Abstract
Localized malignant pleural mesothelioma (LMPM) is a rare occurrence, and gastrointestinal intra-luminal metastases have not previously been reported. Herein, we report a patient with LMPM who presented with a local recurrence 10 mo after initial en bloc surgical resection. Abdominal computed tomography was performed for intractable, vague abdominal pain with episodic vomiting, which showed a “target sign” over the left lower quadrant. Laparotomy revealed several intra-luminal metastatic tumors in the small intestine and colon and a segmental resection of metastatic lesions was performed. Unfortunately, the patient died of sepsis despite successful surgical intervention. Though local recurrence is more frequent in LMPM, the possibility of distant metastasis should not be ignored in patients with non-specific abdominal pain.
Keywords: Localized malignant pleural mesothelioma, Intussusception, Distant metastasis
INTRODUCTION
Localized malignant pleural mesothelioma (LMPM) is a rare occurrence, and only a few cases have been reported in the literature[1,2]. Local recurrence is not uncommon; however, distant metastasis with gastrointestinal involvement, especially bowel intussusception (BI), has not been previously reported. Herein, we report a patient with LMPM who experienced local recurrence and metastases to the bowel with multiple BI. The patient died of sepsis despite successful relief of intestinal obstruction.
CASE REPORT
A 57-year-old male complained of right chest pain and presented to our department with a large, localized chest wall tumor in April 2008. He underwent en bloc chest wall resection with an adequate tumor free margin and the pathological examination revealed LMPM, sarcomatoid type. A full course of adjuvant chemotherapy with cisplatin and pemetrexed was administered; however, local recurrence was diagnosed 10 mo after the initial surgical intervention. At the time of diagnosis, he complained of dizziness, poor appetite, and vague abdominal pain with episodic vomiting. His stool was negative for occult blood and laboratory studies revealed normochromic normocytic anemia (Hgb, 5.9 g/dL). Abdominal computed tomography (CT) revealed a “target sign” in the left lower quadrant (Figure 1).
Figure 1.
Abdominal computed tomography discloses a typical “target sign” over the small intestine (arrow).
An emergent laparotomy was performed and 3 intussusceptions with concomitant leading points of intra-luminal, polypoid tumors were found in the small intestine (Figure 2). No peritoneal seeding or extra-luminal invasion was discovered. After a detailed examination of the whole bowel, 7 tumors were found in the jejunum, ascending colon, and transverse colon (Figure 3). Segmental resection of small bowel with end-to-end anastomosis and radical right hemicolectomy with ileocolostomy, and regional lymph node sampling were performed.
Figure 2.

Intraoperative photo showing intussusceptions in the small intestine (arrows).
Figure 3.

Surgical specimen reveals metastatic localized malignant pleural mesothelioma in the small intestine (arrows) and colon (arrow heads).
Grossly, the surgical specimen consisted of jejunum, ileum, ascending colon and descending colon, 98 cm in length, with 7 polypoid, intra-luminal tumors. Four tumors were in the small bowel, and the others were in the ascending and descending colon. The tumors measured from 2.5 to 8.0 cm in diameter, and the largest, located in the small bowel, was 8.0 cm × 4.0 cm × 3.0 cm in size. When cut, all demonstrated a pinkish-white cut surface without necrosis or hemorrhage.
Microscopically, the 7 tumors were composed of sheets of epithelioid cells and spindle cells which had vesicular nuclei with prominent nucleoli, mixed with inflammatory cells (Figure 4). Mucosal and submucosal involvement was noted. Moreover, tumor metastasis was present in the regional lymph nodes. Immunohistochemical studies showed the tumor cells were negative for calretinin, thyroid transcription factor-1, and cytokeratin 20, and positive for vimentin and cytokeratin. The results were identical to those of the LMPM from the right chest wall.
Figure 4.
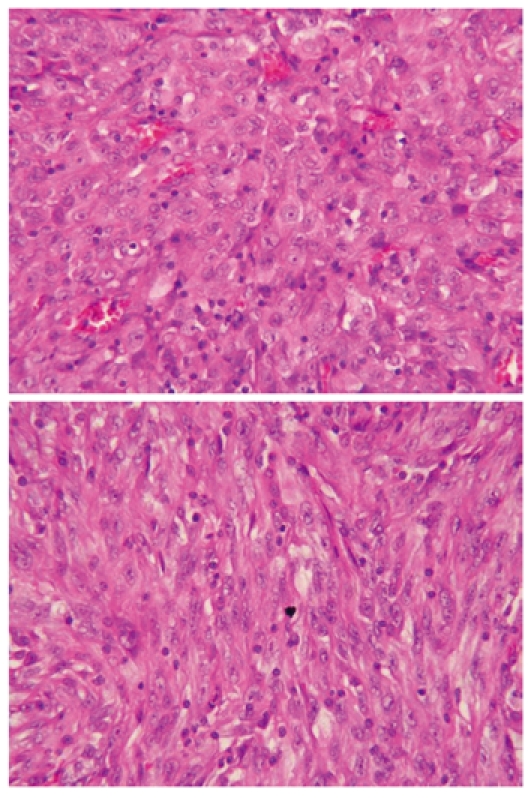
Microscopic examination reveals the tumor to consist of sheets of spindle to epithelioid cells with abundant eosinophilic cytoplasm and vesicular nuclear chromatin with prominent nucleoli (HE stain, × 400).
The patient resumed enteral feeding on the 13th postoperative day. Unfortunately, the patient died of fungemia 32 d after the operation.
DISCUSSION
BI is rare in adults, accounting for 5% of all cases with intussusceptions and almost 5% of bowel obstructions[3]. Secondary BI usually results from organic lesions, such as polyps, inflammatory bowel disease, postoperative adhesions or neoplasms, and manifests with a single leading point. It is reported that malignant tumors are the most common causes of BI in adult patients, accounting for 47% of cases[3]. Nevertheless, distant metastases with multiple BIs are extremely rare, and only few case reports are found in the literature; these have been reported to be associated with melanoma, renal cell carcinoma, or lung cancer[4-6].
LMPMs are extremely rare solitary tumors, and identical to diffuse malignant pleural mesotheliomas microscopically and immunohistochemically. When an extensive review of published English-language literature was carried out, there were found to be a total of 53 LMPMs derived from parietal pleura[1,2,7-9]. Among these reported cases, LMPMs usually presented with local recurrence near prior surgical sites (16 cases, 30%), and there were 2 cases with contralateral recurrence during follow-up. Distant metastasis was less common compared with local recurrence, and only 8 cases were found (2 with brain metastases, 2 with diffuse dissemination, 2 with vertebral metastases, 1 with skin metastasis, and 1 with mediastinal metastasis). No case of intestinal intra-luminal metastases from LMPM has been previously reported. To the best of our knowledge, this is the first case report of multiple BIs from metastatic LMPM despite an initial en bloc chest wall resection and adjuvant chemotherapy.
In the case reported herein, the patient had the symptoms of vague abdominal pain and vomiting, and normocytic anemia. Generally, BIs from distant metastasis or malignancy have diverse manifestations. Most patients present with non-specific symptoms consistent with bowel obstruction, such as nausea, emesis, abdominal pain, melena, or weight loss[3]. However, Goh et al[10] have stated that anemia and colon intussusception are the predictive determinants for adult BIs resulting from malignancy. Moreover, abdominal CT is the most useful imaging modality and carries an acceptable diagnostic accuracy for adult BIs[3,11]. Early application of CT scanning will facilitate definitive diagnosis and prompt treatment.
Compared with pediatric intussusception, hydrostatic reduction is not mandatory, and aggressive surgical treatment is the gold standard for adult intussusception, though long-term survival remains unsatisfactory in patients with BI from metastases. Complete surgical resection of viable tumors is worthwhile in a select group of patients for the purpose of nutritional support from enteral feeding and metastasectomy with tumor eradication.
In conclusion, this case highlights two important issues. Firstly, clinicians should take gastrointestinal involvement, even malignancy-related intussusception, into consideration when treating patients with a past history of malignancy who are experiencing frequent abdominal pain and have unexplainable anemia. Secondly, though distant metastasis is infrequent compared with local recurrence in patients with LMPM, the possibility should be considered in patients with non-specific symptoms.
Footnotes
Peer reviewer: Matthew James Schuchert, MD, FACS, Assistant Professor of Surgery, Heart, Lung and Esophageal Surgery Institute, University of Pittsburgh Medical Center, Shadyside Medical Building, 5200 Centre Avenue, Suite 715, Pittsburgh, PA 15232, United States
S- Editor Tian L L- Editor Logan S E- Editor Lin YP
References
- 1.Allen TC, Cagle PT, Churg AM, Colby TV, Gibbs AR, Hammar SP, Corson JM, Grimes MM, Ordonez NG, Roggli V, et al. Localized malignant mesothelioma. Am J Surg Pathol. 2005;29:866–873. doi: 10.1097/01.pas.0000165529.78945.dc. [DOI] [PubMed] [Google Scholar]
- 2.Nakas A, Martin-Ucar AE, Edwards JG, Waller DA. Localised malignant pleural mesothelioma: a separate clinical entity requiring aggressive local surgery. Eur J Cardiothorac Surg. 2008;33:303–306. doi: 10.1016/j.ejcts.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 3.Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134–138. doi: 10.1097/00000658-199708000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang YJ, Wu MH, Lin MT. Multiple small-bowel intussusceptions caused by metastatic malignant melanoma. Am J Surg. 2008;196:e1–e2. doi: 10.1016/j.amjsurg.2007.05.062. [DOI] [PubMed] [Google Scholar]
- 5.Eo WK, Kim GY, Choi SI. A case of multiple intussusceptions in the small intestine caused by metastatic renal cell carcinoma. Cancer Res Treat. 2008;40:97–99. doi: 10.4143/crt.2008.40.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goh BK, Yeo AW, Koong HN, Ooi LL, Wong WK. Laparotomy for acute complications of gastrointestinal metastases from lung cancer: is it a worthwhile or futile effort? Surg Today. 2007;37:370–374. doi: 10.1007/s00595-006-3419-y. [DOI] [PubMed] [Google Scholar]
- 7.Khan AM, Tlemcani K, Shanmugam N, Y D, Keller S, Berman AR. A localized pleural based mass with intense uptake on positron emission tomography scan. Chest. 2007;131:294–299. doi: 10.1378/chest.06-0655. [DOI] [PubMed] [Google Scholar]
- 8.Takahashi H, Harada M, Maehara S, Kato H. Localized malignant mesothelioma of the pleura. Ann Thorac Cardiovasc Surg. 2007;13:262–266. [PubMed] [Google Scholar]
- 9.Tanzi S, Tiseo M, Internullo E, Cacciani G, Capra R, Carbognani P, Rusca M, Rindi G, Ardizzoni A. Localized malignant pleural mesothelioma: report of two cases. J Thorac Oncol. 2009;4:1038–1040. doi: 10.1097/JTO.0b013e3181a8c874. [DOI] [PubMed] [Google Scholar]
- 10.Goh BK, Quah HM, Chow PK, Tan KY, Tay KH, Eu KW, Ooi LL, Wong WK. Predictive factors of malignancy in adults with intussusception. World J Surg. 2006;30:1300–1304. doi: 10.1007/s00268-005-0491-1. [DOI] [PubMed] [Google Scholar]
- 11.Chang CC, Chen YY, Chen YF, Lin CN, Yen HH, Lou HY. Adult intussusception in Asians: clinical presentations, diagnosis, and treatment. J Gastroenterol Hepatol. 2007;22:1767–1771. doi: 10.1111/j.1440-1746.2007.04907.x. [DOI] [PubMed] [Google Scholar]



