Abstract
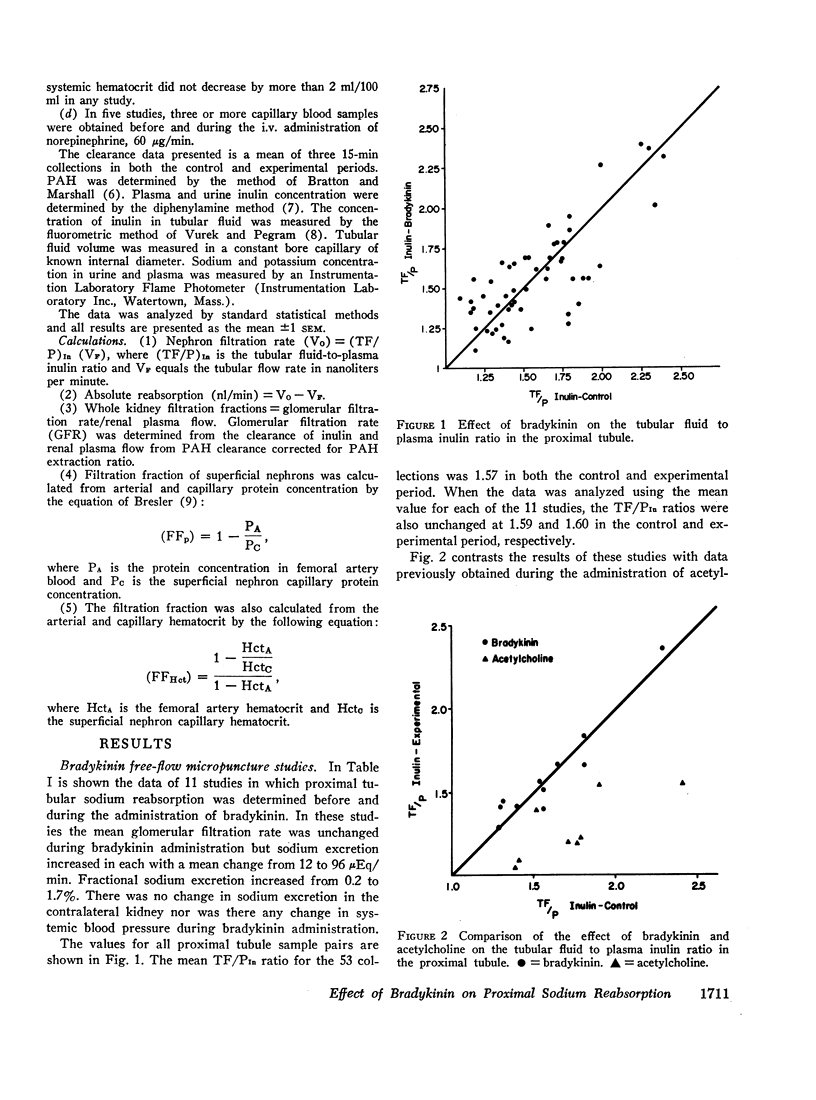
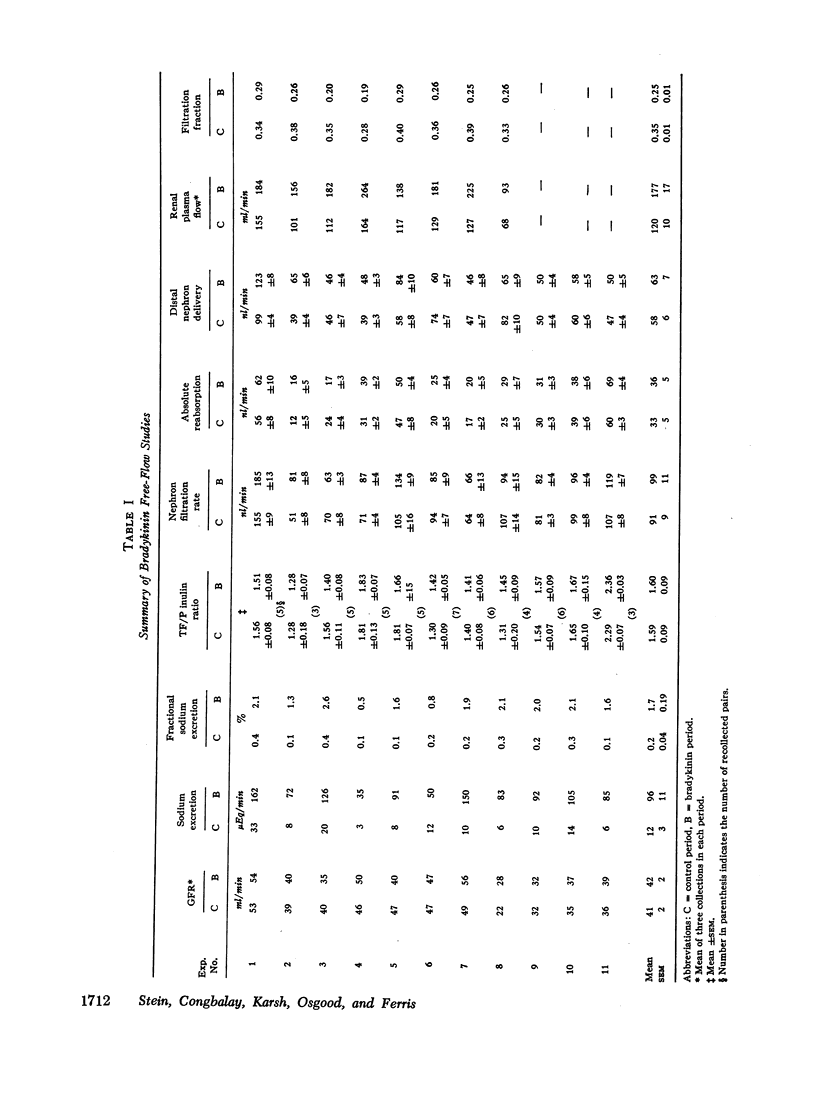
In a previous study we have found that acetylcholine, a renal vasodilator, inhibits fractional and absolute reabsorption of sodium in the proximal tubule of the dog. To delineate whether this effect on proximal tubular sodium reabsorption was related to alterations in renal hemodynamics or to a direct tubular action of the drug, free-flow micropuncture studies were performed in the dog in which the tubular fluid to plasma inulin ratio and nephron filtration rate were determined before and during the administration of a structurally different renal vasodilator, bradykinin. This agent increased sodium excretion from 12 to 96 μEq/min and decreased total kidney filtration fraction from 0.35 to 0.25. However, sodium reabsorption in the proximal tubule of the superficial nephrons was unchanged during bradykinin administration.
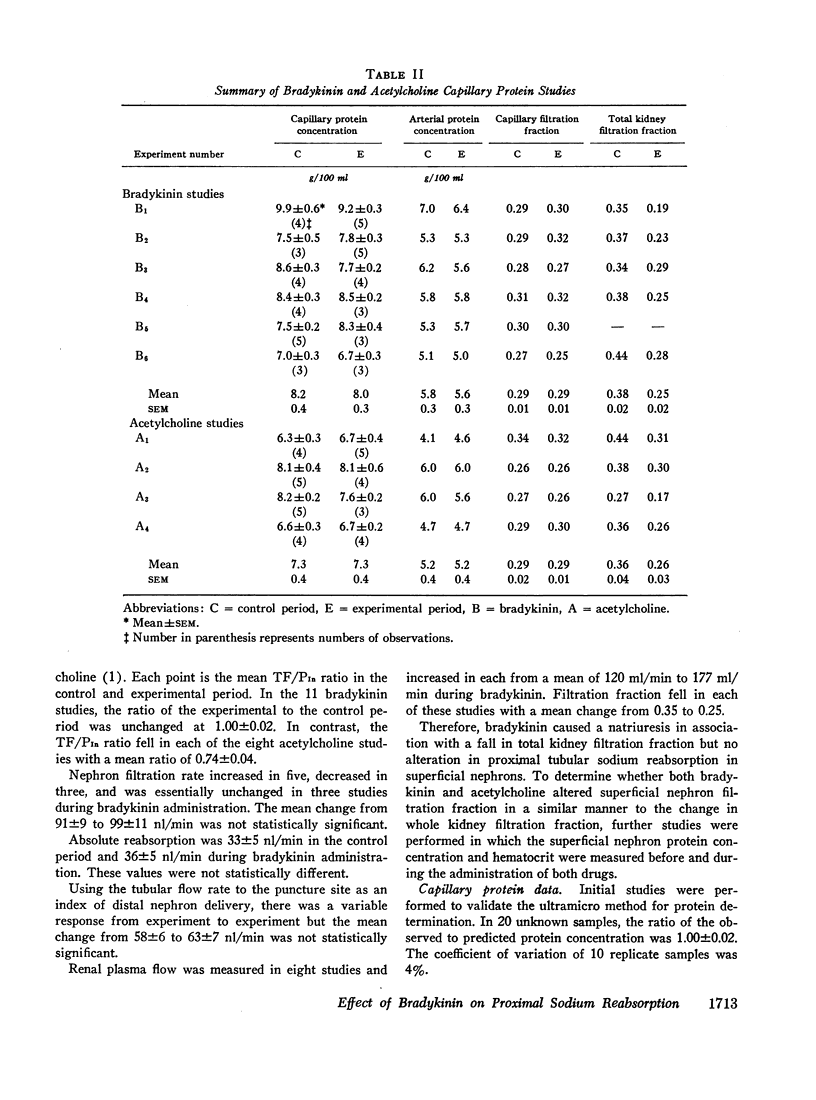
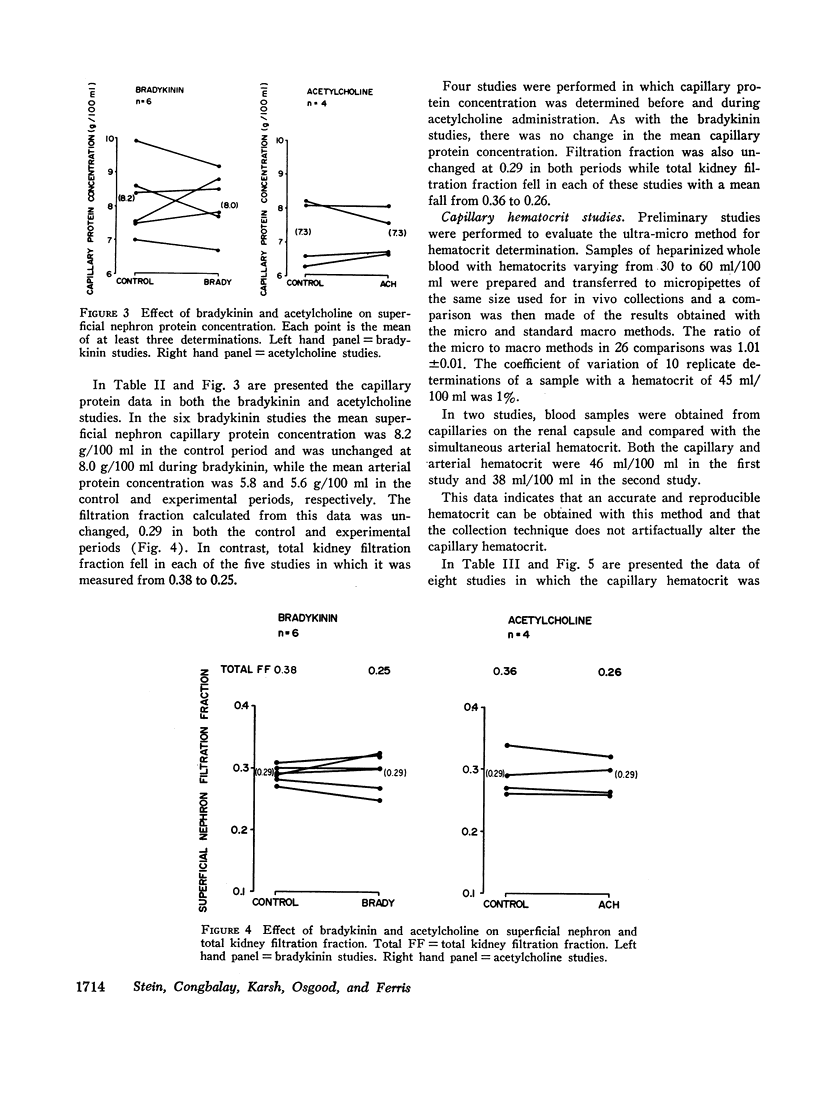
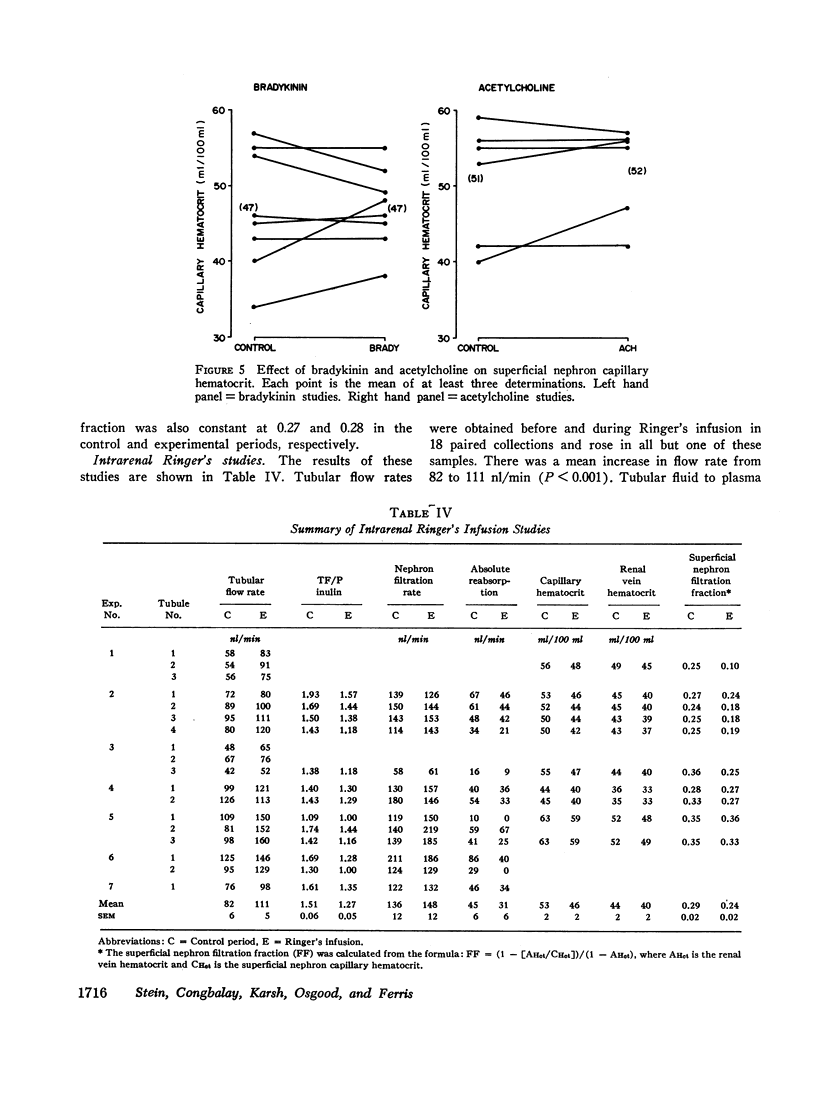
Since it has been shown that a decrease in filtration fraction and presumably peritubular capillary protein concentration will decrease proximal tubular sodium reabsorption, studies were performed to determine whether the fall in total kidney filtration fraction seen with both vasodilators is paralleled by a similar change in the circulation of superficial nephrons. The results of these studies indicate that neither agent altered superficial nephron capillary protein concentration, hematocrit, or filtration fraction.
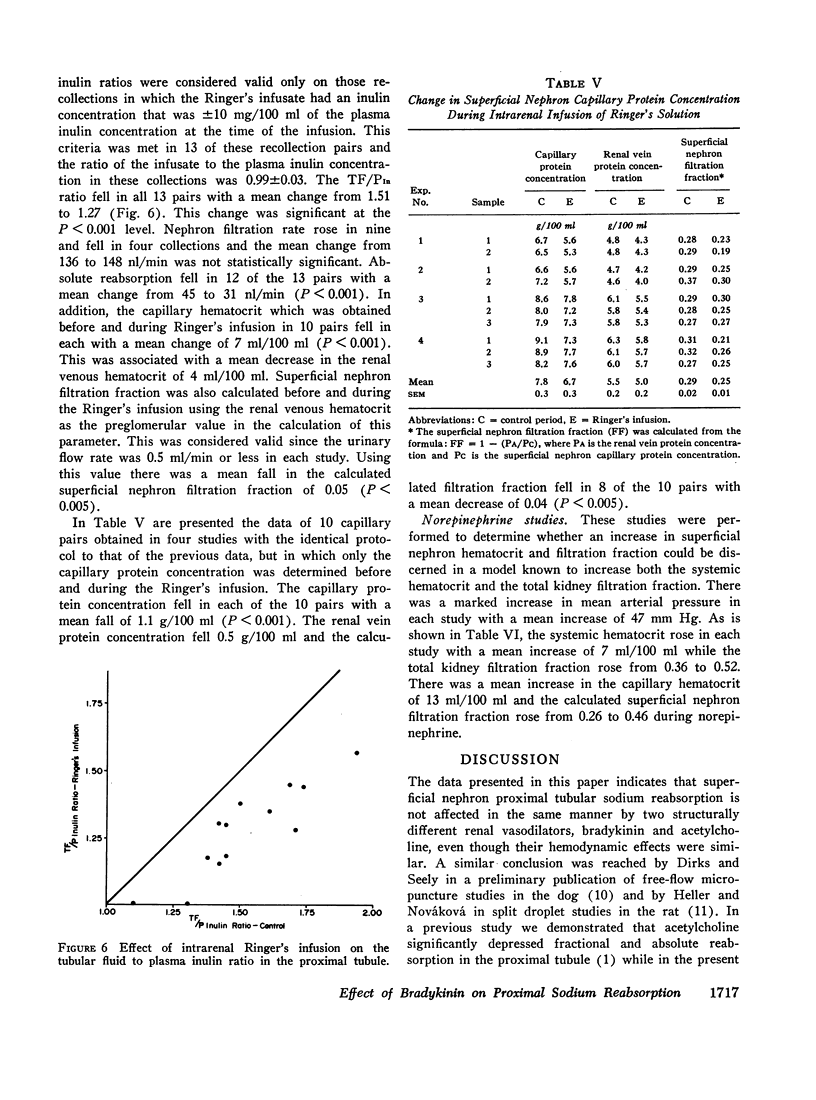
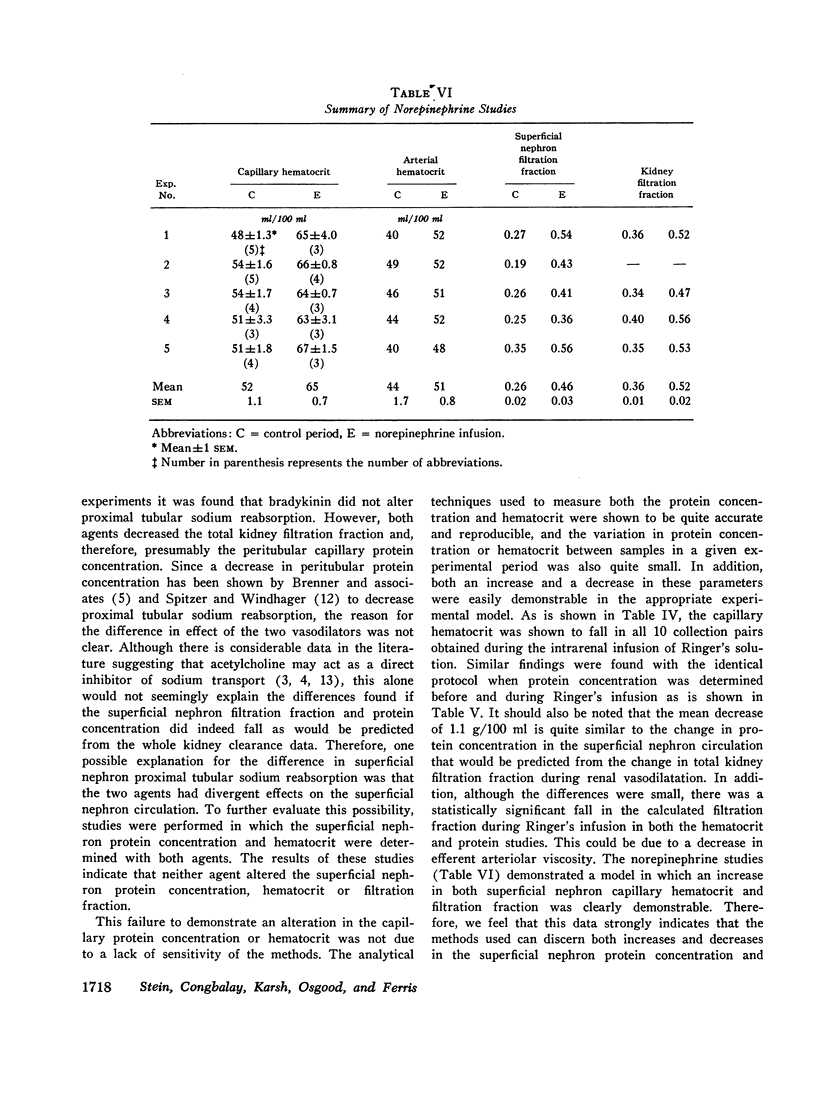
In contrast, a decrease in capillary protein concentration, hematocrit, and filtration fraction was consistently demonstrated during the intrarenal infusion of 7.5-15 ml/min of Ringer's solution while an increase in these parameters occurred during the i.v. administration of norepinephrine, 60 μg/min. In the Ringer's infusion studies, both fractional and absolute sodium reabsorption in the proximal tubule were decreased concomitant with the fall in capillary protein concentration and hematocrit.
This data suggests that: (a) the hemodynamic effect of renal vasodilatation is not the same in the circulation of all nephrons; (b) the inhibitory effect of acetylcholine on proximal tubular sodium reabsorption is due to a direct tubular action; (c) a decrease in capillary protein concentration and/or hematocrit does decrease proximal tubular sodium reabsorption; (d) although proximal reabsorption of sodium is unchanged in the superficial nephrons during bradykinin administration, a decrease in reabsorption may be present in deeper nephrons in which filtration fraction is decreased.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BRESLER E. H. The problem of the volume component of body fluid homeostasis. Am J Med Sci. 1956 Jul;232(1):93–104. doi: 10.1097/00000441-195607000-00014. [DOI] [PubMed] [Google Scholar]
- Brenner B. M., Falchuk K. H., Keimowitz R. I., Berliner R. W. The relationship between peritubular capillary protein concentration and fluid reabsorption by the renal proximal tubule. J Clin Invest. 1969 Aug;48(8):1519–1531. doi: 10.1172/JCI106118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner B. M., Galla J. H. Influence of postglomerular hematocrit and protein concentration on rat nephron fluid transfer. Am J Physiol. 1971 Jan;220(1):148–161. doi: 10.1152/ajplegacy.1971.220.1.148. [DOI] [PubMed] [Google Scholar]
- Daugharty T. M., Belleau L. J., Martino J. A., Earley L. E. Interrelationship of physical factors affecting sodium reabsorption in the dog. Am J Physiol. 1968 Dec;215(6):1442–1447. doi: 10.1152/ajplegacy.1968.215.6.1442. [DOI] [PubMed] [Google Scholar]
- Earley L. E., Friedler R. M. The effects of combined renal vasodilatation and pressor agents on renal hemodynamics and the tubular reabsorption of sodium. J Clin Invest. 1966 Apr;45(4):542–551. doi: 10.1172/JCI105368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller J., Nováková A. Proximal tubular reabsorption during renal vasodilation and increased arterial blood pressure in saline loaded rats. Pflugers Arch. 1969;309(3):250–265. doi: 10.1007/BF00586802. [DOI] [PubMed] [Google Scholar]
- May D. G., Carter M. K. Effect of vasoactive agents on urine and electrolyte excretion in the chicken. Am J Physiol. 1970 Feb;218(2):417–422. doi: 10.1152/ajplegacy.1970.218.2.417. [DOI] [PubMed] [Google Scholar]
- Parmelee M. L., Carter M. K. The diuretic effect of acetylcholine in the chicken. Arch Int Pharmacodyn Ther. 1968 Jul;174(1):108–117. [PubMed] [Google Scholar]
- Schilb T. P. Effect of a cholinergic agent on sodium transport across isolated turtle bladders. Am J Physiol. 1969 Mar;216(3):514–520. doi: 10.1152/ajplegacy.1969.216.3.514. [DOI] [PubMed] [Google Scholar]
- Spitzer A., Windhager E. E. Effect of peritubular oncotic pressure changes on proximal tubular fluid reabsorption. Am J Physiol. 1970 Apr;218(4):1188–1193. doi: 10.1152/ajplegacy.1970.218.4.1188. [DOI] [PubMed] [Google Scholar]
- Stein J. H., Ferris T. F., Huprich J. E., Smith T. C., Osgood R. W. Effect of renal vasodilatation on the distribution of cortical blood flow in the kidney of the dog. J Clin Invest. 1971 Jul;50(7):1429–1438. doi: 10.1172/JCI106626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein J. H., Reineck J. H., Osgood R. W., Ferris T. F. Effect of acetylcholine on proximal tubular sodium reabsorption in the dog. Am J Physiol. 1971 Jan;220(1):227–232. doi: 10.1152/ajplegacy.1971.220.1.227. [DOI] [PubMed] [Google Scholar]
- WALSER M., DAVIDSON D. G., ORLOFF J. The renal clearance of alkali-stable inulin. J Clin Invest. 1955 Oct;34(10):1520–1523. doi: 10.1172/JCI103204. [DOI] [PMC free article] [PubMed] [Google Scholar]



