Abstract
This research examined the preliminary effects of Cognitive Enhancement Therapy (CET) on social cognition in early course schizophrenia, using an objective, performance-based measure of emotional intelligence. Individuals in the early course of schizophrenia were randomly assigned to either CET (n = 18) or Enriched Supportive Therapy (n = 20), and assessed at baseline and after one year of treatment with the Mayer-Salovey-Caruso Emotional Intelligence Test. A series of analyses of covariance showed highly significant (p = .005) and large (Cohen's d = .96) effects favoring CET for improving emotional intelligence, with the most pronounced improvements occurring in patients' ability to understand and manage their own and others' emotions. These findings lend preliminary support to the previously documented benefits of CET on social cognition in schizophrenia, and suggest that such benefits can be extended to patients in the early course of the illness (141 words).
1. Introduction
Despite the introduction of novel antipsychotic agents, many individuals with schizophrenia continue to suffer from marked social disability and diminished functional capacity (Thaker & Carpenter, 2001). Research over the past several decades has increasingly pointed to the important role cognitive deficits play in maintaining poor functional outcomes in schizophrenia (Green, 1996). In particular, research has consistently shown neurocognitive deficits in attention, working memory, and executive function to be linked with poor community functioning and social adjustment (Green et al., 2000). Recently, cognitive deficits associated with the processing and interpretation of social and emotional information have also been noted as important potential contributors to poor functional outcome in schizophrenia (Green et al., 2005; Penn et al., 1997). Several cross-sectional studies have found that these deficits in social cognition are related to poor social and behavioral outcomes (Brune, 2005; Corrigan & Toomey, 1995; Mueser et al., 1996), and indicated that such relationships exist, to some degree, independent of deficits in neurocognition (Penn et al., 1996; Vauth et al., 2004). Unfortunately, to date, effective treatments to address social-cognitive deficits in schizophrenia have been sparse.
Cognitive Enhancement Therapy (CET; Hogarty & Greenwald, 2006) is an integrated, developmental approach to the remediation of neurocognitive and social-cognitive deficits in schizophrenia. Recently we described comprehensive and enduring effects of CET in a randomized-controlled trial of 121 chronically ill (on average 15 years) persons with schizophrenia, treated for 2 years and followed-up 1 year post-treatment (Hogarty et al., 2004; Hogarty et al., in press). Employing highly reliable composites, broadly defined measures of social cognition demonstrated the largest behavioral improvement over time. However, legitimate concerns existed not only with our definition and measure of social cognition, but also its objective assessment by non-blind clinical raters. In preparation for a new trial among early course patients (ill for less than 8 years), we again surveyed the literature on the measurement of social cognition. Although the literature is replete with widely varying definitions of social cognition (Wyer & Srull, 1994), the field has increasingly moved to a better elaboration of the mental processes that are known to support interpersonal functioning, such as emotional processing, social processing, social context appraisal, theory of mind and attributional styles (Pinkham et al., 2003), to name a few. Central to these social-cognitive processes is the ability to process, understand, and manage emotion, commonly referred to as emotional intelligence (Mayer & Salovey, 1997). The Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT; Mayer et al., 2003) provides objective, performance and ability-based assessments of emotional intelligence, that are largely independent of personality traits and self-report attributions. This unique instrument has been included in our ongoing studies of CET and has also been recently recommended by the NIMH-MATRICS project (Green et al., 2005).
We now examine whether previous beneficial effects of CET on social cognition can be identified using the MSCEIT, and extended to individuals in the early course of schizophrenia. Previous reports have shown CET to be effective at improving deficits in social-cognition among more chronic patients (Hogarty et al., 2004, in press). The neurodevelopmental framework upon which CET is based suggests that the treatment should be particularly effective at improving adjustment and forestalling social deteriorating among patients early in the course of the illness, through facilitating the development of the social-cognitive processes that underly appropriate adult socialization closer to the developmental period when these processes emerge among healthy individuals (Hogarty & Flesher, 1999). Furthermore, patients early in the course of their illness are thought to have continuing brain plasticity (Keshavan & Hogarty, 1999). This might facilitate the ability of patients to benefit from a disorder-relevant treatment designed to improve social and neurocognitive deficits, and lead to a better long-term functional outcome.
2. Method
2.1. Participants
Participants were recruited from the outpatient and inpatient services of the Western Psychiatric Institute and Clinic, Pittsburgh and several nearby community clinics. This research was conducted between August, 2001 and January, 2006. All participants provided informed consent prior to participation and this research was approved by the University of Pittsburgh Institutional Review Board. Forty-three participants were recruited, but only 38 completed one year of treatment (2 participants moved, 2 withdrew consent, and 1 did not meet eligibility criteria upon further review). Participants consisted of individuals in the early course of schizophrenia (n = 28) or schizoaffective (n = 10) disorder, confirmed by consensus diagnostic reviews of all available clinical data and the Structured Clinical Interview for DSM-IV (First et al., 1996). To be eligible for this research, participants had to have been diagnosed within the past eight years, have an IQ ≥ 80 (M = 95.68, SD = 11.19; Wechsler, 1981), and not abusing substances during the past two months. Participants were between 17 and 43 years of age (M = 26.14, SD = 6.54), and had been ill for an average of 3.75 years (SD = 2.80). Two-thirds of participants were male (n = 26), and most were Caucasian (n = 26) or African American (n = 6). All participants had completed high-school, over half (n = 25) had attended some college, and nine were currently employed.
2.2. Measures
Social cognition was assessed using the MSCEIT, a unique, performance-based measure of emotional intelligence that assesses a person's ability to accurately perceive emotions, to use emotions to facilitate thinking and decision making, and to understand and manage emotions in oneself and others. These four emotional abilities are theorized to define the overall emotional intelligence construct (Mayer & Salovey, 1997). The MSCEIT provides an overall emotional intelligence quotient (EQ), as well as four subscale scores corresponding to the four abilities that comprise emotional intelligence. The MSCEIT includes 141 multiple choice items, and is "performance-based" in that it requires participants to solve problems related to emotion (e.g., identify the best way to manage an emotion given a certain situation) rather than relying on self-reports or observations. Items are scored by consensus norms from a large healthy sample, and scaled with a mean of 100 (SD = 15). Although the instrument has yet to be applied to psychiatric populations, it has shown excellent reliability and construct validity among a large sample of healthy individuals (Mayer et al., 2003).
2.3. Treatment and Procedures.
Upon recruitment, participants were randomly assigned to either CET (n = 18) or Enriched Supportive Therapy (EST) (n = 20), both of which have been described in detail elsewhere (Hogarty & Greenwald, 2006, Hogarty et al., 2004). Briefly, CET is an integrated approach to the remediation of social-cognitive and neurocognitive deficits in schizophrenia, where participants complete approximately 60 hours of computer training in attention, memory, and problem-solving, and participate in a newly revised 45 session weekly social-cognitive group that focuses on learning how to take the perspective of others, reading non-verbal cues, managing emotions, and appraising the social context (Hogarty & Greenwald, 2006). EST consists of components from the basic and intermediate phases of Personal Therapy (Hogarty, 2002), which focus on stress reduction strategies and psychoeducation. Following randomization, participants underwent computerized assessments with the MSCEIT at baseline and after one year of treatment. No significant differences were found between treatment groups with respect to age, gender, baseline IQ, length of illness at baseline, symptomatology, receipt of atypical antipsychotic medication, or treatment dropout.
3. Results
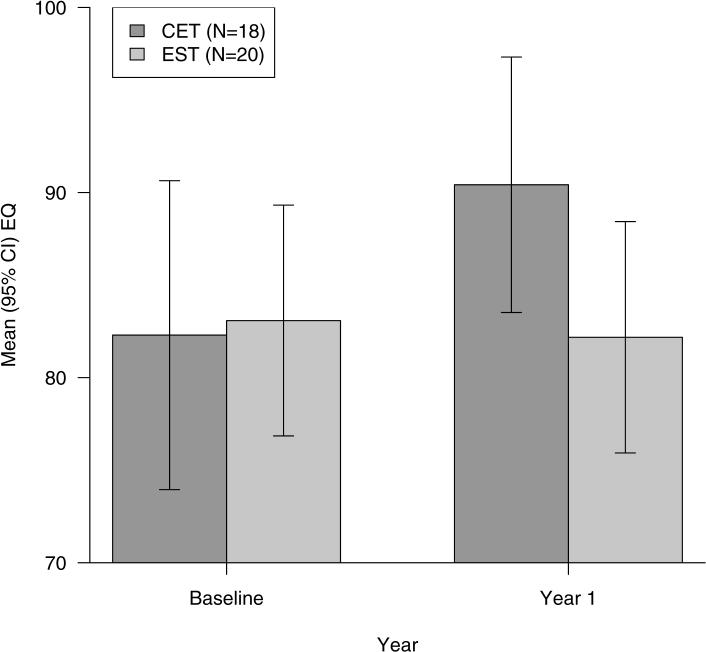
A series of analyses of covariance, covarying baseline emotional intelligence scores, was used to assess the differential effects of CET on changes in emotional intelligence, compared to EST. Cohen's d is used to illustrate the magnitude of these effects, and represents the differential rate of improvement in emotional intelligence of participants in CET compared to those in EST. Positive effect sizes indicate larger differential improvement in CET than EST. Effect sizes greater than .50 are considered medium in size, and those greater than .80 are considered large (Cohen, 1988). As can be seen in Figure 1, participants in CET showed significant and large differential improvements on overall EQ, F(1, 35) = 8.91, p = .005, d = .96, compared to those in EST, such that those participating in CET approached the average EQ of healthy individuals. Analyses of differential improvement on specific areas of emotional intelligence indicated that individuals in CET improved significantly more than participants in EST on their ability to understand, F(1, 35) = 6.38, p = .016, d = .82, and manage emotions, F(1, 35) = 6.59, p = .015, d = .83, as well as their ability to use emotions to facilitate thinking and decision making, F(1, 35) = 4.16, p = .049, d = .66. A non-significant trend was observed favoring CET for improving participants' ability to accurately perceive emotions, F(1, 35) = 2.91, p = .097, d = .55.
Figure 1.
One year effects of Cognitive Enhancement Therapy (CET) and Enriched Supportive Therapy (EST) on Emotional Intelligence Quotient (EQ) scores.a
4. Discussion
Cognitive deficits in the processing of social and emotional information have been widely documented in schizophrenia research and represent important targets for treatment (Pinkham et al., 2003), yet both psychosocial and pharmacological strategies to address these deficits have been lacking. In this research, we provide preliminary evidence from an ongoing trial of CET for early course schizophrenia that some of the social-cognitive deficits associated with the illness can be successfully remediated by this integrated, theory-driven treatment. Using an objective, performance-based measure of social cognition, this evidence supports the efficacy of CET for improving emotional intelligence in schizophrenia, and indicates that these effects can be extended to patients in the early course of the disorder. Specifically, our results indicate that after one year of treatment, CET is particularly beneficial for assisting participants in learning to understand and manage emotions, both in themselves and others. While it will be important for future research to examine the effects of CET on other dimensions of social cognition (e.g., attributional style, social context appraisal), the ability to understand the meaning of emotions within a social context and apply appropriate regulation strategies when necessary is an important cornerstone of healthy social interactions (Carter, 2006). Long-term effects of these improvements in the emotional dimensions of social cognition on functional outcome and social adjustment are awaited from our ongoing, two-year clinical trial (Keshavan, 2005).
In addition to providing continued support for the beneficial effects of CET on social cognition, this research also lends much needed support to the utility of the MSCEIT for assessing changes in social cognition that occur during treatment. Although the MSCEIT was recommended by the MATRICS committee nearly a year ago for assessing social-cognitive deficits in schizophrenia (Green et al., 2005), relatively little research has been published documenting its psychometric properties among psychiatric populations. This research suggests that the MSCEIT at least possesses some sensitivity to treatment-induced changes in social cognition, which is particularly important if the instrument is to be applied in clinical trials. Further, preliminary analyses indicate that improvements on the MSCEIT are paralleling improvements on our other measures of social cognition, lending some credence to its construct validity (Keshavan, 2005). More comprehensive psychometric evaluation of the MSCEIT is expected from our own trial and the MATRICS project.
Acknowledgments
This work was supported by NIMH grant MH 60902 (MSK). We thank Susan Cooley MN.Ed., Anne Louise DiBarry, M.S.N., Konasale Prasad, M.D., Haranath Parepally, M.D., Debra Montrose, Ph.D., Diana Dworakowski, M.S., Mary Carter, Ph.D., and Sara Fleet, M.S. for their help in various aspects of the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Patients in CET exhibit significantly greater improvement in emotional intelligence than those in EST, F(1, 35) = 8.91, p = .005, d = .96.
References
- Brune M. Emotion recognition, 'theory of mind,' and social behavior in schizophrenia. Psychiatry Res. 2005a;133(2−3):135–147. doi: 10.1016/j.psychres.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Carter CS. Understanding the glass ceiling for functional outcome in schizophrenia. Am. J. Psychiatry. 2006;163(3):356–358. doi: 10.1176/appi.ajp.163.3.356. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Corrigan PW, Toomey R. Interpersonal problem solving and information processing in schizophrenia. Schizophr. Bull. 1995;21(3):395–403. doi: 10.1093/schbul/21.3.395. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-Patient Edition. Biometrics Research Department, New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am. J. Psychiatry. 1996;153(3):321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: Are we measuring the right stuff? Schizophr. Bull. 2000;26(1):119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- Green MF, Olivier B, Crawley JN, Penn DL, Silverstein S. Social cognition in schizophrenia: Recommendations from the measurement and treatment research to improve cognition in schizophrenia new approaches conference. Schizophr. Bull. 2005;31(4):882–887. doi: 10.1093/schbul/sbi049. [DOI] [PubMed] [Google Scholar]
- Hogarty GE. Personal Therapy for schizophrenia and related disorders: A guide to individualized treatment. Guilford; New York: 2002. [Google Scholar]
- Hogarty GE, Flesher S. Developmental theory for a cognitive enhancement therapy of schizophrenia. Schizophr. Bull. 1999;25(4):677–692. doi: 10.1093/oxfordjournals.schbul.a033410. [DOI] [PubMed] [Google Scholar]
- Hogarty GE, Greenwald DP. Cognitive Enhancement Therapy: The Training Manual. University of Pittsburgh Medical Center. 2006 www.CognitiveEnhancementTherapy.com Authors. Available through.
- Hogarty GE, Flesher S, Ulrich R, Carter M, Greenwald D, Pogue-Geile M, et al. Cognitive enhancement therapy for schizophrenia. Effects of a 2-year randomized trial on cognition and behavior. Arch. Gen. Psychiatry. 2004;61(9):866–876. doi: 10.1001/archpsyc.61.9.866. [DOI] [PubMed] [Google Scholar]
- Hogarty GE, Greenwald DP, Eack SM. Cognitive Enhancement Therapy: Durability and mechanism of effects. Psychiatr. Serv. doi: 10.1176/ps.2006.57.12.1751. in press. [DOI] [PubMed] [Google Scholar]
- Keshavan M. Rehabilitation, Brain Function and Early Schizophrenia. 2005. NIMH Grant MH60902.
- Keshavan MS, Hogarty GE. Brain maturational processes and delayed onset in schizophrenia. Dev. Psychopathol. 1999;11(3):525–543. doi: 10.1017/s0954579499002199. [DOI] [PubMed] [Google Scholar]
- Mayer JD, Salovey P. What is emotional intelligence? In: Salovey P, Sluyter D, editors. Emotional Development and Emotional Intelligence: Implications for Educators. Basic Books; New York: 1997. pp. 3–31. [Google Scholar]
- Mayer JD, Salovey P, Caruso DR, Sitarenios G. Measuring emotional intelligence with the MSCEIT V2.0. Emotion. 2003;3(1):97–105. doi: 10.1037/1528-3542.3.1.97. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Doonan R, Penn DL, Blanchard JJ, Bellack AS, Nishith P, et al. Emotion recognition and social competence in chronic schizophrenia. J. Abnorm. Psychol. 1996;105(2):271–275. doi: 10.1037//0021-843x.105.2.271. [DOI] [PubMed] [Google Scholar]
- Penn DL, Corrigan PW, Bentall RP, Racenstein J, Newman L. Social cognition in schizophrenia. Psychol. Bull. 1997;121(1):114–132. doi: 10.1037/0033-2909.121.1.114. [DOI] [PubMed] [Google Scholar]
- Penn DL, Spaulding W, Reed D, Sullivan M. The relationship of social cognition to ward behavior in chronic schizophrenia. Schizophr. Res. 1996;20(3):327–335. doi: 10.1016/0920-9964(96)00010-2. [DOI] [PubMed] [Google Scholar]
- Pinkham AE, Penn DL, Perkins DO, Lieberman J. Implications for the neural basis of social cognition for the study of schizophrenia. Am. J. Psychiatry. 2003;160(5):815–824. doi: 10.1176/appi.ajp.160.5.815. [DOI] [PubMed] [Google Scholar]
- Thaker GK, Carpenter WT. Advances in schizophrenia. Nat. Med. 2001;7(6):667–671. doi: 10.1038/89040. [DOI] [PubMed] [Google Scholar]
- Vauth R, Rusch N, Wirtz M, Corrigan PW. Does social cognition influence the relation between neurocognitive deficits and vocational functioning in schizophrenia? Psychiatry Res. 2004;128(2):155–165. doi: 10.1016/j.psychres.2004.05.018. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale-Revised. Psychological Corp; New York: 1981. [Google Scholar]
- Wyer RS, Srull TK, editors. Basic Processes. Vol. 1. Lawrence Earlbaum Association; Hillside, NJ: 1994. Handbook of social cognition. [Google Scholar]