Abstract
Studies examining associations between racial discrimination and cardiovascular health outcomes have been inconsistent, with some studies finding the highest risk of hypertension among African Americans who report no discrimination. A potential explanation of the latter is that hypertension and other cardiovascular problems are fostered by internalization and denial of racial discrimination. To explore this hypothesis, the current study examines the role of internalized negative racial group attitudes in linking experiences of racial discrimination and history of cardiovascular disease among African American men. We predicted a significant interaction between reported discrimination and internalized negative racial group attitudes in predicting cardiovascular disease. Weighted logistic regression analyses were conducted among 1216 African American men from the National Survey of American Life (NSAL; 2001– 2003). We found no main effect of racial discrimination in predicting history of cardiovascular disease. However, agreeing with negative beliefs about Blacks was positively associated with cardiovascular disease history, and also moderated the effect of racial discrimination. Reporting racial discrimination was associated with higher risk of cardiovascular disease among African American men who disagreed with negative beliefs about Blacks. However, among African American men who endorsed negative beliefs about Blacks, the risk of cardiovascular disease was greatest among those reporting no discrimination. Findings suggest that racial discrimination and the internalization of negative racial group attitudes are both risk factors for cardiovascular disease among African American men. Furthermore, the combination of internalizing negative beliefs about Blacks and the absence of reported racial discrimination appear to be associated with particularly poor cardiovascular health. Steps to address racial discrimination as well as programs aimed at developing a positive racial group identity may help to improve cardiovascular health among African American men.
Keywords: USA, African American men, cardiovascular disease, racial discrimination, racial identity
African American men have alarmingly poor health, having the lowest life expectancy and highest mortality rates compared to other racial and gender groups in the United States (National Center for Health Statistics, 2009). African American men are at higher risk for hypertension and major cardiovascular events, such as cardiac death, myocardial infarction, stroke, and heart failure, compared to White men (American Heart Association, 2007; Centers for Disease Control and Prevention, 2006; National Center for Health Statistics, 2009). Cardiovascular disease is the leading cause of death among African American men, and they are more likely to die prematurely from cardiovascular diseases compared to White men (American Heart Association, 2007). Between 2001 and 2004, approximately 42.2% of African American men over 20 years of age were hypertensive, compared to 31.2% of White men (National Center for Health Statistics, 2009). These disparities are apparent even in younger adult men (Heffernan, Jae, Wilund, Woods, & Fernhall, 2008). A recent study found higher incident heart failure among African American men compared to White men 50 years of age and younger, and among those who developed heart failure, 75% were hypertensive prior to 40 years of age (Bibbins-Domingo, et al., 2009). These data indicate that poor cardiovascular health among African American men represents a serious public health concern and highlight the need to identify risk factors for cardiovascular diseases in this population (Kurian & Cardarelli, 2007; Mensah, 2005).
Unique social stressors and psychosocial challenges that African American men experience may contribute to greater risk for developing cardiovascular diseases, including racial discrimination related to racial profiling, and in domains such as employment, housing, education, and health care (Brondolo, et al., 2008; V. R. Clark, 2001; Cooper, 2001; Davis, Liu, Quarells, & Din-Dzietharn, 2005; Ryan, Gee, & Laflamme, 2006; Williams, 1999; Williams, Neighbors, & Jackson, 2003). Experiences of racial discrimination continue to be salient in the lives of African American men despite the existence of protective legislation (e.g., Aguirre & Turner, 2004; U.S. Equal Employment Opportunity Commission, 2007), and these stressful life experiences may impact cardiovascular health indirectly through psychological and behavioral reactions to stress and via its impact on biological systems engaged in the stress response (Clark, Anderson, Clark, & Williams, 1999).
Symbolic interaction and social evaluation theories post that individuals derive self-concept from the values attached to their social groups (Cooley, 1902; Mead, 1934; Pettigrew, 1967). Accordingly, experiences of racial discrimination may lead to poorer self-evaluation and negative affect via the internalization of negative racial group attitudes (Schulz, et. al., 2006; Williams & Williams-Morris, 2000). Such experiences may also lead to negative cognitive reactions, such as depression, anxiety, anger or hostility (Armstead, lawler, Gorden, Cross, & Gibbons, 1989; Fang & Myers, 2001; Klonoff, Landrine, & Ullman, 1999). Indeed, researchers have most consistently found evidence for the negative mental health implications of racial discrimination (Gee, Ryan, Laflamme, & Holt, 2006; Schulz, et al., 2006; Sellers, Caldwell, Schmeelk-Cone, & Zimmerman, 2003), including psychological responses that are linked to worse cardiovascular outcomes (Eaker, Sullivan, Kelly-Hayes, D’Agostino, & Benjamin, 2004; Musselman, Evans, & Nemeroff, 1998). Further evidence comes from experimental studies that find higher levels of cardiovascular reactivity in response to hypothetical scenarios consisting of a racial stressor (Guyll, Matthews, & Bromberger, 2001; Merritt, Bennett, Williams, Edwards, & Sollers, 2006). This dynamic is consistent with evidence of the impact of social stressors on physiology via autonomic nervous, endocrine, and immune systems (Cacioppo, Berntson, Sheridan, & McClintock, 2000; Epel, et al., 2004; Esterling, Kiecolt-Glaser, Bodnar, & Glaser, 1994).
Findings from studies using survey data and self-reports of racial discrimination, however, have been equivocal (Brondolo, Rieppi, Kelly, & Gerin, 2003; Harrell, Hall, & Taliaferro, 2003; Williams & Neighbors, 2001; Williams, et al., 2003). Some studies find no main effect of self-reported discrimination on cardiovascular health outcomes (Broman, 1996; Dressler, 1996), while others find evidence for moderated or curvilinear associations (Huebner & Davis, 2007; Krieger & Sidney, 1996). For example, Krieger and Sidney (1996) found that although the relationship between discrimination and blood pressure was positive among professional African Americans, the association was U-shaped among working-class African Americans, and in fact, blood pressure was highest among working-class African Americans who reported no discrimination. Roberts, Vines, Kaufman, and James (2008) found an inverse relationship between discrimination and blood pressure among African American men, with those reporting no racial discrimination being at greater risk for hypertension. The authors of these studies interpreted their findings as suggesting that internalization and denial of racial discrimination may be associated with worse cardiovascular health outcomes.
Although contentious, these findings may be consistent with theories of racial identity and minority stress. In her model of racial identity, Helms (1990, 1995) distinguished between individuals with less complex racial identity schemas, characterized by ambivalence towards identifying as a racial minority and a minimization of racism, versus those with more complex schemas who display a strong valuation or idealization of their racial group and a greater awareness about issues of racism and social oppression. Accordingly, self-reports of discrimination are contingent not only on the experience of a negatively appraised event, but also on its interpretation as being an instance of racial discrimination, which may be associated with dimensions of racial identity (Krieger, 1999; Meyer, 2003; Pinel, 1999; Sellers & Shelton, 2003). For some African Americans, failure to report racial discrimination may reflect a racial identity schema characterized by a denial of racism. In tandem with negative racial group evaluations, reporting no or low levels of racial discrimination may be associated with worse health outcomes (Chae & Yoshikawa, 2008; Krieger, 1990; Roberts, et al., 2008). Other researchers have theorized that interpreting negative life experiences as instances of systematic discrimination might be protective via the minimization of internal or personal causes (Crocker & Major, 1989; Major, Kaiser, & McCoy, 2003; Weiner, 1985).
Along these lines, racial identity frameworks suggest additional pathways that may be involved in linking racial discrimination and cardiovascular health among African American men. Experiences of racism may not necessarily be internalized, and among those with a more positive racial identity, attributing experiences of unfair treatment or discrimination to race may not have negative health consequences (Branscombe, Schmitt, & Harvey, 1999; Chae & Yoshikawa, 2008; Romero & Roberts, 2003; Schmitt, Branscombe, & Kappen, 2003; Sellers, et al., 2003). On the other hand, those who have internalized negative racial group attitudes may be at greater risk of cardiovascular diseases, particularly if this co-occurs with failure to acknowledge experiencing racial discrimination.
In order to test these hypothesized associations, data from the National Survey of American Life (NSAL) were used to investigate whether self-reported instances of racial discrimination are associated with history of cardiovascular disease among African American men. Based on prior findings suggesting that the internalization of discrimination may account for greater risk of hypertension found among those reporting no discrimination, we investigate whether the endorsement of negative beliefs about Blacks, used as a measure of internalized negative racial group attitudes, is associated with worse cardiovascular health in this population. In addition, we test whether associations between racial discrimination and history of cardiovascular disease are different according to whether someone has internalized negative stereotypes against Blacks. Accordingly, this study examines if failure to report racial discrimination together with the internalization of negative social perceptions of Blacks may be associated with worse cardiovascular health among African American men.
Methods
Sample and Procedure
The sampling design and procedures of the NSAL have been previously documented (Heeringa, et al., 2004; Jackson, Neighbors, Nesse, Trierweiler, & Torres, 2004; Jackson, Torres, et al., 2004). Briefly, the NSAL recruited a nationally representative household sample of Black Americans, including 3570 African American adults, 1621 Blacks of Caribbean descent, and 891 non-Hispanic White adults between February 2001 and June 2003 using a multistage area probability design. For this study, analyses were restricted to the 1271 African American men recruited to the NSAL. We chose to focus on the African American sample given prior studies that have found that Caribbean Blacks and other predominantly immigrant Black populations have health profiles that vary considerably from African Americans, and whose experiences of stress and racial discrimination may be qualitatively different (Seaton, Caldwell, Sellers, & Jackson, 2008; Williams, Gonzalez, et al., 2007; Williams, Haile, et al., 2007). In addition, these associations were examined among men in light of preliminary analyses suggesting that the discrimination items that were assessed may be more relevant to the experiences of African American men.
African American participants were recruited from 64 primary sampling units (PSUs): 21 self-representing metropolitan statistical areas (MSAs) which were selected based on size of the African American population; and 43 MSA and non-MSA PSUs which were selected using a modified probability sampling method. Four hundred fifty-six secondary sampling units were then selected using probabilities proportionate to size. Households were enumerated and screened, from which one eligible participant was selected. Weighting corrections were constructed to take into account the sampling design features of the study. The weighted response rate of African American participants was 70.7%.
Participants were interviewed by a racially-concordant lay interviewer in English (mean duration: 2 hours 20 minutes for African Americans) and were compensated $50.00 for their time. All study procedures and protocols were approved by the University of Michigan.
Measures
Racial discrimination
Experiences of racial discrimination were assessed using the Major Experiences of Discrimination Scale developed by Williams and colleagues (Williams, Yu, Jackson, & Anderson, 1997). Participants were asked whether they had ever experienced any of nine negative events: being fired, not being hired, being denied a promotion, being abused by the police, being discouraged in education, being prevented from renting or buying housing, experiencing poor treatment by neighbors, being denied a loan, and poor treatment from service providers. Following each item reported, participants were asked the main reason for these experiences. Participants who reported experiencing the event and attributed it to race, ancestry, or skin color were classified as having experienced racial discrimination in that situation. In the current study, participants were classified as having experienced no racial discrimination, racial discrimination in 1 situation, 2 situations, and 3 situations or more.
Racial group attitudes
Negative racial group attitudes was measured using three items assessing whether the respondent agreed with negative statements regarding Blacks, specifically, whether Blacks are lazy, give up easily, and are violent. Agreement with each item was measured on a 4-point scale (1 = not at all true, 4 = very true). Scores ranged from 3 to 12, with higher scores representing more negative racial group attitudes (alpha = 0.70).
History of cardiovascular disease
History of cardiovascular disease was measured using four items assessing history of hypertension, atherosclerosis, heart attack, and stroke. Participants were asked whether they ever had any of 22 health conditions. Participants who indicated any of the four cardiovascular problems were categorized as having a history of cardiovascular disease. Although self-report items of history of cardiovascular health are limited, prior studies have found high levels of recall accuracy of cardiovascular health history (Colditz, et al., 1986; Harlow & Linet, 1989). In addition, to help address issues related to comprehension, the NSAL used non-clinical terms that were linguistically appropriate for the general population and culturally relevant, i.e., “high blood pressure” “blood circulation problems or hardening of the arteries” and “heart trouble or heart attack.”
Sociodemographic characteristics
Covariates that were included in analyses were self-reported: age in years; marital status (married, partnered, separated, widowed, divorced, or never married); poverty level based on ratio of household income and composition to the poverty threshold (poor with a poverty ratio of < 1.00, near-poor with a poverty ratio of 1.00–1.99, non-poor with poverty ratio of 2.00–3.00, and non-poor with poverty ratio of 4.00 or more) (National Center for Health Statistics, 1998; U.S. Census Bureau, 2007); educational level (less than 12 years, 12 years, 13–15 years, and 16 years or more); employment status (employed, unemployed, and out of labor force); insurance status (insured or uninsured); and region of residence (South, Northeast, Midwest, and West). Social desirability bias was also measured as the mean of ten items endorsed as “true” (with a value of 1) or “false” (with a value of 0) to control for personality factors that may bias responses to sensitive questions (Marlowe & Crowne, 1961). Example items included: “I have always told the truth”; “I have never been bored”; and “I have never lost anything.” Higher mean scores represented greater levels of social desirability bias.
In addition, two indicators of health were controlled for in multivariable analyses: body mass index, calculated using self-reported height and weight; and self-reported smoking status (never-smoker versus ever smoker).
Statistical Analysis
Fifty-five participants had missing data on history of cardiovascular health. These participants were excluded from all analyses, leaving a total sample size of 1216 comprising the analytic sample. Using listwise deletion to handle missing data representing less than 5% of the sample has been shown to be an acceptable technique (Schafer, 1997). Missing data on basic sociodemographic variables (i.e., marital status, poverty level, education level, employment status, insurance status) were handled by NSAL investigators using hot-deck imputation. Descriptive analyses were conducted using this dataset.
In multivariable analyses, we additionally used multiple imputation to handle remaining missing data on independent variables: 22 had missing data on negative attitudes towards Blacks, three had missing data on social desirability, eight had missing data on BMI, and eight had missing data on smoking. Five imputations for missing values were generated using a Markov chain Monte Carlo technique assuming an arbitrary missing data pattern (Schafer, 1997; Schafer & Graham, 2002; Rubin, 1987). Imputed values were truncated to fit the bounds of possible values but were not rounded (Allison, 2000; Horton, Lipsitz, & Parzen, 2003). Multiple imputation is considered to properly take into account the uncertainty inherent in missing values and lead to valid statistical inferences (Rubin, 1987).
Multivariable logistic regression analyses first examined the main effect of racial discrimination on history of cardiovascular health. We then added racial group attitudes to the model. In addition, whether the influence of racial discrimination on these outcomes was moderated by racial group attitudes was examined by entering the corresponding interaction term. We interpreted interactions at the p < 0.10 level due to known difficulties in detecting statistically significant interactions in non-clinical settings (McClelland & Judd, 1993). In the final model, we controlled for BMI and smoking status.
All analyses took into account sampling weights and study design variables using the PROC RLOGIST and MI_COUNT option in SAS-callable SUDAAN Version 10.0.0 (RTI International, 2004).
Results
Descriptive characteristics of the NSAL sample of African American men by history of cardiovascular disease are presented in Table 1. Approximately 34% of African American men reported having a history of cardiovascular disease. A majority of participants reported having experienced racial discrimination in at least one situation (56%), with approximately 17% reporting having experienced racial discrimination in three or more situations. The mean negative racial group attitude score was 6.53, with 35% of participants indicating overall agreement with negative beliefs about Blacks (a total score of 8 or more on items measuring negative racial group attitudes).
Table 1.
Weighted descriptive characteristics of African American men (n = 1216) in the National Survey of American Life (NSAL; 2001–2003).
| Total | Cardiovascular Disease History |
||
|---|---|---|---|
| No History | Any History | ||
| Cardiovascular Disease, n (%) | |||
| No History | 790 (65.6) | ||
| Any History | 426 (34.4) | ||
| Racial Discrimination, n (%) | |||
| None | 541 (44.1) | 364 (45.4) | 177 (41.8) |
| 1 Situation | 290 (23.7) | 192 (24.3) | 98 (22.5) |
| 2 Situations | 185 (15.3) | 118 (15.4) | 67 (15.1) |
| 3+ Situations | 200 (16.9) | 116 (14.9) | 84 (20.6) |
| Negative Racial Group Attitudes, Mean (SE) | 6.53 (0.09) | 6.43 (0.10) | 6.72 (0.16) |
| Age, Mean (SE) | 41.8 (0.68) | 36.6 (0.67) | 51.7 (0.77) |
| Relationship Status, n (%) | |||
| Married | 431 (40.5) | 244 (34.2) | 187 (52.5) |
| Partnered | 104 (9.3) | 82 (11.2) | 22 (5.7) |
| Separated, Widowed, Divorced | 303 (19.7) | 166 (16.6) | 137 (25.5) |
| Never Married | 378 (30.6) | 298 (38.0) | 80 (16.3) |
| Poverty Level, n (%) | |||
| Poor (< 1.00) | 212 (17.2) | 127 (16.3) | 85 (18.7) |
| Near Poor (1.00–1.99) | 251 (19.2) | 149 (18.2) | 102 (21.1) |
| Non-Poor (2.00–3.99) | 449 (37.9) | 316 (39.9) | 133 (34.1) |
| Non-Poor (4.00+) | 304 (25.8) | 198 (25.6) | 106 (26.2) |
| Work Status, n (%) | |||
| Employed | 853 (71.6) | 625 (78.7) | 228 (57.9) |
| Unemployed | 99 (8.9) | 72 (10.2) | 27 (6.3) |
| Not in Labor Force | 264 (19.6) | 93 (11.0) | 171 (35.8) |
| Education, n (%) | |||
| < 12 years | 301 (22.6) | 148 (17.5) | 153 (32.3) |
| 12 years | 476 (39.8) | 347 (44.3) | 129 (31.0) |
| 13–15 years | 275 (23.0) | 187 (23.3) | 88 (22.3) |
| 16 years or more | 164 (14.7) | 108 (14.8) | 56 (14.4) |
| Insurance Status, n (%) | |||
| Uninsured | 228 (18.6) | 175 (22.1) | 53 (12.0) |
| Insured | 988 (81.4) | 615 (77.9) | 373 (88.0) |
| Region, n (%) | |||
| Northeast | 148 (16.1) | 96 (16.7) | 52 (14.7) |
| Midwest | 184 (16.2) | 114 (15.7) | 70 (17.1) |
| South | 788 (57.2) | 514 (56.6) | 274 (58.3) |
| West | 96 (10.6) | 66 (11.0) | 30 (9.9) |
| Social Desirability Bias, Mean (SE) | 0.22 (0.01) | 0.22 (0.01) | 0.23 (0.01) |
| Body Mass Index, Mean (SE) | 28.08 (0.18) | 27.12 (0.23) | 29.92 (0.30) |
| Smoking Status, n (%) | |||
| Never Smoker | 811 (67.9) | 522 (66.5) | 289 (70.5) |
| Ever Smoker | 397 (32.1) | 263 (33.5) | 134 (29.5) |
Note: Sum of column may not equal total due to missing data.
Logistic Regressions Predicting History of Cardiovascular Disease
Results from weighted logistic regressions predicting history of cardiovascular disease are presented in Table 2. Controlling for sociodemographic factors, reporting more situations of racial discrimination was associated with higher odds of having a history of cardiovascular disease, but these relationships were not significant (Model 1). However, having negative racial group attitudes was associated with increased odds of having a history of cardiovascular disease (Model 2: OR = 1.11, 95% CI = 1.03, 1.20).
Table 2.
Weighted logistic regressions predicting history of cardiovascular disease among African American men (n = 1216) in the National Survey of American Life (NSAL; 2001–2003).
| Odds Ratio (95% Confidence Interval) | ||||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Racial Discrimination (Ref: None) | ||||
| 1 Situation | 1.08 (0.71, 1.64) | 1.09 (0.72, 1.66) | 2.15 (0.50, 9.26) | 2.07 (0.50, 8.62) |
| 2 Situations | 1.15 (0.73, 1.79) | 1.17 (0.74, 1.84) | 4.93 (1.17, 20.68) | 6.69 (1.64, 27.25) |
| 3 or more Situations | 1.27 (0.81, 2.00) | 1.27 (0.82, 1.99) | 4.37 (1.08, 17.74) | 3.54 (0.91, 13.73) |
| Negative Racial Group Attitudes | 1.11 (1.03, 1.20) | 1.22 (1.08, 1.39) | 1.21 (1.07, 1.36) | |
| Discrimination × Racial Attitudes (Ref: None × Racial Attitudes) | ||||
| 1 Situation × Racial Attitudes | 0.91 (0.74, 1.10) | 0.91 (0.75, 1.10) | ||
| 2 Situations × Racial Attitudes | 0.80 (0.65, 0.98) | 0.76 (0.62, 0.93) | ||
| 3 Situations × Racial Attitudes | 0.83 (0.68, 1.02) | 0.85 (0.70, 1.03) | ||
| Age | 1.06 (1.04, 1.08) | 1.06 (1.05, 1.08) | 1.06 (1.05, 1.08) | 1.06 (1.05, 1.08) |
| Marital Status (Ref: Married) | ||||
| Partnered | 0.59 (0.37, 0.92) | 0.57 (0.36, 0.91) | 0.60 (0.37, 0.96) | 0.71 (0.43, 1.20) |
| Separated, Widowed, Divorced | 0.68 (0.44, 1.05) | 0.70 (0.45, 1.09) | 0.71 (0.46, 1.10) | 0.86 (0.54, 1.37) |
| Never Married | 0.67 (0.45, 0.98) | 0.67 (0.45, 0.99) | 0.69 (0.47, 1.01) | 0.79 (0.53, 1.19) |
| Poverty Ratio (Ref: < 1.00) | ||||
| 1.00–1.99 | 0.80 (0.45, 1.42) | 0.80 (0.45, 1.40) | 0.82 (0.46, 1.45) | 0.72 (0.40, 1.29) |
| 2.00–3.99 | 0.69 (0.42, 1.14) | 0.70 (0.43, 1.14) | 0.73 (0.45, 1.19) | 0.60 (0.35, 1.01) |
| 4.00 + | 0.67 (0.35, 1.29) | 0.69 (0.37, 1.27) | 0.72 (0.39, 1.32) | 0.60 (0.31, 1.17) |
| Education (Ref: < 12 years) | ||||
| 12 years | 0.56 (0.38, 0.83) | 0.59 (0.40, 0.88) | 0.61 (0.41, 0.90) | 0.61 (0.39, 0.93) |
| 13–15 years | 0.72 (0.50, 1.04) | 0.80 (0.55, 1.16) | 0.81 (0.56, 1.18) | 0.81 (0.54, 1.22) |
| 16+ years | 0.58 (0.33, 1.02) | 0.68 (0.40, 1.17) | 0.69 (0.40, 1.18) | 0.62 (0.37, 1.06) |
| Work Status (Ref: Employed) | ||||
| Unemployed | 1.16 (0.72, 1.87) | 1.19 (0.74, 1.93) | 1.20 (0.74, 1.94) | 1.16 (0.71, 1.91) |
| Out of Labor Force | 1.53 (1.00, 2.35) | 1.58 (1.02, 2.43) | 1.64 (1.05, 2.55) | 1.82 (1.14, 2.92) |
| Uninsured vs. Insured | 0.62 (0.40, 0.96) | 0.60 (0.38, 0.93) | 0.61 (0.38, 0.96) | 0.67 (0.41, 1.07) |
| Region (Ref: South) | ||||
| Northeast | 0.85 (0.57, 1.26) | 0.83 (0.55, 1.24) | 0.83 (0.56, 1.24) | 0.84 (0.56, 1.25) |
| Midwest | 1.00 (0.59, 1.69) | 1.00 (0.61, 1.64) | 1.02 (0.62, 1.69) | 0.99 (0.62, 1.57) |
| West | 0.85 (0.50, 1.44) | 0.87 (0.49, 1.53) | 0.87 (0.51, 1.47) | 0.96 (0.58, 1.61) |
| Social Desirability Bias | 0.47 (0.21, 1.08) | 0.44 (0.19, 1.01) | 0.43 (0.19, 1.00) | 0.41 (0.18, 0.98) |
| Body Mass Index | 1.11 (1.07, 1.14) | |||
| Ever vs. Never Smoker | 0.83 (0.56, 1.23) | |||
Note: Model 1 is the association between racial discrimination and cardiovascular disease history controlling for socio-demographic factors; Model 2 adds negative racial group attitudes; Model 3 tests the interaction between racial discrimination and negative racial group attitudes; Model 4 adjusts for BMI and smoking status.
The interaction between racial discrimination and racial group attitudes was tested in Model 3. Using Wald tests summarized across the five imputations, results indicated that the effect of reporting two situations of racial discrimination (χ2 = 4.44, 1 df, p = 0.04) and three or more situations of racial discrimination (χ2 = 3.25, 1 df, p = 0.07) significantly varied by racial group attitudes. Adding BMI and smoking status to the model did not substantively change results (Model 4).
To illustrate the relationship between racial discrimination and history of cardiovascular health by racial group attitudes, predicted probabilities were constructed (Figure 1). Values for racial discrimination were manipulated to reflect differences in the number of self-reported situations of racial discrimination. Values of one standard deviation below and above the mean value for racial group attitudes were chosen to represent low and high negative racial group attitudes, respectively. Choosing alternative values for low and high negative racial group attitudes did not significantly alter the shape of plots. Mean values of all other covariates were chosen to illustrate these relationships for the average participant (Jaccard, 2001).
Figure 1.
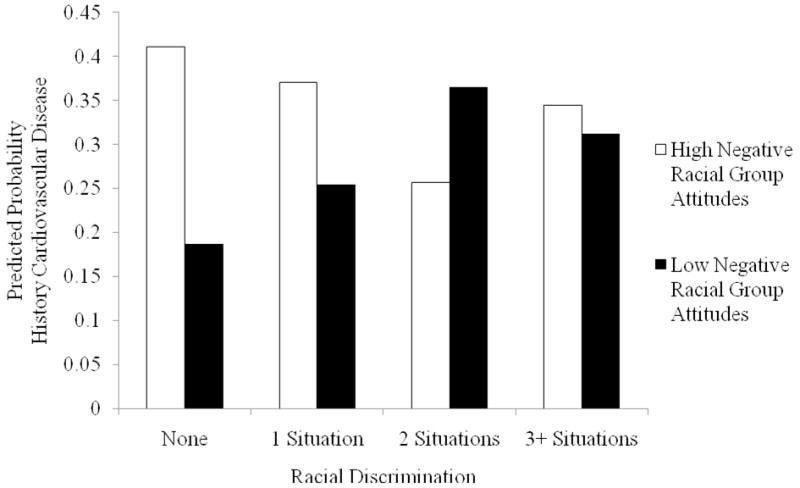
Predicted probabilities of history of cardiovascular disease by racial discrimination and negative racial group attitudes among African American men (n = 1216) in the National Survey of American Life (NSAL; 2001–2003).
Results indicated that among participants with low negative racial group attitudes, there was an inverse U-shaped relationship between self-reports of racial discrimination and the probability of having a history of cardiovascular disease. Specifically, reporting two situations of racial discrimination was associated with the highest probability of having a history of cardiovascular disease, followed by reporting three or more situations of racial discrimination. In contrast, among participants who endorsed more negative racial group attitudes, the association was U-shaped, and reporting no racial discrimination was associated with the highest probability of having a history of cardiovascular disease.
Post-Hoc Analyses
The U-shaped association between racial discrimination and history of cardiovascular disease found among participants with high negative racial group attitudes mirror the findings reported by Krieger and Sidney (1996) among working-class African American men. In order to examine whether the association found by occupational class could be explained by internalized discrimination as posited by the authors, we conducted post-hoc analyses examining whether there was an association between racial group attitudes and measures of socioeconomic position. In a weighted linear regression model predicting negative racial group attitudes, we observed that a significant associations with poverty level. Compared to non-poor participants with a poverty ratio of 4.00 or more, those who non-poor with a poverty ratio of 2.00–3.99 (b = 0.46, p = 0.04) and those who were near-poor with a poverty ratio between 1.00–1.99 (b = 0.81, p < 0.001) had significantly higher negative racial attitude scores, and those below poverty with a ratio < 1.00 had the highest scores (b = 0.85, p = 0.005). In another weighted linear regression model, we found that participants with 12 years (b = −0.38, p = 0.02), 13–15 years (b = −0.93, p < 0.001), and 16 years of education or more (b = −1.65, p < 0.001) had significantly lower negative racial group attitudes compared to those with less than 12 years of education.
Discussion
Findings from the current study help to elucidate psychological mechanisms involved in linking racial discrimination and cardiovascular health and describe the nature of this relationship among African American men. In particular, results point to the importance of internalized racism in the form of negative racial group attitudes in relation to explicit experiences of racial discrimination for cardiovascular health (Clark, 2001; Pinel, 1999). Internalized negative racial group attitudes themselves were associated with history of cardiovascular disease, and they moderated the impact of racial discrimination on these outcomes. Specifically, experiences of racial discrimination were associated with worse cardiovascular health outcomes among African American men with lower levels of internalized negative racial group attitudes, particularly among those reporting two situations of racial discrimination. This finding is consistent with biopsychosocial models of health that suggest that experiencing racial discrimination, as a source of psychosocial stress, may have negative cardiovascular implications (Clark, et al., 1999). However, those reporting racial discrimination in three or more situations were at slightly lower risk compared to those reporting racial discrimination in two situations, albeit higher compared to those reporting no racial discrimination. This finding can be viewed as being concordant with psychological perspectives suggesting that attributing negative experiences to racial discrimination may somewhat buffer their negative health effects (Branscombe, et al., 1999; Schmitt & Branscombe, 2002).
In contrast, when examining associations between racial discrimination and cardiovascular disease history among African American men with high levels of internalized negative racial group attitudes, a strikingly different pattern of associations emerged. In this group, those who reported no racial discrimination had the highest risk of having a history of cardiovascular disease. Among African American men, the combination of internalizing negative racial group attitudes and reporting no experiences racial discrimination may be associated the worst cardiovascular health outcomes. Accordingly, internalizing racist beliefs in tandem with the denial of systematic experiences of racial discrimination or may have particularly adverse health consequences. Although provocative, this finding is concordant with prior work suggesting that internalized racism among those reporting no racial discrimination may be associated with worse cardiovascular health. Results are consistent with findings reported by Krieger & Sidney (1996). Post-hoc analyses revealed significant associations between our measures of socioeconomic position and negative racial group attitudes, supporting their interpretation that internalized discrimination may explain the U-shaped association between self-reported racial discrimination and blood pressure found among working-class African Americans, but not among professional African Americans.
A limitation of the present study, as well as of previous studies, is the use of self-reported measures of cardiovascular health history (e.g., Cozier, et al., 2006; Gee, Spencer, Chen, & Takeuchi, 2007; Krieger, 1990). However, as noted previously, prior research suggests that levels of recall accuracy of medical history are high (Colditz, et al., 1986; Harlow & Linet, 1989). In addition, to help address this concern, a variety of socioeconomic variables were controlled for, including health insurance status, as well as two additional health-related variables. Another novelty of this study was controlling for social desirability bias, which is designed to take into account personality factors that could influence responses to sensitive items. Finally, another limitation of this study is the cross-sectional nature of the data, which potentially limits inferences regarding the direction of causality. However, findings are largely concordant with our theoretical framework and are consistent with those of another study (Krieger & Sidney, 1996).
Despite these caveats, results of the current study help to explain prior findings on the relationship between self-reported racial discrimination and cardiovascular health, and importantly, suggest mechanisms that may be involved in the embodiment of racial discrimination among African American men. Future studies may examine additional pathways linking racial discrimination and cardiovascular health, including other psychological factors and dimensions of racial identity as potential moderators (Chae & Yoshikawa, 2008; Sellers & Shelton, 2003). Findings indicate that public health officials should be concerned with racial discrimination in designing programs and developing policies to address disproportionately poor cardiovascular disease burden in this population. Results of this study also notably suggest that the internalization of negative social evaluations of African Americans is harmful for cardiovascular health, even among those who fail to report racial discrimination. In addition to addressing persistent overt forms of interpersonal racial discrimination through the enforcement of anti-discrimination legislation (e.g., in housing and employment), policy makers should also be concerned with the consequences of racism more broadly, including the internalization and acceptance of negative beliefs and perceptions of Blacks (Jones, 2000, 2001). Educational and media campaigns, as well as community-based interventions may be designed to promote a positive racial identity. Findings from the current study encourage public health researchers and practitioners to confront these issues in improving cardiovascular health among African American men.
Acknowledgments
The National Survey of American Life was supported by the National Institute of Mental Health (NIMH; grant U01-MH57716; P.I.: J.S. Jackson) with supplemental support from the Office of Behavioral and Social Science Research at the National Institutes of Health and the University of Michigan. D.H. Chae was supported by the Robert Wood Johnson Health and Society Scholars Program. The preparation of this manuscript was also supported by a grant from NIMH (grant K01-MH69923) for K.D. Lincoln.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
David H. Chae, Email: david.chae@emory.edu, Rollins School of Public Health, Emory University, Atlanta, GA UNITED STATES
Karen D Lincoln, University of Southern California
Nancy E Adler, University of California, San Francisco
S. Leonard Syme, University of California, Berkeley
References
- Aguirre A, Turner JH. American ethnicity: The dynamics and consequences of discrimination. New York: McGraw-Hill; 2004. [Google Scholar]
- Allison PD. Multiple imputation for missing data - A cautionary tale. Sociological Methods & Research. 2000;28(3):301–309. [Google Scholar]
- American Heart Association. [Accessed on November 20, 2007];African Americans and Cardiovascular Diseases – Statistics. 2007 Retrieved from http://www.americanheart.org/downloadable/heart/1168611462350AFAM07.pdf.
- Armstead CA, Lawler KA, Gorden G, Cross J, Gibbons J. Relationship of racial stressors to blood pressure responses and anger expression in black college students. Health Psychology. 1989;8(5):541–556. doi: 10.1037//0278-6133.8.5.541. [DOI] [PubMed] [Google Scholar]
- Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, et al. Racial differences in incident heart failure among young adults. New England Journal of Medicine. 2009;360(12):1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branscombe NR, Schmitt MT, Harvey RD. Perceiving pervasive discrimination among African Americans: Implications for group identification and well-being. Journal of Personality and Social Psychology. 1999;77(1):135–149. [Google Scholar]
- Broman CL. The health consequences of racial discrimination: a study of African Americans. Ethnicity and Disease. 1996;6(1–2):148–153. [PubMed] [Google Scholar]
- Brondolo E, Libby DJ, Denton EG, Thompson S, Beatty DL, Schwartz J, et al. Racism and ambulatory blood pressure in a community sample. Psychosomatic Medicine. 2008;70(1):49–56. doi: 10.1097/PSY.0b013e31815ff3bd. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Rieppi R, Kelly KP, Gerin W. Perceived racism and blood pressure: a review of the literature and conceptual and methodological critique. Annals of Behavioral Medicine. 2003;25(1):55–65. doi: 10.1207/S15324796ABM2501_08. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Berntson GG, Sheridan JF, McClintock MK. Multilevel integrative analyses of human behavior: social neuroscience and the complementing nature of social and biological approaches. Psychological Bulletin. 2000;126(6):829–843. doi: 10.1037/0033-2909.126.6.829. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Racial/ethnic and socioeconomic disparities in multiple risk factors for heart disease and stroke – United States, 2003. Morbidity and Mortality Weekly Report. 2006;54(5):113–117. [PubMed] [Google Scholar]
- Chae DH, Yoshikawa H. Perceived group devaluation, depression, and HIV-risk behavior among Asian gay men. Health Psychology. 2008;27(2):140–148. doi: 10.1037/0278-6133.27.2.140. [DOI] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans - A biopsychosocial model. American Psychologist. 1999;54(10):805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Clark VR. The perilous effects of racism on blacks. Ethnicity and Disease. 2001;11(4):769–772. [PubMed] [Google Scholar]
- Colditz GA, Martin P, Stampfer MJ, Willett WC, Sampson L, Rosner B, et al. Validation of Questionnaire Information on Risk-Factors and Disease Outcomes in a Prospective Cohort Study of Women. American Journal of Epidemiology. 1986;123(5):894–900. doi: 10.1093/oxfordjournals.aje.a114319. [DOI] [PubMed] [Google Scholar]
- Cooley CH. Human nature and the social order. New York: Charles Scriber’s; 1902. [Google Scholar]
- Cooper RS. Social inequality, ethnicity and cardiovascular disease. International Journal of Epidemiology. 2001;30(Suppl 1):S48–52. doi: 10.1093/ije/30.suppl_1.s48. [DOI] [PubMed] [Google Scholar]
- Cozier Y, Palmer JR, Horton NJ, Fredman L, Wise LA, Rosenberg L. Racial discrimination and the incidence of hypertension in US black women. Annals of Epidemiology. 2006;16(9):681–687. doi: 10.1016/j.annepidem.2005.11.008. [DOI] [PubMed] [Google Scholar]
- Crocker J, Major B. Social Stigma and Self-Esteem - the Self-Protective Properties of Stigma. Psychological Review. 1989;96(4):608–630. [Google Scholar]
- Davis SK, Liu Y, Quarells RC, Din-Dzietharn R. Stress-related racial discrimination and hypertension likelihood in a population-based sample of African Americans: the Metro Atlanta Heart Disease Study. Ethnicity and Disease. 2005;15(4):585–593. [PubMed] [Google Scholar]
- Dressler WW. Social identity and arterial blood pressure in the African-American community. Ethnicity and Disease. 1996;6(1–2):176–189. [PubMed] [Google Scholar]
- Eaker ED, Sullivan LM, Kelly-Hayes M, D’Agostino RB, Sr, Benjamin EJ. Anger and hostility predict the development of atrial fibrillation in men in the Framingham Offspring Study. Circulation. 2004;109(10):1267–1271. doi: 10.1161/01.CIR.0000118535.15205.8F. [DOI] [PubMed] [Google Scholar]
- Epel ES, Blackburn EH, Lin J, Dhabhar FS, Adler NE, Morrow JD, et al. Accelerated telomere shortening in response to life stress. Proceedings of the National Academy of Sciences USA. 2004;101(49):17312–17315. doi: 10.1073/pnas.0407162101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esterling BA, Kiecolt-Glaser JK, Bodnar JC, Glaser R. Chronic stress, social support, and persistent alterations in the natural killer cell response to cytokines in older adults. Health Psychology. 1994;13(4):291–298. doi: 10.1037//0278-6133.13.4.291. [DOI] [PubMed] [Google Scholar]
- Fang CY, Myers HF. The effects of racial stressors and hostility on cardiovascular reactivity in African American and Caucasian men. Health Psycholology. 2001;20(1):64–70. doi: 10.1037//0278-6133.20.1.64. [DOI] [PubMed] [Google Scholar]
- Gee GC, Ryan A, Laflamme DJ, Holt J. Self-reported discrimination and mental health status among African descendants, Mexican Americans, and other Latinos in the New Hampshire REACH 2010 Initiative: the added dimension of immigration. American Journal of Public Health. 2006;96(10):1821–1828. doi: 10.2105/AJPH.2005.080085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Spencer MS, Chen J, Takeuchi D. A nationwide study of discrimination and chronic health conditions among Asian Americans. American Journal of Public Health. 2007;97(7):1275–1282. doi: 10.2105/AJPH.2006.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: relationship to cardiovascular reactivity among African American and European American women. Health Psychology. 2001;20(5):315–325. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- Harlow SD, Linet MS. Agreement between Questionnaire Data and Medical Records - the Evidence for Accuracy of Recall. American Journal of Epidemiology. 1989;129(2):233–248. doi: 10.1093/oxfordjournals.aje.a115129. [DOI] [PubMed] [Google Scholar]
- Harrell JP, Hall S, Taliaferro J. Physiological responses to racism and discrimination: An assessment of the evidence. American Journal of Public Health. 2003;93(2):243–248. doi: 10.2105/ajph.93.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeringa SG, Wagner J, Torres M, Duan NH, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) International Journal of Methods in Psychiatric Research. 2004;13(4):221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heffernan KS, Jae SY, Wilund KR, Woods JA, Fernhall B. Racial differences in central blood pressure and vascular function in young men. American Journal of Physiology—Heart and Circulatory Physiology. 2008;295(6):H2380–2387. doi: 10.1152/ajpheart.00902.2008. [DOI] [PubMed] [Google Scholar]
- Helms JE. An update on Helms’ White and people of color racial identity models. In: Ponterorro JG, Casas JM, Suzuki A, Alexander CM, editors. Handbook of Multicultural Counseling. Thousand Oaks, CA: Sage; 1995. pp. 181–198. [Google Scholar]
- Helms JE. Black and White racial identity attitudes: Theory, practice, and research. New York: Greenwood Press; 1990. [Google Scholar]
- Horton NJ, Lipsitz SR, Parzen M. A potential for bias when rounding in multiple imputation. American Statistician. 2003;57(4):229–232. [Google Scholar]
- Huebner DM, Davis MC. Perceived antigay discrimination and physical health outcomes. Health Psychololgy. 2007;26(5):627–634. doi: 10.1037/0278-6133.26.5.627. [DOI] [PubMed] [Google Scholar]
- Jaccard J. Interaction effects in logistic regression. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- Jackson JS, Neighbors HW, Nesse RM, Trierweiler SJ, Torres M. Methodological innovations in the National Survey of American Life. International Journal of Methods in Psychiatric Research. 2004;13(4):289–298. doi: 10.1002/mpr.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, et al. The National Survey of American Life: a study of racial, ethnic and cultural influences on mental disorders and mental health. International Journal of Methods in Psychiatric Research. 2004;13(4):196–207. doi: 10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CP. Levels of racism: A theoretic framework and a gardener’s tale. American Journal of Public Health. 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CP. Invited commentary: “Race,” racism, and the practice of epidemiology. American Journal of Epidemiology. 2001;154(4):299–304. doi: 10.1093/aje/154.4.299. [DOI] [PubMed] [Google Scholar]
- Klonoff EA, Landrine H, Ullman JB. Racial discrimination and psychiatric symptoms among Blacks. Cultural Diversity and Ethnic Minority Psycholoogy. 1999;5(4):329–339. [Google Scholar]
- Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Social Science and Medicine. 1990;30(12):1273–1281. doi: 10.1016/0277-9536(90)90307-e. [DOI] [PubMed] [Google Scholar]
- Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29(2):295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. American Journal of Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethnicity and Disease. 2007;17(1):143–152. [PubMed] [Google Scholar]
- Major B, Kaiser CR, McCoy SK. It’s not my fault: When and why attributions to prejudice protect self-esteem. Personality and Social Psychology Bulletin. 2003;29(6):772–781. doi: 10.1177/0146167203029006009. [DOI] [PubMed] [Google Scholar]
- Marlowe D, Crowne DP. Social Desirability and Response to Perceived Situational Demands. Journal of Consulting Psychology. 1961;25(2):109. doi: 10.1037/h0041627. [DOI] [PubMed] [Google Scholar]
- McClelland GH, Judd CM. Statistical Difficulties of Detecting Interactions and Moderator Effects. Psychological Bulletin. 1993;114(2):376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Mead GH. Mind, self, and society. Chicago: University of Chicago Press; 1934. [Google Scholar]
- Mensah GA. Eliminating disparities in cardiovascular health: six strategic imperatives and a framework for action. Circulation. 2005;111(10):1332–1336. doi: 10.1161/01.CIR.0000158134.24860.91. [DOI] [PubMed] [Google Scholar]
- Merritt MM, Bennett GG, Jr, Williams RB, Edwards CL, Sollers JJ., 3rd Perceived racism and cardiovascular reactivity and recovery to personally relevant stress. Health Psychology. 2006;25(3):364–369. doi: 10.1037/0278-6133.25.3.364. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Archives of General Psychiatry. 1998;55(7):580–592. doi: 10.1001/archpsyc.55.7.580. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 1998 With Socioeconomic and Health Chartbook. DHHS Publication No. 98–1232. 2008 Retrieved from http://www.cdc.gov/nchs/data/hus/hus98.pdf.
- National Center for Health Statistics. Health, United States, 2008 With Special Feature on the Health of Young Adults. DHHS Publication No. 2009–1232. 2009 Retrieved from http://www.cdc.gov/nchs/data/hus/hus08.pdf. [PubMed]
- Pettigrew TF. Social evaluation theory: Convergences and applications. In: Levine D, editor. Nebraska symposium on motivation. Lincoln: University of Nebraska Press; 1967. pp. 241–304. [Google Scholar]
- Pinel EC. Stigma consciousness: the psychological legacy of social stereotypes. Journal of Personality and Social Psychology. 1999;76(1):114–128. doi: 10.1037//0022-3514.76.1.114. [DOI] [PubMed] [Google Scholar]
- Roberts CB, Vines AI, Kaufman JS, James SA. Cross-sectional association between perceived discrimination and hypertension in African-American men and women: the Pitt County Study. American Journal of Epidemiology. 2008;167(5):624–632. doi: 10.1093/aje/kwm334. [DOI] [PubMed] [Google Scholar]
- Romero AJ, Roberts RE. Stress within a bicultural context for adolescents of Mexican descent. Cultural Diversity and Ethnic Minority Psychology. 2003;9(2):171–184. doi: 10.1037/1099-9809.9.2.171. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley and Sons; 1987. [Google Scholar]
- Ryan AM, Gee GC, Laflamme DF. The Association between self-reported discrimination, physical health and blood pressure: findings from African Americans, Black immigrants, and Latino immigrants in New Hampshire. Journal of Health Care for the Poor and Underserved. 2006;17(2 Suppl):116–132. doi: 10.1353/hpu.2006.0092. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. New York: Chapman and Hall; 1997. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- Schmitt MT, Branscombe NR. The internal and external causal loci of attributions to prejudice. Personality and Social Psychology Bulletin. 2002;28(5):620–628. [Google Scholar]
- Schmitt MT, Branscombe NR, Kappen DM. Attitudes toward group-based inequality: social dominance or social identity? British Journal of Social Psychology. 2003;42(Pt 2):161–186. doi: 10.1348/014466603322127166. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: results from a longitudinal analysis. American Journal of Public Health. 2006;96(7):1265–1270. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seaton EK, Caldwell CH, Sellers RM, Jackson JS. The prevalence of perceived discrimination among African American and Caribbean Black youth. Developmental Psychology. 2008;44(5):1288–1297. doi: 10.1037/a0012747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers RM, Caldwell CH, Schmeelk-Cone KH, Zimmerman MA. Racial identity, racial discrimination, perceived stress, and psychological distress among African American young adults. Journal of Health and Social Behavior. 2003;44(3):302–317. [PubMed] [Google Scholar]
- Sellers RM, Shelton JN. The role of racial identity in perceived racial discrimination. Journal of Personality and Social Psychology. 2003;84(5):1079–1092. doi: 10.1037/0022-3514.84.5.1079. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Poverty thresholds 2000. 2007 Retrieved from http://www.census.gov/hhes/poverty/threshld/thresh00.html.
- U.S. Equal Employment Opportunity Commission. Walgreens sued for job bias against Blacks [press release] 2007 March; Retrieved from: http://www.eeoc.gov/press/3-7-07.html.
- Weiner B. An Attributional Theory of Achievement-Motivation and Emotion. Psychological Review. 1985;92(4):548–573. [PubMed] [Google Scholar]
- Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Annals of the New York Academy of Scienes. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites - Results from the National Survey of American Life. Archives of General Psychiatry. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Williams DR, Haile R, Gonzalez HM, Neighbors H, Baser R, Jackson JS. The mental health of Black Caribbean immigrants: Results from the National Survey of American Life. American Journal of Public Health. 2007;97(1):52–59. doi: 10.2105/AJPH.2006.088211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Neighbors H. Racism, discrimination and hypertension: evidence and needed research. Ethnicity and Disease. 2001;11(4):800–816. [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. American Journal of Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethn Health. 2000;5(3–4):243–268. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socioeconomic status, stress, and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]


