Abstract
Chemical peeling is a popular, relatively inexpensive, and generally safe method for treatment of some skin disorders and to refresh and rejuvenate skin. This article focuses on chemical peels and their use in routine clinical practice. Chemical peels are classified by the depth of action into superficial, medium, and deep peels. The depth of the peel is correlated with clinical changes, with the greatest change achieved by deep peels. However, the depth is also associated with longer healing times and the potential for complications. A wide variety of peels are available, utilizing various topical agents and concentrations, including a recent salicylic acid derivative, β-lipohydroxy acid, which has properties that may expand the clinical use of peels. Superficial peels, penetrating only the epidermis, can be used to enhance treatment for a variety of conditions, including acne, melasma, dyschromias, photodamage, and actinic keratoses. Medium-depth peels, penetrating to the papillary dermis, may be used for dyschromia, multiple solar keratoses, superficial scars, and pigmentary disorders. Deep peels, affecting reticular dermis, may be used for severe photoaging, deep wrinkles, or scars. Peels can be combined with other in-office facial resurfacing techniques to optimize outcomes and enhance patient satisfaction and allow clinicians to tailor the treatment to individual patient needs. Successful outcomes are based on a careful patient selection as well as appropriate use of specific peeling agents. Used properly, the chemical peel has the potential to fill an important therapeutic need in the dermatologist's and plastic surgeon's armamentarium.
Chemical peels are used to create an injury of a specific skin depth with the goal of stimulating new skin growth and improving surface texture and appearance. The exfoliative effect of chemical peels stimulates new epidermal growth and collagen with more evenly distributed melanin. Chemical peels are classified by the depth of action into superficial, medium, and deep peels.1 Specific peeling agents should be selected based on the disorder to be treated and used with an appropriate peel depth, determined by the histological level or severity of skin pathology to maximize success. However, other considerations, such as skin characteristics, area of skin to be treated, safety issues, healing time, and patient adherence, should also be taken into account for best overall results.
Chemical peels are very common in clinical practice. The American Society of Plastic Surgery reported that more than one million peel procedures were performed by its members in 2008.2 Although peels have recently had an upsurge in research interest,3 they are best performed and/or supervised by dermatologists and plastic surgeons who have far more experience and knowledge with cosmetic procedures than other physicians.3
Using the correct depth chemical peel is a critical component for success. Superficial peels affect the epidermis and dermal-epidermal interface. They are useful in the treatment of mild dyschromias, acne, post-inflammatory pigmentation, and AKs and help in achieving skin radiance and luminosity. Because of their superficial action, superficial peels can be used in nearly all skin types. After a superficial peel, epidermal regeneration can be expected within 3 to 5 days, and desquamation is usually well accepted. Superficial peels exert their actions by decreasing corneocyte adhesion and increasing dermal collagen.1 These peels are a good method for rejuvenating the epidermis and upper dermal layers of skin.
Medium-depth peels may be used in the treatment of dyschromias, such as solar lentigines, multiple keratoses, superficial scars, pigmentary disorders, and textural changes. The healing process is longer, with full epithelialization occurring in about one week. Sun protection after a medium-depth peel is recommended for several weeks. Because of the risk of prolonged hyperpigmentation, medium-depth peels should be conducted with caution in patients with dark skin.
Deep peels may be used for severe photoaging, deep or coarse wrinkles, scars, and sometimes precancerous skin lesions. Usually performed with phenol in combination with croton oil, deep peels cause rapid denaturization of surface keratin and other proteins in the dermis and outer dermis. Penetrating the reticular dermis, the deep peel maximizes the regeneration of new collagen. Epithelialization occurs in 5 to 10 days, but deep peels require significant healing time, usually two months or more, and sun protection must always be used. Phenol is rapidly absorbed into the circulation, potentiating cardiotoxicity in the form of arrhythmias. Therefore, special care, such as cardiopulmonary monitoring and intravenous hydration, must be provided to address this concern.4,5 Other complications include hypopigmentation, hyperpigmentation, scarring, and keloid formation, which may occur primarily with phenol peels (similar to laser resurfacing, the occurrence of these problems is both operator- and technique-dependent).6 Phenol peels are primarily performed in operating room settings and are frequently used as adjuncts to surgical procedures. Due to the increased risk of prolonged or permanent pigmentary changes, deep peels are not recommended for most dark-skinned individuals. Currently, new laser techniques are a popular alternative for major deep skin resurfacing because they avoid the adverse effects of deep chemical peels, even if phenol is used in lower concentrations.
Chemical peels are a mainstay in the cosmetic practitioner's armamentarium because they can be used to treat some skin disorders and can provide an aesthetic benefit. In addition, chemical peels may be readily combined with other resurfacing and rejuvenation procedures, often providing synergistic treatment and more flexibility in tailoring treatments to specific patient needs and conditions. Clinicians can customize regimens to the patient's individual needs using several modalities, such as at-home skin regimens, chemical peels, and lasers or dermabrasion, to provide unheralded flexibility in individualized care.
This brief review covers chemical peels and their role in appropriate indications by combining evidence-based medicine with the clinical experience of the authors. The recent introduction of β-lipohydroxy acid, a salicylic acid derivative with antibacterial, anti-inflammatory, antifungal, and anticomedogenic properties, may provide additional therapeutic benefit, and thus its role is highlighted.
Currently Available Peels
A wide variety of peels are available with different mechanisms of actions, which can be modulated by altering concentrations. Agents for superficial peels today include the alpha hydroxy acids (AHAs), such as glycolic acid (GA), and the beta hydroxy acids (BHAs), including salicylic acid (SA). A derivative of SA, β-lipohydroxy acid (LHA, up to 10%) is widely used in Europe and was recently introduced in the United States. Tretinoin peels are used to treat melasma and postinflammatory hyperpigmentation (PIH).7 Trichloroacetic acid (TCA) can be used for superficial (10–20%) peels and for medium-depth peels (35%). Combination peels, such as Monheit's combination (Jessner's solution with TCA),8 Brody's combination (solid carbon dioxide with TCA),9 Coleman's combination (GA 70% + TCA),10 and Jessner's solution with GA,11 have been used for medium-depth peels where a deeper effect on the skin is required but deep peeling is not an option. Deep peels are typically performed with phenol-based solutions, including Baker-Gordon phenol peel and the more recent Hetter phenol-croton oil peel.12
The recent introduction of LHA is important because it not only provides efficient exfoliation at low concentrations, it possesses antibacterial, anti-inflammatory, antifungal, and anticomedonic properties.13–15 An SA derivative with an additional fatty chain, LHA has increased lipophilicity compared to SA, for a more targeted mechanism of action and greater keratolytic effect.13 LHA has good penetration into the sebaceous follicle and through the epidermis, but it penetrates less deeply into the skin than GA or SA (LaRoche-Posay; data on file; 2008) interacting with the more superficial layers of the stratum corneum, specifically the compactum/disjunctum interface. Thus, its activity focuses on the follicle and epidermis. LHA has a pH similar to normal skin (pH 5.5) and has proven to be quite tolerable. Conveniently, the LHA peel does not require neutralization in contrast to a GA peel.
LHA has an interesting mechanism of action. It targets the corneosome/corneocyte interface to cleanly detach individual corneosomes, which may partially explain skin smoothness after an LHA peel, since it minimizes desquamation of clumps, which leads to roughness.14 These effects are visible to the naked eye.13 Similar to SA, LHA does not affect keratin fibers or the corneocyte membrane.13 AHAs and BHAs do not modify corneocyte keratins. The clean and uniform corneocyte separation achieved with LHA more closely mimics the natural turnover of skin. SA and GA can result in only partial detachment of some cells, which leads to uneven exfoliation of cells in clumps. The differences between LHA, SA, and lactic acid with regard to epidermal effects are summarized in Table 1. The histological section of skin samples treated with LHA also shows targeting of the horny layer by LHA along with good epidermal integrity. Studies have demonstrated that LHA targets corneodesmosome protein structures, particularly corneodesmosine, in the horny layer (LaRoche-Posay; data on file; 2008). While SA has the same target, its activity is less specific and is limited to arbitrary intercellular cleaving of some intercellular junctions. Finally, AHAs have far less affinity for these proteins and the less drastic cleaving of the intercellular bonds of SA leads to less precise desquamation than that observed with LHA.
Table 1.
Action of peeling molecules in the skin
| ULTRASTRUCTURE | LHA | SALICYLIC ACID | LACTIC ACID | |||
|---|---|---|---|---|---|---|
| 1% | 5% | 3% | 15% | 3% | 15% | |
| Dermo epidermal junction—separation | + | +++ | +++ | +++ | 0 | 0 |
| Alive epidermis | ||||||
| Expanded spaces | 0 | 0 | +++ | +++ | 0/+ | 0/+ |
| Vacuoles | 0 | 0 | +++ | +++ | 0 | 0 |
| Perinuclear edema | + | + | +++ | +++ | + | + |
| Spoiled membranes | 0 | 0 | +++ | +++ | 0 | 0 |
| Spoiled desmosomes | 0 | 0 | + | ++ | 0 | 0 |
| Granular junction | 0 | 0 | + | +++ | 0 | ++ |
| Spoiled corneodesmosomes | 0 | 0 | ++ | +++ | 0/+ | + |
| Stratum compactum—basket weave pattern (BWP) | 0 | 0 | +++ | +++ | ++ | +++ |
| Central spoiled corneosomes | 0 | 0 | +++ (D) | +++ (D) | ++ | +++ |
| Peripheral spoiled corneosomes | 0 | 0 | ++ | +++ | 0 | 0 |
| Spoiled proteic cornea envelope | 0 | 0 | + | ++ | 0 | 0 |
| Spoiled lipidic cornea envelope | 0 | 0 | + | ++ | 0 | 0 |
| Stratum junction compactum/stratum disjunctum BWP | 0 | + | Nonidentifiable | |||
| Central spoiled corneosomes—rupture | +++ | +++ | ||||
| Peripheral spoiled corneosomes—rupture | 0 | 0 | ||||
| Spoiled cornea envelope | + | ++ | ||||
| Saw tooth corneocytes | + | ++ | ||||
| Stratum disjunctum BWP | + | +++ | +++ | +++ | +++ | +++ |
| Peripheral spoiled corneosomes—rupture | 0 | +++ | +++ | +++ (D) | ++ | +++ |
| Spoiled proteic cornea envelope | + | ++ | +++ | +++ | +++ | +++ |
| Spoiled lipidic cornea envelope | + | +++ | +++ | +++ | +++ | +++ |
| Saw tooth corneocytes | + | +++ | +++ | +++ | +++ | +++ |
| Keratin content | 0 | 0 | 0 | 0 | 0 | 0 |
Adapted from Berson D, et al. J Drugs Dermatol. 2009;8:803–811
Other properties of LHA include modifying the stratum corneum so that postpeel, it is thinner, flexible, and resistant to wrinkling and cracking.16 In-vivo immunohistological study of LHA peels showed increased epidermal thickness and dendrytic hyperplasia without markers of irritation or inflammation.15 Thus, LHA has similar effects to those of SA on epidermal indices, such as thickness of stratum corneum and germinative compartment and number of nuclei.14,17 Additionally, LHA-treated older skin has been shown to recover some physiological characteristics of younger skin, such as more rapid cell cycling.14 LHA has very few side effects. In clinical studies, LHA peels were well tolerated with some patients experiencing burning and crusting after the initial peel. No cases of PIH or scarring have been reported with LHA.18
Applications of Peels in Clinical Practice
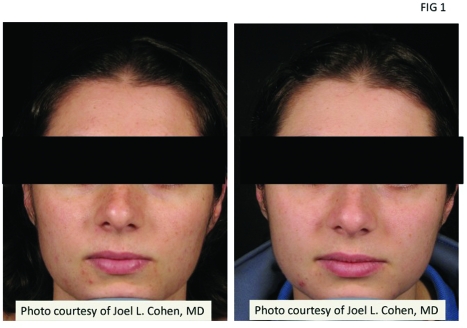
Acne. Clinicians and patients often use chemical peels as an adjunct to medical therapy in acne because they produce complementary rapid therapeutic effects and improvements in skin appearance and textures.19,20 The primary effect may be on comedones with a concomitant reduction in inflammatory lesions (Figures 1–3). Peels may allow topical acne agents to penetrate more efficiently into the skin and may improve PIH.21 With good technique, peels may also be beneficial for dark-skinned patients who have pigmentary changes due to acne.20 While 2009 American Academy of Dermatology guidelines suggest that more evidence is needed to determine best practices,22 clinical experience has shown promising utility. Peels that have been studied for active acne include SA, GA, LHA, and Jessner's solution.
Figure 1.
Patient with mild inflammatory acne before and after LHA peeling shown before (left) and after four sessions at two-week intervals (right). Photo courtesy of Joel L. Cohen, MD.
Figure 3.
Patient with inflammatory acne and postinflamatory hyperpigmentation shown before (left) and after four LHA peeling sessions at two-week intervals (right). Photo courtesy of Marta Rendon, MD.
Figure 2.
Patient with mild inflammatory acne treated with LHA peels shown before (left) and after four sessions at two-week intervals (right). Photo courtesy of Marta Rendon, MD.
SA. SA can be used to treat comedones and inflammatory lesions.21 In the early 1980s, a controlled, double-blind trial (N=49) showed that low concentrations of SA (0.5–3%) helped speed resolution of inflammatory lesions.23 Later, Lee et al18 reported improvement in acne in 35 Korean patients with acne treated with SA 30% peels, and that the reduction in lesion counts increased as the duration of peel continued.18 SA has shown good effects in dark-skinned Asian, African-American, and Hispanic patients with acne.24,25 In addition, this treatment regimen facilitated resolution of PIH as well as a decrease in the overall pigmentation of the face.25
Most recently, Kessler et al26 compared 30% GA versus 30% SA peels in 20 patients with mild-to-moderate acne using a split-face design. Peels were performed every two weeks for a total of six treatments. Both peels improved acne; however, the authors found that the SA peel had better sustained efficacy (number of acne lesions, improvement rating by blinded evaluator) and fewer side effects than GA, presumably due to the increased lipophilicity of SA.26 Overall, the authors of this paper agree with the impression that SA peels are better tolerated than GA peels in acne patients.
LHA. Due to its lipophilicity, LHA targets the sebum-rich pilosebaceous units and has a strong comedolytic effect. Uhoda et al27 studied LHA in acne-prone women and women with comedonal acne (n=28) in a randomized, controlled, clinical trial. As shown with ultraviolet (UV) light video recordings and computerized image analysis, both the number and size of microcomedones were significantly decreased in 10 of 12 LHA-treated patients versus 3 of 10 untreated controls. In addition, image analysis showed a marked reduction in the density of follicular keratotic plugs. As microcomedones resolved, there was also a decrease in follicular bacterial load. There were no reported side effects with LHA use.27
The previously described anticomedogenic properties of LHA include loosening of both intercorneocyte binding and bacterial adhesion inside the follicular openings16 and thinning of the stratum corneum.28 LHA reduced the bacterial population per volume of follicular cast by 21±13 percent following daily treatment with a 2% cream. In addition, bacterial viability was reduced.28,16
GA. GA may be used in acne to normalize keratinization and increase epidermal and dermal hyaluronic acid and collagen gene expression.29 It has been studied in concentrations ranging from 35 to 70%.19,30.31 GA 70% has been shown to reduce comedones in Asian patients.19Lower concentrations (35% or 50%) also achieved significant resolution of both inflammatory and non-inflammatory acne lesions.30 Another study also conducted on Asian patients showed improvement in pigmentation problems and reported that acne flares after the first treatment diminished with subsequent treatments.30 A case series suggested that comedones may improve more readily than inflammatory lesions,31 but this remains to be validated.
Jessner's solution. Superficial Jessner's solution peels have been used to manage acne. Medium-depth peels involving Jessner's solution plus TCA have also been used to treat mild acne scarring. Kim et al19 compared Jessner's solution versus GA 70% in patients with facial acne in a split-face study (n=26). Efficacy was similar between the two types of peels, but Jessner's solution was associated with a significantly greater degree of exfoliation compared with GA (P<0.01).19 Lee et al32 studied the effect of GA and Jessner's solution on facial sebum secretion in patients with acne.32 GA 30% or Jessner's solution peels were performed twice at an interval of two weeks in 38 patients (27% GA, 11% Jessner's solution), and sebum levels were measured. In this study, neither type of peel changed sebum secretion after two peels.32 However, Jessner's solution may be an option for superficial peeling as an adjunctive treatment in patients with acne.
Acne scarring. Acne scars are polymorphic; therefore, it is important to assess and design treatment according to the types of scars, while also keeping in mind patient expectations. Chemical peels, laser resurfacing, dermabrasion, and fractionated laser technology as well as fillers and subcision are commonly used modalities for acne scar therapy. From a peel standpoint, patients with mild-to-moderate acne scarring may be treated. Peels that have been used include SA, GA, TCA, LHA, and Jessner's solution. Peels are used as an adjunct to medical therapy including a retinoid or AHAs.33 Studies of Jessner's solution in combination with TCA in medium-depth peels have also shown benefit in acne scarring.34,35 Medium-depth and deep-depth phenol peels, while useful for treatment of acne scarring, are not recommended for dark skin types IV to VI due to a high risk of permanent pigmentary changes.36 Regional dermabrasion is an effective adjunct to chemical peel for medium-depth scars.37
Phenol solutions. Deep chemical peels may be used to treat acne scarring. The most common solutions are combinations of phenol and croton oil.12, 38–40 These solutions penetrate to the midreticular region and maximize the production of collagen.41 Park et al42 used a modified phenol peel, which was applied to 46 patients of Asian descent, 11 of whom were treated for acne scarring and 28 for wrinkles. Seven of 11 patients (64%) with acne scars improved 51 percent or more based on physician and patient assessment. The most frequent side effect was PIH (74%).42
Photodamage. Photodamaged skin is associated with chronic UV light exposure. Photoaging changes include a thicker dermis due to breakdown of the elastic fiber network and a thinner epidermis having cellular atypia. Often, the result can be irregular pigmentation, wrinkling, loss of elasticity, development of solar lentigines and actinic keratoses, and coarseness. Histologically, peels alter the epidermis creating a more normal pattern with columnar cells showing return of polarity, more regular distribution of melanocytes, and melanin granules. A wide range of chemical peels including AHA, SA, TCA, and phenol are used to treat photodamage; selection is based on patient presentation and severity of photodamage. The efficacy of treating photoaging with tretinoin is well established.16 Efficacy of peels to treat photodamage has also been repeatedly reported. In photodamaged skin, peels cause skin exfoliation and rejuvenation,43 and repeated superficial peels may be used.44 With advanced photoaging changes, a peel may be combined with laser resurfacing or other procedures.
AKs are precancerous lesions that are also a result of chronic UV exposure. Peels have been used to treat AKs and are appropriate treatment for most regions of the body. Chemical peels can eliminate AKs and may be able to provide prophylaxis for a prolonged time period.45 They have also recently shown clinical benefit when AKs were observed in combination with Bowen's Disease.46
SA. Kligman et al47 studied SA 30% in regimens of single and multiple peels at four-week intervals and reported improvement of pigmentation, skin texture, and reduction of fine lines in patients with moderately photodamaged skin. Humphreys et al48 reported that 40% TCA (a borderline medium-depth peel) plus topical retinoid treatment improved solar lentigines, AKs, and skin texture, but had minimal effect on wrinkles.
GA. Rendon et al49 described the use of superficial GA peels in combination with dermal fillers and botulinum toxin, successfully addressing wrinkles, uneven skin tone, skin laxity, and skin clarity. They used a schedule that separates fillers and peels by approximately one week; with botulinum toxin, the peel was administered after the toxin in the same visit or the procedures were separated by one or more days to minimize the potential for side effects.49 Briden et al50 reported good patient satisfaction when using superficial GA peels with microdermabrasion in photoaging.
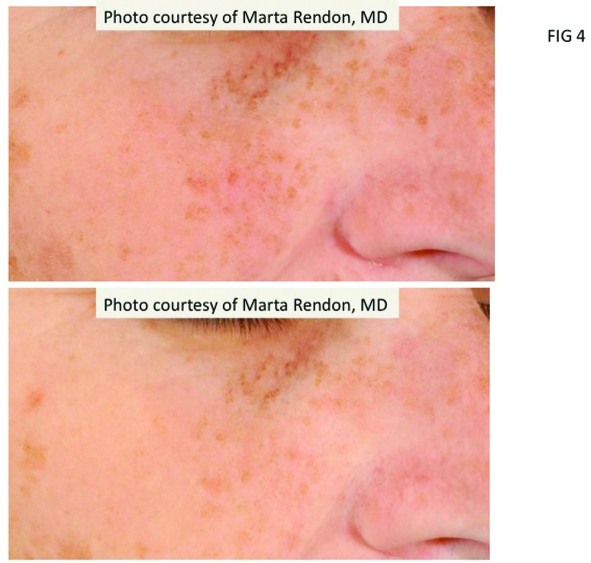
LHA. Efficacy of LHA peeling in photodamage was shown in a randomized, intraindividual-controlled, split-face trial evaluating LHA (5–10%) versus GA peel (20–50%) (LaRoche-Posay; data on file; 2008). A total of 43 women with fine lines, wrinkles, and hyperpigmentation were treated with six applications with both acids over nine weeks. Both treatments showed a significant effect in reducing fine lines, wrinkles, and hyperpigmentation (Figure 4). However, the efficacy of four LHA sessions was equivalent to six sessions of GA. The LHA peel was well tolerated. No patient withdrew from the study, and the most common side effect was transient erythema that persisted for less than two hours (LaRoche-Posay; data on file; 2008).
Figure 4.
Patient with photoaging-related pigmentary changes shown before (top) and after four LHS peel sessions at two-week intervals (bottom). Photo courtesy of Marta Rendon, MD.
Leveque et al14 assessed skin improvement in 80 women who were treated with an excipient containing LHA 1% daily for six months, finding a progressive improvement in complexion, with an onset of action occurring within one month. In a randomized, controlled trial comparing GA 10% versus LHA 2% versus retinoic acid 0.05% on the forearm, LHA and retinoic acid improved surface texture similarly while GA had a very minimal effect.51
AHA increases UV sensitivity,52,53 while LHA increases the skin's resistance to UV-induced damage. Saint-Leger16 reported that the minimal erythema dose was 210mJ/cm2 versus 140mJ/cm2 for untreated and placebo-treated controls (LaRoche-Posay; data on file; 2008).16 This protective effect may be due to the antioxidant properties of LHA, which can inactivate the oxygen singlet (1O2) without reacting with it and thus quench the superoxide anion. It also reacts avidly with hydroxyl radicals to produce 2,5-dihydrobenzoic acid, an excellent scavenger of the superoxide anion (L'Oreal; data on file; 2008).16
Combination solutions. Lawrence et al54 conducted a 15-patient, split face study comparing a medium-depth chemical peel consisting of Jessner's solution and 35% TCA with topical fluorouracil in the treatment of widespread facial AKs. Both treatments reduced the number of visible AKs by 75 percent and produced equivalent reductions in keratinocyte atypia, hyperkeratosis, parakeratosis, and inflammation, with no significant alteration of preexisting solar elastosis and telangiectasia.54 Also, a 70% glycolic peel and a 5% 5-fluorouracil solution (Drogaderma, Sao Paulo, Brazil) was used in actinic porokeratosis every two weeks for four months with benefit, but the results remain to be validated.55
Phenol solutions. A study by Chew et al56 suggested that that there was a greater improvement in upper-lip wrinkles with Baker's phenol chemical peel than with CO2 laser treatment (p<0.03), although the change from baseline was statistically significant for both chemical peel and CO2 laser. In basal cell carcinoma, Kaminaka et al57 demonstrated that nevoid basal cell carcinoma could successfully be treated with phenol and TCA peeling.57 A more recent study by Kaminaka et al46 not only demonstrated a significant benefit of the phenol-base peel in patients with AKs and Bowen's Disease, but also identified biomarkers that assisted in predicting clinical success from failure. They studied 46 patients treated with phenol peels and followed up for one or more years. Biopsy specimens were taken before and after treatment. In this small but important study, 39 patients (84.8%) had a complete response after 1 to 8 treatment sessions. Statistical differences also correlated the number of treatment sessions with histology, personal history of skin cancer, tumor thickness, and cyclin A expression. The authors concluded that tumor thickness and cyclin A could be specific and useful biomarkers as an accurate therapeutic diagnosis tool, thus providing a more useful way to measure potential therapeutic benefit.46
Melasma. Patients with melasma usually present with irregular patches of darkened skin on the cheeks, forehead, upper lip, nose, and chin.58 Melasma has always been very challenging to treat for multiple reasons including the presence of melanin at varying depths in the epidermis and dermis. Because chemical peels remove melanin and improve skin tone and texture, they are commonly used in treating this condition. More superficial and more limited involvement melasma is often more responsive to treatment. Data from small studies suggest that melasma improvement occurs more rapidly when peels are combined with medical therapy. Several peels have been studied (SA, LHA, GA, TCA, tretinoin and resorcinol, retinoic acid and Jessner's), although GA is currently most popular.
SA. Grimes25 reported that a series of five SA peels at concentrations of 20 to 30% plus hydroquinone at two-week intervals resulted in moderate-to-significant improvement in 66 percent of six darker skinned (V–VI) patients. The treatment was well tolerated, and there was no residual hypo- or hyperpigmentation.25 In unpublished data, Grimes noted that SA peels without hydroquinone preparation were associated with hyperpigmentation. Because of the known propensity of darker skin to develop dyschromias, Grimes recommended that even superficial peels be used with care and caution.
GA. In a study of GA 30 to 40% peels plus a modified Kligman's formula (retinoid, corticosteroid, and hydroquinone) versus Kligman's formula alone (n=40), Sarkar58 found a significant decrease in Melasma Area and Severity Index (MASI) score from baseline to 21 weeks in both groups. Figure 5 shows an 80-percent change in score at Week 21 in the peel group and a 63-percent change in the control group (P<.001).58 However, the addition of a peel achieved a significantly greater effect versus the control group of Kligman's formula alone (more rapid and greater improvement, P<.001).58 Erbil et al61 studied serial GA peels (from 35–50% and 70% every second peel) plus combination topical therapy (azelaic acid and adapalene) in 28 women with melasma59 and found better results in the group receiving chemical peels plus topical therapy (P=0.048), but only when the GA concentration was 50% or higher.59 GA peels in concentrations of 20 to 70% administered every three weeks were studied alone or in combination with a topical regimen of hydroquinone plus 10% GA in 10 Asian women60 in which the combination trended toward significance (P>0.059).
In another study, a triple combination cream consisting of fluocinolone acetonide 0.01%, hydroquinone 4%, and tretinoin 0.05% was used in an alternating sequential treatment pattern, cycling with a series of GA peels, for the treatment of moderate-to-severe melasma.61 Spectrometry measurements of the difference in melanin for involved versus uninvolved skin confirmed that hyperpigmentation was significantly reduced at Weeks 6 and 12 compared with baseline (P<0.001 for both), with evaluations showing 90-percent improvement or more by Week 12 with the treatment approach.61
TCA. Kalla et al62 compared 55 to 75% GA versus 10 to 15% TCA peels in 100 patients with recalcitrant melasma. They reported that both the time to response and degree of response were more favorable with TCA compared with GA; however, relapse was more common in the TCA group (25 vs. 5.9% in the GA group).62 Soliman et al63 reported that 20% TCA peels plus topical 5% ascorbic acid was superior to TCA peeling alone in 30 women with epidermal melasma.
Other peels. An early report by Karam64 used a 50% solution of resorcinol in patients with melasma and skin types I to IV.64 A more recent study of 30 patients with mostly Fitzpatrick type IV skin type were treated successfully with lactic acid in a split-face comparison with Jessner's solution (N=30). All patients showed significant improvement as calculated by MASI score before and after treatment.65 Khungar et al described a pilot study in which serial 1% tretinoin peels were as effective a therapy for melasma in dark-skinned individuals as 70% GA.7
Potential side effects of peels. Superficial peels are safe and tolerated with mild discomfort, such as transient burning, irritation, and erythema.66 Scarring is rare in superficial peels, as are PIH and infection. In medium and deep peels, lines of demarcation that are technique related can occur. Care should be taken to feather peel solution at junctions with nonpeeled skin to avoid this effect. Side effects of deeper peels can also include pigmentary changes (e.g., PIH for dark-skinned individuals), infections, allergic reactions, improper healing, hypersensivity, disease exacerbation, and those due to improper application.67,68
Care must also be taken to prophylactically treat patients with a history of herpes simplex infections. Herpetic episodes, usually on the lip or above the vermilion border, may be prevented with prophylactic oral acyclovir, valacyclovir hydrochloride, or famciclovir.69,70 Antiviral agents are especially useful in patients who indicate a strong history of multiple herpetic lesions each year.
The best way to prevent complications is to identify patients at risk and maintain an appropriate peel depth that balances efficacy with known adverse events. Patients at risk include those with PIH, keloid formation, heavy occupational sun exposure, a history of intolerability to sunscreens, and uncooperative patients.
Tolerability of peels may be influenced by many factors, such as peel agents, concentration, depth, skin type, and concomitant use of skin care products. PIH can be exacerbated by sun exposure, so it is important to educate patients and closely monitor their recovery phase. Sunscreens should be used continuously to limit PIH development. Epidermal PIH responds well to various treatments, while dermal PIH remains problematic. Pretreatment with bleaching agents before beginning therapy with peels decreases the appearance of PIH. Treatment options include hydroquinone or kojic acid or other tyrosinase inhibitors.
In medium and deep peels, a common location of scarring is on the lower part of the face,71 due perhaps to greater tissue movement or more aggressive treatment. Other rare causes of scarring include infections and premature peeling, making post-peel monitoring an essential component of management. Delayed healing and persistent redness are early warning signs, and treatment with topical antibiotics and potent topical corticosteroids should be initiated as soon as possible to minimize scarring. Resistant scars may be treated with dermabrasion or pulsed dye laser followed by silicone sheeting therapy.
Acneiform eruptions may occur during or after peeling, presenting as erythematous follicular papules. These eruptions respond to oral antibiotics used in acne treatment. Discontinuation of oily skin preparations is also recommended.
Milia usually appear 2 to 4 months after peels in up to 20 percent of patients undergoing medium and deep peels and may be treated with extraction or electrosurgery.
Medium-depth peels are associated with most of the complications described above, though most can be managed successfully. Medium- and deep-depth peels should be used with great caution on skin types IV to VI. Toxicity, although rare, has been reported with resorcinol, SA, and phenol deep peels.72
Considerations with Ethnic Skin
Indications for peeling in dark-skinned patients include treatment of dyschromia, PIH, acne, melasma, scarring, and pseudofolliculitis barbae. Clinicians should evaluate the Fitzpatrick skin type and ethnic background as part of the process of selecting whether a peel is an appropriate therapy and which peel is best suited for the individual patient.73 Different ethnicities may respond unpredictably to chemical peeling regardless of skin phenotype. An individual patient history of PIH is very important to take into account. Hexsel et al74 point out that Latin-Americans and Hispanics have a diverse range of skin phototypes and pigmentation and are prone to an increased incidence of melasma and PIH. In this subpopulation, they recommend peels as second-line therapy after topical therapies fail.74
Superficial peels may be safely used in patients with dark skin, including LHA 5 to 10%, TCA 10 to 20%, GA 20 to 70%, SA 20 to 30%, lactic acid, and Jessner's solution. In addition, variations of peel technique may be used, including spot treatment of PIH. This may be performed with TCA 25%, Jessner's solution, SA, and LHA. Table 2 provides recommended agents for peeling in dark-skinned individuals by specific indication. Deep phenol peels are not recommended for dark skin types IV to VI due to the high risk of prolonged or permanent pigmentary changes.75 However, Fintsi et al76 described safe use of phenol-based peels in patients with olive and dark skin and dark eyes and hair.76
Table 2.
Overview of chemical peels in dermatological conditions
| ACNE |
|---|
| • Chemical peels can be a useful adjunct to medical therapy for acne—may speed resolution, enhance penetration of topical drugs, and improve associated postinflammatory pigmentary problems |
| • Peels that have been studied for active acne include SA, LHA, GA 30–70%, and TCA 7–25% |
| • Need maintenance regimen—for patients who respond to peels, schedule every 3 months |
| • Primary effect may be on comedones, although reduction in inflammatory lesions may also occur (esp. SA, LHA) |
| • Peels also provide benefit in superficial acne scarring |
| • SA and its derivative LHA may often be the preferred peels for acne due to their action on both inflammatory and noninflammatory lesions |
| PHOTODAMAGE |
|---|
| • At least fair scientific evidence shows that the clinical benefits of chemical peels in photoaging outweigh the potential risks |
| • A range of chemical peels including AHAs, SA, LHA, TCA, and phenol are used to treat photodamage; selection is based on patient presentation (Glaugau, Fitzpatrick, PIH) and severity of photodamage |
| • SA, GA, TCA, phenol are all appropriate |
| MELASMA |
|---|
| • Peels are popular and widely used for melasma |
| • Peels may be most effective when used in combination with medical therapy or other procedures, possibly because peels remove melanin and other treatments inhibit melanocytes or melanogenesis |
| • Few formal studies are currently available; most existing studies have small patient populations |
| • Several peels have been studied in melasma (e.g., SA, LHA, GA, and TCA) |
| • Maintenance therapy is needed when peeling is used for melasma |
General Approach to Skin Care Before and After Peeling
Medical history. Taking a complete history prior to peeling is critical. It can enhance aesthetic results by identifying any factors that may contribute to problems and provides an opportunity to discuss adherence issues necessary for successful management.67,77 It is important to gain insight into patients' perceptions of wound healing and scar formation, as well as prior experience with resurfacing procedures or facelift surgery.67 Current literature recommends waiting at least six months after discontinuing oral isotretinoin therapy before performing resurfacing procedures.67
A current medication list should be obtained, and photosensitizing agents should be discontinued. Some dermatological conditions, including rosacea, seborrheic or atopic dermatitis, and psoriasis, may increase the risk for postoperative problems, such as disease exacerbation, excessive and/or prolonged erythema, hypersensitivity, or delayed healing.67 Prophylactic antiviral agents should be prescribed as required.67 Since sun protection after peeling is essential, discussion in relation to the patient's past habits and experience is important.
Pretreatment. Pretreatment can help to enhance outcomes and is often started 2 to 4 weeks prior to the peel and discontinued 3 to 5 days before the procedure.21 Topical retinoids or a prepeel solution can help to create a smooth stratum corneum to achieve a more even penetration of the peel. Topical retinoids may also speed healing.1 Humphreys et al48 reported that pretreatment with a topical retinoid resulted in more rapid and even frosting as well as a decrease in telangiectasias, which the authors postulated as being due to deeper penetration of TCA with retinoid pretreatment.48
Before a chemical peel, hydroquinone may be used to reduce the likelihood of PIH in dark-skinned individuals.1 Discussing peel after-effects with patients before the peel is also important to aid comprehension of the peeling process.
Postpeel, patients should use a broad-spectrum sunscreen on a daily basis and implement a gentle cleansing regimen with toner and peel serum as prescribed. Moisturizers may also be recommended.
Maintenance. After a chemical peel, edema, erythema, and desquamation may occur for 1 to 3 days for superficial peels and 5 to 10 days for medium to deep peels. A cleansing agent may be used and antibacterial ointment applied especially for deep peels. Patients should be instructed to avoid peeling or scratching the affected skin and to use only simple moisturizers.
A long-term maintenance program will preserve the results of chemical peels in most patients. Patient participation and education is required, emphasizing the importance of sun protection and the use of appropriate skin care regimens that include cleansing, toning, exfoliation, and moisturizers. Patients need to have realistic expectations and understand that achieving benefits from peels requires repeated procedures. If the peel regimen works well for the patient, clinicians should consider a maintenance protocol, which may be one peel per month for six months, then every three months thereafter depending on the need and the season. Topical retinoid maintenance therapy can also help maintain the skin rejuvenation results achieved with a chemical peel. It may be used alone on a daily or intermittent basis or in addition to 2 to 3 weekly light peels periodically. Maintenance regimens may also include products with combinations of kojic acid, hydroquinone, LHA, SA, GA, or ascorbic acid.
Importance of tailoring therapy. It is important to develop a peel program that is tailored to the individual needs of the patient. For example, a patient with visible photodamage who can tolerate social and work downtime may be treated with a 35% TCA peel while another patient may be better treated with a series of lighter peels to minimize downtime. In addition, patients who are treated with peels may also be interested in a variety of other treatments, such as botulinum toxin or fillers, to improve the signs of aging.
Conclusion
Chemical peels remain popular for the treatment of some skin disorders and for aesthetic improvement. Peels have been studied and shown to be effective as treatment for a myriad of conditions including acne, superficial scarring, photodamage, and melasma. Patients who are willing to undergo continued treatment are likely to be the best candidates. Newer molecules such as the LHA superficial peel provide unique characteristics including targeted action and should be studied further. Clinicians should remember that there can be excellent synergy between peels and other procedures. Chemical peels are most effectively used in combination with a topical, at-home regimen, which, depending on the condition, may include exfoliating or moisturizing products, bleaching agents, or retinoids. Using peels less frequently but on a continuing basis is beneficial to help keep improvement ongoing, especially for superficial peels. Medium peels and deep peels are used more judiciously over time, but can address particularly difficult conditions effectively over the course of several treatments. Finally, it is important for patients to maintain a good sun protection regimen to optimize the clinical results achieved with chemical peels.
References
- 1.Coleman WP, 3rd, Brody HJ. Advances in chemical peeling. Dermatol Clin. 1997;15:19–26. doi: 10.1016/s0733-8635(05)70411-3. [DOI] [PubMed] [Google Scholar]
- 2.Surgery ASoP. [February 2, 2009]. http://wwwplasticsurgeryorg/Media/stats /2008-cosmetic-reconstructive-plastic-surgery-minimally-invasive-statisticspdf.
- 3.Housman TS, Hancox JG, Mir MR, et al. What specialties perform the most common outpatient cosmetic procedures in the United States? Dermatol Surg. 2008;34:1–7. doi: 10.1111/j.1524-4725.2007.34000.x. discussion 8. [DOI] [PubMed] [Google Scholar]
- 4.Landau M. Cardiac complications in deep chemical peels. Dermatol Surg. 2007;33:190–193. doi: 10.1111/j.1524-4725.2006.33037.x. [DOI] [PubMed] [Google Scholar]
- 5.Landau M. Chemical peels. Clin Dermatol. 2008;26:200–208. doi: 10.1016/j.clindermatol.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 6.Pandya AG, Guevara IL. Disorders of hyperpigmentation. Dermatol Clin. 2000;18:91–98. doi: 10.1016/s0733-8635(05)70150-9. ix. [DOI] [PubMed] [Google Scholar]
- 7.Khunger N, Sarkar R, Jain RK. Tretinoin peels versus glycolic acid peels in the treatment of melasma in dark-skinned patients. Dermatol Surg. 2004;30:756–760. doi: 10.1111/j.1524-4725.2004.30212.x. discussion 60. [DOI] [PubMed] [Google Scholar]
- 8.Monheit GD. The Jessner's-trichloroacetic acid peel. An enhanced medium-depth chemical peel. Dermatol Clin. 1995;13:277–283. [PubMed] [Google Scholar]
- 9.Brody HJ, Hailey CW. Medium-depth chemical peeling of the skin: a variation of superficial chemosurgery. J Dermatol Surg Oncol. 1986;12:1268–1275. doi: 10.1111/j.1524-4725.1986.tb01066.x. [DOI] [PubMed] [Google Scholar]
- 10.Coleman WP, 3rd, Futrell JM. The glycolic acid trichloroacetic acid peel. J Dermatol Surg Oncol. 1994;20:76–80. doi: 10.1111/j.1524-4725.1994.tb03753.x. [DOI] [PubMed] [Google Scholar]
- 11.Moy LS, Murad H, Moy RL. Glycolic acid peels for the treatment of wrinkles and photoaging. J Dermatol Surg Oncol. 1993;19:243–246. doi: 10.1111/j.1524-4725.1993.tb00343.x. [DOI] [PubMed] [Google Scholar]
- 12.Hetter GP. An examination of the phenol-croton oil peel: part IV. Face peel results with different concentrations of phenol and croton oil. Plast Reconstr Surg. 2000;105:1061–1083. doi: 10.1097/00006534-200003000-00035. [DOI] [PubMed] [Google Scholar]
- 13.Corcuff P, Fiat F, Minondo AM, Leveque JL, Rougier A. A comparative ultrastructural study of hydroxyacids induced desquamation. Eur J Dermatol. 2002;12:XXXIX–XLIII. [PubMed] [Google Scholar]
- 14.Leveque JL, Corcuff P, Rougier A, Pierard GE. Mechanism of action of a lipophilic salicylic acid derivative on normal skin. Eur J Dermatol. 2002;12:XXXV–XXXVIII. [PubMed] [Google Scholar]
- 15.Avila-Camacho M, Montastier C, Pierard GE. Histometric assessment of the age-related skin response to 2-hydroxy-5-octanoyl benzoic acid. Skin Pharmacol Appl Skin Physiol. 1998;11:52–56. doi: 10.1159/000029808. [DOI] [PubMed] [Google Scholar]
- 16.Saint-Leger D, Leveque JL, Verschoore M. The use of hydroxy acids on the skin: characteristics of C8-lipohydroxy acid. J Cosmet Dermatol. 2007;6:59–65. doi: 10.1111/j.1473-2165.2007.00296.x. [DOI] [PubMed] [Google Scholar]
- 17.Pierard G, Leveque JL, Rougier A, Kligman AM. Dermo-epidermal stimulation elicited by a salicylic acid derivative: a comparison with salicylic acid and all trans-retinoic acid. Eur J Dermatol. 2002;12:XLIV–XLVI. [PubMed] [Google Scholar]
- 18.Lee HS, Kim IH. Salicylic acid peels for the treatment of acne vulgaris in Asian patients. Dermatol Surg. 2003;29:1196–1199. doi: 10.1111/j.1524-4725.2003.29384.x. discussion 9. [DOI] [PubMed] [Google Scholar]
- 19.Kim SW, Moon SE, Kim JA, Eun HC. Glycolic acid versus Jessner's solution: which is better for facial acne patients? A randomized prospective clinical trial of split-face model therapy. Dermatol Surg. 1999;25:270–273. doi: 10.1046/j.1524-4725.1999.08251.x. [DOI] [PubMed] [Google Scholar]
- 20.Taub AF. Procedural treatments for acne vulgaris. Dermatol Surg. 2007;33:1005–1026. doi: 10.1111/j.1524-4725.2007.33215.x. [DOI] [PubMed] [Google Scholar]
- 21.Briden ME. Alpha-hydroxy acid chemical peeling agents: case studies and rationale for safe and effective use. Cutis. 2004;73:18–24. [PubMed] [Google Scholar]
- 22.Strauss JS, Krowchuk DP, Leyden JJ, et al. Guidelines of care for acne vulgaris management. J Am Acad Dermatol. 2007;56:651–663. doi: 10.1016/j.jaad.2006.08.048. [DOI] [PubMed] [Google Scholar]
- 23.Shalita AR. Treatment of mild and moderate acne vulgaris with salicylic acid in an alcohol-detergent vehicle. Cutis. 1981;28:556–558. 61. [PubMed] [Google Scholar]
- 24.Ahn HH, Kim IH. Whitening effect of salicylic acid peels in Asian patients. Dermatol Surg. 2006;32:372–375. doi: 10.1111/j.1524-4725.2006.32075.x. discussion 5. [DOI] [PubMed] [Google Scholar]
- 25.Grimes PE. The safety and efficacy of salicylic acid chemical peels in darker racial-ethnic groups. Dermatol Surg. 1999;25:18–22. doi: 10.1046/j.1524-4725.1999.08145.x. [DOI] [PubMed] [Google Scholar]
- 26.Kessler E, Flanagan K, Chia C, Rogers C, Glaser DA. Comparison of alpha- and beta-hydroxy acid chemical peels in the treatment of mild to moderately severe facial acne vulgaris. Dermatol Surg. 2008;34:45–50. doi: 10.1111/j.1524-4725.2007.34007.x. discussion 1. [DOI] [PubMed] [Google Scholar]
- 27.Uhoda E, Pierard-Franchimont C, Pierard GE. Comedolysis by a lipohydroxyacid formulation in acne-prone subjects. Eur J Dermatol. 2003;13:65–68. [PubMed] [Google Scholar]
- 28.Pierard GE, Rougier A. Nudging acne by topical beta-lipohydroxy acid (LHA), a new comedolytic agent. Eur J Dermatol. 2002;12:XLVII–XLVIII. doi: 10.1016/j.jaad.2003.10.079. [DOI] [PubMed] [Google Scholar]
- 29.Bernstein EF, Lee J, Brown DB, Yu R, Van Scott E. Glycolic acid treatment increases type I collagen mRNA and hyaluronic acid content of human skin. Dermatol Surg. 2001;27:429–433. doi: 10.1046/j.1524-4725.2001.00234.x. [DOI] [PubMed] [Google Scholar]
- 30.Wang CM, Huang CL, Hu CT, Chan HL. The effect of glycolic acid on the treatment of acne in Asian skin. Dermatol Surg. 1997;23:23–29. doi: 10.1111/j.1524-4725.1997.tb00003.x. [DOI] [PubMed] [Google Scholar]
- 31.Atzori L, Brundu MA, Orru A, Biggio P. Glycolic acid peeling in the treatment of acne. J Eur Acad Dermatol Venereol. 1999;12:119–122. [PubMed] [Google Scholar]
- 32.Lee SH, Huh CH, Park KC, Youn SW. Effects of repetitive superficial chemical peels on facial sebum secretion in acne patients. J Eur Acad Dermatol Venereol. 2006;20:964–968. doi: 10.1111/j.1468-3083.2006.01695.x. [DOI] [PubMed] [Google Scholar]
- 33.Monheit GD, Chastain MA. Chemical peels. Facial Plast Surg Clin North Am. 2001;9:239–255, viii. [PubMed] [Google Scholar]
- 34.Al-Waiz MM, Al-Sharqi AI. Medium-depth chemical peels in the treatment of acne scars in dark-skinned individuals. Dermatol Surg. 2002;28:383–387. doi: 10.1046/j.1524-4725.2002.01081.x. [DOI] [PubMed] [Google Scholar]
- 35.Monheit GD. Medium-depth chemical peels. Dermatol Clin. 2001;19:413–425, vii. doi: 10.1016/s0733-8635(05)70282-5. [DOI] [PubMed] [Google Scholar]
- 36.Khunger N. Standard guidelines of care for acne surgery. Indian J Dermatol Venereol Leprol. 2008;74(Suppl):S28–S36. [PubMed] [Google Scholar]
- 37.Branham GH, Thomas JR. Rejuvenation of the skin surface: chemical peel and dermabrasion. Facial Plast Surg. 1996;12:125–133. doi: 10.1055/s-0028-1082404. [DOI] [PubMed] [Google Scholar]
- 38.Baker TJ. The ablation of rhytides by chemical means. A preliminary report. J Fla Med Assoc. 1961;48:451–454. [PubMed] [Google Scholar]
- 39.Baker TJ. Chemical face peeling and rhytidectomy. A combined approach for facial rejuvenation. The ablation of rhitides by chemical means. A preliminary report. Plast Reconstr Surg Transplant Bull. 1962;29:199–207. doi: 10.1097/00006534-196202000-00007. [DOI] [PubMed] [Google Scholar]
- 40.Stone PA, Lefer LG. Modified phenol chemical face peels: recognizing the role of application technique. Facial Plast Surg Clin North Am. 2001;9:351–376. [PubMed] [Google Scholar]
- 41.Butler PE, Gonzalez S, Randolph MA, et al. Quantitative and qualitative effects of chemical peeling on photoaged skin: an experimental study. Plast Reconstr Surg. 2001;107:222–228. doi: 10.1097/00006534-200101000-00036. [DOI] [PubMed] [Google Scholar]
- 42.Park JH, Choi YD, Kim SW, Kim YC, Park SW. Effectiveness of modified phenol peel (Exoderm) on facial wrinkles, acne scars and other skin problems of Asian patients. J Dermatol. 2007;34:17–24. doi: 10.1111/j.1346-8138.2007.00210.x. [DOI] [PubMed] [Google Scholar]
- 43.Stagnone JJ. Superficial peeling. J Dermatol Surg Oncol. 1989;15:924–930. doi: 10.1111/j.1524-4725.1989.tb03179.x. [DOI] [PubMed] [Google Scholar]
- 44.Matarasso SL, Salman SM, Glogau RG, Rogers GS. The role of chemical peeling in the treatment of photodamaged skin. J Dermatol Surg Oncol. 1990;16:945–954. doi: 10.1111/j.1524-4725.1990.tb01559.x. [DOI] [PubMed] [Google Scholar]
- 45.Kligman AM, Baker TJ, Gordon HL. Long-term histologic follow-up of phenol face peels. Plast Reconstr Surg. 1985;75:652–659. doi: 10.1097/00006534-198505000-00006. [DOI] [PubMed] [Google Scholar]
- 46.Kaminaka C, Yamamoto Y, Yonei N, et al. Phenol peels as a novel therapeutic approach for actinic keratosis and Bowen disease: prospective pilot trial with assessment of clinical, histologic, and immunohistochemical correlations. J Am Acad Dermatol. 2009;60:615–625. doi: 10.1016/j.jaad.2008.11.907. [DOI] [PubMed] [Google Scholar]
- 47.Kligman D, Kligman AM. Salicylic acid peels for the treatment of photoaging. Dermatol Surg. 1998;24:325–328. doi: 10.1111/j.1524-4725.1998.tb04162.x. [DOI] [PubMed] [Google Scholar]
- 48.Humphreys TR, Werth V, Dzubow L, Kligman A. Treatment of photodamaged skin with trichloroacetic acid and topical tretinoin. J Am Acad Dermatol. 1996;34:638–644. doi: 10.1016/s0190-9622(96)80065-x. [DOI] [PubMed] [Google Scholar]
- 49.Rendon MI, Effron C, Edison BL. The use of fillers and botulinum toxin type A in combination with superficial glycolic acid (alpha-hydroxy acid) peels: optimizing injection therapy with the skin-smoothing properties of peels. Cutis. 2007;79:9–12. [PubMed] [Google Scholar]
- 50.Briden E, Jacobsen E, Johnson C. Combining superficial glycolic acid (alpha-hydroxy acid) peels with microdermabrasion to maximize treatment results and patient satisfaction. Cutis. 2007;79:13–16. [PubMed] [Google Scholar]
- 51.Pierard GE, Kligman AM, Stoudemayer T, Leveque JL. Comparative effects of retinoic acid, glycolic acid and a lipophilic derivative of salicylic acid on photodamaged epidermis. Dermatology. 1999;199:50–53. doi: 10.1159/000018178. [DOI] [PubMed] [Google Scholar]
- 52.Administration USFaD. 2002. Guidance for Industry: Labeling for Topically Applied Cosmetic Products Containing α-Hydroxy Acids as Ingredients.
- 53.Kurtzweil P. Alpha hydroxy acids for skin care. FDA Consum. 1998;32:30–35. [PubMed] [Google Scholar]
- 54.Lawrence N, Cox SE, Cockerell CJ, Freeman RG, Cruz PD., Jr A comparison of the efficacy and safety of Jessner's solution and 35% trichloroacetic acid vs 5% fluorouracil in the treatment of widespread facial actinic keratoses. Arch Dermatol. 1995;131:176–181. [PubMed] [Google Scholar]
- 55.Teixeira SP, de Nascimento MM, Bagatin E, et al. The use of fluor-hydroxy pulse peel in actinic porokeratosis. Dermatol Surg. 2005;31:1145–1148. doi: 10.1097/00042728-200509000-00013. [DOI] [PubMed] [Google Scholar]
- 56.Chew J, Gin I, Rau KA, Amos DB, Bridenstine JB. Treatment of upper lip wrinkles: a comparison of 950 microsec dwell time carbon dioxide laser with unoccluded Baker's phenol chemical peel. Dermatol Surg. 1999;25:262–266. doi: 10.1046/j.1524-4725.1999.08237.x. [DOI] [PubMed] [Google Scholar]
- 57.Kaminaka C, Yamamoto Y, Furukawa F. Nevoid basal cell carcinoma syndrome successfully treated with trichloroacetic acid and phenol peeling. J Dermatol. 2007;34:841–843. doi: 10.1111/j.1346-8138.2007.00397.x. [DOI] [PubMed] [Google Scholar]
- 58.Sarkar R, Kaur C, Bhalla M, Kanwar AJ. The combination of glycolic acid peels with a topical regimen in the treatment of melasma in dark-skinned patients: a comparative study. Dermatol Surg. 2002;28:828–832. doi: 10.1046/j.1524-4725.2002.02034.x. discussion 32. [DOI] [PubMed] [Google Scholar]
- 59.Erbil H, Sezer E, Tastan B, Arca E, Kurumlu Z. Efficacy and safety of serial glycolic acid peels and a topical regimen in the treatment of recalcitrant melasma. J Dermatol. 2007;34:25–30. doi: 10.1111/j.1346-8138.2007.00211.x. [DOI] [PubMed] [Google Scholar]
- 60.Lim JT, Tham SN. Glycolic acid peels in the treatment of melasma among Asian women. Dermatol Surg. 1997;23:177–179. doi: 10.1111/j.1524-4725.1997.tb00016.x. [DOI] [PubMed] [Google Scholar]
- 61.Rendon M. Successful treatment of moderate to severe melasma with triple-combination cream and glycolic acid peels: a pilot study. Cutis. 2008;82(5):372–378. [PubMed] [Google Scholar]
- 62.Kalla G, Garg A, Kachhawa D. Chemical peeling--glycolic acid versus trichloroacetic acid in melasma. Indian J Dermatol Venereol Leprol. 2001;67:82–84. [PubMed] [Google Scholar]
- 63.Soliman MM, Ramadan SA, Bassiouny DA, Abdelmalek M. Combined trichloroacetic acid peel and topical ascorbic acid versus trichloroacetic acid peel alone in the treatment of melasma: a comparative study. J Cosmet Dermatol. 2007;6:89–94. doi: 10.1111/j.1473-2165.2007.00302.x. [DOI] [PubMed] [Google Scholar]
- 64.Karam PG. 50% resorcinol peel. Int J Dermatol. 1993;32:569–574. doi: 10.1111/j.1365-4362.1993.tb05024.x. [DOI] [PubMed] [Google Scholar]
- 65.Sharquie KE, Al-Tikreety MM, Al-Mashhadani SA. Lactic acid chemical peels as a new therapeutic modality in melasma in comparison to Jessner's solution chemical peels. Dermatol Surg. 2006;32:1429–1436. doi: 10.1111/j.1524-4725.2006.32352.x. [DOI] [PubMed] [Google Scholar]
- 66.Bari AU, Iqbal Z, Rahman SB. Tolerance and safety of superficial chemical peeling with salicylic acid in various facial dermatoses. Indian J Dermatol Venereol Leprol. 2005;71:87–90. doi: 10.4103/0378-6323.13990. [DOI] [PubMed] [Google Scholar]
- 67.Monheit GD, Chastain MA. Chemical peels. Facial Plast Surg Clin North Am. 2001;9:239–255. viii. [PubMed] [Google Scholar]
- 68.Zakopoulou N, Kontochristopoulos G. Superficial chemical peels. J Cosmet Dermatol. 2006;5:246–253. doi: 10.1111/j.1473-2165.2006.00254.x. [DOI] [PubMed] [Google Scholar]
- 69.Clark E, Scerri L. Superficial and medium-depth chemical peels. Clin Dermatol. 2008;26:209–218. doi: 10.1016/j.clindermatol.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 70.Cernik C, Gallina K, Brodell RT. The treatment of herpes simplex infections: an evidence-based review. Arch Intern Med. 2008;168:1137–1144. doi: 10.1001/archinte.168.11.1137. [DOI] [PubMed] [Google Scholar]
- 71.Landau M. Chemical peels. Clin Dermatol. 2008;26:200–208. doi: 10.1016/j.clindermatol.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 72.Rubin MG. A peeler's thoughts on skin improvement with chemical peels and laser resurfacing. Clin Plast Surg. 1997;24:407–409. [PubMed] [Google Scholar]
- 73.Robertson JG. Rhytidectomy combined with chemical peeling of the superficial cutaneous tissues. Int Surg. 1967;47:576–579. [PubMed] [Google Scholar]
- 74.Hexsel D, Arellano I, Rendon M. Ethnic considerations in the treatment of Hispanic and Latin-American patients with hyperpigmentation. Br J Dermatol. 2006;156(Suppl 1):7–12. doi: 10.1111/j.1365-2133.2006.07589.x. [DOI] [PubMed] [Google Scholar]
- 75.Khunger N. Standard guidelines of care for chemical peels. Indian J Dermatol Venereol Leprol. 2008;74(Suppl):S5–S12. [PubMed] [Google Scholar]
- 76.Finsti Y LM. Exoderm: phenol-based peeling in olive and dark-skinned patients. Int J Cosm Surg Aesthet Dermatol. 2001;3:173–178. [Google Scholar]
- 77.Roberts WE. Chemical peeling in ethnic/dark skin. Dermatol Ther. 2004;17:196–205. doi: 10.1111/j.1396-0296.2004.04020.x. [DOI] [PubMed] [Google Scholar]