1177/135581969600100403. [DOI] [PubMed] [Google Scholar]
- 46.Torgerson DJ, Sibbald B. Understanding controlled trials. What is a patient preference trial? BMJ. 1998;316:360. doi: 10.1136/bmj.316.7128.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vase L, Robinson ME, Verne GN, Price DD. Increased placebo analgesia over time in irritable bowel syndrome (IBS) patients is associated with desire and expectation but not endogenous opioid mechanisms. Pain. 2005;115:338–347. doi: 10.1016/j.pain.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 48.Ward SE, Gordon DB. Patient satisfaction and pain severity as outcomes in pain management: a longitudinal view of one setting's experience. J.Pain Symptom.Manage. 1996;11:242–251. doi: 10.1016/0885-3924(95)00190-5. [DOI] [PubMed] [Google Scholar]
- 49.Ward SE, Gordon DB. Patient satisfaction and pain severity as outcomes in pain management: a longitudinal view of one setting's experience. J.Pain Symptom.Manage. 1996;11:242–251. doi: 10.1016/0885-3924(95)00190-5. [DOI] [PubMed] [Google Scholar]