Abstract
This randomized clinical trial employed a 2-group (general child behavior management training vs. distraction for pain management training) design across repeated parent-administered needle procedures. Forty-seven children with a chronic illness requiring recurrent injections were observed at baseline and 2 intervention sessions. Videotaped observations of parent–child interactions were coded for child behavioral distress and parents’ use of behavior management strategies. Across groups, many children displayed minimal to no distress at baseline. Among participants with significant distress, neither intervention group displayed consistently decreased procedural distress or increased use of child behavior management strategies.
Children with chronic diseases consider repeated, painful procedures the worst part of having an illness, and do not become desensitized simply as a result of repetition of procedures (Weekes & Savedra, 1988). Lumbar puncture (LP) and bone marrow aspiration (BMA) typically have been the most painful procedures, and are now nearly always performed under sedation or general anesthesia (Cohen, Blount, Cohen, Schaen, & Zaff, 1999; Dahlquist, 1992, 1999; Jay, Elliott, Katz, & Siegel, 1987). Less invasive but frequently repeated procedures, such as venipuncture and subcutaneous (SQ) or intramuscular (IM) injections, have been described as “a major source of distress and apprehension” for children (Jacox, Carr, & Payne, 1994). Similarly, research indicates that a substantial proportion of children display significant levels of distress during pediatric immunization procedures (Jacobson et al., 2001). For example, Jacobson et al. found that at least 20% of children aged 4 to 6 years exhibited levels of distress in the high range of their measures. In addition, results of a national telephone survey (Princeton Survey Research Associates [PSRA], 1996) revealed that needle procedures are the things they dislike most about obtaining health care services.
Pediatric procedural distress disrupts necessary medical care, diminishes the child’s quality of life, and produces psychosocial stress for families. Chronic distress related to repeated painful procedures may place the child at increased risk for behavioral or psychological disturbances outside of the medical context, negatively impacting home and school adjustment. Severe procedure-related behavioral distress can necessitate increased sedation; physical restraint; and, in some cases, general anesthesia. These interventions can increase both the risks associated with treatment and the degree to which the treatment disrupts the child’s life (e.g., due to increased time spent recovering from medication effects; Anderson, Zelter, & Fanurik, 1993). Likewise, 23% of parents with children aged 13 years and younger have delayed or avoided a medical procedure for their child to avoid a pediatric immunization procedure at the same office visit (PSRA, 1996).
Procedure-related distress has been recognized and addressed in clinical literature over the past 3 decades (Dahlquist, 1992; Jay, 1988; Melamed, Robbins, & Graves, 1982). The format of non-pharmacological interventions has varied widely from filmed modeling, to clinic-based training sessions with a psychologist, to hypnosis, to in vivo coaching or distraction (DIS) techniques (Blount, Landolf-Fritsche, Powers, & Sturges, 1991; Blount, Powers, Cotter, Swan, & Free, 1994; Cohen, Blount, & Panopoulos, 1997; Cohen et al., 1999; Dahlquist, 1992; Fanurik, Koh, Schmitz, & Brown, 1997; Melamed et al., 1982; Powers, 1999; Powers, Blount, Bachanas, Cotter, & Swan, 1993). There is evidence to support the short-term benefits of most of these strategies. Behavior therapy interventions such as controlled breathing, progressive muscle relaxation, visual imagery, and DIS have been used with experienced children to supplement pharmacological management during multiple painful procedures, such as injections (Fowler-Kerry & Lander, 1987; Gonzalez, Routh, & Armstrong, 1993; Powers et al., 1993), BMA (Jay et al., 1987; Jay, Elliott, Ozolins, & Pruitt, 1985), and cardiac catheterization (Caire & Erickson, 1986). DIS during painful procedures may be beneficial for children with chronic conditions who require repeated, painful medical procedures.
A variety of DIS techniques have been reviewed in the literature. Auditory DIS in the form of listening to music through earphones during routine immunizations has decreased the self-reported pain in 4- to 6-year-olds (Fowler-Kerry & Lander, 1987). However, when music DIS was compared to provision of a placebo local anesthetic cream with 4- to 16-year-olds during IV access, no differences were found on either self-reported pain or observer’s global ratings of children’s pain (Arts et al., 1994). Breathing exercises alone (French, Painter, & Coury, 1994) or blowing on a party favor plus differential reinforcement for cooperation (Manne et al., 1990) reduced observed behavioral distress, but not the self-reported pain of 3- to 9-year-old children during immunizations or venipuncture.
In another study, 4- to 6-year-old children undergoing immunization injections were found to have significantly lower observed behavioral distress and significantly more observed coping behaviors when a movie DIS plus nurse coaching intervention was provided compared to standard medical care (Cohen et al., 1997). This intervention also resulted in more coping-promoting behavior and less distress-promoting behavior by nurses and parents. Furthermore, this intervention resulted in less parent and nurse self-reported distress, as well as significantly decreased ratings of child distress by nurses and parents. The movie DIS plus nurse coaching intervention, however, was not significantly improved by adding a brief parent and child training intervention for use of the DIS intervention (Cohen et al., 1997).
Two recent studies (Dahlquist, Pendley, Landthrip, Jones, & Steuber, 2002; Pringle et al., 2001) tested a standard DIS intervention, which could be varied along some stimulus dimensions (to match a child’s ability and preference, and to maintain interest over time) and which required a motor response but did not require a highly trained professional (Texas Instruments Touch and Discover toy or a Vtech Little Smart Smarty toy robot). In the first study, behavioral distress decreased during procedures in which the child looked at or played with the distractor. Sessions in which the toy was available, but the child did not attend to it, did not differ from baseline.
The second study examined the longer term effects of interactive DIS (an electronic toy) on 8 preschool children’s distress behaviors during repeated chemotherapy injections. The therapist initially was present during the procedures and prompted the child to play with the distractor. Over subsequent procedures, the parent gradually learned to coach their child in DIS, and the therapist’s prompting was gradually faded out. This intervention reduced overt behavioral distress in 5 of 8 children. Of those who improved, 3 were able to maintain the reductions in behavioral distress over 3 to 16 weeks.
Dahlquist and colleagues (Dahlquist, 1999; Dahlquist et al., 2002) argued that distractors that involve multiple sensory modalities require the child to actively participate rather than merely attend to the distractor, and those that involve more cognitive processing should be the most effective. Although few studies directly test this premise, Mason, Johnson, and Woolley (1999) found that interactive toys can more effectively reduce child distress than those that simply require the child to be a passive listener. Similarly, Dahlquist et al. (2007) demonstrated that active interaction with a distractor resulted in much greater improvement in pain tolerance than attending to the same distracting stimulus without manipulating it. A recent critical review of the literature regarding DIS for distress related to IM injections also concluded that DIS interventions that require an overt behavioral response of the child, and ones that engage multiple sensory modalities, may be most clinically useful (DeMore & Cohen, 2005).
Most pediatric distress management interventions have been implemented in medical clinic settings. However, parents are frequently required to perform numerous medical procedures in the home, as required by various disease management regimens, and because of efforts to contain medical costs. There is currently little literature to examine the prevalence of child distress during parent-administered needle procedures. This relative dearth of literature is concerning, given the correlations documented among inadequately managed pediatric procedural distress and negative psychological outcomes (for a review, see Blount, Piira, & Cohen, 2003), physiological development (Taddio, Goldbach, Ipp, Stevens, & Koren, 1995), and adult health care behaviors (Pate, Blount, Cohen, & Smith, 1996).
One study examining the efficacy of parent training in DIS included some children receiving their needle sticks in the home (Pringle et al., 2001). Of the 8 participating children in this study, 4 children received home-based, parent-administered needle procedures. Graduate student therapists conducted home-based parent training in contingency management, structuring the needle procedure, and coaching their child in DIS via an electronic, interactive toy robot. Results indicated that, although maintenance of treatment gains was variable across participants, the distress management intervention was associated with reductions in an observational measure of child distress during home-based, parent-administered needle sticks. In light of the apparent benefits of DIS interventions, as well as the current paucity of literature regarding the prevalence of child distress during parent-administered needle procedures, it follows that this topic deserves further consideration.
Parent administration of pediatric procedures may pose unique challenges, particularly given the absence of supports typically found in medical settings (e.g., medical staff experienced in calming children during procedures and efficiently administering injections). Inadequate parent training is likely to increase parental anxiety, which has been shown to be associated with both child distress and with poorer response to DIS interventions (Dahlquist & Pendley, 2005). Pediatric distress management interventions tailored for the purposes of parent-administered procedures require that the parent is adequately trained in distress management techniques in a manner that will maximize both treatment effectiveness and long-term skills maintenance.
There currently is no literature examining the efficacy of brief parent training to use behavior pain management techniques for child distress during painful parent-administered procedures. This lack of research is concerning, given the many potentially distressing pediatric procedures parents are expected to perform, as well as the numerous barriers that exist for many families in accessing individualized pain coping skills training delivered by mental health professionals (for a recent review, see Elgar & McGrath, 2003).
Based on the established efficacy of DIS for decreasing child distress during a variety of pediatric needle procedures, it follows that use of a parent-administered, interactive DIS intervention may be effective for decreasing child behavioral distress during parent-performed needle procedures. The primary aim of this study was to document the extent to which children experience behavioral distress during parent-administered needle procedures. In addition, the study compared the effects of two different parent-training interventions on child distress during parent-administered needle procedures. The study also examined caregivers’ behavior management skills in relation to child behavioral distress at baseline and after the parent-training interventions. It was hypothesized that children of families who were randomized to the parent-training DIS group would exhibit significant reductions in child behavioral distress during needle procedures, but no change in the use of recommended behavior management strategies, whereas children in the general behavior management (GBM) group would experience no change in behavioral distress during needle procedures, despite parents’ increased use of recommended child behavior management strategies.
METHOD
Participants
Participants were recruited in an urban setting in the northeastern United States from university-based endocrine clinics, private practices, and via advertisement in local parenting publications. Participant inclusion was limited to children (and their parents) who (a) had a diagnosis of a chronic medical condition requiring repeated needle procedures (i.e., SQ or IM injection, finger stick, or insulin pump needle change) for disease management, (b) were being treated medically with needle procedures administered by his or her parents, and (c) were developing cognitively within the normal or mildly delayed range.
A total of 51 families were screened for participation. Four families who met inclusion criteria did not attend the initial clinic visit and were unable to be reached for rescheduling purposes. These children were similar in both gender (3 males) and age (M = 89 months, SD = 22 months) characteristics, as compared to participating children. Our sample then consisted of 47 children (31 males). Health conditions that required needle procedures included type 1 diabetes (n = 31), growth hormone deficiency (n = 13), hemophilia (n = 2), and rheumatoid arthritis (n = 1). The participants were children between the ages of 2 and 10 years (M = 6.25 years, SD = 2.5 years) and their family members (77% mothers, 19% fathers, 4% both mother and father) were primary caregivers. The majority of the sample was comprised of Caucasian (i.e., 89%) children from intact (i.e., both biological parents in the home; 87%) families in which either the mother (66%) or father (62%) earned at least an undergraduate college degree.
Measures
Demographic form
The demographic form, designed for the purposes of this study, was completed by participants and was utilized to gather descriptive and group assignment information. Data were gathered on age, gender, medical diagnosis, parent years of education, child developmental level, date of initiating injections, number of injections experienced prior to study entry, time since beginning injection regimen, amount of medication being injected, the type of injection, and daily or weekly frequency of prescribed injections.
The Observation Scale of Behavioral Distress (OSBD; Jay, Ozolins, Elliott, & Caldwell, 1983)
The OSBD, a behavioral observation coding system, was used to code the occurrence of distress behaviors. The OSBD consists of 11 verbal, vocal, and motor behaviors indicative of distress in children, which are weighted according to intensity. The OSBD has been shown to be sensitive to changes in levels of behavioral distress following intervention and to correlate with child self-report, parent, and medical professional ratings of child distress during BMA, LP, and medical exams (Dahlquist et al., 1986; Jay et al., 1987; Jay, Elliot, Ozolins, & Pruitt, 1985; Jay et al., 1983;). The occurrence, or not, of each of the behaviors in the OSBD was scored using a 15-sec interval system. Weighted mean per interval scores were calculated for the anticipatory and procedural phases of the observed procedures. Scores were summed to provide a total distress score.
Dyadic Parent–Child Interaction Coding System (DPICS; Eyberg & Robinson, 1982)
Structured observations of the parent–child interactions in a non-medical situation were coded using portions of the DPICS (Hembree-Kigin & McNeil, 1995). The parent and child were filmed interacting in three situations designed by the authors. In the child-directed interaction situation (similar to “The Child’s Game”—Forehand & McMahon, 1981), the child was allowed to play with whatever he or she chose and had the parent’s undivided attention. During the parent-directed interaction situation (similar to the “Parent’s Game”—Forehand & McMahon, 1981), the parent picked the activity and asked the child to play along. During the cleanup situation, the child was directed by the parent to put away the toys in preparation for departure.
During each of the three 5-min interactions, the frequency and type of parent–child behaviors were coded from the videotapes using the research version of the DPICS, which includes 24 operationally defined parent or child behaviors (e.g., descriptive statement, reflective statement, critical statement, disruptive behavior, compliance, etc.). The operationally defined behaviors were coded using a continuous 15-sec interval coding system with partial interval-scoring criterion (Bailey & Bostow, 1979). Data were summarized for each of the three parent–child interaction situations by calculating a ratio of recommended to non-recommended child behavior management strategies.
Interobserver reliability
Before coding videotapes, the observers were trained to an interval-by-interval exact agreement criterion of 80% or better on the OSBD and DPICS. Interobserver agreement was calculated via Cohen’s Kappa coefficient (Bakeman & Gottman, 1986). Training was accomplished by rehearsal with training videotapes. A second observer coded the data for 25% of the filmed sequences analyzed. Kappa coefficients for this study were 0.80 (SD = 0.35) for the OSBD total distress score and 0.82 (SD = 0.08) for the DPICS data scores (overall summary score).
Parent’s ratings of child distress and cooperation (Powers et al., 1993)
The parent performing the injection or participating in the non-medical interactions with the child completed visual analogue scales (VASs) after each observed parent–child interaction to rate the child’s degree of observed distress and cooperation during the interaction. VASs are common methods of assessing child distress and have been shown to be valid (McGrath, 1990). All VASs employed 100 mm lines anchored with “no distress” and “very distressed,” and “not cooperative” and “very cooperative.”
Subject Encounter Form (SEF)
The SEF, designed for the purposes of this study, was completed by participating parents and was utilized to gather date and time information of sessions for each observed injection, including start and stop times of observed injections, as well as date of the last study observation. Data were gathered regarding type and dosage of medication injected and the time that the topical anesthetic, an eutectic mixture of lidocaine 2.5% and prilocaine 2.5% (EMLA® AstraZenica LP, Wilmington, DE 19850) was applied by the parent to the injection site. These data were used for preliminary analyses to identify possible covariates. Data also were recorded on any other medications that the child was known to be on that day, which may have confounding effects on behavior (e.g., anxiolytics, corticosteroids).
Child Behavior Checklist (CBCL; Achenbach, 1991, 1992)
The CBCL is a commonly used, 138-item parent questionnaire of child behavioral adjustment. It yields standardized t scores on two empirically derived broad dimensions of behavior (internalizing and externalizing) and for total behavior problems. The criterion of greater than 2 SDs above the mean is used to determine clinically significant score elevation on any subscale. The reliability and validity of this instrument have been extensively demonstrated (Achenbach, 1991). The child’s parent was asked to complete the CBCL to calculate a total externalizing problems score. These data were employed in this study as descriptive assessments of child-externalizing behavioral difficulties.
Interstitial score (IS)
The IS, designed for the purposes of this study, was completed by participants and was utilized to gather descriptive information regarding the occurrence, and quality, of various possible medical events (e.g., admissions to the hospital, dental procedures, immunizations) in (a) the month prior to baseline assessment and (b) the time period occurring between study visits. Participants also rated the quality of each of these experiences on a 7-point Likert-type scale ranging from 1 (very positive) to 7 (very negative). An IS score was generated by adding the quality ratings of all the medical events that were endorsed as having occurred during the designated time period; the total rating score was divided by the number of experiences.
Parent treatment adherence
A random selection of 20% of sessions (n = 30) were reviewed to assess parent implementation of recommended strategies. Specifically, 18 sessions in the DIS group and 12 sessions in the GBM group were reviewed. Sessions were coded as compliant for instances of adherence to three primary recommendations for DIS (i.e., parent presentation of distractor to child, parent praise for child use of DIS, and prompts for child to engage with distractor) and GBM groups (parent use of positive attention, effective instruction delivery, and planned ignoring). Parents in 53% of these sessions implemented skills they were taught in the parent-training sessions. Parents displayed recommended strategies during 45% and 68% of sessions in the DIS and GBM groups, respectively. This difference in percentage of treatment adherence by group assignment is not statistically significant, χ2(1, N = 76) = 2.67, p = .102.
Design and Procedure
This randomized clinical trial employed a 2-group (GBM training and DIS for pain management training) by 2-context (parent-administered injections and non-medical parent–child interaction activities) experimental design with repeated measures across three time points. The three measurement time points included baseline, immediately following the parent-training module, and follow up (1 month after completion of the parent-training module). Assignment of the parent–child dyads to the two experimental groups was balanced using a semi-random assignment strategy with group matching across child age and gender, parent’s education, and length of time the child has been receiving injections.
Both informed consent and assent were obtained from the parent and child, respectively, in accordance with institutional review board guidelines. Each group received one baseline observation, as well as two intervention sessions scheduled approximately 1 month apart wherein training was provided using verbal description, therapist modeling and behavioral rehearsal with therapist prompting, and both verbal and visual feedback (viewing portions of videotapes).
At each time point, parents completed the SEF and VAS rating forms. Child and parent also were videotaped at each time point in the clinic setting while (a) the parent performed an injection on the child and (b) during three non-medical situations (i.e., “Child’s Game,” “Parent’s Game,” “Clean Up”; Forehand & McMahon, 1981). At each intervention session, a 60-min training module was conducted. Following training, observations of the injection procedure and of non-medical interactions were conducted. The child and parent received cash remuneration for participating and a gift certificate after each completed session.
At baseline, parents completed the demographic form. The child was provided with the usual and customary procedures that the parent followed at home when performing the needle procedures, as prescribed by the child’s health care providers. During the videotaping of the parent-administered procedures, parents were instructed to “Prepare and perform the procedures just the way you are currently doing it at home.” No attempt was made to modify the parent’s routine or strategies in any way. At the conclusion of the session, the parent was informed about to which experimental condition parent and child were assigned, and an appointment for the next study session was scheduled.
The essential therapist responses for each of the intervention protocols were detailed in task-analysis data sheets detailing the precise protocol for each session. Therapists used these sheets to guide their protocol implementation and to document each step as they provided it.
Participants in the DIS condition received a parent-training module on the use of DIS during parent-administered injections (parent handouts are presented in Appendix A). The therapist explained the role of DIS in pain management (based on McCaul & Malott, 1984) and demonstrated the use of an electronic toy (standardized across participants) for DIS. The standard distracting toy was a LeapFrog LeapPad Learning System® (LeapFrog Enterprises, Emeryville, CA). This toy includes a system of interactive books and cartridges aimed at helping children learn the alphabet, numbers, phonics, vocabulary, spelling, and so forth at an age-appropriate level. Each book includes interactive games, activities, and stories. The child uses a “magic” pen to touch color pictures in the book and thereby hear words, letter sounds, numbers, and stories read aloud to answer questions and to receive verbal feedback. Parents were advised to, when possible, hold the toy in a way that interfered with the child’s view of the needle. Parents also were told to prompt the child to interact with the toy (e.g., by commenting on toy functions), encourage cooperation, and block or redirect avoidance behavior. Training consisted of verbal instruction, demonstration by the therapist, and role playing with the therapist, followed by a mock needle rehearsal with the child (e.g., using a needleless, empty syringe) and verbal and video feedback.
Participants in the GBM condition were provided a basic introduction to behavior principles and tactics for child behavior management via a parent-training module (parent handouts are shown in Appendix B). This parent training included verbal and written descriptions, modeling, role playing, and rehearsal of child behavior management strategies (e.g., use of labeled praise, giving effective instructions, differential positive reinforcement). The previous videotape was reviewed, and verbal feedback was provided.
RESULTS
Summary of Baseline Distress and Clinical Characteristics
At baseline, 61% of the children exhibited no distress during the first session (defined as OSBD total score <1). Among children who exhibited distress, the average total OSBD score was 3.8 (SD = 3.1). Similarly, 80% and 71% of the children exhibited no distress during the anticipatory and procedural OSBD phases, respectively, at baseline. Among the children who exhibited distress during these two phases, the average OSBD score was 3.6 (SD = 3.6) and 3.3 (SD = 2.8) for the anticipatory and procedural scales, respectively. There were no significant differences in the pattern of results across total, anticipatory, and procedural OSBD score; therefore, all subsequent discussions are based on the total OSBD scores only. The children had average CBCL total externalizing problems scores of 50.8 (SD = 15.5), with 2 children exhibiting clinical symptoms on this scale (i.e., scores >70). Mean time since diagnosis (in months) was 39.0 (SD = 30, Mdn = 34).
Association Between Baseline Characteristics and Distress
We found no statistically significant associations between the demographic variables and whether a child exhibited distress at baseline (based on the total OSBD score). In addition, we did not find any statistically significant differences in the distribution of OSBD scores across the categorical (binary) predictors among children with distress. Table 1 displays the results of the study based on the mean total distress (OSBD) scores and the fraction of observed children displaying no distress across sessions and groups.
TABLE 1.
Child Behavioral Distress Results Based on OSBD Scores Across Sessions and Treatment Groups
| Variable | Session | All Participants (N = 47) | DIS (n = 23) | GBM (n = 24) | p |
|---|---|---|---|---|---|
| Percentage of children with no distress (total OSBD ≤ 1.0) | 1 | 61.0 | 60.0 | 62.0 | >.99 |
| 2 | 68.0 | 58.0 | 76.0 | .31 | |
| 3 | 71.0 | 72.0 | 70.0 | >.99 | |
| Mean distress score among distressed children | 1 | 3.8 | 2.5 | 5.1 | .05 |
| 2 | 3.5 | 2.5 | 5.3 | .09 | |
| 3 | 4.2 | 2.1 | 5.9 | .25 | |
| Percentage of children that transitioned from distress to no distress | 1 to 2 | 21.0 | 14.0 | 29.0 | >.99 |
| 2 to 3 | 36.0 | 43.0 | 25.0 | >.99 | |
| Change in mean distress scores among distressed children | 1 to 2 | 0.2 | –0.6 | 1.1 | .43 |
| 2 to 3 | –0.9 | 0.2 | –2.4 | >.99 |
Note. OSBD = Observation Scale of Behavioral Distress; DIS = distraction; GBM = general behavior management.
Changes in Level of Distress Over Sessions
There were 19 children who exhibited no distress at any of the three sessions and 6 children who exhibited distress at all three sessions. The remaining 22 children fluctuated across sessions between levels of distress and no distress.
Compared to the 61% of children exhibiting no distress at baseline, 68% and 71% exhibited no distress during Sessions 2 and 3, respectively. A logistic regression model was used to compare the odds of no distress across the three sessions. There was no statistically significant difference in the odds of no distress across the three sessions.
Among children with distress during Session 1 (n = 16), 21% transitioned to no distress at Session 2 (confidence interval [CI .95] = 0%–43%). Among children with distress during Session 2 (n = 13), 36% transitioned to no distress during Session 3 (CI [.95] = 7%–65%). These transition probabilities were not statistically significant.
Among children with distress, the average level of total distress was 3.8 (SD = 3.1) at baseline, 3.5 (SD = 2.5) at Session 2, and 4.2 (SD = 5.7) at Session 3. Of the children who exhibited distress across any two consecutive sessions, the change in distress across consecutive sessions was not statistically significant (Wilcoxon’s signed rank test, p = .966 and p = .578, respectively).
Differences in OSBD Scores by Treatment Group
Among all children, 61% exhibited little or no distress during the first session. Among the 39% of children who exhibited distress at baseline, the mean total OSBD score was 3.8 (CI [.95] = 2.3–5.4). There was no statistically significant difference between the percentage of children in the DIS group (60%; CI [.95] = 38%–82%) and the percentage of children in the GBM group (62%; CI [.95] = 41%–83%) who exhibited no distress at baseline (p ≥ .99). Among children who exhibited distress during the first observation, the average total OSBD score was 2.5 (CI [.95] = 1.2–3.8) and 5.1 (CI [.95] = 2.6–7.7) for the DIS and GBM groups, respectively, which was a statistically significant difference (p = .05). There were no statistically significant differences across the DIS and GBM treatment groups in terms of likelihood to transition from distress to no distress, or the degree of change in distress scores.
Differences in the Ratio of Recommended to Non-Recommended Child Behavior Management Strategies by Treatment Group
The results for the ratio of recommended to non-recommended behavior management strategies are displayed in Figure 1. During Session 1, the average ratio of recommended to non-recommended child behavior management strategies was 0.5 and 0.4 for the DIS and GBM groups, respectively (0.3–0.7 for DIS; 0.3–0.6 for GBM), a difference that was not statistically significant (p = .62). There also were no statistically significant differences in the ratios by treatment group during Sessions 2 (p = .413) and 3 (p = .411).
FIGURE 1.
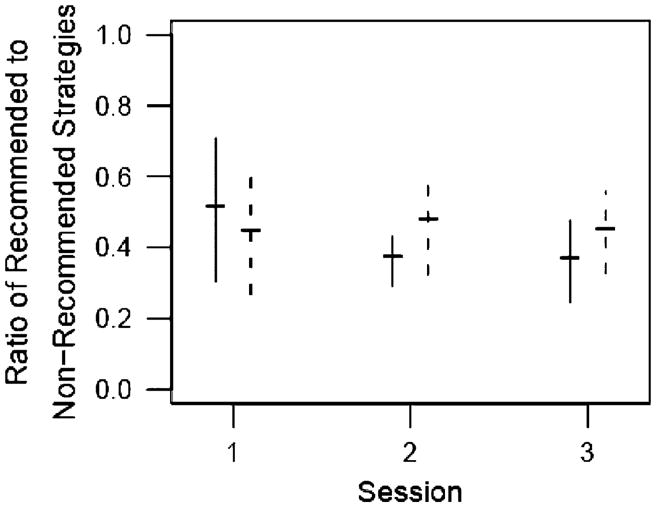
Ratio of recommended to non-recommended strategies.
From Session 1 to 2, the average changes in the ratio were 0.2 (CI [.95] = 0–0.4) and 0 (CI [.95] = –0.2–0.1) for the DIS and GBM groups, respectively, which was not a statistically significant difference across groups (p = .102). From Session 2 to 3, the average change in the ratio was 0 (CI [.95] = 0.1–0.1) and 0.1 (CI [.95] = 0–0.2) for the DIS and GBM groups, respectively (also not a statistically significant difference across groups, p = .922).
DISCUSSION
Results of our research indicated that the majority of children in this sample exhibited little to no behavioral distress during parent-administered needle procedures. The reason for these unexpected findings remains unclear, but the positive implication of these results is that children may have fewer than anticipated problems coping with parent-administered needle procedures. The unexpected, low levels of behavioral distress observed in this sample could be related to sample characteristics. Perhaps most important, we were not able to enroll our participants immediately after diagnosis and initiation of parent–administered needle procedures. Therefore, we may have missed the period of greatest distress for many of our participants. It is generally reported in the literature that procedural distress decreases with age. This sample also was homogenous in that almost all participating children displayed externalizing behavior within the normal range. In addition, the majority of participating children hailed from intact families (i.e., biological parents married and living in the same house as the child) of college-educated backgrounds. It is possible that these or other variables served to buffer against elevations in behavioral distress during parent-administered needle procedures. Future research should attempt to enroll participants immediately after beginning their parent-administered procedures and should include a more diverse sample across family characteristics to elucidate possible protective variables in the prevention or remediation of child procedural distress during parent-administered needle procedures.
The lack of significant differences between treatment groups may be due to the surprisingly low number of children who had distress and the modest magnitude of their distress. It is possible that, in a sample of children with a wider range of behavioral distress severity, there may have been greater potential for distress reduction by our interventions.
Finally, the interventions (parent training on the use of DIS to manage acute medical procedure-related child distress vs. parent training on child GBM strategies) were designed to be brief and feasible to teach in a busy pediatric clinic, but apparently were not sufficient to effect a significant change in the already low levels of distress observed in our study sample. Based on our parent treatment adherence integrity check with a sample of participating dyads, parents implemented strategies that were taught about one half (53%) of the time; this did not significantly differ across groups. However, the majority of participating parents exhibited no significant change in their displayed ratio of recommended versus non-recommended child behavior management behaviors from baseline and across session observations. This suggests that the children may not have come into contact with the interventions to a sufficient degree to derive significant benefits in behavioral distress reduction. This limited treatment amount resulting from only two treatment sessions seems to indicate that the interventions simply were too brief to change parent behavior at this level of analysis.
Because home care of children with chronic conditions will likely continue to rely on parents to perform repeated invasive procedures, a better understanding of other alternative variables that may predict behavioral adjustment problems should be pursued in future studies. Additional research comparing GBM parent training versus parent training on use of specific DIS strategies should be conducted with a more diverse sample; with participant enrollment immediately after diagnosis; with greater than two 1-hr intervention sessions; and, if possible, as a multi-site, randomized clinical trial.
Limitations of the Study
This study has several possible limitations that deserve discussion. First, this study evidenced some constraints on external validity—that is, the restricted geographical region in which data were collected, as well as several other homogeneous characteristics of the sample (e.g., predominately Caucasian children from families of mostly college-educated backgrounds), may limit the generalizability of the findings to other groups of children.
Another possible limitation is that, obviously, because of human participant considerations, participation was necessarily voluntary, which suggests the possibility of selection bias in that those families in greatest need may have declined participation because of time constraints, difficulties with transportation, or other unknown variables. For example, they may have avoided participation out of embarrassment about their child’s behavior or fear of judgment or other negative consequences, if their child’s difficulty with home-based medical procedures was fully known to their medical providers.
Another potential shortcoming of this study is its limited statistical power given the relatively small sample size examined. A larger and more diverse sample, particularly with respect to severity of child behavioral distress, likely would have yielded greater variability in outcome measures and, therefore, increased the opportunity for treatment effects to occur.
The limited treatment integrity of this study could pose another study limitation. Although it was a primary aim of this study to examine the efficacy of a brief intervention on behavioral distress reduction, it may have been helpful in interpreting the results of this study, had the brevity of the intervention been more systematically varied across participant groups to note any possible changes in treatment integrity as a result of the duration or intensity of the parent-training interventions. Future studies should include varying “doses” of intervention and examine the degree of association between amount of intervention provided and effects on behavioral distress. Similarly, a more fine-grained analysis of parent behavior may have provided more information regarding treatment integrity and the ability of parents to exhibit behavior change in response to this study’s brief intervention.
Implications for Practice
To conclude, most children undergoing parent-administered needle procedures exhibited minimal to no behavioral distress in this homogenous school-aged sample of children with chronic illness. Moreover, a comparison of two brief (i.e., two 1-hr sessions) interventions indicated no significant effects on child behavioral distress during a parent-administered needle procedure or on observed parent–child behavior management practices. Although plausible reasons for these findings can be generated, the unexpected nature of our results suggests, at the least, that this study deserves replication, perhaps while taking a broader approach. For example, a larger sample would increase statistical power to detect more subtle changes in behavior. A more diverse multi-site sample may result in a wider range of behavioral distress severity and greater opportunity for behavior change. A direct comparison of shorter versus lengthier parent-training intervention formats would allow for analysis of treatment duration on treatment integrity and behavior change. With a more extensive and diverse sample, various mediator and moderator relationships (Holmbeck, 1997) could be examined to identify possible predictors of and protective factors for behavioral distress.
Future studies should be conducted in close collaboration with clinic and home health nurses who can identify children and parents who show early evidence of behavioral distress when parent-administered needle procedures are first introduced. These parent–child dyads should be prospectively studied with repeated direct observations of child behavioral distress during needle procedures, as well as standard assessment of parent anxiety and self-efficacy about performing the procedures. This clinically referred group should be compared to an age-, gender-, and diagnosis-matched control group of children who exhibit little to no distress when the parent-administered procedures are performed. Ideally, the observations should be conducted in the home environment where the parent performs the procedures. Antecedent environmental variables plus observed and self-reported parent behavior, anxiety, and self-efficacy could then be related to child behavior in the distress group compared to the control group. Multiple regression or correlation analyses could be conducted to identify environmental, parent, and child variables most associated with high behavioral distress. This type of research may shed additional light on variables that predict high distress and those that could be modified to prevent or reduce child distress in vulnerable children or families.
Despite the shortcomings of this investigation, there are several tentative conclusions that can be drawn that have implications for treatment and prevention of problems with regard to child behavioral distress during parent-administered needle procedures in chronically ill children. The data suggest that many children with chronic illness requiring repeated, parent-administered needle procedures as part of their illness management regimen exhibit minimal to no behavioral distress during these procedures. However, even in this study conducted with a less diverse sample and in which the parent-administered needle procedures had begun prior to study enrollment, there was a small minority of children who experienced clinically significant behavioral distress and who may benefit from behavioral intervention with the parent and child. It would seem important to develop and refine efficient screening methods to identify these dyads, as well as clinical procedures for providing effective intervention resources to these more at-risk families.
APPENDIX A Parent Handout for Distraction Group
Using Distraction for Management of Chronic Pain
During periods of increased pain, it may be helpful for your child to participate in distracting activities. Any activity that diverts the child’s attention away from his or her pain may help to lessen it. The more concentration required for the activity, the better. It is particularly helpful if the activity is something interesting, fun, and pleasant.
General Tips
Participate in the activity with your child.
If the activity doesn’t hold your child’s interest, change activities.
Distraction may be combined with other pain management strategies, such as using a cold pack, repositioning, etc.
Distraction Bag
It may be helpful to create a distraction bag filled with your child’s favorite activities. Although these items do not have to be new, it may be helpful if they are not used/played with frequently.
Examples of Distraction for School Aged Kids
Conversation about preferred topics (favorite things, friends at school, etc.)
Singing
Interactive toys
Games
Bubbles
Party blowers
Cartoons or videos
Puzzles
Music
Stuffed animals
Examples of Distraction for Adolescents
Non-pain related conversation with family or friends
Handheld videogames
Portable DVD player
Crossword puzzles
Games
Books
Crafts
Gardening
Music
Card games
Relaxation Exercises (see additional handouts)
Utilize a relaxation CD or help coach your child through relaxation exercises (e.g., abdominal breathing, guided imagery) to help the patient focus on something other than his or her pain.
APPENDIX B Parent Handout for General Behavior Management Group
Effective Instructions and Guided Compliance
Teaching your child to comply with simple commands can be very helpful to you in managing your child’s behavior. It helps you learn effective ways of praising your child for doing things you like him/her to do. It also helps you teach your child how to gain attention and approval for appropriate behavior. Therefore, the way you issue instructions to your child is very important. By following these general guidelines, you can greatly increase the likelihood that your child will comply with your instructions.
Get your child’s attention BEFORE issuing an instruction. Do this by making direct eye contact with your child. You may need to bend your knees, say his/her name, and gently turn his/her face toward you to obtain direct eye contact.
Issue only one instruction at a time. Young children often get confused or overwhelmed when asked to do several things at one time. Therefore, it will be helpful for you to break down large tasks into small steps to obtain compliance. For example, if you want your child to complete his/her homework first say “Please sit in your chair.” Once your child has complied, then say “Open your math book.” Remember to always provide verbal praise and positive attention to your child when he/she complies with your instruction.
Be specific and clear. Use short sentences and specific words to give instructions. For example, if you want your child to clean up his/her room say “Put your shoes in the closet” rather than “Put your things away.”
Avoid using questions, especially those that have a yes/no answer. For example, avoid questions like “Are you ready to do your homework now?” because you have given your child the opportunity to say no. Simply say “It is time to do your homework now.”
Use “do” commands. Compliance often increases when you tell your child what you want him/her to do. For example, “Please walk” is a more effective statement than “Don’t run” when you are trying to increase compliance.
Provide enthusiastic praise immediately following compliance.
Common Mistakes
Offering a choice when there is no choice. For example, don’t ask your child if he/she wants to go to the grocery store with you if he/she must, in fact, accompany you to the grocery store. Simply state “It is now time to go to the grocery store”.
Contaminating verbal praise with a negative statement. For example, “You did a great job picking up the book. Why don’t you do that all the time when I ask?”
| Examples of Good Instructions | Examples of Poor Instructions |
|---|---|
| “Look at the picture” | “Be careful” |
| “Pull up your shirt sleeve” | “Calm down” |
| “Sit in the chair” | “Stop that” |
| “Give me your finger” | “Let’s put your toys away” |
| “Put your bear in the toy box” | “Can you put your toys away now?” |
What if my child does not comply with essential demands?
The following three-step sequence can be helpful for parents to use when essential demands (i.e., wearing a seat belt, checking blood sugar levels, brushing teeth, taking medicine, eating appropriate foods, etc.) need to be completed quickly and efficiently. This sequence also helps parents teach children they can not get out of completing essential demands
TELL your child what to do. For example, “Sit in the chair.” Be sure to be clear and concise. If your child completes the demand, provide verbal praise (e.g., “Great job sitting in the chair!”)
If your child does not complete the essential demand within five seconds, provide him/her with a VERBAL WARNING: “Sit in the chair or I will help you.” If he/she completes the demand, provide verbal praise (e.g. “Great job sitting in the chair!”).
If your child does not complete the demand following the verbal warning, PHYSICALLY GUIDE him/her using as little contact as necessary to complete the demand. For example, lightly guide him/her by the arm toward the chair and repeat the verbal prompt, “You need to sit in the chair.” Always use the minimum amount of physical contact necessary for the request to be completed. Gradually, remove physical contact as your child begins to comply. Provide verbal praise when your child complies with the instruction (e.g., “Great job sitting in the chair!”).
Positive Attention
One of the most important rules about human behavior is: Behaviors that are rewarded will increase in frequency.
Giving positive attention for good behaviors (those you want your child to do more often) is a good way to teach children to behave better. Most children enjoy getting attention from adults. We say that positive attention motivates children to continue being good. During this part of our training you will practice the skills we call “paying attention” and learn how to use these positive-attending skills to strengthen your child’s good behavior such as following your instructions.
The rule of thumb is to give positive attention to your child whenever there is an opportunity. We call this “catching kids being good.” Here are the steps we want you to practice.
Watch what your child is doing.
Select a behavior that you want your child to do more often (following your instructions, waiting patiently, playing quietly, etc.)
Give positive attention immediately following that behavior.
To give positive attention, make eye contact with your child, speak enthusiastically, and tell your child exactly what he or she did that pleased you, then express your pleasure with praise, a smile, quick hug, kiss, pat on the back, “thumbs-up,” “high-five,” or promise of a specific treat or privilege.
If you promise a treat or privilege, keep your promise at the time you promised!
Common Mistakes or Misconceptions
In many families good behavior goes unnoticed and bad behavior gets all the attention.
Parents think they should “leave well enough alone” and ignore calm, pleasing behavior because praising good behavior will disrupt it and cause your child to misbehave. (It might at first, but once your child is used to it, it simply teaches that good behavior will get your attention).
Don’t sneak in criticism for past behavior! (“You did a great job sitting still! Why didn’t you do that when I told you before.”)
If you promise a reward, don’t try to back out of it or tell your child you will do it another time. Give it when you said you would.
Examples of Giving Positive Attention
Your child is playing quietly with a toy while you are talking on the phone. You notice the good behavior and politely interrupt your call for the few seconds it takes to lean over, gently touch your child on the shoulder and whisper, “You are playing so nicely, when I finish talking to uncle John, I will play with you for a little while.”
You take your child to the doctor for a check-up. When you get to the waiting area, you tell your child to sit down and look at a child’s book you brought along. Your child sits down and opens the book. You give her a quick kiss on the top of her head and say, “It is so nice when you do what I tell you right away.”
You and your child are getting out of the car at the supermarket. You tell your child to hold your hand to walk to the store from the parking lot. Your child whines a little, but takes your hand. You ignore the whining and say, “That was good listening. I like it when you hold my hand so I can keep you safe.” Your child looks at you and you smile back.
Your child is playing all by herself in the living room with an electronic toy. You look in from the kitchen (where you are cleaning up the dinner dishes). You take a very brief break, walk near your child and say, “I really like that you are keeping yourself busy while I finish my work in the kitchen. I’m so proud of you. I’ll be finished soon and then I can read to you from your storybook.” You return to the kitchen.
Planned Ignoring
Another important rule about human behavior is: Behaviors that are not rewarded with attention will decrease in frequency.
Ignoring is a highly effective technique to reduce inappropriate behavior. It is effective because children are often seeking adult attention by misbehaving. When attention is not provided (i.e., when it is ignored), the behavior decreases. However, ignoring is often difficult for parents to carry out. During this part of our training you will practice the skills we call “planned ignoring,” and learn how to use this skill to decrease your child’s inappropriate behavior.
It is important to know which behaviors to ignore. Ignore only those behaviors that will not be harmful or dangerous to your child. For example, it is not safe to ignore running out into the street or sticking fingers into electrical sockets. You should also not ignore aggressive behavior or property destruction. Examples of inappropriate behaviors that should be ignored are whining, crying, teasing, arguing, tantrums, screaming, interrupting, or making faces. If your child is engaging in a behavior that cannot be ignored, you must interrupt the behavior and physically prevent it from occurring again.
The rule of thumb is to be careful to remove all attention to your child for misbehavior when it is occurring. Here are some tips on how to use effective ignoring.
Ignoring means not looking at your child at all or giving any nonverbal cues (laughing, rolling your eyes, making a face) during the inappropriate behavior. Break eye contact and keep your expression neutral.
Ignoring means not talking to your child about the behavior at all. Do not tell your child that you are ignoring him/her, and do not comment to others around you about the behavior.
Ignoring means no physical contact with your child during the inappropriate behavior. Once you start ignoring the behavior, it is possible that your child will attempt to get your attention in some manner (e.g., climb on your lap, yell/scream, tug on your clothing). Stand up and/or walk away if possible.
While the inappropriate behavior is occurring, it is important to continue to do whatever you were doing before your child displayed the behavior. For instance, if you were giving a demand to your child, continue to give the demand despite whining or some other inappropriate behavior.
As soon as the inappropriate behavior ceases, it is very important to redirect your child back to the activity or conversation that was going on before the behavior occurred or to another activity or conversation.
As soon as the problem behavior ceases and your child engages in some other activity or appropriate behavior, look for something you can reward. Try to give your child positive attention within 30 seconds of the stopped behavior. This is a very important time to teach your child what behaviors are inappropriate and will be ignored, and which behaviors are appropriate and will get your positive attention.
Common Mistakes and Misconceptions
In many families, inappropriate behavior may get attention while good behavior may get ignored.
Parents sometimes think that ignoring inappropriate behavior means that they are “not doing anything” to change or “fix” the behavior, and think that scolding and other forms of attention are a more appropriate response. For many children, any attention (even negative, such as scolding) may result in the continuation or increase of the behavior, while ignoring may teach them that they must have positive behavior to get attention.
Examples of Effective Planned Ignoring
You tell your child to play quietly while you talk on the phone. Your child begins to whine. You do not make eye contact or comment on the behavior, but continue to talk on the phone. After a few minutes, your child gets tired of whining and begins to play with a toy. You briefly leave your phone conversation to praise your child for playing nicely.
It is time to give your child his/her medicine. Your child makes a face and says that he/she hates the taste. You do not make any comment, but continue getting what you need to give the medicine (medication, spoon, etc.). You tell your child in a neutral tone of voice “it is time to take your medicine”. Despite making more faces, you child takes his/her medicine. You immediately give praise for taking it.
Contributor Information
Keith J. Slifer, Department of Behavioral Psychology, The Kennedy Krieger Institute, Baltimore, MD, The Johns Hopkins University School of Medicine, Baltimore, MD
Melissa DeMore, Department of Behavioral Psychology, The Kennedy Krieger Institute, Baltimore, MD, The Johns Hopkins University School of Medicine, Baltimore, MD.
Natalie Vona-Messersmith, Department of Behavioral Psychology, The Kennedy Krieger Institute, Baltimore, MD, The Johns Hopkins University School of Medicine, Baltimore, MD.
Valerie Pulbrook-Vetter, Department of Behavioral Psychology, The Kennedy Krieger Institute, Baltimore, MD.
Melissa Beck, Department of Behavioral Psychology, The Kennedy Krieger Institute, Baltimore, MD, The Johns Hopkins University School of Medicine, Baltimore, MD.
Lynnda Dalhquist, Department of Psychology, University of Maryland, Baltimore County, Baltimore, MD.
Kimberly Bellipanni, Department of Behavioral Psychology, The Kennedy Krieger Institute, Baltimore, MD, The Johns Hopkins University School of Medicine, Baltimore, MD.
Elizabeth Johnson, Department of Biostatistics, The Johns Hopkins University School of Medicine, Baltimore, MD.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- Achenbach TM. Manual for the Child Behavior Checklist/2–3 and 1992 profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1992. [Google Scholar]
- Anderson CTM, Zelter LK, Fanurik D. Procedural pain. In: Schechter NL, Berde CV, Yaster M, editors. Pain in infants, children and adolescents. Baltimore, MD: Williams & Wilkins; 1993. pp. 435–458. [Google Scholar]
- Arts S, Abu-Saad H, Champion G, Crawford M, Fisher R, Juniper K, et al. Age-related response to lidocaine-prilocaine (EMLA) emulsion and effects of music distraction on the pain of intravenous cannulation. Pediatrics. 1994;93:797–801. [PubMed] [Google Scholar]
- Bailey JS, Bostow DE. Research methods in applied behavior analysis. Tallahassee, FL: Copy Grafix; 1979. [Google Scholar]
- Bakeman R, Gottman JM. Observing interaction: An introduction to sequential analysis. New York: Cambridge University Press; 1986. [Google Scholar]
- Blount RL, Landolf-Fritsche B, Powers SW, Sturges JW. Differences between high and low coping children and between parent and staff behaviors during painful medical procedures. Journal of Pediatric Psychology. 1991;16:795–809. doi: 10.1093/jpepsy/16.6.795. [DOI] [PubMed] [Google Scholar]
- Blount RL, Piira T, Cohen LL. Management of pediatric pain and distress due to medical procedures. In: Roberts M, editor. Handbook of pediatric psychology. 3. New York: Guilford; 2003. pp. 216–233. [Google Scholar]
- Blount RL, Powers SW, Cotter MW, Swan S, Free K. Making the system work: Training pediatric oncology patients to cope and their parents to coach them during BMA/LP procedures. Behavior Modification. 1994;18:6–31. doi: 10.1177/01454455940181002. [DOI] [PubMed] [Google Scholar]
- Caire JB, Erickson S. Reducing distress in pediatric patients undergoing cardiac catheterization. Children’s Health Care. 1986;14:146–152. doi: 10.1207/s15326888chc1403_4. [DOI] [PubMed] [Google Scholar]
- Cohen LL, Blount RL, Cohen RJ, Schaen ER, Zaff JF. Comparative study of distraction versus topical anesthesia for pediatric pain management during immunizations. Health Psychology. 1999;18:591–598. doi: 10.1037//0278-6133.18.6.591. [DOI] [PubMed] [Google Scholar]
- Cohen LL, Blount RL, Panopoulos G. Nurse coaching and cartoon distraction: An effective intervention to reduce child, parent and nurse distress during immuninzations. Journal of Pediatric Psychology. 1997;22:355–370. doi: 10.1093/jpepsy/22.3.355. [DOI] [PubMed] [Google Scholar]
- Dahlquist L. Coping with aversive medical treatments. In: LaGreca A, Siegel L, Wallander J, Walker W, editors. Stress and coping in child health. New York: Guilford; 1992. pp. 345–376. [Google Scholar]
- Dahlquist L. Pediatric pain management. New York: Plenum; 1999. [Google Scholar]
- Dahlquist L, Gil KM, Armstrong FD, DeLawyer D, Greene P, Wuori D. Preparing children for medical examinations: The importance of previous medical experience. Health Psychology. 1986;5:249–259. doi: 10.1037//0278-6133.5.3.249. [DOI] [PubMed] [Google Scholar]
- Dahlquist L, McKenna K, Jones KK, Dillinger L, Weiss KE, Sonntag C. Active and passive distraction using a head-mounted display helmet: Effects on cold pressor pain in children. Health Psychology. 2007;26:794–801. doi: 10.1037/0278-6133.26.6.794. [DOI] [PubMed] [Google Scholar]
- Dahlquist L, Pendley JS. When distraction fails: Parental anxiety and children’s responses to distraction during cancer procedures. Journal of Pediatric Psychology. 2005;30:623–628. doi: 10.1093/jpepsy/jsi048. [DOI] [PubMed] [Google Scholar]
- Dahlquist L, Pendley J, Landthrip D, Jones C, Steuber CP. Distraction intervention for preschoolers undergoing intramuscular injections and subcutaneous port access. Health Psychology. 2002;21:94–99. [PubMed] [Google Scholar]
- DeMore M, Cohen LC. A critical review of distraction interventions for pain management during childhood immunizations. Journal of Clinical Psychology in Medical Settings. 2005;12:281–291. [Google Scholar]
- Elgar FJ, McGrath PJ. Self-administered psychosocial treatments for children and families. Journal of Clinical Psychology. 2003;59:321–339. doi: 10.1002/jclp.10132. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Robinson EA. Parent–child interaction training: Effects on family functioning. Journal of Clinical Child Psychology. 1982;11:130–137. [Google Scholar]
- Fanurik D, Koh J, Schmitz M, Brown R. Pharmacological intervention: Integrating pharmacologic and behavioral techniques for pediatric medical procedures. Children’s Health. 1997;26:31–46. [Google Scholar]
- Forehand RL, McMahon RJ. Helping the noncompliant child: A clinicians guide to parent training. New York: Guilford; 1981. [Google Scholar]
- Fowler-Kerry S, Lander JR. Management of injection pain in children. Pain. 1987;30:69–175. doi: 10.1016/0304-3959(87)91072-4. [DOI] [PubMed] [Google Scholar]
- French G, Painter E, Coury S. Blowing away shot pain: A technique for pain management during immunizations. Pediatrics. 1994;93:384–388. [PubMed] [Google Scholar]
- Gonzalez JC, Routh DK, Armstrong FD. Effects of maternal distraction versus reassurance on children’s reactions to injections. Journal of Pediatrics Psychology. 1993;18:593–604. doi: 10.1093/jpepsy/18.5.593. [DOI] [PubMed] [Google Scholar]
- Hembree-Kigin TL, McNeil C. Parent–child interaction therapy. New York: Plenum Press; 1995. [Google Scholar]
- Holmbeck GN. Toward terminological, statistical, and conceptual clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology. 1997;65:599–610. doi: 10.1037//0022-006x.65.4.599. [DOI] [PubMed] [Google Scholar]
- Jacobson RM, Swan A, Adegbenro A, Ludington SL, Wollan PC, Poland GA. Making vaccines more acceptable—Methods to prevent and minimize pain and other common adverse events associated with vaccines. Vaccine. 2001;19:2418–2427. doi: 10.1016/s0264-410x(00)00466-7. [DOI] [PubMed] [Google Scholar]
- Jacox A, Carr DB, Payne R. New clinical practice guidelines for management of pain in patients with cancer. The New England Journal of Medicine. 1994;330:651–655. doi: 10.1056/NEJM199403033300926. [DOI] [PubMed] [Google Scholar]
- Jay SM. Invasive medical procedures: Psychology intervention and assessment. In: Routh DK, editor. Handbook of pediatric psychology. New York: Guilford; 1988. pp. 401–425. [Google Scholar]
- Jay SM, Elliott CH, Katz E, Siegel S. Cognitive behavioral and pharmacologic interventions for children’s distress during painful medical procedures. Journal of Consulting and Clinical Psychology. 1987;55:860–865. doi: 10.1037//0022-006x.55.6.860. [DOI] [PubMed] [Google Scholar]
- Jay SM, Elliott CH, Ozolins RA, Pruitt SD. Behavioral management of children’s distress during painful medical procedures. Behavior Research Therapy. 1985;23:513–520. doi: 10.1016/0005-7967(85)90098-1. [DOI] [PubMed] [Google Scholar]
- Jay SM, Ozolins M, Elliott CH, Caldwell S. Assessment of children’s distress during painful medical procedures. Health Psychology. 1983;2:133–147. [Google Scholar]
- Manne S, Redd W, Jacobson P, Gorfinkle K, Schorr O, Rapkin B. Behavioral intervention to reduce child and parent distress during venipuncture. Journal of Consulting and Clinical Psychology. 1990;58:565–572. doi: 10.1037//0022-006x.58.5.565. [DOI] [PubMed] [Google Scholar]
- Mason S, Johnson MH, Woolley C. A comparison of distractors for controlling distress in young children during medical procedures. Journal of Clinical Psychology in Medical Settings. 1999;6:239–248. [Google Scholar]
- McCaul KD, Malott JM. Distraction and coping with pain. Psychological Bulletin. 1984;95:516–533. [PubMed] [Google Scholar]
- Melamed BG, Robbins RL, Graves S. Preparation for surgery and medical procedures. In: Russo DC, Varni JW, editors. Behavioral pediatrics: Research and practice. New York: Plenum; 1982. pp. 225–267. [Google Scholar]
- Pate JT, Blount RI, Cohen LL, Smith AJ. Childhood medical experience and temperament as predictors of adult functioning in medical situations. Children’s Health Care. 1996;25:281–296. [Google Scholar]
- Powers SW. Empirically supported treatments in pediatric psychology: Procedure-related pain. Journal of Pediatric Psychology. 1999;24:131–145. doi: 10.1093/jpepsy/24.2.131. [DOI] [PubMed] [Google Scholar]
- Powers SW, Blount RL, Bachanas PJ, Cotter MW, Swan SC. Helping preschool leukemia patients and their parents cope during injections. Journal of Pediatric Psychology. 1993;18:681–695. doi: 10.1093/jpepsy/18.6.681. [DOI] [PubMed] [Google Scholar]
- Princeton Survey Research Associates. Benchmark surveys on childhood immunization. Princeton, NJ: Gallup Poll; 1996. [Google Scholar]
- Pringle B, Hilley L, Gelfand K, Dahlquist LM, Switkin M, Diver T, et al. Decreasing child distress during needle sticks and maintaining treatment gains over time. Journal of Clinical Psychology in Medical Settings. 2001;8:119–130. [Google Scholar]
- Taddio A, Goldbach M, Ipp M, Stevens B, Koren G. Effect of neonatal circumcision on pain response during vaccination in boys. Lancet. 1995;345:291–292. doi: 10.1016/s0140-6736(95)90278-3. [DOI] [PubMed] [Google Scholar]
- Weekes DP, Savedra MS. Adolescent cancer: Coping with treatment-related pain. Journal of Pediatric Nursing. 1988;3:318–328. [PubMed] [Google Scholar]


