Abstract
Objective
Although there has been a socioeconomic gradient in smoking prevalence, cessation, and disease burden for decades, these disparities have become even more pronounced over time. The aim of the current study was to develop and test a conceptual model of the mechanisms linking socioeconomic status (SES) to smoking cessation.
Design
The conceptual model was evaluated using a latent variable modeling approach in a sample of 424 smokers seeking treatment (34% African American; 33% Latino; 33% White). Hypothesized mechanisms included social support, neighborhood disadvantage, negative affect/stress, agency, and craving.
Main Outcome Measure
The primary outcome was week 4 smoking status.
Results
As hypothesized, SES had significant direct and indirect effects on cessation. Specifically, neighborhood disadvantage, social support, negative affect/stress, and agency mediated the relation between SES and smoking cessation. A multiple group analysis indicated that the model was a good fit across racial/ethnic groups.
Conclusion
The present study yielded one of the more comprehensive models illuminating the specific mechanisms that link SES and smoking cessation. Policy, community, and individual-level interventions that target low SES smokers and address the specific pathways identified in the current model could potentially attenuate the impact of SES on cessation.
Keywords: Smoking cessation, socioeconomic status, structural equation model
Although the number of smokers in the United States has been declining over the past four decades, there are striking socioeconomic status (SES) gradients in smoking prevalence and cessation (Barbeau, Krieger, & Soobader, 2004; Centers for Disease Control and Prevention, 2007). Further, there is evidence that these gradients are worsening (e.g., Gilman, Abrams, & Buka, 2003). Individuals with lower education, income, and occupational status are both more likely to smoke and less likely to quit smoking (Barbeau et al., 2004; Centers for Disease Control and Prevention, 2007; Harwood, Salsberry, Ferketich, & Wewers, 2007; Healton & Nelson, 2004). Other SES-related variables, such as insurance and employment status, have also been implicated in smoking prevalence and cessation (Ayanian, Weissman, Schneider, Ginsburg, & Zaslavsky, 2000; Centers for Disease Control and Prevention, 1998; Lee, Crombie, Smith, & Tunstall-Pedoe, 1991). Nevertheless, relatively few studies have delineated the mechanisms through which SES influences smoking cessation. Gaining a greater understanding of the pathways through which SES influences smoking cessation may help to identify treatment targets within disadvantaged populations, improve current smoking cessation interventions, and ultimately reduce the burden of smoking related disease.
Models Linking SES to Health Behavior and Smoking Cessation
The relation between SES and health behavior has been well documented (e.g., Lynch, Kaplan, & Salonen, 1997) and several conceptual models have been proposed that identify key mechanisms linking SES to health behavior (Adler & Ostrove, 1999; Gallo & Matthews, 2003). Adler and Ostrove (1999) hypothesize that SES (e.g., education, income, occupation) directly influences environmental (e.g., neighborhood crime, social support) and psychosocial variables (e.g., affect, cognition), that in turn, impact health behavior. Thus, Adler and Ostrove (1999) posit that socioeconomically disadvantaged individuals tend to be less healthy than more advantaged individuals due to higher exposure to stress, lower access to physical and environmental resources, greater environmental constraints, fewer affective/cognitive resources, and poorer health behavior. Similarly, Gallo and Matthews (2003) hypothesized that low SES individuals are exposed to high levels of stress due to the nature of their environment and have fewer interpersonal and intrapersonal resources (i.e., reserve capacity) to cope with these stressors compared with individuals in higher SES groups. Additionally, these variables are hypothesized to play a role in the relationship between SES and health behavior through their effects on affect and cognition. Although the two models diverge on some hypothesized pathways, they are very similar overall.
General models of drug relapse also identify key mechanisms that may link SES to cessation. Witkiewitz and Marlatt’s (2004) cognitive-behavioral model of substance abuse delineates stable and contextual risk factors thought to be important in the cessation process. Cognitive variables, withdrawal, coping, and affect are considered important mediating variables that link distal risk factors (e.g., family substance abuse history, years of dependence) to substance cessation. Importantly, Witkiewitz and Marlatt posited reciprocal relationships between cognitive processes, affect, and coping behavior in order to emphasize the interaction between these factors. For instance, negative affect may increase negative cognitions about smoking cessation and vice versa, and either direction of causality may increase the chance of relapse. Thus, there may be multiple precipitants of relapse and these precipitants may also interact to increase the likelihood of relapse.
Other conceptual models that posit mechanisms linking SES and smoking have also been developed. Harwood et al. (2007) posited that psychosocial factors, such as social ties, perceived control, perceived stress, and affective states, mediate the relation between SES and smoking. Honjo, Tsutsumi, Kawachi, and Kawakami (2006) used path analysis to demonstrate that the relationship between SES and smoking cessation was mediated by the use of smoking cessation resources (e.g., nicotine replacement, quit line) and exposure to other smokers while at home. Higher SES individuals were more likely to use quit aids and less likely to be exposed to smokers in their home, and therefore were less likely to relapse relative to lower SES individuals. Finally, Manfredi, Cho, Crittenden, and Dolecek (2007) reported that several psychosocial variables, including stress, situational self-efficacy, and plans to quit, were involved in complex mediational relationships between education and smoking status at six months post-quit. Thus, although conceptual models have begun to be developed to illuminate the complex relationship between SES and smoking cessation, there are very few studies that have empirically tested these models.
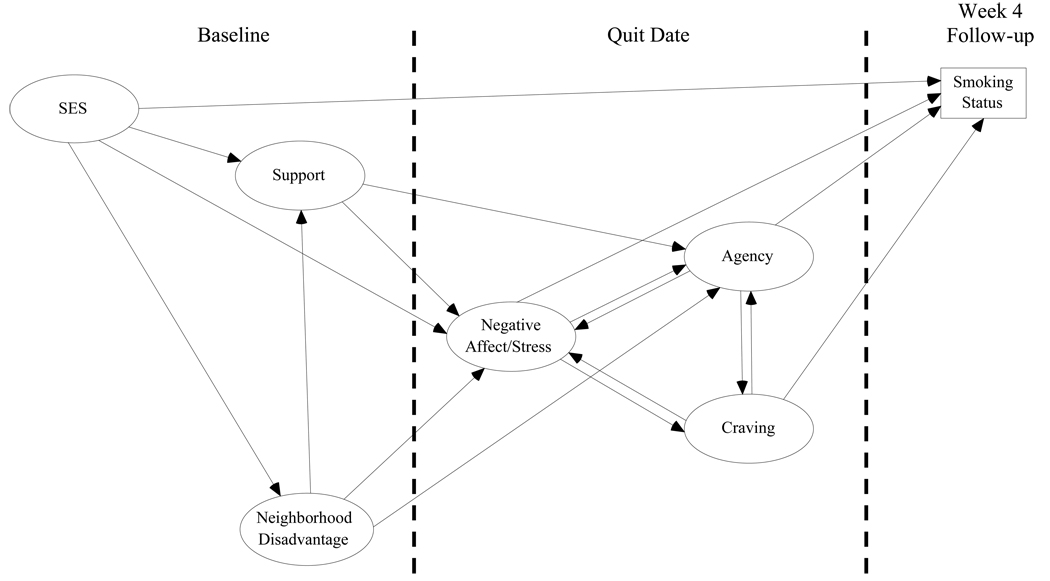
The purpose of the current study was to develop and test a conceptual model of the pathways through which SES influences smoking cessation. A model was developed by integrating current conceptual models and findings from previous research. The hypothesized conceptual model is depicted in Figure 1. As shown in Figure 1, baseline measures of social support and neighborhood disadvantage, and quit date measures of negative affect/stress, craving for nicotine, and agency were hypothesized to mediate the relationship between SES and smoking cessation. It is notable that the conceptual model includes reciprocal relationships between negative affect/stress, agency, and craving as hypothesized by the Witkiewitz and Marlatt (2004) model of relapse. Most of the individual links among constructs in the conceptual model are supported by previous research as described below.
Figure 1.
Tested conceptual model.
Hypothesized Mediators of the Relation between SES and Smoking Cessation
Social support
Individuals of low SES report fewer close social relationships and use their support network to a lesser extent than individuals of higher SES (see Belle 1983 for a review). Additionally, greater social support has consistently been shown to have a positive influence on smoking cessation (Gulliver, Hughes, Solomon, & Dey, 1995; Mermelstein, Cohen, Lichtenstein, Baer, & Kamarck, 1986). Social support may influence smoking cessation by increasing self-efficacy (Gulliver et al., 1995; Sorensen, Barbeau, Hunt, & Emmons, 2004) and reducing negative affect/stress (e.g., Berkman, Glass, Brissette, & Seeman, 2000; Schulz et al., 2006). However, whether social support functions as a mediator of the relation between SES and smoking cessation remains to be determined.
Neighborhood disadvantage
Overall, individuals of lower SES report greater exposure to neighborhood problems (e.g., crime and other environmental stressors), are more vigilant for threat in their neighborhoods, and perceive less neighborhood social cohesion compared to those of higher SES (Patterson, Eberly, Ding, & Hargreaves, 2004; Steptoe & Feldman, 2001). Although little is known about the relation between neighborhood disadvantage and smoking cessation, recent studies have indicated that neighborhood disadvantage (e.g., perceived neighborhood problems, perceived neighborhood safety) is associated with an increased likelihood of smoking and engaging in other detrimental health behaviors (Ellaway & Macintyre, 2009; Miles, 2006; Pampalon, Hamel, De Koninck, & Disant, 2007; Yen et al., 2006). Hypothesized mechanisms through which various measures of neighborhood disadvantage may impact health behavior include exacerbation of negative affect and stress (Cutrona, Wallace, & Wesner, 2006), disruption of social ties (Cutrona et al., 2006), and weakening a person’s sense of agency (e.g., self-control; Pampalon et al., 2007). For example, Hill and Angel (2005) showed that exposure to high levels of neighborhood disadvantage (e.g., crime, unsafe streets) resulted in increased anxiety and depression, and some individuals may use heavy drinking as an attempt to reduce this tension. Thus, neighborhood disadvantage could help to explain the relationship between SES and smoking cessation.
Negative affect/stress
Numerous studies have shown that negative affect and stress are associated with both SES and smoking cessation, and it has been hypothesized that negative affect/stress plays an important mediational role in the relation between these two variables (Manfredi et al., 2007). Individuals of lower SES tend to report more stressors and greater overall negative affect relative to those of higher SES (see Gallo & Matthews, 2003 for a review). Additionally, high post-quit negative affect has been repeatedly implicated as one of the best predictors of smoking cessation (e.g., Kenford et al., 2002; Shiffman, Paty, Gnys, Kassel, & Hickcox, 1996). Thus, compared to smokers of higher SES, low SES smokers are likely to encounter more stressors and experience greater negative affect during a quit attempt, and may therefore experience greater temptation to reduce negative affect by smoking. Furthermore, studies have shown that negative affect/stress reduces self-efficacy and increases craving, both of which increase the odds of relapse (Cinciripini et al., 2003; Kassel et al., 2007; Manfredi et al., 2007; Maude-Griffin & Tiffany, 1996; Niaura, Shadel, Britt, & Abrams, 2002; Shiffman & Waters, 2004).
Agency
Agency (e.g., self-efficacy) for quitting smoking has been linked to SES and is an important predictor of smoking cessation. For example, individuals who have achieved higher levels of education report higher confidence in their ability to quit smoking (Droomers, Schrijvers, & Mackenbach, 2004). An individual’s confidence in their ability to maintain abstinence from smoking predicts smoking cessation (e.g., Baer, Holt, & Lichtenstein, 1986; Gwaltney, Shiffman, Balabanis, & Paty, 2005; Matheny & Weatherman, 1998). Importantly, Gwaltney and colleagues (2005) showed that quit day self-efficacy ratings, but not self-efficacy measured at a baseline visit, predicted individual lapse and progression from lapse to relapse. Additionally, it has been demonstrated that postcessation self-efficacy is a significant mediator of the relation between negative affect and smoking cessation (Cinciripini et al., 2003). Although some researchers have hypothesized a mediating influence of agency in the relationship between SES and smoking cessation (Droomers et al., 2004), this relationship remains to be empirically validated.
Craving
Nicotine craving may be an important, although understudied, mediator in the relation between SES and smoking cessation. Although little is known about the relationship between SES and craving, some research has shown that tobacco advertising is often more prevalent in low SES neighborhoods (Laws, Whitman, Bowser, & Krech, 2002) and it is possible that SES may have an indirect influence on nicotine craving through exposure to tobacco advertisements. In addition, numerous studies have shown that the frequency and intensity of nicotine craving can predict subsequent smoking relapse (Bagot, Heishman, & Moolchan, 2007; Killen, Fortmann, Newman, & Varady, 1991; Shiffman et al., 1997; Stapleton, 1998). Further, there is some evidence that craving may increase negative affect (Drobes, Meier, & Tiffany, 1994) and reduce self-efficacy (Nordgren, van der Pligt, & van Harreveld, 2008; Shadel & Cervone, 2006). Thus, the possibility that craving plays a mediating role in the relation between SES and smoking cessation, and the inter-relationships among proximal predictors of cessation such as craving, negative affect/stress, and self-efficacy warrant further study.
The primary purpose of the current study was to extend previous research on the relation between SES and smoking cessation by examining potential mediational pathways using a structural equation modeling approach. Several mediational pathways were hypothesized and tested in the current study (see Figure 1). For example, we hypothesized that low SES would increase neighborhood disadvantage which would increase negative affect and reduce agency, and ultimately increase the odds of relapse. A second hypothesized indirect pathway was from low SES through low social support. Low social support was hypothesized to contribute to high negative affect and low agency, ultimately resulting in higher odds for relapse.
Method
Participants
Data for the current study were collected as part of a longitudinal cohort study designed to examine the pathways linking social determinants (e.g., race/ethnicity, gender, SES) to smoking cessation. The sample consisted of similar numbers of African-American (n = 144), White (n = 139), and Latino (n = 141) males and females. Participants were recruited via local print and radio advertisements to take part in a smoking cessation study. Participants were required to be at least 21 years of age, have smoked at least five cigarettes per day for the past year, have a home address and functioning telephone number, demonstrate proficiency in English at a 6th grade level or higher, and be motivated to quit smoking in the next 30 days. Potential participants were excluded if the nicotine patch was contraindicated, if they reported use of tobacco products other than cigarettes, or if they reported participation in a smoking cessation program within the past 90 days.
Procedures
The study was approved by the Institutional Review Board of the University of Texas M. D. Anderson Cancer Center. Potential participants were screened over the phone to determine eligibility (n = 944). Those who met eligibility criteria (n = 837) were invited for an in-person screening and orientation session. A total of 424 eligible individuals attended the orientation session and were enrolled in the study. At this session, participants were further screened, informed consent was obtained, literacy was measured, and all baseline measures were collected. Participant recruitment and flow through the study have been reported elsewhere (Kendzor et al., 2008).
All participants received smoking cessation treatment based on recommendations made in the Treating Tobacco Use and Dependence guidelines (Fiore et al., 2008). Specifically, six weeks of nicotine patch therapy was provided, and participants were instructed to begin using the patches on their quit date. Additionally, participants received six smoking cessation therapy sessions, each lasting from 10 to 20 minutes. Therapy sessions were scheduled to coincide with assessment visits. Participants completed assessments and received smoking cessation therapy at each of the following visits: week −1 (baseline), week 0 (quit date), week 1, week 2, and week 4. An additional therapy session was conducted by telephone during the third week post-cessation. Participants were compensated with $30 gift cards for completing each assessment session.
Measures
Demographics
Demographics were obtained during the screening and orientation sessions including age, race/ethnicity, education, income, employment status, and insurance status.
Tobacco use
The Tobacco History Questionnaire was administered to collect information including the onset of regular smoking, previous quit attempts, abstinence history, and smoking rate. Continuous abstinence since the quit date was assessed at each scheduled assessment by self-report and confirmed via carbon monoxide (CO) reading of less than 10 parts per million (ppm).
Neighborhood disadvantage
Three measures, administered at the orientation session, were used to assess perceived disadvantage at the neighborhood level. Neighborhood Problems is a 10-item self-report measure of problems such as vandalism, litter, and traffic within a neighborhood (Feldman & Steptoe, 2004). Scores on the measure range from 10 to 30, with higher scores indicating greater neighborhood problems. The coefficient alpha for this sample was .83. Neighborhood Vigilance is a self-report measure of vigilance for threat within an individual’s neighborhood (John D. and Catherine T. MacArthur Research Network on Socioeconomic Status and Health, 1999). Items are rated on a 5-point Likert-type scale, and scores range from 6 to 30. Higher scores indicate greater vigilance for threat (α = .78). Social Cohesion and Trust is a self-report measure of beliefs about an individual’s neighbors (e.g., neighbors' willingness to help, trustworthiness, shared values; Sampson, Raudenbush, & Felton, 1997). Items were measured on a 5-point Likert-type scale, and scores ranged from 5 to 25. Higher scores suggest greater neighborhood social cohesion and trust (α = .78).
Social support
The Interpersonal Support Evaluation List (ISEL; Brummett et al., 2006; Cohen, Mermelstein, Kamarck, & Hoberman, 1985) was used to measure perceived levels of social support. The 12-item version of this measure includes three subscales, each measuring a different aspect of social support: Appraisal support (e.g., availability of significant others for talking or confiding), Belonging support (e.g., availability of significant others to participate in some activity), and Tangible support (e.g., availability of others in a time of need). Each item is rated on a 4-point scale. Subscale scores range from 4 to 16, with higher scores representing higher perceived support. Coefficient alphas for the three ISEL subscales were .74, .70, and .70, respectively. The ISEL was administered at the orientation session.
Negative affect/stress
Three measures were administered to assess self-reported negative affect/stress on the day the participant quit smoking. The Center of Epidemiologic Studies Depression Scale (CES-D) is a 20-item measure developed to assess depressive symptoms in community non-clinical populations (Radloff, 1977). Scores range from 0 to 60 and scores ≥ 16 indicate clinically significant distress (α = .90). The Positive and Negative Affect Scale (PANAS; Watson, Clark, & Tellegen, 1988) consists of 20 adjectives that form two highly reliable subscales: Positive Affect and Negative Affect. Subscale scores range from 10 to 50 and higher scores indicate higher positive and negative affect. Only the Negative Affect subscale of the PANAS (α = .91) was used in the current study. The Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) is a 4-item measure designed to assess the degree to which respondents find their lives to be stressful. Scores range from 0 to 16 and higher scores indicate greater perceived stress (α = .76).
Craving
The Wisconsin Inventory of Smoking Dependence Motives (WISDM-68; Piper et al., 2004) is a 68-item self-report questionnaire that yields an overall dependence score as well as subscale scores for 13 dimensions of tobacco dependence. Individual item responses range from “not true of me at all” to “extremely true of me” on a seven-point scale. The 4-item Craving subscale of the WISDM-68 was used as a measure of craving for nicotine on the quit date (α = .86).
Agency
The Affective Information Processing Questionnaire (AIPQ; Wetter, Brandon, & Baker, 1992) measures expectancies related to affect regulation. Participants read vignettes characterized by negative affect and provided ratings of the controllability of their affect in that situation by smoking and by means other than smoking. Only the control of affect by means other than smoking subscale (α = .91) was used in the current study. The Self-Efficacy/Confidence Scale (SECS; Velicer, Diclemente, Rossi, & Prochaska, 1990) measures an individual’s confidence that they can cope with high-risk situations without smoking. The SECS is comprised of three subscales: Positive Affect/Social Situations, Negative Affect Situations, and Habitual/Craving Situations. Each subscale consists of three items scored on a 5-point scale ranging from “not at all confident” to “extremely confident.” Coefficient alphas for the three SECS subscales were .76, .89, and .77 respectively. Each of the agency measures was administered on the quit date.
Analytic Plan
Structural equation modeling was used to evaluate the hypothesized model using the Mplus software package (version 5.1; Muthén & Muthén, 2007). Six latent variables were developed (i.e., SES, social support, neighborhood disadvantage, negative affect/stress, agency, and craving), five of which were included as mediators in the relation between the SES latent variable and week 4 smoking status. The SES latent variable included measures of education, income, insurance status, and employment status. It is important to note that the SES latent variable was comprised of both categorical and continuous variables. Mplus handles this situation by estimating “probit regression coefficients for the categorical factor indicators, and linear regression coefficients for the continuous factor indicators” (Muthén & Muthén, 2007). The neighborhood disadvantage latent variable was made up of the Neighborhood Problems, Social Cohesion, and Neighborhood Vigilance questionnaires. The social support latent variable was comprised of the three ISEL-12 subscales (i.e., Tangible support, Belonging support, and Appraisal support). The negative affect/stress latent variable included the CES-D, PSS, and the Negative Affect subscale of the PANAS. The craving latent variable was made up of the four items that comprise the Craving subscale of the WISDM-68. The agency latent variable consisted of the AIPQ subscale related to control of affect by means other than smoking, and the three subscales that comprise the SECS.
Most of the observed variables were treated as continuous variables. Insurance status (i.e., insured = 1; uninsured = 0), employment status (i.e., employed = 1; unemployed = 0), income (i.e., > $20,000 per year = 1; ≤ $20,000 per year = 0), and smoking status (i.e., relapsed = 1; continuous abstinence = 0) were treated as categorical variables. Week 4 intent to treat smoking status was the dependent variable in the current study. Thus, none of the data were missing for smoking status (i.e., missing were counted as relapsed). However, there were missing data on other variables in the model. As a result, the data were analyzed using maximum-likelihood estimation under the assumption that data are missing at random.
Due to the inclusion of categorical variables, weighted least squares with robust standard errors (WLSMV) parameter estimation was used to estimate free parameters in the current study. In order to determine how well the model fit the observed data, the following goodness of fit indices were used: 1) chi-square goodness of fit index (e.g., Brown, 2006; Hu & Bentler, 1998), 2) comparative fit index (CFI; Bentler, 1990), 3) Tucker-Lewis Index (TLI; Tucker & Lewis, 1973); 4) root mean square error of approximation (RMSEA; Steiger, 1990); and 5) the weighted root mean square residual (WRMR). Published rules for significance levels of fit indices were followed (Bentler, 1990; Browne & Cudeck, 1993; Hu & Bentler, 1998; Yu & Muthén, 2002). Specifically, minimum TLIs and CFIs of .90 were required for model acceptance, and values of .95 or greater were accepted as an indication of good model fit. Additionally, RMSEAs of less than .06 and WRMRs of less than 1.0 were accepted as indicators of a good fitting model. Indirect pathways between SES and smoking status were tested using the Mplus “Model Indirect” command. Thus, standard errors for the indirect effects were estimated using the Delta method (Bollen, 1989) and indirect path coefficients were tested for significance using z-tests.
Results
Participant Characteristics
A total of 424 participants were enrolled in the current study (34% African American, 33% Latino, and 33% White). Participant characteristics are shown in Table 1.
Table 1.
Participant Characteristics
| Characteristic | Mean/Percentile (SD) |
|---|---|
| Demographics | |
| Age (years) | 41.2 (±11.2) |
| Gender (% female) | 53.3 |
| Marital status (% single) | 65.2 |
| Smoking Characteristics | |
| Cigarettes per day | 21.1 (±10.3) |
| Years smoked | 21.6 (±11.1) |
| Smoke within 5 minutes of waking (%) | 49.3 |
| CO (parts per million) | 24.7 (±12.5) |
| Cotinine (ng/ml) | 323.3 (±198.6) |
| SES | |
| Education (years) | 12.90 (2.00) |
| Insurance (% no) | 58.6 |
| Income (% < $20,000) | 42.1 |
| Employed (% no) | 41.9 |
| Neighborhood Disadvantage | |
| Neighborhood Problems | 14.86 (4.02) |
| Neighborhood Vigilance | 16.41 (4.52) |
| Social Cohesion | 16.38 (3.75) |
| Social Support | |
| Appraisal | 12.67 (2.97) |
| Belonging | 12.56 (2.70) |
| Tangible Support | 12.58 (2.80) |
| Negative Affect/Stress | |
| PANAS Negative Affect | 19.57 (8.10) |
| CES-D | 14.10 (11.24) |
| PSS | 5.25 (3.40) |
| Agency | |
| AIPQ | 5.14 (1.26) |
| SECS: Positive Affect Situations | 9.90 (2.70) |
| SECS: Negative Affect Situations | 8.70 (3.12) |
| SECS: Habit/Craving Situations | 10.34 (2.73) |
| Craving | |
| Urges | 2.51 (1.08) |
| Desire | 2.33 (1.11) |
| Thoughts | 1.99 (1.18) |
| Focus | 1.85 (1.09) |
N = 424; SES = Socioeconomic Status; PANAS = Positive and Negative Affect Scale; CES-D = Center of Epidemiologic Studies Depression Scale; PSS = Perceived Stress Scale; AIPQ = Affective Information Processing Questionnaire; SECS = Self-efficacy/Confidence Scale
Note: The first factor in each construct was used to define the metric for that construct in the model.
Attrition
Week 4 continuous abstinence data was available for 85.6% of the sample. Among individuals with week 4 data, 18.5% had been abstinent since their quit date. Individuals who attended the week 4 follow-up were of greater age (42.1 years vs. 36.2 years), F(1, 422) = 14.62, p < .001, more likely to be married or living with a significant other (90.4% vs. 83.2%), χ2(1, N = 420) = 4.03, p = .05, and less likely to be Latino (White = 89.2%, African American = 88.2%, Latino = 79.4%) compared to those who did not attend. No other demographic variables significantly differed between individuals who did or did not attend the week 4 assessment visit. Because week 4 intent to treat smoking status was used as the dependent variable, all participants who did not attend the week 4 visit were coded as relapsed.
Correlations Among Predictors
Appropriate zero-order correlations (e.g., Pearson product moment, point-biserial) between all observed variables are displayed in Table 2. As shown, indicators of SES, social support, and neighborhood disadvantage were collected at baseline and indicators of negative affect/stress, craving, and agency were collected on the quit date. As expected, the highest correlations were found between variables within the same latent construct and many of the observed variables were significantly correlated. Most notably, nearly all of the observed variables were significantly related to week 4 smoking status, with the exception of the Neighborhood Problems scale, the Neighborhood Vigilance scale, the Negative Affect subscale of the PANAS, the AIPQ, and each of the individual items in the Craving subscale. Means and standard deviations for all measured variables are listed in Table 1.
Table 2.
Zero Order Correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SES* | |||||||||||||||||||||
| 1. Education | - | ||||||||||||||||||||
| 2. Insurance1 | .262a | - | |||||||||||||||||||
| 3. Income2 | .213a | .537a | - | ||||||||||||||||||
| 4. Employment3 | .180a | .447a | .449a | - | |||||||||||||||||
| Social Support* | |||||||||||||||||||||
| 5. Tangible | .107c | .249a | .189a | .175a | - | ||||||||||||||||
| 6. Belonging | .075 | .185a | .164a | .178a | .661a | - | |||||||||||||||
| 7. Appraisal | .114c | .156a | .158b | .097c | .657a | .632a | - | ||||||||||||||
|
Neighborhood Disadvantage* | |||||||||||||||||||||
| 8. Problems | −.141b | −.151b | −.230a | −.086 | −.220a | −.144b | −.219a | - | |||||||||||||
| 9. Vigilance | −.185a | −.057 | −.177a | −.074 | −.279a | −.162a | −.266a | .467a | - | ||||||||||||
| 10. Cohesion | .145b | .126b | .190a | .052 | .310a | .199a | .241a | −.502a | −.563a | - | |||||||||||
|
Negative Affect/Stress§ | |||||||||||||||||||||
| 11. PANAS-NA | .058 | −.014 | −.084 | −.074 | −.321a | −.286a | −.298a | .171a | .208a | −.173a | - | ||||||||||
| 12. CES-D | −.063 | −.062 | −.193a | −.174a | −.485a | −.469a | −.492a | .206a | .301a | −.256a | .761a | - | |||||||||
| 13. PSS | −.057 | −.052 | −.069 | −.116c | −.432a | −418a | −.432a | .175a | .280a | −.234a | .664a | .752a | - | ||||||||
| Craving§ | |||||||||||||||||||||
| 14. Urge | .035 | .040 | .029 | −.057 | −.029 | −.048 | −.044 | −.023 | −.009 | .013 | .267a | .213a | .165a | - | |||||||
| 15. Desire | .026 | −.007 | −.035 | −.070 | −.090 | −.087 | −.115c | .057 | .060 | −.013 | .237a | .199a | .147b | .640a | - | ||||||
| 16. Thoughts | .162b | .060 | .084 | −.015 | .014 | −.004 | −.037 | −.056 | −.034 | .050 | .278a | .188a | .157b | .615a | .556a | - | |||||
| 17. Focus | .057 | .057 | .068 | −.006 | −.060 | −.053 | −.122c | −.038 | −.034 | .094 | .304a | .255a | .238a | .553a | .562a | .663a | - | ||||
| Agency§ | |||||||||||||||||||||
| 18. AIPQ | −.001 | −.013 | .013 | .101 | .268a | .236a | .293a | −.061 | −.136b | .131c | −.262a | −.328a | −.401a | −.181a | −.201a | −.194a | −.287a | - | |||
| 19. Positive Affect Situations |
−.002 | −.020 | .019 | .024 | .130b | .188a | .165a | −.033 | −.085 | .107c | −.174a | −.267a | −.288a | −.216a | −.283a | −.241a | −.318a | .420a | - | ||
| 20. Negative Affect Situations |
−.010 | −.020 | .010 | .029 | .172a | .164b | .177a | −.071 | −.154b | .135b | −.345a | −.357a | −.390a | −.290a | −.280a | −.287a | −.333a | .554a | .679a | - | |
| 21. Habitual/Craving Situations |
.059 | −.018 | .044 | .095 | .161b | .160b | .207a | −.062 | −.131c | .094 | −.234a | −.296a | −.356a | −.253a | −.266a | −.206a | −.316a | .503a | .731a | .770a | - |
| 22. Week 4 Relapse4 | −.129b | −.148b | −.127c | −.115c | −.144b | −.098c | .138b | .075 | .087 | −.120c | .040 | .148b | .155b | .006 | .053 | .004 | .011 | −.078 | −.179a | −.186a | −.167b |
N = 424;
0 = not insured, 1 = insured;
0 = < 20,000 per year, 1 = ≥20,000 per year;
0 = unemployed, 1 = employed;
0 = continuous abstinence, 1 = relapsed
p ≤ .001;
p ≤ .01;
p ≤ .05;
assessed at baseline;
assessed on the quit date; SES = Socioeconomic Status; PANAS NA = Positive and Negative Affect Scale-Negative Affect; CES-D = Center of Epidemiologic Studies Depression Scale; PSS = Perceived Stress Scale; AIPQ = Affective Information Processing Questionnaire.
Structural Equation Model
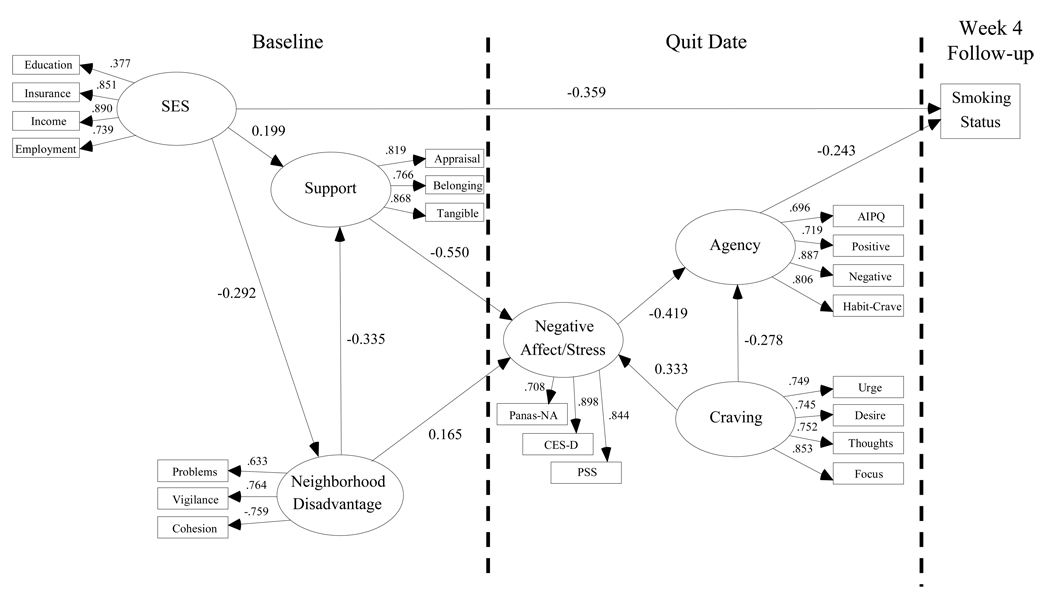
The hypothesized conceptual model fit the data reasonably well: χ2(54, N = 424) = 100.36, p < .001; CFI = .920; TLI = .959; RMSEA = .045; WRMR = .799. Because a primary goal of the current study was to develop a useful and parsimonious model, we systematically deleted non-significant paths (weakest paths were deleted first), until all paths were significant based on the methods described by MacCallum (1986). Deleting non-significant paths resulted in slightly improved fit statistics on most indices: χ2(42, N = 424) = 74.75, p = .001; CFI = .944; TLI = .962; RMSEA = .043; WRMR = .885. It is important to note that no significant indirect paths that were present in the original model were deleted due to the removal of insignificant direct paths. None of the modification indices suggested by the LaGrange Multiplier test made theoretical sense and inspection of residuals indicated no localized areas of strain; therefore, no further changes were made to the model (Chou & Bentler, 1990). The final trimmed model is presented in Figure 2, with the significance of individual paths and final factor loadings indicated.
Figure 2.
Final model. All paths significant at the p ≤ .05 level. Standardized coefficients are displayed.
SES = Socioeconomic Status; PANAS-NA = Positive and Negative Affect Scale-Negative Affect; CES-D = Center of Epidemiologic Studies Depression Scale; PSS = Perceived Stress Scale; AIPQ = Affective Information Processing Questionnaire.
As hypothesized, SES had significant direct and indirect effects on week 4 smoking status. Two of the three indirect paths that link SES to week 4 cessation were significant, while the third path approached significance. Specifically, the path SES → Neighborhood Disadvantage → Social Support → Negative Affect/Stress → Agency → week 4 cessation was significant (standardized structural coefficient = −.005; p = .02) and the path SES → Social Support → Negative Affect/Stress → Agency → week 4 cessation was also significant (standardized structural coefficient = −.011; p = .04). The path: SES → Neighborhood Disadvantage → Negative Affect/Stress → Agency → week 4 cessation approached significance (standardized structural coefficient = −.005; p = .08). Importantly, neighborhood disadvantage, social support, negative affect/stress, and craving also had significant indirect effects on smoking status. A breakdown of all indirect and total effects on smoking status for each of the latent variables is depicted in Table 3.
Table 3.
Standardized Indirect and Total Effects of Predictors on Smoking Status at Week 4 Post-Quit
| Variable | Indirect | Total |
|---|---|---|
| SES | −.02 | −.38 |
| Social Support | −.06 | −.06 |
| Neighborhood Disadvantage | .04 | .04 |
| Negative Affect/Stress | .10 | .10 |
| Craving | .10 | .10 |
| Agency | - | −.24 |
Note: All indirect and total effects are significant at the p < .05 level; SES = socioeconomic status.
We conducted a nested model comparison in order to determine whether the model containing the direct and indirect effects of SES on smoking cessation was a better fit for the data as compared to a more restricted model that included only the direct path from SES to smoking cessation. The Mplus “DIFFTEST” indicated that the simpler direct model was clearly misspecified and fit the data significantly worse than the presented final model: χ2(2, N = 424) = 40.14, p < .001. Thus, retention of the direct and indirect pathways from SES to smoking status resulted in a better fitting model.
A multiple group analysis was conducted to examine whether the model was a good fit for each of the three represented racial/ethnic groups. Overall, the model was a good fit for each group with few differences among groups.1
Other Issues
Previous research has indicated that level of nicotine dependence is related to SES (Jarvis & Wardle, 1999; Siahpush, McNeill, Borland, & Fong, 2006) and smoking cessation (e.g., Hyland et al., 2004; Killen, Fortmann, Kraemer, Varady, & Newman, 1992). However, in the current study, measures of nicotine dependence (i.e., Wisconsin Inventory of Smoking Dependence Motives-68 total score, heaviness of smoking index score) were related to SES, but were not related to smoking status. Attempts to include measures of nicotine dependence into the model resulted in a reduction of model fit. Therefore, these measures were not included in the final model.
Discussion
The current study developed and tested a conceptual model of the mechanisms that link SES to smoking cessation. The study expanded previous models of SES and smoking cessation and yielded several key findings. Specifically, the results demonstrated that neighborhood disadvantage, social support, negative affect/stress, and agency were key mediators of the relation between SES and smoking cessation. Additionally, the results indicated that the model was valid across three racial/ethnic groups, with few differences between groups. These findings increase our understanding of the process through which SES impacts smoking cessation and may aid the development of more effective treatments for at-risk populations, such as low-SES smokers.
The findings indicated that there were significant direct and indirect relationships between SES and cessation. Because the model did not incorporate all possible mediators of the SES-cessation relationship, it is not surprising that the direct path between SES and cessation in the final model continued to be significant. Other possible mediators (e.g., social pressure to quit, health concerns), likely play a mediational role in this relation (Manfredi et al., 2007), but were not assessed in the current study. In order to expand and improve upon the current model, future research should include other variables that may mediate the relation between SES and cessation including both biological measures (e.g., allostatic load) and broader population level measures (e.g., social and physical environment).
The current model took the timing of assessments into account. Previous research has indicated that negative affect, stress, and craving tend to increase on the quit date (e.g., McCarthy, Piasecki, Fiore, & Baker, 2006) and are robust predictors of cessation (e.g., Abrantes et al., 2008; Gwaltney et al., 2005; Kenford et al., 2002; Shiffman et al., 1996). This is consistent with our use of quit date, rather than baseline, measures of these variables. The results of individual analyses indicated that quit date measures generally predicted cessation, with or without controlling for baseline measures.
Although many of the hypothesized relationships in the proposed model were supported, others were not. For instance, a number of previous studies, including one conducted by the investigators (Kendzor et al., under review), have found significant direct paths between SES and negative affect/stress. However, only indirect pathways between these two variables were significant in the current study. This finding is consistent with the Gallo & Matthews model (1999; 2003), which suggests that low SES tends to increase negative affect and negative health outcomes by increasing the likelihood of negative experiences (e.g., via neighborhood disadvantage), and decreasing reserve capacity (e.g., social support).
Previous research has shown that social support and neighborhood characteristics can directly impact self-efficacy for completing specific behaviors (e.g., Bennett et al., 2007; Sorensen et al., 2004). However, the hypothesized direct impacts of social support and neighborhood disadvantage on agency were nonsignificant in the current study. Instead, these paths were mediated by negative affect/stress. This finding is important because it elucidates potential targets for smoking cessation interventions. For example, interventions that attempt to improve agency may target agency directly, and may also target social support and neighborhood disadvantage, which may indirectly impact negative affect/stress and agency.
It is important to note that the hypothesized direct pathways from negative affect/stress and craving to smoking status were not significant. However, negative affect/stress and craving indirectly increased the chance of relapse by reducing agency. This finding builds upon several previous studies that have demonstrated that heightened negative affect and craving may result in decreased self-efficacy (Manfredi et al., 2007; Nordgren et al., 2008; Shadel & Cervone, 2006). Additionally, this finding is congruent with results from a previous study conducted by the investigators, showing that postcessation self-efficacy mediated the relationship between pre-cessation depression and smoking cessation (Cinciripini et al., 2003). Results of the current study suggest that agency may be a final common pathway linking negative affect/stress and craving to smoking cessation.
Although reciprocal relationships between quit date measures of agency, craving, and negative affect/stress were hypothesized in the original model, only unidirectional relationships were found in the final model. As expected, quit date craving tended to increase negative affect/stress and decrease agency. Unexpectedly, the path from negative affect/stress to craving was not significant. This finding seems to be at odds with the Witkiewitz and Marlatt (2004) model of relapse. However, self-report data collected at a single time point (e.g., questionnaire data collected on the quit date) may not have been ideal for the examination of such reciprocal relationships. Shiffman and Waters (2004) recently noted the reciprocal relationship between withdrawal and negative affect and called for further study of the ways in which these two variables interact to increase the chances of relapse. Future research might use ecological momentary assessment techniques to gain a better understanding of how negative affect/stress, craving, and agency interact on a moment to moment basis to influence smoking cessation.
This study has several strengths. The study utilized a prospective design that incorporated baseline and quit date predictors of week 4 cessation. Also, multiple indicators of SES were used to create a SES latent variable, which may have provided a more complete picture of socioeconomic context. Additionally, the use of structural equation modeling techniques allowed us to concurrently examine complex mediational relationships among latent variables. Finally, the sample was made up of nearly identical numbers of White, African American, and Latino smokers, which allowed us to test the model across several racial/ethnic groups.
Several limitations temper our findings and should be addressed in future research. First, over 42% of our participants reported that their household income was less than $20,000 per year. This overrepresentation of the lower end of the SES spectrum may have resulted in underestimation of the direct and indirect effects of SES on smoking cessation. Second, the CES-D, PANAS Negative Affect scale, and PSS were used to form a single latent variable. This was done because these measures were highly correlated and we believed that the items were an acceptable gauge of current psychological distress. However, future research in this area may benefit from parsing the effects of stress and negative affect. Additionally, inclusion of subjective (e.g., perceived stress) and objective measures (e.g., biological markers of stress, number of current stressors) of both acute and chronic stress may result in more powerful smoking cessation models. Finally, although our model adequately fit the data, it is possible that other models may have been an equivalent or better fit for the data. Therefore, our findings simply imply that the current model is plausible. Although this research may provide insight into the complex relation between SES and smoking cessation, this study was only the first step in exploring these relations. Validation within multiple samples is needed to provide additional support for the validity of this model (Ullman, 2006).
An improved understanding of the relationship between SES and smoking cessation is important for the development of treatments that specifically target underserved populations. Our findings demonstrate the complex relationship between SES and cessation and highlight potential targets for future public policy changes and smoking cessation interventions. Specifically, public policies that have a positive impact on SES variables (e.g., employment, education, insurance, income) and policies that reduce the high level of tobacco exposure often seen in low SES neighborhoods are likely to enhance smoking cessation. At the neighborhood level, community based interventions focused on reducing neighborhood problems (e.g., crime, litter), such as neighborhood watch, may result in reductions in smoking by increasing social capital and reducing perceptions that one lives in a dangerous environment. At the individual level, it may be particularly important to address negative affect/stress and self-efficacy among underserved populations given that these variables appear to function as key mediators in the pathways between SES, neighborhood disadvantage, social support, craving, and smoking cessation. Continued examination of the variables linking SES and cessation will be necessary for the development of novel treatments that aim to improve cessation rates in underserved and at-risk populations.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/hea
Interested readers may contact the primary author for more information related to this issue.
References
- Abrantes AM, Strong DR, Lejuez CW, Kahler CW, Carpenter LL, Price LH, et al. The role of negative affect in risk for early lapse among low distress tolerance smokers. Addictive Behaviors. 2008;33(11):1394–1401. doi: 10.1016/j.addbeh.2008.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler NE, Ostrove JM. Socioeconomic status and health: What we know and what we don't. Annals of the New York Academy of Sciences. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. Journal of the American Medical Association. 2000;284(16):2061–2069. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- Baer JS, Holt CS, Lichtenstein E. Self-efficacy and smoking reexamined: Construct validity and clinical utility. Journal of Consulting & Clinical Psychology. 1986;54(6):846–852. doi: 10.1037//0022-006x.54.6.846. [DOI] [PubMed] [Google Scholar]
- Bagot KS, Heishman SJ, Moolchan ET. Tobacco craving predicts lapse to smoking among adolescent smokers in cessation treatment. Nicotine & Tobacco Research. 2007;9(6):647–652. doi: 10.1080/14622200701365178. [DOI] [PubMed] [Google Scholar]
- Barbeau EM, Krieger N, Soobader M. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. American Journal of Public Health. 2004;94(2):269–278. doi: 10.2105/ajph.94.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belle DE. The impact of poverty on social networks and supports. Marriage & Family Review. 1983;5(4):89–103. [Google Scholar]
- Bennett GG, McNeill LH, Wolin KY, Duncan DT, Puleo E, Emmons KM. Safe to walk? Neighborhood safety and physical activity among public housing residents. Public Library of Science. 2007;4(10):1599–1607. doi: 10.1371/journal.pmed.0040306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural Equations with Latent Variables. New York: John Wiley & Sons; 1989. [Google Scholar]
- Brown TA. Confirmatory Factor Analysis for Applied Research. New York: Guilford Press; 2006. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Beverly Hills, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Brummett BH, Babyak MA, Siegler IC, Vitaliano PP, Ballard EL, Gwyther LP, et al. Associations among perceptions of social support, negative affect, and quality of sleep in caregivers and noncaregivers. Health Psychology. 2006;25(2):220–225. doi: 10.1037/0278-6133.25.2.220. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Self-assessed health status and selected behavioral risk factors among persons with and without health-care coverage - United States, 1994–1995. Morbidity and Mortality Weekly Report. 1998;47(9):176–180. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Cigarette smoking among adults - United States, 2006. Morbidity and Mortality Weekly Report. 2007;56(44):1157–1161. [PubMed] [Google Scholar]
- Chou CP, Bentler PM. Model Modification in Covariance Structure Modeling: A Comparison among Likelihood Ratio, Lagrange Multiplier, and Wald Tests. Multivariate Behavioral Research. 1990;25(1):115–136. doi: 10.1207/s15327906mbr2501_13. [DOI] [PubMed] [Google Scholar]
- Cinciripini PM, Wetter DW, Fouladi RT, Blalock JA, Carter BL, Cinciripini LG, et al. The effects of depressed mood on smoking cessation: Mediation by postcessation self-efficacy. Journal of Consulting & Clinical Psychology. 2003;71(2):292–301. doi: 10.1037/0022-006x.71.2.292. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A gobal measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the Functional Components of Social Support. In: Sarason IG, Sarason BR, editors. Social Support: Theory, Research and Application. The Hague, Holland: Martinus Nijhoff; 1985. [Google Scholar]
- Cutrona CE, Wallace G, Wesner KA. Neighborhood characteristics and depression: An examination of stress processes. Current Directions in Psychological Science. 2006;15(4):188–192. doi: 10.1111/j.1467-8721.2006.00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drobes DJ, Meier EA, Tiffany ST. Assessment of the effects of urges and negative affect on smokers' coping skills. Behaviour Research and Therapy. 1994;32(1):165–174. doi: 10.1016/0005-7967(94)90099-x. [DOI] [PubMed] [Google Scholar]
- Droomers M, Schrijvers CTM, Mackenbach JP. Educational differences in the intention to stop smoking: Explanations based on the Theory of Planned Behaviour. European Journal of Public Health. 2004;14(2):194–198. doi: 10.1093/eurpub/14.2.194. [DOI] [PubMed] [Google Scholar]
- Ellaway A, Macintyre S. Are perceived neighbourhood problems associated with the likelihood of smoking? Journal of Epidemiology and Community Health. 2009;63(1):78–80. doi: 10.1136/jech.2007.068767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman PJ, Steptoe A. How neighborhoods and physical functioning are related: The roles of neighborhood socioeconomic status, perceived neighborhood strain, and individual health risk factors. Annals of Behavioral Medicine. 2004;27(2):91–99. doi: 10.1207/s15324796abm2702_3. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: Department of Health and Human Services. Public Health Service; 2008. [Google Scholar]
- Gallo LC, Matthews KA. Do negative emotions mediate the association between socioeconomic status and health? In: Adler NE, Marmot M, McEwen BS, Stewart J, editors. Socioeconomic Status and Health in Industrial Nations: Social, Psychological, and Biological Pathways. New York: New York Academy of Science; 1999. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129(1):10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Abrams DB, Buka SL. Socioeconomic status over the life course and stages of cigarette use: Initiation, regular use, and cessation. Journal of Epidemiology and Community Health. 2003;57(10):802–808. doi: 10.1136/jech.57.10.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver SB, Hughes JR, Solomon LJ, Dey AN. An investigation of self-efficacy, partner support and daily stresses as predictors of relapse to smoking in self-quitters. Addiction. 1995;90(6):767–772. doi: 10.1046/j.1360-0443.1995.9067673.x. [DOI] [PubMed] [Google Scholar]
- Gwaltney CJ, Shiffman S, Balabanis MH, Paty JA. Dynamic self-efficacy and outcome expectancies: Prediction of smoking lapse and relapse. Journal of Abnormal Psychology. 2005;114(4):661–675. doi: 10.1037/0021-843X.114.4.661. [DOI] [PubMed] [Google Scholar]
- Harwood GA, Salsberry P, Ferketich AK, Wewers ME. Cigarette smoking, socioeconomic status, and psychosocial factors: Examining a conceptual framework. Public Health Nursing. 2007;24(4):361–371. doi: 10.1111/j.1525-1446.2007.00645.x. [DOI] [PubMed] [Google Scholar]
- Healton C, Nelson K. Reversal of Misfortune. American Journal of Public Health. 2004;94(2):186–191. doi: 10.2105/ajph.94.2.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill TD, Angel RJ. Neighborhood disorder, psychological distress, and heavy drinking. Social Science & Medicine. 2005;61(5):965–975. doi: 10.1016/j.socscimed.2004.12.027. [DOI] [PubMed] [Google Scholar]
- Honjo K, Tsutsumi A, Kawachi I, Kawakami N. What accounts for the relationship between social class and smoking cessation? Results of a path analysis. Social Science & Medicine. 2006;62(2):317–328. doi: 10.1016/j.socscimed.2005.06.011. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3(4):424–453. [Google Scholar]
- Hyland A, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine & Tobacco Research. 2004;6 Supplement 3:S363–S369. doi: 10.1080/14622200412331320761. [DOI] [PubMed] [Google Scholar]
- Jarvis MJ, Wardle J. Social patterning of individual health behaviours: The case of cigarette smoking. In: Marmot M, Wilkinson RG, editors. Social Determinants of Health. Oxford: Oxford University Press; 1999. [Google Scholar]
- John D, Catherine T. MacArthur Research Network on Socioeconomic Status and Health. Reactive Responding – Long Form. 1999 Retrieved June 2, 2008, from http://www.macses.ucsf.edu/Research/Psychosocial/notebook/RR-42.html. [Google Scholar]
- Kassel JD, Evatt DP, Greenstein JE, Wardle MC, Yates MC, Veilleux JC. The acute effects of nicotine on positive and negative affect in adolescent smokers. Journal of Abnormal Psychology. 2007;116(3):543–553. doi: 10.1037/0021-843X.116.3.543. [DOI] [PubMed] [Google Scholar]
- Kendzor DE, Businelle MS, Mazas CA, Cofta-Woerpel LM, Reitzel LR, Vidrine JI, et al. Pathways between socioeconomic status and health behavior among African American smokers. doi: 10.1007/s10865-009-9226-3. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendzor DE, Costello TJ, Li Y, Vidrine JI, Mazas CA, Reitzel LR, et al. Race/ethnicity and multiple cancer risk factors among individuals seeking smoking cessation treatment. Cancer Epidemiology, Biomarkers & Prevention. 2008;17(11):2937–2945. doi: 10.1158/1055-9965.EPI-07-2795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenford SL, Smith SS, Wetter DW, Jorenby DE, Fiore MC, Baker TB. Predicting relapse back to smoking: Contrasting affective and physical models of dependence. Journal of Consulting and Clinical Psychology. 2002;70(1):216–227. [PubMed] [Google Scholar]
- Killen J, Fortmann S, Newman B, Varady A. Prospective study of factors influencing the development of craving associated with smoking cessation. Psychopharmacology. 1991;105(2):191–196. doi: 10.1007/BF02244308. [DOI] [PubMed] [Google Scholar]
- Killen JD, Fortmann SP, Kraemer HC, Varady A, Newman B. Who will relapse? Symptoms of nicotine dependence predict long-term relapse after smoking cessation. Journal of Consulting & Clinical Psychology. 1992;60(5):797–801. doi: 10.1037//0022-006x.60.5.797. [DOI] [PubMed] [Google Scholar]
- Laws MB, Whitman J, Bowser DM, Krech L. Tobacco availability and point of sale marketing in demographically contrasting districts of Massachusetts. Tobacco Control. 2002;11 Suppl 2:ii71–ii73. doi: 10.1136/tc.11.suppl_2.ii71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee AJ, Crombie IK, Smith WCS, Tunstall-Pedoe HD. Cigarette smoking and employment status. Social Science & Medicine. 1991;33(11):1309–1312. doi: 10.1016/0277-9536(91)90080-v. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Social Science & Medicine. 1997;44(6):809–819. doi: 10.1016/s0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- MacCallum R. Specification searches in covariance structure modeling. Psychological Bulletin. 1986;100(1):107–120. [Google Scholar]
- Manfredi C, Cho YI, Crittenden KS, Dolecek TA. A path model of smoking cessation in women smokers of low socio-economic status. Health Education Research. 2007;22(5):747–756. doi: 10.1093/her/cyl155. [DOI] [PubMed] [Google Scholar]
- Matheny KB, Weatherman KE. Predictors of smoking cessation and maintenance. Journal of Clinical Psychology. 1998;54(2):223–235. doi: 10.1002/(sici)1097-4679(199802)54:2<223::aid-jclp12>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Maude-Griffin PM, Tiffany ST. Production of smoking urges through imagery: The impact of affect and smoking abstinence. Experimental & Clinical Psychopharmacology. 1996;4(2):198–208. [Google Scholar]
- McCarthy DE, Piasecki TM, Fiore MC, Baker TB. Life before and after quitting smoking: An electronic diary study. Journal of Abnormal Psychology. 2006;115(3):454–466. doi: 10.1037/0021-843X.115.3.454. [DOI] [PubMed] [Google Scholar]
- Mermelstein R, Cohen S, Lichtenstein E, Baer JS, Kamarck T. Social support and smoking cessation and maintenance. Journal of Consulting & Clinical Psychology. 1986;54(4):447–453. doi: 10.1037//0022-006x.54.4.447. [DOI] [PubMed] [Google Scholar]
- Miles R. Neighborhood disorder and smoking: Findings of a European urban survey. Social Science & Medicine. 2006;63(9):2464–2475. doi: 10.1016/j.socscimed.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. 5th Edition ed. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- Niaura R, Shadel WG, Britt DM, Abrams DB. Response to social stress, urge to smoke, and smoking cessation. Addictive Behaviors. 2002;27(2):241–250. doi: 10.1016/s0306-4603(00)00180-5. [DOI] [PubMed] [Google Scholar]
- Nordgren LF, van der Pligt J, van Harreveld F. The instability of health cognitions: Visceral states influence self-efficacy and related health beliefs. Health Psychology. 2008;27(6):722–727. doi: 10.1037/0278-6133.27.6.722. [DOI] [PubMed] [Google Scholar]
- Pampalon R, Hamel D, De Koninck M, Disant MJ. Perception of place and health: Differences between neighbourhoods in the Québec City region. Social Science & Medicine. 2007;65(1):95–111. doi: 10.1016/j.socscimed.2007.02.044. [DOI] [PubMed] [Google Scholar]
- Patterson JM, Eberly LE, Ding Y, Hargreaves M. Associations of smoking prevalence with individual and area level social cohesion. Journal of Epidemiology and Community Health. 2004;58(8):692–697. doi: 10.1136/jech.2003.009167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Piasecki TM, Federman EB, Bolt DM, Smith SS, Fiore MC, et al. A multiple motives approach to Tobacco Dependence: The Wisconsin Inventory of Smoking Dependence Motives (WISDM-68) Journal of Consulting & Clinical Psychology. 2004;72(2):139–154. doi: 10.1037/0022-006X.72.2.139. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Sampson RJ, Raudenbush SW, Felton E. Neighborhoods and Violent Crime: A Multilevel Study of Collective Efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Israel BA, Zenk SN, Parker EA, Lichtenstein R, Shellman-Weir S, et al. Psychosocial stress and social support as mediators of relationships between income, length of residence and depressive symptoms among African American women on Detroit's eastside. Social Science & Medicine. 2006;62(2):510–522. doi: 10.1016/j.socscimed.2005.06.028. [DOI] [PubMed] [Google Scholar]
- Shadel WG, Cervone D. Evaluating social-cognitive mechanisms that regulate self-efficacy in response to provocative smoking cues: An experimental investigation. Psychology of Addictive Behaviors. 2006;20(1):91–96. doi: 10.1037/0893-164X.20.1.91. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Engberg JB, Paty JA, Perz WG, Gnys M, Kassel JD, et al. A day at a time: Predicting smoking lapse from daily urge. Journal of Abnormal Psychology. 1997;106(1):104–116. doi: 10.1037//0021-843x.106.1.104. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: Within-subjects analysis of real-time reports. Journal of Consulting & Clinical Psychology. 1996;64(2):366–379. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Waters AJ. Negative affect and smoking lapses: A prospective analysis. Journal of Consulting & Clinical Psychology. 2004;72(2):192–201. doi: 10.1037/0022-006X.72.2.192. [DOI] [PubMed] [Google Scholar]
- Siahpush M, McNeill A, Borland R, Fong GT. Socioeconomic variations in nicotine dependence, self-efficacy, and intention to quit across four countries: findings from the International Tobacco Control (ITC) Four Country Survey. Tobacco Control. 2006;15 Suppl 3:ii71–0. doi: 10.1136/tc.2004.008763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E, Hunt MK, Emmons K. Reducing social disparities in tobacco use: A social-contextual model for reducing tobacco use among blue-collar workers. American Journal of Public Health. 2004;94(2):230–239. doi: 10.2105/ajph.94.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapleton J. Cigarette smoking prevalence, cessation and relapse. Statistical Methods in Medical Research. 1998;7(2):187–203. doi: 10.1177/096228029800700206. [DOI] [PubMed] [Google Scholar]
- Steiger JH. Structural model equation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine. 2001;23(3):177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Ullman JB. Structural equation modeling: Reviewing the basics and moving forward. Journal of Personality Assessment. 2006;87(1):35–50. doi: 10.1207/s15327752jpa8701_03. [DOI] [PubMed] [Google Scholar]
- Velicer WF, Diclemente CC, Rossi JS, Prochaska JO. Relapse situations and self-efficacy: An integrative model. Addictive Behaviors. 1990;15(3):271–283. doi: 10.1016/0306-4603(90)90070-e. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality & Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Brandon TH, Baker TB. The relation of affective processing measures and smoking motivation indices among college-age smokers. Advances in Behaviour Research & Therapy. 1992;14(3):169–193. [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Yen IH, Yelin EH, Katz P, Eisner MD, Blanc PD, Yen IH, et al. Perceived neighborhood problems and quality of life, physical functioning, and depressive symptoms among adults with asthma. American Journal of Public Health. 2006;96(5):873–879. doi: 10.2105/AJPH.2004.059253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu CY, Muthén B. Evaluation of model fit indices for latent variable models with categorical and continuous outcomes (Technical Report) Los Angeles: University of California at Los Angeles, Graduate School of Education and Information Studies; 2002. [Google Scholar]