Abstract
Background
Previous studies have shown evidence of residual scar tissue at the musculotendon junction following an acute hamstring strain injury, which could influence re-injury risk. The purpose of this study was to investigate whether bilateral differences in strength, neuromuscular patterns, and musculotendon kinematics during sprinting are present in individuals with a history of unilateral hamstring injury, and whether such differences are linked to the presence of scar tissue.
Methods
Eighteen subjects with a previous hamstring injury (>5 months prior) participated in a magnetic resonance (MR) imaging exam, isokinetic strength testing, and a biomechanical assessment of treadmill sprinting. Bilateral comparisons were made for peak knee flexion torque, angle of peak torque, and hamstrings:quadriceps strength ratio during strength testing, and muscle activations and peak hamstring stretch during sprinting. MR images were used to measure the volumes of the proximal tendon/aponeurois of the biceps femoris, with asymmetries considered indicative of residual scar tissue.
Findings
A significantly enlarged proximal biceps femoris tendon volume was measured on the side of prior injury. However, no significant differences between the previously injured and uninjured limbs were found in strength measures, peak hamstring stretch, or muscle activation patterns. Further, the degree of asymmetry in tendon volume was not correlated to any of the functional measures.
Interpretation
The results of this study indicate that injury-induced changes in morphology do not seem discernable from strength measures, running kinematics, or muscle activity patterns. Further research is warranted to ascertain whether residual scarring alters localized musculotendon tissue mechanics in a way that may contribute to the high rates of muscle re-injury that are observed clinically.
Keywords: muscle injury, running, electromyography, magnetic resonance imaging, isokinetic strength
Introduction
Hamstring strain injuries are extremely common in sports that involve sprinting, such as track, soccer, and football (Woods et al., 2004, Arnason et al., 2004, Bennell and Crossley, 1996, Orchard and Seward, 2002, Askling et al., 2003). Effective treatment and rehabilitation of individuals with hamstring injuries remains a challenge, as demonstrated by a re-injury rate of approximately 30% (Woods et al., 2004, Orchard and Best, 2002). A better understanding of the long term effects of a prior injury on hamstring morphology, mechanics, and function could provide a basis for improving current rehabilitation strategies and predicting re-injury risk.
Following a strain injury, muscle tissue is often unable to fully regenerate to its pre-injury state. For example, imaging studies have found evidence of scar tissue as soon as 6-weeks post injury (Connell et al., 2004), and animal models have shown that such scarring persists indefinitely (Best et al., 2001, Kaariainen et al., 2000). In a recent study, we presented evidence of scar tissue many months following an athlete's return to sport (Silder et al., 2008). It is likely that this injury-induced change alters in-vivo musculotendon mechanics. Specifically, the replacement of contractile tissue with connective scar tissue could change force transmission paths (Huijing, 2003) and alter the series stiffness experienced by adjacent muscle fibers. This may, in turn, influence force-length properties of the musculotendon unit and joint movement patterns.
It has also been shown that athletes who sustained a previous unilateral hamstring injury tend to develop peak knee flexion torque at a greater knee flexion angle (i.e., shorter muscle length) during isokinetic strength testing, when compared to the uninjured limb (Brockett et al., 2004). It was speculated that this difference may reflect a shorter optimal fiber length. Unfortunately, this study did not include image data, which prevents recognizing whether the observed bilateral differences in angle of peak torque evolved from injury-induced changes in musculotendon morphology. In a prior study (Silder et al., 2008), we found that significant atrophy of the biceps femoris long head and corresponding hypertrophy of the biceps femoris short head were present following injury, which could influence knee flexion strength patterns. Several authors have also suggested injury and re-injury risk may be influenced by hamstring weakness and/or a hamstrings:quadriceps strength imbalance (Orchard et al., 1997, Croisier et al., 2008, Yeung et al., 2009, Lee et al., 2009). Specifically, a relatively stronger quadriceps may act to increase the knee extension velocity during the second half of swing, thereby imposing large inertial loads on the active lengthening hamstrings (Orchard et al., 1997). In addition to muscular strength, neuromuscular adaptations can directly influence musculotendon mechanics during sprinting (Chumanov et al., 2007). Hence, previously injured athletes may display altered limb motion during the second half of swing phase, with the previously injured hamstrings to operating at shorter lengths compared to the contralateral uninjured limb. Such a compensation, if present, may either result directly from injury-induced morphological changes (Silder et al., 2008) or as a protective mechanism, aimed at diminishing the chance of over-stretching and re-injuring the muscle.
The primary purpose of this study was to investigate whether athletes with a history of a unilateral hamstring strain injury exhibit bilateral differences in (a) isokinetic strength characteristics and (b) musculotendon kinematics and neuromuscular control patterns during treadmill sprinting. Our secondary goal was to determine whether the magnitude of any functional asymmetries correlate with bilateral differences in tendon volumes, as measured using magnetic resonance (MR) imaging. We hypothesized that the previously injured limb would achieve peak force generation at a shorter hamstring length during isokinetic strength testing and display decreased hamstring stretch during treadmill sprinting compared to the uninjured limb, and finally, that the degree of functional asymmetry would increase with the amount of residual scar.
Methods
Eighteen athletes (ages 18-45 yrs) were tested who had experienced a unilateral hamstring strain between 5-13 months prior (Table 1). The initial diagnosis was made on the basis of subject questioning and clinical history and was confirmed using MR images obtained during the current study. Clinical notes indicated that all subjects sustained injuries to the biceps femoris (BF) on one or more occasions (Table 1). Eight subjects sustained at least one re-injury, with seven of these re-injuries clinically determined to occur in the same region (i.e. proximal or distal). For the 17 subjects with single injuries or isolated re-injuries (i.e. same location), 12 of these were proximal, one was mid-belly, and four were distal. The remaining subject sustained separate proximal and distal BF injuries. All subjects were involved in running-related sports, participated in a supervised rehabilitation program for a minimum of two weeks, and had since returned to full sporting participation.
Table 1.
Demographics and information regarding the prior hamstring injuries of the subjects participating in this study. Abbreviations: BF = biceps femoris.
| Subject | Gender | Age (yrs) | Months Since Injury | Side of Recent Injury | Location of Recent Injury | Number of Prior Injuries | Activity at Time of Injury |
|---|---|---|---|---|---|---|---|
| 1 | Male | 18 | 5 | Right | Proximal BF | 1 | Soccer |
| 2 | Male | 23 | 5 | Right | Distal BF | 2 | Track |
| 3 | Male | 19 | 13 | Left | Proximal BF | 2 | Track |
| 4 | Male | 31 | 5 | Left | Proximal BF | 2 | Football |
| 5 | Female | 19 | 7 | Left | Proximal BF | 2 | Track |
| 6 | Male | 18 | 10 | Right | Proximal BF | 1 | Track |
| 7 | Male | 19 | 7 | Right | Proximal BF | 1 | Track |
| 8 | Male | 18 | 8 | Left | Proximal BF | 1 | Track |
| 9 | Male | 46 | 7 | Left | Distal BF | 1 | Chasing kids |
| 10 | Male | 25 | 7 | Right | Proximal BF | 1 | Rugby |
| 11 | Female | 45 | 6 | Right | Distal BF | 1 | 10km race |
| 12 | Female | 43 | 9 | Right | Proximal BF | 2 | Softball |
| 13 | Male | 17 | 7 | Right | Proximal BF | 2 | Football |
| 14 | Female | 17 | 5 | Right | Distal BF | 2 | Track |
| 15 | Male | 20 | 7 | Right | Distal BF | 1 | Track |
| 16 | Male | 21 | 7 | Right | Mid-belly BF | 1 | Baseball |
| 17 | Male | 20 | 7 | Right | Proximal BF | 1 | Basketball |
| 18 | Male | 18 | 8 | Right | Proximal BF | 3 | Track |
Exclusion criteria included complete hamstring muscle disruption (grade III) or avulsion, current other lower extremity injury, history of hip or knee joint surgery, lower extremity nerve entrapment, and presence of lower extremity or back pain with running. Each subject or guardian provided written informed consent prior to testing, in accordance with the University of Wisconsin's Health Sciences Internal Review Board. The testing protocol included three parts: MR imaging, isokinetic knee flexion/extension strength testing, and a biomechanical assessment of treadmill sprinting.
MR Imaging Protocol
The presence of post-injury remodeling was assessed by collecting high resolution static images of both limbs using an investigational version of a previously described T1 weighted chemical shift based water-fat separation method known as IDEAL (Iterative Decomposition of water and fat with Echo Asymmetry and Least squares estimation) combined with three-dimensional spoiled gradient echo (SPGR) imaging (Reeder et al., 2007). IDEAL provides water-only images with uniform suppression of fat-signal over large fields-of-view. All subjects were scanned in a relaxed prone position using a clinical 1.5T MR scanner (Signa HDx v14.0 TwinSpeed, GE Healthcare, Waukesha, WI, USA). A phased array torso coil was used with the following scan parameters: coronal 3D slab, TR=12.5ms, 3 echoes (1 echo/TR) with TE=4.4, 5.0, 6.6ms, 15° flip angle; matrix, ±41.7kHz bandwidth, partial ky acquisition; 384×256 matrix with 46×46cm field-of-view with 84 slices, and 1.4mm slice thickness for a true spatial resolution of 1.2×1.8×1.4mm3 (interpolated to 0.9×0.9×7mm3). Water and fat images were created using homodyne reconstruction performed on-line (Reeder et al., 2005, Yu et al., 2005). The IDEAL image set was used to perform a bilateral comparison of the proximal BF tendon/aponeurosis. Tendon volumes were quantified for both limbs using manual segmentation on each image in which the structure was present. Volumes were calculated as the product of the inter-slice distance and the summed cross-sectional areas from all slices.
Strength Testing
Subjects were positioned on an isokinetic dynamometer (Biodex Multi-Joint System 2, Biodex Medical Systems, Inc., Shirley, NY, USA) such that the hip was flexed to 90 degrees and the dynamometer and knee joint axes were aligned. Strapping was used over the shank, thigh, and waist to constrain secondary joint movement. Each subject performed five consecutive concentric isokinetic (60 degree/s) knee flexion/extension cycles through his/her available range of motion and was verbally encouraged to perform at maximum effort. Joint angle and torque were recorded, and torque measurements were corrected for gravity. For each strength test, we determined the three cycles during which peak knee flexion torque was greatest, and then extracted the corresponding knee flexion angle of peak torque. Peak knee extension torque was found in an equivalent manner. Together, these data were used to quantify the hamstrings:quadriceps peak torque ratio.
Biomechanical Assessment of Treadmill Sprinting
Fifteen of the 18 subjects performed treadmill running at 60, 80, 90, and 100% of maximum sprinting speed. The inclusion of multiple running speeds enabled us to evaluate whether the presence of a bilateral asymmetry was speed dependent. Maximum sprinting speed (7.60±1.0 m/s) was determined using each subject's estimated 100m time. Whole body kinematics were recorded (200Hz) using an eight-camera passive marker system (Motion Analysis Corporation, Santa Rosa, CA, USA), which tracked 48 reflective markers, 30 of which were placed on anatomical landmarks. An upright calibration trial was first performed to establish joint centers, body segment coordinate systems, segment lengths, and the local positions of tracking markers. A voluntary hip circumduction movement was also performed, with the corresponding kinematic data used to estimate the hip joint center in the pelvis reference frame (Piazza et al., 2004). Trials were collected in order of increasing speed for subject safety, with five strides analyzed at each speed (total time per trial <10 s). Marker kinematics were used to compute three-dimensional lower extremity joint angles. These data were then used together with a scaled lower extremity musculoskeletal model (Delp et al., 1990, Hoy et al., 1990) to estimate bilateral musculotendon lengths for the BF throughout the running gait cycle. Peak musculotendon stretch was found at each speed by normalizing musculotendon lengths during sprinting to those measured from an upright standing posture. Software to perform the kinematic analyses were generated using SIMM Dynamics Pipeline (Motion Analysis; Santa Rosa, CA, USA) and SDFast (Parametric Technology Corp.; Needham, MA, USA).
Electromyography (EMG)
Bilateral muscle activities of the rectus femoris (RF), vastus lateralis (VL), BF, and medial hamstrings (MH) were recorded at 2000Hz using pre-amplified single differential surface electrodes (DE-2.1, DelSys, Inc, Boston, MA, USA). In preparation for electrode placement, each subject's skin was shaved and cleaned with alcohol. The electrodes were coated with conducting gel prior to application and interfaced with an amplifier/processor unit (CMRR > 85dB at 60Hz; input impedance > 100MΩ). The electrode locations were determined by the same investigator for each subject using standardized locations (Basmajian, 1985). EMG signals were bandpass filtered (20–500Hz) and then full wave rectified. Each signal was normalized to the mean signal for that muscle over an entire gait cycle from the 100% sprinting speed (Yang and Winter, 1984). The onset, offset, and duration of muscle activity, relative to a gait cycle, was manually determined (Li and Aruin, 2005). Magnitude of normalized EMG activity was assessed by finding the root-mean-square (RMS) value during each of four distinct phases of the gait cycle: loading, propulsion, initial swing, and terminal swing. These phases were defined by the instantaneous events of initial contact, stance phase reversal, toe-off, and swing phase reversal, where stance phase and swing phase reversal were each defined as the transition from knee flexion to extension (Novacheck, Ounpuu, 1990).
Statistical Analyses
Isokinetic strength measures (peak knee flexion torque; knee angle at peak flexion torque; hamstrings:quadriceps peak torque ratio) were compared between limbs using paired t-tests. Peak stretch of the BF and muscle activities during sprinting (timing and duration) were compared between limbs and across speeds using two way repeated measures ANOVAs. RMS muscle activities were compared between limbs, gait cycle phases, and across speeds using a three way repeated measures ANOVAs. Finally, Pearson correlations were used to determine if the amount of scarring influenced the degree of bilateral asymmetries measured during the strength testing and sprinting. Statistical significance was set at p<0.05 for all tests, with bilateral differences reported relative to the uninjured limb as either percent (100% * (injured - uninjured) / uninjured) or absolute (injured - uninjured).
Results
Strength testing measures revealed no significant bilateral differences in peak knee flexion torque (8.2±31.4%, p=0.44), angle of peak torque (2.0±14.4deg, p=0.33), or the hamstrings:quadriceps peak torque ratio (6±28%, p=0.63).
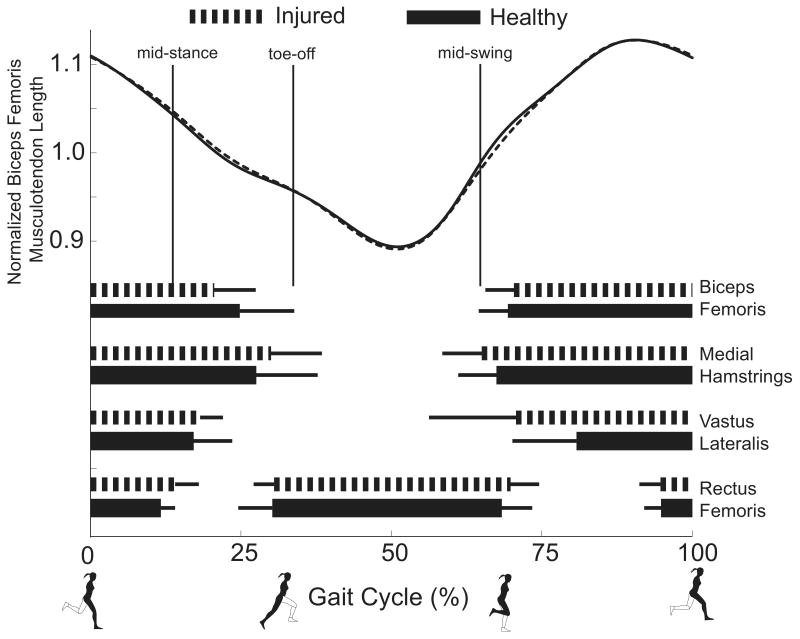
Peak BF musculotendon stretch during sprinting displayed no speed-by-limb interaction (p=0.86) and no significant main effect between limbs (absolute difference in peak stretch, 1±2mm, p=0.36). The ensemble averaged musculotendon length curves for both limbs across the gait cycle were nearly indistinguishable (Fig. 1).
Figure 1.
The ensemble averaged biceps femoris musculotendon lengths normalized to upright standing posture were nearly identical between the injured and uninjured limbs during sprinting (100% speed shown). The thick horizontal lines (standard deviation, thin line) represent when the rectus femoris, vastus lateralis, medial hamstrings, and biceps femoris muscles were active during the gait cycle. The combination of timing and musculotendon lengths emphasizes the role of the lengthening hamstrings to decelerate the limb prior to foot contact. Vertical lines depict the four phases analyzed: loading, propulsion, initial swing, and terminal swing
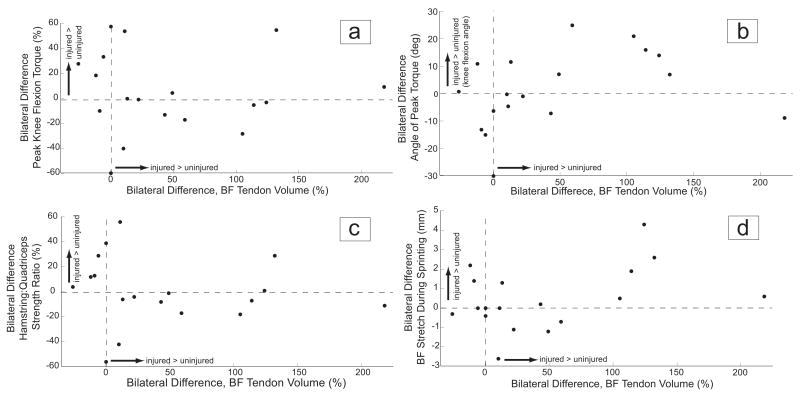
BF tendon volume was, on average, significantly larger for the previously injured limb (45±67%, p=0.01). However, the volumetric asymmetry was not correlated with the bilateral differences in isokinetic strength testing measures (peak knee flexion torque (Fig 3a), p=0.58, r=-0.16; angle of peak flexion torque (Fig. 3b), p=0.48, r=0.20; hamstring:quadriceps ratio (Fig. 3c), p=0.18, r=-0.37) or peak BF musculotendon stretch during sprinting (p=0.13, r=0.41) (Fig. 3d).
Figure 3.
Scatter plots demonstrate no significant relationship between bilateral differences in proximal biceps femoris (BF) tendon volume and bilateral differences in isokinetic strength measures: (a) peak knee flexion torque, (b) angle of peak knee flexion torque, and (c) the hamstrings:quadriceps strength ratio; or bilateral differences in (d) peak musculotendon stretch during sprinting. Note that bilateral differences in angle of peak torque and peak hamstring stretch are reported in absolute measures (injured-uninjured), while bilateral differences in peak knee flexion torque and hamstrings:quadriceps strength ratio are reported as a percent difference (=100%*(injured - uninjured) / uninjured).
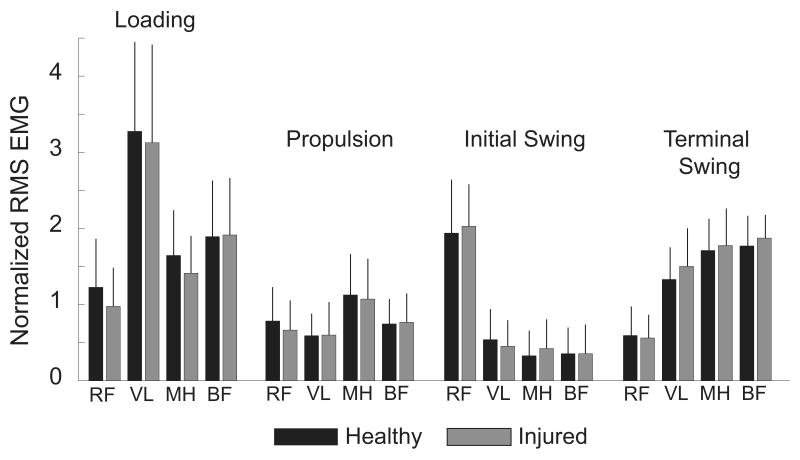
Onset, offset, and duration of muscle activities showed no significant interaction between limbs or across running speed. Further, there were no significant limb-by-speed interactions or main effects for the magnitudes of MH, BF, VL, or RF activity. A speed-by-phase interaction was observed for the VL (p=0.03), MH (p<0.01), and BF (p<0.01) muscles, but not RF (p=0.29). Specifically, both MH and BF activity were greatest during terminal swing and loading (Fig. 2).
Figure 2.
Ensemble averaged electromyographic (EMG) signals for the four muscles recorded (100% speed shown). No significant differences in the mean root-mean-square (RMS) activity were observed between limbs within any of the four phases (loading, propulsion, initial swing, and terminal swing). Abbreviations: RF, rectus femoris; VL, vastus lateralis; MH, medial hamstrings; BF, biceps femoris
As speed increased from 80-100%, BF activity during terminal swing increased an average of 67% while the MH showed a 37% increase. In contrast, during loading, BF activity increased only 34%, while MH activity increased 66%.
Discussion
In this study, we investigated how a prior hamstring injury and the presence of residual scar tissue might affect both the strength and function of the musculotendon unit. In a recent study, we used MR imaging to show that a significant degree of scar tissue can exist along the proximal musculotendon junction in individuals with a prior BF long head strain injury (Silder et al., 2008). These significant changes led us to hypothesize that functional adaptations may be detectable at the joint level. The current study included 11 subjects from the prior study (Silder et al., 2008), as well as seven additional subjects. All of the subjects sustained at least one injury to the proximal BF, which is the most common location for hamstring injury to occur (Verrall et al., 2003, Askling et al., 2007, Connell et al., 2004). Our results suggest that, while scar tissue may be present in subjects with a prior hamstring injury, these underlying morphological changes do not appear to be discernable in terms of functional strength measures, or musculotendon stretch and neuromuscular patterns during sprinting.
We hypothesized that the replacement of muscle with scar tissue following injury would reduce the optimum length for active force generation. Such a change would be detectable at the joint level in terms of peak isokinetic knee flexion torque occurring at a more flexed posture. Contrary to our hypothesis, we did not observe a consistent shift in the angle of peak torque across subjects. It is interesting to note that if we limited our analysis to only those nine subjects whose bilateral difference in tendon size exceeded the 95% confidence interval observed for uninjured athletes (±15% bilateral difference (Silder et al., 2008)), we found an average increase of 8° for the knee flexion angle of peak torque. However, this shift was inconsistent even within this subgroup of subjects (range, -8.8° to +25.0; standard deviation, 12°). Brockett and colleagues (Brockett et al., 2004) tested a group of previously injured athletes from the Australian Football League and found that peak torque in the previously injured limb occurred at a greater knee flexion angle (12° more) than the contralateral limb. They speculated that this change could be attributable to post-injury musculotendon remodeling, or alternatively, may be a training effect resulting from the repeat performance of concentric strengthening exercises during rehabilitation. While all subjects in our study underwent supervised rehabilitation, the rehabilitation program itself was not standardized across subjects. As a result, the observed differences between subjects may be influenced by specific aspects of the rehabilitation strategies employed. For example, we have observed hypertrophy of the biceps femoris short head in some subjects with prior hamstring injuries (Silder et al., 2008), which could be an exercise-induced compensation for injury to the biceps femoris long head. Such a compensation, which is enabled by the separate innervations of the long and short heads of biceps femoris, may allow for the preservation of overall knee flexion strength and thus contribute to the similar peak knee flexion torque observed in this, and other studies (Croisier, 2004).
Running mechanics were quantitatively assessed to ascertain how injury induced changes at the muscle level might be evidenced during running. Hamstring strain injuries are generally believed to occur during terminal swing (Heiderscheit et al., 2005, Wood, 1987). During this time, the hamstrings undergo an active lengthening contraction, with a reversal to musculotendon shortening prior to foot contact (Fig. 1). In the current study, we were not able to ascertain joint or muscle kinetics during sprinting. However, a prior simulation study suggested that increasing running speed magnifies the amount of energy absorbed by the lengthening hamstrings during terminal swing (Chumanov et al., 2007). Hence, a protective mechanism may involve adapting running in such a way that reduces the stretch and energy absorption of the previously injured hamstrings, particularly as speed increases. In this study, we assessed running kinematics at four speeds ranging from 60-100% of maximum sprinting speed. Contrary to our hypothesis, we detected no significant asymmetries in peak hamstring musculotendon stretch (Fig. 1) at any of the speeds tested. These kinematic results are in agreement with two similar studies (Lee et al., 2009, Brughelli et al., 2009) that tested a group of athletes with prior unilateral hamstring injuries running at submaximal running speeds. Thus, we conclude that changes in running mechanics due to a previous unilateral hamstring strain injury are likely not discernable in terms of asymmetric joint kinematic patterns.
We also measured muscle activities during running to assess whether compensatory strategies are reflected in neuromuscular control. While individual subjects exhibited some asymmetries in the timing and magnitude of hamstring activities, no consistent trends emerged. Of potential interest are the seemingly distinct roles of the medial and lateral hamstrings during terminal swing and loading as sprinting speed increased. Specifically, during terminal swing, BF activity increased nearly twice that of the MH. This factor could relate to the high prevalence of BF injuries, compared to the other hamstring muscles (Askling et al., 2007, Orchard and Best, 2002, Silder et al., 2008), and merits further investigation.
It is important to note that all of our sprint testing was done in a non-fatigued state with data collected for < 10s per speed. It has been previously shown that repeated tests at maximal sprinting effort can cause significant changes in running technique (Pinniger et al., 2000), such that asymmetries may arise due to fatigue. Additionally, our sprint testing protocol was conducted on a treadmill rather than over-ground. However, it has been shown that the mechanics of treadmill running are relatively similar to that observed over-ground (Riley et al., 2008). We also acknowledge the limitations of using generic musculoskeletal models (Thelen et al., 2005) to predict muscle lengths. In spite of this, analyses of hip and knee angles did not reveal asymmetries in running kinematics, thus supporting our results at the musculotendon level. Finally, since the method of computing percent change between limbs can lead to a skewed distribution, a non-parametric approach to the statistical analyses may be more appropriate. To account for this, repeat analysis using the non-parametric Wilcoxon rank test was conducted, but led to the same conclusions drawn from parametric tests.
Despite finding consistent morphological differences between limbs using MR imaging methods, we did not find bilateral differences in strength or running characteristics. This may be influenced, in part, by the heterogeneity (e.g. sport, rehabilitation, age) of our subject population, which is similar to a recent study that also included a variety of athletes (e.g. triathletes, soccer players, Australian Football players) (Lee et al., 2009). Yet, the findings of a more homogeneous group of semi-professional 22 year-old Australian Rules Football players also found no significant differences in sagittal plane kinematics during sub-maximal running (Brughelli et al., 2009).
Of note is that our protocol consisted of isokinetic concentric strength testing for both the hamstrings and quadriceps. Recent studies have found that the eccentric hamstring to concentric quadriceps strength ratio may be the more important measure as a predictor of injury (Croisier et al., 2008), as well as an indicator of full recovery following a hamstring strain injury (Lee et al., 2009, Croisier et al., 2002). Further, this study was purely retrospective such that we cannot truly determine whether observed asymmetries were already present prior to the hamstring injury occurrence and what injury risk factors may have been pre-existing. Although the greatest risk factor for strain injury is a previous injury (Orchard, 2001, Jonhagen et al., 1994, Askling et al., 2006), re-injury risk has also been linked with a number of factors including age, inadequate rehabilitation and hamstring/quadriceps strength imbalances (Lee et al., 2009, Gabbe et al., 2006, Croisier et al., 2008). Finally, when interpreting the results of this study, it is important to recognize that asymmetries during running and strength testing may be influenced by limb dominance, severity of the initial injury, and the frequency and intensity of training upon return to sport.
In conclusion, the results of this study further demonstrate that residual scar tissue can persist in persons with a prior acute muscle strain injury, but that such morphological changes are not likely discernable from joint level mechanics or neuromuscular control patterns. Further research is warranted to ascertain whether residual scarring may alter more localized musculotendon tissue mechanics and thereby contribute to high rates of muscle re-injury that are observed clinically.
Acknowledgments
The authors would like to acknowledge Mike Tuite, MD, for his assistance in MR imaging collection and analysis. We would also like to thank Marc Sherry, DPT, LAT, CSCS, PES, and Nathan Brown for their help with subject recruitment as well as Sijian Wang, PhD for his statistical consultation. This work was funded by a National Science Foundation Predoctoral Fellowship (AS), the National Football League Charities, the University of Wisconsin Sports Medicine Classic Grant, and the National Institutes of Health (1UL2RR025012, AR056201).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arnason A, Sigurdsson SB, Gudmundsson A, Holme I, Engebretsen L, Bahr R. Risk factors for injuries in football. Am J Sports Med. 2004;32:5S–16S. doi: 10.1177/0363546503258912. [DOI] [PubMed] [Google Scholar]
- Askling C, Karlsson J, Thorstensson A. Hamstring injury occurrence in elite soccer players after preseason strength training with eccentric overload. Scandinavian Journal of Medicine & Science in Sports. 2003;13:244–250. doi: 10.1034/j.1600-0838.2003.00312.x. [DOI] [PubMed] [Google Scholar]
- Askling C, Saartok T, Thorstensson A. Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. Br J Sports Med. 2006;40:40–4. doi: 10.1136/bjsm.2005.018879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during slow-speed stretching: clinical, magnetic resonance imaging, and recovery characteristics. Am J Sports Med. 2007;35:1716–24. doi: 10.1177/0363546507303563. [DOI] [PubMed] [Google Scholar]
- Basmajian JV, De Luca CJ. Muscles Alive: Their Functions Revealed by Electromyography. Baltimore: Williams & Wilkins; 1985. [Google Scholar]
- Bennell KL, Crossley K. Musculoskeletal injuries in track and field: incidence, distribution and risk factors. Aust J Sci Med Sport. 1996;28:69–75. [PubMed] [Google Scholar]
- Best TM, Shehadeh SE, Leverson G, Michel JT, Corr DT, Aeschlimann D. Analysis of changes in mRNA levels of myoblast- and fibroblast-derived gene products in healing skeletal muscle using quantitative reverse transcription-polymerase chain reaction. Journal of Orthopaedic Research. 2001;19:565–72. doi: 10.1016/S0736-0266(00)00067-X. [DOI] [PubMed] [Google Scholar]
- Brockett CL, Morgan DL, Proske U. Predicting hamstring strain injury in elite athletes. Medicine & Science in Sports & Exercise. 2004;36:379–87. doi: 10.1249/01.mss.0000117165.75832.05. [DOI] [PubMed] [Google Scholar]
- Brughelli M, Cronin J, Mendiguchia J, Kinsella D, Nosaka K. Contralateral Leg Deficits in Kinetic and Kinematic Variables During Running in Australian Rules Football Players With Previous Hamstring Injuries. J Strength Cond Res. 2009 doi: 10.1519/JSC.0b013e3181b603ef. [DOI] [PubMed] [Google Scholar]
- Chumanov ES, Heiderscheit BC, Thelen DG. The effect of speed and influence of individual muscles on hamstring mechanics during the swing phase of sprinting. J Biomech. 2007;40:3555–62. doi: 10.1016/j.jbiomech.2007.05.026. [DOI] [PubMed] [Google Scholar]
- Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, Burke F, Bass C. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR American Journal of Roentgenology. 2004;183:975–84. doi: 10.2214/ajr.183.4.1830975. [DOI] [PubMed] [Google Scholar]
- Croisier JL. Factors associated with recurrent hamstring injuries. Sports Medicine. 2004;34:681–95. doi: 10.2165/00007256-200434100-00005. [DOI] [PubMed] [Google Scholar]
- Croisier JL, Forthomme B, Namurois MH, Vanderthommen M, Crielaard JM. Hamstring muscle strain recurrence and strength performance disorders. American Journal of Sports Medicine. 2002;30:199–203. doi: 10.1177/03635465020300020901. [DOI] [PubMed] [Google Scholar]
- Croisier JL, Ganteaume S, Binet J, Genty M, Ferret JM. Strength imbalances and prevention of hamstring injury in professional soccer players: a prospective study. Am J Sports Med. 2008;36:1469–75. doi: 10.1177/0363546508316764. [DOI] [PubMed] [Google Scholar]
- Delp SL, Loan JP, Hoy MG, Zajac FE, Topp EL, Rosen JM. An interactive graphics-based model of the lower extremity to study orthopaedic surgical procedures. IEEE Trans Biomed Eng. 1990;37:757–67. doi: 10.1109/10.102791. [DOI] [PubMed] [Google Scholar]
- Gabbe BJ, Bennell KL, Finch CF, Wajswelner H, Orchard JW. Predictors of hamstring injury at the elite level of Australian football. Scand J Med Sci Sports. 2006;16:7–13. doi: 10.1111/j.1600-0838.2005.00441.x. [DOI] [PubMed] [Google Scholar]
- Heiderscheit BC, Hoerth DM, Chumanov ES, Swanson SC, Thelen BJ, Thelen DG. Identifying the time of occurrence of a hamstring strain injury during treadmill running: a case study. Clin Biomech (Bristol, Avon) 2005;20:1072–8. doi: 10.1016/j.clinbiomech.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Hoy MG, Zajac FE, Gordon ME. A musculoskeletal model of the human lower extremity: the effect of muscle, tendon, and moment arm on the moment-angle relationship of musculotendon actuators at the hip, knee, and ankle. J Biomech. 1990;23:157–69. doi: 10.1016/0021-9290(90)90349-8. [DOI] [PubMed] [Google Scholar]
- Huijing PA. Muscular force transmission necessitates a multilevel integrative approach to the analysis of function of skeletal muscle. Exerc Sport Sci Rev. 2003;31:167–75. doi: 10.1097/00003677-200310000-00003. [DOI] [PubMed] [Google Scholar]
- Jonhagen S, Nemeth G, Eriksson E. Hamstring injuries in sprinters. The role of concentric and eccentric hamstring muscle strength and flexibility. American Journal of Sports Medicine. 1994;22:262–6. doi: 10.1177/036354659402200218. [DOI] [PubMed] [Google Scholar]
- Kaariainen M, Jarvinen T, Jarvinen M, Rantanen J, Kalimo H. Relation between myofibers and connective tissue during muscle injury repair. Scandinavian Journal of Medicine & Science in Sports. 2000;10:332–7. doi: 10.1034/j.1600-0838.2000.010006332.x. [DOI] [PubMed] [Google Scholar]
- Lee MJ, Reid SL, Elliott BC, Lloyd DG. Running Biomechanics and Lower Limb Strength Associated with Prior Hamstring Injury. Med Sci Sports Exerc. 2009 doi: 10.1249/MSS.0b013e3181a55200. [DOI] [PubMed] [Google Scholar]
- Li X, Aruin A. Muscle activity onset time detection using teager-kaiser energy operator. Conf Proc IEEE Eng Med Biol Soc. 2005;7:7549–52. doi: 10.1109/IEMBS.2005.1616259. [DOI] [PubMed] [Google Scholar]
- Novacheck TF. Walking, running, and sprinting: a three-dimensional analysis of kinematics and kinetics. [PubMed] [Google Scholar]
- Orchard J, Best TM. The management of muscle strain injuries: an early return versus the risk of recurrence. Clinical Journal of Sport Medicine. 2002;12:3–5. doi: 10.1097/00042752-200201000-00004. [DOI] [PubMed] [Google Scholar]
- Orchard J, Marsden J, Lord S, Garlick D. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am J Sports Med. 1997;25:81–5. doi: 10.1177/036354659702500116. [DOI] [PubMed] [Google Scholar]
- Orchard J, Seward H. Epidemiology of injuries in the Australian Football League, seasons 1997-2000. Br J Sports Med. 2002;36:39–44. doi: 10.1136/bjsm.36.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orchard JW. Intrinsic and extrinsic risk factors for muscle strains in Australian football. American Journal of Sports Medicine. 2001;29:300–3. doi: 10.1177/03635465010290030801. [DOI] [PubMed] [Google Scholar]
- Ounpuu S. The biomechanics of running: a kinematic and kinetic analysis. Instr Course Lect. 1990;39:305–18. [PubMed] [Google Scholar]
- Piazza SJ, Erdemir A, Okita N, Cavanagh PR. Assessment of the functional method of hip joint center location subject to reduced range of hip motion. J Biomech. 2004;37:349–56. doi: 10.1016/s0021-9290(03)00288-4. [DOI] [PubMed] [Google Scholar]
- Pinniger GJ, Steele JR, Groeller H. Does fatigue induced by repeated dynamic efforts affect hamstring muscle function? Med Sci Sports Exerc. 2000;32:647–53. doi: 10.1097/00005768-200003000-00015. [DOI] [PubMed] [Google Scholar]
- Reeder SB, Hargreaves BA, Yu H, Brittain JH. Homodyne reconstruction and IDEAL water-fat decomposition. Magn Reson Med. 2005;54:586–93. doi: 10.1002/mrm.20586. [DOI] [PubMed] [Google Scholar]
- Reeder SB, Mckenzie CA, Pineda AR, Yu H, Shimakawa A, Brau AC, Hargreaves BA, Gold GE, Brittain JH. Water-fat separation with IDEAL gradient-echo imaging. J Magn Reson Imaging. 2007;25:644–52. doi: 10.1002/jmri.20831. [DOI] [PubMed] [Google Scholar]
- Riley PO, Dicharry J, Franz J, Della Croce U, Wilder RP, Kerrigan DC. A kinematics and kinetic comparison of overground and treadmill running. Med Sci Sports Exerc. 2008;40:1093–100. doi: 10.1249/MSS.0b013e3181677530. [DOI] [PubMed] [Google Scholar]
- Silder A, Heiderscheit BC, Thelen DG, Enright T, Tuite MJ. MR observations of long-term musculotendon remodeling following a hamstring strain injury. Skeletal Radiol. 2008;37:1101–9. doi: 10.1007/s00256-008-0546-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thelen DG, Chumanov ES, Hoerth DM, Best TM, Swanson SC, Li L, Young M, Heiderscheit BC. Hamstring muscle kinematics during treadmill sprinting. Medicine and Science in Sports and Exercise. 2005;37:108–114. doi: 10.1249/01.mss.0000150078.79120.c8. [DOI] [PubMed] [Google Scholar]
- Verrall GM, Slavotinek JP, Barnes PG, Fon GT. Diagnostic and prognostic value of clinical findings in 83 athletes with posterior thigh injury: comparison of clinical findings with magnetic resonance imaging documentation of hamstring muscle strain. Am J Sports Med. 2003;31:969–73. doi: 10.1177/03635465030310063701. [DOI] [PubMed] [Google Scholar]
- Wood G. Biomechanical limitations to sprint running. Med Sci Sports Exerc. 1987;25:58–71. [Google Scholar]
- Woods C, Hawkins RD, Maltby S, Hulse M, Thomas A, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football--analysis of hamstring injuries. Br J Sports Med. 2004;38:36–41. doi: 10.1136/bjsm.2002.002352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang JF, Winter DA. Electromyographic amplitude normalization methods: improving their sensitivity as diagnostic tools in gait analysis. Arch Phys Med Rehabil. 1984;65:517–21. [PubMed] [Google Scholar]
- Yeung SS, Suen AM, Yeung EW. A prospective cohort study of hamstring injuries in competitive sprinters: preseason muscle imbalance as a possible risk factor. Br J Sports Med. 2009;43:589–94. doi: 10.1136/bjsm.2008.056283. [DOI] [PubMed] [Google Scholar]
- Yu H, Reeder SB, Shimakawa A, Brittain JH, Pelc NJ. Field map estimation with a region growing scheme for iterative 3-point water-fat decomposition. Magn Reson Med. 2005;54:1032–9. doi: 10.1002/mrm.20654. [DOI] [PubMed] [Google Scholar]