Abstract
This study aimed to determine if a joint attention intervention would result in greater joint engagement between caregivers and toddlers with autism. The intervention consisted of 24 caregiver-mediated sessions with follow-up 1 year later. Compared to caregivers and toddlers randomized to the waitlist control group the immediate treatment (IT) group made significant improvements in targeted areas of joint engagement. The IT group demonstrated significant improvements with medium to large effect sizes in their responsiveness to joint attention and their diversity of functional play acts after the intervention with maintenance of these skills 1 year post-intervention. These are among the first randomized controlled data to suggest that short-term parent-mediated interventions can have important effects on core impairments in toddlers with autism. Clinical Trials #: NCT00065910.
Keywords: Joint engagement intervention, Joint attention, Autism
Introduction
Joint attention has been the focus of a number of recent early intervention studies in autism. Joint attention refers to the development of specific skills that involve sharing attention with others through pointing, showing, and coordinating looks between objects and people, as well as the development of attention states that involve mutually sustained joint engagement with others. For children with autism, both joint attention skills and sustained joint engagement are significantly impaired.
Qualitative differences or a complete absence of joint attention often raises a red flag for parents early in the child’s development. Parents notice that their child seems to be happy on his/her own (not jointly engaged), may not respond to his/her name, and may not bring toys to show the parent. Using videotapes of early development, several researchers have noted that infants later diagnosed with autism do not smile and look to others very often, and do not attempt to direct another’s attention (Charman et al. 2003; Osterling and Dawson 1994). Prospective studies of early development also highlight the lack of joint attention and shared positive affect between children who go on to develop an autism diagnosis and their family members (Landa et al. 2007). Although a failure to talk becomes a major benchmark of concern for which parents seek help, the underlying lack of reciprocal engagement and joint attention ultimately are among the most deleterious features of the disability.
Why Develop Joint Attention in Autism?
Joint attention skills are important because the ability to engage others non-verbally (with eye contact, smiles and gestures) and the ability to talk are related. Young children communicate with others long before they actually “talk” with words. Studies of both typically developing children and children with autism find that children who engage the caregiver in sharing communications (e.g., pointing to events or toys of interest, showing toys, and looking between events and people to share interest) acquire language faster (Mundy et al. 1990; Tomasello and Farrar 1986). This is possibly because joint attention skills mark the development of the child’s awareness that other people can see the same objects and/or events that the child sees and regulates attention and affect between self, other, and these events/objects (Bakeman and Adamson 1984; Rheingold et al. 1976; Mundy et al. 1990; Kasari et al. 1990). Given the importance of joint attention skills to language learning, joint attention skills would seem to be an important target of early interventions with young children with autism.
Joint Attention Interventions for Children with Autism
Several recent studies have focused on teaching joint attention to children with autism. These studies vary in the approach used for teaching, in their behavioral targets, and the agent used for changing joint attention. Most rely on an approach that is grounded in applied behavior analysis, and teach skills at a table rather than within naturalistic play settings. Researchers often use an interventionist mediated approach and test outcomes using single subject designs involving a small number of children. Moreover, studies usually target a limited skill set (e.g., one joint attention skill, or only responding skills), and they focus on skills rather than joint engagement states. Thus, there is great variability in studies that all claim to target “joint attention”.
Regardless of this variability, most studies find that they can successfully teach skills to the majority of the children in the study, but that the mastered skills are limited in their generalization to other people or to new contexts. For example, Whalen and Schreibman (2003) demonstrated that an interventionist could teach joint attention skills of pointing and gaze shifting to five preschool children with autism. However, the generalization of the skills to interactions with an untrained adult (the mother) was limited to two of the five children demonstrating joint attention in this context. Other studies note similar effects of the joint attention training with some success in the acquisition of specific targeted joint attention skills but less success in generalization of these skills to mothers or teachers (Jones et al. 2006; Martins and Harris 2006).
There may be several reasons why skills are not generalized. One is that the intervention may teach children joint attention skills in a structured and possibly unnatural context, such as at a table and in response to predictable and contrived stimuli. The child may learn to produce a “joint attention skill” in a “work” situation but is unable to generalize the skills to naturally occurring situations during play or with new people in part because the skill is not integrated into his/her behavioral repertoire. This interpretation would suggest that true learning did not take place. The inability to generalize could also be the result of teaching the child a skill that she/he may not have been developmentally ready to learn. Few studies have carefully tested joint attention skills prior to initiating an intervention, and then used this information to select the skill targeted for intervention. Another possibility is that the generalization context did not offer enough opportunity to demonstrate a joint attention skill (e.g., the person was too directive in their interactions to allow for an initiation from the child). The generalization context is rarely tested for the child’s opportunity to respond to or initiate joint attention.
Joint Attention Interventions for Toddlers with Autism
As clinicians begin to identify younger and younger children with autism, several of the above concerns must be addressed in research designs. Young children are less likely to spend as much time working at tables in highly structured contexts. They also spend more time with parents and less time in school. In addition, infants and toddlers have more limited behavioral repertoires, thus there is a need to carefully address the developmental readiness of children to learn specific joint attention skills. Moreover, mediating the intervention through the parent rather than an interventionist may help in generalizing the learned skills.
For the foregoing reasons, parent-mediated models become an important consideration in teaching joint attention skills to infants and toddlers with autism. Several examples of parent-mediated interventions exist, and similar to therapist-mediated interventions, these studies also vary on a number of factors, including teaching approach, targets for intervention, and dose.
Two parent-training programs were implemented in the UK utilizing relatively low intensity (approximately one visit per month) parent visitation models (Aldred et al. 2004; Drew et al. 2002). In both studies, joint attention skills were addressed in a comprehensive model of social communication but it is unclear how directly joint attention skills or joint engagement was targeted. Using a randomized controlled design in which the experimental intervention was contrasted to a no intervention control, Aldred et al (2004) found significant improvements in social communication outcomes (including joint attention) for the experimental group. Other studies have used single subject designs and focused on parents as the targets of intervention in teaching young children a limited set of joint attention skills (Rocha et al. 2007; Schertz and Odom 2007). Consistent with interventionist-led interventions, most parents were able to improve the joint attention skills that were specifically targeted in their children with autism. Thus, these studies underscore the potential benefit of parent-mediated interventions for teaching joint attention skills. However, similar to therapist-mediated studies, issues in maintenance and generalization of the “learned” skills also exist with only two-thirds of the children maintaining their joint attention skills with their caregiver when tested in a follow up session (Schertz and Odom 2007).
Factors Affecting Intervention Outcomes
These parent-mediated intervention studies have ranged widely in dosage and format; parents received sessions with experimenters in clinics or homes from once a month to several times per week. Depending on the age of the child, and geographical location, parents may or may not be providing the only treatment for their child. Thus, parent training could be an ‘added in’ component of the child’s clinical or preschool program. The intervention services that a child receives outside of the study procedures could influence outcomes in parent-mediated studies. For example, in the Drew et al. (2002) study, children in the control group received a greater number of intervention hours than did the experimental group—perhaps to counter the assignment to the control group. The small sample size of the study contributed to only marginally significant findings, but it may also be that engagement in other interventions worked against the experimental intervention effects. In the current study, we examine the amount and type of services the child received concurrently along with our intervention in order to test whether concurrent services predicted treatment outcomes.
Another factor that may affect children’s outcomes in parent-mediated interventions is the quality of caregiver participation in the treatment. Several studies have found that mere attendance in parent-focused interventions is not enough to predict child treatment outcome; rather, the quality of parental participation appears to make a difference (e.g., Nix et al. 2009). Quality of participation involves more than fidelity to treatment methods, and includes factors such as the parent’s enthusiasm, their confidence, the quality of parent–child sharing, and the completion of homework between sessions. Thus, in the current study, parents’ own ratings of their involvement and ‘buy in’ to the treatment goals as well as the interventionist’s ratings of caregiver quality of participation were examined.
The Current Study
The current study follows from an earlier randomized, controlled trial with 58 preschoolers with autism that was mediated through interventionists in a laboratory setting. This study used a combination of behavioral and developmental procedures, targeted initiations and responses of joint attention skills, facilitated these skills within joint engagement play routines and tested maintenance and generalization of taught skills (Kasari et al. 2006, 2008). Results yielded a number of significant improvements in joint attention skills, play skills, and joint engagement that were generalized to caregivers (Kasari et al. 2006), and that were maintained over a 1-year follow up (Kasari et al 2008).
Results from this study yielded findings that were used to design the current study. In our previous study, skills selected for children were based on their developmental readiness for learning. For example, children demonstrating no joint attention skills were first taught to respond and then to initiate skills, and if they also showed no requesting skills then requesting was taught before joint attention skills. Therefore, in the current study we followed this same approach and individualized our intervention to the developmental readiness of the child. Second, joint engagement achieved through the development of play routines was associated with later language outcomes (Kasari et al. 2008). In the current study, we focused our intervention on the development of play routines in which the adult could follow in on the child’s interests, maintain and then expand upon their play activities. These expansions encouraged longer “topics” in which children had more opportunities to communicate. Finally, because we found that children with the least amount of language benefitted the most from the joint engagement intervention (Kasari et al. 2008) we focused our efforts on toddlers who were expected to have minimal language abilities. We also mediated the intervention through parents since it was unlikely that many children would be in preschool programs; rather the majority of their time would be spent in the care of their parents.
We predicted that (a) compared to a delayed treatment control condition, a targeted intervention for caregivers of toddlers with autism would result in increased joint engagement between caregivers and toddlers and increased child joint attention skills and play diversity, and (b) that changes made during the intervention would be maintained during a follow-up period. A secondary goal was to investigate whether the type and amount of other intervention services and interventionist-rated caregiver quality of participation in the intervention or caregiver-rated adherence and competence predicted treatment outcomes.
Methods
Participants
A total of 42 children were screened for participation in the study from January 2002 to September 2005. Two children did not meet study criteria and two parents declined participation, one for health reasons, and one due to an incompatible work schedule. Active participants included 38 caregivers and their toddlers with autism: 19 caregiver–child dyads in the waitlist control (WL) group and 19 dyads in the immediate treatment (IT) group. The 19 dyads in the IT group were seen for follow-up assessments 1 year later. See Fig. 1.
Fig. 1.
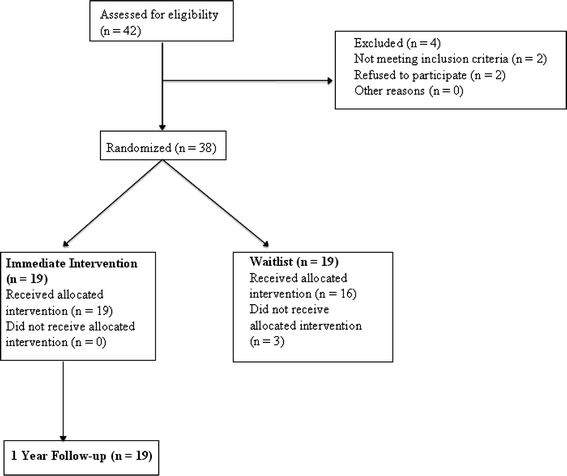
Enrollment and study design
Tables 1 and 2 summarize the background characteristics for both the toddlers and their caregivers who participated in the study. The families were recruited from a large urban city through advertisements posted at local regional centers and early intervention sites. The children ranged in chronological age from 21 to 36 months old with an average age of 30.82 months. The average mental age was 19.2 months. Twenty-nine of the participants were male and nine were female. The sample was diverse with just over 40% of the sample from ethnic minority backgrounds. No exclusions were made based upon gender, ethnicity or developmental age. The large majority of children (83%) were first born or only children. The majority of caregivers had completed college and had graduate or professional training. Caregiver’s average age was 34.5 years. There were no statistically significant differences between IT and WL groups in pretreatment characteristics including child chronological age, mental age, developmental IQ, ethnicity, birth order, or caregiver’s age and education.
Table 1.
Child demographics
| M (SD)/frequency (%) | X 2/F | ||
|---|---|---|---|
| IT (N = 19) | WL (N = 19) | ||
| Gender | |||
| Male | 15 (79%) | 14 (74%) | X 2 (1) = 0.146, p = 0.70 |
| Female | 4 (21%) | 5 (26%) | |
| Ethnicity | |||
| Caucasian | 10 (53%) | 12 (63%) | X 2 (5) = 3.52, p = 0.62 |
| Minority | 9 (47%) | 7 (37%) | |
| Birth order | |||
| Only child | 10 (53%) | 7 (36%) | X 2 (3) = 2.63, p = 0.45 |
| First born | 7 (36%) | 5 (26%) | |
| Second born | 2 (11%) | 2 (11%) | |
| Twin | 0 | 2 (11%) | |
| Missing data | 0 | 3 (16%) | |
| Child chronological age (months) | 30.35 (0.93) | 31.31 (0.90) | F(1,35) = 0.53, p = 0.47 |
| Mullen scales of early learning | |||
| Mental age (months) | 19.83 (1.80) | 18.57 (1.09) | F(1,35) = 0.36, p = 0.55 |
| Developmental quotient | 64.80 (5.35) | 59.81 (3.14) | F(1,34) = 0.61, p = 0.44 |
Table 2.
Parent demographics
| M (SD)/frequency (%) | X 2/F | ||
|---|---|---|---|
| IT (N = 19) | WL (N = 19) | ||
| Caregiver’s age (years) | 34.82 (0.99) | 34.23 (1.11) | F(1,33) = 0.15, p = 0.71 |
| Caregiver’s highest level of education | |||
| Some college/vocational training | 3 (16%) | 2 (11%) | X2 (2) = 1.58, p = 0.45 |
| College | 12 (63%) | 11 (58%) | |
| Professional/graduate | 4 (21%) | 6 (31%) | |
| Caregiver’s employment status | |||
| Not employed | 14 (74%) | 12 (63%) | X2 (1) = 0.504, p = 0.48 |
| Employed part or full-time | 5 (26%) | 7 (37%) | |
Design Overview
A randomized wait list control design was implemented using a random numbers list to assign families to WL or IT groups. Children were randomized using the random numbers method after meeting study criteria. Inclusionary criteria included that the child was younger than 36 months, met criteria for autism following DSM-IV criteria by an independent clinician, and did not have additional syndromes. To validate that children entering the study met the clinical diagnosis of autism, parents were interviewed with the Autism Diagnostic Interview-Revised (Lord et al. 1999). Once study eligibility was determined and randomization occurred, children were then assessed with the Mullen Scales of Early Learning (Mullen 1997), and the caregiver and child were observed playing with each other with a standard set of toys for 15 min. Children who were randomized to the IT group began the 8-week intervention directly after initial assessments. Children randomized to the WL group underwent a waiting period for 8 weeks. The Mullen was not readministered due to the relatively short amount of time (2 months) in the WL condition. The caregiver–child interaction was repeated at the end of IT or WL (8 weeks) and 12 months after intervention was completed (roughly 14 months from entry into active treatment) and the Mullen was repeated at the 12-month follow-up. Additionally, caregiver diaries and caregiver involvement scales were obtained weekly during the 8-week intervention period and are described below.
Primary Outcome Measures
A 15 minute videotaped interaction was collected for each caregiver–child dyad prior to beginning the study, at the start of intervention, at the end of intervention (8 weeks later), and at the 12-month follow-up visit. Caregivers were asked to engage in free play with their child with autism as they normally would at home using a standard set of toys (including dolls, dishes, puzzles, trucks, shape sorter, blocks). The videotapes were coded by reviewers blind to group status and time point scored (pre, post or follow-up) for the percentage of time in engagement states between caregivers and their toddlers with autism (Adamson et al. 2004). Previous research has found this coding system to be reliable, correlates as expected with other measures of social-communication, and sensitive to treatment-related changes (Kasari et al. 2006, 2008).
The child’s activity was segmented into a series of mutually exclusive engagement states that characterize the child’s attention to people and objects. Eleven engagement states were coded and then collapsed into 3 macro categories that served as the primary outcome variables for hypothesis testing: unengaged/other, object engagement, and joint engagement (see Table 3 for definitions). We reduced the number of coding variables given (1) the young mental ages of the children (and expectation of infrequent observations of some codes), (2) the need to reduce the risk of Type I error by limiting multiple comparisons, and (3) precedent in previous studies (Adamson et al. 2004; Kasari et al. 2006; McArthur and Adamson 1996). The play interaction was continuously coded for the predominant state of engagement and a three second decision rule was instituted in order to distinguish clear shifts in engagement states and the lowest quality code took precedence. The codes are mutually exclusive and therefore proportion scores were derived for each engagement state category to represent the relative amount of time children spent in each state.
Table 3.
Engagement state definitions (from Adamson et al. 2004)
| Engagement state | Definition |
|---|---|
| Unengaged/other engagement | Includes unengaged, onlooking and person only engaged. Child may be uninvolved with objects, or unengaged as when scanning the environment. Child may be onlooking by showing one-way awareness of another person in the room. Child may be person engaged by engaging in a song or game without the use of objects |
| Object engagement | Child is actively involved in playing with objects alone, and oblivious to people. The child may be producing language or symbolic gestures, and symbols do not have a clear external referent |
| Joint engagement | Child and partner are actively involved with the same object or event. The child may not overtly acknowledge the partner’s presence, but there is evidence of awareness of partner. Partner must be involved with same object and/or event (supported joint engagement). Or, the child and partner are actively involved with the same object or event, and the child is actively and repeatedly acknowledging the partner’s participation by coordinating his or her attention to both another person and an object or event0 they are sharing (coordinated joint engagement). Symbols or the production or understanding of language may be present in both supported and coordinated joint states |
Independent raters blind to condition and time point calculated reliability for a randomly selected 20% of the tapes. Intraclass correlation coefficients for proportion scores derived from the scoring made by the two independent coders ranged from 0.89 to 0.98.
The child’s play behaviors during the caregiver–child interaction were coded for types of functional and symbolic play acts (Kasari et al. 2006; Lifter et al. 1993). Functional play type refers to the total number of novel, child-initiated functional play acts. These functional acts included simple object manipulation (e.g. pushing a button), combining objects (e.g. puzzles, putting together train tracks), and self and doll directed play (e.g. feeding self or extending a cup to a doll). An example of the functional play type code would be a child who puts a spoon to his mouth several times as if to eat (type 1), and puts a comb to his hair several times (type 2). The number of times the child does each act is irrelevant, but the number of different types would be two. Symbolic play type refers to the total number of different novel, child-initiated symbolic play acts including doll as agent acts (e.g. doll talks and walks), substitutions with objects (e.g. child pretends block is a piece of food), substitutions without objects (e.g. child shakes fist over a piece of bread to simulate a salt shaker), multi-scheme sequences of play (e.g. doll wakes up, eats breakfast and goes to school) and fantasy/sociodramatic play (e.g. child pretends to be a superhero). Previous research has found this coding system to be reliable, valid, and sensitive to treatment-related changes (Kasari et al. 2006, 2008; Lifter et al 1993). Raters who were blind to condition and time point coded children’s individual functional and symbolic play types. The average intraclass correlation coefficient established between two independent coders was 0.84, with a range of 0.60–1.00 for all types of play.
The child’s frequency of joint attention skills was also coded in the caregiver–child interaction, and included initiating joint attention (coordinated looking, pointing to share attention, and showing), and responding to joint attention (responding to experimenter points and gaze). Previous research demonstrates high reliability, validity, and sensitivity to treatment-related changes (Kasari et al. 2006, 2008). We collapsed the frequencies into summary variables of initiating joint attention and responding to joint attention. The overall intraclass coefficient between two independent coders was 0.78 with a range of 0.65–0.95.
Secondary Measures
Caregiver Quality of Involvement
The Caregiver Quality of Involvement Scale is a four-item experimenter report that measures how well the caregivers performed in terms of the quality of strategies learned during the intervention session, and their enthusiasm, confidence and comfort in performing what they had learned. Each item is rated on a 1–5 scale, where scores of (1), (3), and (5) have specific anchors. For example, for parent comfort level, the interventionist would rate whether parents were (1) not comfortable at all (shifting around, looking at interventionist to check, nervous talking/laughter, not touching child much, strained), (3) neutral (does things easily but not really relaxed, some affection with child but may be somewhat hesitant), (5) very comfortable (relaxed, easy movements, affectionate with child, talking freely and easily, smiling).
Experimenters completed the involvement scale at the end of each of the 24 intervention sessions. To assess the overall quality of participation, an average total quality of participation score was calculated using the scores from the 24 sessions. Cronbach’s alpha for the measure is 0.86.
Parent Adherence to Treatment and Competence
A six-item self-report adherence-to-treatment and competence measure was administered to caregivers at the beginning of each week’s intervention session(s). The measure consists of four questions concerning adherence to treatment protocol: (1) made time to carry out the learned strategies, (2) found it complex to carry out the learned strategies, (3) thought it natural to carry out the learned strategies, and (4) made an effort to carry out the learned strategies. The measure also consists of two questions concerning parental competence: (1) was confident carrying out the learned strategies, and (2) was comfortable carrying out the learned strategies. All items consist of a series of ratings on a 5-point scale. Each item was rescaled so that a rating of 5 represented the highest level of parental adherence and competence and a rating of 1 represented the lowest level of parental adherence and competence. Average adherence and competence scores were calculated across the weekly sessions. Cronbach’s alpha for the measure is 0.82.
Service Utilization Measure
The Service Utilization Measure is a five-item parent report that was administered to caregivers at the beginning of the study, and monitored for changes throughout the intervention. Caregivers were asked to list the programs and/or therapies their children were involved in, the type of service that was provided, and the amount of time (in hours per week) their children spent in each as well as their satisfaction with each program and/or therapy.
Joint Attention Intervention
The target intervention was adapted from an earlier intervention with preschool aged children with autism (Kasari et al. 2006, 2008). Core principals of the intervention were developed into 10 modules. The modules were individualized to each dyad so that the beginning point was determined from the initial caregiver–child interaction session. Each dyad completed the modules in the 24 sessions, three sessions per week for 8 weeks.
Trained interventionists (graduate students in educational psychology experienced with children with autism) worked with each caregiver–child dyad. A total of four female graduate students directly intervened with families consisting of roughly 8–9 families per individual interventionist. Training consisted of two pilot subjects with supervision prior to beginning the study and continued supervision in a group format for an hour weekly by the PI throughout the study duration.
Each intervention session included interventionist coaching of caregiver and child engaging in play routines that were established through collaboration between parent and interventionist. The approach involved developmental procedures of responsive and facilitative interaction methods as well as aspects of applied behavior analysis. Principles applied included following the child’s lead and interest in activities, imitating child actions, talking about what the child was doing, repeating back what the child said, expanding on what the child said, giving corrective feedback, sitting close to the child and making eye-contact, and making environmental adjustments to engage the child. Each caregiver–child dyad received approximately 30 minutes of direct instruction, modeling, guided practice, and feedback from the interventionist in each session. Caregivers were presented with handouts that summarized the main objectives of each module. In the last 10 minutes, the caregiver practiced using the techniques learned in that session, and previous sessions.
Fidelity
We rated caregivers’ fidelity in adhering to treatment strategies. Eighteen objectives were established from the 10 treatment modules. From the videotapes pre and post treatment, caregivers were rated on a four-point Likert scale (1–4) for how well they demonstrated each objective or aspect of the treatment protocol. The average intraclass correlation coefficient established between two independent coders on 20% of the tapes was 0.89, range 0.68–0.98.
We also rated the interventionist’s fidelity to treatment protocols using a parallel version of the fidelity measure for caregivers. Twenty percent of each participant’s sessions were rated . The mean intraclass correlation coefficient was 0.86, range 0.74–0.99.
Statistical Analyses
An ANCOVA compared the outcomes of the IT and WL groups to explore if the treatment differed from no treatment. The model included baseline scores and the total number of days either in WL or IT as covariates. A regression analysis was performed to examine the relationship between caregiver quality of involvement, adherence to treatment/competence, and treatment outcomes. All analyses were conducted using SPSS version 16.
Results
Preliminary analyses were conducted to compare the IT and WL groups on pretreatment scores on the primary outcome measures as well as service utilization during the IT and WL period. There were no group differences on the pretreatment scores for the primary outcome measures including engagement states, joint attention or play, nor did service utilization rates differ during the IT and WL period. As noted above, caregivers and interventionists were rated on a 1–4 scale across 18 intervention objectives. Overall, caregivers were rated with high fidelity on treatment objectives at the end of the treatment period. An overall average score of 3.37 (SD = 0.32) was found with a minimum average score of 2.56 and a maximum average score of 3.94.
Primary Analyses: Engagement States, Joint Attention and Play
Children in the IT group engaged in significantly less object-focused play (F(3,34) = 4.45, p < 0.01) and significantly more joint engagement (F(3, 34) = 3.21, p < 0.05) compared to children in the WL group. See Table 4 and Figs. 2 and 3. There was no significant difference between groups for the category of unengaged/other engagement. Children randomized to the IT group showed greater responsiveness to joint attention than the WL group (F(3,34) = 4.06, p < 0.05). Children in the IT group also displayed significantly more types of functional play acts compared to the WL group (F(3,34) = 6.21, p < 0.05). Children in the IT group did not show greater initiations of joint attention or increased diversity of symbolic play compared to children in the WL. Hence, of the primary outcome variables, there was greater improvement for families in IT than WL on two of three joint engagement outcomes, one of two joint attention skill outcomes, and one of two play quality outcome variables.
Table 4.
Means, standard deviations, and ES for IT and WL groups at pre- and post-treatment, and IT at follow-up
| M (SD) | Cohen’s d | |||||
|---|---|---|---|---|---|---|
| IT pre (N = 19) | IT post (N = 19) | WL pre (N = 19) | WL post (N = 19) | IT F-UP (N = 19) | ||
| Unengaged/other engagement | 20.80 (19.03) | 22.01 (18.24) | 19.52 (14.95) | 17.31 (10.17) | 15.87 (13.55) | NS |
| Object engagement | 48.58 (21.87) | 34.75 (18.39) | 54.97 (17.43) | 54.69 (18.15) | 28.35 (15.87) | 1.09 |
| Joint engagement | 30.26 (14.91) | 42.85 (19.96) | 24.98 (10.74) | 27.87 (14.01) | 52.27 (20.56) | 0.87 |
| Frequency of joint attention initiations | 3.0 (2.77) | 3.11 (3.41) | 3.62 (5.92) | 3.77 (3.76) | 4.44 (5.61) | NS |
| Frequency of joint attention responses | 0.42 (0.69) | 0.79 (0.23) | 0.63 (0.23) | 0.05 (0.23) | 0.61 (0.70) | 0.74 |
| Type of functional play acts | 3.00 (2.38) | 5.29 (2.37) | 4.42 (3.17) | 3.29 (2.30) | 8.44 (4.77) | 0.88 |
| Type of symbolic play acts | 0.11 (0.46) | 0.26 (0.65) | 0.42 (0.84) | 0.53 (1.43) | 1.11 (2.37) | NS |
Note. Object and joint engagement are percentages of total time during the mother–child play interaction. Joint attention responses and play acts are frequency counts during the mother–child play interaction
Fig. 2.
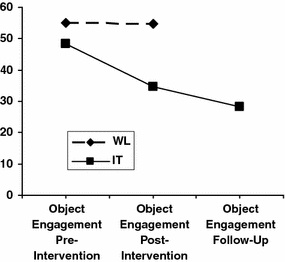
Percent object engagement by group
Fig. 3.
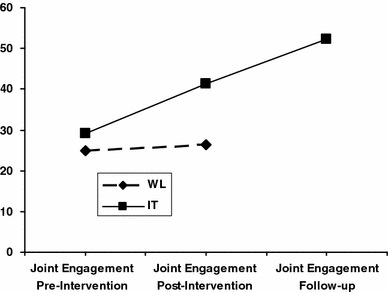
Percent joint engagement by group
We explored whether treatment gains in object and joint engagement states, responsiveness to joint attention, and types of play acts were maintained at the 1-year follow-up visit for the IT group. Similar to other published studies using small data sets (e.g., Wood et al. 2009) we used a paired samples t-test to test for maintenance from posttest to follow up period. The results suggested that maintenance occurred for the states of object engagement, t(18) = 1.07, p > 0.05, and joint engagement, t(18) = −1.67, p > 0.05. In addition, gains during treatment were maintained at the follow-up for responsiveness to joint attention, t(18) = 0.32, p > 0.05. Regarding types of functional play acts, children in the IT group improved in this skill from posttreatment to follow-up, t(18) = −3.34, p < 0.01. Hence, treatment-related gains in joint engagement, joint attention responding skills, and types of functional play acts were either maintained or improved 1 year following termination of the intervention. See Table 4.
Secondary Analyses: Factors Related to Outcome
The average scores on the interventionist-rated Caregiver Quality of Involvement scale and the parent-rated Adherence and Competence scales were examined in relationship to the primary outcome measures. The 19 children in the IT group were included in these analyses. A regression analysis showed that higher Caregiver Quality of Involvement scores significantly predicted increased joint engagement scores at posttreatment after controlling for pretreatment scores, β = 0.49, t(16) = 2.31, p < 0.05. Caregiver involvement was not related to the duration of object engagement or the unengaged/other category in the caregiver–child dyad at posttreatment, nor did it predict increases in play or joint attention skills. See Table 5.
Table 5.
Caregiver quality of involvement and parental adherence to treatment and competence descriptives
| IT | ||||
|---|---|---|---|---|
| Min | Max | Mean (SD) | ||
| Caregiver quality of involvement | Experimenter rating of 4 items: confidence, enthusiasm, comfort, quality | 3.60 | 5.0 | 4.51 (0.41) |
| Parental adherence to treatment | Parent report of 4 items: time, complexity, natural, effort | 2.72 | 5.0 | 3.97 (0.65) |
| Parental competence | Parent report of 2 items: confidence and comfort | 3.27 | 5.0 | 4.35 (0.53) |
Note. A rating of 5 is the maximum score
Neither parent-rated questions regarding adherence and competence predicted level of engagement, type of play or joint attention in the caregiver–child play interaction. Overall, parents reported uniformly high adherence (M = 3.97, SD = 0.65) and competence (M = 4.35, SD = .0.53) ratings on this measure.
Service Utilization
We also examined the amount and type of intervention services that the IT children received during treatment and the WL children received during the waitlist period in relation to the primary outcome measures at posttreatment (controlling for pretreatment scores) as well as parent-reported adherence and competence and caregiver-rated involvement. Total number of hours received during the different types of interventions, school-based instruction, applied behavior analysis (ABA)-based therapies, speech and language therapies or occupational therapies did not significantly predict any of the variables of interest including caregiver involvement, parental adherence, the level of engagement, play type or joint attention seen in the caregiver–child dyad. Descriptive data of service usage can be found in Table 6.
Table 6.
Service usage descriptives
| WL | IT | p Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Min | Max | Mean (SD) | N | Min | Max | Mean (SD) | ||
| ABA hours per week | 6 | 2 | 20 | 11.5 (7.45) | 6 | 2 | 30 | 14.17 (11.04) | 0.63 |
| School hours per week | 13 | 15 | 30 | 21.15 (4.16) | 19 | 4 | 30 | 19.37 (7.59) | 0.45 |
| Speech hours per week | 11 | 1 | 7 | 2.18 (1.66) | 12 | 1.5 | 4 | 2.37 (0.71) | 0.71 |
| OT hours per week | 6 | 1 | 4 | 2.0 (1.10) | 10 | 1 | 6 | 2.20 (1.40) | 0.77 |
| Misc hours per week | 4 | 1 | 12 | 6.5 (5.32) | 8 | 0.5 | 14 | 4.94 (4.81) | 0.62 |
Discussion
The primary goal of this study was to determine if an intervention that taught parents to follow their toddlers’ interest in topics and maintain this interest could improve their toddlers’ social communication outcomes. A major finding was that caregivers implemented the intervention with a high degree of fidelity and helped their toddlers move from primarily object-focused engagement to increased levels of joint engagement between people and objects. Moreover, parents were able to help their children improve in their responding to joint attention and in the diversity of their play. The IT group outperformed the WL group on the majority of primary outcome measures, with generally large effect sizes. These data highlight the importance of joint engagement as a platform for improving child joint attention and play skills.
The two other high-dose studies of direct teaching of parents to improve joint attention in their children with autism (Rocha et al. 2007; Schertz and Odom 2007), both using single subject designs, reported an intervention effect on responding to joint attention. One of the two interventions only taught responding to joint attention (rather than initiating) and all three children improved with intervention and 2 out of the 3 children maintained their skill at a 3 month follow up (Rocha et al. 2007). The other study achieved better responding skills than initiating skills in toddlers, even though initiating skills were directly taught (Schertz and Odom 2007). In the current study, initiations also did not improve significantly although they were directly targeted. Taken together, these findings suggest that initiating joint attention skills may be particularly difficult for children with autism to learn, and perhaps also for parents to develop in their children. These findings are in contrast to our earlier intervention, which was therapist-mediated and delivered more densely (an every-day intervention) (Kasari et al. 2006). Perhaps the expertise of trained clinicians made it possible to achieve changes in initiations, in contrast with the caregiver-mediated model used in this study. On the other hand, an alternate reason for the difference may be the younger age of the children in this study as compared to Kasari et al. (2006) and the possibility that toddlers were ready to learn responding skills, but not yet ready to initiate joint attention skills. Initiating joint attention skills are generally more difficult to demonstrate for children with autism, and likely need longer and more intense interventions (Mundy et al. 1986).
A second main finding was the importance of looking at multiple caregiver factors that could affect treatment outcome. The goal for caregiver-mediated interventions is to increase density of intervention by having parents trained so they can deliver the intervention to their child over the course of every day. If parents do not buy into the intervention or the intervention is too difficult to implement, parents likely will not achieve high fidelity of implementation or adhere to the treatment techniques when on their own. Treatment fidelity has been a longstanding concern with studies finding that when individuals implement interventions with a high degree of fidelity they achieve better treatment success (e.g., Moncher and Prinz 1991). In this study, all parents were able to implement the treatment with high fidelity, and, perhaps due to a restricted range, fidelity was not associated with outcome. However, even with high fidelity, caregivers may not achieve an optimal density of delivery of the intervention, thus reducing the effects of the intervention. In this study, we asked caregivers weekly for feedback on their ability to carry out the intervention, and to tell us how well the intervention strategies fit into their lives. These caregiver self-reports of adherence and competence in delivering the intervention were also high on average, but of course, respondent bias cannot be ruled out (e.g., the demand characteristics of reporting on use of techniques to the study team that taught them could have inflated reports of usage). Thus, these data did not differentiate between caregivers and children who had better or poorer treatment outcomes.
The quality of caregiver involvement in the intervention as rated by the interventionist did predict child outcomes. This measure differentiated caregiver–child joint engagement at the end of treatment, with higher quality of involvement associated with greater joint engagement and less child object-only focused engagement. Thus, even with high fidelity to treatment, and self-reported adherence to the treatment goals, the quality of involvement varied for caregivers, and these differences were associated with an important aspect of child outcome in this study.
Findings for service utilization were nonsignificant. In autism treatment research, a concern is whether children and parents are involved in other treatments and if the dose or content of these interventions are consistent with the goals of the intervention under study. For example, a parent could be learning to deliver a behavioral treatment that is very structured and adult-driven in the home, which could potentially be at odds with an intervention that teaches the parent to engage in a developmental and relationship-based technique. Thus, it is critical that research studies measure dose and type of these additional services. In the current study, toddlers were involved in early intervention, ranging from 9 to 40 hours per week, with no differences between IT and WL groups in dose and types of early intervention services. The services involved mostly ABA/educational services, and speech and occupational therapy. The current treatment study did not coordinate with the child’s service providers and we may have used both an approach and a focus on skills (e.g. joint attention and play) that were quite different from community intervention programs. However, type and amount of additional services did not seem to affect our experimental treatment effects. Future studies might consider whether parent belief in or preference for a particular approach strengthens or lessens the effects of an experimental intervention.
These data, while limited by a small sample size, are promising since they suggest that positive changes can be made in core deficits in young children with autism when intervention is mediated through parents and conducted over an 8-week period. These are among the first randomized controlled data suggesting that a caregiver-mediated intervention can improve aspects of child engagement, joint attention and play skills in toddlers with autism. Most models of early intervention for children with ASD continue to focus exclusively on therapist-mediated models of intervention. Whether a parent mediated model is as effective as a therapist delivered model for toddlers with autism has not been tested. This issue is significant and worthy of further attention since a parent mediated model may prove to be a cost effective way to widely disseminate effective interventions to young children with ASD.
Acknowledgments
This study was supported by NIMH grant MH064927 awarded to Connie Kasari. We thank the parents and children who participated, and the research assistants who contributed countless hours of testing and coding, Eric Ishijima, Leslie Pruitt, Lisa Lee and Grace Cho. We especially appreciate the statistical support of Jeff Wood and Fiona Whalen.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Appendix A: Intervention Procedures and Modules
The child and caregiver met with a trained interventionist for a total of 24 sessions each lasting 45 minutes in length. Sessions were held three times per week for a total of 8 weeks. One module was presented approximately weekly. As new information was presented, the interventionist both modeled and facilitated the information for the caregiver with subsequent sessions used to practice both new and previously learned information. The caregiver–child dyad and interventionist met in a laboratory setting that consisted of a fully stocked playroom.
The modules were presented to caregivers with specific content and examples for how to teach joint attention and symbolic play to their young children with autism. Caregivers received written information corresponding to each module. The module themes are listed below:
- Module 1
Setting up the environment
- Module 2
Allowing the child to initiate an activity
- Module 3
Playing within established routines
- Module 4
Facilitating and maintaining states
- Module 5
Scaffolding an engagement state
- Module 6
Facilitating joint engagement
- Module 7
Allowing the child to initiate communication
- Module 8
Recognizing and responding to the child’s joint attention skills
- Module 9
Imitating and expanding language
- Module 10
Generalizing skills to other routines
During intervention sessions, the caregiver practiced strategies such as following the child’s lead, expanding on emerging play and joint attention skills, and imitating the child and modeling as necessary to keep the child engaged. The goal was to keep the child engaged on the same topic (toy play) for longer periods of time in which child social communication and language behaviors could be facilitated.
References
- Adamson LB, Bakeman R, Deckner DF. The development of symbol-infused joint engagement. Child Development. 2004;75:1171–1187. doi: 10.1111/j.1467-8624.2004.00732.x. [DOI] [PubMed] [Google Scholar]
- Aldred C, Green J, Adams C. A new social communication intervention for children with autism: Pilot randomized controlled treatment study suggesting effectiveness. Journal of Child Psychology and Psychiatry. 2004;45:1420–1430. doi: 10.1111/j.1469-7610.2004.00338.x. [DOI] [PubMed] [Google Scholar]
- Bakeman R, Adamson LB. Coordinating attention to people and objects in caregiver-infant and peer-infant interaction. Child Development. 1984;55:1278–1289. doi: 10.2307/1129997. [DOI] [PubMed] [Google Scholar]
- Charman T, Baron-Cohen S, Sweetenham J, Baird G, Drew A, Cox A. Predicting language outcome in infants with autism and pervasive developmental disorder. International Journal of Language & Communication Disorders. 2003;38:265–285. doi: 10.1080/136820310000104830. [DOI] [PubMed] [Google Scholar]
- Drew A, Baird G, Baron-Cohen S, Cox A, Slonims V, Wheelwright S, Swettenham J, Berry B, Charman T. A pilot randomised control trial of a parent training intervention for pre-school children with autism: Preliminary findings and methodological challenges. European Child and Adolescent Psychiatry. 2002;11:266–267. doi: 10.1007/s00787-002-0299-6. [DOI] [PubMed] [Google Scholar]
- Jones EA, Carr EG, Feeley KM. Mulitple effects of joint attention intervention for children with autism. Behavior Modification. 2006;30:782–834. doi: 10.1177/0145445506289392. [DOI] [PubMed] [Google Scholar]
- Kasari C, Sigman M, Mundy P, Yirmiya N. Affective sharing in the context of attention interaction of normal, autistic, and mentally retarded children. Journal of Autism and Developmental Disorders. 1990;20:87–100. doi: 10.1007/BF02206859. [DOI] [PubMed] [Google Scholar]
- Kasari C, Freeman SF, Paparella T. Joint attention and symbolic play in young children with autism: A randomized controlled intervention study. Journal of Child Psychology and Psychiatry. 2006;47:611–620. doi: 10.1111/j.1469-7610.2005.01567.x. [DOI] [PubMed] [Google Scholar]
- Kasari C, Paparella T, Freeman SF, Jahromi LB. Language outcome in autism: Randomized comparison of joint attention and play interventions. Journal of Consulting and Clinical Psychology. 2008;76:125–137. doi: 10.1037/0022-006X.76.1.125. [DOI] [PubMed] [Google Scholar]
- Landa RJ, Holman KC, Garrett-Mayer E. Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Archives of General Psychiatry. 2007;64:853–864. doi: 10.1001/archpsyc.64.7.853. [DOI] [PubMed] [Google Scholar]
- Lifter K, Sulzer-Azaroff B, Anderson S, Cowdery GE. Teaching play activities to preschool children with disabilities: The importance of developmental considerations. Journal of Early Intervention. 1993;17:139–159. doi: 10.1177/105381519301700206. [DOI] [Google Scholar]
- Lord, C., Rutter, M. L., & LeCouteur, A. (1999). Autism diagnostic interview-revised. ADI-R Short Edition. Developmental Disorders Clinic.
- Martins MP, Harris SL. Teaching children with autism to respond to joint attention initiations. Child & Family Behavior Therapy. 2006;28:51–68. doi: 10.1300/J019v28n01_04. [DOI] [Google Scholar]
- McArthur D, Adamson LB. Joint attention in preverbal children: Autism and developmental language disorder. Journal of Autism and Developmental Disorders. 1996;26:481–496. doi: 10.1007/BF02172271. [DOI] [PubMed] [Google Scholar]
- Moncher FJ, Prinz RJ. Treatment fidelity in outcome studies. Clinical Psychology Review. 1991;11:247–266. doi: 10.1016/0272-7358(91)90103-2. [DOI] [Google Scholar]
- Mullen E. Mullen scales of early learning. Circle Pines, MN: American Guidance Service; 1997. [Google Scholar]
- Mundy P, Sigman MD, Ungerer J, Sherman T. Defining the social deficits of autism: The contribution of non-verbal communication measures. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1986;27:657–669. doi: 10.1111/j.1469-7610.1986.tb00190.x. [DOI] [PubMed] [Google Scholar]
- Mundy P, Sigman M, Kasari C. A longitudinal study of joint attention and language development in autistic children. Journal of Autism and Developmental Disorders. 1990;20:115–128. doi: 10.1007/BF02206861. [DOI] [PubMed] [Google Scholar]
- Nix RL, Bierman KL, McMahon RJ. How attendance and quality of participation affect treatment response to parent management training. Journal of Consulting and Clinical Psychology. 2009;77:429–438. doi: 10.1037/a0015028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterling J, Dawson G. Early recognition of children with autism: A study of first birthday home videotapes. Journal of Autism and Developmental Disorders. 1994;24:247–256. doi: 10.1007/BF02172225. [DOI] [PubMed] [Google Scholar]
- Rheingold H, Hay D, West M. Sharing in the second year of life. Child Development. 1976;83:898–913. [Google Scholar]
- Rocha ML, Schreibman L, Stahmer AC. Effectiveness of training parents to teach joint attention in children with autism. Journal of Early Intervention. 2007;29:154–172. doi: 10.1177/105381510702900207. [DOI] [Google Scholar]
- Schertz HH, Odom SL. Promoting joint attention in toddlers with autism: A parent-mediated developmental model. Journal of Autism and Developmental Disorders. 2007;37:1562–1575. doi: 10.1007/s10803-006-0290-z. [DOI] [PubMed] [Google Scholar]
- Tomasello M, Farrar MJ. Joint attention and early language. Child Development. 1986;57:1454–1463. doi: 10.2307/1130423. [DOI] [PubMed] [Google Scholar]
- Whalen C, Schreibman L. Joint attention training for children with autism using behavior modification procedures. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2003;44:456–468. doi: 10.1111/1469-7610.00135. [DOI] [PubMed] [Google Scholar]
- Wood J, McLeod B, Piacentini J, Sigman M. One-year follow-up of family versus child CBT for anxiety disorders: Exploring the roles of child age and parental intrusiveness. Child Psychiatry and Human Development. 2009;40:301–316. doi: 10.1007/s10578-009-0127-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


