A 58-year-old woman presented with 3 weeks of progressive apathy, irritability, and confusion. MRI (figure 1) demonstrated a contrast-enhancing, bifrontal lesion crossing the corpus callosum, suggestive of high-grade glioma. Pathology showed active demyelination (figure 2). Tumefactive demyelinating lesions typically demonstrate partial or complete ring enhancement, absent in this case.1 Although butterfly lesions commonly represent high-grade glioma or lymphoma, demyelinating disease must be considered. Our patient received steroids with complete clinical resolution. Expected long-term outcome for such patients remains controversial. Patients do not universally develop clinically definite multiple sclerosis, and may fare better than typical relapsing-remitting cases, despite the striking radiologic appearance.2
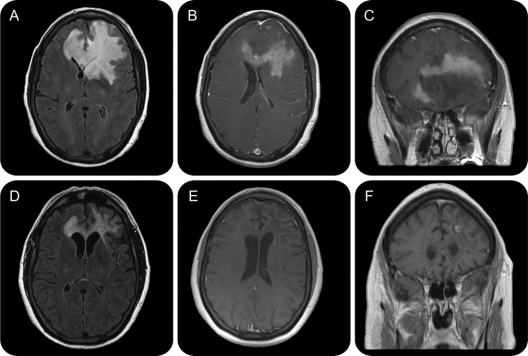
Figure 1 MRI of demyelinating disease mimicking tumor
(A) Fluid-attenuated inversion recovery (FLAIR) image demonstrates homogeneous hyperintense T2 signal abnormality. (B, C) Axial and coronal T1 postcontrast images demonstrate fluffy enhancement in the central portion of the mass, and crossing the genu of the corpus callosum. (D-F) Corresponding FLAIR and T1 postcontrast axial and coronal images 3 months later.
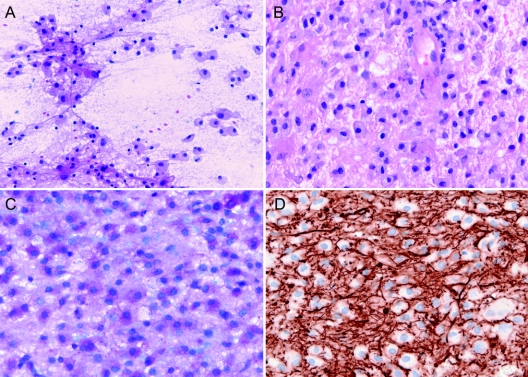
Figure 2 Pathology confirming demyelination
Intraoperative smears (A) and hematoxylin-eosin section (B) highlight the presence of a large number of foamy macrophages and scattered reactive astrocytes. Luxol fast blue/periodic acid-Schiff stain (C) demonstrates myelin loss while axons are preserved, as demonstrated by neurofilament stain (D).
Address correspondence and reprint requests to Dr. Michelle L. Mauermann, 200 First Street SW, Rochester, MN 55905 mauermann.michelle@mayo.edu
*These authors contributed equally to the manuscript.
Disclosure: Dr. Bower, Dr. Burrus, and Dr. Giannini report no disclosures. Dr. Erickson serves as an Associate Editor of the Journal of Digital Imaging; may accrue revenue on patents re: Automatic windowing method for MR Images; Method for automated change detection in brain MRI, Method for detection of aneurysm detection on MRA, and Method for prediction of cryoablation treatment zone; serves as Director of a collaborative center with IBM Corporation; and receives research support from the NIH (NCI R21CA121539 [PI]). Dr. Meyer serves as co-chairman of the editorial board of the Journal of Neurosurgery. Dr. Pirko serves as Clinical Editor for Nanomedicine: NBM; and receives research support from the NIH (R01NS058698 [PI]). Dr. Mauermann reports no disclosures.
REFERENCES
- 1.Schwartz KM, Erickson BJ, Lucchinetti C. Pattern of T2 hypointensity associated with ring-enhancing brain lesions can help to differentiate pathology. Neuroradiology 2006;48:143–149. [DOI] [PubMed] [Google Scholar]
- 2.Lucchinetti CF, Gavrilova RH, Metz I, et al. Clinical and radiographic spectrum of pathologically confirmed tumefactive multiple sclerosis. Brain 2008;131:1759–1775. [DOI] [PMC free article] [PubMed] [Google Scholar]