Abstract
The aim of this study was to test the hypothesis that a prolonged re-feeding duration after successful VLED-induced weight loss beneficially affects weight development and eating behaviour. 269 patients were recruited to a one-year obesity treatment program with 12 weeks of initial very-low-energy diet (VLED). After VLED, patients with ≥10% weight loss were randomly allocated to one week (Group 1) or six weeks (Group 6) of re-feeding to an ordinary, energy-reduced diet, and thereafter followed and actively treated for an additional 40 weeks. Eating behaviour was measured with the revised Three-Factor Eating Questionnaire (TFEQ-R21) at baseline, during and after re-feeding, and at week 52. Weight change over time in the two treatment groups was tested by repeated measures analysis in completers and by intention-to-treat (ITT). 169 patients (109 women and 60 men) lost ≥10% during VLED and were randomised. At randomization, weight loss was −16.5 ± 3.7% in Group 1 and −16.7 ± 4.3% in Group 6 (P = 0.73). Between week 12 and 52, completers in Group 6 regained significantly less weight (3.9 ± 9.1%) as compared to Group 1 (8.2 ± 8.3%), (P = 0.006), (ITT, P = 0.05). Patients with six weeks of re-feeding maintained a higher level of dietary restraint after re-feeding was completed but eating behaviour did not differ significantly between the two groups at week 52. The results suggest that longer re-feeding duration after successful weight loss with VLED improves weight maintenance in a one-year perspective.
Keywords: Obesity, Randomised Trial, VLCD, TFEQ
INTRODUCTION
Very low energy diets (VLEDs) can be used to accomplish rapid and substantial weight reduction in obese patients(1). VLEDs are liquid formulas containing all essential nutrients with a caloric content of 1.9-3.3 MJ per day(2). The low energy level results in weight losses of 1.5-2.5 kg per week(2) with concurrent risk factor improvements(3,4).
During a VLED food choice is easy since energy-free fluid is the only complement needed. Also, it has been suggested that food cravings are more reduced with VLEDs than with food-based low energy diets(5), which may contribute to better dietary adherence(6). Studies have shown that greater early weight reduction(7 - 10) and the use of VLED(8) predicts greater weight loss long term. However, after a VLED period, gradual weight rebound is generally seen(11 - 13). Alternative strategies have been suggested to prevent or limit weight regain after a VLED. Different supplementations don't seem to have an effect on post-VLED weight development(14 - 16), but improved weight maintenance has been observed with pharmacological therapy(17,18), exercise(19), continued use of VLED as part of the dietary allowance(20), and protein supplementation(21).
An important phase in VLED programs is when ordinary foods are re-introduced. Throughout re-feeding patients are required to adopt strategies to adjust eating behaviour and dietary intake to the lower energy requirements of a reduced body weight. Thus, the duration of re-feeding may have an impact on the ability to achieve long-term weight control. Re-feeding periods of one to six weeks(5,13,18,20,22 - 27) have been reported, but the long-term effect of different re-feeding strategies has not been examined. Therefore, our objective was to test the hypothesis that prolonged re-feeding duration after successful VLED-induced weight loss beneficially affects weight development and eating behaviour in a one-year perspective.
EXPERIMENTAL METHODS
Study design and subjects
A non-blinded, randomised, one-year clinical trial with parallel treatment groups was conducted to examine the effect of prolonged re-feeding on weight maintenance and eating behaviour in obese patients after a VLED-induced weight loss.
Patients referred to the Obesity Unit at Sahlgrenska University Hospital were eligible if aged 18–60 years, BMI >30.0 kg/m2 and Swedish speaking. Subjects were not eligible if contraindications for VLED treatment were identified at an initial medical and dietary examination. Contraindications included pregnancy and lactation, unstable type 1 diabetes or cardiac disease, recent cerebrovascular disease, a history of eating disorder, severe psychiatric disorder or other severe disease. Weight loss medication was not allowed during the trial. All patients were recruited to participate in a one-year structured obesity intervention with 12 initial weeks of VLED. The study was approved by the regional ethical review board and registered in www.clinicaltrials.gov, number NCT00694811. All participants gave written informed consent.
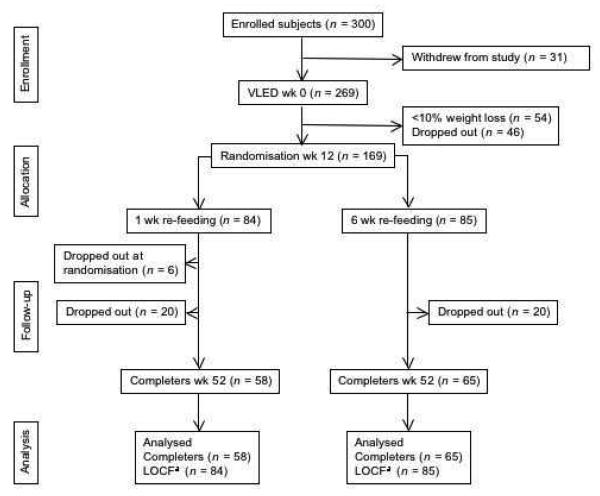
In total, 300 patients were enrolled between August 2004 and January 2007 (Figure 1). Of these, 31 withdrew from the study before treatment started. Thus, 269 patients started the VLED phase of the study and 169 were subsequently randomised after 12 weeks to one or six re-feeding weeks, and followed and actively treated for an additional 40 weeks. Weight loss criteria for randomization was ≥10% over the 12 week VLED period. This cut-off was chosen as studying optimal re-feeding time after VLED is only relevant for subjects who comply with their VLED diets. Non-randomised patients were offered routine treatment at the obesity unit.
Figure 1.
Flow chart. a LOCF, last observation carried forward.
VLED program
During the 12 initial weeks, patients were encouraged to follow a strict liquid very-low-energy diet (2.0-3.4 MJ/day). Patients selected and paid themselves (total cost 5–7 EUR/day) for one of the following, commercially available diets; Modifast® (3.4 MJ/day), Nutrilett® (2.3 MJ/day) or Cambridgekuren® (2.0 MJ/day). Free consumption of non-caloric beverages (<25 kJ/100 g) was allowed. All patients had scheduled nurse visits at weeks 0 (baseline), 2, 5, 8, and 12. Body weight was registered at each visit and patients were given support and counselling to enhance VLED compliance. Side effects were monitored and more frequent contacts were offered if needed. All patients were encouraged to be physically active.
Dietary treatment
Following VLED, dietary treatment advice was given during nine individual sessions with a dietician (week 12, 15, 18, 21, 26, 32, 38, 44, and 52). At week 12 (the first dietician visit), the dietician assigned patients with ≥10% weight loss to treatment group according to randomization. Standardized written and oral instructions for one or six weeks re-feeding were provided; hence, participants as well as study staff were aware of group assignment. During re-feeding, ordinary meals were gradually re-introduced and VLED portions removed. Patients with one week re-feeding (Group 1) started with breakfast for three days, added lunch or dinner the next four days, and thereafter the third meal was re-introduced and VLED discontinued. Patients with six weeks re-feeding (Group 6) started with one regular meal (patient's choice) for three weeks. A second meal was added the next three weeks, and at week seven the third meal was re-introduced and VLED discontinued. Low energy between-meal snacks (e.g. fruit) were allowed from week 14 for Group 1 and week 15 for Group 6.
Recommended energy intake was based on estimated energy requirement minus 30% to achieve an energy-reduced level. Energy requirement was calculated from the equation of Harris-Benedict(28) for estimation of basal metabolic rate, and multiplied by a factor of 1.3 for total energy expenditure (moderate physical activity level). Recommended energy distribution was for breakfast 20%, lunch 35%, and dinner 35% of daily energy intake, and 10% from snacks. Dietary prescriptions followed Swedish Nutrition Recommendations(29).
All patients received written dietary advice based on three main meals with portion sizes in grams of different meal components. The purpose of the dietary treatment was to provide each patient with tailored counselling based on individual needs in order to maintain achieved weight loss. The treatment focused on long-term behavioural change and self-monitoring tasks were used. The specific dietary advice covered meal pattern and composition, food choice, portion size, eating behaviour and physical activity. With the exception of re-feeding strategies both groups received the same treatment and advice.
Measurements
Body weight was measured at all visits, in underwear and without shoes to the nearest 0.1 kg using electronic scales. Height was measured at baseline in standing position, without shoes, to the nearest 0.5 cm. Body mass index (BMI) was calculated (kg/m2).
At baseline and week 26 and 52, body circumferences and blood pressure were measured and overnight fasting blood samples drawn. Waist circumference was measured midway between the costal arch and the iliac crest and hip circumference at the symphysis-trochanter femoris level to the nearest 1.0 cm. At baseline, systolic and diastolic blood pressure were measured once in both arms, where after the arm with highest pressure was used throughout the study. At week 26 and 52, systolic and diastolic blood pressure were measured twice in sitting position after 5 minutes rest, registering the mean value. All measurements were performed with calibrated equipment by trained staff. Blood chemistry included fasting plasma (P)-Glucose, serum (S)-High density lipoprotein cholesterol (S-HDL), and S-Triacylglycerol (STAG). S-Insulin was measured at baseline.
The following cut-offs for cardiovascular risk factors were used for hypertension: systolic and diastolic blood pressure ≥135/85 mmHg, hyperglycaemia: P-Glucose ≥6.1 mmol/l, low HDL-cholesterol: S-HDL <1.3 and 1.0 mmol/l for women and men, hypertriacylglycerolemia: S-TAG ≥1.7 mmol/l, and central obesity: waist circumference >88 and 102 cm for women and men(30).
Self-assessed eating behaviour was measured at baseline and weeks 15, 21, 26, and 52, using the revised Three-Factor Eating Questionnaire (TFEQ-R21), which covers three eating behaviour domains: cognitive restraint, emotional eating, and uncontrolled eating(31,32).
Power calculation and randomization
Sample sizes for recruitment and randomization was calculated using information from a similar study(11). Based on 80% power to detect a 4 kg weight loss difference, standard deviation 7 kg, statistical significance level P <0.05, and 35% drop-out between week 12 and 52, a sample size of 75 patients per treatment arm was required for randomization (week 12). As some patients were expected to drop out from the VLED phase of the study and others not to lose enough weight, a total of 300 patients were recruited to the study.
Patients were eligible for randomization if they had lost ≥10% of the initial body weight after 12 VLED weeks. The randomization was stratified by sex and degree of weight loss (strictly greater than or less than 17.1%). Eligible patients were randomly assigned within each of the four strata to one of the two treatments (one or six weeks re-feeding) in blocks of size two, with equal allocation of treatments within each block. The randomization list was generated with a pseudo-random number generator. The treatment allocation order was arranged in numbered, sealed envelopes and kept in separate boxes for each stratum. At patient assignment, the next envelope in order was drawn from the appropriate box.
Analysis and statistics
Primary outcome measure was the difference in weight change (%) from week 12 to 52 between the two treatment groups. A secondary weight change analysis from week 18 to week 52 was also carried out to study the effect of re-feeding period on weight maintenance independent of the group differences in recommended energy intake during the re-feeding periods. Other secondary outcome measures were, changes in eating behaviour scores (TFEQ-R21) and cardiovascular risk factors at week 52 as compared to baseline. Results are reported as means ± SDs or as frequencies if not otherwise stated. Differences between groups were tested by two-sample t-test (parametric variables) or Wilcoxon two sample test (nonparametric variables). Changes within groups were tested by paired t-test. Chi-square test was used to compare dichotomous data. Baseline to week 52 weight changes in the two treatment groups were tested by repeated measures analysis in completers, and on an intention-to-treat (ITT) basis with the last weight observation carried forward (LOCF). ANCOVA was used to test the difference in weight change from week 18 to week 52, with weight at week 18 as a covariate. Statistical significance was set at two-tailed P<0.05. All statistical analyses were performed using SAS-PC software, version 9.1 (SAS Institute Inc, Cary, NC, USA).
RESULTS
Participants
After 12 weeks of VLED, 169 patients met the randomization criteria (Figure 1). Baseline characteristics for patients assigned to one (Group 1, n = 84) or six weeks (Group 6, n = 85) re-feeding are shown in Table 1. Sixty-four percent of the patients were women. Sex distribution, age, anthropometry or cardiovascular risk factors at baseline did not differ between the groups.
Table 1.
Patient characteristics at baseline and body weight at randomization. a (Mean values and standard deviations)
|
Group 1
b (n = 84) |
Group 6
c (n = 85) |
|||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| n (female;male) | 54;30 | 55;30 | ||
| Age (y) | 40.6 | 9.2 | 41.9 | 10.2 |
| Height (m) | 1.72 | 0.1 | 1.72 | 0.1 |
| Weight at baseline (kg) | 122.9 | 23.0 | 124.6 | 25.8 |
| Weight at randomization (kg) d | 102.8 | 20.7 | 104.0 | 23.0 |
| BMI at baseline (kg/m2) | 41.4 | 5.7 | 41.7 | 6.3 |
| Waist circumference (cm) | 124.8 e | 14.8 | 125.5 f | 15.9 |
| Systolic blood pressure (mmHg) | 128.8 | 16.4 | 130.8 | 16.5 |
| Diastolic blood pressure (mmHg) | 84.0 | 10.3 | 85.7 | 12.7 |
| S-Insulin (mU/l) | 21.7 e | 14.3 | 25.2 | 25.4 |
| P-Glucose (mmol/l) | 5.5 | 1.3 | 5.4 e | 1.3 |
| S-HDL-cholesterol (mmol/l) | 1.3 e | 0.2 | 1.3 f | 0.3 |
| S-Triacyglycerol (mmol/l) | 1.6 e | 0.8 | 1.5 f | 0.7 |
For details of subjects and procedures, see Experimental methods. No significant differences were observed between the groups.
Group 1 – one week of re-feeding
Group 6 – six weeks of re-feeding
Measured at week 12 (after VLED, very-low-energy diet)
n = 83
n = 84
Body weight
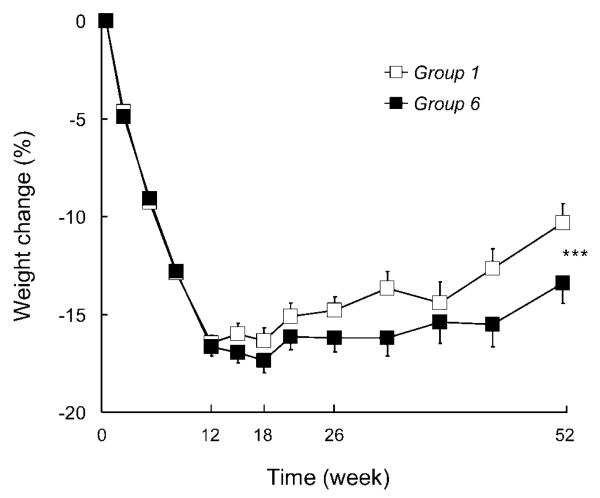
Figure 2 shows relative weight change over one year for the 123 completers by treatment group. At randomization, mean weight loss was −16.5 ± 3.7% in Group 1 and −16.7 ± 4.3% in Group 6 (P = 0.73). Between week 12 and 52, weight increased with 8.2 ± 8.3% in Group 1 and 3.9 ± 9.1% in Group 6. Group 6 regained significantly less weight over time, both in a completers analysis (P = 0.006) and in an intention-to-treat analysis with last observation carried forward (P = 0.05). Furthermore, the overall weight loss at week 52 compared to baseline was significantly greater in Group 6 (−13.4 ± 8.4%) than in Group 1 (−10.3 ± 7.5%), (P = 0.03). Of patients allocated to Group 1 and Group 6, 31 (37%) and 41 (48%) respectively had achieved a weight reduction of ≥10% at week 52 (P = 0.13). Eight (10%) and 20 (24%) patients in Group 1 and Group 6 respectively, continued to lose weight after ordinary foods were re-introduced and had a lower weight at week 52 than at week 12 (P = 0.01).
Figure 2.
Changes (%) in weight (mean ± SEM) among completers during one treatment year with 12 initial weeks VLED followed by one (Group 1) or six weeks (Group 6) of re-feeding to an ordinary, energy-reduced diet. *** P = 0.006 for difference between groups over time in completers-analyses and P = 0.05, ITT-analysis (repeated measures analysis).
To remove the effect of the difference in recommended energy intake between the groups weight change between week 18 and week 52 was also considered. The weight change was 7.4 ± 6.4 % in Group 1 and 4.3 ± 7.5 % in Group 6 and P was 0.02 when controlling for difference in body weight between the groups at week 18.
Eating behaviour
Baseline eating behaviour did not differ between the two treatment groups (Table 2). Substantial changes were observed in both groups after the VLED period, i.e., cognitive restraint increased, while uncontrolled and emotional eating decreased. All changes were statistically significant, except for emotional eating at week 52. At week 21 (P = 0.01) and 26 (P = 0.02), dietary restraint was significantly higher in Group 6 than in Group 1. After one year, cognitive restraint and uncontrolled eating had significantly improved in both groups as compared to baseline, while emotional eating did not differ from baseline values. The changes in eating behaviour at week 52 as compared to baseline did not differ significantly between treatment groups.
Table 2.
Self-assessed eating behavior (TFEQ-R21) before and after weight loss with VLED. a, b, c, d (Mean values and standard deviations)
| Time | Week 0 |
Week 15 |
Week 21 |
Week 26 |
Week 52 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| n (Group 1;Group 6) | 82;83 | 63;72 | 57;66 | 58;73 | 53;62 | |||||
| Cognitive Restraint | ||||||||||
| Group 1 | 41.9 | 17.5 | 65.3 | 15.0 | 61.8 | 15.5 | 59.5 | 17.4 | 56.4 | 20.6 |
| Group 6 | 43.0 | 20.9 | 67.6 | 17.4 | 67.9 e | 17.2 | 66.0 e | 15.2 | 59.4 | 18.3 |
| Uncontrolled Eating | ||||||||||
| Group 1 | 44.5 | 19.2 | 28.0 | 17.1 | 32.0 | 17.0 | 30.4 | 19.2 | 38.0 | 24.6 |
| Group 6 | 45.0 | 22.1 | 29.9 | 19.6 | 33.0 | 20.8 | 32.3 | 20.5 | 35.5 | 23.3 |
| Emotional Eating | ||||||||||
| Group 1 | 54.3 | 28.7 | 37.1 | 23.2 | 40.5 | 24.5 | 42.6 | 26.8 | 46.6 | 28.8 |
| Group 6 | 50.6 | 28.3 | 33.1 | 23.1 | 40.9 | 28.7 | 42.5 | 28.7 | 44.9 | 31.4 |
TFEQ-R21, the Three-Factor Eating Questionnaire (revised version).
VLED, very-low-energy diet.
Scale range is 0-100. Higher scores represent more restraint, uncontrolled, and emotional eating.
Group 1 – one week re-feeding, Group 6 – six weeks of re-feeding
Measured at week 0 (before VLED) and 3 (study wk 15), 9 (study wk 21), 14 (study wk 26) and 40 (study wk 52) weeks after randomization (wk 12, end of VLED).
Within the two groups, all values were significantly different from baseline (P < 0.01), with the exception for emotional eating at week 52 (ns).
P < 0.05 compared with Group 1
Cardiovascular risk factors
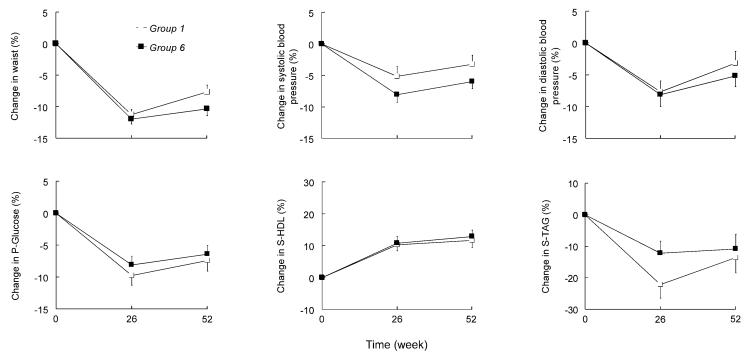
At week 52, waist circumference, systolic and diastolic blood pressure, P-Glucose, S-HDL, and S-Triacylglycerol were significantly improved in both treatment groups as compared to baseline, with the exception of diastolic blood pressure in Group 1 (Figure 3). However, there were no significant differences between groups at week 52. From baseline to week 52, the number of patients with three or more risk factors, the ATPIII criteria for the metabolic syndrome(30), decreased from 26% to 10% (P <0.0001).
Figure 3.
Changes (%) in risk factors (mean ± SEM) after 26 and 52 weeks of treatment. All risk factors were significantly improved in both treatment groups at week 52, except for diastolic blood pressure in Group 1. No significant differences were found between treatment groups at week 52.
Drop-out and adverse events
Six patients allocated to Group 1 dropped out at randomization and 20 subjects from each group dropped out during the post-VLED dietary intervention (Figure 1). The entire treatment program was completed by 37 of 54 women and 21 of 30 men in Group 1 and by 40 of 55 women and 25 of 30 men in Group 6. Drop-out rate did not differ by sex or by treatment arm. In total, 58 (69%) and 65 (76%) of participants in Group 1 and Group 6 completed the entire study (P = 0.28).
In general, the re-feeding period and the following dietary treatment were well tolerated. Three women in each group became pregnant and were therefore excluded. One woman in Group 1 died of heart failure at week 35.
DISCUSSION
The focus of this study was to evaluate the impact of re-feeding duration on post-VLED weight development in obese patients referred to an obesity clinic. Our results show that weight loss was better maintained with a re-feeding period of six weeks than with a re-feeding period of one week.
It has previously been shown that strict VLED adherence is better than a liberal VLED regime(23), and that the incorporation of VLED in the meal plan after the weight loss period improves long-term weight maintenance(20). To our knowledge, this is the first study that has evaluated the effects of re-feeding on weight regain. We compared one and six weeks of re-feeding in obese patients who had successfully lost weight during a 12-week VLED. Consistent with our hypothesis, patients with a prolonged, six-week, re-feeding period lost significantly more weight over one year of treatment than the group with one week of re-feeding due to a significantly smaller post-VLED weight regain. The smaller weight regain in patients with longer re-feeding duration could partly be explained by a lower energy intake per se during the re-feeding period, but also by an improved eating behaviour due to the fact that patients with six re-feeding weeks could focus on one meal at a time and had longer time to practice and adjust to each meal. The lower weight regain over the last 34 weeks of the study in the group with longer re-feeding duration, compared with the group with shorter re-feeding duration, suggests that a longer initial re-feeding period also improve eating behaviour long term. This is supported by the fact that patients with prolonged re-feeding maintained a higher level of dietary restraint at three and eight weeks after re-feeding was completed, reflecting an improved ability to restrict food intake and thus to follow dietary prescriptions. Re-feeding over six weeks instead of one week is also associated with a lower recommended energy intake. For patients recommended 6.3 MJ per day, the energy deficit over the first six weeks after VLED was about 54.4 MJ more for patients on six weeks re-feeding compared to patients on one week re-feeding. Although this corresponds to approximately 2 kg of fat mass, the calculation is entirely theoretical as it assumes a hundred percent compliance to the recommended meal plans. Based on our clinical experience this is very unlikely and efforts related to improving patients compliance to a low energy intake is essential for long-term weight maintenance. A weakness of this study is that we have no information on energy intake during the re-feeding. Ideally, the patients should have recorded their food intake during the re-feeding phase of the study, but in this group of obese patients, we considered food diaries too extensive and the energy intake information that we would get unreliable(33).
The observed changes in eating behaviour are in accordance with previous studies, describing an increase in restrained eating(19,34,35) and a decrease in uncontrolled and emotional eating(19,35) during weight loss. This overall pattern of eating behaviour changes has been associated with favourable changes in dietary intake(35). Also, high scores in cognitive restraint has been associated with weight loss and adaptation of weight-controlling behaviour(34). Although eating behaviour tended to return towards baseline level over time, cognitive restraint and uncontrolled eating were still significantly improved in both treatment groups after one year.
As previously observed, one-year weight losses in the order of ten percent were related to significant improvements in cardiovascular risk factors(11). In Group 6 improvements in the range of 10% were seen for blood lipids and waist circumference, whereas the improvements for P-Glucose and blood pressure were about 5%. The improvements were slightly smaller in Group 1 for most of the risk factors, but the differences were not statistically significant.
It should be noted that the patients included in this study are obese patients referred to a specialist obesity clinic by their GPs. Average weight was therefore higher and co-morbidities more prevalent than in most VLED studies. This may explain why not all not patients reached the randomization phase of the study (17% of the patients dropped out during the VLED period and 20% did not lose enough weight). We chose to randomise patients with weight losses greater than ten percent after VLED. Thus, only successful patients were included. This is a strategy used in other studies(18) and it could be argued that re-feeding is relevant only when a substantial VLED-induced weight loss has actually been achieved. After one year, 43% of the 169 randomised patients maintained a weight reduction of at least ten percent, whereas 17% continued to lose weight after the VLED period and had a greater weight loss at week 52 than after the 12-week VLED.
Twenty-seven percent of the patients dropped out during the 40 weeks of treatment after VLED. Similar attrition rates have been reported from other randomised VLED programs(20,23). However, it should be noticed that six women were excluded due to pregnancy and should therefore not be regarded as actual drop-outs. Increased fertility in obese women who lose weight has also been observed in other studies(20,36).
A difficulty in most dietary interventions is that patients and study staff cannot be blinded to treatment allocation. Although all patients agreed to the study protocol at baseline, six patients from Group 1 chose to drop out at randomization while no patients from Group 6 left the trial at randomization. This implies that some participants considered one week of re-feeding as a less advantageous alternative. Nevertheless, long-term drop-out was similar in the two treatment groups. In the present study, patients were followed for 40 weeks, which is a relatively short time period considering that obesity is a chronic disorder. However, although a longer follow up is desirable, we believe that the achieved one-year improvements in body weight and risk factors are clinically relevant and our results contribute to a better understanding of how to improve weight maintenance after VLED in obesity treatment programs.
In conclusion, after successful VLED-induced weight loss, patients with six weeks of re-feeding maintained a significantly greater weight loss over one year of treatment than patients with only one week of re-feeding due to a significantly smaller post-VLED weight regain. Accordingly, our study implies that ordinary foods should be re-introduced slowly after a VLED period to enhance weight control. In addition to dietary counselling and support, the prolonged re-feeding could be combined with other post-VLED approaches, such as a high-protein diet(21), physical activity(19), and/or pharmacological therapy(18), to further improve long-term treatment outcome.
ACKNOWLEDGMENTS
We want to thank the staff at the Obesity Unit at Sahlgrenska University Hospital for their committed work with this study. We also thank dr Markku Peltonen for statistical advice and Karin Lantz and Margareta Rystedt for excellent assistance with collating data. None of the authors had a personal or financial conflict of interest. The authors' responsibilities were as follows—LG, JT, JK, and AKL: conception and design of the study and obtaining funding; LG: acquisition of data; LG, JT, JK, and AKL: analysis and interpretation of data, and writing the manuscript. Research relating to this manuscript was funded by The Health & Medical Care Committee of the Region Västra Götaland.
REFERENCES
- 1.Gilden Tsai A, Wadden TA. The evolution of very-low-calorie diets: an update and meta-analysis. Obesity (Silver Spring) 2006;14:1283–1293. doi: 10.1038/oby.2006.146. [DOI] [PubMed] [Google Scholar]
- 2.SCOOP-VLCD Task 7.3 Reports on tasks for scientific cooperation. Collection of data on products intended for use in very-low-calorie-diets. 2002. htpp://europa.eu.int/comm/comm/food/fs/scoop/7.3_en.pdf (last accessed 09/11/2008)
- 3.Bryson JM, King SE, Burns CM, et al. Changes in glucose and lipid metabolism following weight loss produced by a very low calorie diet in obese subjects. Int J Obes Relat Metab Disord. 1996;20:338–345. [PubMed] [Google Scholar]
- 4.Colles SL, Dixon JB, Marks P, et al. Preoperative weight loss with a very-low-energy diet: quantitation of changes in liver and abdominal fat by serial imaging. Am J Clin Nutr. 2006;84:304–311. doi: 10.1093/ajcn/84.1.304. [DOI] [PubMed] [Google Scholar]
- 5.Martin CK, O'Neil PM, Pawlow L. Changes in food cravings during low-calorie and very-low-calorie diets. Obesity (Silver Spring) 2006;14:115–121. doi: 10.1038/oby.2006.14. [DOI] [PubMed] [Google Scholar]
- 6.Heymsfield SB, Harp JB, Reitman ML, et al. Why do obese patients not lose more weight when treated with low-calorie diets? A mechanistic perspective. Am J Clin Nutr. 2007;85:346–354. doi: 10.1093/ajcn/85.2.346. [DOI] [PubMed] [Google Scholar]
- 7.Wadden TA, Foster GD, Wang J, et al. Clinical correlates of short- and long-term weight loss. Am J Clin Nutr. 1992;56:271S–274S. doi: 10.1093/ajcn/56.1.271S. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001;74:579–584. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- 9.Stotland SC, Larocque M. Early treatment response as a predictor of ongoing weight loss in obesity treatment. Br J Health Psychol. 2005;10:601–614. doi: 10.1348/135910705X43750. [DOI] [PubMed] [Google Scholar]
- 10.Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 11.Lantz H, Peltonen M, Agren L, Torgerson JS. Intermittent versus on-demand use of a very low calorie diet: a randomised 2-year clinical trial. J Intern Med. 2003;253:463–471. doi: 10.1046/j.1365-2796.2003.01131.x. [DOI] [PubMed] [Google Scholar]
- 12.Torgerson JS, Lissner L, Lindroos AK, et al. VLCD plus dietary and behavioural support versus support alone in the treatment of severe obesity. A randomised two-year clinical trial. Int J Obes Relat Metab Disord. 1997;21:987–994. doi: 10.1038/sj.ijo.0800507. [DOI] [PubMed] [Google Scholar]
- 13.Kaukua J, Pekkarinen T, Sane T, Mustajoki P. Health-related quality of life in obese outpatients losing weight with very-low-energy diet and behaviour modification--a 2-y follow-up study. Int J Obes Relat Metab Disord. 2003;27:1233–1241. doi: 10.1038/sj.ijo.0802379. [DOI] [PubMed] [Google Scholar]
- 14.Lejeune MP, Kovacs EM, Westerterp-Plantenga MS. Effect of capsaicin on substrate oxidation and weight maintenance after modest body-weight loss in human subjects. Br J Nutr. 2003;90:651–659. doi: 10.1079/bjn2003938. [DOI] [PubMed] [Google Scholar]
- 15.Kovacs EM, Lejeune MP, Nijs I, Westerterp-Plantenga MS. Effects of green tea on weight maintenance after body-weight loss. Br J Nutr. 2004;91:431–437. doi: 10.1079/BJN20041061. [DOI] [PubMed] [Google Scholar]
- 16.Pasman WJ, Westerterp-Plantenga MS, Saris WH. The effectiveness of long-term supplementation of carbohydrate, chromium, fibre and caffeine on weight maintenance. Int J Obes Relat Metab Disord. 1997;21:1143–1151. doi: 10.1038/sj.ijo.0800528. [DOI] [PubMed] [Google Scholar]
- 17.Svendsen M, Rissanen A, Richelsen B, et al. Effect of orlistat on eating behavior among participants in a 3-year weight maintenance trial. Obesity (Silver Spring) 2008;16:327–333. doi: 10.1038/oby.2007.82. [DOI] [PubMed] [Google Scholar]
- 18.Mathus-Vliegen EM. Long-term maintenance of weight loss with sibutramine in a GP setting following a specialist guided very-low-calorie diet: a double-blind, placebo-controlled, parallel group study. Eur J Clin Nutr. 2005;59(Suppl. 1):S31–38. doi: 10.1038/sj.ejcn.1602172. discussion S39. [DOI] [PubMed] [Google Scholar]
- 19.Fogelholm M, Kukkonen-Harjula K, Oja P. Eating control and physical activity as determinants of short-term weight maintenance after a very-low-calorie diet among obese women. Int J Obes Relat Metab Disord. 1999;23:203–210. doi: 10.1038/sj.ijo.0800825. [DOI] [PubMed] [Google Scholar]
- 20.Ryttig KR, Rossner S. Weight maintenance after a very low calorie diet (VLCD) weight reduction period and the effects of VLCD supplementation. A prospective, randomised, comparative, controlled long-term trial. J Intern Med. 1995;238:299–306. doi: 10.1111/j.1365-2796.1995.tb01202.x. [DOI] [PubMed] [Google Scholar]
- 21.Westerterp-Plantenga MS, Lejeune MP, Nijs I, et al. High protein intake sustains weight maintenance after body weight loss in humans. Int J Obes Relat Metab Disord. 2004;28:57–64. doi: 10.1038/sj.ijo.0802461. [DOI] [PubMed] [Google Scholar]
- 22.Erondu N, Wadden T, Gantz I, et al. Effect of NPY5R antagonist MK-0557 on weight regain after very-low-calorie diet-induced weight loss. Obesity (Silver Spring) 2007;15:895–905. doi: 10.1038/oby.2007.620. [DOI] [PubMed] [Google Scholar]
- 23.Torgerson JS, Agren L, Sjostrom L. Effects on body weight of strict or liberal adherence to an initial period of VLCD treatment. A randomised, one-year clinical trial of obese subjects. Int J Obes Relat Metab Disord. 1999;23:190–197. doi: 10.1038/sj.ijo.0800816. [DOI] [PubMed] [Google Scholar]
- 24.LeCheminant JD, Jacobsen DJ, Hall MA, Donnelly JE. A comparison of meal replacements and medication in weight maintenance after weight loss. J Am Coll Nutr. 2005;24:347–353. doi: 10.1080/07315724.2005.10719484. [DOI] [PubMed] [Google Scholar]
- 25.Foster GD, Wadden TA, Peterson FJ, et al. A controlled comparison of three very-low-calorie diets: effects on weight, body composition, and symptoms. Am J Clin Nutr. 1992;55:811–817. doi: 10.1093/ajcn/55.4.811. [DOI] [PubMed] [Google Scholar]
- 26.Wadden TA, Bartlett S, Letizia KA, et al. Relationship of dieting history to resting metabolic rate, body composition, eating behavior, and subsequent weight loss. Am J Clin Nutr. 1992;56:203S–208S. doi: 10.1093/ajcn/56.1.203S. [DOI] [PubMed] [Google Scholar]
- 27.Raymond NC, de Zwaan M, Mitchell JE, et al. Effect of a very low calorie diet on the diagnostic category of individuals with binge eating disorder. Int J Eat Disord. 2002;31:49–56. doi: 10.1002/eat.1110. [DOI] [PubMed] [Google Scholar]
- 28.Harris JA, Benedict FG. A Biometric Study of Basal Metabolism in Man. The Carnegie Institute; Washington, DC: 1912. [Google Scholar]
- 29.Livsmedelsverket . Svenska Näringsrekommendationer. PO Box 622, S-751 26; Uppsala, Sweden: 1997. [Google Scholar]
- 30.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 31.Karlsson J, Persson LO, Sjostrom L, Sullivan M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. Int J Obes Relat Metab Disord. 2000;24:1715–1725. doi: 10.1038/sj.ijo.0801442. [DOI] [PubMed] [Google Scholar]
- 32.Tholin S, Rasmussen F, Tynelius P, Karlsson J. Genetic and environmental influences on eating behavior: the Swedish Young Male Twins Study. Am J Clin Nutr. 2005;81:564–569. doi: 10.1093/ajcn/81.3.564. [DOI] [PubMed] [Google Scholar]
- 33.Lindroos AK, Lissner L, Sjostrom L. Validity and reproducibility of a self-administered dietary questionnaire in obese and non-obese subjects. Eur J Clin Nutr. 1993;47:461–481. [PubMed] [Google Scholar]
- 34.McGuire MT, Jeffery RW, French SA, Hannan PJ. The relationship between restraint and weight and weight-related behaviors among individuals in a community weight gain prevention trial. Int J Obes Relat Metab Disord. 2001;25:574–580. doi: 10.1038/sj.ijo.0801579. [DOI] [PubMed] [Google Scholar]
- 35.Borg P, Fogelholm M, Kukkonen-Harjula K. Food selection and eating behaviour during weight maintenance intervention and 2-y follow-up in obese men. Int J Obes Relat Metab Disord. 2004;28:1548–1554. doi: 10.1038/sj.ijo.0802790. [DOI] [PubMed] [Google Scholar]
- 36.Clark AM, Thornley B, Tomlinson L, et al. Weight loss in obese infertile women results in improvement in reproductive outcome for all forms of fertility treatment. Hum Reprod. 1998;13:1502–1505. doi: 10.1093/humrep/13.6.1502. [DOI] [PubMed] [Google Scholar]