Abstract
Background
Digoxin has been shown to reduce heart failure (HF) hospitalizations with no overall effect on mortality in HF patients. We used cluster analysis to delineate the clinical characteristics of HF patients in whom digoxin therapy was associated with improved or worsened clinical outcomes.
Methods
The Digitalis Investigation Group (DIG) database was partitioned into 20 clusters. Multivariate Cox regression analyses was used, to identify clusters in which digoxin was associated with either an increase (MortalitydigHR>1), decrease (MortalitydigHR<1), or no association with all cause mortality (MortalitydigHR-NS); and separately, with an increase (HFAdigHR>1), decrease (HFAdigHR<1), or no association (HFAdigHR-NS) with HF admissions (HFA).
Results
We identified 938 patients in the MortalitydigHR>1 group, 6,818 patients in the MortalitydigHR-NS group, and none in MortalitydigHR<1 group. The MortalitydigHR>1 group had a higher prevalence of females, diabetes mellitus, hypertension, higher age, systolic blood pressure (SBP), heart rate and ejection fraction (EF), compared to the MortalitydigHR-NS group.
Similarly, 6,325 patients clustered in the HFAdigHR<1 group, 1,431 patients in the HFAdigHR-NS group, and none in the HFAdigHR>1 group. The HFAdigHR-NS group had a higher prevalence of females and hypertension, higher SBP, body mass index and EF; and lower prevalence of peripheral edema and third heart sound, compared with the HFAdigHR<1 group.
Conclusion
Thus, the baseline characteristics of patients who did not have reduction in HF hospitalization or who had increased mortality were very similar and included females with hypertension, higher EF and higher SBP. Thus, use of digoxin in patients with this profile may need to be avoided.
Keywords: Cluster analysis, digoxin, heart failure
Introduction
The Digitalis Investigation Group (DIG) Trial (1) was a landmark randomized, double-blind, placebo controlled multi-center trial on the effectiveness of digoxin in patients with congestive heart failure (HF). The DIG trial showed that although digoxin did not reduce overall mortality, it reduced admissions due to HF. Subsequent post-hoc analyses of the DIG trial data by other investigators raised some concerns that digoxin treatment was non-beneficial or harmful in certain subgroups of patients, in particular females and elderly with high serum digoxin levels (2–4). Currently, American College of Cardiology/American Heart Association HF guidelines (5,6) recommend consideration of adding digoxin in patients with persistent symptoms of HF during therapy with diuretics, angiotensin converting enzyme (ACE) inhibitors, and beta-blockers (Class II indication). At the present time, it is not clear whether digoxin treatment should be avoided in females, elderly, or in patients with preserved ejection fraction (EF) or any other subgroup of patients (7). The guidelines acknowledge the suggested concern regarding safety and efficacy of digoxin in certain subgroups, but do not provide clear recommendations against digoxin use in any subgroups.
We hypothesized that the response to digoxin among HF patients is heterogeneous and will differ according to severity of HF, i.e. patients with advanced HF will benefit from digoxin therapy, whereas patients with mild HF will not benefit from digoxin therapy. Furthermore, use of digoxin in patients with mild HF may lead to increased morbidity and mortality due to added burden of side effects. Realizing that advanced HF is characterized by multiple features including high NYHA class, low systolic blood pressure (SBP), low EF, increased prevalence of comorbidities etc. we also hypothesized that cluster analysis will allow us identify specific subgroups of patients, with compounding risk features more comprehensively than the formerly identified simple single step subgroup analyses, that may have harm or benefit with digoxin therapy. To characterize subpopulations of HF patients in which digoxin therapy is associated with improved or worsened clinical outcomes, we analyzed the DIG data by using cluster analysis, a method by which large heterogeneous data are divided into homogeneous groups. Using this method, the effect of intervention can be analyzed separately in each such group. Cluster analysis allows for the creation of respondent groupings characterized by their similar responses to the intervention. (8) As the number of subjects in a study increases, the assumptions surrounding smooth approximation of association (hazards) by a single universal predictive model begin to break down. Patient sub-populations derived from cluster analysis represent natural groupings, such as clustering of preserved EF with hypertension, older age and female gender. These patients are more homogeneous than class labeled sequential subgroups, which may not capture the cluster with the presence of all the relevant harmful or beneficial characteristics.
Therefore, in this study we employed cluster analysis followed by cluster-specific survival analysis to identify homogenous groups of patients for which digoxin may be beneficial or harmful.
Methods
DIG Trial
The rationale, design and results of the DIG trial have been previously reported (1,9). A total of 7,788 ambulatory adults with chronic HF, in sinus rhythm were randomized to receive either digoxin or placebo. These patients were recruited from 302 clinical centers in the United States and Canada from 1991 to 1993. Most patients were receiving diuretics (82%) and ACE inhibitors (94%) and the mean duration of follow up was 37 months.
Patients, Baseline Variables and Outcomes
Thirty-two patients out of total 7,788 patients were removed from the analysis because of missing data for 1 or more variables. Variables with significant univariate association with outcomes of all cause mortality were included in the analysis, and were: age, gender, race, diabetes mellitus (DM), hypertension, ischemic cause of HF, NYHA class, limitation of activity, SBP, heart rate, body mass index, third heart sound, edema in extremities, congestion on chest x-ray, EF, cardiothoracic ratio, creatinine, and medication use including ACE inhibitors, potassium-sparing diuretics and other classes of diuretics. On the other hand, 4 variables were excluded from further analyses due to high multicollinearity, namely: dyspnea on exertion (r=0.421 with NYHA class, p<0.001), dyspnea at rest (r=0.336 with NYHA class, p<0.001), pulmonary rales (r=0.442 with congestion on X-ray, p<0.001), and jugular venous distension (r=0.310 with congestion on X-ray, p<0.001). The primary time-to-event outcomes used for this investigation were days to all cause mortality (henceforth referred to as mortality) and days to admission due to HF (henceforth referred to as HF admission).
Statistical Analysis
Cluster analysis of patients was performed using K-means cluster analysis and self-organizing maps (SOM) as described by Kohonen (8). All of the variables (features) described above were used in K means and SOM analysis except for digoxin treatment and time (days) to an event. Because of scaling requirements of SOM analysis, input variable values were transformed using mean-zero standardization or normalization into the range [0,1]. Altogether, this resulted in 3 clustering methods.
An initial K-means cluster analysis was performed to identify the optimal number of K clusters. Ten-fold cross-validation was used to identify the value of K for which the average sample-to-centroid distance was the lowest. Results indicated that the lowest average sample-to-centroid distance occurred at K=21 clusters, so it was decided to round down to K=20. Patients were partitioned into 20 clusters using K-means (K=20) and SOM based on a 20-node (4×5) map. During SOM runs, patient cluster assignments were based on the best matching node. Using K=20 clusters, there were more than 350 subjects in each cluster including treated and untreated patients.
Multivariate Cox regression analysis was performed separately on each cluster to obtain a hazard ratio of digoxin treatment for mortality and HF admission. Backward stepping was used with variable removal set at p=0.05. Variables used for Cox regression analysis were digoxin and the 20 variables described above. Time to admission was based on days and the outcome events defining failure were mortality and HF hospitalization.
For mortality, there were no clusters for which there was a significant protective effect (hazard ratio<1). On the other hand, there were clusters for which digoxin was associated with a significant increase in mortality (hazard ratio>1), specifically, 1 cluster each from analysis with K-means and SOM using standardized features and 2 from analysis with SOM using normalized features. Patients belonging to any of these clusters were merged together to form a MortalitydigHR>1 group, with the remainder merged into MortalitydigHR-NS group.
There were no clusters with a significant increase in HF hospitalization with digoxin (hazard ratio>1). However, there were clusters with a significant reduction in HF hospitalizations (hazard ratio<1) with digoxin, specifically, 9 each from analysis with K-means and SOM using standardized features, and 10 from analysis with SOM using normalized features. Patients belonging to any of these clusters were merged together to form a HFAdigHR<1 group, with the remainder merged into a HFAdigHR-NS group.
Univariate tests of independence were performed on the 20 baseline characteristics to identify significantly different factors between treated and untreated patients within the 2 mortality groups (MortalitydigHR>1 and MortalitydigHR-NS) and the 2 HFA groups (HFAdigHR<1 and HFAdigHR-NS) (Table 1). Chi-square contingency table analysis was used for categorical variables and the non-parametric Mann-Whitney test was used for continuous data. A significance level of p<0.05 was considered significant, while p<0.001 was considered highly significant. Kaplan-Meier analysis of digoxin treatment was performed within the mortality and HFA groups to demonstrate the risks of digoxin treatment. Baseline characteristics were compared between MortalitydigHR>1 vs. MortalitydigHR-NS and HFAdigHR<1 vs. HFAdigHR-NS to identify characteristics associated with these outcomes. Effect sizes were considered large if the odds ratio was <0.5 or >2.0 for binary categorical variables and |Z|>10 for continuous variables. Variables with large size effect (odds ratio <0.5 or >2 or |Z|>10) and a highly significant difference (p<0.001) between comparison groups were included in the results and discussion. This was done to restrict our discussion to the most relevant characteristics with large effect. To validate the contributory role of cluster analysis, we also carried out stepwise Cox proportional multivariate analyses with expanding subgroups. Statistical analyses were performed using SPSS Version 17 (Chicago, IL).
Table 1A.
Baseline characteristics of patients in MortalitydigHR-NS group and MortalitydigHR>1 group.
| Mortality digHR-NS, n=6818 | MortalitydigHR>1, n=938 | |||||
|---|---|---|---|---|---|---|
| Digoxin (n=3400) | Placebo (n=3418) | p value | Digoxin (n=470) | Placebo (n=468) | p value | |
| Continuous/ordinal variables (mean±SD) | ||||||
| Age (yrs) | 63±11 | 63±11 | 0.61 | 68±9 | 68±9 | 0.69 |
| NYHA class | 2.2±0.7 | 2.2±0.7 | 0.97 | 2.2±0.7 | 2.2±0.7 | 1.0 |
| SBP (mmHg) | 124±17 | 124±17 | 0.42 | 148±17 | 147±18 | 0.62 |
| Heart rate (bpm) | 78±13 | 78±13 | 0.07 | 83±13 | 83±12 | 0.79 |
| BMI | 27.0±5.2 | 27.2±5.2 | 0.05 | 28±6 | 29±6 | 0.67 |
| Cardiothoracic ratio | 0.5±0.07 | 0.5±0.07 | 0.93 | 0.5±0.08 | 0.5±0.08 | 0.88 |
| EF (%) | 31±12 | 31±12 | 0.57 | 40±15 | 40±15 | 0.79 |
| Creatinine (mg/dl) | 1.3±0.4 | 1.3±0.4 | 0.53 | 1.3±0.4 | 1.3±0.5 | 0.65 |
| Categorical variables (%) | ||||||
| Females | 20 | 20 | 1 | 58 | 58 | 1.0 |
| Race (Caucasians) | 86 | 86 | 0.63 | 84 | 84 | 0.86 |
| DM | 25 | 25 | 0.98 | 54 | 59 | 0.09 |
| Hypertension | 43 | 43 | 0.86 | 76 | 75 | 0.82 |
| Ischemic etiology | 70 | 69 | 0.56 | 65 | 67 | 0.54 |
| Limitation-activity | 75 | 76 | 0.61 | 77 | 77 | 0.94 |
| Peripheral edema | 21 | 21 | 1 | 22 | 19 | 0.22 |
| S3 | 26 | 23 | 0.02 | 20 | 20 | 0.87 |
| X-ray congestion | 14 | 14 | 0.84 | 16 | 14 | 0.65 |
| ACE inhibitor use | 93 | 94 | 0.22 | 92 | 92 | 0.63 |
| Diuretic use | 77 | 77 | 0.75 | 83 | 85 | 0.42 |
| Potassium sparing diuretic use | 7 | 9 | 0.02 | 7 | 6 | 0.35 |
BMI: body mass index; DM: diabetes mellitus; EF: ejection fraction; MortalitydigHR-NS: group with non-significant association of digoxin use with all cause mortality; MortalitydigHR>1: group with increase in all cause mortality with use of digoxin; S3: third heart sound; SBP: systolic blood pressure.
Results
Mortality
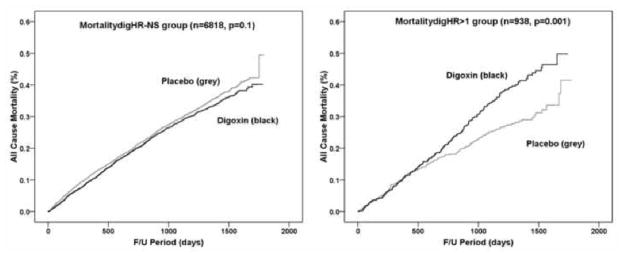
Of the 7,756 patients studied, we identified 938 patients in MortalitydigHR>1 group and 6,818 patients in MortalitydigHR-NS group. Among the 20 baseline variables compared between treatment and placebo in MortalitydigHR-NS group and MortalitydigHR>1 group, only body mass index, the presence of a third heart sound, and use of potassium-sparing diuretic were significantly different in MortalitydigHR-NS group (Table 1A). Kaplan-Meier analysis of digoxin treatment within MortalitydigHR-NS group revealed no significant reduction in mortality (days to death = 1,380 for patients on digoxin vs. 1,356 for patients on placebo logrank χ2=2, p=0.1) (Figure 1A). Kaplan-Meier analysis of digoxin treatment within MortalitydigHR>1group showed a significant increase in mortality with the use of digoxin (mean days to death = 1,292 for patients on digoxin vs. 1,414 for patients on placebo, logrank χ2=12, p=0.001) (Figure 1A). After confirming that MortalitydigHR-NS and MortalitydigHR>1 groups were 2 clinically distinct groups in relation to the response to digoxin (Figure 1A) and intrinsically homogenous (Table 1A), we compared the baseline variables between these 2 groups. MortalitydigHR>1 group had a greater proportion of females, higher prevalence of DM and hypertension; older age; higher SBP, heart rate and EF when compared with MortalitydigHR-NS group, (Table 2A).
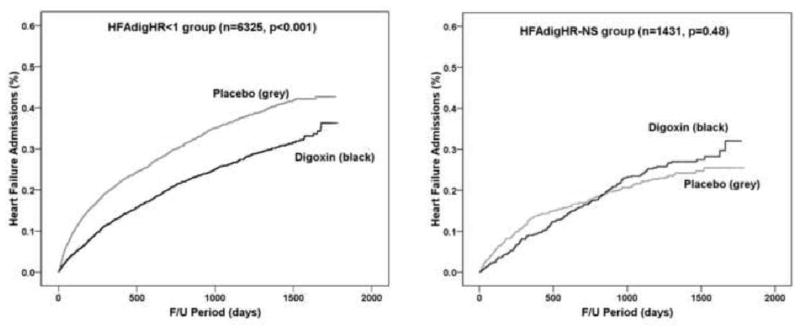
Figure 1. Survival analysis using Kaplan Meier curves comparing digoxin use with placebo.
A. All cause mortality in the digoxin and placebo treatment groups. Left panel represents the Kaplan Meier 1-survival curves for all cause mortality among clusters of patients with no significant association of digoxin with mortality (MortalitydigHR-NS). Right panel represents the Kaplan Meier 1-survival curves for all cause mortality among clusters of patients with a significant increase in mortality with the use of digoxin (MortalitydigHR>1). B. Incidence of hospitalization due to worsening HF (HF Admission) in the digoxin and placebo groups. Left panel represents the Kaplan Meier 1-survival curves for hospitalization due to worsening HF among clusters of patients with a significant reduction in HF hospitalization with the use of digoxin (HFAdigHR<1). Right panel represents the Kaplan Meier 1-survival curves for hospitalization due to worsening HF among clusters of patients with no significant association of digoxin with HF hospitalization (HFAdigHR-NS).
Table 2A.
Baseline characteristics of patients in MortalitydigHR-NS group vs. MortalitydigHR>1 group.
| MortalitydigHR-NS | MortalitydigHR>1 | Odds ratio | |Z| | p value | |
|---|---|---|---|---|---|
| n=6818 | n=938 | ||||
| Continuous/ordinal variables (mean±SD) | |||||
| Age (yrs) | 63±11 | 68±9 | 12 | <0.001 | |
| NYHA class | 2.2±0.7 | 2.2±0.7 | 0.10 | ||
| SBP (mmHg) | 124±17 | 147±17 | 33 | <0.001 | |
| Heart rate (bpm) | 78±13 | 83±12 | 12 | <0.001 | |
| BMI | 27±5 | 29±6 | 7 | <0.001 | |
| Cardiothoracic ratio | 0.53±0.07 | 0.54±0.08 | 3 | 0.002 | |
| EF (%) | 31±12 | 40±15 | 18 | <0.001 | |
| Creatinine (mg/dl) | 1.3±0.4 | 1.3±0.4 | 0.84 | ||
| Categorical variables (%) | |||||
| Females | 20 | 58 | 5.6 | <0.001 | |
| Race (Caucasians) | 86 | 84 | 0.137 | ||
| DM | 25 | 56 | 3.3 | <0.001 | |
| Hypertension | 43 | 75 | 3.3 | <0.001 | |
| Ischemic etiology | 69 | 66 | 0.07 | ||
| Limitation - activity | 76 | 77 | 0.27 | ||
| Peripheral edema | 21 | 20 | 0.58 | ||
| S3 | 24 | 20 | 0.77 | 0.004 | |
| X-ray congestion | 14 | 15 | 0.55 | ||
| ACE inhibitor use | 94 | 92 | 0.05 | ||
| Diuretic use | 77 | 84 | 1.7 | <0.001 | |
| Potassium sparing diuretic use | 8 | 6 | 0.13 | ||
| Digoxin use | 50 | 50 | 0.92 | ||
p value of <0.001 was considered highly significant. Odds ratio and Z score are for variables in MortalitydigHR>1 group in comparison with MortalitydigHR:NS group. Odds ratio <0.5 or >2 and |Z|>10 was considered as a large effect size. Bold variables indicate a highly significant difference with a large effect size. BMI: body mass index; DM: diabetes mellitus; EF: ejection fraction; MortalitydigHR-NS: group with non-significant association of digoxin use with all cause mortality; MortalitydigHR>1: group with increase in all cause mortality with use of digoxin; S3: third heart sound; SBP: systolic blood pressure.
To validate the contributory role of cluster analysis in defining the natural clusters in which digoxin was not beneficial, we also carried out stepwise Cox proportional multivariate analyses with expanding subgroups. The hazard ratio for the effect of digoxin on mortality in the subgroup of females was 1.2 (p<0.05), females with EF≥40 was 1.5 (p<0.05), females with EF≥40 and SBP at baseline ≥ 140 mm Hg was 1.7 (p<0.05), females with EF≥40 and history of hypertension was 1.8 (p<0.01). Further, by Cox proportional multivariate analyses, the hazard ratio for the effect of digoxin on mortality in the subgroup of patients with hypertension is 1.3, and for EF≥40 is 1.1.
HF admission
Among the 7,756 patients studied, we identified 6,325 patients in HFAdigHR<1 group and 1,431 patients in HFAdigHR-NS group. Baseline variables were compared between treatment and placebo in HFAdigHR<1 group and HFAdigHR-NS group separately, and only body mass index and the presence of third heart sound, in HFAdigHR<1 group and hypertension in HFAdigHR-NS group were different (Table 1B). Kaplan-Meier analysis of digoxin treatment among subjects within HFAdigHR<1 group showed a significant reduction in admissions due to HF (days to HF admission = 1,393 for patients on digoxin vs. 1,234 for patients on placebo, logrank χ2=75, p<0.001) (Figure 1B). In contrast, Kaplan-Meier analysis of digoxin treatment among subjects within HFAdigHR-NS group did not show a reduction in HF admission with the use of digoxin (days to HF admission = 1,443 for patients on digoxin vs. 1,464 for patients on placebo, logrank χ2=0.5, p=0.5) (Figure 1B). HFAdigHR-NS group had a greater proportion of females, higher prevalence of hypertension, higher SBP and EF, and lower proportion of peripheral edema and third heart sound (Table 2B) when compared with HFAdigHR<1 group.
Table 1B.
Baseline characteristics of patients in HFAdigHR<1 group and HFAdigHR-NS group.
| HFAdigHR<1, n=6325 | HFAdigHR-NS, n=1431 | |||||
|---|---|---|---|---|---|---|
| Digoxin (n=3164) | Placebo (n=3161) | p | Digoxin (n=706) | Placebo (n=725) | p | |
| Continuous/ordinal variables (mean±SD) | ||||||
| Age (yrs) | 64±11 | 64±11 | 0.63 | 63±14 | 62±11.5 | 0.93 |
| NYHA class | 2.2±0.7 | 2.2±0.7 | 0.97 | 2.1±0.65 | 2.1±0.64 | 0.69 |
| SBP (mmHg) | 123±18 | 123±17 | 0.43 | 141±17 | 140±18 | 0.40 |
| Heart rate (bpm) | 79±12 | 79±12 | 0.14 | 76±14 | 77±14 | 0.34 |
| BMI | 26.9±5.2 | 27.2±5.2 | 0.01 | 28±5.9 | 29±5.9 | 0.69 |
| Cardiothoracic ratio | 0.5±0.07 | 0.5±0.07 | 0.65 | 0.5±0.07 | 0.5±0.07 | 0.54 |
| EF (%) | 30±12 | 30±12 | 0.92 | 41±13 | 40±13 | 0.08 |
| Creatinine (mg/dl) | 1.3±0.4 | 1.3±0.4 | 0.41 | 1.2±0.36 | 1.3±0.4 | 0.99 |
| Categorical variables (%) | ||||||
| Females | 22 | 22 | 0.69 | 38 | 38 | 0.33 |
| Race (Caucasians) | 87 | 86 | 0.44 | 80 | 81 | 0.50 |
| DM | 28 | 28 | 0.76 | 30 | 32 | 0.53 |
| Hypertension | 41 | 42 | 0.39 | 74 | 69 | 0.04 |
| Ischemic etiology | 70 | 69 | 0.87 | 67 | 66 | 0.78 |
| Limitation - activity | 76 | 76 | 1 | 73 | 75 | 0.31 |
| Peripheral edema | 23 | 23 | 0.77 | 12 | 11 | 0.74 |
| S3 | 29 | 26 | 0.02 | 7 | 6 | 0.98 |
| X-ray congestion | 16 | 16 | 1 | 9 | 8 | 0.30 |
| ACE inhibitor use | 93 | 94 | 0.35 | 92 | 92 | 0.85 |
| Diuretic use | 79 | 80 | 0.53 | 71 | 71 | 0.95 |
| Potassium sparing diuretic use | 7 | 8 | 0.05 | 10 | 10 | 0.93 |
BMI: body mass index; DM: diabetes mellitus; EF: ejection fraction; HFAdigHR<1: group with reduction in heart failure admissions with use of digoxin; HFAdigHR-NS: group with non-significant association of digoxin use with admissions due to heart failure; S3: third heart sound; SBP: systolic blood pressure.
Table 2B.
Baseline variables of HFAdigHR<1 group vs. HFAdigHR-NS group.
| HFAdigHR<1, n=6325 | HFAdigHR-NS, n=1431 | Odds ratio | |Z| | p value | |
|---|---|---|---|---|---|
| Continuous/Ordinal variables (mean±SD) | |||||
| Age (yrs) | 64±11 | 62±12 | 6.1 | <0.001 | |
| NYHA class | 2.2±0.7 | 2.1±0.6 | 8 | <0.001 | |
| SBP (mmHg) | 123±18 | 141±17 | 30.4 | <0.001 | |
| Heart rate (bpm) | 79±12 | 77±14 | 5.9 | <0.001 | |
| BMI | 27±5 | 29±6 | 9.2 | <0.001 | |
| Cardiothoracic ratio | 0.5±0.07 | 0.5±0.07 | 2.3 | 0.02 | |
| EF (%) | 30±12 | 40±13 | 26.6 | <0.001 | |
| Creatinine (mg/dl) | 1.3±0.4 | 1.3±0.4 | 4.7 | <0.001 | |
| Categorical Variables (%) | |||||
| Females | 22 | 37 | 2.1 | <0.001 | |
| Race (Caucasians) | 87 | 81 | 0.6 | <0.001 | |
| DM | 28 | 31 | 1.3 | 0.009 | |
| Hypertension | 42 | 71 | 3.3 | <0.001 | |
| Ischemic etiology | 70 | 66 | 0.8 | 0.02 | |
| Limitation of activity | 76 | 74 | 0.07 | ||
| Peripheral edema | 23 | 12 | 0.4 | <0.001 | |
| S3 | 28 | 6 | 0.2 | <0.001 | |
| X-ray congestion | 16 | 9 | 0.5 | <0.001 | |
| ACE inhibitor use | 94 | 92 | 0.8 | 0.03 | |
| Diuretic use | 80 | 71 | 0.6 | <0.001 | |
| Potassium sparing diuretic use | 7 | 10 | 1.4 | 0.001 | |
| Digoxin use | 50 | 49 | 0.64 | ||
p value of <0.001 was considered highly significant. Odds ratio and Z score are for variables in HFAdigHR-NS group in comparison with HFAdigHR<1 group. Odds ratio <0.5 or >2 and |Z|>10 was considered as a large effect size. Bold variables indicate a highly significant difference with a large effect size. BMI: body mass index; DM: diabetes mellitus; EF: ejection fraction; HFAdigHR<1: group with reduction in heart failure admissions with use of digoxin; HFAdigHR-NS: group with non-significant association of digoxin use with admissions due to heart failure; S3: third heart sound; SBP: systolic blood pressure.
Discussion
In this study, we demonstrated that digoxin treatment was associated with an increased mortality in clusters of patients with higher SBP, heart rate, age and EF, and higher prevalence of hypertension, DM and females. Similarly, there was no reduction in HF hospitalizations with the use of digoxin in clusters of patients with higher SBP and EF and higher prevalence of hypertension and females. We did not identify any clusters of patients in which HF hospitalizations were increased or mortality was reduced.
Hypertension, DM, obesity and female gender are commonly associated with the clinical phenotype of “HF with preserved EF” or diastolic HF. The profile of patients in clusters associated with no benefit in HF hospitalizations or increased mortality with digoxin therapy in our study resembles this typical “phenotype” of a patient with diastolic HF (EF=40% vs. 30% in patients with increased mortality with digoxin and patients with no association of mortality with digoxin use, respectively). Our study supports findings of former studies that digoxin treatment is not associated with a benefit in clinical outcomes in patients with HF with preserved EF (EF>45%). In the ancillary DIG trial (3), HF patients with preserved EF did not have a significant reduction in admissions due to HF, all cause mortality and combined outcome of HF hospitalization or HF mortality with the use of digoxin. Interestingly, in a post hoc analysis of DIG trial data by propensity matching, Meyer et al. (10) reported that digoxin was equally effective in reducing the combined end point of HF hospitalizations, or HF mortality in patients with diastolic HF similar to patients with systolic HF. These findings contradict our findings, the results of the main DIG trial (1) and the ancillary DIG trial (3); in which, digoxin did not reduce all-cause mortality, cause-specific mortality or the combined end-point of heart failure hospitalization and heart failure mortality in HF patients with preserved EF. It should be noted that the study by Meyer et al. (10) did not report independent all-cause mortality, but rather the combined end point of HF hospitalizations and HF mortality. This difference in the clinical outcomes may partially explain the discrepancy between the study by Meyer et al., and our and former DIG trial findings (1,3). Second, Meyer et al. reported that the reduction in HF admissions was significant only in the first 2 years and not beyond. The investigators attributed this to loss of benefit due to potential cross over or higher cumulative digoxin serum concentrations in later years. (10) The follow up duration in our study, the main DIG (1) and the ancillary DIG trial was beyond two years, with an average of 37 months (range 28–58 months), and the analyses were not limited to the first two years as was reported in the study by Meyer et al. (10), which again may explain the discrepancy in the findings. Our study expands upon the existing body of literature by demonstrating, for the first time, that digoxin treatment is not only associated with a lack of benefit, but actually with increased mortality in clusters of patients with higher EF.
The reason for our findings may be unmasking of the escalating risk for patients who have all the characteristics that tend to cluster with each other, i.e. preserved EF, hypertension and DM. According to the current AHA/ACCF guidelines (6), use of digitalis to minimize symptoms of HF may be considered in HF patients with preserved EF. Our findings, however, raise a concern about this recommendation in clusters of patients with preserved EF, especially when accompanied with other clustering characteristics of hypertension, older age and female gender. On the other hand, our study still shows that most of the patients, who do not have these characteristics, may still benefit from the use of digoxin by reduction in admissions due to HF.
Similarly, to our knowledge this is the first study demonstrating increased mortality with digoxin in clusters of patients with higher SBP and/or higher prevalence of hypertension. The original DIG trial (1) and the subsequent reports of the Ancillary DIG trial (3) did not report survival or HF hospitalization outcomes for subgroups of patients with hypertension. The current HF guidelines do not specify high blood pressure as a contraindication to use of digoxin (6), but in clinical practice, digoxin is prescribed less frequently in patients with hypertension (11). Our results support the clinical practice pattern that treatment with digoxin is not beneficial in clusters of patients with higher SBP or history of hypertension.
In our study, clusters with older age were associated with a significantly increased mortality with digoxin treatment. Interestingly, our results also showed that older age was associated with reduced admissions due to HF with digoxin treatment. So far, the only other large scale available data regarding older age and HF admissions with digoxin is an analysis by Rich et al. (12), where no significant association was found between age and the effect of digoxin on admissions due to HF. However, in this analysis, baseline characteristics of the patients were not matched within the subgroups (13). In a sub-group analysis by Ahmed et al (14), in patients who were more than 65 years of age, there was a significant reduction in admissions due to HF and significant reduction in all cause mortality at low serum digoxin concentration, but a non-significant increase in mortality at high serum digoxin concentrations. However, in that study, patients who died within 1 month and patients who did not have digoxin levels were excluded (N=2240). In our study, despite an association with increased mortality, clusters with older patients had a reduction in HF admissions with digoxin therapy. These and former studies suggest a bidirectional opposite effect on mortality and HF hospitalization in elderly with digoxin treatment; digoxin treatment may improve symptoms of HF, but may worsen survival in elderly. We did not see a bidirectional effect in outcomes in other clusters; the clusters of patients with hypertension, females and higher left ventricular EF in whom digoxin was associated with increased mortality, also had no reduction in HF hospitalizations.
Our results indicate that in clusters with females, digoxin treatment was associated with higher mortality and no reduction in HF hospitalizations. These are consistent with findings of former studies. In a previous post hoc analyses of main DIG trial data of patients with systolic HF (2), digoxin therapy was associated with an increased all cause mortality; and a smaller digoxin-associated reduction in admissions due to HF in comparison with men. Our findings strengthen the concept that women do not benefit from digoxin therapy and may be at increased risk for death with such therapy (6).
Finally, although there was no benefit in survival, in our study, digoxin treatment was associated with a reduction in HF hospitalization in “sicker” patients with systolic dysfunction and evidence of congestion. Specifically, in clusters with a higher prevalence of peripheral edema and third heart sound; and lower SBP, and EF, digoxin treatment was associated with significant reduction in HF admissions and was not associated with increased mortality. These findings support the results of the original DIG trial, in which the benefit of digoxin (combined end-points of HF admissions and all cause mortality) appeared to be greater among patients with severe HF disease state, suggested by lower EF (<25%), enlarged heart and advanced NYHA functional class (III/IV) (1). Majority of benefit in this combined end point in the DIG trial was driven from reduction in HF hospitalizations. Thus, our results are in accordance with the results of the main trial and have taken it one step further by identifying low SBP, signs of congestion as a marker for a higher benefit from digoxin in patients with systolic dysfunction.
We believe this new analysis on the only existing large scale randomized clinical trial with digoxin sheds some light into the true and broader phenotype of the HF patients who may or may not benefit from digoxin therapy than what has been described before. We were able to validate the contributory role of cluster analysis by using stepwise Cox proportional multivariate analyses, and demonstrated the escalating risk with expanding subgroups identified by cluster analysis. Further, even though by Cox regression multivariate analyses, independent hazard ratios for the effect of digoxin on mortality in the subgroup of patients with hypertension or for patients with EF≥40 were not significant; by cluster analysis, patients with hypertension or EF≥ 40 were significantly associated with increased mortality. Thus cluster analysis seems to unmask the presence of risk with digoxin in such groups of patients that tend to cluster together. Second, all permutations to create new subgroups containing all possible variations of risk are too numerous and may not be feasible. Third, post-hoc analysis of certain combined subgroups without pre-identified criteria would add bias.
Limitations
This investigation was a post hoc analysis of the DIG trial. Our analyses were limited by covariates collected by trial design, and residual unmeasured confounding factors may exist. Similarly, data on serum digoxin levels was available in less than 20% of patients (n=1485) and thus limits our ability to elaborate on potential harmful effects with higher serum digoxin levels and/or the safety margin of digoxin levels in the elderly population. Our findings can only suggest an association, rather than a causality of no benefit or harm with digoxin treatment in certain subgroups of patients. Further studies may be needed to confirm our findings, especially for particular subsets of patients identified to have no benefit and potential harm with digoxin therapy.
Conclusion
We identified clusters of patients, within the DIG population, who had increased mortality with digoxin treatment. These patients were more likely to be females; with a higher prevalence of hypertension; and higher left ventricular EF and higher SBP. We also identified clusters of patients who had a significant reduction in admissions due to HF but no effect on mortality with digoxin treatment. These patients had lower EF and SBP, higher prevalence of males, third heart sound and peripheral edema. This study strengthens the recommendations against the use of digoxin in the typical HF with preserved EF phenotype, i.e. female patients, with hypertension; but the continued use of digoxin in advanced or sicker HF patients with depressed EF, lower SBP, and signs of congestion or decompensation. Recognition of these characteristics is important for appropriate selection of patients for digoxin therapy and can help improve care in patients with HF.
Acknowledgments
This study is not supported by any grant.
The Digitalis Investigation Group (DIG) study is conducted and supported by the NHLBI in collaboration with the Digitalis Investigation Group (DIG) Investigators. This manuscript was not prepared in collaboration with investigators of the Digitalis Investigation Group (DIG) and does not necessarily reflect the opinions or views of the Digitalis Investigation Group (DIG) or the NHLBI. Dr. Bozkurt is a recipient of Merit Entry Level grant support from Veterans Affairs Medical Research Service (MRS). X.H.T.W. is a W.M. Keck Foundation Distinguished Young Scholar in Medical Research, and is also supported by NIH/NHLBI grants R01-HL089598 and R01HL091947.
The authors of this manuscript have certified that they comply with the Principles of Ethical Publishing in the International Journal of Cardiology (15).
Abbreviations
- DIG
Digitalis Investigation Group
- DM
Diabetes mellitus
- EF
Ejection fraction
- HF
Heart failure
- SBP
Systolic blood pressure
Footnotes
None of the authors have any financial or other relations that could lead to a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.The effect of digoxin on mortality and morbidity in patients with heart failure. The Digitalis Investigation Group. N Engl J Med. 1997;336:525–33. doi: 10.1056/NEJM199702203360801. [DOI] [PubMed] [Google Scholar]
- 2.Rathore SS, Wang Y, Krumholz HM. Sex-based differences in the effect of digoxin for the treatment of heart failure. N Engl J Med. 2002;347:1403–11. doi: 10.1056/NEJMoa021266. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed A, Rich MW, Fleg JL, et al. Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation. 2006;114:397–403. doi: 10.1161/CIRCULATIONAHA.106.628347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rathore SS, Curtis JP, Wang Y, Bristow MR, Krumholz HM. Association of serum digoxin concentration and outcomes in patients with heart failure. JAMA. 2003;289:871–8. doi: 10.1001/jama.289.7.871. [DOI] [PubMed] [Google Scholar]
- 5.Hunt SA American College of Cardiology, American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) J Am Coll Cardiol. 2005;46:e1–82. doi: 10.1016/j.jacc.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 6.Jessup M, Abraham WT, Casey DE, et al. 2009 focused update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:1977–2016. doi: 10.1161/CIRCULATIONAHA.109.192064. [DOI] [PubMed] [Google Scholar]
- 7.Francis GS. The contemporary use of digoxin for the treatment of heart failure. Circ Heart Fail. 2008;1:208–9. doi: 10.1161/CIRCHEARTFAILURE.108.806646. [DOI] [PubMed] [Google Scholar]
- 8.Kohonen T. Self-Organizing Maps. Berlin, Germany: Springer; 2001. [Google Scholar]
- 9.Rationale, design, implementation, and baseline characteristics of patients in the DIG trial: a large, simple, long-term trial to evaluate the effect of digitalis on mortality in heart failure. Control Clin Trials. 1996;17:77–97. doi: 10.1016/0197-2456(95)00065-8. [DOI] [PubMed] [Google Scholar]
- 10.Meyer P, White M, Mujib M, et al. Digoxin and reduction of heart failure hospitalization in chronic systolic and diastolic heart failure. Am J Cardiol. 2008;102:1681–6. doi: 10.1016/j.amjcard.2008.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dhaliwal AS, Bredikis A, Habib G, Carabello BA, Ramasubbu K, Bozkurt B. Digoxin and clinical outcomes in systolic heart failure patients on contemporary background heart failure therapy. Am J Cardiol. 2008;102:1356–60. doi: 10.1016/j.amjcard.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Rich MW, McSherry F, Williford WO, Yusuf S Digitalis Investigation Group. Effect of age on mortality, hospitalizations and response to digoxin in patients with heart failure: the DIG study. J Am Coll Cardiol. 2001;38:806–13. doi: 10.1016/s0735-1097(01)01442-5. [DOI] [PubMed] [Google Scholar]
- 13.Boehmke FJ, Morey DS, Shannon M. Selection bias and continuous-time duration models: Consequences and a proposed solution. American Journal of Political Science. 2006;50:192–207. [Google Scholar]
- 14.Ahmed A. Digoxin and reduction in mortality and hospitalization in geriatric heart failure: importance of low doses and low serum concentrations. J Gerontol A Biol Sci Med Sci. 2007;62:323–9. doi: 10.1093/gerona/62.3.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coats AJ. Ethical authorship and publishing. Int J Cardiol. 2009;131:149–50. doi: 10.1016/j.ijcard.2008.11.048. [DOI] [PubMed] [Google Scholar]