Abstract
The following case describes a 68 year-old woman with a 7½ year history of worsening head and neck pain diagnosed as trigeminal neuralgia following surgical resection of a brain tumor. After years of unsuccessful management with medication and physical therapies, a therapeutic trial of chiropractic was carried out. Chiropractic care included ultrasound, manual therapies (manipulation and mobilization), soft tissue therapies, and home stretching exercises. After an initial treatment period followed by 18 months of supportive care the patient reported satisfactory improvement. It became evident that there were at least three sources of her symptoms: mechanical and/or degenerative neck pain, temporomandibular joint syndrome, and trigeminal neuralgia. While never completely pain-free, the patient continued to report that her pains reduced to minimal at times. At the most recent follow-up, the pain had not returned to pre-treatment intractable levels. This case study demonstrates the importance of diagnosing and treating multiple sources of pain and the positive role chiropractic care can have in the management of patients with these clinical conditions. The potential for convergence of sensory input from the upper three cervical segments and the trigeminal nerve via the trigeminocervical nucleus is discussed.
Keywords: trigeminal neuralgia, spinal nucleus, facial pain, neck pain, head pain, chiropractic
Abstract
Le cas suivant décrit une femme de 68 ans qui présente un historique de 7,5 ans de douleurs qui s’aggravent au niveau de la tête et du cou.Le diagnostic : névralgie essentielle du trijumeau à la suite d’une résection chirurgicale d’une tumeur cérébrale. Après des années de tentatives de gestion infructueuses au moyen de médicaments et de physiothérapie, elle a suivi un essai de traitements thérapeutiques chiropratique. Les soins chiropratiques reçus incluent des ultrasons, de la thérapie manuelle (manipulation et mobilisation), des thérapies de tissus mous et des exercices d’étirement à domicile. Après une période initiale de traitement suivie de soins de soutien pendant 18 mois, la patiente a rapporté une amélioration satisfaisante. Il est devenu évident que ses symptômes découlaient de trois sources : douleurs mécaniques ou dégénératives au cou, syndrome de l’articulation temporomandibulaire, et névralgie essentielle du trijumeau. Bien qu’elle ne soit toujours pas entièrement libre de douleur, la patiente continue à rapporter que ses douleurs sont minimales à certains moments. Lors du suivi le plus récent, la douleur n’était pas revenue aux niveaux réfractaires prétraitement. Cette étude de cas démontre l’importance du diagnostic et du traitement des sources multiples de douleur, ainsi que le rôle positif que joue les soins chiropratiques dans la gestion des patients qui présentent ces troubles cliniques. Le potentiel pour la convergence de l’apport sensoriel provenant des trois nerfs rachidiens cervicaux supérieurs et du nerf trijumeau par le biais du noyau trigéminocervical fait l’objet d’une discussion.
Keywords: névralgie essentielle du trijumeau, noyau rachidien, douleur faciale, cervicalgie, céphalalgie, chiropratique
Introduction
The International Association for the Study of Pain (IASP) defines Trigeminal neuralgia (TN) as a sudden, usually unilateral, severe, brief, stabbing recurrent pain in the distribution of one or more branches of the fifth cranial nerve.1
The lifetime prevalence has been reported at 107.5/1,000,000 for men and 200.2/1,000,000 for women, the incidence has been reported at ranging from 3.4–4.7/100,000 for men and 5.9–7.1/100,000 for women.2 TN is roughly twice as common in females compared to males.3,4 However, epidemiological research on TN is limited.
Based on its rarity, it has been estimated that the primary care physician would encounter this disease entity up to four times within a thirty-five year professional career.5 Chiropractors will likely encounter TN with even less frequency. However, chiropractors may play a role in the management of TN through recognition, diagnosis, referral (when necessary), symptom monitoring and management.
The following case describes a patient with a long standing history of TN, neck and head pain.
Case
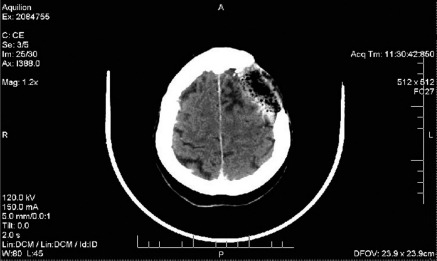
A 68 year old female presented with a 7½ year history of right-sided head and neck pain and parasthesia. In 1995, she had surgical resection of a brain tumor (meningioma). She had further resection in March, 2000 following a recurrence (See Figure 1). Ten days following the second surgery she developed severe facial and head pain. She was subsequently diagnosed with TN by her neurosurgeon. In the 7½ years since the onset of symptoms, her pain had gradually worsened. She had tried acupuncture, physiotherapy, pain medications and anti-seizure medications for pain control. Unfortunately, longer-term relief could not be obtained. She also experienced negative side-effects from several of the medications, including dry mouth, lethargy, and loss of concentration.
Figure 1.
Contrast enhanced computed tomography taken of patient in March, 2000 showing surgical site. Resection of a portion of the left cranium and underlying grey matter is observed
Upon presentation to the chiropractor’s office, her pains were constant, fluctuating between moderate and, at times, intractable levels. Head and facial pain and parasthesia had insidiously become progressively more severe over the previous few months and were now significantly impacting activities of daily living. She rated her pain at 10/10 on a numerical rating scale, “the worst pain she had ever experienced”. She was seeking chiropractic care on the recommendation of a friend as a “last straw” in search of relief. She could not identify any precipitating or aggravating factors for her pains.
Although she was not considered suicidal, she said the pains were so severe that she could not take it anymore. Aside from this pain response, she was considered to have a normal psychosocial profile. She is married and lives at home with her husband, who runs his own business. She enjoys gardening in the summers and going to the casino in the winters. Her children are grown and out of the house. She describes herself as a worrier, and has disturbed sleep as a result at times. She is a non-smoker, and infrequently drinks alcohol. She has hypertension and hypothyroidism, both of which are managed with medication. There was no family history of brain tumour or neuralgia.
Her pain was located over the right parietal and temporal regions of the head, and the lateral face including the cheek, mandible, and mouth. Pain was described variably, ranging from sharp, to deep, to electric like, to feeling like hot water or formication (bugs crawling on the skin). She also described painful and bumpy “lesions” on the inside of the mouth. In addition to the head and facial pains, she also had right-sided pain in both the upper and mid-cervical regions. There was no associated extremity or upper dorsal pain or paresthesia.
On examination, the patient stood with a straight spine on a level pelvis, without observable lateral curvatures to her spine. Slight anterior head carriage was apparent. Facial features were symmetrical without signs of paralysis. There was cranial asymmetry over the surgical site.
Neurological examination of the upper extremity, including motor power, deep tendon reflexes and sensation to light touch, was unremarkable. Cranial nerve screening tests were within normal limits, with the exception of an area of hyper-sensitivity over the face and hemicranium on the right. Light pressure over these regions produced severe pain, especially over the cheek, and less so over the scalp and jaw/anterior neck. Tongue pressure inside the right cheek produced pain to the right side of the face. There were no visible lesions inside the mouth.
Physical examination revealed tenderness upon digital palpation and segmental joint dysfunction of the right C0-1, C1-2 and C2-3 facet joints, and at the C5-6 joint bilaterally. Overlying spasm in the suboccipital and upper cervical paraspinal muscles was apparent. Palpation of the upper cervical paraspinal tissues referred pain to the lateral head and face. The right temperomandibular joint (TMJ) was tender to palpation as were the masseter, pterygoid and temporalis muscles. Cervical axial compression testing with and without rotation was positive for neck pain, but no dorsal or arm pain was produced. Right cervical rotation and extension were painfully restricted during range of motion testing and produced pain in the mid-upper cervical region that did not refer to the face or upper back. Other cervical ranges of motion were within normal limits.
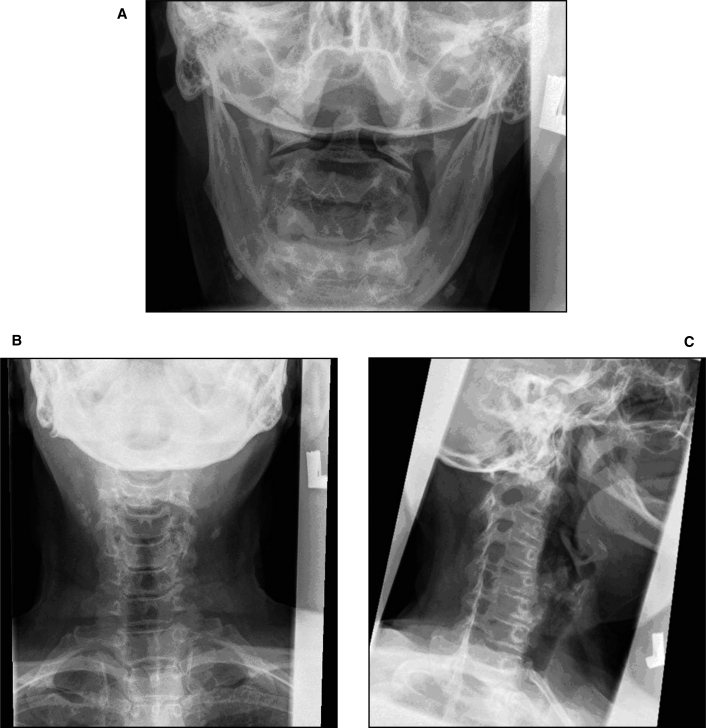
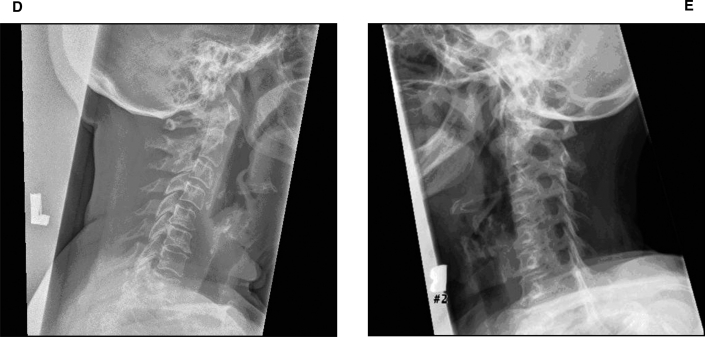
Radiographs of the cervical spine, taken approximately 18 months prior to the initial visit to the chiropractor, showed a loss of the normal cervical lordosis and disc space narrowing with moderate osteophyte formation at the C5-6 and C6-7 levels. The neural foramina were narrowed bilaterally at C5-6 (See Figure 2). These age-related degenerative changes were expected, and were not considered directly related to her symptoms of TN.
Figure 2.
Five view cervical spine radiographic series taken approximately 18 months prior to initial chiropractic visit showing degenerative changes at C5, C6 and C7.
The patient was diagnosed with upper cervical joint and muscle dysfunction, and OA of the mid-lower cervical spine. She was also told that TMJ dysfunction may be contributing to her symptoms. She was offered a course of manual therapy consisting of soft-tissue therapy and joint mobilization/manipulation to the cervical spine. It was also recommended that she perform cervical spine lateral flexion exercises at home. It was explained to her that the cervical dysfunction could be related to the symptoms of TN, or could be a separate entity altogether. The trial of therapy was to consist of two-to-three treatments per week for about two-to-four weeks, after which she would be reassessed. As it was just before the Christmas holiday, it was suggested she do a series of stretches for a week or two and return for treatments after the holidays. She was treated with ultrasound (3 minutes pulsed, 1.9 watts/cm2) over the upper cervical joints on the right, mobilization (rotary and lateral flexion impulses, and manual intermittent long axis traction) and soft tissue therapy (long-fibre and cross-fibre massage). She was shown again how to perform the stretches at home, and released.
The patient returned one week later and was very excited about the relief she had obtained. She reported a 50% improvement that started within a day or two after the first session. She reported her symptom improvement verbally using a scale of 1–10 (or 0–100%), with no improvement being 0 and all better being 10 (or 100%). It was explained to her that this immediate relief was not uncommon, and that time would tell if the relief would be sustained. She was treated again in the same manner, and released until after the New Year holiday. One week later she returned to start the recommended course of therapy. Some of her symptoms (lateral face/chin tenderness and electric “shock-like” pains) had returned, but not to the same intolerable level.
In the following three weeks the patient received six treatments. She was treated with the same methods described above, with additional manual therapies (soft tissue and mobilization) to the temporomandibular joint when required, and manipulation (diversified technique) to the cervical spine when required. Following these treatments she reported 75% improvement in symptoms, with considerably less facial pain. There was less tenderness and hypertonicity to palpation over the right upper cervical muscles, and the upper cervical joints were less restricted. The TMJ region became less tender to palpation.
Over the next eleven days, symptoms gradually worsened. In particular, her temporal and mandibular pains flared, and were made worse with speaking. Despite the recommendation that she return for further treatment, the patient did not return. Symptoms continued to worsen. When the patient returned two weeks after the last treatment, she detailed new medications (carbamazepine and pregabalin) that had been prescribed by her physician. In addition, the patient inquired about a home TENS unit she had previously acquired through a trial of physiotherapy, and was instructed on its use. Two manual therapy sessions within three days of each other were performed, without effect. The patient was then advised to try the home TENS unit, and to return in about two-to-three weeks.
Three weeks later, the patient returned reporting that she had discontinued using the TENS unit. It had apparently aggravated symptoms. Since she stopped using the TENS the symptoms began to improve again, and when she returned to the clinic she rated her pain intensity at 2–3/10. While the frequency of pain was still daily, it was now more controlled. She was advised to continue with the home stretches and massage to the neck, and to return in one month.
Contrary to advice, the patient did not return for five months, with complaints of increased pain which compared to her initial presentation. She was treated with ultrasound, mobilization, and soft tissue therapies to the right upper cervical spine, and anterior thoracic manipulation to the upper thoracic spine. She was given seven treatments over three weeks, to which she reported a 60% improvement. Treatment frequency was reduced to once per week, and she was seen for eight weeks at this frequency. Treatment frequency was then tapered to once every two-to-three weeks, to which the patient was seen five more times. At this time point the patient reported feeling ‘really good’ and that her pain was ‘very manageable.’ Pain intensity was rated as lower than 2/10 on most days and she was able to perform all of her activities of daily living without trouble. The tenderness over the upper cervical joints was considerably reduced. Compression tests were negative, and while right rotation remained slightly restricted, it was no longer painful.
Over the next six months, the patient was seen on an as-needed basis. She returned as needed to keep the neck and face and head pains ‘at bay.’ During flare-ups, treatment frequency increased as necessary, up to six treatments provided over a three week period, to control the pain. Otherwise the patient would span two-to-three weeks between treatment sessions before neck or head/face symptoms would return. Overall, she was pleased with the treatment outcome as it helped to control pain and improve function without the use of medications. She continues to receive chiropractic treatments on an as-needed basis, and at the most recent follow-up, she is “better than ever”, without significant head or face pain for the past 4 months.
Discussion
The International Headache Society (IHS) describes two classifications of TN: classical and symptomatic. In short, if there is no neurological deficit and an underlying cause cannot be identified the condition is labeled as classical TN. Symptomatic TN however may demonstrate neurological loss and is attributable to an underlying lesion that has been determined through specialized testing.6 The full IHS criteria for TN are listed in Table 1.
Table 1.
Diagnostic criteria for trigeminal neuralgia according to the International Headache Society.2
Diagnostic Criteria for Classical Trigeminal Neuralgia
|
Diagnostic criteria for Symptomatic Trigeminal Neuralgia
|
Defining a predominant age group for TN is difficult, though the majority of patients are over the age of 50 years upon presentation.7 The pathological origins most frequently identified are vascular compression and de-myelination, however patients under the age of 40 years are most likely to have multiple sclerosis or a tumor identified as the causative lesion.4
The painful episodes which characterize TN are described as shooting, cutting or lancinating in character by 95% of patients. Pain is primarily felt in one distribution of the trigeminal nerve, unilaterally.2 Attack duration has been found to average 6.5 seconds (SD 6.1; 2–32) when experienced in the V1 distribution, with episodic attacks lasting less than 10 seconds in 82.3% of patients.8 Attack durations longer than 30 seconds were only found in 0.5% of TN episodes.8 Further study examining 229 patients with TN found that all but one patient stated that painful episodes lasted for seconds in duration, versus minutes.9 It should be considered however, that patients may overestimate attack duration given the subjective experience of high-intensity pain.8 Patients were only able to specifically mark a date of onset, therefore defining an acute 1st episode, in 55% of cases. In addition, 75% of attacks were spontaneous in nature.9
Attacks typically involve a stereotypical pattern of oral-facial stimulation for each patient, such as shaving or a light touch within a certain facial zone.4 This mechanism is purported to arise from a sensitization of the wide dynamic range (WDR) neurons, suggested to occur in TN patients.10 This allows for non-noxious myelinated fibres (such as A-delta fibres) to deliver a maximal stimulus to the spinal nucleus of the trigeminal nerve through the WDR neurons.10 The result is light touch perceived as pain. This is the proposed ‘central mechanism’ of TN and explains how the trigeminal nerve can be affected by the stimulus of convergent structures.10 This theory has been similarly explained elsewhere and coined the ‘ignition hypothesis’ for TN attacks, stating that stimulus from peripheral sources are abnormally processed via hyperexcitable afferents of the trigeminal system, resulting in pain.11
Current medical management of TN involves the use of carbamazepine as a first line therapy. Other drugs such as gabapentin, pregabalin and tricyclic antidepressants have shown efficacy with neuropathic pain as well.12 Surgical intervention may include microvascular decompression, balloon compression, rhizolysis or rhizotomies and radio-frequency thermocoagulation.13
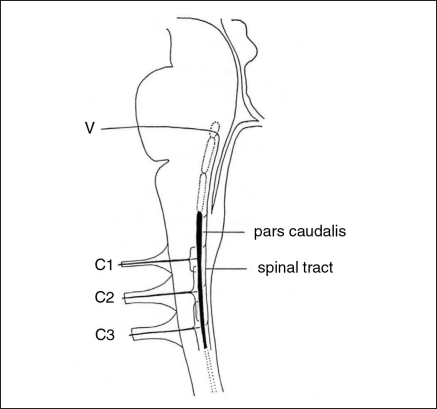
To evaluate manual therapy principles for TN, we must look to proposed mechanisms which initiate pain. It has been postulated that noxious stimulation of cervical afferents can result in headache disorders such as migraine and cervicogenic headache.14,15 This mechanism centres on convergent neurology within the dorsal horn neurons of the upper cervical segments and the spinal nucleus of the trigeminal nerve (medullary dorsal horn), to which are not separated by definitive boundaries.15,16 This single column of grey matter is referred to as the trigeminocervical nucleus.15 Essentially, nociceptive stimulus of the head, face, throat and upper cervical area are all delivered through afferents which terminate on second-order neurons within the trigeminocervical nucleus (Figure 3).
Figure 3.
A sketch of the brainstem demonstrating convergence of the upper cervical segments with trigeminocervical nucleus.14
Reprinted with permission from Elesevier.
The neurophysiologic basis of cervical headache is thought to originate from a prolonged and sustained exposure to deep somatic pain.17 As the central nervous system becomes sensitized to this input, nociception from cervical afferents converges with the dorsal horn neurons shared with the trigemino-cervical system and is projected.17 As the trigeminal system is primarily responsible for processing input from cutaneous sources, projected pain is ‘felt’ within the respective trigeminal fields.17
An animal model of central sensitization of the upper cervical dorsal horns and the medullary dorsal horn has been documented via noxious stimulation of the deep cervical paraspinal muscles.19 Threshold lowering is specifically noted within the WDR neurons of the upper cervical segments, and is relevant in many painful syndromes of the head and neck.19 Similar concepts of sensitization have been reviewed by Mense.20 It is subsequently theorized that treatment of the cervical source can relieve symptomatology in relevant headache disorders.21 To date, there is a growing body of scientific literature supporting the use of manual therapies, such as joint manipulation and mobilization, in the treatment of such headache disorders.17,18,22–24
Based on the central mechanism described earlier, disorders involving neck pain and cervicogenic headache may play a role in lowering the threshold of convergent neurons and sensitizing the trigeminocervical system. This has recently been demonstrated via pressure-pain hyper-algesia in the trigeminal region of patients suffering non-traumatic mechanical neck pain, supporting a sensitizing effect.25 Therefore, manual therapy of a primary source of sensitization (such as in the cervical region) may improve symptoms through decreased sources of amplification. It should be considered however, that manual therapy of the cervical spine is unlikely to completely resolve a patients TN.
Also, it should be considered that patients may present with more than one type of headache disorder and more than one source of head, neck and facial pain. The discussed patient presented with multiple sources of pain: pain arising from the trigeminal nerve itself, the cervical spine and the TMJ. In addition, the patient presented with multiple classifications of cephalalgia: TN and probable cervicogenic headache. Therefore, this patient presented with multiple potential triggers for TN episodes that included mechanical origins.
Special consideration should be made of other effects of cervical spine pain and dysfunction such as joint position sense error,26,27 decreased strength and endurance in the local and global cervical musculature,28–30 allodynia,31 mechanical hypersalgesia32–34 and sensory hypersensitivity.34,35 From these examples, it is clear that nociceptive stimulation within the cervical spine demonstrates broad neuromusculoskeletal effects. With consideration, the broad and sensitizing effects of cervical pain having further effects on the trigeminal system via convergence is a reasonable theoretical assumption. Additionally, the Johansson/Sojka hypothesis surrounding the role of gamma-motor feedback loops could be considered, though this hypothesis remains an unproven theory.36
Within the chiropractic literature, a case surrounding the previously described central mechanism of pain has been published. The case describes a patient with TN who induced an accidental and maximum surge from a home-use TENS unit during a painful attack, and the pain terminated immediately. At three year follow-up the patient remained symptom free. It was postulated that through a diffuse noxious stimulus of the A-delta and C fibres, an inhibitory mechanism was generated on the wide dynamic range neurons thought to be responsible for painful episodes in TN.10 Drawbacks to this case are that the theory of complete symptom resolution is not adequately explained and it provides minimal insight into the use of manual therapy for symptom management in TN patients.
A second case from the chiropractic literature supports the use of manual therapy in a patient with a six year history of TN. However, it pertains to the use of muscle-energy techniques, toggle-recoil manipulation of the atlas and non-specific thoracic and lumbar spine manipulation. Cranial suture manipulation was also employed. The patient received three treatments within close proximity and was then told to return for a two week follow-up. At this time the patient reported of decreased use of carbamazepine and their pain score had decreased to 0.5/10 from 9.5/10. A further three week follow-up revealed exacerbation of symptoms, scoring a 7–8/10 in intensity. Following another three week follow-up period the patient returned reporting slow ablation of symptoms without recurrence. Three month follow-up revealed no recurrence and telephone follow-up at eighteen months revealed that the patient had once again become symptomatic and sought a medical practitioner for laser therapy, which had provided relief.37 While this case does not demonstrate long term improvement following the withdrawal of care, improvement with concurrent manual therapy and sustained short term improvement is noted. Additionally, the case supports the hypothesis that the trigeminal nerve may be affected via convergent structures of the head and neck.
It is important to consider that within this case report, the patient’s symptoms improved via natural history, holding a temporal relationship with the chiropractic treatment plan. This could be possible as TN patients do experience pain-free intervals which range from days to months.9 However, the discussed patient experienced quick relief with chiropractic care subsequent to a long duration of symptoms prior to care, her symptoms returned with non-compliance to her treatment plan, and she once again experienced relief with return to care and sustained improvement when compliant with supportive care. Additionally, as the natural history of TN is known to last beyond thirty years, a theory of spontaneous resolution is cautioned.9 Nonetheless, the hypothesis within this report is speculative. Causation cannot be determined from a single-case design, and our theory requires further validation.
Conclusion
Accepting the limitations of a single-case design, the presented hypothesis may offer new insight into the contribution and exacerbation of TN symptoms in afflicted patients. If such symptoms are augmented by cervical spine syndromes, TMJ syndromes, or other causes of head and facial pain, a trial of manual therapy for those concurrent syndromes may be worth consideration in an attempt to lessen the debilitating impact to patients.
This being said, reliable and reproducible measures of cervical pain and dysfunction which may indicate arthrogenic patterns of pain should be used and monitored during care. Determinants of cervical segmental dysfunction such as motion palpation or static palpation should not be used in isolation when determining the intervention strategy.
More research in the area of TN and cervical spine pain and dysfunction should be conducted to clarify the relationship between them.
Acknowledgments
Special thanks to Dr. Peter Cauwenbergs and Dr. Howard Vernon for their assistance and content expertise in the preparation of this manuscript. In addition, special thanks to the Canadian Memorial Chiropractic College for their continued support of Chiropractic research.
References
- 1.Merskey H, Bogduk N. Classification of chronic pain. Descriptors of chronic pain syndromes and definitions of pain terms. 2nd ed. Seattle: IASP Press; 1994. [Google Scholar]
- 2.Manzoni GC, Torelli P. Epidemiology of typical and atypical craniofacial neuralgias. Neuro Sci. 2005;26:S65–7. doi: 10.1007/s10072-005-0410-0. [DOI] [PubMed] [Google Scholar]
- 3.Tin Goh B, et al. The importance of routine magnetic resonance imaging in trigeminal neuralgia diagnosis. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2001;92:424–9. doi: 10.1067/moe.2001.115130. [DOI] [PubMed] [Google Scholar]
- 4.Yang J, et al. Magnetic resonance imaging used to assess patients with trigeminal neuralgia. Oral Surg Oral Med Oral Path Oral Radiol Endod. 1996;81(3):343–50. doi: 10.1016/s1079-2104(96)80335-0. [DOI] [PubMed] [Google Scholar]
- 5.Krafft RM. Trigeminal neuralgia. Amer Acad Fam Phys. 2008;77(9):1291–6. [PubMed] [Google Scholar]
- 6.Headache Classification Subcommittee of the International Headache Society . The international classification of headache disorders. 2nd edn. Suppl 1. Vol. 24. Cephalalgia: 2004. pp. 9–160. [DOI] [PubMed] [Google Scholar]
- 7.Rasmussen P. Facial Pain I: a prospective survey of 1052 patients with a view of: definition, delimitation, classification, general data, genetic factors, and previous diseases. Acta Neurochir (Wien) 1990;107:111–120. doi: 10.1007/BF01405789. [DOI] [PubMed] [Google Scholar]
- 8.Pareja JA, et al. Duration of attacks of first division trigeminal neuralgia. Cephalalgia. 2005;25:305–8. doi: 10.1111/j.1468-2982.2004.00864.x. [DOI] [PubMed] [Google Scholar]
- 9.Rasmussen P. Facial Pain II: a prospective survey of 1052 patients with a view of: character of the attacks, onset, course and character of pain. Acta Neurochir (Wien) 1990;107:121–8. doi: 10.1007/BF01405790. [DOI] [PubMed] [Google Scholar]
- 10.Thorsen SW, Lumsden SG. Trigeminal neuralgia and long-term remission with transcutaneous electrical nerve stimulation. J Manip Phys Ther. 1997;20(6):415–9. [PubMed] [Google Scholar]
- 11.Devor M, Amir R, Rappaport H. Pathophysiology of trigeminal neuralgia: the ignition hypothesis. Clin J Pain. 2002;18:4–13. doi: 10.1097/00002508-200201000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Jorns TP, Zakrzeksak JM. Evidence-based approach to the medical management of trigeminal neuralgia. Br J Neurosurg. 2007;21(3):253–61. doi: 10.1080/02688690701219175. [DOI] [PubMed] [Google Scholar]
- 13.Spatz AL, et al. Decision analysis of medical and surgical treatments for trigeminal neuralgia: how patient evaluations of benefits and risks affect the utility of treatment decisions. Pain. 2007;131:302–10. doi: 10.1016/j.pain.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 14.Bogduk N. The anatomical basis for cervicogenic headache. J Manipulative Physiol Ther. 1992;15(1):67–70. [PubMed] [Google Scholar]
- 15.Bodguk N. Anatomy and physiology of headache. Biomed & Pharmacother. 1995;45:435–45. doi: 10.1016/0753-3322(96)82687-4. [DOI] [PubMed] [Google Scholar]
- 16.Olszewski J. On the anatomical and functional organization of the spinal trigeminal nucleus. J Comp Neurol. 1950;92:401–3. doi: 10.1002/cne.900920305. [DOI] [PubMed] [Google Scholar]
- 17.Vernon H. The effectiveness of chiropractic manipulation in the treatment of headache: an exploration in the literature. J Manipulative Physiol Ther. 1995;18:611–17. [PubMed] [Google Scholar]
- 18.Vernon H. Spinal manipulation in the management of tension-type migraine and cervicogenic headaches: the state of the evidence. Top Clin Chiropr. 2002;9(1):14–20. [Google Scholar]
- 19.Vernon H, Sun K, Zhang Y, Yu XM, Sessle B. Central sensitization induced in trigeminal and upper cervical dorsal horn neurons by noxious stimulation of deep cervical paraspinal tissues in rats with minimal surgical trauma. J Manipulative Phsyiol Ther. 2009;32(7):506–514. doi: 10.1016/j.jmpt.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mense S. Muscle pain: mechanisms and clinical significance. Dtsch Arztebl Int. 2008;105(12):214–9. doi: 10.3238/artzebl.2008.0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vernon H. Spinal Manipulation and headaches: an update. Top Clin Chiropr. 1995;2(3):34–47. [Google Scholar]
- 22.Tuchin PJ, Pollard H, Bonello R. A randomized controlled trial of chiropractic spinal manipulative therapy for migraine. J Manipulative Physiol Ther. 2000;23(2):91–5. [PubMed] [Google Scholar]
- 23.Vernon H, Jansz G, Goldsmith CH, McDermaid C. A randomized, placebo-controlled clinical trial of chiropractic and medical prophylactic treatment of adults with tension-type headache: results from a stopped trial. J Manipulative Physiol Ther. 2009;32(5):344–51. doi: 10.1016/j.jmpt.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 24.Haas M, Spegman A, Peterson D, Aickin M, Vavrek D. Dose response and efficacy of spinal manipulation for chronic cervicogenic headache: a pilot randomized controlled trial. The Spine Journal. 2010;10:117–128. doi: 10.1016/j.spinee.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.La Touche R, Fernandez-de-las-Penas C, Fernandez-Carnero J, Diaz-Parreno S, Paris-Alemany A, Arendt-Nielsen L. Bilateral mechanical-pain sensitivity over the trigeminal region in patients with chronic mechanical neck pain. The Journal of Pain. 2010;11(3):256–263. doi: 10.1016/j.jpain.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 26.Feipel V, Salvia P, Klein H, Rooze M. Head repositioning accuracy in patients with whiplash-associated disorders. Spine. 2006;31(2):E51–8. doi: 10.1097/01.brs.0000194786.63690.54. [DOI] [PubMed] [Google Scholar]
- 27.Revel M, Andre-Deshays C, Minguet M. Cervicocephalic kinesthetic sensibility in patients with cervical pain. Arch Phys Med Rehabil. 1991;72(5):288–91. [PubMed] [Google Scholar]
- 28.O’Leary S, Jull G, Kim M, Vincenzino B. Cranio-cervical flexor muscle impairement at maximal, moderate, and low loads is a feature of neck pain. Man Ther. 2007;12(1):34–9. doi: 10.1016/j.math.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 29.Barton PM, Hayes KC. Neck flexor muscle strength, efficiency, and relaxation times in normal subjects and subjects with unilateral neck pain and headache. Arch Phys Med Rehabil. 1996;77(7):680–7. doi: 10.1016/s0003-9993(96)90008-8. [DOI] [PubMed] [Google Scholar]
- 30.Falla DL, Jull GA, Hodges PW. Patients with neck pain demonstrate reduced electromyographic activity of the deep cervical flexor muscles during performance of the craniocervical flexion test. Spine. 2004;29(19):2108–14. doi: 10.1097/01.brs.0000141170.89317.0e. [DOI] [PubMed] [Google Scholar]
- 31.Koelbaek Johansen M, Graven-Nielsen T, Schou Olesen A, Arendt-Nielsen L. Generalised muscular hyperalgesia in chronic whiplash syndrome. Pain. 1999;83:229–34. doi: 10.1016/s0304-3959(99)00106-2. [DOI] [PubMed] [Google Scholar]
- 32.Koltzenburg M, Torebork HE, Wahren LK. Nocicepter modulated central sensitization causes mechanical hyperalgesia in acute chemogenic and chronic neuropathic pain. Brain. 1994;117(3):579–91. doi: 10.1093/brain/117.3.579. [DOI] [PubMed] [Google Scholar]
- 33.Kasch H, Stengaard-Pedersen K, Arendt-Nielsen L, Staehelin Jensen T. Pain thresholds and tenderness in neck and head following acute whiplash injury: a prospective study. Cephalalgia. 2001;21(3):189–97. doi: 10.1046/j.1468-2982.2001.00179.x. [DOI] [PubMed] [Google Scholar]
- 34.Sterling M, Jull G, Vincenzino B, Kenardy J. Sensory hypersensitivity occurs soon after whiplash injury and is associated with poor recovery. Pain. 2003;104(3):509–17. doi: 10.1016/S0304-3959(03)00078-2. [DOI] [PubMed] [Google Scholar]
- 35.Scott D, Jull G, Sterling M. Widespread sensory hypersensitivity is a feature of chronic whiplash-associated disorder but not chronic idiopathic neck pain. Clin J Pain. 2005;21(2):175–81. doi: 10.1097/00002508-200503000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Knutson GA. The role of the gamma-motor system in increasing muscle tone and muscle pain syndromes: a review of the Johannson/Sojka hypothesis. J Manipulative Physiol Ther. 2000;23(8):564–72. doi: 10.1067/mmt.2000.109674. [DOI] [PubMed] [Google Scholar]
- 37.Pederick FO. Cranial and other chiropractic adjustments in the conservative treatment of chronic trigeminal neuralgia: a case report. Chiropr J Aust. 2005;35:9–15. [Google Scholar]