Abstract
Introduction. Disease management modules (DMM), including education, tracking, support, and medical care, have improved health for patients with asthma and diabetes. For rural patients, novel ways of delivery are needed to access clinical expertise from urban or academic specialists. Telemedicine (telephone and televideo) could be instrumental in this process, though no randomized, controlled trials have assessed their effectiveness.
Methods. Self-report and structured psychiatric interviews were used to screen potential depressed subjects. Subjects were randomized to: 1) usual care with a DMM using telephone and self-report questionnaires; or 2) a DMM using telephone, questionnaires, and monthly televideo psychiatric consultation emphasizing primary care physician (PCP) skill development. Subjects' depressive symptoms, health status, and satisfaction with care were tabulated at three, six, and 12 months after study entry.
Results. There was significant clinical improvement for depression in both groups, with a trend toward significance in the more intensive module. Satisfaction and retention was superior in the more intensive group. There was no overall change in health functioning in either group.
Conclusions. Intensive modules using telepsychiatric educational interventions toward PCPs may be superior, but the most critical ingredient may be administrative tracking of patients, prompted intervention by PCPs, and (when necessary) new ideas by a specialist.
Keywords: telemedicine, rural, primary care, depression
Introduction
Primary care medicine is crucial to mental healthcare delivery in the United States, serving as the main point of contact for over half of those suffering from mental disorders.1 In rural areas, where approximately 25 percent of the US population lives, local agencies report an even greater problem with access to specialists than their urban counterparts.2 This lack of mental health services leads to poor outcomes, such as higher rates of homicide and suicide, as well as increased use of emergency services, hospitalizations, and placement in mental health institutions.3,4 Primary care providers (PCPs) in rural areas also report having inadequate skills to manage these mental health issues, and they would benefit from assistance.5 However, rural areas inherently have provider shortages, particularly with regard to consultation-liaison psychiatrists.
Health providers use a number of psychiatric, health service, and disease management models to reach primary care patients, predominantly in suburban and urban locales. Psychiatric consultation-liaison models include the traditional referral, the consultation care, and the collaborative care models.6,7 Variations on these models also include use of mental health extenders and a stepped care to judiciously use scarce psychiatric resources.8 Quality improvement programs also improve treatment rates and outcomes for depressed patients with comorbid medical illness in primary care and are cost-effective too.9 Chronic disease management for depression is now being implemented subsequent to modules developed for asthma and diabetes.
Telemedicine technology is one strategy to improve the accessibility of mental healthcare, particularly to areas underserved by physicians.10 Telecommunications technology has been used to link specialists at academic health centers with healthcare professionals in rural areas for the management of patients.11,12 The initial application of telemedicine to psychiatry was videoconferencing. However, telephone and computer-based (e.g., e-mail) interventions allowed PCPs to gain ready access to specialists in order to enhance the quality of local care for patients.13,14 Early research shows that patients whose PCPs received feedback plus care management had a higher likelihood of receiving adequate doses of antidepressants and greater improvement in the management of depression.15
The goal of this study was to compare two modules for helping primary care physicians and staff intervene for patients with depression: 1) usual care with a DMM using telephone and self-report questionnaires; or 2) usual care with an intensive DMM (IDMM) using telephone, questionnaires, and repeated televideo psychiatric consultation coupled with training of the PCP. We hypothesize that subjects with the more intensive module will have significantly decreased depressive symptoms, significantly better health functioning, and higher satisfaction at three, six, and 12 months after study entry (primary outcome measures). In addition, study retention will be higher and comorbid symptoms (e.g., anxiety) will be reduced in the intensive patients compared to other patients (secondary outcome measures).
Methods
Overview. A total of 121 subjects were recruited from rural primary care sites over a 24-month period. Subjects were English-speaking men and women, between ages of 18 and 80 years, who were willing to take an antidepressant medication. PCPs referred subjects with suspected depression for screening. Subjects completed self-report questionnaires and a structured diagnostic interview (i.e., mood and psychotic sections of the Structured Clinical Interview for DSM-IV [SCID-I, research version])15 to confirm depression. They received $10 for screening and each follow-up assessment at three, six, and 12 months after study entry. Subjects with major depression were randomized by the study team to: 1) usual care with a DMM using telephone and self-report questionnaires; or 2) usual care with an IDMM using telephone, questionnaires, and repeated televideo psychiatric consultation coupled with training of the PCP. The groups were compared at three, six, and 12 months after study entry in terms of depressive symptoms, health functioning, and satisfaction with care. Procedures are reviewed in Appendix 1. The project was approved by the UC Davis Medical Center Committee on the Protection of Human Subjects.
Screening and power analysis. Subjects were recruited from eight rural primary care sites with 17 clinics over a 24-month period (Table 1). The sites were an average of 140 miles from the medical center, and they averaged nine PCPs, serving populations of 6,550, with 22,264 encounters per year. Only one site had a psychiatrist technically available, though this physician worked mainly in mental health (Table 1). Based on studies in the literature with different interventions and populations,6,16,17 approximately 50 percent of the subjects in the IDMM group and 80 percent of the subjects in the DMM group were likely to be depressed at six months after study entry. Therefore, approximately 42 subjects were needed in each group to test for a difference with the power set at 0.80 and an alpha level of significance set at 0.05.
Table 1.
Description of rural primary care sites
| Community | Population | Miles from UCDMC | Practitioners | Patient Encounters Per Year | Presence of Local Psychiatrists |
|---|---|---|---|---|---|
| Colusa | 5,000 | 68 | 6 (IM 2 & FP 4) |
25,819 | No |
| Downieville | 400 | 106 | 1 (FP 1) | 6,483 | No |
| Humboldt | 10,000 | 302 | 8 (FP 8) | 28,400 | Yes (5)* |
| Oroville | 10,000 | 68 | 29 (IM 14 & FP 15) |
27,899 | Yes (3)* |
| Portola | 10,000 | 153 | 5 (FP 5) |
19,200 | No |
| Quincy | 2,000 | 148 | 5 (FP 5) |
21,470 | No |
| Shasta | 10,000 | 162 | 10 (FP 10) |
23,700 | Yes (5)* |
| Sonora | 5,000 | 98 | 9 (IM 2 & FP 7) |
25,138 | Yes (1) |
| AVERAGE TOTAL | 6,550 | 140 | 9 | 22,264 |
Key:
- IM
Internal Medicine
- FP
Family Practice
- UCDMC
University of California Davis Medical Center, Sacramento, CA
Psychiatrists in county mental health sites only, with almost no interaction with primary care.
Within a week of referral, a telemedicine coordinator met with the potential subject in person to obtain informed consent and facilitate screening; the coordinator passed consent training in line with the National Institute of Health. Self-report instruments included the: 1) Beck Depression Inventory, a 13-item (BDI-13), well-validated instrument to detect and measure severity of depressive symptoms;18 2) Symptom Checklist-90 Revised (SCL-90-R), a 90-item, well-validated instrument;19 3) Medical Outcomes Study Short Form 36 (SF-36), which measures physical functioning, role functioning, overall mental health, perception of general health, and bodily pain.20 A structured interview with the mood and psychotic sections of the SCID-I, research version, was conducted via telephone by a board-certified psychiatrist to verify unipolar depression and exclude bipolar, schizoaffective, and schizophrenic disorders.15 A derivative of the SCID, the Diagnostic Interview Schedule (DIS), has been shown to be equivalent by in-person and telephone administration.21 All measures except the SCID-I were repeated at three, six, and 12 months follow-up. Data collection on use of health services also included outpatient visits with the PCP and telepsychiatric consultations, as measured by clinic logs and PCP chart review.
Exclusion criteria. Subjects without a primary diagnosis of major depression based on the semi-structured interview were excluded. Subjects with suicidal intention or plans, as demonstrated by a rating of 2 or 3 on the suicide question of the BDI and confirmed by interview, were also excluded and immediately referred to care in their community by communication with the PCP. As has been done in other studies,6 subjects with dementia, pregnancy, terminal illness, and plans to move in the next 12 months were not enrolled. All other psychiatric and medical disorders were noted for the purposes of analysis, but did not exclude subjects.
Other data collected included sociodemographic information and satisfaction with care. During the screening period, the subject completed a four-page questionnaire regarding satisfaction with mental health care, if applicable. The satisfaction questionnaire has been used for previous studies comparing telemedicine and usual psychiatric care.22,23 It assessed subjects' general satisfaction with care, as well as experience of the provider of mental health services, ability to communicate with the provider, and willingness to use identical care in the future. Satisfaction was also measured during the screening period and at three, six, and 12 months after study entry.
Treatment interventions. Immediately after screening, subjects were randomized using a random table of numbers, such that onsite staff would not inadvertently refer more seriously ill subjects to one condition or another. The IDMM group received a handout and a video on the biology of depression and how an antidepressant works, similar to collaborative care subjects.6 PCP visits were attempted to be scheduled at one, four, eight, 12, and 16 weeks. Telephone calls by the study nurse or an investigator occurred at Weeks 2 and 4 to assess adherence and side effects of medication, with referral to the PCP or telepsychiatrist if needed. Telepsychiatric consultations were offered at two (50 minutes), six (20 minutes thereafter), 10, 14, and 18 weeks. Telemedicine equipment included the following technology: Dial-up integrated service digital network (ISDN) lines at 384 kilobits/second; PictureTel Live 100 color monitors; and Canon VCC-1 cameras with local and remote pan-tilt-zoom control camera control. The 384 kilobits/second transmission offers a picture quality similar to television, without significant distortions or audiovisual delays.
Training of PCP. The PCP and the telepsychiatrist collaborated for the IDDM group by discussing the case by telephone or via televideo after the subject's first telepsychiatric appointment and on follow-up. The telepsychiatrist trained the PCP to administer care in accordance to national guidelines for mental healthcare of subjects in the primary care setting, by providing medication options,24 but did not literally prescribe medication as in the collaborative care model.6 The PCP was permitted to contact the psychiatrist by telephone regarding questions. The DMM group saw the PCP as indicated and some subjects received a one-time telepsychiatry visit, as this was the pre-study “standard” that was not withheld. If subjects in the IDDM group missed an appointment or either group had not turned in questionnaires in a timely fashion, the telemedicine and/or study coordinator telephoned them. If information signified an emergency, or a patient wrote of significant distress, the study coordinator notified the telemedicine coordinator, PCP, and the investigator for subjects in both groups; the PCP and local agencies took the lead.
Data analysis. Descriptive statistics for sociodemographic variables, severity of depression, number of lifetime depressive episodes, comorbid psychiatric disorders, and health status, and number of visits to the PCP and telepsychiatrist were tabulated for both groups. The groups were compared for equal distributions of potential confounds. Primary outcome measures were the BDI-13, SCL-90-R depression subscale, SF-36, and satisfaction scores. Secondary outcome measures were change in comorbid symptoms on the SCL-90-R (somatization, phobia, and anxiety) and study retention. Analysis of variance (ANOVA) was planned to test for a significant effect of the intervention, but the number of drop outs and measurements at four time periods better suited repeated measures random effects models (RMREM) and linear mixed-effects models (LMEM.25 Total variance into within group and between group variance was assessed over time. A residual analysis was completed in order to assess the goodness-of-fit of the models, as well to test for the accuracy of the models' assumptions. Subject stratified into moderate and severe depression groups based on their BDI-13 and SCL-90-R scores was planned, but since over 80 percent were severe, no post-hocanalyses were completed. Outcome analysis included the intent-to-treat sample and the treatment-completer sample. Attrition was tabulated from the time of randomization and an analysis was carried out to compare the groups, as well as sociodemographic and clinical predictors (e.g., age 44 vs. ≥45, or divided into 4 groups with equal numbers of subjects [<38, 38–45, 35–52, and >52]).
Results
The study included 94 subjects, 80 percent female, 50 percent married, 84 percent Caucasian, 49 percent employed (full- or part-time), with a mean age of 46 and a median age of 46 (Table 2). Over 50 percent of subjects had private insurance. There were no significant differences between the DMM and IDDM groups in terms of sociodemographics and types of insurance. The majority (n=81; 86%) of subjects came from two sites that employed active site coordinators. The mean number of depressive episodes for the groups measured by the SCID-I was 4.23 and 4.20, respectively. The DMM subjects averaged 0.5 telepsychiatric consultations and the IDMM subjects averaged 4.52 telepsychiatric consultations over 12 months. In terms of their use of primary care services, they averaged 8.4 and 9.9 visits, respectively (no significant difference).
Table 2.
Patient sociodemographics
| Parameter | Usual Care DMM | Intensive DMM | Total |
|---|---|---|---|
| N = 41 | N = 52 | N = 94 | |
| Caucasian | 40 (98%) | 44 (85%) | 84 (90%) |
| Female | 33 (80%) | 42 (80%) | 75 (80%) |
| Married | 18 (44%) | 29 (54%) | 47 (50%) |
| Some HS (only) | 10 (24%) | 22 (42%) | 32 (34%) |
| Some College | 22 (54%) | 19 (36%) | 41 (41%) |
| College + | 9 (22%) | 11 (21%) | 20 (21%) |
| Work: Full or Part | 22 (54%) | 10 (19%) | 49 (53%) |
| Work: Unemployed | 7 (17%) | 16(31%) | 19 (20%) |
| Work: Retired | 12 (29%) | 26 (50%) | 25 (27%) |
| Private | 25 (61%) | 26 (50%) | 51 (54%) |
| Medicare | 4 (10%) | 10 (19%) | 14 (17%) |
| MediCal | 12 (29%) | 16 (31%) | 28 (29%) |
Notes/Definitions:
Part-time work = 20 hrs
College + = graduate school or specialized training
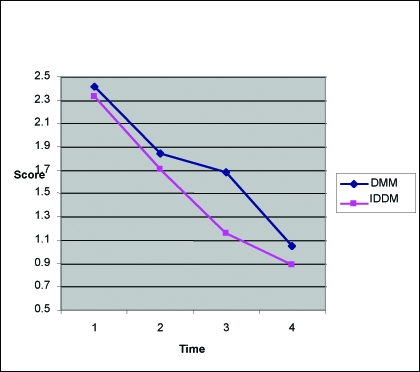
For all subjects, baseline BDI-13 scores for the current episode of depression ranged from 8 to 33, with a mean of 18.2 (severe depression). Average scores decreased to 13 (30% reduction), 12 (35%), and 11 (40%) at three, six, and 12 months, respectively (Figure 1). There was no significant difference between the groups, though there was greater variability (i.e., scores wavered much more from baseline) in the DMM group as measured by a permutation test (p<0.05). Overall, 39 (42.5%) subjects had a 50-percent reduction in depressive symptoms. There were 22 (42%) subjects with a 50-percent reduction in symptoms in the DMM group in the intent-to-treat analysis, and 28 (53%) when dropouts within three months were excluded; compared to 22 (42%) and 29 (56%) in the IDMM group.
Figure 1.
BDI-13 Scores over time
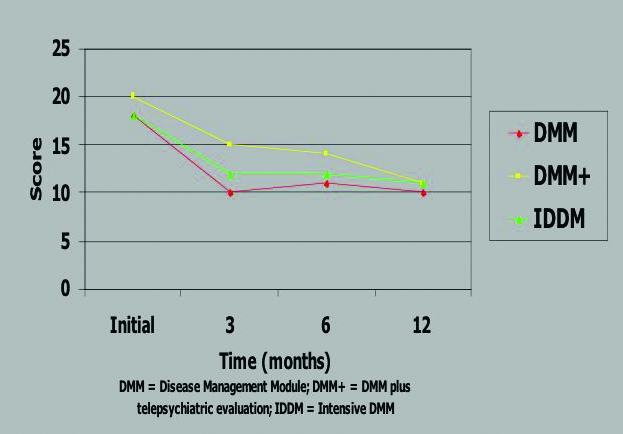
Overall, SCL-90-R depression subscale scores decreased gradually over time, from about 2. to 1.0, but there was no significant difference between the groups at other time intervals (Figure 2). Notably, of 45 (48%) people who reduced their SCL-90 Depression Scale score by 50 percent at some point in the study, 17 (42%) were DMM and 28 (53%) were IDDM. That percentage increases to 72 percent when people who dropped out before three months are removed. An unplanned post-hoc analysis showed that by removing the “DMM plus” group (DMM with the initial telepsychiatric evaluation at baseline), IDDM was nearly significantly better than DMM at three, six, and 12 months.
Figure 2.
SCL-90-R depression subscores over time
Other measures included satisfaction, SF-36 and comorbidity. SF-36 scores did not statistically change over the study and there was no difference between the groups, with a mean surprisingly low at around 40 for duration of the study. Comorbid somatization, phobia, and anxiety scores were not different at baseline, but the IDDM subjects significantly improved in all categories by end-point, and earlier, in most instances (Table 3). Satisfaction on a 1 to 7-point Likert scale at three, six and 12 months were 5.1, 4.9, and 5.6 for IDDM, compared to 5.1, 4.5, and 4.5 for DDM; p<0.05 at six and 12 months.
Table 3.
SCL-90-R somatization, phobia, and anxiety scores over time
| Indices | 0 | 3 Months | 6 Months | 12 Months |
|---|---|---|---|---|
| Somatization | ||||
| UC | 78 | 90 | 88 | 72 |
| T | 83 | 83 | 70^ | 50*^ |
| Phobia | ||||
| UC | 43 | 69 | 64 | 58 |
| T | 54 | 58 | 42^ | 28*^ |
| Anxiety | ||||
| UC | 98 | 80 | 82 | 60* |
| T | 90 | 80 | 58*^ | 46*^ |
Notes:
Significant change vs. baseline.
Significant change vs. comparison group.
Study retention as measured by survival curves was significantly better for the IDMM group compared to the DMM group, and even more so when the DMM group was analyzed in separate groups (with and without one-time telepsychiatric consultations) (Figure 3). Interestingly, older subjects were more likely to complete the study: approximately 10 percent more subjects in the 45+ group remained at zero, three, six, and 12 months, though this was not statistically significant. When the population was stratified into four groups with equal numbers of subjects (<38, 38–45, 35–52, and >52), the latter group was significantly more likely to stay in the study than the other groups (0.48, 0.58, and 0.58 vs. 0.78, respectively) (Figure 4). IDDM significantly bettered DDM. There were no differences based on other sociodemographics or clinical comorbidity.
Figure 3.
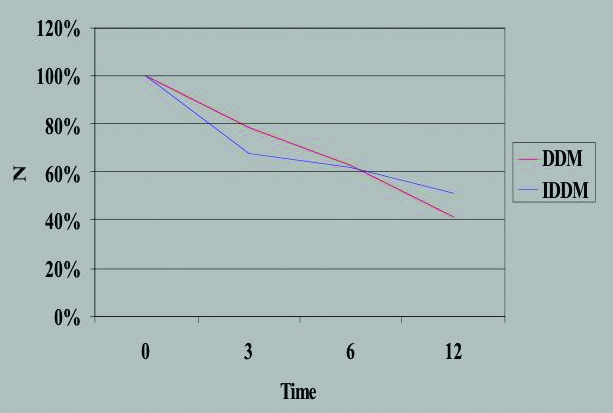
Study retention per group over time
Figures 4a–c.
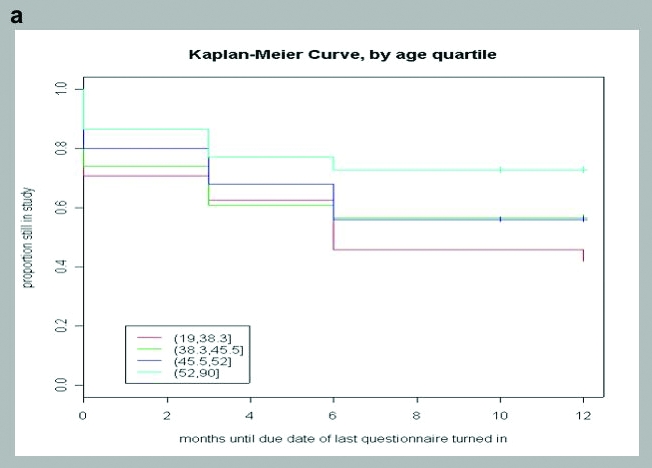
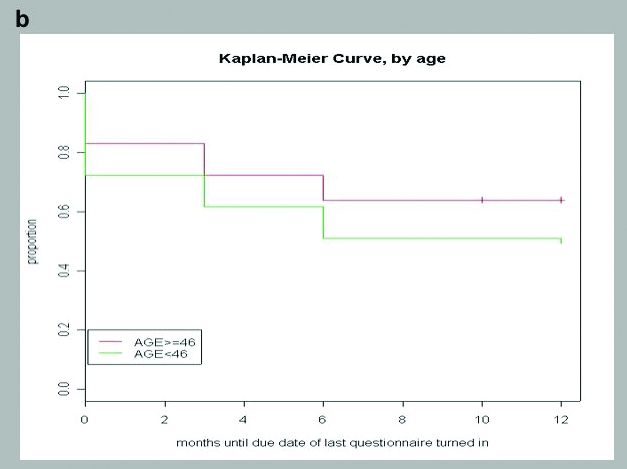
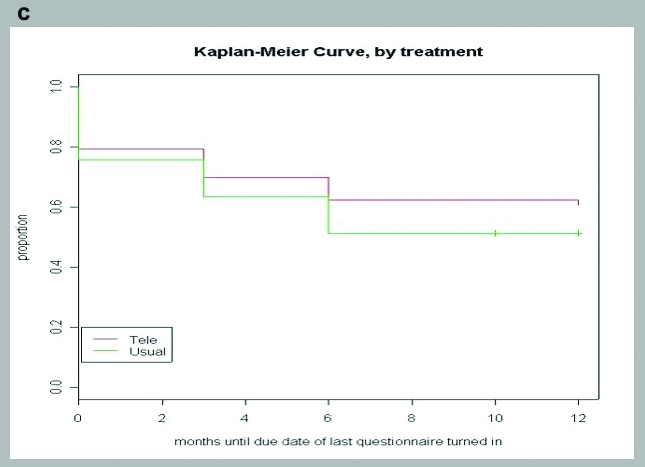
Study retention over time for a) quartile age; b) age less or above 46; and c) DMM vs. DMM plus telepsychiatry vs. IDDM.
In terms of regression and correlation analysis, there was a relationship between depression and health functioning scores. There was no relationship noted between depression scores and satisfaction, nor satisfaction and health functioning.
Discussion
The study showed that BDI-13 decreased significantly over time, and SCL-90 R depression subscales decreased initially, but there was no significant difference between the usual care with DMM and IDMM groups; a post-hoc analysis revealed that SCL-90-R depression subscale scores were nearly significant for IDMM vs. DDM, when those in the DMM with an initial telepsychiatric consultation were subtracted out. Comorbid somatization, phobia, and anxiety scores improved significantly in the IDMM subjects compared to the DMM subjects. Study retention as measured by survival curves was significantly better for the IDMM group compared to the DMM group, and even more so when the DMM group was analyzed in separate groups (with and without one-time telepsychiatric consultation).
The model used and the outcomes of our data are somewhat different from the results other intervention studies done in suburban, not rural, primary care. Katon, et al., and Schulberg, et al., noted a 40-percent reduction of depressive symptoms in usual care groups with no formal intervention other than screening; approximately 70 percent were still depressed at study's end.6,16,17 None of these studies used DMM and furthermore, they intervened with suburban subjects rather than rural subjects, who could be less healthy in terms of depressive symptoms, more comorbidities, less options for care, and other socioeconomic factors (i.e., a rural primary care may be more ill).26 Typical randomized trials are very structured over a short time, some with psychiatrist prescribing,6,8 which enhances ability of a study to determine outcomes, but may not fit a diverse rural network in terms of outright feasibility (e.g., none of our sites had ever participated in research). Finally, notification (only) interventions, historically, are not often sufficient to change outcomes,6,16,17 but this program and others notify and advise. For example, telemedicine specialty consultation (including telepsychiatry) changed the diagnosis in 91 percent of cases, changed medication in 57 percent, and improved clinical global measures in 56 percent of patients over a three-month study.27
The study's failure in outcomes but success in both difficult rural groups may be attributed to its disease management module, which allowed it to “fit” service delivery at the rural sites rather than a randomized controlled trial that might “dictate” the delivery of care. The monitoring system we employed with questionnaires and telephone interventions (e.g., rescheduling, education, encouragement regarding questionnaires), contact with PCPs, or a side-by-side design (i.e., they randomized clinics typically). The study, in that sense, provided a tracking system for all subjects, in which appointments were triggered if subjects were ill in either group, PCPs received data on subjects in an ongoing fashion, and PCPs were aware a study was in progress. This “administrative” intervention, using technology is the key component in disease management modules used for children with asthma28 and diabetes.29,30
Limitations and the complexity, though, of thoroughly regulating rural sites may have diluted intensity of the IDMM intervention. Furthermore, since subjects came from all clinics, rather than intervening at only select clinics, the interventions to PCPs may have been transferred to non IDDM subjects. This was conceived of pre-study, but an inclusive approach was taken as an investment in future studies. These are important considerations for the planning, implementation, and success of future rural health studies, with or without the use of telemedicine. The small sample size, high drop-out rate, and severity of illness (e.g., baseline health functioning scores around 40 on the SF-36) may have limited the study. In addition, it is unclear if medication was prescribed and taken according to national guidelines.24 Medication adherence, comorbid medical diagnosis(es), and utilization of overall health services was not tabluated. The latter two issues are being addressed in an add-on study in progress. Sites were not able to collect information on those who may have been asked to participate, but who refused, and who never came to our attention; this could limit how applicable study findings are to other settings. Finally, other limitations are mentioned as applicable above in the Discussion.
Conclusions
Clinical and administrative interventions by telemedicine may have significant benefit for rural populations, though more study is indicated. A balance needs to be struck between a health services design that “fits” these settings and a randomized, controlled design that provides structure and sufficient intensity of the intervention to measure its benefit. New models of service delivery are needed, as is evaluation of delivery of pre-existing disease management modules by new technologies.
Contributor Information
Donald M. Hilty, Dr. Hilty is Associate Professor of Clinical Psychiatry.
Shayna Marks, Ms. Marks is Postgraduate Researcher, Center for Health and Technology, University of California, Davis Medical Center.
Jacob Wegelin, Dr. Wegelin is with the Department of Biostatistics Unit Department of Public Health Sciences.
Edward J. Callahan, Dr. Callahan is Associate Dean of Academic Personnel and Professor of Family and Community Medicine.
Thomas S. Nesbitt, Dr. Nesbitt is Executive Associate Dean, Clinical and Administrative Affairs, Director, Center for Health and Technology, and Professor of Family and Community Medicine—All with University of California, Davis School of Medicine..
References
- 1.Kessler RC, Demler O, Frank RG, et al. Prevalance and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515–23. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Office of Technology Assessment. Healthcare in Rural America. Washington, DC: US Government Printing Office; 1990. (Publication No. OTA-H-434) [Google Scholar]
- 3.Lishner DM, Richardson M, Levine P, et al. Access to Primary Care Among Persons with Disabilities in Rural Areas: A Review of the Literature. Seattle, WA: WAMI Rural Health Research Center; 1995. [DOI] [PubMed] [Google Scholar]
- 4.Health Data Summaries for California Counties. Department of Health Services; State of California: 2000. [Google Scholar]
- 5.Geller JM. Rural primary care providers' perceptions of their roles in the provision of mental health services: Voices from the plains. J Rural Health. 1999;15(3):326–34. doi: 10.1111/j.1748-0361.1999.tb00754.x. [DOI] [PubMed] [Google Scholar]
- 6.Katon WJ. The Institute of Medicine “Chasm” report: Implications for depression collaborative care models. Gen Hosp Psychiatry. 2003;25(4):222–9. doi: 10.1016/s0163-8343(03)00064-1. [DOI] [PubMed] [Google Scholar]
- 7.Pincus H: Patient-oriented models for linking primary care and mental health care. Gen Hosp Psychiatry. 1987;9:95–101. doi: 10.1016/0163-8343(87)90020-x. [DOI] [PubMed] [Google Scholar]
- 8.Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve depression treatment guidelines. J Clin Psychiatry. 1997;58(Suppl 1):20–4. [PubMed] [Google Scholar]
- 9.Wells KB, Unutzer J, Sherbourne C, et al. Cost-effectiveness of practice-initiated quality improvement for depression. JAMA. 2001;286(11):1325–30. doi: 10.1001/jama.286.11.1325. [DOI] [PubMed] [Google Scholar]
- 10.Hilty DM, Marks SL, Urness D, et al. Clinical and educational applications of telepsychiatry: A review. Can J Psychiat. 2004;49(1):12–23. doi: 10.1177/070674370404900103. [DOI] [PubMed] [Google Scholar]
- 11.Hilty DM, Yellowlees PM, Cobb HC, et al. Models of telepsychiatric consultation-liaison service to rural primary care. Psychosomatics. 2006;47(2):152–7. doi: 10.1176/appi.psy.47.2.152. [DOI] [PubMed] [Google Scholar]
- 12.Nesbitt TS, Hilty DM, Kuenneth T, et al. Development of a successful telemedicine program. Western J Med. 2000;173:1674. doi: 10.1136/ewjm.173.3.169-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hilty DM, Ingraham RL, Yang SP, et al. Multispecialty phone and email consultation to primary care providers for patients with developmental disabilities in rural California. J Telemed E-Health. 2004;10:413–21. doi: 10.1089/tmj.2004.10.413. [DOI] [PubMed] [Google Scholar]
- 14.Chan DS, Callahan CW, Sheets SJ, et al. An Internet-based store-and-forward video home telehealth system for improving asthma outcomes in children. Am J Health Syst Pharm. 2003;60(19):1976–81. doi: 10.1093/ajhp/60.19.1976. [DOI] [PubMed] [Google Scholar]
- 15.Zanarini MC, Skodol AE, Bender D, et al. The Collaborative Longitudinal Personality Disorders Study: Reliability of axis I and II diagnoses. J Personal Disord. 2000;14(4):291–9. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- 16.Schulberg HC, Block MR, Madonia MJ, et al. Treating major depression in primary care practice. Arch Gen Psychiatry. 1996;53:913–9. doi: 10.1001/archpsyc.1996.01830100061008. [DOI] [PubMed] [Google Scholar]
- 17.Schulberg H, Coulehan J, Block M, et al. Strategies for evaluating treatments for major depression in primary care patients. Gen Hosp Psychiatry. 1991;13:9–18. doi: 10.1016/0163-8343(91)90004-g. [DOI] [PubMed] [Google Scholar]
- 18.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1998;8:77–100. [Google Scholar]
- 19.Derogatis LR. SCL-90-R Administration, Scoring, and Procedural Manual-II. Towson, MD: Clinical Psychometric Research; 1983. [Google Scholar]
- 20.Wells KB, Hays R, Burman MA, et al. Detection of depressive disorder for patients receiving prepaid or fee-for-service care: Results from the Medical Outcomes Study. JAMA. 1989;262:3298–302. [PubMed] [Google Scholar]
- 21.Wells KB, Burnam MA, Leake B, et al. Agreement between face-to-face and telephone administered versions of the depression section of the NIMH Diagnostic Interview Schedule. J Psychiatric Res. 1998;22:207–20. doi: 10.1016/0022-3956(88)90006-4. [DOI] [PubMed] [Google Scholar]
- 22.Von Korff M, Katon W, Lin E, et al. Treatment costs, cost offset, and cost-effectiveness of collaborative management of depression. Psychosom Med. 1998;60:143–9. doi: 10.1097/00006842-199803000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Hilty DM, Servis ME, Nesbitt TS, et al. The use of telemedicine to provide consultation-liaison service to the primary care setting. Psychiatr Ann. 1999;29:421–7. [Google Scholar]
- 24.Depression in Primary Care, Volume 2. Treatment. Clinical Practice Guideline, No. 5. Rockville, MD: US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; AHCPR Publication No. 93-0551, April, 1993. [Google Scholar]
- 25.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38(4):963–74. [PubMed] [Google Scholar]
- 26.Hilty DM, Nesbitt TS, Kuenneth TA, et al. Telepsychiatric consultation to primary care: Rural vs. suburban needs, utilization and provider satisfaction. J Rural Health. doi: 10.1111/j.1748-0361.2007.00084.x. In Press. [DOI] [PubMed] [Google Scholar]
- 27.Marcin JP, Nesbitt TS, Cole SL, et al. Changes in diagnosis, treatment, and clinical improvement among patients receiving telemedicine consultations. J Tel e-Health. 2005;11(1):36–43. doi: 10.1089/tmj.2005.11.36. [DOI] [PubMed] [Google Scholar]
- 28.Goldberg HI, Ralston JD, Hirsch IB, et al. Using an Internet co-management module to improve the quality of chronic disease care. J Comm J Qual Saf. 2003;29(9):443–51. doi: 10.1016/s1549-3741(03)29053-5. [DOI] [PubMed] [Google Scholar]
- 29.Lehmann ED, Deutsch T, Roudsari AV, et al. An integrated approach for the computer-assisted treatment of diabetic patients on insulin. Med Inform. 1992;17(2):105–23. doi: 10.3109/14639239209085014. [DOI] [PubMed] [Google Scholar]
- 30.Carson ER, Carey S, Harvey FE, et al. Information technology and computer-based decision support in diabetic management. Comput Methods Programs Biomed. 1990;32:179–88. doi: 10.1016/0169-2607(90)90100-n. [DOI] [PubMed] [Google Scholar]