ABSTRACT
OBJECTIVE
To identify the essential components of a mentorship program as the first step in the ongoing development of a mentorship program for primary care physicians.
DESIGN
Mixed-methods study.
SETTING
Saskatchewan.
PARTICIPANTS
Forty-nine of 170 physicians responded positively to a letter of invitation. Of these, 25 physicians were purposively sampled based on location, sex, and experience. Fourteen participants practised in urban areas and 11 in rural settings; 11 were men and 14 were women; and 10 were junior physicians and 15 were senior. Junior physicians were defined as those who had graduated from medical school after 1995, and senior physicians were those who had graduated before 1980.
METHODS
This study employed qualitative, in-depth, semistructured interviews. Interview questions, based on an environmental scan, were developed then pilot-tested with a family physician. Interviews lasted approximately 60 minutes and were audiotaped. Digital audio files were transcribed verbatim and analyzed thematically.
MAIN FINDINGS
Family physicians described positive and negative aspects of mentoring, or having a lack of experience with mentoring. They also outlined key components of a potential mentorship program: matching mentees with mentors; integrating formal and informal mentorship; and the evaluation process of the mentorship relationship and program.
CONCLUSION
Based on the feedback from family physicians, mentorship is viewed as an important and meaningful program of action that regional health stakeholders and medical educators in Saskatchewan could implement. A pilot test of a mentorship program model will be the culmination of this study. Further research will be undertaken to evaluate the model once it is implemented. This will have important implications for establishing a national mentorship program for family physicians across the country.
RÉSUMÉ
OBJECTIF
Identifier les éléments essentiels d’un programme de mentorat comme première étape de l’élaboration courante d’un tel programme pour les médecins de première ligne.
TYPE D’ÉTUDE
Étude par des méthodes variées.
CONTEXTE
La Saskatchewan.
PARTICIPANTS
Sur 170 médecins, 49 ont répondu favorablement à la lettre d’invitation. Parmi eux, 25 ont été retenus pour faire partie d’un échantillon raisonné fondé sur le lieu de pratique, le sexe et l’expérience. Quatorze participants pratiquaient en milieu urbain et 11 en milieu rural; l’échantillon comprenait 11 hommes et 14 femmes, dont 10 médecins juniors et 15 séniors. Les juniors avaient obtenu leur diplôme de médecine après 1995, les séniors, avant 1980.
MÉTHODES
L’étude utilisait des entrevues semi-structurées en profondeur de type qualitatif. Les questions de l’entrevue, choisies à partir d’une enquête sur le milieu, ont été formulées puis testées auprès d’un médecin de famille. Les entrevues d’une durée approximative de 60 minutes ont été enregistrées sur bande magnétique. Les dossiers sonores numérisés ont été transcrits mot à mot et soumis à une analyse thématique.
PRINCIPALES OBSERVATIONS
Les médecins participants ont souligné les aspects positifs et négatifs du mentorat ou déclaré en avoir peu d’expérience. Ils ont aussi indiqué les éléments clés d’un éventuel programme de mentorat : association mentor-mentoré judicieuse, intégration des aspects formels et informels, et évaluation de l’évolution de la relation mentor-mentoré et du programme.
CONCLUSION
Les médecins participants estiment que le mentorat est un programme d’action important et pertinent qui pourrait être instauré par les responsables régionaux de la santé et de l’enseignement médical en Saskatchewan. L’essai pilote d’un modèle de programme de mentorat sera le point culminant de cette étude. Une fois en place, ce modèle devra être évalué par des études additionnelles. Cela aura des conséquences importantes pour la création d’un programme national de mentorat pour les médecins de famille canadiens.
While the number of physicians practising in Canada has risen slightly in the past 5 years, there is a marked shortage of family physicians in some regions.1–11 Saskatchewan is such a region, and counterstrategies are needed to alleviate this trend. The World Health Organization (WHO) indicates that there are no criterion standards with which to assess optimal physician density.12 Nonetheless, the WHO uses the measure of “physicians per 1000 population” to describe global numbers of practising physicians.13 In 2005, Saskatchewan had 0.89 family physicians per 1000 population compared with the national rate of 0.98 family physicians per 1000 population.10 From 2005 to 2007, the Canadian rate remained stable at 0.98 per 1000.9,10 As of December 31, 2008, Saskatchewan had 1010 practising family physicians on its roster, with an estimated population of 1 023 810 people.11,14 The current number of family physicians per capita in Saskatchewan is 0.99 per 1000 population, up from 0.89 in 2005 and up somewhat from the 2007 Canadian national rate of 0.98.9,10 However, as Saskatchewan’s economy remains robust relative to other areas in Canada, the demand for family physicians in Saskatchewan will increase commensurate with continued population growth connected to positive economic development15–17 and to the anticipated medical needs of an aging population.18–20
Nationally, in 2006, 13.2% of Canadians were 65 years of age or older; provincially, in 2006, 14.9% of Saskatchewan’s total population was 65 years of age or older.21 The projected 2031 population estimate for Saskatchewan indicates a 10% increase from 14.9% to 24.9% for that age demographic, and the comparable Canadian figure increases roughly the same amount from 13.2% to 23.4%.21 These projected population estimates were based on census data obtained before Saskatchewan’s dramatic economic upturn and before the province’s population burgeoned. Saskatchewan’s population for 2008 was projected to be 986 90021; in reality it was considerably higher at 1 023 810 people.17 More dire projections forecast Saskatchewan’s population will plummet to 975 800 people by 2031.21 Yet, projections are not predictions; and according to Statistics Canada, Saskatchewan’s provincial population was estimated to be 1 027 092 as of April 1, 2009, higher than the long-term Statistics Canada projections.22
While socioeconomic circumstances (eg, provincial population numbers and income) can shift rapidly, some conditions, such as a population’s rate of aging, are not subject to such rapid reversals.23 The elderly in Canada comprise a growing percentage of the total population, and aging residents require more health services. Kondro points out that physicians themselves are not immune to the passing of time, as the average age of family physicians in 2007 was 48.9 years.9 Further, in Canada, 85.9% of the population had regular medical doctors in 2003; this rate dropped to 84.4% in 2008.24 Correspondingly, in Saskatchewan, the rate of people who reported having regular medical doctors fell from 85.6% (2003) to 82.3% (2008).24 Saskatchewan’s population is increasing faster than was projected, the population is aging, and fewer people have regular physicians. The supply of family physicians per capita in Canada and Saskatchewan is not keeping pace with demand—and that demand is growing.
Physician attrition, fee-for-service payment differentials, physician retirement, low interest in family medicine (recruitment problems), a growing and aging provincial demographic, physician stress and burnout, and the challenges of rural practice have converged to create a “perfect storm” of physician shortages in Canada.1–14,16–41 Rapid changes in the practice of medicine that include an increasing incidence of chronic illness, the adoption of innovative medical information technologies, and the complexity of care further complicate this situation.32,33
Mentorship
Physician mentorship might be a feasible and meaningful strategy to address physician shortages and a declining interest in family medicine.4,5,15,42–48 This article focuses on the qualitative findings of a mixed-methods physician mentorship research program in Saskatchewan. Mentorship implies different things to different people. Implementing a mentorship program can be problematic, depending on how mentorship is imagined, the actors involved in the mentorship process, and the environment in which it is introduced.49 Leslie et al defined mentorship as informal and confidential mentoring to support mentee career development.48 Day and Allen50 and Lankau and Scandura51 described Kram’s52 notable conceptualization of the mentorship process as including career and psychosocial functions. Career functions consist of sponsorship, exposure and visibility, coaching perception, and challenging work assignments; psychosocial functions promote an interpersonal relationship, which includes role modeling, acceptance and confirmation, counseling, and friendship.50–52 Day and Allen outlined the positive effects that mentorship has on career motivation, as it facilitates “self-directedness, career involvement, career success, and positive attitudes toward the protégé’s career.”50 According to Hay, transformational mentoring begins with acknowledgment of mentorship as “a relationship between equals in which one or more of those involved is enabled to: increase awareness, identify alternatives and initiate action, and develop themselves.”53 Traditional mentoring often involves “older, wiser, and senior” mentors who groom younger mentees; there is a hierarchical standard that might value the wise senior above the unversed junior. Transformational mentoring places the mentor-mentee relationship on an even plane; the mentorship partners learn from each other. In this model, not only is knowledge of and expertise in the discipline exchanged, but also the skills of mentoring are honed and passed on. Hay explains that transformational mentoring encompasses more than just sharing expertise and technical know-how. Transformational mentoring taps into the human capacity for inner growth and development.
Studies indicate that recruitment and retention issues can be addressed through education and exposure to family medicine via mentorship. Experienced senior physicians can share knowledge and expertise that might reduce stereotypes about family medicine.27–31,54 As well, mentoring can contribute to ongoing professional development that facilitates a shift to chronic illness management.32,33,42–46 Mentorship has the potential to minimize attrition by increasing physicians’ job satisfaction.5,6,28,36–41 However, mentorship programs for Canadian physicians are conspicuous in their absence.
Our research addresses the gap in knowledge about mentorship from the perspective of family physicians. Using qualitative research methods, this study queried primary care physicians (PCPs) about their mentorship experiences and their suggestions for program development in order to create opportunities for mentorship practices that would be meaningful for physicians as mentors and mentees.55–58 The overarching research goals of the study include the following:
identify the essential components of a mentorship program;
determine what family physicians would be prepared to contribute to a mentorship program; and
develop a mentorship program model based on data collected from family physicians who are either new to practice or who have a number of years of experience.
The focus of this article is on the first goal. Primary care physicians in Saskatchewan were invited to engage in the design of a mentorship program model for PCPs by participating in in-depth interviews.
METHODS
Qualitative techniques explore and reveal participants’ first-hand knowledge of a topic.39,59,60 In this study, we combined a participatory research strategy with an adapted grounded-theory methodology (GTM). Participatory research uses “a dynamic process of action, reflection and collective investigation.”61 The report “Guidelines and Categories for Classifying Participatory Research Projects in Health” defines participatory research as “a systematic inquiry [done in] collaboration [with] those affected by the issue … for purposes of education and taking action or effecting change.”62 This study incorporated these aspects of an adapted GTM and participatory research, as PCPs’ views about mentorship will form the basis of the mentorship model.
Grounded-theory methodology uses a theoretical sampling of participants and emphasizes an inductive process of “constant comparison,” which facilitates integration of a variety of participants’ perspectives.63 Theoretical sampling is a means of identifying significant data “to develop … emerging theory [and to] elaborate and refine the categories … until no new properties arise [and] you saturate your categories with data.”63 An adapted GTM provided tools for the development of the model of a mentorship program, which will be pilot-tested by regional health stakeholders and medical educators in Saskatchewan. Combining a participatory research approach with the adapted GTM strategy ensured that the development of the mentorship survey model included physician input and recommendations drawn directly from physicians’ mentorship experiences.
Procedure
This ongoing mixed-methods study consists of an environmental scan, qualitative interviews with family physicians in Saskatchewan, physician responses to a mentorship model survey, and development of a mentorship model, which will be pilot-tested at the College of Medicine at the University of Saskatchewan in Saskatoon. The first stage of the study included the environmental scan, qualitative interviews, and design and distribution of the mentorship model survey. The next stage of the program included analysis of the survey and development of the model. The environmental scan featured a systematic literature review of the terms physicians and mentorship, mentorship and health, mentor and doctor, and research mentorship. Another component of the scan included online searches of provincial and territorial departments of health and colleges of medicine in New Brunswick, Nova Scotia, Ontario, Manitoba, Saskatchewan, Alberta, and British Columbia. Data from the scan guided the formulation of in-depth, semistructured interview questions for physicians.
An invitation to participate was sent to 170 physicians with faculty appointments in the Department of Medicine at the University of Saskatchewan. Forty-nine physicians responded to the invitation, and 25 of them were purposively sampled based on location, sex, and years of experience. Fourteen were urban physicians and 11 were rural; 11 were men and 14 were women; and 10 were junior faculty and 15 were senior. Senior physicians were defined as those who graduated from medical school before 1980, and junior physicians were those who graduated after 1995. Family physicians who participated in this research project received 4 Mainpro-M1 credits from the Saskatchewan College of Family Physicians, as the study met the accreditation criteria for continuing education as defined by the College of Family Physicians of Canada. Participants also received honoraria in recognition of their time.
The study was approved by the University of Saskatchewan’s Research Ethics Board. All identifying information was removed from the data and pseudonyms were attached to each transcript file. Written data are kept in locked cabinets in locked offices at the University of Saskatchewan. Audio, transcript, and NVivo 864 computer files are kept on a password-protected computer.
Semistructured interview questions, generated from information collated during the environmental scan, were pilot-tested with a family physician. Each interview was approximately 60 minutes long; and interviews were audiotaped and transcribed verbatim. Thematic codes and a standardized coding structure were created using NVivo 8.64 Categories, or themes, were identified via thorough reading of transcripts. The coding structure was initially developed by the research assistant who conducted the interviews. The interview guide was adapted during interview analysis in order to refine interview questions and create “novel questions” based on “constant comparison” of participant views.63 Discussion between 2 researcher team members and the research assistant provided additional verification and trustworthiness of the coding structure, codes, and categories (or themes). The interview sample size (n = 25) is consistent with Charmaz’s discussion regarding the criteria for category saturation for analysis of data from a small group.63 After the completion of 25 interviews, and concurrent and cumulative data analysis, the team believed that saturation was achieved.
Interviews revealed details of physicians’ experiences with and understanding of mentorship. An aggregate mentorship model survey (Figure 1) was developed as a visual representation of the attributes and processes of initiating and maintaining a mentorship protocol. The mentorship model survey was sent to the 49 physicians who originally responded to the letter of invitation. The survey questions, which were derived from the interviews, provided physicians with a selection of configurations to choose from. This study is ongoing, and quantitative data gathered from the survey and physician responses will be used to design a mentorship program model for use in the pilot program.
Figure 1.
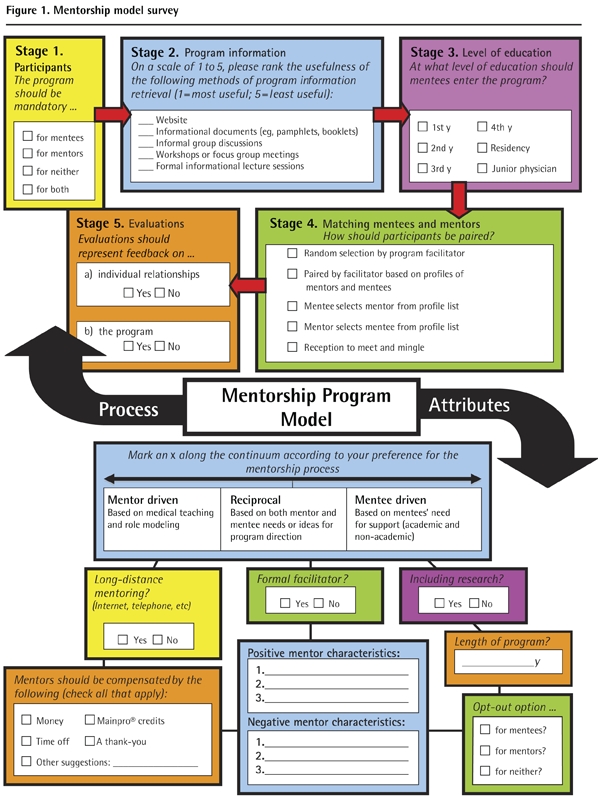
Mentorship model survey
FINDINGS
This part of our research focuses on physician mentorship experiences and on program conceptualization and development. Physician responses identified positive and negative aspects of mentoring or a complete lack of mentorship opportunities. Program development suggestions centred on matching mentors and mentees, integrating formal and informal relationships, and determining the process for evaluating mentorship relationships.
Experiences with mentorship
Many physicians’ experiences highlighted the importance of the mentorship role and described positive experiences with mentorship:
My mentor in family medicine … was a true gentleman, the typical, stereotypical family physician. He was kind and gentle. I was fortunate to do my family medicine training under him. I learned lots from him.
(MRS24)*
A physician spoke positively of her role as a mentor, even though she was at a distance from the physician she mentored:
[My mentee] just knew … where to find me, and she knew I was a source of information she could trust, and she knew I wouldn’t mind being called and it would be a quick 3-minute mentoring experience and it was thousands of miles away.
(FUS2)
Positive mentorship experiences also involved a sense of being “excited” about primary care (noted by MRS12). Further, mentorship did not always involve a formal relationship. One participant described someone who supported her work: “She was just a good person. And I learned a lot from her. But I didn’t have a specific mentor medically.” (FRS15)
Other participants spoke of negative experiences with mentorship: “I remember having an anti-mentor …. He was so unhappy about his work and expressed that to us as students and that was the reason I didn’t go into internal medicine.” (FUJ19) Another physician also used the concept of the “anti-mentor” to describe her experiences:
And it’s been hit and miss, and you’re just darn lucky if you found someone that was really a terrific mentor to you, just really lucky. And lots of people don’t have that at all. They don’t have anybody. In fact they have sort of a negative mentor … anti-mentors who make you feel awful and can actually scar you for life and your confidence is in the toilet. And you only get your confidence back after you’ve been practising for a while and realize that “Gee, I can do this. They were wrong. I can do this.” Boy, it takes a long time to dig yourself out of that hole if you were given a really bad experience.
(FUJ22)
While physicians commented on positive and negative mentorship experiences, some physicians described a lack of availability of mentors and clearly felt the absence of a mentor:
I started here as junior faculty … I asked actually if there is an opportunity to get a mentor … lots of times, I’ve been disappointed. I’ve needed help, I needed to talk to someone, but it wasn’t there. So I think it’s a good thing to have someone.
(FUJ20)
One physician addressed both the lack of mentorship and the need for it:
I think a lot of people come out of medical school feeling pretty rough, and it’s really nice to have someone along the way, giving you gentle encouragement, and I think a lot of people miss out on that. We don’t get a lot of that in med school.
(FUJ22)
Program development
Based on their experiences with mentorship, physicians had a number of suggestions related to the development of a mentorship scheme and program model.
Matching mentors and mentees
Opinions differed about the appropriate methods for matching mentors and mentees (or vice versa). The interviewer suggested several matching options to the physicians (Figure 1): random selection by the program facilitator; pairing by the facilitator based on profiles of mentors and mentees; mentee selection of mentor from a profile list; mentor selection of mentee from a profile list; and a reception to meet and mingle. Random assignment of a mentor to a mentee was often seen as problematic. But one physician stated that a randomly assigned mentor would be better than none at all:
Assigning a mentor, I think, is a problem, but it does give mentees an idea of, hey people are there to help you, and people who sign up for faculty advising or student advising usually want to help. So they get to meet a helpful person. They may learn how to work with somebody who’s already in the field, act as a role model, act as a friend, act as a guide, a guide through life, or a guide through their professional career.
(FUS17)
In contrast to random assignments, it was suggested that mentors and mentees could create personal profiles that included information pertaining to family medicine interests, hobbies outside of work, ideal sorts of practice settings, and desirable mentor or mentee traits. A mediator could act as a liaison between mentors and mentees to complete the matching process. Some physicians did not think this was workable, as potential mentors might “not look good on paper” even if they possessed positive mentorship qualities.
A reception was also suggested as a venue for facilitating the matching process. Mentors and mentees could meet, and mentees would note their top 3 choices on a form. As before, a mediator would facilitate the matching process. Some physicians preferred this plan over profile matching:
Well, I actually like the idea of meeting … rather than a match process quite honestly … because learning styles are so unique and teaching styles are so unique. I’ve done a lot of teaching … and I’ve had students where we connected immediately and it became a mentorship, and I’ve had others where we didn’t connect at all. So, maybe that kind of personal opportunity to interact gives you some idea of whether this is gonna work or it isn’t.
(FUS2)
Concerns expressed around this type of reception included issues of time, shyness, and the potential for the matching process to devolve into a “popularity contest” between mentors and mentees. One physician suggested offering several modes of matching to accommodate to the different personal and professional styles of the individuals involved.
Formal and informal aspects of the program
Formal and informal aspects of the program were discussed. The interviewer asked if physicians envisioned the process generally to be formal or informal or if specific components of the program could be formal, informal, or both. Several physicians viewed mentorship as a formal process. A senior physician said, “I would say the biggest portion of mentorship I see is a formal training program.” (MRS24)
Similarly, a junior physician stated, “I think it’s important to have some formal discussion established beforehand that this … will take place once a week.” (MRJ14)
Other physicians thought mentorship could be informal:
I think you have to sort of differentiate mentoring from preceptoring. Preceptoring is sort of a formal teaching role with more formal expectations. “I’m going to teach you something. I’m going to evaluate you.” While the mentoring, I think of more as socialization into the roles of the professional.
(MUS11)
Another senior physician recalled her previous experiences: “Well in my case [mentorship has] certainly been all informal. There was never any kind of formal thing. I don’t know how you would do it formally.” (FUS22) Thus, the interviewees indicated there is need to integrate both formal and informal components into a mentorship program.
Evaluating the relationship
Analysis of interview data indicated that evaluation was an important but controversial component of any mentorship relationship and program. Physicians who supported an evaluative process noted both potentially negative and positive aspects. Evaluation would represent feedback on specific relationships, the entire program, or both. Viewpoints differed regarding whether the evaluations would be confidential (eg, accessible only to the mentor and mentee), or if collected evaluations would be analyzed by someone or some group external to the process. For example, some physicians thought that evaluation of those being mentored (ie, the mentees) should not be included in the process. One participant said that evaluation was the role of the faculty advisor, not of a mentor:
I mean, as a faculty advisor, we are supposed to look after the educational needs of that resident and make sure that they are on track, and that’s sort of your advocate, as a resident, when it comes to evaluations. Your faculty advisor will talk for you or speak for you or help you, steer you a little bit. I still think mentorship is something else, and that faculty advisor is more a formal process that’s recommended or that’s part of the residency program.
(MRJ10)
A junior physician who was against evaluation within the mentorship program explained the following:
I think it’s better not to be [evaluated as a mentee] because that gives more confidence to the trainee to trust the person. If you’re thinking that person’s going to evaluate you, you’re always thinking maybe the stuff that you are confessing or admitting to may affect their judgment. It’s so difficult to, uh, establish that trust.
(FUJ20)
Other physicians spoke about the need for a process that would evaluate the mentors’ abilities. A senior physician (FUS17) stated that mentors should be evaluated according to whether or not they were knowledgeable, organized, and able to establish rapport and accessibility.
Other participants suggested that program evaluation, rather than evaluation of individuals, was key:
Without some process of evaluating, I don’t know how you can adequately learn, ensure that you’re doing what you’re supposed to be doing as a mentor, and also ensure that whoever’s learning with you is getting what they need out of the experience.
(MRJ14)
Thus, the issue of evaluation in mentorship was complex and there was no clear consensus on the most suitable approach.
DISCUSSION
All participants supported the development of some form of mentorship program. Their responses reflected the definitions of mentorship by Leslie et al,48 Hay,53 and Kram.52 Leslie et al describe informal and confidential mentoring that supports mentee career development.48 Career development was reflected in the response of one physician, who explained that the mentor had fostered a feeling of “excitement” about primary care. Another physician commented that mentorship could provide “gentle encouragement” after the rigours of medical school. These observations bring to mind Hay’s concepts of mentorship, which incorporate career development and personal growth.53 Kram’s description of the career and psychosocial functions of mentors highlight the 2-fold functions of mentoring.52
Physicians, as professionals who deal with humanity in life-and-death situations, are increasingly called upon to treat not only physical symptoms but also the whole person. Training in the biomedical sciences might not adequately prepare physicians for the immediacy of patient-doctor relationships. Knowing that a mentor is accessible for support, guidance, and expertise can ease the concerns of physicians who need the “gentle encouragement” that goes beyond the scope of professional competency. This relationship is an opportunity for mentors to reaffirm personal commitment to their vocation. The benefits and consequences of investing energy in treating patients holistically might come with a cost, and by having a mentor, a physician can have a “friend … a guide through life, or a guide through their professional career.” Career development, for professional health workers, includes more than ongoing technical education that ensures competent execution of medical procedures; as such, the need for collegiality and peer support through mentorship is apparent.
Confidentiality was a concern mentioned by some physicians with respect to evaluation of mentees, mentors, and the program. Confidentiality would enhance trust between mentorship partners; mentees are less likely to bond with mentors if evaluation occurs (of the mentee, the mentor, or the program) during the mentorship process. Further, Leslie et al discuss the “evaluative role” as a potential barrier and that the notion of mentee evaluation might negatively affect mentee confidence.48 This is not to say that evaluative functions are not a necessary part of a mentorship relationship, as program development is informed by members’ feedback. Monitoring of program delivery and fine-tuning programs to specific mentor and mentee needs depend on user input, and all participants have a stake in making the program a good “fit” for everyone involved. Any program model requires inclusion of both formal and informal dimensions to allow for trust-building and to facilitate program growth and evolution. Transparency, accountability, and maintenance of high standards of professional conduct are foundational aspects that underline the mentor-mentee process, and evaluations keep that process viable and dynamic. Confidential feedback protocols would protect both mentees and mentors.
Day and Allen’s50 discussion of the beneficial effect of mentoring upon career motivation is clearly expressed in the view of one physician who responded that his mentor kept him excited about primary care. To avoid negative experiences like the one participant’s encounter with an “anti-mentor,” careful attention must be paid to matching criteria and protocols as key aspects of program design. Hay’s concept of equality is important when contemplating matches and for fostering the mentee-mentor relationship.53 Kram’s career functions are in line with formal mentoring and might include filters that ensure appropriate mentor knowledge and accessibility.52
The emergent nature of GTM and the principles of participatory research furnished us with the desired breadth of data for the preliminary findings presented in this paper. In this study, the use of an adapted GTM allows for an inductive process of “constant comparison” and integration of a variety of physician perspectives.63 Further, this combined research method reflects the guidelines for participatory research in health in that it is “a systematic inquiry [done in] collaboration [with] those affected by the issue … for purposes of education and taking action or effecting change.”62 This study incorporates the aspects of an adapted GTM and participatory research. Primary care physicians’ views about mentorship being an extension of and change to current medical education models generated the development of the survey (Figure 1), which will be the foundation of the final program.
The variety of perspectives offered by participants illustrates the importance of considerable and ongoing collaborative dialogue with physicians in the development of a mentorship program. Critical assessment of the needs and preferences of PCPs with respect to mentorship are inherent to the creation of a useful and successful program. Our subsequent analysis of survey material, pooled with the qualitative data presented in this paper, will ensure that the forthcoming mentorship program model will be consistent with the expressed needs and interests of physicians in Saskatchewan. Developing such a program requires careful consideration of both the roles and responsibilities of mentors and mentees across several dimensions: matching mentors and mentees; integrating formal and informal components to the program; and determining the evaluation process of the various program elements, including the relationships.
As a result of the qualitative data analysis presented in this article, our team developed a survey in order to reach a wider sample of physicians. Like any qualitative research, the initial phase did not seek generalizability.38 Rather, we sought a diversity of ideas and perspectives knowing that we could reach a wider sample if necessary in the follow-up, quantitative phase. Analysis of the quantitative data will provide us with a broader sense of where consensus might be reached, while still relying on the ideas put forward by the family physicians themselves. Additional research into the experiences of family medicine residents could also inform such a program. Reaching this population constitutes a further phase of our team’s program of research into mentorship.
Conclusion
This multiphase project, which is ongoing and in collaboration with several stakeholders, seeks to develop a practicable mentorship program model for PCPs in Saskatchewan. Extended objectives include a national mentoring program designed from the pilot study.
Family physicians spoke about the definite need for a mentorship program and were able to identify key components for future discussion and refinement. The qualitative findings were used to generate a survey, the responses to which can be readily integrated in the development of a mentorship model and the eventual pilot testing of a mentorship program.
Acknowledgments
Funding for this study was supplied by the Saskatchewan Health Research Foundation.
EDITOR’S KEY POINTS
Physician mentorship might be a feasible and meaningful strategy to address physician shortages and a declining interest in family medicine.
Developing the model for a mentorship program for primary care physicians in Saskatchewan is a multi-phase and ongoing project. The focus of this article is to identify the essential components of a mentorship program.
Matching mentees with mentors, integrating formal and informal aspects of a mentorship program, and determining the process for evaluation of the relationships and program were the key components family physicians outlined for a mentorship program.
POINTS DE REPÈRE DU RÉDACTEUR
Un mentorat pour les médecins pourrait être une stratégie réalisable et pertinente pour réagir à la pénurie de médecins et à la perte d’intérêt pour la médecine familiale.
L’instauration d’un programme de mentorat pour les médecins de première ligne en Saskatchewan est un projet en développement qui comporte plusieurs étapes.
Selon les participants, les éléments-clés d’un tel programme sont : bien apparier mentor et mentoré, intégrer les aspects formels et informels du programme et établir le processus d‘évaluation de la relation et du programme.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and the writing and editing of this article.
Competing interests
None declared
Interviewee pseudonyms indicate the following: sex (male [M], female [F]), location of practice (urban [U], rural [R]), experience (senior [S], junior [J]), and a unique number.
References
- 1.College of Family Physicians of Canada, Canadian Medical Association, Royal College of Physicians and Surgeons of Canada . National Physician Survey 2007. Mississauga, ON: College of Family Physicians of Canada; 2007. Available from: www.nationalphysiciansurvey.ca/nps/2007_Survey/2007nps-e.asp. Accessed 2010 May 6. [Google Scholar]
- 2.Future Canadian physicians will bring changes to health care [news release] Ottawa, ON: National Physician Survey; 2008. Apr 28, Available from: www.nationalphysiciansurvey.ca/nps/news/PDF-e/NPS%20-%20Student%20and%20resident%20media%20release.pdf. Accessed 2010 May 6. [Google Scholar]
- 3.Sullivan P. No quick fix for wait times. MDPulse. 2008. pp. 27–30. Available from: www.nationalphysiciansurvey.ca/nps/MDPulse08/10-MDPulse08_sec2-waittimes.pdf. Accessed 2010 May 7.
- 4.Wilson CR. Access for all. Can Fam Physician. 2007;53:2217, 2218. (Fr). Eng. [PMC free article] [PubMed] [Google Scholar]
- 5.Andrews H, Biggar S, Byers D, Davies L, Everett G, Jenkins T, et al. Across Canada. Nat Rev Med. 2007;4(19) Available from: www.nationalreviewofmedicine.com/across_canada/2007/ac4_issue19_nov15-30.html. Accessed 2010 May 7. [Google Scholar]
- 6.CBC News [website] Toronto, ON: CBC; 2008. Tories survive another confidence vote, MPs vote in favour of Bill CV-150. Available from: www.cbc.ca/canada/story/2008/06/09/immigration-vote.html. Accessed 2010 May 7. [Google Scholar]
- 7.Bueckert D. No quick fix in sight for Canada’s shortage of doctors, study finds. Canadian Press. 2003. Mar 19,
- 8.Hodge R. The evolving role of the primary care physician. Physician Exec. 1994;20(10):15–8. [PubMed] [Google Scholar]
- 9.Kondro W. Trends in the profile of the Canadian physician pool. CMAJ. 2009;180(3):284. doi: 10.1503/cmaj.081959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kondro W. Trends in the physician supply. CMAJ. 2006;175(11):1362. doi: 10.1503/cmaj.061434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Government of Saskatchewan [website] Regina, SK: Government of Saskatchewan; 2010. Physician recruitment strategy. Available from: www.gov.sk.ca/adx/aspx/adxGetMedia.aspx?mediaId=810&PN=Shared. Accessed 2010 May 7. [Google Scholar]
- 12.World Health Organization [website] World Health statistics 2009. Geneva, Switz: World Health Organization; 2009. Available from: www.who.int/whosis/whostat/2009/en/index.html. Accessed 2010 May 7. [Google Scholar]
- 13.Dal Poz MR, Kinfu Y, Dräger S, Kunjumen T. Counting health workers: definitions, data, methods, and global results. Geneva, Switz: World Health Organization; 2006. Available from: www.who.int/hrh/documents/counting_health_workers.pdf. Accessed 2010 May 7. [Google Scholar]
- 14.Government of Saskatchewan [website] Census and population. Regina, SK: Government of Saskatchewan; 2010. Available from: www.stats.gov.sk.ca/pop/. Accessed 2010 May 7. [Google Scholar]
- 15.Statistics Canada Study: resource boom in Saskatchewan and Newfoundland and Labrador. The Daily. 2008. May 15, Available from: www.statcan.ca/Daily/English/080515/d080515b.htm. Accessed 2010 May 7.
- 16.Wyman D. From lagging to leading: Newfoundland and Saskatchewan dig into the resource boom. In: Statistics Canada, editor. Canadian economic observer, May 2008. Ottawa, ON: Statistics Canada; 2008. Catalogue No. 11-010-XIB. Available from: www.statcan.gc.ca/pub/11-010-x/11-010-x2008005-eng.pdf. Accessed 2010 May 7. [Google Scholar]
- 17.Saskatchewan to lead in growth. Diversified resource mix helping to buffer downturn, says BMO economist. Saskatoon StarPhoenix. 2009. Jan 15, Sect.C:5.
- 18.Wojszel ZB, Bien B, Politynska B. The assessment of the functional state of elderly people by family physician with the help of EASY-Care questionnaire [article in Polish] Pol Merkur Lekarksi. 1999;6(33):167–70. [PubMed] [Google Scholar]
- 19.Béland F, Bergman H, Lebel P, Dallaire L, Fletcher J, Contandriopoulos A, et al. Integrated services for frail elders (SIPA): a trial of a model for Canada. Can J Aging. 2006;25(1):5–42. [PubMed] [Google Scholar]
- 20.Iliffe S. Family medicine in an aging society. Can Fam Physician. 2009;55:463–4. 466–7. Eng. (Fr). [PMC free article] [PubMed] [Google Scholar]
- 21.Statistics Canada . Population projections for Canada, provinces and territories. 2005–2031. Ottawa, ON: Statistics Canada; 2005. Catalogue No. 91-520XWE. Available from: www.statcan.gc.ca/pub/91-520-x/91-520-x2005001-eng.pdf. Accessed 2010 May 7. [Google Scholar]
- 22.Government of Saskatchewan [website] Saskatchewan population report— Quarter 1, 2009. Regina, SK: Government of Saskatchewan; 2009. Available from: www.aeel.gov.sk.ca/1st-quarter-2009-population-report. Accessed 2010 May 10. [Google Scholar]
- 23.College of Family Physicians of Canada . Family medicine in Canada. Vision for the future. Mississauga, ON: College of Family Physicians of Canada; 2004. Available from: www.cfpc.ca/local/files/Communications/Health%20Policy/FAMILY_MEDICINE_IN_CANADA_English.pdf. Accessed 2010 May 10. [Google Scholar]
- 24.Statistics Canada [website] Population with a regular medical doctor, by sex, provinces, and territories (percent) Ottawa, ON: Statistics Canada; 2010. Available from: www40.statcan.ca/l01/cst01/health76b-eng.htm. Accessed 2010 May 10. [Google Scholar]
- 25.Wright B, Scott I, Woloschuk W, Brenneis F, Bradley J. Career choice of new medical students at three Canadian universities: family medicine versus specialty medicine. CMAJ. 2004;170(13):1920–4. doi: 10.1503/cmaj.1031111. Erratum in: CMAJ 2004;170(11):1327. Erratum in: CMAJ 2004;171(3):222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Campos-Outcalt D, Midtling JE. Family medicine role models at US medical schools. Why their relative numbers are declining. Arch Fam Med. 1993;2(8):827–32. doi: 10.1001/archfami.2.8.827. [DOI] [PubMed] [Google Scholar]
- 27.Ivers NM, Abdel-Galil R. Marketing family medicine. Challenging misconceptions. Can Fam Physician. 2007;53:793–4. 796–7. Eng. (Fr). [PMC free article] [PubMed] [Google Scholar]
- 28.Scott I, Gowans MC, Wright B, Brenneis F. Why medical students switch careers. Changing course during the preclinical years of medical school. Can Fam Physician. 2007;53:94–5. Available from: www.cfp.ca/cgi/reprint/53/1/94. Accessed 2010 May 10. [PMC free article] [PubMed] [Google Scholar]
- 29.Olchanski V, Marsland DW, Rossiter LF, Johnson RE. Behind the physician licensure numbers: false impressions, retirement crisis, and migration. Clin Perform Qual Health Care. 1998;6(3):142–6. [PubMed] [Google Scholar]
- 30.Results from the 2002 Physician Resource Questionnaire. CMAJ. 2002;176(5) Available from: www.cmaj.ca/cgi/content/full/167/5/521/DC1. Accessed 2010 May 10. [PMC free article] [PubMed] [Google Scholar]
- 31.Ginzburg VE. Feeding stereotypes [Letters] Can Fam Physician. 2007;53:812. author reply 812–3. [PMC free article] [PubMed] [Google Scholar]
- 32.Bury M. Illness narratives: fact or fiction? Sociol Health Illn. 2001;23(3):263–85. [Google Scholar]
- 33.Sullivan M. The new subjective medicine: taking the patient’s point of view on health care and health. Soc Sci Med. 2003;56(7):1595–604. doi: 10.1016/s0277-9536(02)00159-4. [DOI] [PubMed] [Google Scholar]
- 34.Evans J, Lambert T, Goldacre M. GP recruitment and retention: a qualitative analysis of doctors, comments about training for and working in general practice. Occas Pap R Coll Gen Pract. 2002;(83):iii–vi. 1–33. [PMC free article] [PubMed] [Google Scholar]
- 35.Evans C, Jones R. Really making it happen in Wiltshire: the experience of service users evaluating social care. In: Lowes L, Hulatt I, editors. Involving services users in health and social care research. New York, NY: Taylor and Francis Inc; 2005. pp. 132–9. [Google Scholar]
- 36.Macaulay AC, Commanda LE, Freeman WE, Gibson NJ, Freeman W, McCabe M, et al. Participatory research maximizes community and lay involvement. BMJ. 1999;319(7212):774–8. doi: 10.1136/bmj.319.7212.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ramsden V, Cave A. Participatory methods to facilitate research. Can Fam Physician. 2002;48:548–9. [PMC free article] [PubMed] [Google Scholar]
- 38.Pathman DE, Konrad TR, Agnew CR. Studying the retention of rural physicians. J Rural Health. 1994;10(3):183–92. doi: 10.1111/j.1748-0361.1994.tb00228.x. [DOI] [PubMed] [Google Scholar]
- 39.Pathman DE, Williams ES, Konrad TR. Rural physician satisfaction: its sources and relationship to retention. J Rural Health. 1996;12(5):366–77. doi: 10.1111/j.1748-0361.1996.tb00804.x. [DOI] [PubMed] [Google Scholar]
- 40.Randall CS, Bergus GR, Schlechte JA, McGuinness G, Mueller CW. Factors associated with primary care residents’ satisfaction with their training. Fam Med. 1997;29(10):730–5. [PubMed] [Google Scholar]
- 41.Comeau M. Personal satisfaction among Canadian physicians: a retrospective look at survey results. Ottawa, ON: National Physician Survey; 2007. Available from: www.nationalphysiciansurvey.ca/nps/reports/PDF-e/Professional_Satisfaction_26-01-07.pdf. Accessed 2010 May 10. [Google Scholar]
- 42.Barondess JA. On mentoring. J R Soc Med. 1997;90(6):347–9. doi: 10.1177/014107689709000617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Birch DW, Asiri AH, de Gara CJ. The impact of a formal mentoring program for minimally invasive surgery on surgeon practice and patient outcomes. Am J Surg. 2007;193(5):589–92. doi: 10.1016/j.amjsurg.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 44.Coddington CC, Satin AJ. Mentorship: discovering a key to the future. Fertil Steril. 2008;90(5):1571–3. doi: 10.1016/j.fertnstert.2007.10.051. Epub 2008 Feb 4. [DOI] [PubMed] [Google Scholar]
- 45.Gutkin C. Family physician shortages. Are nurses the answer? Can Fam Physician. 2008;54:479, 480. Fr. (Eng). [PMC free article] [PubMed] [Google Scholar]
- 46.Heaton CJ. Making it personal; mentoring future family docs. Fam Med. 2007;39(1):11–2. [PubMed] [Google Scholar]
- 47.Sambunjak D, Straus SE, Marusic A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103–15. doi: 10.1001/jama.296.9.1103. [DOI] [PubMed] [Google Scholar]
- 48.Leslie K, Lingard L, Whyte S. Junior faculty experiences with informal mentoring. Med Teach. 2005;27(8):693–8. doi: 10.1080/01421590500271217. [DOI] [PubMed] [Google Scholar]
- 49.Eby LT, Rhodes JE, Allen TD. Definition and evolution of mentoring. In: Allen TD, Eby LT, editors. The Blackwell handbook of mentoring. A multiple perspectives approach. Victoria, Australia: Blackwell Publishing Ltd; 2007. pp. 7–20. [Google Scholar]
- 50.Day R, Allen TD. The relationship between career motivation and self-efficacy with protégé career success. J Vocat Behav. 2004;64(1):72–91. [Google Scholar]
- 51.Lankau MJ, Scandura TA. Mentoring as a forum for personal learning in organizations. In: Ragins BR, Kram KE, editors. The handbook of mentoring at work. Theory, research and practice. Los Angeles, CA: Sage Publications; 2007. pp. 95–122. [Google Scholar]
- 52.Kram KE. Mentoring at work. Developmental relationships in organizational life. Glenview, IL: Scott, Foresman & Company; 1985. [Google Scholar]
- 53.Hay J. Transformational mentoring. Creating developmental alliances for changing organizational cultures. London, Engl: McGraw-Hill Book Company; 1995. [Google Scholar]
- 54.Kanaskie ML. Mentoring—a staff retention tool. Crit Care Nurs Q. 2006;29(3):248–52. doi: 10.1097/00002727-200607000-00010. [DOI] [PubMed] [Google Scholar]
- 55.Rebick G, Kittler A, Cadesky E. Adding evidence. The value of researching family medicine interest groups. Can Fam Physician. 2007;53:1064–6. [PMC free article] [PubMed] [Google Scholar]
- 56.Armson H, Kinzie S, Hawes D, Roder S, Wakefield J, Elmslie T. Translating learning into practice. Lessons from the practice-based small group learning program. Can Fam Physician. 2007;53:1477–85. [PMC free article] [PubMed] [Google Scholar]
- 57.MacLeod S. The challenge of providing mentorship in primary care. Postgrad Med J. 2007;83(979):317–9. doi: 10.1136/pgmj.2006.054155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Omary MB. Mentoring the mentor: another tool to enhance mentorship. Gastroenterology. 2008;135(1):13–6. doi: 10.1053/j.gastro.2008.05.065. Epub 2008 Jun 6. [DOI] [PubMed] [Google Scholar]
- 59.Westfall JM, VanVorst RF, Main DS, Herbert C. Community-based participatory research in practice-based networks. Ann Fam Med. 2006;4(1):8–14. doi: 10.1370/afm.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Minker M, Wallerstein N, editors. Community-based participatory research for health. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]
- 61.Gaventa J, Cornwall A. Power and knowledge. In: Carroll WK, editor. Critical strategies for social research. Toronto, ON: Canadian Scholars’ Press Inc; 2005. pp. 320–33. [Google Scholar]
- 62.Frankish CJ, George A, Daniel M, Doyle Waters M, Walker M, editors. Participatory research in health promotion in Canada. Ottawa, ON: Health Canada; 1997. Guidelines and categories for classifying participatory research projects in health. Available from: www.lgreen.net/guidelines.html. Accessed 2010 May 10. [Google Scholar]
- 63.Charmaz K. Constructing grounded theory. A practical guide through qualitative analysis. London, Engl: Sage Publications; 2006. [Google Scholar]
- 64.Richards L. Handling qualitative data. A practical guide. Thousand Oaks, CA: Sage Publications; 2005. [Google Scholar]


