EDUCATIONAL OBJECTIVES.
Understand the prevalence of co-occurring anxiety disorders and substance use disorders.
List the major diagnostic considerations in assessing co-occurring anxiety disorders among individuals with substance use disorders.
Demonstrate awareness of the pharmacologic and psychosocial treatments to date in this area.
Anxiety disorders, symptoms of anxiety, and substance use disorders (SUDs) commonly co-occur. The interactions between SUDs and anxiety are multifaceted and variable. Symptoms of anxiety often emerge during the course of chronic intoxication and withdrawal from a number of substances. Anxiety disorders are a risk factor for the development of SUDs and may modify the presentation and course of illness for SUDs. Similarly, SUDs may modify the presentation and course of anxiety disorders. In this article, co-occurring SUDs and anxiety disorders will be briefly reviewed, including prevalence, diagnostic issues, and treatment options.
EPIDEMIOLOGY
The most recent and largest (N > 43,000) comorbidity study to date, the National Epidemiological Survey on Alcohol and Related Conditions (NESARC), found that 17.7% of respondents with a current SUD also met criteria for an anxiety disorder.1 Treatment-seeking samples also demonstrate high rates of comorbid anxiety and SUDs. One study of 422 outpatients in the United States with opioid use disorders reported that 12% of men and 21% of women met criteria for a lifetime anxiety disorder.2 Merikangas and colleagues3 found that, in general, anxiety disorders precede the development of co-occurring alcohol (57% to 80%) and drug (67.6% to 100%) use disorders.
SCREENING AND DIFFERENTIAL DIAGNOSIS
One of the greatest difficulties in the area of co-occurring anxiety and SUDs is that of differential diagnosis. Substances of abuse impact the neurotransmitter systems involved in the pathophysiology of anxiety disorders and may unmask vulnerability or lead to organic changes that manifest as an anxiety disorder. The best way to differentiate substance-induced, transient symptoms of anxiety from anxiety disorders that warrant treatment is through observation of symptoms during a period of abstinence. Transient substance-induced symptoms improve with time. The duration of abstinence necessary for accurate diagnosis remains controversial and is likely to be based on both the diagnosis being assessed and the substance used. Long half-life drugs (eg, some benzodiazepines, methadone) may require several weeks of abstinence for withdrawal symptoms to subside. However, shorter-acting substances (eg, alcohol, cocaine, short half-life benzodiazepines) require shorter periods of abstinence to make valid diagnoses. A family history of anxiety disorder, the onset of anxiety symptoms before the onset of the SUD, and sustained anxiety symptoms during lengthy periods of abstinence all suggest an anxiety disorder that will need to be addressed with specific treatment.
ETIOLOGIC CONNECTIONS
A number of recent studies have focused on exploration of the etiologic relationships between anxiety and SUDs. Studies do not consistently support “self-medication” as an explanation for the relationship between anxiety and substance use. Although some substances can provide short-term relief of anxiety symptoms, in general there is anxiety induction with chronic substance use and withdrawal, which can initiate a feed-forward cycle of increasing anxiety symptoms and substance consumption.4
In the basic science arena, the role of neuroadaptation and stress in relapse to substance use has been an area of intense investigation. Corticotrophin releasing hormone (CRH), one of the key hormones involved in the stress response, has been implicated in the pathophysiology of anxiety, as well as in addictive disorders.5 Nor-adrenergic and other neurotransmitter systems, as well as endogenous opiates, may also provide a neurobiologic link between anxiety and substance use disorders.
GENERAL TREATMENT CONSIDERATIONS
In general, treatment efforts addressing anxiety disorders and SUDs have developed in parallel. The integration of effective treatments from both fields will be critical to the optimal treatment of individuals with co-occurring disorders. It is important to maximize the use of nonpharmacologic treatments. Learning strategies to self-regulate anxiety symptoms can interrupt the “self-medication” cycle and help individuals to acquire alternative coping strategies. Among psychosocial treatments, cognitive behavioral therapies (CBT) are among the most effective for both anxiety disorders and SUDs. Promising pilot work investigating the integration of treatments to develop therapies specifically targeting co-occurring disorders will be discussed in the sections that follow.
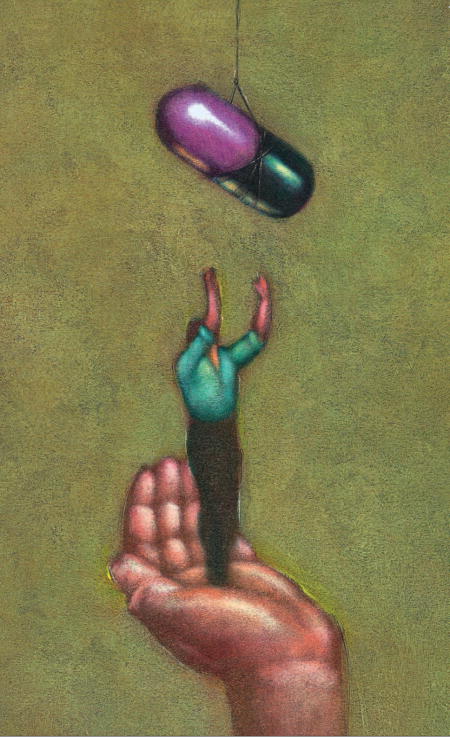
Research investigating pharmacotherapeutic treatments for both SUDs and anxiety disorders is progressing rapidly. The pharmacotherapeutic treatment of specific anxiety disorders will be discussed, but there are some general issues that apply to the treatment of co-occurring disorders, which will be discussed in this section. First, individuals in recovery from SUDs may have complex and conflicting feelings about the use of medications and may see the need for medications as a sign of defectiveness or failure. It is important to proactively discuss feelings and attitudes about medications and emphasize the need for medication adherence before prescribing. In cases where the relationship of psychiatric symptoms and substance use is unclear, the risk/benefit ratio of using medications must be carefully considered. When medications are used, treatment should generally follow routine clinical practice for treatment of the anxiety disorder with some exceptions. It is important to consider potential toxic interactions between the prescription medications and substances of abuse, in case relapse should occur. It is also important to use the agent with the least abuse potential. Despite their effectiveness in immediate relief of panic and other anxiety symptoms, benzodiazepines are generally not considered a “first-line” of treatment for SUD patients because of abuse potential. They may be considered as adjunctive medication during the early treatment phase when activation or latency of onset of the antidepressants is an issue. If a benzodiazepine is prescribed to a patient with a co-occurring SUD, close monitoring for relapse and limited amounts of medication should be given. Medication adherence contracts, similar to those used with chronic pain patients receiving prescription opioids, may also be useful in patients with a co-occuring SUD.
Finally, the use of agents specifically targeting SUDs in individuals with co-occurring anxiety disorders is under-explored. In one study of 254 outpatients with alcohol dependence and a variety of comorbid psychiatric disorders, Petrakis and colleagues6 investigated the efficacy of disulfiram and naltrexone, or their combination, in a 12-week randomized trial. Participants treated with either medication had significantly more consecutive weeks of abstinence and fewer drinking days per week. The effects of the medications by specific comorbid psychiatric disorder were not discussed, but active medication was associated with greater anxiety symptom improvement. No clear advantage of combining medications was observed.
In the sections that follow, the prevalence rates, differential diagnosis and treatment of specific anxiety disorders will be briefly reviewed.
SPECIFIC DISORDERS
Generalized Anxiety Disorder
SUDs are one of the most common comorbid psychiatric disorders among individuals with generalized anxiety disorder (GAD).7 A recent epidemiologic study of 5,877 adults found that GAD was the anxiety disorder most often associated with using alcohol or drugs to self-medicate symptoms.8 Comorbid GAD is associated with an accelerated progression from first use to the onset of dependence,9 and the presence of comorbid SUDs has been shown to significantly decrease the likelihood of recovery from GAD.10
As GAD symptoms can be mimicked by substance use or withdrawal, diagnostic complications can arise. Assessment of GAD should be delayed until intoxication or withdrawal has terminated. For short-acting drugs (eg, cocaine), it may be possible to assess GAD after one week of abstinence, but longer periods of time (eg, 4 to 8 weeks) may be required for longer-acting drugs (eg, methadone, valium).11 Patients should also be assessed for use of over-the-counter substances that can induce anxiety (eg, caffeine, diet pills). The Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV), requires that a core number of anxiety symptoms be present for at least 6 months in order to meet diagnostic criteria for GAD. Substance use during those 6 months needs to be considered. Symptoms of GAD must have been present during times other than when the patient was using or recovering from alcohol or drugs. This can be challenging to assess because many SUD patients presenting for treatment and complaining of anxiety will not have had 6 months of abstinence.
The treatment of GAD in the context of addiction can also be challenging. Although benzodiazepines are effective in the treatment of GAD, their use in individuals with current or former SUDs is controversial because of their abuse liability. Some authors suggest, however, that the empirical evidence regarding these concerns is lacking. They also suggest that benzodiazepines may be safely used to treat anxiety disorders in some SUD patients.12 Buspirone, a partial 5-hydroxytryptamine [5-HT]1A agonist with low abuse potential, has been shown to be efficacious in some studies in anxious alcoholics,11,13,14 but the results are mixed.15,16 Selective serotonin reuptake inhibitors (SSRIs) are efficacious in reducing GAD symptoms;17 however, no clinical trials of SSRIs among comorbid GAD/SUD patients have been conducted.
Among psychosocial treatments, CBT may help decrease both anxiety symptoms and risk of relapse. Patients with both GAD and SUDs may benefit from education surrounding relaxation techniques, coping skills, cognitive restructuring, behavioral activation, problem solving, and sleep hygiene.11 Nutritional counseling and regular exercise may also prove to be beneficial for GAD/SUD patients, although empirical trials are lacking.
Posttraumatic Stress Disorder
The National Comorbidity Study (NCS) found that adults with posttraumatic stress disorder (PTSD) were two to four times more likely to have a comorbid SUD as compared with those without PTSD.18 Similarly, data from a more recent multisite longitudinal study of almost 1,000 individuals showed that a history of PTSD predisposes individuals to elevated rates of drug abuse and dependence.19 Among treatment-seeking substance abusers, the prevalence of lifetime PTSD has been reported as high as 50% or greater.20 In the majority of cases, the development of PTSD precedes the development of the SUD.21
In comparison with other anxiety disorders, there is greater empirical research on the treatment of comorbid PTSD and SUDs. In a double-blind, placebo-controlled, 12-week trial, Brady and colleagues22 investigated the use of sertraline, which has been approved by the Food and Drug Administration (FDA) for the treatment of PTSD. The study included 94 individuals with PTSD and alcohol dependence. Individuals with less severe alcohol dependence and early onset PTSD demonstrated greater improvement in alcohol use severity when treated with sertraline as compared to placebo. Among 254 out-patients with alcohol dependence and comorbid psychiatric disorders (42.9% met DSM-IV criteria for comorbid PTSD), Petrakis and colleagues6 found that patients treated with naltrexone or disulfiram, as compared with placebo, had more consecutive weeks of abstinence and fewer drinking days per week. In comparison with naltrexone-treated participants, disulfiram-treated participants reported less craving from pre- to post-treatment. No clear advantage of combining disulfiram and naltrexone was observed.
A number of investigations of integrative psychotherapies have demonstrated that addressing trauma/PTSD among SUD patients is beneficial and typically leads to significant reductions in both PTSD and SUD symptoms. The most widely studied integrated therapy to date is Seeking Safety (SS), a 25-session, manualized treatment that provides psychoeducation and teaches coping skills.23 In a controlled study,24 107 women were randomized to SS, relapse prevention (RP), or treatment-as-usual (TAU). Patients who received TAU failed to show improvement (and in the case of PTSD symptoms, worsened over time), while patients who received either SS or RP demonstrated significant improvement in substance use, PTSD, and global psychiatric symptoms. No significant difference between SS and RP treatment groups were observed.
To date, two small studies have systematically examined treatments that integrate gold-standard exposure-based techniques for PTSD with empirically validated treatments for SUDs. Triffleman and colleagues developed a 20-week, manualized treatment that utilizes RP, coping skills, psychoeducation, and in vivo exposure. In a small (N = 19) pilot trial it was shown to be as effective as, but not superior to, Twelve-Step Facilitation Therapy with regard to PTSD symptoms and drug use.25 In another uncontrolled trial (N = 39), Brady and colleagues26 developed a 16-session, manualized treatment consisting of combined imaginal and in vivo exposure therapy for PTSD and cognitive-behavioral RP techniques for cocaine dependence. The intervention was associated with significant reductions in all three clusters of PTSD symptoms and cocaine use. Several other studies have preliminarily explored the use of psychosocial treatments among SUD/PTSD patients with favorable results.27,28 Although more randomized, controlled trials in this area are needed, the studies to date demonstrate that for the majority of SUD/PTSD patients, addressing PTSD confers substantial therapeutic benefits.
Social Phobia
Data from the NCS found that 16.4% of socially phobic individuals endorsed self-medicating with alcohol and drugs.29 Individuals with social phobia (SP) are two to three times more likely than individuals without SP to develop an alcohol use disorder.30 As the average onset of social phobia is before adolescence, symptoms of social anxiety typically precede the initiation of alcohol or drug use.31
In a placebo-controlled trial, Randall and colleagues32 examined the effectiveness of paroxetine, an SSRI, in 15 outpatients with alcohol dependence and SP. The paroxetine-treated group had significantly lower SP symptoms at the end of the 8-week trial, as compared with the placebo group; however, no significant group differences in measures of alcohol use severity were revealed. Gabapentin is an anticonvulsant agent with demonstrated efficacy in the treatment of SP.33 This is of particular interest because gabapentin has also demonstrated efficacy in the treatment of alcohol withdrawal34 and unlike benzodiazepines, gabapentin has no abuse potential. One case report of a polysubstance-dependent individual with comorbid SP who was treated with gabapentin documented significant improvement in craving and substance use,35 but there are currently no controlled trials examining the efficacy of gabapentin in co-occurring SP and SUDs.
Several controlled trials have examined the efficacy of psychosocial treatments for SP/SUD patients. In 93 outpatients with comorbid SP and alcohol dependence, Randall and colleagues36 compared a 12-week, manual-based CBT for alcohol dependence with an integrated manual-based CBT for both disorders. Contrary to expectations, patients who received the alcohol dependence-only treatment evidenced better outcomes than patients who received the integrated treatment. Although the reasons for this unexpected finding are unclear, the authors hypothesized that exposure to feared social situations during early recovery may have led to increases in alcohol use to cope. Schade and colleagues37 randomly assigned 96 individuals with alcohol dependence and comorbid SP and/or agoraphobia to receive relapse prevention (RP), or RP plus CBT for the anxiety disorder. The majority (89/96) of the sample had SP. Both groups were offered concomitant SSRI pharmacotherapy (fluvoxamine), but almost half (53%) refused it. Individuals who received the combined psychosocial treatment (alcohol + anxiety) had significantly greater improvement in anxiety symptoms than those who received treatment addressing alcohol dependence only. No significant differences between groups in alcohol use severity were observed and the use of fluvoxamine was not associated with improved anxiety or alcohol use severity outcomes.
Obsessive-compulsive Disorder
In comparison with other anxiety disorders, the association between obsessive compulsive disorder (OCD) and SUDs is less robust.38 For example, in a clinical sample of 254 individuals, approximately 4% of OCD patients met criteria for a lifetime SUD.39 The lower rates of OCD among SUD patients may be due, in part, to the generally low levels of impulsive or spontaneous behaviors and high levels of harm avoidance exhibited among individuals with OCD. When OCD patients do use substances, they typically choose sedating agents (eg, alcohol, marijuana).
Some substances of abuse (eg, alcohol, stimulants) and medications (eg, benzodiazepines) can produce obsessive-compulsive behaviors.11,40 This potential confound should be ruled out when diagnosing OCD among SUD patients. In general, the differential diagnosis of OCD in individuals with SUDs is not as difficult as that of some of the other anxiety disorders because there is less symptom overlap. For SUD patients, the content of obsessions and compulsions is restricted to alcohol or drug use. Obsessions and compulsions focused on procuring and using drugs alone, or that occur only during intoxication, do not meet diagnostic criteria for OCD.
Little research on the treatment of co-occurring OCD and SUDs has been conducted to date. There are no randomized controlled trials examining the use of a pharmacologic treatment for this patient population. SSRIs have been shown to be effective in treating OCD among non-substance dependent patients41 and would likely be helpful among SUD patients, but this has not been systematically tested. One controlled clinical trial has demonstrated promising results for an integrated OCD/SUD psychotherapy.42
CONCLUSIONS
Interest in the co-occurrence of anxiety disorders and SUDs has grown tremendously in recent years, as the evidence of the prevalence and impact of comorbidity has become increasingly clear. There have been a number of recent advances in the treatment of both anxiety disorders and SUDs, and treatment addressing both disorders can improve long-term therapeutic outcomes. Specific considerations in choosing a pharmacologic agent for use in patients with SUDs include safety, toxicity, and abuse liability. In conclusion, although the co-occurrence of SUDs and anxiety disorders is an important area in which recent developments provide cause for considerable optimism, much work remains to be done.
Footnotes
Dr. Back and Dr. Brady have disclosed no relevant financial relationships.
References
- 1.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch General Psych. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 2.Kidorf M, Disney ER, King VL, Neufeld K, Beilenson PL, Brooner RK. Prevalence of psychiatric and substance use disorders in opioid abusers in a community syringe exchange program. Drug Alcohol Depend. 2004;74(2):115–122. doi: 10.1016/j.drugalcdep.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 3.Merikangas KR, Mehta RL, Molnar BE, et al. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict Behav. 1998;23(6):893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- 4.Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: A review of major perspectives and findings. Clin Psychol Rev. 2000;20(2):149–171. doi: 10.1016/s0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- 5.Koob G, Kreek MJ. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am J Psychiatry. 2007;164(8):1149–1159. doi: 10.1176/appi.ajp.2007.05030503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petrakis IL, Poling J, Levinson C, Nich C, Carroll K, Rounsaville B. Naltrexone and disulfiram in patients with alcohol dependence and comorbid psychiatric disorders. Biol Psychiatry. 2005;57(10):1128–1137. doi: 10.1016/j.biopsych.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 7.Wittchen H-U, Zhao S, Kessler RC, Eaton WW. DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(5):355–364. doi: 10.1001/archpsyc.1994.03950050015002. [DOI] [PubMed] [Google Scholar]
- 8.Bolton JM, Sareen J. Lifetime mood, anxiety, and drug use disorders are common in the United States population. Evid Based Ment Health. 2006;9(4):113. doi: 10.1136/ebmh.9.4.113. [DOI] [PubMed] [Google Scholar]
- 9.Sartor CE, Lynskey MT, Heath AC, Jacob T, True W. The role of childhood risk factors in initiation of alcohol use and progression to alcohol dependence. Addiction. 2007;102(2):216–225. doi: 10.1111/j.1360-0443.2006.01661.x. [DOI] [PubMed] [Google Scholar]
- 10.Bruce SE, Yonkers KA, Otto MW, et al. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am J Psychiatry. 2005;162(6):1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKeehan MB, Martin D. Assessment and treatment of anxiety disorders and comorbid alcohol/other drug dependency. Alcoholism Treatment Quarterly. 2002;20(1):45–59. [Google Scholar]
- 12.Posternak MA, Mueller TI. Assessing the risks and benefits of benzodiazepines for anxiety disorders in patients with a history of substance abuse or dependence. Am J Addict. 2001;10(1):48–68. doi: 10.1080/105504901750160484. [DOI] [PubMed] [Google Scholar]
- 13.Kranzler HR, Burleson JA, Del Boca FK, et al. Buspirone treatment of anxious alcoholics. a placebo-controlled trial. Arch Gen Psychiatry. 1994;51(9):720–731. doi: 10.1001/archpsyc.1994.03950090052008. [DOI] [PubMed] [Google Scholar]
- 14.Malec E, Malec T, Gagne MA, Dongier M. Buspirone in the treatment of alcohol dependence: a placebo-controlled trial. Alcohol Clin Exp Res. 1996;20(2):307–312. doi: 10.1111/j.1530-0277.1996.tb01644.x. [DOI] [PubMed] [Google Scholar]
- 15.Malcolm R, Anton RF, Randall CL, Johnston A, Brady K, Thevos A. A placebo-controlled trial of buspirone in anxious inpatient alcoholics. Alcohol Clin Exp Res. 1992;16(6):1007–1013. doi: 10.1111/j.1530-0277.1992.tb00691.x. [DOI] [PubMed] [Google Scholar]
- 16.Tollefson GD, Montague-Clouse J, Tollefson SL. Treatment of comorbid generalized anxiety in a recently detoxified alcoholic population with a selective serotonergic drug (buspirone) J Clin Psychopharmacol. 1992;12(1):19–26. doi: 10.1097/00001573-199202000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Lydiard RB, Roy-Byrne PP, Ballenger JC. Recent advances in the psychopharmacological treatment of anxiety disorders. Hosp Community Psychiatry. 1988;39(11):1157–1165. doi: 10.1176/ps.39.11.1157. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 2005;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 19.Reed PL, Anthony JC, Breslau N. Incidence of drug problems in young adults exposed to trauma and posttraumatic stress disorder: do early life experiences and predispositions matter? Arch Gen Psychiatry. 2007;64(12):1435–1442. doi: 10.1001/archpsyc.64.12.1435. [DOI] [PubMed] [Google Scholar]
- 20.Dansky BS, Brady KT, Roberts JT. Post-traumatic stress disorder and substance abuse: empirical findings and clinical issues. Substance Abuse. 1994;15(4):247–257. [Google Scholar]
- 21.Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. Am J Psychiatry. 2001;158(8):1184–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- 22.Brady KT, Sonne S, Anton RF, Randall CL, Back SE, Simpson K. Sertraline in the treatment of co-occurring alcohol dependence and post-traumatic stress disorder. Alcohol Clin Exp Res. 2005;29(3):395–401. doi: 10.1097/01.alc.0000156129.98265.57. [DOI] [PubMed] [Google Scholar]
- 23.Najavits LM. Seeking Safety: A Treatment Manual for PTSD and Substance Abuse. New York: Guilford Press; 2002. [Google Scholar]
- 24.Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. Am J Psychiatry. 2004;161(8):1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- 25.Triffleman E. Gender differences in a controlled pilot study of psychosocial treatments in substance dependent patients with post-traumatic stress disorder: Design considerations and outcomes. Alcoholism Treatment Quarterly. 2000;18(3):113–126. [Google Scholar]
- 26.Brady KT, Dansky BS, Back SE, Foa EB, Carroll KM. Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: preliminary findings. J Subst Abuse Treat. 2001;21(1):47–54. doi: 10.1016/s0740-5472(01)00182-9. [DOI] [PubMed] [Google Scholar]
- 27.Donovan B, Padin-Rivera E, Kowaliw S. “Transcend”: initial outcomes from a posttraumatic stress disorder/substance abuse treatment program. J Trauma Stress. 2001;14(4):757–772. doi: 10.1023/A:1013094206154. [DOI] [PubMed] [Google Scholar]
- 28.Harris M. Trauma Recovery and Empowerment: A Clinician’s Guide for Working with Women in Groups. New York: Free Press; 1998. [Google Scholar]
- 29.Bolton J, Cox B, Clara I, Sareen J. Use of alcohol and drugs to self-medicate anxiety disorders in a nationally representative sample. J Nerv Ment Dis. 2006;194(11):818–825. doi: 10.1097/01.nmd.0000244481.63148.98. [DOI] [PubMed] [Google Scholar]
- 30.Kushner MG, Sher KJ, Beitman BD. The relation between alcohol problems and the anxiety disorders. Am J Psychiatry. 1990;147(6):685–695. doi: 10.1176/ajp.147.6.685. [DOI] [PubMed] [Google Scholar]
- 31.Sareen J, Chartier M, Kjernisted KD, Stein MB. Comorbidity of phobic disorders with alcoholism in a Canadian community sample. Can J Psychiatry. 2001;46(8):733–740. doi: 10.1177/070674370104600806. [DOI] [PubMed] [Google Scholar]
- 32.Randall CL, Johnson MR, Thevos AK, et al. Paroxetine for social anxiety and alcohol use in dual-diagnosed patients. Depress Anxiety. 2001;14(4):255–262. doi: 10.1002/da.1077. [DOI] [PubMed] [Google Scholar]
- 33.Pande AC, Davidson JR, Jefferson JW, et al. Treatment of social phobia with gabapentin: a placebo-controlled study. J Clin Psychopharmacol. 1999;19(4):341–348. doi: 10.1097/00004714-199908000-00010. [DOI] [PubMed] [Google Scholar]
- 34.Malcolm R, Myrick H, Brady KT, Ballenger JC. Update on anticonvulsants for the treatment of alcohol withdrawal. Am J Addict. 2001;10(Suppl):16–23. doi: 10.1080/10550490150504100. [DOI] [PubMed] [Google Scholar]
- 35.Verduin ML, McKay S, Brady KT. Gabapentin in comorbid anxiety and substance use. Am J Addict. 2007;16(2):142–143. doi: 10.1080/10550490601186238. [DOI] [PubMed] [Google Scholar]
- 36.Randall CL, Thomas S, Thevos AK. Concurrent alcoholism and social anxiety disorder: a first step toward developing effective treatments. Alcohol Clin Exp Res. 2001;25(2):210–220. [PubMed] [Google Scholar]
- 37.Schade A, Marquenie LA, Van Balkom, et al. Alcohol-dependent patients with comorbid phobic disorders: a comparison between comorbid patients, pure alcohol-dependent and pure phobic patients. Alcohol. 2004;39(3):241–246. doi: 10.1093/alcalc/agh039. [DOI] [PubMed] [Google Scholar]
- 38.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sbrana A, Bizzarri JV, Rucci P, et al. The spectrum of substance use in mood and anxiety disorders. Compr Psychiatry. 2005;46(1):6–13. doi: 10.1016/j.comppsych.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 40.Satel SL, McDougle CJ. Obsessions and compulsions associated with cocaine abuse. Am J Psychiatry. 1991;148(7):947. doi: 10.1176/ajp.148.7.947a. [DOI] [PubMed] [Google Scholar]
- 41.Greist J, Chouinard G, DuBoff E, et al. Double-blind parallel comparison of three dosages of sertraline and placebo in outpatients with obsessive-compulsive disorder. Arch Gen Psychiatry. 1995;52(4):289–295. doi: 10.1001/archpsyc.1995.03950160039008. [DOI] [PubMed] [Google Scholar]
- 42.Fals-Stewart W, Schafer J. The treatment of substance abusers diagnosed with obsessive-compulsive disorder: an outcome study. J Subst Abuse Treat. 1992;9(4):365–370. doi: 10.1016/0740-5472(92)90032-j. [DOI] [PubMed] [Google Scholar]


