Abstract
We present evidence from a five year longitudinal study for the prospective associations between loneliness and depressive symptoms in a population-based, ethnically diverse sample of 229 men and women who were 50-68 years old at study onset. Cross-lagged panel models were used in which the criterion variables were loneliness and depressive symptoms considered simultaneously. Variations on this model evaluated the possible effects of gender, ethnicity, education, physical functioning, medications, social network size, neuroticism, stressful life events, perceived stress, and social support on the observed associations between loneliness and depressive symptoms. Cross-lag analyses indicated that loneliness predicted subsequent changes in depressive symptomatology but not vice versa, and that this temporal association was not attributable to demographic variables, objective social isolation, dispositional negativity, stress, or social support. The importance of distinguishing between loneliness and depressive symptoms and the implications for loneliness and depressive symptomatology in older adults are discussed.
Keywords: depressive symptoms, loneliness, social isolation, stress, social support
Loneliness and the feeling of being unwanted is the most terrible poverty. (Mother Teresa)
The word “solitude” expresses the glory of being alone, whereas the word “loneliness” expresses the pain of feeling alone (Tillich, 1959). Millions of people suffer daily from loneliness (Rubenstein & Shaver, 1982; Steffick, 2000), a debilitating psychological condition characterized by a deep sense of emptiness, worthlessness, lack of control, and personal threat (Booth, 2000; Cacioppo & Patrick, 2008; Weiss, 1973). Twin studies reveal that loneliness is temporally stable and heritable, with approximately equal parts attributable to heritable and non-shared environmental factors in adulthood (Boomsma, Willemsen, Dolan, Hawkley, & Cacioppo, 2005; Boomsma, Cacioppo, Muthen, Asparouhov, & Clark, 2007). People can feel lonely in a marriage or in a crowd (Cacioppo et al., 2000; Tornstam, 1992), but certain situational factors heighten the risk for increased loneliness. These include low socioeconomic status, poor marital quality, infrequent contact with friends and family, few social roles, lack of participation in voluntary organizations, physical health symptoms, and physical limitations (Hawkley et al., 2008; Savikko, Routasalo, Tilvis, Strandberg, & Pitkala, 2005).
Loneliness, in turn, is a risk factor for various physiological and health outcomes. Moreover, these outcomes are not adequately predicted by objective social isolation or social support, constructs that are often mistakenly equated with loneliness. Independent of objective social isolation or social support, loneliness has been associated with increased vascular resistance (Cacioppo, Hawkley, Crawford et al., 2002), elevated blood pressure (Cacioppo, Hawkley, Crawford et al., 2002; Hawkley, Masi, Berry, & Cacioppo, 2006), increased hypothalamic pituitary adrenocortical activity (Adam, Hawkley, Kudielka, & Cacioppo, 2006; Steptoe, Owen, Kunz-Ebrecht, & Brydon, 2004), under-expression of genes bearing anti-inflammatory glucocorticoid response elements (GREs) and over-expression of genes bearing response elements for pro-inflammatory NF-κB/Rel transcription factors (Cole et al., 2007), impaired sleep (Cacioppo, Hawkley, Berntson et al., 2002; Pressman et al., 2005), altered immunity (Kiecolt-Glaser et al., 1984; Pressman et al., 2005), alcoholism (Akerlind & Hornquist, 1992; Bell, 1956), progression of Alzheimer's Disease (Wilson et al., 2007), obesity (Lauder, Mummery, Jones, & Caperchione, 2006), and poorer physical health (Caspi, Harrington, Moffitt, Milne, & Poulton, 2006; Cornwell & Waite, 2009; Lynch, 1977). Moreover, loneliness has been shown to prospectively predict admission to a nursing home (Russell, Cutrona, De La Mora, & Wallace, 1997). Finally, loneliness has been associated with psychiatric conditions such as personality disorders (Overholser, 1992; Richman & Sokolove, 1992), hypochondriasis (Brink & Niemeyer, 1993), schizophrenia (Deniro, 1995; Neeleman & Power, 1994), suicidal ideation and behavior (Goldsmith, Pellmar, Kleinman, & Bunney, 2002; Wenz, 1977), and depression (Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006; Peplau, Russell, & Heim, 1979; Russell, 1982; Russell, Cutrona, Rose, & Yurko, 1984; Russell, Peplau, & Ferguson, 1978; Sergin, 1998; Weeks, Michela, Peplau, & Bragg, 1980; Weiss, 1973).
The conceptual association between loneliness and depressive symptoms has led to items such as “I felt lonely” being included in putative measures of depressive symptomatology (Radloff, 1977). From a theoretical perspective, loneliness and depression are overlapping aversive, unpleasant states, but Weiss (Weiss, 1973) distinguished between them by characterizing loneliness as how people feel about their social connections in particular and depression as how people feel generally. Empirical studies designed to determine the relationship between loneliness and depressive symptoms have found them to be distinct conditions statistically (e.g.,(Bell, 1985; Cacioppo, Hawkley et al., 2006; Cacioppo, Hughes et al., 2006; Rook, 1987; Russell, 1996; Weeks et al., 1980) and functionally (e.g., Adam et al., 2006; Cole et al., 2007; Hawkley et al., 2006). Moreover, loneliness and depressive symptoms are only moderately correlated (r's=.4-.6) in middle age and older adults (Adams, Sanders, & Auth, 2004; Cacioppo, Hughes et al., 2006). The existing longitudinal research further supports the distinction between loneliness and depressive symptomatology, and loneliness predicts increases in depressive symptomatology above and beyond what can be explained by initial levels of depressive symptomatology (e.g., Cacioppo, Hughes et al., 2006; Green et al., 1992; Hagerty & Williams, 1999; Heikkinen & Kauppinen, 2004; Wei, Russell, & Zakalik, 2005); cf. (Weeks et al., 1980).
Although the finding that loneliness predicts increases in depressive symptoms appears well-established, there are several limitations in these longitudinal studies that we sought to address in the present research. First, longitudinal analyses have relied on regression or latent growth models in which depressive symptomatology served as the criterion measure. In the present study, we used cross-lag panel models in which the criterion variables are loneliness and depressive symptoms, considered together, which makes it possible to formally test for reciprocal predictive relationships.
Second, loneliness and depressive symptoms each have been found to be associated with other individual characteristics, including objective social isolation, general negativity, objective and perceived stress, and low social support (e.g., see (Berscheid & Reis, 1998; Cacioppo, Hawkley et al., 2006; Peplau & Goldston, 1984). The extent to which loneliness predicts depressive symptoms by the operation of one of these factors acting as a spurious third variable is not clear. In the present study, a series of cross-lag panel analyses were performed to determine the extent to which any of these variables could account for any observed longitudinal associations between loneliness and depressive symptoms. Because each of these variables could change annually, they were modeled accordingly in our longitudinal analyses.
Third, most studies have not considered the possible effects of gender, ethnicity, education, psychiatric diagnosis, use of antidepressant medications, or physical functioning. We incorporated these factors into the cross-lag panel analyses, and those variables that could change (e.g., psychiatric diagnosis, use of antidepressant medication, physical functioning) were modeled accordingly.
Finally, most prior longitudinal studies of loneliness and depressive symptoms cannot be generalized easily to our aging population. For instance, most have relied on convenience samples. The present study uses a population-based sample of middle aged and older Euro-American, African American, and Latino American women and men to permit generalization of the results to older American adults. In addition, the longitudinal analyses have been limited to one or two waves of measurement, typically across a year or less. The paucity of waves in these studies may constrain the varieties of life events to which middle age and older adults are exposed. In the present study, we report data from five one-year waves of data collection to determine the relationship between loneliness and depressive symptoms in a sample of individuals born between 1935 and 1952.
Method
Participants
Data for this study were collected annually for five years, from 2002-2006, as part of the Chicago Health, Aging, and Social Relations Study (CHASRS). CHASRS is a longitudinal, population-based study of non-Hispanic White, African American, and non-Black Latino American persons born between 1935 and 1952, and living in Cook County, IL. The sample was selected using a multistage probability design in which the first stage involved identifying a subset of households estimated to have high probability of containing at least one adult aged 50-65 years (24 percent of the total frame). A stratified, equal-probability-of-selection sample was drawn from this subset. The three strata were (1) households from census tracts in which at least 80 percent of the residents were African American, (2) households for which the associated surname was identified by the U.S. Census Department as “Hispanic”, and (3) all remaining households. The second stage involved selecting one age-eligible individual per household, and screening selected individuals to include only those who belonged to one of the three racial/ethnic groups of interest and were sufficiently ambulatory to come to the University and participate in the study. A quota sampling strategy was used at both the household and individual levels to achieve an approximately equal distribution of participants across the six gender by racial/ethnic group combinations. Response rates approached 45% overall, an impressive rate given that participation in our study involved predominantly working adults spending an entire day at the University. The final sample consisted of 229 individuals who ranged from 50-68 years of age on the first testing occasion.
The target population was non-Hispanic Caucasian, African American, and non-black Latino American persons (hereafter referred to as White, Black, and Hispanic, respectively) between the ages of 50 and 68 living in Cook County, IL, who were English-speaking and sufficiently ambulatory to come to the University of Chicago for a daylong visit to the laboratory. The sample was selected using a multistage probability design in which African Americans and Latino Americans were oversampled and gender equality maintained. The final sample size in Year 1 of CHASRS is 229. Sample attrition over the course of the 5-year study averaged 7.2% annually, resulting in a sample size of 163 in Year 5. Sample attrition did not differ as a function of depressive symptoms (p = .08) or loneliness (p = .15). Subjects were paid $126US each year for participating in the study.
Procedures
Annual testing of subjects occurred over the entire 12-month calendar year, and the testing interval averaged 11.6 months (SD=1.1). Subjects arrived at the laboratory between 8:00 and 9:00 a.m. for a full day of testing that included standard psychological and demographic surveys, health and medication interviews, anthropometric measurements, and a cardiovascular protocol. All psychological and demographic measures reported in this paper were obtained in the first survey packet completed by participants. Participants were asked to bring their medications with them to the laboratory, and experimenters recorded drug name, dosage, and frequency for subsequent coding.
The UCLA Loneliness Scale-Revised (UCLA-R) has been shown to possess construct validity (Russell, Peplau, & Cutrona, 1980; Russell, 1996) as a measure of general loneliness and degree of satisfaction with one's social network. The UCLA-R captures a three-dimensional representation of loneliness that reflects inadequate intimate attachments as well as inadequate relational and collective attachments (Hawkley, Browne, & Cacioppo, 2005). Each of the 20 items is rated on a scale of 1 (never), 2 (rarely), 3 (sometimes), and 4 (often). Cronbach's alpha across all 20 items ranged from .90 to .92 across all 5 years of CHASRS (mean = .91). After reverse scoring appropriate items, loneliness scores are calculated by summing all items. The range of possible scores is 20 to 80, with higher scores signifying greater loneliness.
The Center for Epidemiologic Studies Depression Scale (CESD) is a 20-item self-report questionnaire that assesses depressive feelings and behaviors experienced during the past week. Radloff (Radloff, 1977) reported good psychometric properties of this scale. In our sample, Cronbach's alpha across all 20 items ranged from .88 to .89 across all 5 years of CHASRS (mean = .89). Responses to each item were recorded using a 4-point Likert scale that ranged from 0 (rarely or none of the time) to 3 (most or all of the time). One item in the CESD asks whether the respondent felt lonely, and responses to this item were not included when calculating the total score on the CESD to ensure any prediction of depressive symptoms by loneliness was not due to item overlap. A depressive symptom score was computed by summing the responses to the remaining 19 items, yielding a scale score range of 0 (low depressive symptoms) to 56 (high depressive symptoms). We refer to this total score as CESDML (i.e., CESD Minus the Loneliness item).
Demographic covariates included because of their known associations with depressive symptoms and/or loneliness were age at study onset, gender, years of education, and marital status (Pinquart & Sorenson, 2003), as well as race/ethnicity (George & Lynch, 2003). Time-varying covariates known to be associated with loneliness and/or depressive symptoms included antidepressant medications, psychiatric diagnosis (self-report), and physical functioning. Antidepressant medications were coded using a standardized scheme available from www.multum.com. The Multum database permits coding of generic and brand name drugs by pharmacologic and therapeutic categories. Antidepressant medications include SNRI's, SSRI's, MAO inhibitors, and phenylpiperazine, tetracyclic, and tricyclic antidepressants. A psychiatric diagnosis was recorded if, during a health interview, subjects reported having had or having been told by a doctor that they have emotional, nervous, or psychiatric problems. Physical functioning was assessed using the corresponding subscale of the RAND 36-Item Health Survey (Version 1.0) (Ware & Sherbourne, 1992). Scores range from 0 to 100% and reflect the ability to engage in light (e.g., walking one block, dressing oneself), moderate (e.g., pushing a vacuum cleaner), and vigorous activities (e.g., running, lifting heavy objects).
In additional models, the social network index, neuroticism, stressful life events, perceived stress, and social support were employed as covariates to assess whether reciprocal lagged relationships between loneliness and depressive symptoms were independent of the lagged effects of these related psychosocial variables.
The social network index (SNI) was computed by following, as closely as possible, the procedure described by Berkman and Syme (Berkman & Syme, 1979). Four dichotomous variables were summed to generate a total SNI: being married or living with a partner, having close friends or relatives, belonging to a voluntary group or club, attending church services at least twice a month. Scores could range from 0 (no connections) to 4 (most connections); in our sample, no one scored “0” and only 8% of the sample scored “1.” Because the SNI incorporates marital status, marital status was not included as a covariate when modeling the effect of SNI on the lagged relationships between loneliness and depressive symptoms. . The Big 5 personality inventory (Goldberg, 1992) was used to measure emotional stability (the opposite of neuroticism), and in the reporting of results, we reverse the direction of the effects of emotional stability to correspond to the construct of neuroticism. Life events that had occurred in the prior 12 months were assessed using a 51-item checklist (based on the revised social readjustment rating scale (Hobson et al., 1998); and events were summed to represent exposure to significant life stress. Perceptions of stress were measured using the Perceived Stress Scale (PSS; (Cohen, Kamarck, & Mermelstein, 1983). Social support was measured using the 12-item Interpersonal Support Evaluation List (ISEL; (Cohen & Hoberman, 1983; Cohen, Mermelstein, Kamarck, & Hoberman, 1985), and responses were averaged across the three subscales (i.e., tangible, appraisal, and belonging). The psychometric characteristics of these scales in the CHASRS study have been reported elsewhere (Hawkley et al., 2006).
Data Analysis
Cross-lagged path analysis is widely used to infer causal associations in data from longitudinal research designs. Analyses were conducted using an autoregressive cross-lagged (ARCL) panel model approach (Curran, 2000) to simultaneously address reciprocal influences on loneliness and depressive symptoms. Using a cross-lagged modeling technique, the pattern of effects is conceptually replicated at each timepoint. We report unstandardized regression coefficients (B) and 95% confidence intervals throughout. The cross-lagged panel analyses were conducted with MPlus (version 5; (Muthen & Muthen, 2002). Missing data were not imputed; rather, available data from all 229 subjects were used in analyses, and all analyses were conducted using full information maximum likelihood estimation with robust standard errors (MLR). In the present study, covariance coverage values, which indicate the proportion of data present to estimate each pairwise relationship, ranged from 66% to 100%.
The degree of model fit was assessed using the chi-square goodness of fit statistic and the root mean square error of approximation (RMSEA; (Browne & Cudeck, 1992). MacCallum, Browne, and Sugawara (Maccallum, Browne, & Sugawara, 1996) characterize a model with an RMSEA of .08 or less as an adequate fit; Hu and Bentler (Hu & Bentler, 1999) characterize a model with an RMSEA of .05 or less as a good fit, and .10 or more as a poor fit.
Results
Table 1 provides sample characteristics of the CHASRS cohort. Table 2 lists means, standard deviations, and intercorrelations for the CESDML and UCLA-R loneliness values at each annual assessment. The CESDML and UCLA-R showed moderate temporal stability across years, r's > 0.6. Intercorrelations between the CESDML and UCLA-R when measured at the same point in time were also significant, r's = .42-.68.
Table 1.
Characteristics of the CHASRS sample (N=229, unless otherwise indicated).
| Age (yrs) | 57.4 (SD=4.5) |
| Female (%) | 52.4 |
| Ethnicity (%) | |
| White | 35.8 |
| Black | 35.4 |
| Hispanica | 28.8 |
| Education (years) (N = 223) | 13.3 (SD=3.1) |
| Married/living with partner | 61.6% |
| Anti-depressant medications (%) (N = 228) | 7.5 |
| Psychiatric diagnosis reported (%) (N = 226)b | 12.4 |
| Social Network Index (N = 225) | 2.9 (SD=0.9) |
| Physical functioning (N = 225) | 80.4 (SD=24.2) |
| Emotional stability (N = 213) | 5.6 (SD=0.9) |
| Life events (N = 228) | 4.4 (SD=3.2) |
| Perceived Stress (N = 223) | 13.3 (SD=6.4) |
| Social support (N = 218) | 12.9 (SD=2.2) |
CHASRS: Chicago Health, Aging, and Social Relations Study.
The greatest majority of these individuals are Mexican (72%), with the remaining individuals representing a wide range of ethnicities (e.g., Puerto Rican, Cuban, Chilean, Colombian, Dominican, etc.).
A psychiatric diagnosis was recorded if, during a health interview, subjects reported having had or having been told by a doctor that they have emotional, nervous, or psychiatric problems.
Table 2.
Means, standard deviations, and intercorrelations among CESDML and UCLA loneliness scores.
| Variable | M | SD | CESD ML, Year 1 | CESD ML, Year 2 | CESD ML, Year 3 | CESD ML, Year 4 | CESD ML, Year 5 | Loneliness, Year 1 | Loneliness, Year 2 | Loneliness, Year 3 | Loneliness, Year 4 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| CESDML, Year 1 (223) | 9.8 | 8.5 | 1 | ||||||||
| CESDML, Year 2 (205) | 10.2 | 8.7 | .70** | 1 | |||||||
| CESDML, Year 3 (190) | 9.0 | 8.0 | .67** | .69** | 1 | ||||||
| CESDML, Year 4 (176) | 8.9 | 8.0 | .61** | .66** | .70** | 1 | |||||
| CESDML, Year 5 (162) | 8.7 | 7.9 | .64** | .61** | .67** | .71** | 1 | ||||
| Loneliness, Year 1 (225) | 36.0 | 9.8 | .57** | .51** | .46** | .50** | .42** | 1 | |||
| Loneliness, Year 2 (206) | 35.4 | 9.7 | .54** | .68** | .58** | .61** | .54** | .76** | 1 | ||
| Loneliness, Year 3 (191) | 35.6 | 9.5 | .54** | .55* | .61** | .60** | .55** | .74** | .84** | 1 | |
| Loneliness, Year 4 (177) | 38.1 | 8.6 | .54** | .53** | .60** | .67** | .55** | .65** | .75** | .79** | 1 |
| Loneliness, Year 5 (162) | 36.8 | 8.1 | .48** | .53** | .58** | .61** | .57** | .63** | .78** | .79** | .83** |
CESDML = Depressive symptoms, minus loneliness item
p < .01
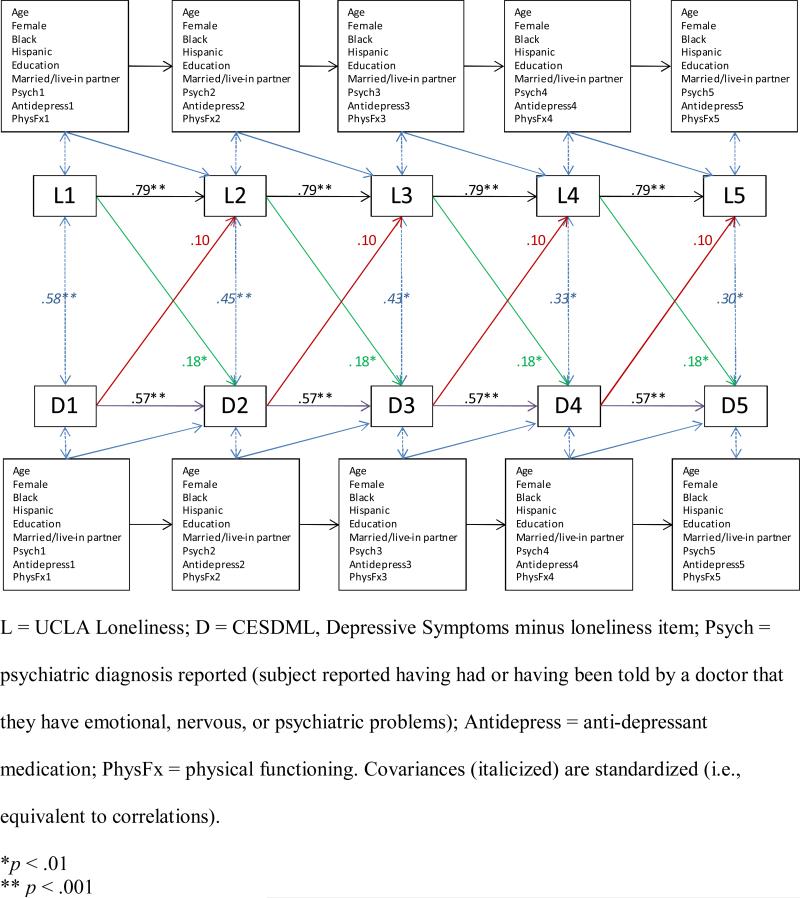
Cross-lagged panel models were specified to examine reciprocal relationships between depressive symptoms and loneliness over a total of four one-year intervals. Our theoretical model assumes that prospective relationships between variables are stable over time. These assumptions were modeled by applying equality constraints to the autoregressive and cross-lagged paths, thereby imposing “stationarity” on the relationships among variables in the model. In Figures 1– 5, autoregressive effects are represented as single-headed arrows running from a given variable at one time point to the same variable at the next time point. The abilities of depressive symptoms to prospectively predict loneliness and for loneliness to prospectively predict depressive symptoms over a one-year interval (i.e., cross-lagged effects) are illustrated by diagonal single-headed arrows. We also assumed that the one-year prospective effects of covariates (i.e., age, gender, race/ethnicity, years of education, married or live-in partner status, anti-depressant medication, psychiatric diagnosis, and physical functioning) on depressive symptoms and loneliness did not differ from year to year, and equality constraints were therefore applied to each of these covariates over the four one-year intervals. The effects of covariates are illustrated by diagonal single-headed arrows. Correlations between variables at a given time are illustrated by double-headed arrows.
Figure 1.
Cross-lagged panel model showing that loneliness predicts increases in depressive symptoms independent of covariates. Regression weights are unstandardized.
Figure 5.
Cross-lagged panel model showing that loneliness predicts increases in depressive symptoms independent of perceived stress (and demographic, health, and medication covariates included in Figure 1, but not shown here). Regression weights are unstandardized.
The results for the model summarized in Figure 1 supported the stationary process assumption and fit the data adequately, χ2(225) = 476.332, p < .0001; RMSEA = .070, 90% CI: .061, .079. The UCLA-R exhibited significant temporal stability (B = 0.79, 95% C.I.: 0.66, 0.92), as did the CESDML (B = 0.570, 95% C.I.: 0.36, 0.71). In addition, the one-year lagged effect of loneliness on depressive symptoms was significant (B = 0.18, 95% C.I.: 0.09, 0.30). The one-year lagged effect of depressive symptoms on loneliness did not achieve statistical significance (B = 0.10, 95% C.I.: -0.05, 0.20). These pathways and estimates are displayed in Figure 1 and provide evidence that supports conceptual and empirical distinctions between loneliness and depressive symptoms.
Significant cross-sectional associations were evident among measures at baseline (Year 1; see Table 3). Loneliness levels and depressive symptoms were higher in those with a psychiatric diagnosis and with a greater degree of physical functional impairment, and lower in those with higher levels of education. Depressive symptoms were also higher among Hispanics than Whites and higher in those on anti-depressant medication. A psychiatric diagnosis was more likely among the more educated, and less likely among married individuals. Females were less likely to be married or have a live-in partner at baseline. Physical functioning was less impaired among females and more highly educated individuals, and tended to be more impaired among older individuals. Hispanics were significantly younger than Whites. The only covariate with a significant lagged effect was age. With each additional year, loneliness decreased (B = -0.45, 95% C.I.: -0.66, -0.32). This effect did not alter the influence of loneliness on depressive symptoms.
Table 3.
Intercorrelations among variables at baseline (Year 1).a
| Variable | CESDML | Loneliness | Psych | Anti-depress | PhysFx | Age | Female | Black (vs. other) | Hispanic (vs. other) | Years education |
|---|---|---|---|---|---|---|---|---|---|---|
| CESDML | 1 | |||||||||
| Loneliness | .58** | 1 | ||||||||
| Psych | .21* | .19* | 1 | |||||||
| Anti-depress | .35** | .13 | .40** | 1 | ||||||
| PhysFx | −.30** | −.22* | −.10 | −.06 | 1 | |||||
| Age | −.14 | −.08 | −.05 | −.07 | −.15 | 1 | ||||
| Female | .08 | −.12 | .13 | .15 | −.22** | −.02 | 1 | |||
| Black (vs. other) | .11 | .06 | −.08 | −.01 | −.10 | .14 | .02 | 1 | ||
| Hispanic (vs. other) | .20* | .12 | .12 | .08 | −.05 | −.26** | −.00 | −.47** | 1 | |
| Years education | −.25** | −.15* | .16** | .01 | .17* | −.02 | .04 | −.13 | −.22** | 1 |
| Married/live-in partner | −.10 | −.11 | −.15* | −.09 | .10 | −.01 | −.30** | −.12 | −.08 | −.03 |
CESDML = Depressive symptoms, minus loneliness item; Psych = psychiatric diagnosis reported (subject reported having had or having been told by a doctor that they have emotional, nervous, or psychiatric problems); Antidepress = anti-depressant medication; PhysFx = physical functioning.
Correlation coefficients are standardized regression coefficients obtained in the cross-lagged panel analysis depicted in Figure 1.
p < .05
p < .01.
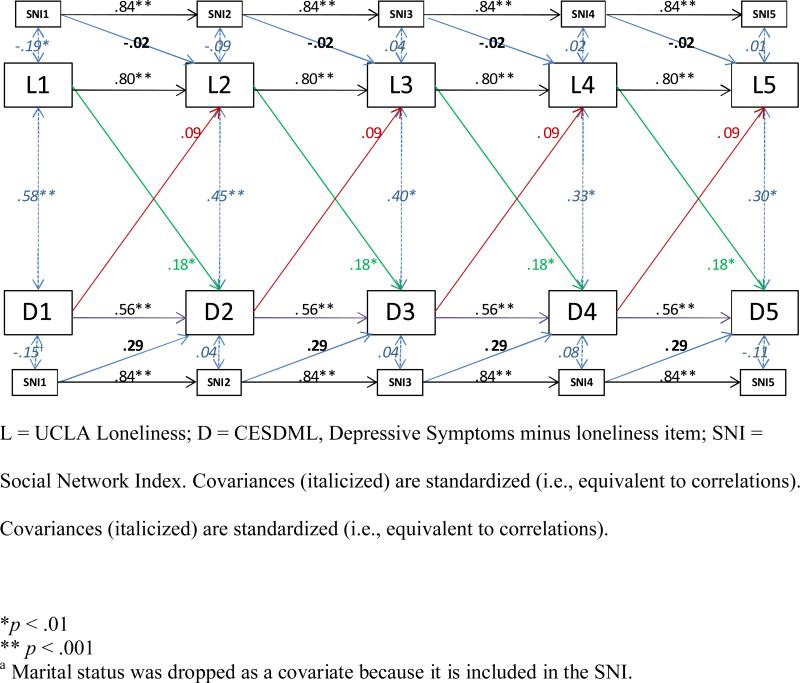
Are the relationships between loneliness and depressive symptoms attributable to differences in social isolation?
The next model examined whether the association between loneliness and depressive symptoms might be attributable to actual isolation. At baseline, social network size was found to be associated with loneliness (r = -.19, p < .05) and depressive symptoms (r = -.17, p < .05). Building on the model displayed in Figure 1, social network size was added as a covariate with one-year lagged effects on loneliness and depressive symptoms. This model, depicted in Figure 2, fit the data adequately, χ2(334) = 649.970, p < .0001; RMSEA = .064, 90% CI: .057, .072. The stationary lagged effect of social network size was not significant for loneliness (B = -0.02, 95% C.I.: -0.65, 0.49) or depressive symptoms (B = 0.28, 95% C.I.: -0.26, 0.91). Independent of neuroticism, the stationary cross-lagged effect of loneliness on depressive symptoms retained statistical significance (B = 0.18, 95% C.I.: 0.08, 0.29), and the influence of depressive symptoms on loneliness remained nonsignificant (B = 0.09, 95% C.I.: -0.07, 0.20).
Figure 2.
Cross-lagged panel model showing that loneliness predicts increases in depressive symptoms independent of social network size (and demographica, health, and medication covariates included in Figure 1, but not shown here). Regression weights are unstandardized.
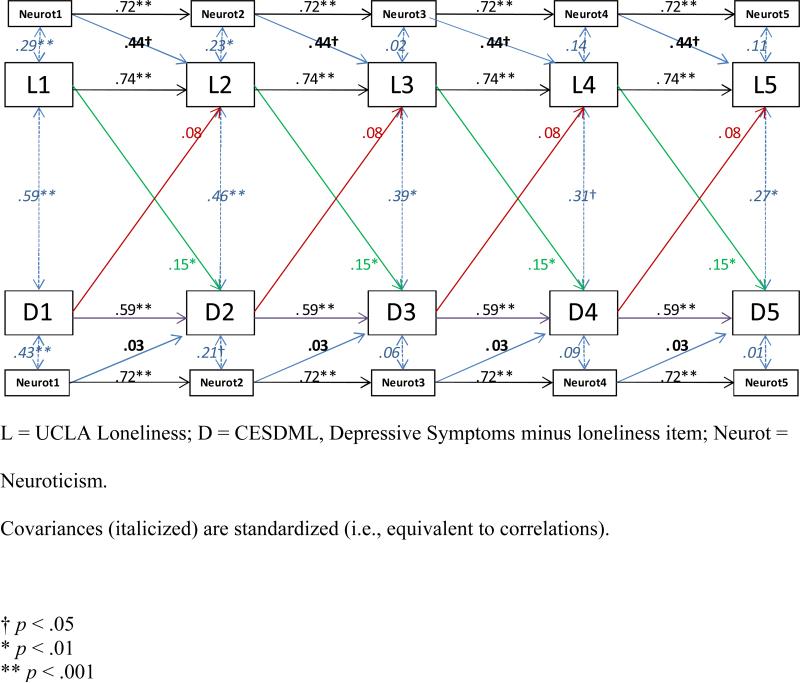
Are the relationships between loneliness and depressive symptoms reducible to general negativity?
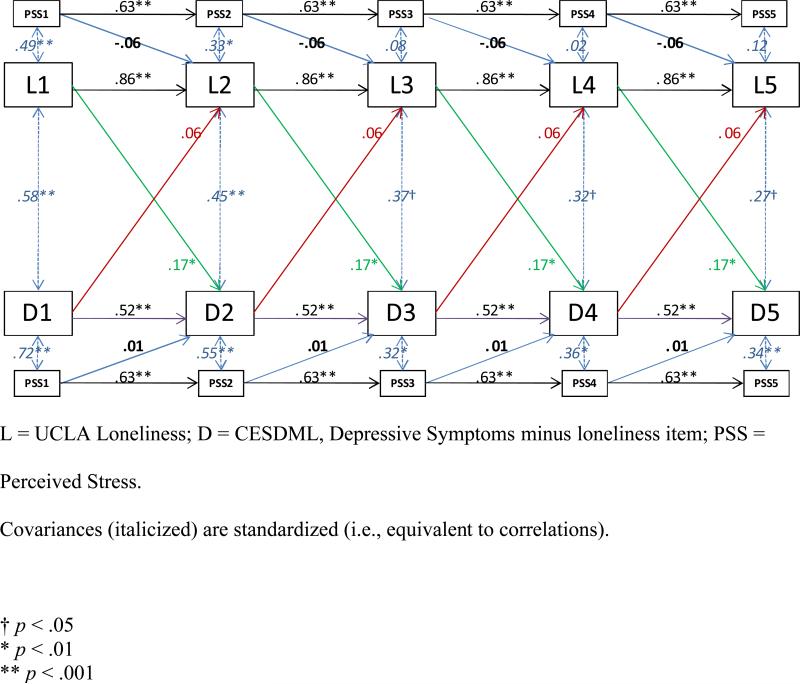
The next model examined whether the association between loneliness and depressive symptoms might be attributable to a more general negativity factor. At baseline, neuroticism was found to be associated with loneliness (r = .26, p < .05) and depressive symptoms (r = .39, p < .05). Building on the model displayed in Figure 1, neuroticism was added as a covariate with one-year lagged effects on loneliness and depressive symptoms. This model, depicted in Figure 3, fit the data adequately, χ2(332) = 722.891, p < .0001; RMSEA = .072, 90% CI: .065, .079. The stationary lagged effect of neuroticism was not significant for loneliness (B = 0.44, 95% C.I.: -0.45, 1.26) or depressive symptoms (B = 0.03, 95% C.I.: -0.83, 0.88). Independent of neuroticism, the stationary cross-lagged effect of loneliness on depressive symptoms retained statistical significance (B = 0.15, 95% C.I.: 0.04, 0.27), and the influence of depressive symptoms on loneliness remained nonsignificant (B = 0.08, 95% C.I.: -0.08, 0.18).
Figure 3.
Cross-lagged panel model showing that loneliness predicts increases in depressive symptoms independent of neuroticism (and demographic, health, and medication covariates included in Figure 1, but not shown here). Regression weights are unstandardized.
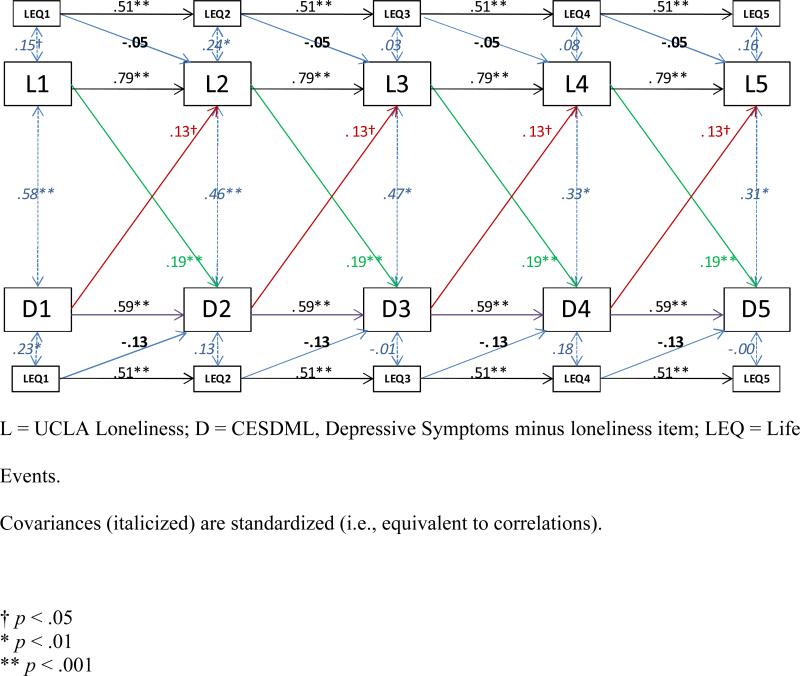
Are the relationships between loneliness and depressive symptoms reducible to exposure to stressful life events?
The number of stressful life events was found to be associated with loneliness (r = .15, p < .05) and depressive symptoms (r = .23, p < .05). To examine whether the association between loneliness and depressive symptoms was attributable to stressful events influencing both loneliness and depressive symptoms, a life event count was added as a covariate with one-year lagged effects on loneliness and depressive symptoms. The model, depicted in Figure 4, fit the data adequately, χ2(332) = 685.965, p < .0001; RMSEA = .068, 90% CI: .061, .075. Although life events exhibited small cross-sectional correlations with loneliness and depressive symptoms in Year 1, the stationary lagged effects of life events on loneliness, B = -0.05, and depressive symptoms, B = -0.13, were non-significant, p's > .1. The stationary cross-lagged effect of loneliness on depressive symptoms retained statistical significance independent of life events (B = 0.19, p < .01), and depressive symptoms had a significant influence on loneliness when life events were held constant (B = 0.13, 95% C.I.: 0.01, 0.27). Thus, the cross-lag association between loneliness and depressive symptoms does not appear to be attributable to stressful life events acting on both.
Figure 4.
Cross-lagged panel model showing a reciprocal association between loneliness and depressive symptoms independent of life events (and demographic, health, and medication covariates included in Figure 1, but not shown here). Regression weights are unstandardized.
Are the relationships between loneliness and depressive symptoms reducible to perceived stress?
Perceived stress was associated with loneliness (r = .49, p < .01) and depressive symptoms (r = .72, p < .001). To examine whether the temporal association between loneliness and depressive symptoms were attributable to the subjective experience of stress, perceived stress was added as a covariate to the base model with one-year lagged effects on loneliness and depressive symptoms. This model, depicted in Figure 5, fit the data adequately, χ2(332) = 707.318, p < .0001; RMSEA = .070, 90% CI: .063, .077. The stationary lagged effects of perceived stress were not significant for loneliness, B = -0.06, or depressive symptoms, B = 0.005, p's > .4. Independent of perceived stress, loneliness continued to exert a significant influence on depressive symptoms, B = 0.17, p < .01, but depressive symptoms did not exert a significant reciprocal effect on loneliness, B = 0.06, p > .4.
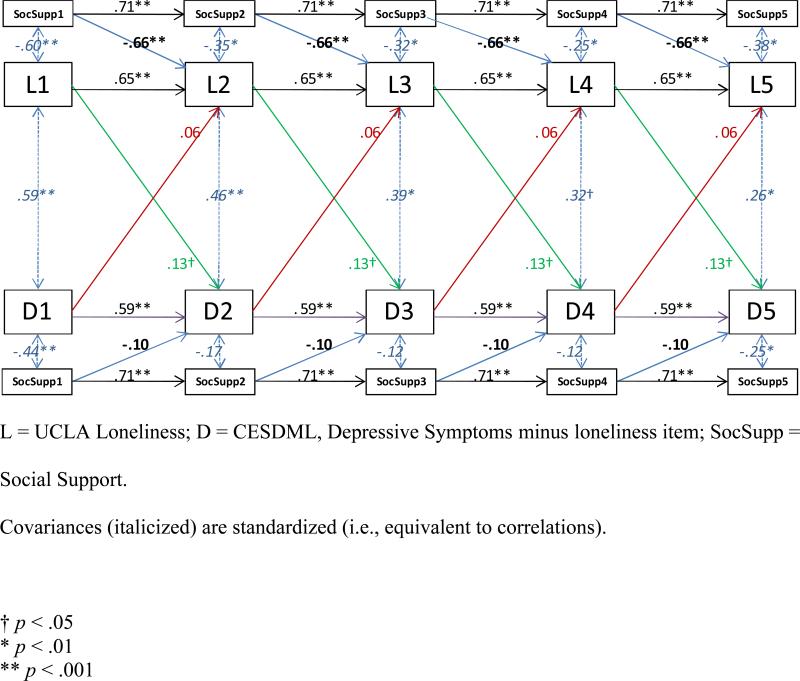
Are the relationships between loneliness and depressive symptoms reducible to social support?
The final model examined whether the reciprocal influences between loneliness and depressive symptoms were attributable to perceptions of social support that might attenuate the effects of stress. As expected, social support was associated with loneliness (r = -.58, p < .01) and depressive symptoms (r = -.41, p < .01). This model, depicted in Figure 6, fit the data adequately, χ2(332) = 774.096, p < .0001; RMSEA = .076, 90% CI: .069, .083. The stationary lagged effects of social support were significant for loneliness (B = -0.66, 95% C.I.: -1.09, -0.43), but not depressive symptoms, B = -0.10, p >.6. Independent of the effects of social support, loneliness continued to exert a significant influence on depressive symptoms, B = 0.13, p < .05, and depressive symptoms did not influence loneliness, B = 0.06, p > .3.
Figure 6.
Cross-lagged panel model showing that loneliness predicts increases in depressive symptoms independent of social support (and demographic, health, and medication covariates included in Figure 1, but not shown here). Regression weights are unstandardized.
Discussion
Much of the prior research on loneliness and depressive symptoms, particularly in the United States, has relied on convenience samples. Data from representative samples are needed if we are to understand loneliness as a risk factor for depressive symptomatology in middle age and older adults. The present study serves this purpose; adds to growing evidence for the conceptual, stochastic, and functional distinctions between loneliness and depressive symptoms; and provides evidence that loneliness predicts if not promotes increases in depressive symptomatology regardless of age, gender, or ethnicity. First, we found loneliness and depressive symptoms, as measured by the UCLA-R and CESDML, to be statistically separable. Second, we found loneliness in year n-1 to predict changes in depressive symptoms in year n above and beyond what could be explained by depressive symptoms in year n-1. Third, when demographic variables were considered in the models, the cross-lag analyses revealed that loneliness in year n-1 still predicted changes in depressive symptoms in year n above and beyond what could be explained by depressive symptoms in year n-1, but depressive symptomatology in year n-1 did not predict changes in loneliness in year n.
We constructed additional cross-lag analytic models to test alternative interpretations for these findings. To determine whether the possible effect of loneliness on depressive symptoms reflected the effects of objective rather than perceived social isolation, we performed the cross-lag model in which demographic factors and the time-varying factor of social network index served as covariates. To determine whether the possible effect of loneliness on depressive symptoms reflected different manifestations of personality differences in general negativity, we constructed a cross-lag model in which demographic factors and the time-covarying factor of neuroticism served as covariates. To determine whether the possible effect of loneliness on depressive symptoms reflected differences in exposure to stressful life events, we constructed a cross-lag model in which demographic factors and the time-covarying factor of stressful life events served as covariates. To determine whether perceived stress was the important variable, we performed the cross-lag model using perceived stress in the place of stressful life events. Finally, to determine whether the relationship between loneliness and depressive symptoms simply reflected the effects of social support, we constructed a cross-lag analytic model in which demographic factors and the time-covarying factor of social support served as covariates. In each case, we found loneliness to remain the significant predictor of changes in depressive symptomatology above and beyond what could be predicted by concurrent depressive symptomatology and the covariates. Thus, loneliness and its association with increases in depressive symptomatology cannot be reduced to demographic factors, objective social isolation, exposure to life stressors, perceived stress, negative affectivity, or social support.
Loneliness decreased over the course of the study, a finding that is consistent with prior research (Nolen-Hoeksema & Ahrens, 2002) showing that loneliness decreases from middle (45-55 yrs) to older age (65-75 yrs). These results correspond to increasing emotional closeness in relationships as people age and place greater priority on a select few relationships (Carstensen, Isaacowitz, & Charles, 1999). Nevertheless, the cross-sectional association between loneliness and depressive symptoms remains stable over the adult life span despite changes in loneliness (Nolen-Hoeksema & Ahrens, 2002), and our findings indicate that the prospective influence of loneliness on depressive symptoms is likewise independent of decreases in loneliness with age.
In addition, evidence was found to suggest why, in some prior studies, depressive symptomatology appeared to predict changes in loneliness. Specifically, when we performed the cross-lag panel model in which exposure to life stressors served as a covariate, depressive symptoms emerged as a significant predictor of changes in loneliness. This latter effect was small and warrants replication, but it suggests that exposure to life stressors masks the effect of depressive symptoms on changes in loneliness. Notably, it was the objective exposure to stressors, and not the perception of stress, that masked the effect of depressive symptoms on changes in loneliness. Importantly, exposure to life stressors did not alter or mask the effect of loneliness on subsequent changes in depressive symptoms. We conducted ancillary analyses to explore the source of masking (i.e., statistical suppression) and identified the presence of a psychiatric diagnosis as an explanation for the impact of depressive symptoms on loneliness changes when the lagged effect of life events was held constant. Specifically, when we excluded subjects with a psychiatric diagnosis at study onset (N = 28), depressive symptoms no longer predicted changes in loneliness (B = 0.03, SE = 0.08, p > .6) when life events were held constant. Loneliness, however, continued to predict changes in depressive symptoms (B = 0.19, SE = 0.05, p < .001). The subset of the sample with a psychiatric diagnosis was too small to obtain reliable estimates in a parallel cross-lagged model, but we infer that the effect of depressive symptoms on changes in loneliness is greater in those with than without a psychiatric diagnosis. Moreover, individuals with a self-reported psychiatric diagnosis also reported a greater number of stressful life events, r(226)Year 1 = .15, p <.05, suggesting that the influence of depressive symptoms on increases in loneliness among these individuals may be explained by greater exposure to life event stress. Additional research is needed to test this hypothesis.
In light of the possible role of loneliness in depressive symptoms, greater attention to loneliness may be important to maximize the likelihood people remain healthy and functional across the life span. The prior literature has tended to emphasize social support as the panacea. A literature search using PsycNet netted 2,904 articles in which the terms “social support” and “health” appeared in the abstract and the participants were middle age or older. When “loneliness” was used rather than “social support,” the search yielded only 320 articles. When the term “depression” was used in place of “health” in this search, “social support” yielded 1,422 articles whereas “loneliness” yielded only 228 articles. Of the articles on social support and depressive symptoms, only one appeared to be a longitudinal study (Heponiemi et al., 2006) – a 14 year study of social support and depressive symptoms in children and adolescents in Finland (loneliness was not included). This state of the literature is surprising in light of our empirical findings that we found: (a) loneliness is a strong longitudinal predictor of changes in depressive symptomatology even after covarying out any effects of social support, and (b) social support did not emerge as a significant longitudinal predictor of changes in depressive symptomatology in middle age and older adults.
Several limitations of this study should also be noted. First, although cross-lagged path analysis is widely used to infer causal associations in data from longitudinal research designs, experimental evidence would confer greater confidence in the causal role of loneliness on depressive symptoms and vice versa. Second, although our use of a population-based design has the advantage of permitting generalizations of the observed reciprocal associations between loneliness and depressive symptomatology to the population of middle-aged and older adults, clinical patients were not specifically recruited for study, and clinical depression was not measured. Whether or not the reciprocal association between loneliness and clinical depression is similar to the reciprocal influences observed in the current study participants is not known. Third, we relied on self-reported rather than examiner-rated assessments of depressive symptoms, and because the loneliness measure was similarly assessed by self-report, shared methodology may have confounded loneliness and depressive symptoms. On the other hand, our cross-lag analytic models held constant the concurrent associations between loneliness and depressive symptoms, and the reciprocal lagged relationships between loneliness and depressive symptoms were retained when this potential confounding was statistically controlled. Moreover, to the extent that general negativity (i.e., neuroticism) captures shared method variance in values of loneliness and depressive symptoms, statistical control for general negativity did not alter the reciprocal lagged relationships between loneliness and depressive symptoms.
In sum, the human need for social connection does not fade away in middle age and older adulthood. Five year cross-lag longitudinal analyses of data from an ethnically diverse representative sample show that loneliness predicts changes in depressive symptoms, and this temporal association is not attributable to objective social isolation, general negative affectivity, stress, or social support. Recognition of the importance of loneliness as a risk factor for changes in depressive symptoms may be important in mitigating its potentially deleterious effects on the quality of life of middle aged and older adults.
Acknowledgments
This research was supported by National Institute of Aging Program Project Grant No. PO1 AG18911 & RO1 AG034052-01.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/pag
Contributor Information
John T. Cacioppo, Center for Cognitive and Social Neuroscience, University of Chicago
Louise C. Hawkley, Center for Cognitive and Social Neuroscience, University of Chicago
Ronald A. Thisted, Department of Health Studies, University of Chicago
References
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience - cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Science USA. 2006;103(45):17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams KB, Sanders S, Auth EA. Loneliness and depression in independent living retirement communities: Risk and resilience factors. Aging and Mental Health. 2004;8(6):475–485. doi: 10.1080/13607860410001725054. [DOI] [PubMed] [Google Scholar]
- Akerlind I, Hornquist JO. Loneliness and alcohol abuse: A review of evidences of an interplay. Social Science and Medicine. 1992;34(4):405–414. doi: 10.1016/0277-9536(92)90300-f. [DOI] [PubMed] [Google Scholar]
- Bell RA. Conversational involvement and loneliness. Communication Monographs. 1985;52(3):218. [Google Scholar]
- Bell RG. Alcoholism and loneliness. Journal of Social Therapy. 1956;2:171–181. [Google Scholar]
- Berkman LF, Syme SL. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. American Journal of Epidemiology. 1979;109(2):186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- Berscheid E, Reis HT. Attraction and close relationships. In: Gilbert DT, Fiske ST, Lindzey G, editors. The Handbook of Social Psychology. 4th ed. Vol. 2. McGraw Hill; New York: 1998. pp. 193–281. [Google Scholar]
- Boomsma D, Willemsen G, Dolan C, Hawkley L, Cacioppo J. Genetic and environmental contributions to loneliness in adults: The Netherlands twin register study. Behavior Genetics. 2005;35(6):745–752. doi: 10.1007/s10519-005-6040-8. [DOI] [PubMed] [Google Scholar]
- Boomsma DI, Cacioppo JT, Muthen B, Asparouhov T, Clark S. Longitudinal genetic analysis for loneliness in Dutch twins. Twin Research & Human Genetics. 2007;10(2):267–273. doi: 10.1375/twin.10.2.267. [DOI] [PubMed] [Google Scholar]
- Booth R. Loneliness as a component of psychiatric disorders. Medscape General Medicine. 2000;2(2):1–7. [Google Scholar]
- Brink TL, Niemeyer L. Hypochondriasis, loneliness, and social functioning. Psychological Reports. 1993;72(3 Pt 2):1241–1242. doi: 10.2466/pr0.1993.72.3c.1241. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods Research. 1992;21(2):230–258. [Google Scholar]
- Cacioppo JT, Ernst JM, Burleson MH, McClintock MK, Malarkey WB, Hawkley LC, et al. Lonely traits and concomitant physiological processes: the MacArthur social neuroscience studies. International Journal of Psychophysiology. 2000;35(2-3):143–154. doi: 10.1016/s0167-8760(99)00049-5. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Berntson GG, Ernst JM, Gibbs AC, Stickgold R, et al. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychological Science. 2002;13(4):384–387. doi: 10.1111/1467-9280.00469. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalewski RB, et al. Loneliness and health: potential mechanisms. Psychosomatic Medicine. 2002;64(3):407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, et al. Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality. 2006;40(6):1054–1085. [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychology and Aging. 2006;21(1):140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Patrick B. Loneliness: Human nature and the need for social connection. W. W. Norton & Company; New York: 2008. [Google Scholar]
- Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: A theory of socioemotional selectivity. American Psychologist. 1999;54(3):165–181. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- Caspi A, Harrington H, Moffitt TE, Milne BJ, Poulton R. Socially isolated children 20 years later: Risk of cardiovascular disease. Archives of Pediatrics and Adolescent Medicine. 2006;160(8):805–811. doi: 10.1001/archpedi.160.8.805. [DOI] [PubMed] [Google Scholar]
- Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13(2):99–125. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason BR, Sarason IG, editors. Social Support: Theory, Research, and Applications. Martinus Nijhoff; The Hague, Netherlands: 1985. pp. 73–94. [Google Scholar]
- Cole SW, Hawkley LC, Arevalo JM, Sung CY, Rose RM, Cacioppo JT. Social regulation of gene expression in human leukocytes. Genome Biology. 2007;8(9):R189.181–R189.113. doi: 10.1186/gb-2007-8-9-r189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior. 2009;50:31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ. A latent curve framework for the study of developmental trajectories in adolescent substance use. In: Rose JS, Chassin L, Presson CC, Sherman SJ, editors. Multivariate applications in substance use research: New methods for new questions. Lawrence Erlbaum Associates; Mahwah, NJ: 2000. pp. 1–4. [Google Scholar]
- DeNiro DA. Perceived alienation in individuals with residual-type schizophrenia. Issues in Mental Health Nursing. 1995;16(3):185–200. doi: 10.3109/01612849509006934. [DOI] [PubMed] [Google Scholar]
- George LK, Lynch SM. Race differences in depressive symptoms: a dynamic perspective on stress exposure and vulnerability. Journal of Health and Social Behavior. 2003;44(3):353–369. [PubMed] [Google Scholar]
- Goldberg LR. The development of markers for the Big-Five factor structure. Psychological Assessment. 1992;4(1):26–42. [Google Scholar]
- Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE. Reducing suicide: A national imperative. National Academy Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- Green BH, Copeland JR, Dewey ME, Sharma V, Saunders PA, Davidson IA, et al. Risk factors for depression in elderly people: A prospective study. Acta Psychiatrica Scandinavica. 1992;86(3):213–217. doi: 10.1111/j.1600-0447.1992.tb03254.x. [DOI] [PubMed] [Google Scholar]
- Hagerty BM, Williams AR. The effects of sense of belonging, social support, conflict, and loneliness on depression. Nursing Research. 1999;48(4):215–219. doi: 10.1097/00006199-199907000-00004. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Browne MW, Cacioppo JT. How can I connect with thee? Let me count the ways. Psychological Science. 2005;16(10):798–804. doi: 10.1111/j.1467-9280.2005.01617.x. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, Cacioppo JT. From social structural factors to perceptions of relationship quality and loneliness: The Chicago Health, Aging, and Social Relations Study. Journal of Gerontology: Social Sciences. 2008;63B:S375–S384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychology and Aging. 2006;21(1):152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- Heikkinen R-L, Kauppinen M. Depressive symptoms in late life: A 10-year follow-up. Archives of Gerontology and Geriatrics. 2004;38(3):239–250. doi: 10.1016/j.archger.2003.10.004. [DOI] [PubMed] [Google Scholar]
- Heponiemi T, Elovainio M, Kivimaki M, Pulkki L, Puttonen S, Keltikangas-Jarvinen L. The longitudinal effects of social support and hostility on depressive tendencies. Social Science and Medicine. 2006;63(5):1374–1382. doi: 10.1016/j.socscimed.2006.03.036. [DOI] [PubMed] [Google Scholar]
- Hobson CJ, Kamen J, Szostek J, Nethercut CM, Tiedmann JW, Wojnarowicz S. Stressful life events: A revision and update of the social readjustment rating scale. International Journal of Stress Management. 1998;5(1):1–23. [Google Scholar]
- Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1. [Google Scholar]
- Kiecolt-Glaser JK, Garner W, Speicher C, Penn GM, Holliday J, Glaser R. Psychosocial modifiers of immunocompetence in medical students. Psychosomatic Medicine. 1984;46(1):7–14. doi: 10.1097/00006842-198401000-00003. [DOI] [PubMed] [Google Scholar]
- Lauder W, Mummery K, Jones M, Caperchione C. A comparison of health behaviors in lonely and non-lonely populations. Psychology, Health & Medicine. 2006;11(2):233–245. doi: 10.1080/13548500500266607. [DOI] [PubMed] [Google Scholar]
- Lynch JJ. The broken heart: the medical consequences of loneliness. Basic Books; New York: 1977. [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1(2):130–149. [Google Scholar]
- Muthen B, Muthen L. MPlus: The comprehensive modeling program for applied researchers. Muthen & Muthen; Los Angeles: 2002. [Google Scholar]
- Neeleman J, Power MJ. Social support and depression in three groups of psychiatric patients and a group of medical controls. Social Psychiatry and Psychiatric Epidemiology. 1994;29(1):46–51. doi: 10.1007/BF00796448. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Ahrens C. Age differences and similarities in the correlates of depressive symptoms. Psychology and Aging. 2002;17(1):116–124. doi: 10.1037//0882-7974.17.1.116. [DOI] [PubMed] [Google Scholar]
- Overholser JC. Sense of humor when coping with life stress. Personality and Individual Differences. 1992;13(7):799–804. [Google Scholar]
- Peplau L, Russell D, Heim M. The experience of loneliness. In: Frieze IH, Bar-Tal D, Carroll JS, editors. New approaches to social problems: Applications of attribution theory. Jossey - Bass; San Francisco: 1979. pp. 53–78. [Google Scholar]
- Peplau LA, Goldston SE. Preventing the harmful consequences of severe and persistent loneliness. National Institute of Mental Health; Rockville, MD: 1984. [Google Scholar]
- Pinquart M, Sorenson S. Risk factors for loneliness in adulthood and old age - a meta-analysis. In: Shohov SP, editor. Advances in Psychology Research. Vol. 19. Nova Publishers; Hauppauge, NY: 2003. pp. 111–143. [Google Scholar]
- Pressman SD, Cohen S, Miller GE, Barkin A, Rabin BS, Treanor JJ. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychology. 2005;24(3):297–306. doi: 10.1037/0278-6133.24.3.297. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Richman NE, Sokolove RL. The experience of aloneness, object representation, and evocative memory in borderline and neurotic patients. Psychoanalytic Psychology. 1992;9:77–91. [Google Scholar]
- Rook KS. Social support versus companionship: effects on life stress, loneliness, and evaluations by others. Journal of Personality and Social Psychology. 1987;52(6):1132–1147. doi: 10.1037//0022-3514.52.6.1132. [DOI] [PubMed] [Google Scholar]
- Rubenstein C, Shaver PR. The experience of loneliness. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research, and therapy. Wiley - Interscience; New York: 1982. pp. 206–223. [Google Scholar]
- Russell D. The measurement of loneliness. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research, and therapy. John Wiley & Sons; New York: 1982. pp. 81–104. [Google Scholar]
- Russell D, Cutrona CE, Rose J, Yurko K. Social and emotional loneliness: An examination of Weiss's typology of loneliness. Journal of Personality and Social Psychology. 1984;46(6):1313–1321. doi: 10.1037//0022-3514.46.6.1313. [DOI] [PubMed] [Google Scholar]
- Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology. 1980;39(3):472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Russell D, Peplau LA, Ferguson ML. Developing a measure of loneliness. Journal of Personality Assessment. 1978;42(3):290–294. doi: 10.1207/s15327752jpa4203_11. [DOI] [PubMed] [Google Scholar]
- Russell DW. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Russell DW, Cutrona CE, de la Mora A, Wallace RB. Loneliness and nursing home admission among rural older adults. Psychology and Aging. 1997;12(4):574–589. doi: 10.1037//0882-7974.12.4.574. [DOI] [PubMed] [Google Scholar]
- Savikko N, Routasalo P, Tilvis RS, Strandberg TE, Pitkala KH. Predictors and subjective causes of loneliness in an aged population. Archives of Gerontology and Geriatrics. 2005;41(3):223–233. doi: 10.1016/j.archger.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Segrin C. Interpersonal communication problems associated with depression and loneliness. In: Andersen PA, Guerrero LA, editors. Handbook of communication and emotion: Research, theory, applications, and contexts. Academic Press, Inc.; San Diego, CA: 1998. pp. 215–242. [Google Scholar]
- Steffick DE. Documentation on affective functioning measures in the Health and Retirement Study. University of Michigan, Survey Research Center; Ann Arbor: 2000. [Google Scholar]
- Steptoe A, Owen N, Kunz-Ebrecht SR, Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology. 2004;29(5):593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- Tillich P. The eternal now. In: Feifel H, editor. The meaning of death. McGraw-Hill; New York: 1959. pp. 30–38. [Google Scholar]
- Tornstam L. Loneliness in marriage. Journal of Social and Personal Relationships. 1992;9(2):197–217. [Google Scholar]
- Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF- 36). I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Weeks DG, Michela JL, Peplau LA, Bragg ME. Relation between loneliness and depression: A structural equation analysis. Journal of Personality and Social Psychology. 1980;39(6):1238–1244. doi: 10.1037/h0077709. [DOI] [PubMed] [Google Scholar]
- Wei M, Russell DW, Zakalik RA. Adult attachment, social self-efficacy, self-disclosure, loneliness, and subsequent depression for freshman college students: A longitudinal study. Journal of Counseling Psychology. 2005;52(4):602–614. [Google Scholar]
- Weiss RS. Loneliness: The experience of emotional and social isolation. MIT Press; Cambridge, MA: 1973. [Google Scholar]
- Wenz FV. Seasonal suicide attempts and forms of loneliness. Psychological Reports. 1977;40(3 Pt 2):807–810. doi: 10.2466/pr0.1977.40.3.807. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. Loneliness and risk of Alzheimer disease. Archives of General Psychiatry. 2007;64(2):234–240. doi: 10.1001/archpsyc.64.2.234. [DOI] [PubMed] [Google Scholar]