Abstract
Glucose levels 2 h after an oral glucose challenge are a clinical measure of glucose tolerance used in the diagnosis of type 2 diabetes. We report a meta-analysis of nine genome-wide association studies (n = 15,234 nondiabetic individuals) and a follow-up of 29 independent loci (n = 6,958–30,620). We identify variants at the GIPR locus associated with 2-h glucose level (rs10423928, β (s.e.m.) = 0.09 (0.01) mmol/l per A allele, P = 2.0 × 10−15). The GIPR A-allele carriers also showed decreased insulin secretion (n = 22,492; insulinogenic index, P = 1.0 × 10−17; ratio of insulin to glucose area under the curve, P = 1.3 × 10−16) and diminished incretin effect (n = 804; P = 4.3 × 10−4). We also identified variants at ADCY5 (rs2877716, P = 4.2 × 10−16), VPS13C (rs17271305, P = 4.1 × 10−8), GCKR (rs1260326, P = 7.1 × 10−11) and TCF7L2 (rs7903146, P = 4.2 × 10−10) associated with 2-h glucose. Of the three newly implicated loci (GIPR, ADCY5 and VPS13C), only ADCY5 was found to be associated with type 2 diabetes in collaborating studies (n = 35,869 cases, 89,798 controls, OR = 1.12, 95% CI 1.09–1.15, P = 4.8 × 10−18).
Type 2 diabetes (T2D) is defined as a state of chronic hyperglycemia defined as elevated glucose levels measured either when fasting or 2 h after glucose challenge (2-h glucose) during an oral glucose tolerance test (OGTT). GWAS have contributed to the identification of many established T2D-associated loci1. More recently, collaborative efforts of the Meta-Analysis of Glucose and Insulin-related traits Consortium (MAGIC) and other investigators have led to the discovery of genetic variation associated with fasting glucose levels in nondiabetic individuals, with MTNR1B additionally conferring risk of T2D2–5. Not all loci associated with fasting glucose showed association with T2D3,4, suggesting that GWAS of quantitative traits related to diabetes can also identify physiological loci that provide mechanistic insights into normal trait variation. An accompanying study by MAGIC has identified 16 loci associated with fasting glucose or fasting insulin in a GWAS-based meta-analysis; 9 of these loci are newly identified, and 5 also show evidence for association with T2D6.
Although there are common mechanisms, such as insulin secretion, that regulate fasting and stimulated glucose levels, there are distinct mechanisms regulating glucose levels after an oral glucose challenge. For example, oral glucose intake engenders the incretin effect, in which intestinal cells release insulin secretagogues, mainly glucagon-like peptide 1 (GLP1) and gastric inhibitory polypeptide (GIP), leading to a higher insulin response compared to that from a matched intravenous glucose stimulation. Additionally, numerous epidemiological studies have shown that OGTT 2-h glucose levels predict cardiovascular disease morbidity and mortality7, even in the nondiabetic range of hyperglycemia8 and independently of fasting glucose levels9.
Two-hour glucose level is a heritable quantitative trait (heritability (h2) = 0.40)10 that has been associated with diabetes, and assessing the genetic contribution to variability in 2-h glucose provides an opportunity to identify genetic variation underlying this trait in nondiabetic individuals and to test the secondary hypothesis that these loci may also contribute to T2D susceptibility. Here we performed a meta-analysis of several 2-h glucose GWAS to expand our understanding of post–oral glucose challenge physiology in nondiabetic individuals.
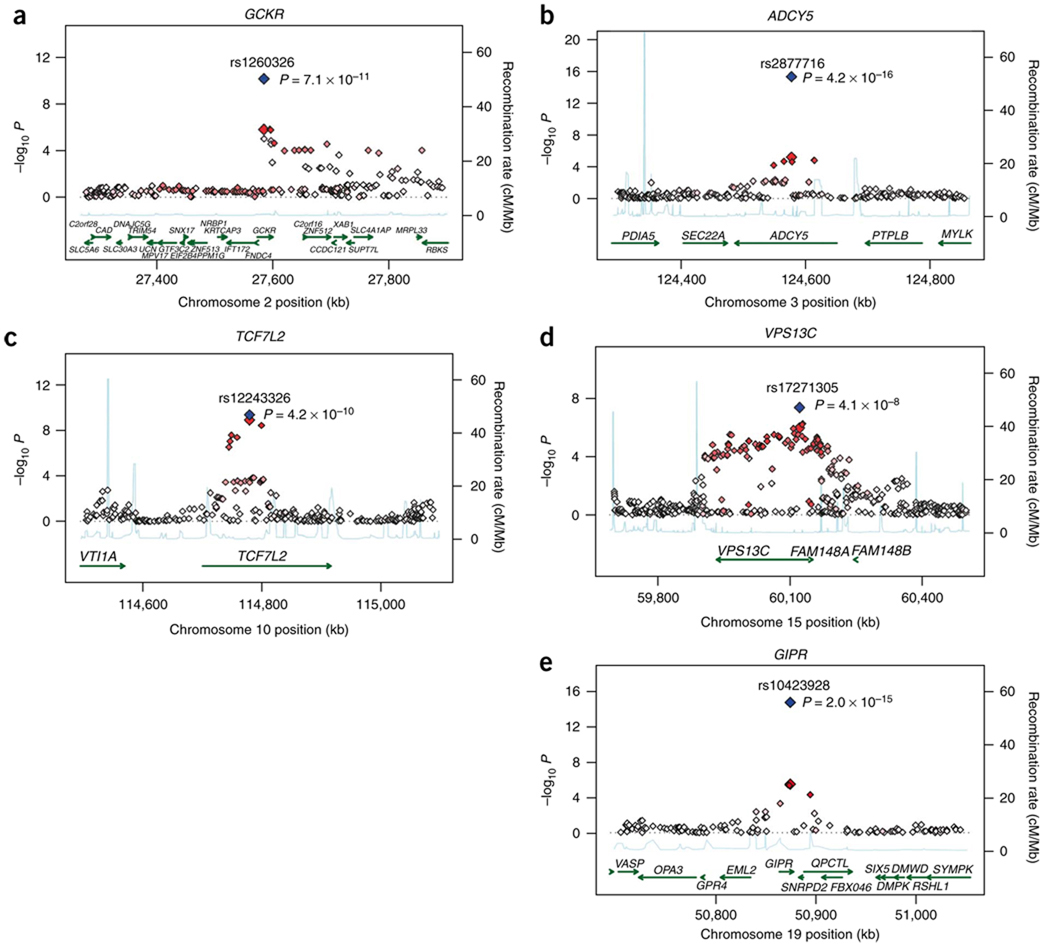
A meta-analysis combining 9 discovery GWAS (n = 15,234) and replication stages with up to 29 SNPs in 17 studies comprising up to 30,620 individuals of European descent revealed 5 loci associated with 2-h glucose at genome-wide significance (P = 5 × 10−8; see Online Methods, Table 1, Fig. 1, Supplementary Fig. 1 and Supplementary Tables 1 and 2). Three loci were newly associated with 2-h glucose in an analysis adjusted for age, sex, BMI and study-specific covariates: GIPR (gastric inhibitory polypeptide receptor, rs10423928, β (s.e.m.) = 0.09 (0.01) mmol/l per A allele, P = 2.0 × 10−15), VPS13C (vacuolar protein sorting 13 homolog C, rs17271305, β (s.e.m.) = 0.06 (0.01) mmol/l per G allele, P = 4.1 × 10−8) and ADCY5 (adenylate cyclase, 5 rs2877716, β (s.e.m.) = 0.09 (0.01) mmol/l per C allele, P = 4.2 × 10−16). The ADCY5 locus was also identified by an accompanying study reporting meta-analysis in MAGIC for fasting glucose levels (r2 = 0.82 to the most significant fasting glucose SNP rs11708067)6. The remaining loci identified here included the previously published fasting glucose–associated gene GCKR (glucokinase (hexokinase 4) regulator, missense SNP rs1260326, P = 7.1 × 10−11)11 and the established T2D-associated gene TCF7L2 (transcription factor 7-like 2, rs12243326 with r2 = 0.79 to most significant T2D SNP rs7903146, P = 4.2 × 10−10)12.
Table 1.
Genome-wide significant loci for 2-h glucose during an OGTT from 26 studies in nondiabetic individuals
| Discovery | Replication | Discovery and replication | Discovery and replication (FG adj) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SNP | Chr | Position (bp) |
Nearest gene |
Alleles (+/−) |
Freq (+)1 |
Effect (s.e.m.) mmol/l |
P value | Effect (s.e.m.) mmol/l |
P value | Effect (s.e.m.) mmol/l |
P value |
P value (no BMI) |
Effect (s.e.m.) mmol/l |
P value |
P value (no BMI) |
| rs1260326 | 2 | 27584444 | GCKR | T/C | 0.40 | 0.09 (0.02) | 1.53 × 10−6 | 0.06 (0.01) | 5.33 × 10−6 | 0.07 (0.01) | 7.05 × 10−11 | 3.00 × 10−10 | 0.10 (0.01) | 9.23 × 10−21 | 2.26 × 10−21 |
| rs2877716 | 3 | 124577141 | ADCY5 | C/T | 0.77 | 0.10 (0.02) | 6.26 × 10−6 | 0.09 (0.01) | 1.21 × 10−11 | 0.09 (0.01) | 4.19 × 10−16 | 7.41 × 10−16 | 0.07 (0.01) | 1.68 × 10−11 | 7.98 × 10−12 |
| rs12243326 | 10 | 114778805 | TCF7L2 | C/T | 0.21 | 0.13 (0.02) | 1.20 × 10−9 | 0.05 (0.02) | 1.27 × 10−3 | 0.08 (0.01) | 4.23 × 10−10 | 1.12 × 10−7 | 0.07 (0.01) | 9.99 × 10−9 | 1.17 × 10−10 |
| rs17271305 | 15 | 60120272 | VPS13C | G/A | 0.42 | 0.09 (0.02) | 1.04 × 10−6 | 0.05 (0.02) | 1.58 × 10−3 | 0.06 (0.01) | 4.11 × 10−8 | 1.30 × 10−7 | 0.07 (0.01) | 4.33 × 10−11 | 8.41 × 10−11 |
| rs10423928 | 19 | 50874144 | GIPR | A/T | 0.18 | 0.15 (0.03) | 3.33 × 10−6 | 0.09 (0.01) | 2.30 × 10−11 | 0.09 (0.01) | 1.98 × 10−15 | 3.20 × 10−12 | 0.11 (0.01) | 2.56 × 10−20 | 5.94 × 10−18 |
| n11,268–15,234 | 15,103–30,121 | 30,337–43,104 | 30,114–42,354 | ||||||||||||
Results from fixed effects, inverse variance meta-analysis of 9 GWA (ARIC, BLSA, CHSstage1&2, CoLaus, DGI, Fenland, FHS, FUSION, Sorbs) and 17 follow-up studies (Amish, BotniaPPP, CHSstage3, DIAGEN, ELY, FrenchFamilyMembers, FrenchHaguenau, FrenchObeseAdults, FUSIONstage2, Hertfordshire, Inter99, METSIM, NHANES, RISC, Roche, ULSAM, Whitehall II) with adjustment for age, sex and BMI. Position based on hg18, NCBI build36. Combined discovery and replication P values for 2-h glucose adjusted for age and sex (no BMI), and further adjusted for fasting glucose are also presented. Replication meta-analysis results and joint discovery and replication meta-analysis results include proxy SNPs with r2 > 0.8 in HapMap CEU.
Allele frequencies based on HapMap phase II CEU sample. FG adj, adjusted for fasting glucose in addition to age, sex, BMI and study-specific covariates (center).
Figure 1.
Regional plots of five genome-wide significant associations for 2 hour glucose based on 2 hour glucose discovery analysis adjusted for age, sex, BMI and study-specific covariates. (a–e) For each of the GCKR (a), ADCY5 (b), TCF7L2 (c), VPS13C (d) and GIPR (e) regions, directly genotyped and imputed SNPs are plotted with their meta-analysis P values (as −log10 values) as a function of genomic position (NCBI Build 36; hg 18). In each panel, the SNP taken forward for replication (large red diamond) and joint discovery and replication P value (blue diamond) are shown. Estimated recombination rates (HapMap) are plotted to reflect the local linkage disequilibrium structure around the associated SNPs and their correlated proxies (0 < r2 < 1, represented on a white to red scale, based on pairwise r2 values from HapMap CEU). Gene annotations were taken from the UCSC genome browser.
To determine whether these associations reflected differences in fasting glucose levels or whether they primarily influenced the incremental response to a glucose challenge, we repeated our association analysis including fasting glucose as a covariate (Table 1 and Supplementary Table 2). Adjusting for fasting glucose resulted in increased effect size for the GCKR, GIPR and VPS13C loci and supported their specific role in post-challenge glucose regulation. In contrast, adjusting for fasting glucose slightly decreased the effect for the ADCY5 and TCF7L2 loci, which suggested that the risk alleles in both genes increase glucose levels both in the fasting and post-challenge state.
In meta-analyses available from MAGIC6, fasting glycemic traits variants at the GIPR, VPS13C and ADCY5 loci were not associated with fasting insulin or insulin resistance as measured by homeostasis model assessment13, which may reflect the inadequacy of the crude measures used here or may reflect a lack of power to detect small effects (Supplementary Table 3). Associations of risk alleles in GCKR and TCF7L2 with fasting glycemic traits have been reported previously6. In a large Swedish meta-analysis (n = 27,628), the GIPR rs10423928 2-h glucose–raising allele was significantly associated with lower BMI (Pmeta = 7.5 × 10−5, V.L. and L.G., unpublished data).
GIP is one of the two incretin hormones that stimulate insulin response after an oral glucose challenge. It has been shown that the incretin effect is impaired in individuals with T2D14; specifically, in individuals with T2D, stimulated GIP secretion appears normal and their insulinotropic response to GIP is reduced15. GIPR is therefore a biologically plausible candidate for mediating insulin secretion after oral glucose challenge. We tested associations of GIPR variants with indices of oral glucose–stimulated insulin secretion in up to 13 studies with samples measured at multiple times during the OGTT (Table 2 and Supplementary Table 4). The rs10423928 A allele associated with increased 2-h glucose was also associated with lower insulinogenic index (β (s.e.m.) = −0.08 (0.01) µU/mmol, P = 1.0 × 10−17), which represents a reduction in the early phase of insulin secretion16. The rs10423928 A allele was also associated with a lower ratio of insulin to glucose area under the curve (AUC ins/gluc, β (s.e.m.) = −0.05 (0.01) pmol/mmol, P = 1.3 × 10−16), which is an integrated measure of insulin response over the 2-h OGTT16. Furthermore, the rs10423928 A allele was associated with lower 2-h insulin level (adjusted for 2-h glucose, β (s.e.m.) = −0.04 (0.01) pmol/l, P = 2.0 × 10−13).
Table 2.
Effect of ADCY5, VPS13C and GIPR variants on indices of insulin response during an OGTT
| Insulinogenic index | AUCins/gluc | 2-h insulin, adjusted for 2-h glucose | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SNP | Chr | Nearest gene |
Effect allele |
n | Effect (s.e.m.) µU/mmol (BMI-adj) |
P value (BMI-adj) |
P value | n | Effect (s.e.m.) pmol/mmol (BMI-adj) |
P value (BMI-adj) |
P value | n | Effect (s.e.m.) pmol/l (BMI-adj) |
P value (BMI-adj) |
P value |
| rs2877716 | 3 | ADCY5 | C | 19,461 | −0.011 (0.009) | 0.23 | 0.22 | 20,435 | –0.010 (0.007) | 0.16 | 0.18 | 30,987 | −0.029 (0.006) | 1.43 × 10−6 | 3.09 × 10−6 |
| rs17271305 | 15 | VPS13C | G | 13,911 | 0.024 (0.010) | 0.01 | 0.02 | 13,666 | –0.001 (0.007) | 0.86 | 0.76 | 23,842 | −0.037 (0.006) | 7.45 × 10−11 | 2.58 × 10−10 |
| rs10423928 | 19 | GIPR | A | 22,529 | −0.076 (0.009) | 1.00 × 10−17 | 2.44 × 10−20 | 22,209 | −0.051 (0.007) | 9.50 × 10−17 | 3.39 × 10−20 | 32,204 | –0.044 (0.006) | 1.99 × 10−13 | 3.67 × 10−16 |
AUCins/gluc, area under the curve for insulin divided by area under the curve for glucose.
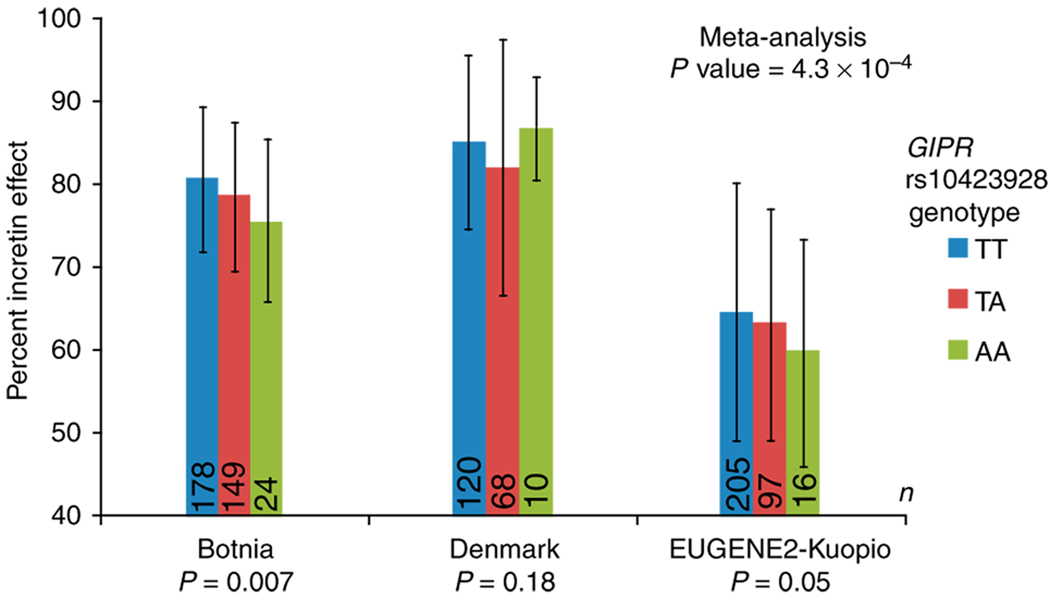
Because GIP is involved in the insulin response specific to an oral glucose challenge, GIPR variation was not expected to influence the insulin response to an intravenous glucose load. We tested the insulin response in 1,509 nondiabetic participants from four studies who underwent an intravenous glucose tolerance test (IVGTT). No association was observed with measures of acute insulin response (AIR) from the IVGTT (P = 0.12; Supplementary Table 5), even though the study had >97% power to detect an effect explaining 1% trait variance (α = 0.05). We also derived an estimate of the incretin effect by comparing the insulin response to oral versus intravenous glucose administered to the same 804 nondiabetic individuals from the Botnia17, Denmark and EUGENE2-Kuopio studies18. Individuals carrying the A risk allele of rs10423928 in GIPR showed a significantly lower incretin effect (β (s.e.m.) = −0.012 (0.004), P = 4.3 × 10−4; Fig. 2 and Supplementary Table 5). Our results are consistent with animal studies, in which mice with targeted deletion of Gipr showed mild glucose intolerance and reduced insulin secretion in response to an oral glucose challenge but showed normal fasting glucose and normal insulin secretion in response to an intraperitoneal glucose challenge19.
Figure 2.
Percent incretin effect in the Botnia, Denmark and EUGENE2-Kuopio studies of nondiabetic individuals (n = 804) by GIPR rs10423928 genotype. Mean and s.d. for each study are displayed by genotype (see Supplementary Table 5 for details). Incretin effect was adjusted for age, sex and BMI and study-specific covariates.
The variant in GIPR most significantly associated with 2-h glucose (rs10423928) is an intronic SNP with no known function based on FastSNP (see URL section). Notably, rs10423928 is in strong linkage disequilibrium (r2 = 0.93) with a missense mutation (at rs1800437, resulting in the substitution E354Q). Some groups have explored the E354Q substitution as a candidate for association with T2D. One study showed that people homozygous for the Gln354-encoding allele of this gene had lower fasting and post oral-load C-peptide levels, suggesting a role for GIPR in insulin secretion20; this is in line with our observations. In small T2D case-control studies, no association has been observed at GIPR20–22. We performed a meta-analysis of 16 T2D association studies (n = 19,091 diabetic individuals (cases), 38,508 nondiabetic individuals) and found that the rs10423928 A allele was moderately associated with increased risk of T2D (OR = 1.07, 95% CI 1.03–1.12; P = 1.8 × 10−4; Table 3 and Supplementary Table 6). This result, although suggestive of association, highlights the challenge of genetic approaches to complex diseases, whereby important genes involved in pathophysiology might be difficult to identify even in large case-control collections due to small individual odds ratios23.
Table 3.
Meta-analysis of T2D association studies for SNPs at previously unknown 2-h glucose–associated loci
| T2D fixed effects | T2D random effects | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SNP | Chr | Nearest gene | Effect allele | n studies | n cases | n controls | OR (95% CI) | P value | I2 (%) | OR (95% CI) | P value |
| rs2877716 | 3 | ADCY5 | c | 25 | 35,869 | 89,798 | 1.12 (1.09–1.15) | 4.8 × 10−18 | 35.2 (0–59.3) | 1.12 (1.08–1.16) | 9.4 × 10−11 |
| rs17271305 | 15 | VPS13C | g | 13 | 15,180 | 32,556 | 0.97 (0.94–1.00) | 0.083 | 48.7 (0–72.8) | 0.99 (0.94–1.04) | 0.62 |
| rs10423928 | 19 | GIPR | a | 16 | 19,091 | 38,508 | 1.07 (1.03–1.12) | 1.8 × 10−4 | 39.3 (0–60.3) | 1.07 (1.02–1.12) | 9.6 × 10−3 |
Proxies rs11708067 with r2 = 0.82 in HM CEU to rs2877716 used in eight studies; rs11717195 with r2 = 0.95 in HM CEU used in two studies. Proxy rs12913951 with r2 = 0.71 in HM CEU to rs17271305 used in two studies.
Proxy rs11672660 with r2 = 0.95 in HM CEU to rs10423928 used in three studies.
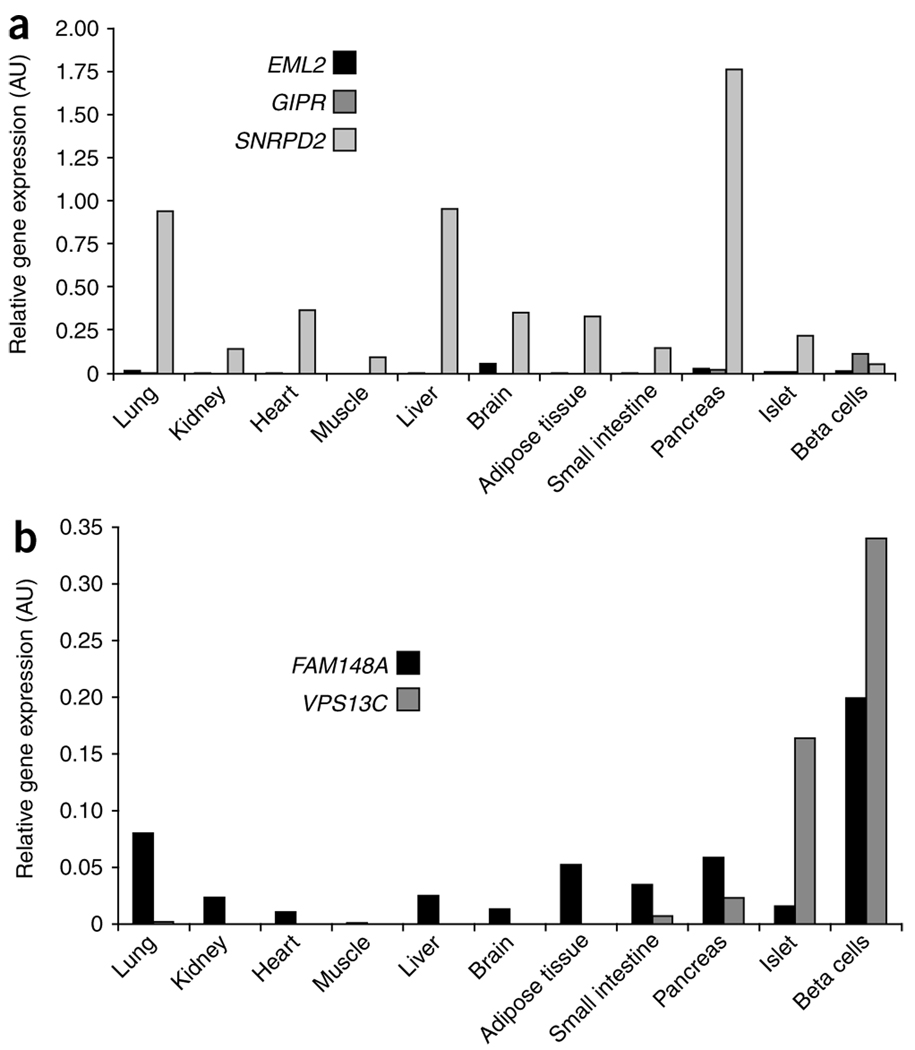
We assessed the mRNA expression patterns of GIPR and the nearest upstream (EML2) and downstream (SNRPD2) genes in a human tissue panel (Fig. 3). All three genes were expressed in the pancreas, but only GIPR had strong specific mRNA expression in the sorted pancreatic beta cells, supporting the implication of GIPR in insulin secretion. No significant difference in GIPR, EML2 or SNRPD2 mRNA expression in pancreatic islets was seen based on the rs10423928 genotype (for GIPR P = 0.76, n = 19; Supplementary Note).
Figure 3.
mRNA expression in human tissues of the genes located in the GIPR (a) and VPS13C (b) regions. Expression data is relative expression levels measured by quantitative RT-PCR. All samples were run in triplicate and normalized to the GAPDH relative expression level. AU, arbitrary units.
As adenylate cyclases have been implicated in the cAMP pathway of GLP-1 and GIP-induced insulin release by beta cells24,25, we also tested for association of the most significant ADCY5 variant with measures of insulin response and risk of T2D. The 2-h glucose-raising C allele of rs2877716 was associated with lower 2-h insulin (P = 1.4 × 10−6) but was not associated with AUCins/gluc (P = 0.16) or with the insulinogenic index (P = 0.23; Table 2 and Supplementary Table 4). The lack of association with the two latter indices suggests that ACDY5 is unlikely to be directly involved in insulin secretion in response to an oral glucose challenge and may not operate in the same pathway as GIPR. In support of our observations, the mRNA expression pattern of ADCY5 reported in the recent MAGIC study on fasting glucose traits6 shows that ADCY5 is most highly expressed in heart and brain tissues, with weaker expression in the pancreas, islets and sorted beta cells. Finally, we found that the rs2877716 C allele was also associated with increased risk of T2D (OR = 1.12, 95% CI 1.09–1.15, P = 4.8 × 10−18) in a separate meta-analysis of 25 association studies (total n = 35,869 cases, 89,798 controls; Table 3 and Supplementary Table 6) and was associated with increased risk of developing future T2D in 16,061 individuals from the Malmo Preventive Project (OR = 1.19, 95% CI 1.10–1.29, P = 3.13 × 10−5; see Supplementary Note). Taken together, our results do not support a role for ADCY5 in early insulin secretion in response to an oral glucose load, but it remains to be determined how it (or another causal gene at the locus) contributes to risk for T2D.
We tested association of the VPS13C variant with insulin secretion indices because of its novelty and unknown function (Table 2 and Supplementary Table 4). The risk allele G of rs17271305 associated with higher 2-h glucose was also associated with lower 2-h insulin (P = 7.5 × 10−11). rs17271305 showed no association with AUCins/gluc (P = 0.86) but was nominally associated with insulinogenic index (P = 0.01). The VPS13C variant was not associated with T2D (OR = 0.97, 95% CI 0.94–1.00, P = 0.08) (Table 3 and Supplementary Table 6), suggesting that it may contribute to normal variation in 2-h glucose but not susceptibility to T2D. Investigation of the mRNA expression profiles of VPS13C revealed the presence of transcripts in several organs including brain, adipose tissue, liver, pancreas, and, most strongly, in sorted beta cells (Fig. 3). Analysis of the neighboring gene FAM148A indicated a pancreatic tissue-specific mRNA expression profile, mainly in beta cells (Fig. 3); however, its expression was not altered by VPS13C genotype in pancreatic islets (P = 0.9, n = 19; Supplementary Note).
VPS13C spans 208 kb on chromosome 15 and encodes a protein homolog of the yeast vacuolar protein sorting 13. This family of proteins is involved in trafficking of membrane proteins between the trans-Golgi network and the prevacuolar compartment26. rs17271305, identified by the 2-h glucose meta-analysis, is 101 kb from the FAM148B association signal (rs11071657) identified by the MAGIC fasting glucose meta-analysis6, but could represent an independent signal, as rs17271305 is weakly correlated with rs11071657 (r2 = 0.28 in HapMap CEU, P2-h glucose = 0.002). Detailed fine-mapping and functional analyses will be needed to definitively establish the causal gene and variant(s) at this locus.
In conclusion, we report a GWAS for glucose levels 2 h after an oral glucose challenge, and we have investigated the role of newly discovered 2-h glucose variants in influencing normal physiology and potentially influencing risk of T2D. We identified five loci associated with 2-h glucose, in GIPR, VPS13C, ADCY5, GCKR and TCF7L2. As the physiological roles of GCKR and TCF7L2 variants have been examined in detail previously17,27, we focused on the three newly identified associated loci. ADCY5 variants are associated with fasting6 and 2-h glucose levels and with an increased risk of T2D, highlighting the fact that investigation of diabetes-related quantitative traits can lead to identification of additional T2D-associated loci. VPS13C variants may contribute to normal variation in 2-h glucose, but their effect on T2D pathogenesis is unclear.
Our association results suggest a role for GIPR in the incretin effect and in early pathophysiologic pathways that could lead to impaired glucose tolerance and T2D in humans. Previously, it was hypothesized that patients with T2D might express a smaller amount of GIPR or defective GIPR28. Meier et al. observed that individuals with T2D and a subgroup of the first-degree relatives of these individuals had a blunted insulin response to GIP, supporting the hypothesis that a defect of the GIPR could be part of the T2D pathophysiology29. Future studies should examine how GIPR variants may modify response to treatments targeting the enteroinsular axis.
Methods
Methods and any associated references are available in the online version of the paper at http://www.nature.com/naturegenetics/.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank the many colleagues who contributed to collection and phenotypic characterization of the clinical samples, as well as genotyping and analysis of the GWA data. We gratefully acknowledge those who agreed to participate in these studies. A full list of acknowledgments and funding support for each study is described in the Supplementary Note.
Footnotes
Note: Supplementary information is available on the Nature Genetics website.
AUTHOR CONTRIBUTIONS
Writing group: R. Saxena, M.-F.H., C. Langenberg., T. Tanaka, J.S.P., P.V., V.L., N.B.-N., J.C.F., M.I.M., M.B., I.B., R. Sladek, P.F., J.B.M., L.G., N.J.W., R.M.W.
Project design, management and coordination: (Amish) B.D.M., A.R.S.; (ARIC) J.S.P., W.H.L.K., S.J. Bielinski, E. Boerwinkle; (BLSA) A. Singleton, L.F.; (BotniaPPP) L.G., T. Tuomi., B.I.; (CHS) N.L.G., K.R., N.L.S., B.M.P., J.I.R.; (Colaus) P.V., M.F., V. Mayor, G.W., D.M.W., V. Mooser; (Danish) K.B.J., A.S., T. Jørgensen, T.L., T.H., O.P.; (DIAGEN) P. Schwartz, S.R.B.; (DGI) R. Saxena, D.A., L.G.; (Ely) C. Langenberg, N.J.W.; (Fenland) C. Langenberg, N.G.F., R.J.F.L., N.J.W.; (FHS) J.D., J.B.M.; (French) N.B.-N., P.F.; (FUSION) R.N.B., F.S.C., K.L.M., L.J.S., J. Tuomilehto, M.B., R.M.W.; (Hertfordshire) A.A.S., H.S., C.C.; (METSIM) J.K., M.La.; (MPP) P.N.; (Partners/Roche) J.B.M., D.M.N., G.H.W.; (RISC) M.W., L.P.; (Sorbs) A.T., M.S.; (ULSAM) E.I.; (Whitehall II) E. Brunner, A.H., M. Kivimaki, M. Kumari, M.M.
Sample collection and phenotyping: (Amish) A.R.S.; (BLSA) J.M.E.; (BotniaPPP) L.G., V.L., B.I., T. Tuomi; (CHS) B.M.P., D.S.S, N.L.S.; (CoLaus) P.V., G.W.; (Danish) T.W.B., K.B.J, A.S., T. Jørgensen, T.L., T.H., O.P.; (DIAGEN) J.G., P. Schwartz; (DGI) L.G., V.L., B.I., T. Tuomi; (Ely) N.J.W.; (Fenland) N.G.F., R.J.F.L., N.J.W.; (French) P.F., D.M., B.B., C.L.-M., G.C., F. Pattou; (FHS) J.B.M., C.S.F.; (FUSION) R.N.B., T.A.B., J. Tuomilehto, T.T.V.; (Hertfordshire) A.A.S., H.S., C.C.; (METSIM) J.K., M. Laakso; (Partners/Roche) J.B.M., D.M.N., G.H.W.; (Sorbs) P.K., A.T.; (Whitehall II) E. Brunner, M. Kumari, M.M.
Genotyping: (Amish) R.P.; (ARIC) E. Boerwinkle.; (BLSA) A. Singleton; (BotniaPPP) G.J.C.; (CHS) Y.-D.I.C., M.O.G., J.I.R.; (CoLaus) V. Mooser, D.M.W.; (Danish) T.H., T.S., C.H.A., N.G., O.P.; (DGI) D.A., V.L., R. Saxena; (DIAGEN) D.P., A.J.S.; (Ely) I.B., S.J. Bumpstead, F. Payne, N.J.W.; (Fenland) R.J.F.L., N.J.W.; (FHS) J.C.F., J.B.M.; (French) N.B.-N., J.D., R. Sladek, D.M., A.W.; (FUSION) L.L.B., M.R.E., P.S.C.; (FUSION stage 2) P.S.C., A.J.S.; (Hertfordshire) I.B., S.J. Bumpstead, F. Payne, N.J.W.; (METSIM) M.A.M., N.N.; (Partners/Roche) J.C.F., J.B.M.; (Sorbs) Y.B., P.K., K.K.; (ULSAM) A.-C.S.; (Whitehall II) M. Kumari, C. Langenberg, N.J.W.
Statistical analysis: (Meta-analyses) R. Saxena, J.D., D.R., W.H.L.K., A.U.J.; (Amish) J.O.; (ARIC) W.H.L.K., M.L., A.K., D.J.C.; (BLSA) T. Tanaka; (BotniaPPP) V.L.; (CHS) N.L.G., K.R.; (CoLaus) T. Johnson, K. Song; (Danish) T.S., C.H.A., T.W.B., N.G.; (DGI) R. Saxena; (Ely) C. Langenberg, S.J.S.; (Fenland) C. Langenberg, J.L., J.H.Z.; (French) N.-B.N, C. Lecoeur, C.C-P., A.B., C.D.; (FHS) J.D., A.K.M., D.R., P. Shrader; (FUSION) A.U.J., H.M.S.; (FUSION stage 2) A.U.J., H.M.S.; (Hertfordshire) C. Langenberg, S.J.S.; (Partners/Roche) P.Shr.; (RISC) C. Langenberg, S.J.S.; (Sorbs) I.P.; (ULSAM) E.I.; (Whitehall II) C. Langenberg.
Expression analysis: (Malmo) J. Taneera, V.L., L.G; (French) N.B.-N., O.L.B., F. Patou, P.F.
Type 2 Diabetes association: (DGI) D.A., L.G., R. Saxena, B.F.V., K.A.; (deCODE) V.S., G.T., U.T., K. Stefansson; (EUROSPAN) Y.S.A., J.F.W., M.v.H., E.S., C.v.D.; (French) N.B.-N., J. Deplanque, C. Lecoeur, G.C., P.F.; (Addition-Ely) C. Langenberg, F. Payne, S.J. Bumpstead, I.B., N.J.W.; (Norfolk Diabetes Case-Control Study) C. Langenberg, F. Payne, S.J. Bumpstead, I.B., M.S., N.J.W.; (Cambridgeshire Case-Control Study) C. Langenberg, F. Payne, S.J. Bumpstead, I.B., N.J.W.; (KORA) H.G., W.R., T.I., H.E.W.; (MPP) P.N., V.L., L.G.; (NHS/HPFS) F.B.H. L.Q., M.C.C.; (UKT2D/58BC/OXGN) A.D., C.N.A.P., A.T.H., A.D.M.; T.M.F., M.I.M.; (WTCCC-UKT2D) M.N.W., E.Z.
COMPETING INTERESTS STATEMENT
The authors declare competing financial interests: details accompany the full-text HTML version of the paper at http://www.nature.com/naturegenetics/.
Reprints and permissions information is available online at http://npg.nature.com/reprintsandpermissions/.
Full membership list of the GIANT consortium is provided in the Supplementary Note.
References
- 1.Prokopenko I, McCarthy MI, Lindgren CM. Type 2 diabetes: new genes, new understanding. Trends Genet. 2008;24:613–621. doi: 10.1016/j.tig.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bouatia-Naji N, et al. A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk. Nat. Genet. 2009;41:89–94. doi: 10.1038/ng.277. [DOI] [PubMed] [Google Scholar]
- 3.Bouatia-Naji N, et al. A polymorphism within the G6PC2 gene is associated with fasting plasma glucose levels. Science. 2008;320:1085–1088. doi: 10.1126/science.1156849. [DOI] [PubMed] [Google Scholar]
- 4.Chen WM, et al. Variations in the G6PC2/ABCB11 genomic region are associated with fasting glucose levels. J. Clin. Invest. 2008;118:2620–2628. doi: 10.1172/JCI34566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prokopenko I, et al. Variants in MTNR1B influence fasting glucose levels. Nat. Genet. 2009;41:77–81. doi: 10.1038/ng.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dupuis J, et al. Novel genetic loci implicated in fasting glucose homeostasis and their impact on related metabolic traits. Nat. Genet. 2010 January 17; doi: 10.1038/ng.520. advance online publication, doi:10.1038/ng.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ceriello A, et al. Postprandial glucose regulation and diabetic complications. Arch. Intern. Med. 2004;164:2090–2095. doi: 10.1001/archinte.164.19.2090. [DOI] [PubMed] [Google Scholar]
- 8.Qiao Q, Tuomilehto J, Borch-Johnsen K. Post-challenge hyperglycaemia is associated with premature death and macrovascular complications. Diabetologia. 2003;46 Suppl 1:M17–M21. doi: 10.1007/s00125-002-0932-4. [DOI] [PubMed] [Google Scholar]
- 9.Meigs JB, Nathan DM, D’Agostino RB, Sr, Wilson PW. Fasting and postchallenge glycemia and cardiovascular disease risk: the Framingham Offspring Study. Diabetes Care. 2002;25:1845–1850. doi: 10.2337/diacare.25.10.1845. [DOI] [PubMed] [Google Scholar]
- 10.Schousboe K, et al. Twin study of genetic and environmental influences on glucose tolerance and indices of insulin sensitivity and secretion. Diabetologia. 2003;46:1276–1283. doi: 10.1007/s00125-003-1165-x. [DOI] [PubMed] [Google Scholar]
- 11.Orho-Melander M, et al. Common missense variant in the glucokinase regulatory protein gene is associated with increased plasma triglyceride and C-reactive protein but lower fasting glucose concentrations. Diabetes. 2008;57:3112–3121. doi: 10.2337/db08-0516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grant SF, et al. Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat. Genet. 2006;38:320–323. doi: 10.1038/ng1732. [DOI] [PubMed] [Google Scholar]
- 13.Matthews DR, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 14.Gautier JF, Choukem SP, Girard J. Physiology of incretins (GIP and GLP-1) and abnormalities in type 2 diabetes. Diabetes Metab. 2008;34 Suppl 2:S65–S72. doi: 10.1016/S1262-3636(08)73397-4. [DOI] [PubMed] [Google Scholar]
- 15.Nauck MA, et al. Incretin effects of increasing glucose loads in man calculated from venous insulin and C-peptide responses. J. Clin. Endocrinol. Metab. 1986;63:492–498. doi: 10.1210/jcem-63-2-492. [DOI] [PubMed] [Google Scholar]
- 16.Ahren B, Pacini G. Importance of quantifying insulin secretion in relation to insulin sensitivity to accurately assess beta cell function in clinical studies. Eur. J. Endocrinol. 2004;150:97–104. doi: 10.1530/eje.0.1500097. [DOI] [PubMed] [Google Scholar]
- 17.Lyssenko V, et al. Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J. Clin. Invest. 2007;117:2155–2163. doi: 10.1172/JCI30706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Laakso M, et al. Insulin sensitivity, insulin release and glucagon-like peptide-1 levels in persons with impaired fasting glucose and/or impaired glucose tolerance in the EUGENE2 study. Diabetologia. 2008;51:502–511. doi: 10.1007/s00125-007-0899-2. [DOI] [PubMed] [Google Scholar]
- 19.Miyawaki K, et al. Glucose intolerance caused by a defect in the entero-insular axis: a study in gastric inhibitory polypeptide receptor knockout mice. Proc. Natl. Acad. Sci. USA. 1999;96:14843–14847. doi: 10.1073/pnas.96.26.14843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Almind K, et al. Discovery of amino acid variants in the human glucose-dependent insulinotropic polypeptide (GIP) receptor: the impact on the pancreatic beta cell responses and functional expression studies in Chinese hamster fibroblast cells. Diabetologia. 1998;41:1194–1198. doi: 10.1007/s001250051051. [DOI] [PubMed] [Google Scholar]
- 21.Kubota A, et al. Identification of two missense mutations in the GIP receptor gene: a functional study and association analysis with NIDDM: no evidence of association with Japanese NIDDM subjects. Diabetes. 1996;45:1701–1705. doi: 10.2337/diab.45.12.1701. [DOI] [PubMed] [Google Scholar]
- 22.Nitz I, et al. Association analyses of GIP and GIPR polymorphisms with traits of the metabolic syndrome. Mol. Nutr. Food Res. 2007;51:1046–1052. doi: 10.1002/mnfr.200700048. [DOI] [PubMed] [Google Scholar]
- 23.Hardy J, Singleton A. Genomewide association studies and human disease. N. Engl. J. Med. 2009;360:1759–1768. doi: 10.1056/NEJMra0808700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drucker DJ. The role of gut hormones in glucose homeostasis. J. Clin. Invest. 2007;117:24–32. doi: 10.1172/JCI30076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leech CA, Castonguay MA, Habener JF. Expression of adenylyl cyclase subtypes in pancreatic beta-cells. Biochem. Biophys. Res. Commun. 1999;254:703–706. doi: 10.1006/bbrc.1998.9906. [DOI] [PubMed] [Google Scholar]
- 26.Velayos-Baeza A, Vettori A, Copley RR, Dobson-Stone C, Monaco AP. Analysis of the human VPS13 gene family. Genomics. 2004;84:536–549. doi: 10.1016/j.ygeno.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 27.Sparso T, et al. The GCKR rs780094 polymorphism is associated with elevated fasting serum triacylglycerol, reduced fasting and OGTT-related insulinaemia, and reduced risk of type 2 diabetes. Diabetologia. 2008;51:70–75. doi: 10.1007/s00125-007-0865-z. [DOI] [PubMed] [Google Scholar]
- 28.Holst JJ, Gromada J, Nauck MA. The pathogenesis of NIDDM involves a defective expression of the GIP receptor. Diabetologia. 1997;40:984–986. doi: 10.1007/s001250050779. [DOI] [PubMed] [Google Scholar]
- 29.Meier JJ, et al. Reduced insulinotropic effect of gastric inhibitory polypeptide in first-degree relatives of patients with type 2 diabetes. Diabetes. 2001;50:2497–2504. doi: 10.2337/diabetes.50.11.2497. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.