Abstract
AIM: To determine the prevalence of steatosis and steatohepatitis in a series of autopsies in Northwestern Greece.
METHODS: Liver biopsy material from a total of 600 autopsies performed over a period of 2 years (2006-2008) to define the cause of death was subjected to histological examination. Patient demographic data were also collected. Tissue sections were stained with different dyes for the evaluation of liver architecture, degree of fibrosis and other pathological conditions when necessary.
RESULTS: Satisfactory tissue samples for histological evaluation were available in 498 cases (341 male, 157 female) with a mean age of 64.51 ± 17.78 years. In total, 144 (28.9%) had normal liver histology, 156 (31.3%) had evidence of steatosis, and 198 (39.8%) had typical histological findings of steatohepatitis. The most common causes of death were ischemic heart disease with or without myocardial infarction (43.4%), and traffic accidents (13.4%).
CONCLUSION: A high prevalence of steatosis and steatohepatitis was detected in postmortem biopsies from Northwestern Greece. Since both diseases can have serious clinical consequences, they should be considered as an important threat to the health of the general population in Greece.
Keywords: Fatty liver, Non-alcoholic liver disease, Steatosis, Steatohepatitis, Autopsy
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD), the accumulation of fat within liver cells in individuals who deny a significant history of alcohol ingestion, is emerging as the most frequent liver disease in developed countries[1,2]. The diagnosis of NAFLD and non-alcoholic steatohepatitis (NASH) is based on histological findings of either fat alone, fat plus inflammation, fat plus hepatocyte injury (ballooning degeneration), or fat with fibrosis and cirrhosis[3]. The significance of these histological categories rests on the fact that both the prevalence and clinical outcome vary by histological category[4].
NAFLD is commonly associated with severe obesity, defined as body mass index (BMI) > 35 kg/m2, with 74%-90% of liver biopsies showing fatty change[5,6]. NASH, first named by Ludwig et al[7], is probably a less aggressive condition than alcoholic hepatitis, but nevertheless might progress through necro-inflammatory change and early fibrosis to cirrhosis[8,9]. In contrast, NAFLD without necro-inflammatory change is generally a benign condition[10,11].
There are few published data on the frequency of NASH and NAFLD in Greece, but without biopsies[12]. The present study aimed to determine the prevalence of these diseases in a series of autopsy material from Northwestern Greece.
MATERIALS AND METHODS
Study protocol
The aim of the present study was to estimate the prevalence of steatosis and steatohepatitis in postmortem material from Northwestern Greece. For this purpose, a number of liver specimens from people who died suddenly or in a traffic accident and had undergone autopsy to define the cause of death, were investigated.
The survey took place at the regional University Hospital of Ioannina, from 15 March 2006 until 20 December 2008. The collaborating centers were the Department of Internal Medicine, the Laboratory of Pathology and the Department of Forensic Medicine and Toxicology. The study protocol was approved by the Hospital Ethical Committee.
Autopsy material from 600 people (391 men and 209 women) aged 3-94 years was investigated. All autopsies were forensic cases, being performed in those with unnatural death, such as sudden death and accidents (especially traffic accidents). No academic cases were included.
Demographic information, history of alcohol use and previous hepatic and non-hepatic chronic diseases, such as diabetes mellitus, and use of medication, were obtained from the first-degree relatives of the cases. Gross appearance of the liver was also recorded. Sampling was performed by the same physician.
Cases with a history of liver disease of any type and those with autolysed liver samples were excluded. Wedge biopsies (2 cm × 2 cm × 2 cm) from the right and left lobes and one biopsy of the same size from deeper areas of the liver parenchyma were obtained in each case. Any visually grossly abnormal areas were also sampled.
Isolation of liver specimens and histological assessment
Liver tissue sections from the necrotomic material were fixed in 40 g/L neutral formaldehyde for 24 h. After that, the tissues were dehydrated, embedded in paraffin, cut at 4 μm, and stained with hematoxylin-eosin for light microscopy.
For histochemical staining, additional 4-μm thick tissue sections were cut from paraffin blocks and were stained with silver reticulin and Masson’s trichrome methods for the evaluation of liver architecture and the degree of fibrosis, when necessary. In addition, Perl's Prussian blue staining was performed to evaluate iron load based on a grading system of 0-4, as previously described[13].
Immunohistochemical study for the hepatitis B virus surface and core antigens was performed on formalin-fixed, paraffin-embedded liver tissue sections by the labeled streptavidin-avidin-biotin method, using appropriate antibodies (anti-HbsAg monoclonal mouse antibody, clone 3E7; DAKO, Germany; anti-HbcAg polyclonal rabbit antibody; DAKO). Immunohistochemical cytoplasmic and nuclear staining of hepatocytes was shown as HbsAg and HbcAg positivity, respectively.
Each biopsy was scored on a scale for steatosis, injury/inflammation and fibrosis. The grading and staging of steatohepatitis was based on criteria developed by Brunt et al[14]. Most specimens contained 12-24 portal tracts.
The two histopathologists involved in this study agreed on terms, definitions and the histological criteria of the pathologic lesions. The liver sections were examined under an Olympus optical microscope and the histopathologists were blind to the patients’ personal history. All positive findings were reevaluated for grading and staging by both histopathologists. In cases of diagnostic discrepancy, the result was reported according to the consensus of a joint slide review session. Histological findings were recorded in a standard form.
Statistical analysis
Data are presented as mean ± SD, unless otherwise stated. One-way ANOVA or ANOVA based on ranks, followed by multiple pairwise comparisons, was used for multigroup comparisons. Correlations between variables were determined with the use of the f factor. All statistical tests were performed with the use of the Statistica software, version 6.0. P < 0.05 was considered significant unless otherwise noted.
An overall statistical analysis was performed at first. After that, the cases were divided into subgroups based on sex, and comparison was performed in correlation with the degree of steatosis and steatohepatitis. The cases were also divided into four age subgroups: < 45 years (65 cases, 13%, age group a); 45-60 years (97 cases, 19.4%, age group b); 60-75 years (187 cases, 37.6%, age group c); and > 75 years (149 cases, 30%, age group d). Statistical analysis based on the histological findings was performed in each age subgroup. Finally, the cases were divided in to two subgroups according to the cause of death: in the first subgroup the cause of death was ischemic heart disease with or without myocardial infarction, and in the second, all other vascular diseases. Further correlations with liver histology, age and sex were also performed.
RESULTS
During the study period, 600 cases were assessed. One hundred and two cases were excluded because of moderate to severe autolysis in liver tissue, positive immunohistochemical findings for hepatitis B surface antigen (HBsAg) and hepatitis B core antigen (HBcAg) or a history of known chronic liver disease. Thus, 498 cases were evaluable and included 341 men and 157 women with a mean age of 64.51 ± 17.78 years. Most of the cases (255) were residents of Ioannina, the largest town in Northwestern Greece.
The most common causes of death were: ischemic heart disease with or without myocardial infarction (47.6%), traffic accidents (13.4%), pneumonic embolism (8.2%), cerebrovascular incidents (4.2%), rupture of aortic aneurysm and trauma (3.2%), neoplasm (2.8%), and others (21%). Table 1 presents a detailed description of the causes of death in our study population.
Table 1.
Detailed causes of death in the population study
| Cause of death | n (%) | |
| Ischemic heart disease and/or myocardial infarction | 237 (47.59) | |
| Traffic accidents | 67 (13.45) | |
| Pneumonic embolism | 41 (8.23) | |
| Cerebrovascular incidents | 21 (4.2) | |
| Trauma | 16 (3.2) | |
| Rupture of aortic aneurysm | 16 (3.2) | |
| Neoplasm | 14 (2.8) | |
| Cerebrovascular trauma | 12 (2.4) | |
| Drowning | 12 (2.4) | |
| Heroin overdose and other toxic agents | 11 (2.2) | |
| Hanging | 7 (1.4) | |
| Cirrhosis | 6 (1.2) | |
| Severe burns | 5 (1.0) | |
| Thrombosis of the mesentery with peritonitis | 4 (0.8) | |
| Sepsis | 3 (0.6) | |
| Lower gastrointestinal bleeding | 3 (0.6) | |
| Upper gastrointestinal bleeding | 2 (0.4) | |
| Inhalation of CO | 2 (0.4) | |
| Subdural hematoma | 2 (0.4) | |
| Endocarditis | 2 (0.4) | |
| Lobular pneumonia | 1 (0.2) | |
| Other (infections, electrocution, etc.) | 14 (2.8) | |
From the 498 cases, 144 (28.9%) had normal liver histology, whilst 156 (31.3%) had evidence of steatosis, and 198 (39.8%) had histological findings typical of steatohepatitis. In the subgroup with steatosis, 112 (71.8%) had steatosis < 33%, 28 (18%) had steatosis between 33 and 66%, and 16 (10%) had steatosis of > 66%. In the steatohepatitis subgroup, 113 (57%) cases were classified as grade 1, 61 (30.8%) as grade 2, and 24 (12.1%) as grade 3. Staging was categorized as stages 1, 2, 3 and 4, respectively. Thus, 69 (35%) were stage 1, 69 (35%) stage 2, 36 (18%) stage 3, and 24 (12) stage 4. Correlations of the grades and the stages of the 198 cases with steatohepatitis are depicted in Table 2. As in other types of chronic hepatitis, the grade and stage of the disease might be disparate, as they are meant to reflect different aspects of liver injury. The degrees of steatosis are presented.
Table 2.
Correlation of grade and stage in patients with steatohepatitis
| Grade |
Stage |
Totals | ||||
| 0 | 1 | 2 | 3 | 4 | ||
| Mild (I) | 0 | 55 | 44 | 13 | 1 | 113 |
| Moderate (II) | 0 | 13 | 21 | 14 | 13 | 61 |
| Severe (III) | 0 | 1 | 4 | 9 | 10 | 24 |
| Totals | 0 | 69 | 69 | 36 | 24 | 198 |
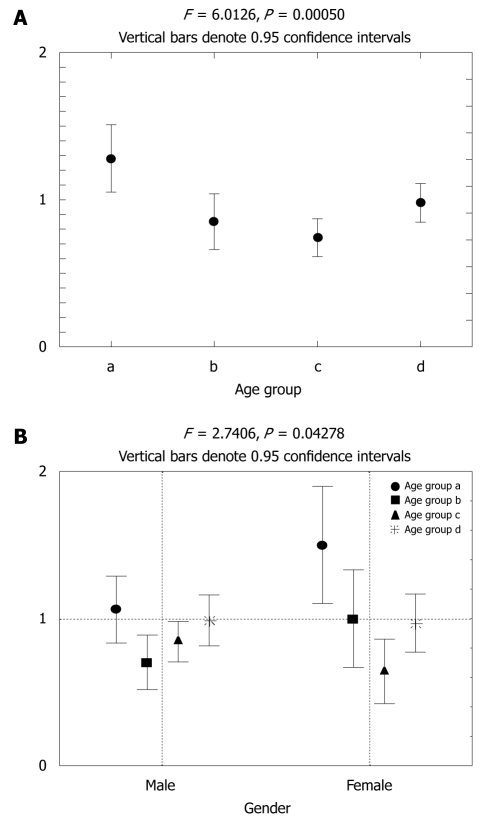
The analysis of steatosis, steatohepatitis and normal liver tissues in the aging groups was statistically significant (P = 0.0005, f = 6, Figure 1). The same analysis in correlation with sex was not significant (P = 0.148). Overall analysis of the age groups and sex in correlation with steatosis, steatohepatitis and normal liver tissues showed borderline significance (P = 0.043, f = 3, Figure 1). Table 3 presents the number of subjects by sex and age group.
Figure 1.
Correlations of age subgroups in different subjects. A: Correlation of age subgroups (a, b, c and d) in subjects with steatohepatitis (0) and steatosis (1), and normal subjects (2). Mean values for each group are presented. The four age subgroups were defined as follows: < 45 years (group a), 45-60 years (group b), 60-75 years (group c), and > 75 years (group d); B: Correlation of sex and age in subjects with steatohepatitis (2) and steatosis (1), and in normal subjects (0). Data are shown for male and female subjects separately, according to age group.
Table 3.
Number of subjects in every age group according to sex
| Age groups | a | b | c | d | Totals |
| Male | 49 | 74 | 134 | 84 | 341 |
| Female | 16 | 23 | 53 | 65 | 157 |
| Total | 65 | 97 | 187 | 149 | 498 |
a: < 45 years; b: 45-60 years; c: 60-75 years; d: > 75 years.
History of diabetes mellitus was found in 18 cases with steatosis and in 30 cases with steatohepatitis. Mild iron loading (1+ to 2+) was detected in 41 cases (23 men, 18 women), which accounted for 8.2% of the study population. From these, 39 cases had also steatohepatitis and therefore only two cases of steatosis were detected. Furthermore, analyses based on the age subgroups revealed mild iron loading (1+ to 2+) in eight cases between 45 and 60 years, in 18 cases between 60 and 75, and in 15 cases > 75 years.
Finally, from the 236 ischemic heart disease deaths with or without myocardial infarction, 47 (20%) had normal liver histology, 90 (38%) had steatosis, and 99 (42%) had histological findings typical of steatohepatitis. In the same subgroup, only 11 cases had mild iron loading.
DISCUSSION
The present study demonstrated that steatosis and steatohepatitis are emerging as common silent liver diseases in Northwestern Greece. The true incidence and prevalence of these diseases in different populations is largely unknown[15], even if it is believed that they are the most common liver diseases in the general population[2,16,17]. This might be explained partly because liver histology is required as the gold standard for precise diagnosis of these conditions, and the relatively invasive procedure of liver biopsy is still not considered essential for the management of NAFLD by many physicians. In addition, most of the reports on the prevalence rates of NAFLD are based on ultrasonographic studies and/or the presence of elevated serum levels of aminotransferases, in the absence of any other known liver disease or significant alcohol consumption[2,18].
In clinical practice, diagnostic liver biopsy is performed only for highly selected patients. For this reason, the reported rates that are based on liver biopsies cannot reflect the true prevalence of NAFLD and NASH in the general population[19,20]. In addition, histological lesions of NASH are unevenly distributed throughout the liver parenchyma; therefore, sampling errors of liver biopsies can result in misdiagnosis and staging inaccuracies[21]. Furthermore, NASH and alcoholic steatohepatitis can share common histological findings[22,23].
Autopsies, performed for those who have passed away for reasons other than liver diseases, are certainly better sources for the determination of a more reliable prevalence for NAFLD and NASH[24]. The particular characteristics of forensic autopsies are the relatively young age of the subjects and their usually better general health before death. Among our cases, male sex was predominant; most of the subjects had no history of chronic diseases, and in > 80%, the causes of death were acute events such as cardiovascular diseases, traffic accidents and trauma. To the best of our knowledge, this is the first report concerning liver diseases based on an autopsy series in Greece.
Obesity is a major clinical problem in Greece[25]. Unfortunately, we were not able to measure BMI in the study population. As a result, no correlations of steatosis and steatohepatitis with BMI could be performed. In addition, although 10 patients had positive immunohistochemical findings for the HBsAg and HBcAg, serological viral markers for hepatitis B and hepatitis C virus infection were not performed in the present study. However, the prevalence of both infections is low in Greece[26-28].
In none of our cases was the use of medication that induced or predisposed to the progression of NASH[29]. The higher prevalence of NAFLD and NASH in patients with diabetes mellitus has been well documented before[30-32] and is in accordance with our findings. Silent cirrhosis was found in only six of our patients, which indicates a low prevalence of this condition in Northwestern Greece, in comparison with other autopsy series[24,33]. The correlation of cirrhosis with NAFLD and NASH is one of the most controversial issues. Although there is substantial evidence that NASH might lead to cirrhosis in about 20% of cases, and is the most common etiology for cryptogenic cirrhosis[34], well-designed, prospective long-term studies for determination of outcome in patients with NAFLD are lacking[2,3]. However, it seems that older age, obesity and the presence of diabetes mellitus are factors that predispose towards progression of NASH to cirrhosis[35-37]. In particular, the aggressive form of NAFLD is best based on the pathological diagnosis of steatonecrosis with Mallory hyaline and fibrosis[38,39]. The clinical implications of this alarming prevalence of NAFLD and NASH are derived from the fact that these liver conditions may progress to end-stage liver disease and cancer[40,41].
Mild iron loading was detected in 41 cases in our study population. It is clear that, in our cases with steatohepatitis, the role of increased iron stores in the development of fibrosis seemed to be of less importance. The role of lipogenesis and fatty acid oxidation in the development of NAFLD and NASH has been well established[42]. In particular, the complex progression of NAFLD is related to metabolic abnormalities associated with massive steatosis, insulin resistance and reductions in fatty acid oxidation[43-45]. NASH is attributed to tumor necrosis factor-α, free fatty acid toxicity, toxicity caused by dicarboxylic acids, a decrease in mitochondrial and peroxisomal β-oxidation, generation of reactive oxygen species, lipid peroxidation and many other events that lead to apoptosis and inflammation[46,47].
The reported prevalence of steatosis in our study is in accordance with other studies[24]. However, the reported prevalence of steatohepatitis in this Greek population is much higher in comparison with other population studies[48-51]. Although results from this autopsy study cannot be extrapolated to the general healthy population, the reason for such a high rate could possibly be attributed to the decreased physical activity and the alterations in dietary habits in the Greek population over recent decades.
In conclusion, it seems that steatosis and steatohepatitis are very common liver diseases among postmortem material in Northwestern Greece. Since both diseases can have serious clinical consequences, they should be considered as an important threat to the health of the general population in Greece. Further studies to confirm this prevalence and assess the etiology and natural history of these lesions in the general healthy Greek population, in combination with possible therapeutic strategies, are therefore mandatory.
COMMENTS
Background
The incidence of steatosis and steatohepatitis is currently rising faster than any other liver disease in the western world, although the cause of this increase is largely unknown. These diseases progress from necro-inflammatory change and early fibrosis to cirrhosis and liver cancer. Both diseases can result in end-stage liver disease. Liver biopsy remains the gold standard for diagnosis and treatment. The present study aimed to determine the prevalence of steatosis and steatohepatitis in a series of autopsies in Northwestern Greece.
Research frontiers
Many predisposing factors for the development of non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH) have been proposed. Age seemed to be an important one in our population study, whereas the role of sex remains to be investigated. In addition, further studies are important to define the role of genetic factors in both diseases.
Innovations and breakthroughs
Many reports have highlighted the evolution of steatosis and steatohepatitis in liver fibrosis and carcinogenesis. This is believed to be the first study in Greece to report the prevalence of steatosis and steatohepatitis, based on liver histology in the general population. Among our cases, male sex was predominant, most of the subjects had no history of chronic diseases (reported healthy subjects), and in > 80% of the cases, the causes of death were acute events such as cardiovascular diseases, traffic accidents and trauma.
Applications
By understanding the rising prevalence of NAFLD and NASH, this study could represent a future strategy for early therapeutic intervention in the treatment of patients with steatosis and steatohepatitis. Screening of the general population and detecting the possible risk factors is also advisable.
Terminology
Tissue sections were stained with different dyes for the evaluation of liver architecture, degree of fibrosis and other pathological conditions when necessary. Simple steatosis of the liver was staged as follows: < 33%, 33%-66%, > 66%. NASH was diagnosed after excluding other causes of liver inflammation.
Peer review
This paper is interesting and well written. Finding a steatohepatitis prevalence of about 40% is important news in Greece and could have implications throughout Europe.
Footnotes
Peer reviewer: Mark D Gorrell, PhD, Professor, Centenary Institute of Cancer Medicine and Cell Biology, Locked bag No. 6, Newtown, NSW 2042, Australia
S- Editor Wang YR L- Editor Kerr C E- Editor Ma WH
References
- 1.Ong JP, Younossi ZM. Epidemiology and natural history of NAFLD and NASH. Clin Liver Dis. 2007;11:1–16, vii. doi: 10.1016/j.cld.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Bellentani S, Marino M. Epidemiology and natural history of non-alcoholic fatty liver disease (NAFLD) Ann Hepatol. 2009;8 Suppl 1:S4–S8. [PubMed] [Google Scholar]
- 3.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 4.Youssef WI, McCullough AJ. Steatohepatitis in obese individuals. Best Pract Res Clin Gastroenterol. 2002;16:733–747. doi: 10.1053/bega.2002.0334. [DOI] [PubMed] [Google Scholar]
- 5.Luyckx FH, Desaive C, Thiry A, Dewé W, Scheen AJ, Gielen JE, Lefèbvre PJ. Liver abnormalities in severely obese subjects: effect of drastic weight loss after gastroplasty. Int J Obes Relat Metab Disord. 1998;22:222–226. doi: 10.1038/sj.ijo.0800571. [DOI] [PubMed] [Google Scholar]
- 6.Clain DJ, Lefkowitch JH. Fatty liver disease in morbid obesity. Gastroenterol Clin North Am. 1987;16:239–252. [PubMed] [Google Scholar]
- 7.Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:434–438. [PubMed] [Google Scholar]
- 8.Sheth SG, Gordon FD, Chopra S. Nonalcoholic steatohepatitis. Ann Intern Med. 1997;126:137–145. doi: 10.7326/0003-4819-126-2-199701150-00008. [DOI] [PubMed] [Google Scholar]
- 9.Powell EE, Cooksley WG, Hanson R, Searle J, Halliday JW, Powell LW. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years. Hepatology. 1990;11:74–80. doi: 10.1002/hep.1840110114. [DOI] [PubMed] [Google Scholar]
- 10.Teli MR, James OF, Burt AD, Bennett MK, Day CP. The natural history of nonalcoholic fatty liver: a follow-up study. Hepatology. 1995;22:1714–1719. [PubMed] [Google Scholar]
- 11.Preiss D, Sattar N. Non-alcoholic fatty liver disease: an overview of prevalence, diagnosis, pathogenesis and treatment considerations. Clin Sci (Lond) 2008;115:141–150. doi: 10.1042/CS20070402. [DOI] [PubMed] [Google Scholar]
- 12.Papatheodoridis GV, Goulis J, Christodoulou D, Manolakopoulos S, Raptopoulou M, Andrioti E, Alexandropoulos N, Savvidou S, Papachristou A, Zervou E, et al. High prevalence of elevated liver enzymes in blood donors: associations with male gender and central adiposity. Eur J Gastroenterol Hepatol. 2007;19:281–287. doi: 10.1097/MEG.0b013e328011438b. [DOI] [PubMed] [Google Scholar]
- 13.Di Bisceglie AM, Axiotis CA, Hoofnagle JH, Bacon BR. Measurements of iron status in patients with chronic hepatitis. Gastroenterology. 1992;102:2108–2113. doi: 10.1016/0016-5085(92)90339-z. [DOI] [PubMed] [Google Scholar]
- 14.Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–2474. doi: 10.1111/j.1572-0241.1999.01377.x. [DOI] [PubMed] [Google Scholar]
- 15.Angulo P. GI epidemiology: nonalcoholic fatty liver disease. Aliment Pharmacol Ther. 2007;25:883–889. doi: 10.1111/j.1365-2036.2007.03246.x. [DOI] [PubMed] [Google Scholar]
- 16.Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology. 2003;37:1202–1219. doi: 10.1053/jhep.2003.50193. [DOI] [PubMed] [Google Scholar]
- 17.Choudhury J, Sanyal AJ. Clinical aspects of fatty liver disease. Semin Liver Dis. 2004;24:349–362. doi: 10.1055/s-2004-860864. [DOI] [PubMed] [Google Scholar]
- 18.Pendino GM, Mariano A, Surace P, Caserta CA, Fiorillo MT, Amante A, Bruno S, Mangano C, Polito I, Amato F, et al. Prevalence and etiology of altered liver tests: a population-based survey in a Mediterranean town. Hepatology. 2005;41:1151–1159. doi: 10.1002/hep.20689. [DOI] [PubMed] [Google Scholar]
- 19.Hultcrantz R, Glaumann H, Lindberg G, Nilsson LH. Liver investigation in 149 asymptomatic patients with moderately elevated activities of serum aminotransferases. Scand J Gastroenterol. 1986;21:109–113. doi: 10.3109/00365528609034632. [DOI] [PubMed] [Google Scholar]
- 20.Propst A, Propst T, Judmaier G, Vogel W. Prognosis in nonalcoholic steatohepatitis. Gastroenterology. 1995;108:1607. doi: 10.1016/0016-5085(95)90724-6. [DOI] [PubMed] [Google Scholar]
- 21.Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, Grimaldi A, Capron F, Poynard T. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128:1898–1906. doi: 10.1053/j.gastro.2005.03.084. [DOI] [PubMed] [Google Scholar]
- 22.Lee RG. Nonalcoholic steatohepatitis: a study of 49 patients. Hum Pathol. 1989;20:594–598. doi: 10.1016/0046-8177(89)90249-9. [DOI] [PubMed] [Google Scholar]
- 23.Reid AE. Nonalcoholic steatohepatitis. Gastroenterology. 2001;121:710–723. doi: 10.1053/gast.2001.27126. [DOI] [PubMed] [Google Scholar]
- 24.Sotoudehmanesh R, Sotoudeh M, Ali-Asgari A, Abedi-Ardakani B, Tavangar SM, Khakinejad A, Sadeghi Z, Malekzadeh R. Silent liver diseases in autopsies from forensic medicine of Tehran. Arch Iran Med. 2006;9:324–328. [PubMed] [Google Scholar]
- 25.Papandreou C, Mourad TA, Jildeh C, Abdeen Z, Philalithis A, Tzanakis N. Obesity in Mediterranean region (1997-2007): a systematic review. Obes Rev. 2008;9:389–399. doi: 10.1111/j.1467-789X.2007.00466.x. [DOI] [PubMed] [Google Scholar]
- 26.Gogos CA, Fouka KP, Nikiforidis G, Avgeridis K, Sakellaropoulos G, Bassaris H, Maniatis A, Skoutelis A. Prevalence of hepatitis B and C virus infection in the general population and selected groups in South-Western Greece. Eur J Epidemiol. 2003;18:551–557. doi: 10.1023/a:1024698715741. [DOI] [PubMed] [Google Scholar]
- 27.German V, Giannakos G, Kopterides P, Liaskonis K, Falagas ME. Serologic indices of hepatitis B virus infection in military recruits in Greece (2004-2005) BMC Infect Dis. 2006;6:163. doi: 10.1186/1471-2334-6-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dalekos GN, Zervou E, Merkouropoulos MH, Tsianos EV. Prevalence of hepatitis B and C viruses infection in chronic alcoholics with or without liver disease in Ioannina, Greece: low incidence of HCV infection. Eur J Epidemiol. 1996;12:21–25. doi: 10.1007/BF00144423. [DOI] [PubMed] [Google Scholar]
- 29.Farrell GC, Liddle C. Drugs and the liver updated, 2002. Semin Liver Dis. 2002;22:109–113. [PubMed] [Google Scholar]
- 30.Itoh S, Yougel T, Kawagoe K. Comparison between nonalcoholic steatohepatitis and alcoholic hepatitis. Am J Gastroenterol. 1987;82:650–654. [PubMed] [Google Scholar]
- 31.Diehl AM, Goodman Z, Ishak KG. Alcohollike liver disease in nonalcoholics. A clinical and histologic comparison with alcohol-induced liver injury. Gastroenterology. 1988;95:1056–1062. [PubMed] [Google Scholar]
- 32.Angulo P, Lindor KD. Management of nonalcoholic steatohepatitis. In: Krawwitt ED, editor. Medical management of liver disease. New York, NY: Marcel Dekker, Inc; 1999. pp. 367–379. [Google Scholar]
- 33.Bethke BA, Schubert GE. Primary hepatic cancer and liver cirrhosis. Autopsy study covering fifty years. Hepatogastroenterology. 1984;31:211–214. [PubMed] [Google Scholar]
- 34.Caldwell SH, Oelsner DH, Iezzoni JC, Hespenheide EE, Battle EH, Driscoll CJ. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology. 1999;29:664–669. doi: 10.1002/hep.510290347. [DOI] [PubMed] [Google Scholar]
- 35.Angulo P, Keach JC, Batts KP, Lindor KD. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology. 1999;30:1356–1362. doi: 10.1002/hep.510300604. [DOI] [PubMed] [Google Scholar]
- 36.Dixon JB, Bhathal PS, O’Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology. 2001;121:91–100. doi: 10.1053/gast.2001.25540. [DOI] [PubMed] [Google Scholar]
- 37.Jaskiewicz K, Rzepko R, Sledzinski Z. Fibrogenesis in fatty liver associated with obesity and diabetes mellitus type 2. Dig Dis Sci. 2008;53:785–788. doi: 10.1007/s10620-007-9942-x. [DOI] [PubMed] [Google Scholar]
- 38.Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–1419. doi: 10.1016/s0016-5085(99)70506-8. [DOI] [PubMed] [Google Scholar]
- 39.Harrison SA, Torgerson S, Hayashi PH. The natural history of nonalcoholic fatty liver disease: a clinical histopathological study. Am J Gastroenterol. 2003;98:2042–2047. doi: 10.1111/j.1572-0241.2003.07659.x. [DOI] [PubMed] [Google Scholar]
- 40.Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 41.Ekstedt M, Franzén LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, Kechagias S. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–873. doi: 10.1002/hep.21327. [DOI] [PubMed] [Google Scholar]
- 42.Reddy JK, Rao MS. Lipid metabolism and liver inflammation. II. Fatty liver disease and fatty acid oxidation. Am J Physiol Gastrointest Liver Physiol. 2006;290:G852–G858. doi: 10.1152/ajpgi.00521.2005. [DOI] [PubMed] [Google Scholar]
- 43.Reddy JK. Nonalcoholic steatosis and steatohepatitis. III. Peroxisomal beta-oxidation, PPAR alpha, and steatohepatitis. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1333–G1339. doi: 10.1152/ajpgi.2001.281.6.G1333. [DOI] [PubMed] [Google Scholar]
- 44.Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, Grundy SM, Hobbs HH. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–1395. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 45.Schreuder TC, Verwer BJ, van Nieuwkerk CM, Mulder CJ. Nonalcoholic fatty liver disease: an overview of current insights in pathogenesis, diagnosis and treatment. World J Gastroenterol. 2008;14:2474–2486. doi: 10.3748/wjg.14.2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Day CP, James OF. Steatohepatitis: a tale of two “hits”? Gastroenterology. 1998;114:842–845. doi: 10.1016/s0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 47.Begriche K, Igoudjil A, Pessayre D, Fromenty B. Mitochondrial dysfunction in NASH: causes, consequences and possible means to prevent it. Mitochondrion. 2006;6:1–28. doi: 10.1016/j.mito.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 48.Hilden M, Christoffersen P, Juhl E, Dalgaard JB. Liver histology in a ‘normal’ population--examinations of 503 consecutive fatal traffic casualties. Scand J Gastroenterol. 1977;12:593–597. doi: 10.3109/00365527709181339. [DOI] [PubMed] [Google Scholar]
- 49.Ono M, Saibara T. Clinical features of nonalcoholic steatohepatitis in Japan: Evidence from the literature. J Gastroenterol. 2006;41:725–732. doi: 10.1007/s00535-006-1876-0. [DOI] [PubMed] [Google Scholar]
- 50.Amarapurkar A, Ghansar T. Fatty liver: experience from western India. Ann Hepatol. 2007;6:37–40. [PubMed] [Google Scholar]
- 51.Wanless IR, Lentz JS. Fatty liver hepatitis (steatohepatitis) and obesity: an autopsy study with analysis of risk factors. Hepatology. 1990;12:1106–1110. doi: 10.1002/hep.1840120505. [DOI] [PubMed] [Google Scholar]