Abstract
Objectives
To examine African American women's perception of their risk for obesity-related comorbid illnesses compared to their weight category.
Methods
Participants were recruited from urban health centers in Atlanta, Georgia. Anthropometric measurements and self-reported demographics, medical conditions, and health beliefs about obesity and its related comorbid diseases were recorded.
Results
More than 80% of the women (N = 323) were either overweight or obese. Among overweight women, 44% reported being a normal weight. Seventy-two percent of the obese women reported being overweight, and 13.6% reported that they were obese. All women reported that each disease was "very serious;" however, overweight women reported having the same risk for each disease as normal weight women. Obese women reported having a higher risk of each disease (p < .05 for all diseases).
Conclusion
Overweight and obese women underestimate their weight categories. Overweight, but not obese, women reported the same perceived susceptibility for obesity-related comorbid diseases as normal-weight women. An increase in the perceived threat to health may motivate women to increase prevention efforts in the early stage of overweight to prevent or delay morbidity or mortality.
Keywords: obesity, body weight
INTRODUCTION
Obesity has reached an all time high in the United States.1 According to the National Health and Nutrition Examination Survey (NHANES) 2005–2006, it is estimated that more than 1 in 3 adults, or 72 million people, are obese. Although these figures are alarming, the prevalences of overweight and obesity are even higher among minority females. Almost 82% of African American women have a body mass index (BMI) greater than or equal to 25 (overweight), and 54% have a BMI greater than or equal to 30 (obese).2 Although numerous public health and governmental agencies have produced numerous reports on the state of obesity in the United States to raise awareness, it is unclear if those who are most at risk are aware of their overweight or obesity diagnosis and the risk associated with being overweight or obese.3–5 According to the health belief model (HBM), the perceived threat of a health condition can help predict an individual’s changes in health behaviors, although it is not the only factor,6 The concept of perceived “threat” to health has 2 components: perceived susceptibility, which is one’s subjective perception of the risk of contracting a health condition, and perceived severity, which is one’s feelings concerning the seriousness of contracting an illness or of leaving it untreated. We undertook this important study to determine if (1) African American women accurately perceive their weight category and (2) if there was a relationship among measured weight category, perceived weight category and perceived threat of comorbidities associated with overweight and obesity.
There have been several studies that discussed perception of body size for Americans.7–9 In general, it has been shown that for obese (BMI ≥30) women there may be no difference between African American and white women regarding accurate perception of overweight (87% vs 90%). However, for overweight women (BMI 25–29.9), African American women are less likely than their white counterparts to accurately perceive their weight status (55% vs 82%).8,9 Many studies have shown that African American women are also more likely to be satisfied with a higher body weight than their white counterparts.10–12 Perception of weight status may have more cultural connotations with less societal pressure to be thin for African American women compared to white women.10,12 While this may be protective to self-esteem for African American women, it stands to reason that underestimating their weight category places these women at higher risk for continuance of overweight and obesity. There is little information about the relationship of accurate recognition of weight categories and the perceived threat of obesity-related comorbid illnesses by African American women.
The comorbid diseases associated with overweight and obesity are well published include hypertension or high blood pressure, type 2 diabetes mellitus, and high cholesterol, all of which significantly increase the risk of developing cardiovascular disease (CVD).13 Hypertension is the most common comorbid disease associated with overweight in adults among all ages, races, and sexes.14 Type 2 diabetes mellitus affects more than 23 million Americans, with 5.7 million unaware of their diagnosis.15
According to the Centers for Disease Control and Prevention (CDC), CVD is the number 1 killer of Americans, killing 685 089 in 2003 (51% of them women), thus accounting for 28% of all US deaths.16 According to the CDC, “in 2002, age-adjusted death rates for heart disease were higher among black women (169.7 per 100000) than among white women (131.2 per 100000).”17 Although CVD awareness has increased from 1997 to 2003, there still remains a significant gap in the perceived and actual risk of CVD in women, especially minority women.18 Although 55% of all women correctly identified heart disease as the leading cause of death in women, minority women were more likely to underestimate their risk for CVD than white women. In addition, previous research also indicates that fewer African American women identify being overweight or obese as a major risk factor of heart disease compared with the white women.19 The study concluded that most women do not perceive that heart disease is a substantial health concern and report that they are not well informed about their risk. In a study in the African American community, Graham et al reported that there was “a significant proportion of individuals who scored at high risk for diabetes or hypertension [who] were unaware of their risk for these conditions.”20 Type 2 diabetes and high blood pressure, as well as high cholesterol, are significant modifiable risk factors for CVD.21
METHODS
This was a cross-sectional study of African American women conducted between 2004 and 2006, using The Morehouse School of Medicine Obesity Health Belief Survey (MSM-OHBS), which was developed by the investigators. The survey recorded the women’s measured anthropometric measurements and assessed self-reported demographics, medical conditions, and health beliefs about obesity and related comorbid diseases. Participants were a convenience sample of women visiting urban health centers located in Atlanta, Georgia. Descriptive statistics were calculated for all relevant variables. A χ2 was used to identify associations between the dichotomous and categorical data. Medians, ranges, and the Student’s t test were calculated and compared for continuous variables.
Trained research assistants recruited participants from the waiting room of the clinic, and written informed consent was obtained. Inclusion criteria were (1) women who self-identified as African American, (2) were born in the United States and were at least 18 years of age. Exclusion criteria were (1) women with a preexisting disease (eg, hypothyroidism, Cushing’s syndrome, etc) or medication usage (eg, corticosteroids, synthroid, etc) that could cause excessive weight gain and (2) pregnant women. Surveys with missing data on key variables were excluded from analysis.
Questionnaire
The questionnaire recorded demographic variables, such as age, annual income, insurance type, and education level. To determine self-perception of weight category, participants were asked to respond to “I feel I am,” with choices of underweight, normal weight, overweight, or obese. Participants were then asked (yes/no) if they had been diagnosed with high blood pressure, type 2 diabetes, high cholesterol, or heart disease. To assess perceived seriousness of obesity-related illness, subjects were asked to indicate how serious they believed each of the conditions related to obesity were. Possible responses were “not serious” = 1, “a little” = 2, “somewhat serious” = 3, “very serious” = 4, and “extremely serious” = 5. To assess perceived susceptibility, women were then asked “How likely do you think you are to develop “X” (X = CVD, high blood pressure, type 2 diabetes mellitus and high cholesterol) given your current weight?” Possible responses were “not at all” = 1, “a little” = 2, “somewhat” = 3, “very” = 4, and “extremely = 5.
Each Likert item was then converted to a numerical equivalent (1–5); and the means, medians, and standard deviations were calculated for each question. Higher scores indicated a higher agreement with the statement.
RESULTS
A total of 323 women who answered the question about weight perception and had both a weight and height recorded were included in the final analysis (Table 1). More than 90% of the women completed high school, and 72% had some type of insurance. The mean age was 37.6 (SD ± 13.6). In our study, 25.7% and 54.5% of the women were overweight or obese, respectively, for a total of 259 women. Among the overweight women, 44% actually reported being a normal weight. Seventy-two percent of the obese women reported they were overweight, and 13.6% reported that they were as obese (Table 2).
Table 1.
Demographics of Study Participants
| N | % | |
|---|---|---|
| Total study participants | 323 | 100 |
| Measured body mass index category | ||
| Underweight | 5 | 1.5 |
| Normal weight | 59 | 18.3 |
| Overweight | 83 | 25.7 |
| Obese | 176 | 54.5 |
| Education level | ||
| Less than high school | 16 | 5.0 |
| Completed high school | 173 | 53.9 |
| Completed technical school | 76 | 23.7 |
| Completed college or higher | 56 | 17.5 |
| Insurance type | ||
| Medicaid | 159 | 50 |
| Medicare | 23 | 7.2 |
| Private | 47 | 14.8 |
| None | 89 | 28 |
| Age | ||
| 18–24 | 44 | 14.2 |
| 25–34 | 113 | 36.6 |
| 35–44 | 52 | 16.8 |
| ≥45 | 100 | 32.4 |
Table 2.
Measured Weight Category Compared to Reported Weight Category
| Reported Weight Category |
|||||
|---|---|---|---|---|---|
| Underweight | Normal Weight | Overweight | Obese | Total | |
| Measured Weight | |||||
| Category | N(%) | N(%) | N(%) | N(%) | N(%) |
| Underweight | 1 (20.0%) | 4 (80.0%) | 0 (0%) | 0 (0%) | 5 (100%) |
| Normal weight | 7 (11.9%) | 47(79.7%) | 1 (6.8%) | 4(1.7%) | 59 (100%) |
| Overweight | 3 (3.6%) | 37 (44.6%) | 43 (51.8%) | 0 (0%) | 83 (100%) |
| Obesea | 1 (0.6%) | 24 (13.6%) | 127 (72.2%) | 24 (13.6%) | 176 (100%) |
P values < .001 compared to both normal weight and overweight women.
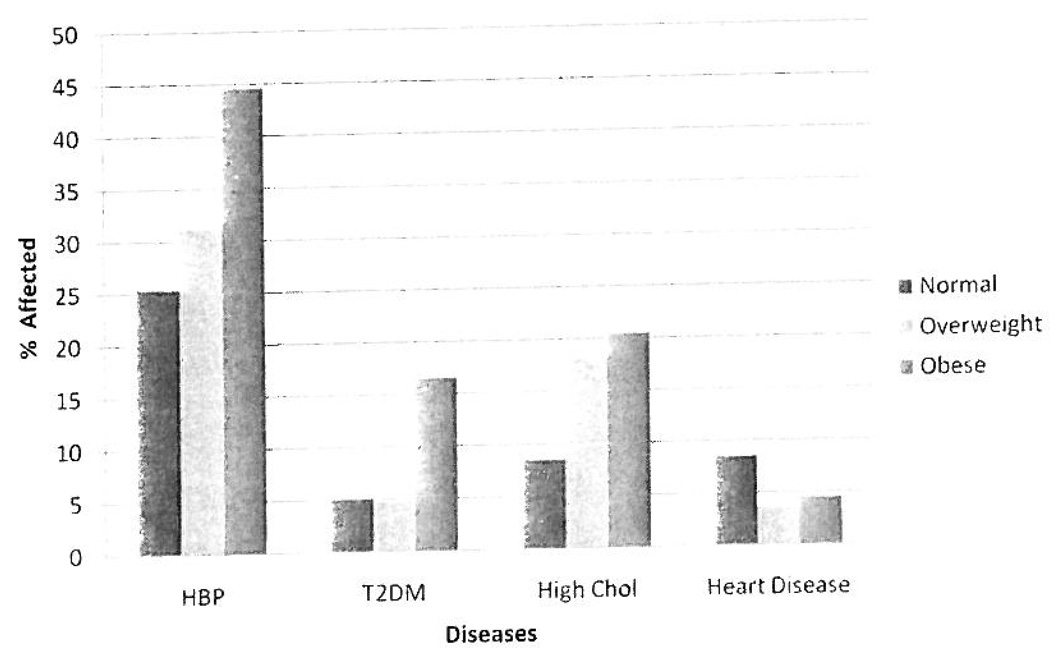
Overall, 43% of all the women reported having at least 1 target disease, and 16% reported having at least 2 target diseases. Specifically, 37% of women reported having a diagnosis of high blood pressure, 11.3% reported type 2 diabetes, 17.7% reported high cholesterol, and 5.1% reported heart disease (CVD). Obese women were more likely to report a diagnosis of high blood pressure and type 2 diabetes, compared with normal-weight women and overweight women (P = .19 and .027, respectively) (Figure).
Figure.
Obesity-Related Diseases by Weight Category
There were no significant differences in perception of the seriousness of high blood pressure, type 2 diabetes, high cholesterol, and CVD among normal-weight, overweight, and obese women. The mean response in each group ranged from 3.92 to 4.47 (very serious), and each median was either 4 or 5. The mean perceived risk (susceptibility) for the 4 target diseases ranged from 2.2 to 2.7 (medians were either 1 or 2) for normal-weight and overweight women and did not differ significantly. When overweight women were stratified into those who thought they were overweight and those who thought they were of normal weight, both groups perceived themselves to have a relatively low risk for these diseases (mean range, 2.3–2.7). Obese women reported having a higher susceptibility of each disease than women of normal weight, with mean responses ranging from 3.17 to 3.51 (compared to 2.21–2.27 for normal-weight women). Perceived susceptibility was statistically significant for each target disease (p < .02 for all diseases) for obese women compared to normal-weight women (Table 3).
Table 3.
Perceived Likelihood of Developing Obesity Comorbid Disease
| Comorbid Diseases |
||||
|---|---|---|---|---|
| Measured Weight Category | High Blood Pressure |
Type 2 Diabetes Mellitus |
High Cholesterol |
Cardiovascular Disease |
| Normal weight | % | % | % | % |
| Not likely at all = 1 | 51.9 | 51.0 | 47.1 | 46.9 |
| A little = 2 | 15.4 | 13.7 | 19.6 | 16.3 |
| Somewhat = 3 | 9.6 | 13.7 | 9.8 | 12.2 |
| Very = 4 | 9.6 | 9.8 | 11.8 | 10.2 |
| Extremely = 5 | 9.6 | 5.9 | 5.9 | 6.1 |
| Don't know = 6 | 3.8 | 5.9 | 5.9 | 8.1 |
| Mean of answersa | 2.21 | 2.23 | 2.27 | 2.24 |
| Median of answersb | 1.0 | 1.0 | 2.0 | 2.0 |
| Overweight | ||||
| Not likely at all = 1 | 29.4 | 43.5 | 29.4 | 42.9 |
| A little = 2 | 22.1 | 10.1 | 27.9 | 12.9 |
| Somewhat = 3 | 17.6 | 17.4 | 23.5 | 20.0 |
| Very = 4 | 13.2 | 11.6 | 8.8 | 10.0 |
| Extremely = 5 | 13.2 | 5.8 | 5.9 | 5.7 |
| Don't know = 6 | 4.4 | 11.6 | 4.4 | 8.6 |
| Mean of answersa | 2.72 | 2.60 | 2.47 | 2.49 |
| Median of answersa | 2.0 | 2.0 | 2.0 | 2.0 |
| Obese | ||||
| Not likely at all = 1 | 11.7 | 21.9 | 16.8 | 19.5 |
| A little = 2 | 14.8 | 14.6 | 11.6 | 15.4 |
| Somewhat = 3 | 17.3 | 16.6 | 21.9 | 19.5 |
| Very = 4 | 24.7 | 21.2 | 24.5 | 22.8 |
| Extremely = 5 | 29.6 | 22.5 | 21.3 | 19.5 |
| Don't know = 6 | 1.9 | 3.3 | 3.9 | 3.4 |
| Mean of answersab | 3.51 | 3.17 | 3.33 | 3.17 |
| Median of answersa | 4.0 | 3.0 | 3.0 | 3.0 |
Means and medians were calculated by assigning numerical values to the Likert scale Items.
Means for obese women were statistically significant (p > .02) compared lo normal-weight women.
DISCUSSION
The percentage of overweight and obesity was very high in the sample population, with more than 80% belonging to either category. Results indicated that overweight and obese women are likely to underestimate their weight category. This study showed almost half of overweight women reported that they were of normal weight; and while obese women were more likely to recognize themselves as overweight, they were not likely to categorize themselves as obese. This suggests that for African American overweight and obese women, overweight is more recognized at higher BMIs than the standard cutoffs of 25 and 30, respectively. This trend has been also reported by others.23,23 Possible reasons for weight category underestimation may be the lack of information on the definition of overweight, not being informed about their weight category, or a genuine belief that they are of normal weight, despite having knowledge about their actual weight category as told by a health care provider. Some have suggested that different cultural norms and a shift to a more overweight society in general have skewed perceptions.10,24,25 If people do not believe that they are overweight, public health campaigns that address obesity may not engage them.
The most commonly reported obesity-related comorbid illness was high blood pressure for all weight categories, which is consistent with a nationally representative sample of overweight and obese US adults.14 In that same study, approximately 30% to 40% of all black women reported having at least 1 obesity-associated comorbid condition, which is similar to findings of 43%. However, the prevalence of at least 2 obesity-associated comorbid conditions in overweight and obese black women ranged from approximately 20% to 40% in the national representative study, but was only 16% in our study. There is not a clear explanation for these inconsistent findings, but underdiagnosis may be more prevalent in our sample.
Overweight African American women in this survey perceived themselves to be at the same risk for CVD, high blood pressure, type 2 diabetes and high cholesterol as normal-weight women. Even if overweight women believed that they were overweight, their perceived susceptibility of developing a comorbid illnesses was not different from those who thought they were of a normal weight. The lack of perceived increase in susceptibility may be accurate because there was no difference in the reported rates of diseases between normal-weight and overweight women. This lack of difference between the 2 groups could be a true finding or represent an underdiagnosis of comorbidities in the overweight group. Although most of them misclassified themselves as overweight, obese women did report having the target diseases more often and being at higher risk for developing them.
Many of the target diseases can have an insidious onset or milder symptomatology at the onset, so this is a critical time for initiating lifestyle changes to improve the conditions (secondary prevention). Thus, it is important to move forward with public health campaigns to help overweight African American women recognize and prevent overweight and obesity. Early recognition and understanding of the health impacts of overweight may heighten the perceived threat of excess weight gain, thus motivating women to change behaviors to prevent overweight and obesity.
Longitudinal studies to assess the impact of early recognition of overweight on lifestyle modification to reduce comorbid diseases and subsequent mortality are needed. It is important to note that it is not clear the strength of the relationship of high BMI on all-cause mortality for African American women. The evidence linking overweight to higher mortality in black women (as compared to white women) is inconsistent. Several studies suggest that amongst African Americans, the death rate increases with increasing levels of BMI, but not as much as it does for whites.26,27 While modifying weight-related risk factors may improve overall health, there still may exist other factors (environmental) that contribute to the disparities in overall mortality between black and white women.
Awareness campaigns, community interventions, and individual physician-patient interaction should reinforce awareness of the risk of disease in African American women. Novel approaches to help overweight African American women (more so than obese African American women) must be developed and tested since this group is less aware of the health risks associated with their condition and obesity. The medical community should continue efforts to work with the private sector to create and market awareness and prevention messages culturally tailored to this segment of the population.
This study was a cross-sectional design, so a causal relationship could not be established. This was a very homogenous sample, so the results cannot be generalized to women of different ethnicity or economic status. As this study did not verify the health conditions of the women, some self-reports may not be accurate.
ACKNOWLEDGMENTS
Thanks to West End Medical Center Inc, Atlanta, Georgia, and Grady Memorial Hospital Neighborhood Center at East Point, Atlanta, Georgia.
Funding/Support: Funding was provided by a grant (5P20RR11104) from the National Center for Research Resources, a component of the National Institutes of Health.
REFERENCES
- 1.Ogden CL, Carroll MD, McDowell MA, Flegal KM. NCHS data brief no 1. Hyattsville, MD: National Center for Health Statistics; 2007. Obesity among adults in the United States—no change since 2003–2004. [PubMed] [Google Scholar]
- 2.Ogden C, Carroll M, Curtin L, McDowell M, Tabak C, Flegal K. Prevalence of overweight and obesity in The United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 3.Levi J, Gadolo E, Segal LM. F as in fal: how obesity policies are failing in America. Washington, DC: Trust for America's Health; 2007. [Google Scholar]
- 4.Washington, DC: Institute of Medicine; 2006. [Accessed March 23, 2009]. Report Brief: Progress in preventing childhood obesity: How do we measure up? http://www.iom.edu/Object.File/Master/36/984/11722_reportbrief.pdf. [Google Scholar]
- 5.US Department of Health and Human Services. Rockville, MD: Government Printing Office; 2001. [Accessed March 10, 2009]. The Surgeon General's Call to Action to Prevent and Decrease Over-weight and Obesity. http;//www.surgeongeneral.gov/topics/obesity/. [Google Scholar]
- 6.Arlington, VA: Family Health International; 2007. [Accessed March 20, 2009]. Behavior Change: A Summary of Four Major Theories. http://www.fhi.org/NR/rdonlyres/ei26vbslp-sidmahhxc332vwo3g233xsqw22er3volqvrfjvubwyzclvqjcbdgexyzl3msu4m-n6xv5j/BCCSummaryFourMajorTheories.pdf. [Google Scholar]
- 7.Nielsen L. Black undergraduate and white undergraduate eating disorders and related altitudes. Coll Stud J. 2002;34:353. [Google Scholar]
- 8.Demarest J, Allen R. Body image: gender, ethnic, and age differences. J Soc Psychol. 2000;140:465. doi: 10.1080/00224540009600485. [DOI] [PubMed] [Google Scholar]
- 9.Flynn KJ, Fitzgibbon M. Body images and obesity risk among black females; A review of the literature. Ann Behav Med. 1998;20:13. doi: 10.1007/BF02893804. [DOI] [PubMed] [Google Scholar]
- 10.Chang VW, Christakis NA. Self-perception of weight appropriateness in the United States. Am J Prev Med. 2003;24:332–339. doi: 10.1016/s0749-3797(03)00020-5. [DOI] [PubMed] [Google Scholar]
- 11.Rand CSW, Kuldau JM. The epidemiology of obesity and self-defined weight problem in the general population; gender race, age, and social class. Int J Eat Disord. 1990;9:329–343. [Google Scholar]
- 12.Powell AD, Kahn AS. Racial differences in women's desires to be thin. Int J Eat Disord. 1995;17:191–195. doi: 10.1002/1098-108x(199503)17:2<191::aid-eat2260170213>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 13.NHLBI Obesity Task Force. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res. 1998;6 suppl 2:51S–209S. [PubMed] [Google Scholar]
- 14.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. National Diabetes Fact Sheet, 2007. [Accessed March 10, 2009]; http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf.
- 16.Centers for Disease Control and Promotion, Division of Heart Disease and Stroke Prevention. Heart Disease Fact Sheet. [Accessed March 10, 2009]; http://www.cdc.gov/DHDSP/library/fs_heart_disease.htm.
- 17.Centers for Disease Control and Promotion, Division of Heart Disease and Stroke Prevention. Women and Heart Disease Fact Sheet. [Accessed March 10, 2009]; http://www.cdc.gov/DHDSP/library/fs_women_heart.htm.
- 18.Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking women's awareness of heart disease: an American Heart Association national study. Circulation. 2004;109:573–579. doi: 10.1161/01.CIR.0000115222.69428.C9. [DOI] [PubMed] [Google Scholar]
- 19.Mosca L, Jones WK, King KB, Ouyang P, Redberg RF, Hill MN for the American Heart Association Women's Heart Disease and Stroke Campaign Task Force. Awareness, perception, and knowledge of heart disease risk and prevention among women in The United Slates. Arch Fam Med. 2000;9:506–515. doi: 10.1001/archfami.9.6.506. [DOI] [PubMed] [Google Scholar]
- 20.Graham GN, Leath B, Payne K, et al. Perceived versus actual risk for hypertension and diabetes in The African American community. Health Promot Pract. 2006;7(1):34–46. doi: 10.1177/1524839905283891. [DOI] [PubMed] [Google Scholar]
- 21.American Heart Association. Risk Factors and Coronary Artery Disease. [Accessed August 1, 2008]; http://www.americanheart.org/presenter.jhtml?identifier=4726.
- 22.Bennett GG, Wolin KY. Satisfied or unaware? Racial differences in perceived weight status. Int J Behav Nutr Phys Act. 2006;3:40. doi: 10.1186/1479-5868-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paeralakul S, While MA, Williamson DA, Ryan DH, Bray GA. Sex, race/ethnicity, socioeconomic status, and BMI in relation to self-perception of overweight. Obes Res. 2002;10(5):345–350. doi: 10.1038/oby.2002.48. [DOI] [PubMed] [Google Scholar]
- 24.Dawson DA. Ethnic differences in female overweight: data from the 1985 National Health Interview Survey. Am J Public Health. 1988;78:1326–1329. doi: 10.2105/ajph.78.10.1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuk JL, Ardern CI, Church TS, Hebert JR, Sui X, Blair SN. Ideal weight and weight satisfaction: association with health practices. Am J Epidemiol. 2009;170(4):456–463. doi: 10.1093/aje/kwp135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW., Jr Body-mass index and mortality in a prospective cohort of US adults. N Engl J Wed. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 27.Stevens J, Keil JE, Rust PF, Tyroler HA, Davis CE, Gazes PC. Body mass index and body girths as predictors of mortality in black and white women. Arch Intern Med. 1992;152:1257–1262. [PubMed] [Google Scholar]