Abstract
Poor adherence to treatment can have negative effects on outcomes and healthcare cost. However, little is known about the barriers to treatment adherence within physiotherapy. The aim of this systematic review was to identify barriers to treatment adherence in patients typically managed in musculoskeletal physiotherapy outpatient settings and suggest strategies for reducing their impact. The review included twenty high quality studies investigating barriers to treatment adherence in musculoskeletal populations. There was strong evidence that poor treatment adherence was associated with low levels of physical activity at baseline or in previous weeks, low in-treatment adherence with exercise, low self-efficacy, depression, anxiety, helplessness, poor social support/activity, greater perceived number of barriers to exercise and increased pain levels during exercise. Strategies to overcome these barriers and improve adherence are considered. We found limited evidence for many factors and further high quality research is required to investigate the predictive validity of these potential barriers. Much of the available research has focussed on patient factors and additional research is required to investigate the barriers introduced by health professionals or health organisations, since these factors are also likely to influence patient adherence with treatment.
Keywords: Adherence, Barriers, Treatment, Musculoskeletal
1. Introduction
Adherence with treatment is an important factor which can influence the outcome of that treatment (Hayden et al., 2005). Adherent patients may have better treatment outcomes than non-adherent patients (Vermeire et al., 2001; WHO, 2003). Poor adherence to treatment has been identified across many healthcare disciplines including physiotherapy (Vasey, 1990; Friedrich et al., 1998; Campbell et al., 2001). The extent of non-adherence with physiotherapy treatment is unclear. One study found that 14% of physiotherapy patients did not return for follow-up outpatient appointments (Vasey, 1990). Another suggested that non-adherence with treatment and exercise performance could be as high as 70% (Sluijs et al., 1993). Poor adherence has implications on treatment cost and effectiveness.
Adherence has been defined as: “the extent to which a person's behaviour… corresponds with agreed recommendations from a healthcare provider” (WHO, 2003). Within physiotherapy, the concept of adherence is multi-dimensional (Kolt et al., 2007) and could relate to attendance at appointments, following advice, undertaking prescribed exercises, frequency of undertaking prescribed exercise, correct performance of exercises or doing more or less than advised. Many factors related to the patient, the healthcare provider and the healthcare organisation are thought to influence patient adherence with treatment (Miller et al., 1997). Within physiotherapy it is not clear which factors act as barriers to adherence.
Identification of barriers may help clinicians identify patients at risk of non-adherence and suggest methods to reduce the impact of those barriers thereby maximising adherence. The aim of this review is twofold. Firstly, to identify important barriers to adhering with musculoskeletal outpatient treatment. Secondly, to discuss strategies that may help clinicians to overcome these barriers.
2. Methods
2.1. Literature search
The following databases were searched from their inception to December 2006: AMED, CINAHL, EMBASE, MEDLINE, PUBMED, PSYCINFO, SPORTDISCUSS, the Cochrane Central Register of Controlled Trials and PEDro. The following keywords were used: ‘barriers’, ‘prognostic’, ‘predictor’, ‘adherence’, ‘compliance’, ‘concordance’, ‘therapy’, ‘physical’, ‘physiotherapy’, ‘osteopath’, ‘chiropractor’, ‘sports’, ‘pain’, ‘joint’, ‘muscle’, ‘musculoskeletal’, and ‘outpatients’. The references of primary studies identified were scanned to identify further relevant citations. Internet searches of Google and Google Scholar were conducted.
2.2. Study selection
Studies were included if they: (1) were RCTs, prospective studies, CCTs or cross-sectional surveys which were peer-reviewed and published in the English language, (2) investigated patients with mechanical musculoskeletal dysfunctions, (3) related to treatment or therapeutic exercise administered by physical or exercise therapists and (4) identified barriers or predictors of adherence.
Studies were excluded if they investigated non-attendance at initial appointments, asymptomatic populations, in-patient populations, life threatening conditions/reduced mortality, non-musculoskeletal conditions or systemic musculoskeletal conditions being managed primarily by drug therapy or a multidisciplinary team approach.
A three phase screening strategy was used to identify relevant articles. Firstly, one investigator (KJ) identified potentially relevant studies by scanning their titles and abstracts. Secondly, remaining citations were examined independently by two investigators (KJ & SMc) and agreement reached on articles which did not meet the selection criteria. Finally, both investigators (KJ & SMc) independently reviewed the full text of remaining articles against the selection criteria and consensus was reached for their inclusion in the review. In the event of disagreement, a third reviewer (JKM) arbitrated.
2.3. Quality assessment of studies
The quality tool used in this review was modified from tools used in previous systematic reviews (Borghouts et al., 1998; Scholten-Peeters et al., 2003). Since adherence was the focus of this study, “loss to follow-up” was eliminated as an item of assessment from the quality tool. Therefore the quality assessment tool consisted of 13 criteria (see Table 1). The standard of information required to meet each criterion was set a-priori. Criterion meeting the quality standard were given a score of 1, while those not meeting the standard were given a zero score. Studies scoring ≥7 were considered ‘high quality’, while those scoring <7 were considered ‘low quality’ (Borghouts et al., 1998; Scholten-Peeters et al., 2003). Multiple publications derived from a single cohort were awarded one quality score based on the information available from all the publications (Scholten-Peeters et al., 2003). Two reviewers (KJ & SMc) independently assessed and scored the included studies. Where there was disagreement a third reviewer (EG) made the final decision.
Table 1.
Quality Assessment Tool (adapted from Borghouts et al., 1998; Scholten-Peeters et al., 2003).
| Criteria | Score |
|---|---|
| Study population | |
| (A) Description of source population | +/−/? |
| (B) Description of inclusion and exclusion criteria | +/−/? |
| Study design | |
| (C) Prospective study design | +/−/? |
| (D) Study size ≥ 300 | +/−/? |
| Drop-outs | |
| (E) Information completers versus loss to follow-up/drop-outs | +/−/? |
| Prognostic factors | |
| (F) Description of potential prognostic factors | +/−/? |
| (G) Standardised or valid measurements | +/−/? |
| (H) Data presentation of most important prognostic factors | +/−/? |
| Outcome measures | |
| (I) Relevant outcome measures | +/−/? |
| (J) Standardised or valid measurements | +/−/? |
| (K) Data presentation of most important outcome measures | +/−/? |
| Analysis and data presentation | |
| (L) Appropriate univariate crude estimates | +/−/? |
| (M) Appropriate multivariate analysis techniques | +/−/? |
[+ = positive (design/conduct adequate, scores 1 point); — = negative (design or conduct inadequate, scores 0 points); ? = unclear (item insufficiently described, scores 0 points)].
2.4. Data extraction and synthesis
A standardised template was used to extract data regarding the study population, study design, predictor variables, outcome measures, study quality, data analysis and results.
Inter-observer agreement of quality assessment was determined by calculating percentage agreement and a kappa co-efficient (Viera and Garrett, 2005). Information extracted is presented in table format to highlight methodological quality, similarities and differences between the studies. Narrative summaries of the results are provided. Qualitative conclusions are based on levels of evidence (see Table 2) which have been used in previous reviews (Karjalainen et al., 2001; Verhagen et al., 2004).
Table 2.
Levels of evidence.
| Strong | Consistent findings in at least 2 high quality cohorts/RCTs |
| Moderate | Findings from 1 high quality cohort/RCT and consistent findings from 1 or more low quality cohorts/RCTs |
| Limited | Findings from 1 high quality cohort/RCT or consistent findings from 1 or more low quality cohorts/RCTs |
| Conflicting | Inconsistent findings regardless of quality |
| No Evidence | No studies found |
Where possible, the significance of factors affecting adherence and the levels of evidence were derived from multivariate analyses. Significant associations of p < 0.05 or relevant estimated odds ratios or risk ratios were used; these were defined as meaningful when ≤0.5 or ≥2.0 (Ariens et al., 2000).
3. Results
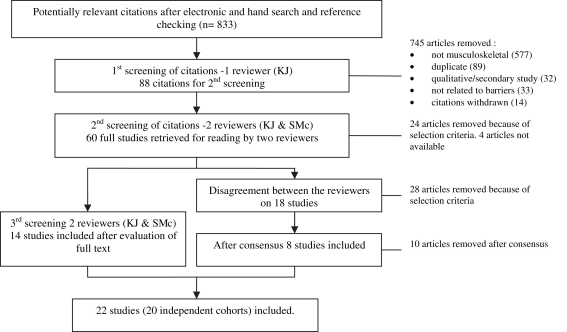
Fig. 1 shows the process of study selection. Initial searching identified 833 citations. Following the first screening, 745 articles were excluded and 88 citations were retained for the second screening. Using inclusion and exclusion criteria a further 24 articles were excluded. Of the remaining 64 articles, four were unavailable. Initial disagreement over the selection of 18 papers occurred. Following discussions, six of these were included, with two further papers referred to the third reviewer (EG) for arbitration. In total, 22 articles reporting on 20 independent cohort studies were selected for the review.
Fig. 1.
Flow diagram of selection process of studies.
3.1. Methodological quality
The reviewers scored 286 items and disagreed on 29 items (10%). The overall inter-observer agreement (κ = 0.72) represents substantial agreement between the reviewers (Viera and Garrett, 2005). Consensus was not achieved on 2 items. In each case the third reviewer (EG) made the final decision. The results of the quality assessment are shown in Table 3. Articles relating to the same cohort, e.g. Dobkin et al. (2005, 2006) and Brewer et al. (2000, 2003), had their quality assessment scores combined to prevent bias in assessing the levels of evidence. The quality scores ranged from six to 11 indicating that all but one study were of high quality. The most common methodological shortfalls related to description of the source population (item A), the study size (item D) and failing to present univariate analysis (item M).
Table 3.
Results of methodological assessment.
| Study | A | B | C | D | E | F | G | H | I | J | K | L | M | Quality Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Schoo et al. (2005) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 11 |
| Alexandre et al. (2002) | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 10 |
| Dobkin cohorta | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 10 |
| Fekete et al. (2006) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 10 |
| Alewijnse et al. (2003) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 10 |
| Stenstrom et al. (1997) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 10 |
| Brewer cohortb | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 |
| Castenada et al. (1998) | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 |
| Funch and Gale (1986) | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 |
| Kenny (2000) | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 9 |
| Laubach et al. (1996) | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 |
| Rejeski et al. (1997) | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 9 |
| Shaw et al. (1994) | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 |
| Sluijs et al. (1993) | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 |
| Milne et al. (2005) | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 8 |
| Oliver and Cronan (2002) | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 8 |
| Chen et al. (1999) | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 8 |
| Taylor and May (1996) | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 8 |
| Minor and Brown (1993) | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 7 |
| Kolt and McEvoy (2003) | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 6 |
3.2. Study characteristics
The main characteristics of the study populations, barriers and outcome measures for each cohort are outlined in the Supplementary electronic file. Of the 20 studies, seven recruited from osteoarthritis/rheumatoid arthritis populations attending physiotherapy (Stenstrom et al., 1997; Schoo et al., 2005), part of a health organisation (Shaw et al., 1994; Castenada et al., 1998), post-surgical patients (Fekete et al., 2006) or exercise trials (Minor and Brown, 1993; Rejeski et al., 1997); four studies investigating lower back pain recruited from general outpatient populations (Sluijs et al., 1993; Alexandre et al., 2002; Kolt and McEvoy, 2003) or a tertiary rehabilitation agency (Kenny, 2000); three studies recruited from a sporting population (Laubach et al., 1996; Taylor and May, 1996; Milne et al., 2005); two studies investigated fibromyalgia patients (Oliver and Cronan, 2002; Dobkin et al., 2006); one study investigated an anterior cruciate ligament post-operative population (Brewer et al., 2003); one study recruited females suffering from urinary incontinence (Alewijnse et al., 2003); one study recruited patients with temporo-mandibular joint pain (Funch and Gale, 1986) and one study recruited patients from an upper limb rehabilitation centre (Chen et al., 1999). All studies investigated at least one aspect of treatment adherence including attendance at appointments, adherence with home exercises and in-clinic adherence. Only one study (Stenstrom et al., 1997) did not report multivariate analysis.
3.3. Barriers that predict poor treatment adherence
Table 4 presents a summary of the barriers to treatment adherence. There was strong evidence that low levels of physical activity at baseline (4 trials,728 participants) or in previous weeks (2 trials, 883 participants), low self-efficacy (6 trials, 1296 participants), depression (4 trials, 1367 participants), anxiety (2 trials, 159 participants), helplessness (2 trials, 792 participants), poor social support or activity (6 trials, 2286 participants), greater perceived number of barriers to exercise (3 trials, 857 participants) and increased pain levels during exercise (2 trials, 159 participants) were barriers to treatment adherence. There was also strong evidence that low in-treatment adherence with exercise (3 trials, 287 participants) was a barrier to longer term exercise adherence. There was conflicting evidence that age and greater pain at baseline were barriers to treatment adherence. Limited evidence was found for a range of other variables with one good quality study supporting each of them.
Table 4.
Physical, psychological, socio-demographic and clinical barriers to adhering with treatment.
| Barrier to adherence | Level of evidence | Studies | Comments |
|---|---|---|---|
| Physical barriers | |||
| Low level of physical activity or aerobic capacity at baseline | strong | Schoo et al. (2005) | Older subjects with OA who were physically active at baseline were 14 times more likely to adhere to a home exercise programme |
| Stenstrom et al. (1997) | Undertaking regular range of motion exercise prior to the study predicted adherence with a one year home exercise programme in subjects with inflammatory rheumatoid disease. | ||
| Minor and Brown (1993) | In subjects with OA/RA, low aerobic capacity at baseline predicted negative exercise behaviour 3 months and 18 months after participating in an exercise class. | ||
| Rejeski et al. (1997) | In subjects with OA knee, lower baseline VO2PEAK predicted poor attendance at an aerobic class and less time spent undertaking aerobic exercise. | ||
| Low in-treatment adherence with exercise | Strong | Schoo et al. (2005) | Subjects with OA who reported adhering well to a prescribed home exercise in the first 4 weeks of the programme were 20 times more likely to report adhering with exercise in the final 4 weeks. |
| Dobkin cohort | In women with fibromyalgia, in-treatment adherence with stretching and aerobic exercise predicted future adherence with the stretching and aerobic programme. | ||
| Alewijnse et al. (2003) | In women with urinary incontinence, short term adherence with a pelvic floor muscle exercise programme predicted long term adherence with the programme at 1-year follow-up. | ||
| Low levels of exercise adherence in previous weeks | Strong | Rejeski et al. (1997) | In subjects with OA knee, exercise behaviour 3 and 9 months post exercise intervention predicted follow-up exercise behaviour at 9 and 16 months respectively. |
| Oliver and Cronan (2002) | In women with fibromyalgia, engaging in regular exercise at previous time points predicted engaging in regular exercise at future time points. | ||
| Recreational athlete (v competitive) | Milne et al. (2005) | Competitive athletes were predicted to be more adherent with exercise rehabilitation than recreational athletes. | |
| Psychological barriers | |||
| Low self-efficacy (for exercise, tasks and coping) | Strong | Stenstrom et al. (1997) | In subjects with inflammatory rheumatoid disease, high self-efficacy for exercise predicted compliance with a one year home exercise programme |
| Shaw et al. (1994) | In subjects with OA, lower efficacy for exercise predicted poor attendance at an education group about appropriate use of the healthcare system. | ||
| Milne et al. (2005) | Greater task self-efficacy predicted adherence with rehabilitation; greater coping self-efficacy predicted frequency of exercising in an athletic population. | ||
| Taylor and May (1996) | In an athletic population patient's self-efficacy predicted physiotherapist's estimate of the patient's compliance with prescribed modalities and rest | ||
| Oliver and Cronan (2002) | In women with fibromyalgia, greater exercise self-efficacy predicted continued engagement in exercise behaviour at future time points. | ||
| Chen et al. (1999) | In subjects attending an upper limb rehabilitation centre, greater self-efficacy contributed to greater adherence with a home exercise programme. | ||
| High level of depression at baseline | Strong | Shaw et al. (1994) | In subjects with OA, very high levels and very low levels of depression predicted poor attendance at a social support and education group. |
| Minor and Brown, (1993) | In subjects with OA/RA, less depression at baseline predicted exercise maintenance 3 months after participating in an exercise programme. | ||
| Oliver and Cronan, (2002) | In women with fibromyalgia, low levels of depression predicted subjects who exercised regularly at baseline or who started doing regular exercise throughout the 18 month follow-up period. | ||
| Rejeski et al. (1997) | In subjects with OA knee, higher levels of depression predicted reduced attendance at a 12 week exercise programme. | ||
| No change or worse depression compared with baseline | Minor and Brown (1993) | In subjects with OA/RA, improvements in depression from baseline predicted participation in regular exercise 3 months, 9 months and 18 months after participating in a 3 month exercise class. | |
| Anxiety/stress at baseline | strong | Minor and Brown (1993) | In subjects with OA/RA, higher levels of anxiety at baseline predicted poor exercise maintenance at 3 months and 6 months after participating in a 3 month exercise class. |
| Dobkin cohort | In women with fibromyalgia, high levels of stress or increases of stress during a 12 week stretching programme predicted poor maintenance of that programme | ||
| High degree of helplessness | strong | Castenada et al. (1998) | Women with OA who registered low helplessness scores were predicted to exercise more than those with high helplessness scores |
| Sluijs et al. (1993) | In subjects with musculoskeletal pain (mainly LBP), subjects with a greater feeling of helplessness were predicted to be non-adherent with a home exercise programme prescribed as part of physical therapy rehabilitation. | ||
| Low extroversion scores | Castenada et al. (1998) | Women with OA who registered high extroversion scores were predicted to participate in exercise compared with those who registered low scores. | |
| Low quality of well being (QWB) score | Castenada et al. (1998) | In women with OA, high QWB score predicted participation in exercise compared to those with low score. | |
| Lower sense of personal control | Laubach et al. (1996) | In injured athletes, a greater sense of personal control predicted subjects designated by the PT/AT as being adherent with rehabilitation | |
| Lower level of stability | Laubach et al. (1996) | In injured athletes, a greater sense of stability predicted subjects designated by the PT/AT as being adherent with rehabilitation | |
| High internal health locus of control | Chen et al. (1999) | In subjects attending an upper limb rehabilitation centre, internal health locus of control was inversely related to adherence with a home exercise programme. | |
| Low self motivation | Brewer et al. (2000, 2003) | For older patients undergoing ACL reconstruction, lower self motivation contributed to decreased adherence with a home exercise programme | |
| Socio-demographic barriers | |||
| Age | Conflicting | Castenada et al. (1998) | In women with OA, those who were older (i.e. closer to 90 years) tended to exercise less than their younger counterparts (i.e. closer to 60 years) |
| Shaw et al. (1994) | In subjects with OA (age range 60–87 years), the oldest and the youngest were predicted to be poor attendees in an education group about the appropriate use of the health care system. | ||
| Dobkin cohort | In women with fibromyalgia (mean age 49.2 (8.7) years), older women were predicted to have reduced participation in aerobic exercise. They were also more likely to reduce their participation with aerobic exercise programme at a faster rate than their younger counterparts | ||
| Brewer cohort | Younger patients with poor athletic identity were less likely to adhere to treatment than those with positive athletic identity. Older patients with lower social support or motivation were less likely to adhere with home treatment. Age range not reported | ||
| Oliver and Cronan (2002) | In women with fibromyalgia, younger subjects were predicted to engage with exercise behaviour. Age range not reported | ||
| Poor social or family support for activity | Strong | Funch and Gale (1986) | In subjects with chronic TMJ pain, social factors (i.e. family attitudes and general attitudes) predicted completion of a behavioural therapy programme. It was not clear what specific attitudes were helpful and which hindered completion. |
| Shaw et al. (1994) | In subjects with OA, restricted social activity predicted poor attendance at a social support and education group. In addition having a small informational support network predicted poor attendance at a social support group. | ||
| Rejeski et al. (1997) | In subjects with OA knee, poor social support predicted poor attendance with aerobic and resistance exercise programme conducted over 3 months. | ||
| Oliver and Cronan (2002) | In women with fibromyalgia, having a larger social, support network predicted subjetcs who exercised regularly at baseline or who started doing regular exercise throughout the 18 month follow-up period. | ||
| Minor and Brown (1993) | In subjects with OA/RA, having the support of friends for exercise positively predicted exercise behaviour 9 months after participating in an exercise class. | ||
| Sluijs et al. (1993) | In subjects with musculoskeletal pain (mainly LBP), lack of positive feedback from a physical therapist predicted non-adherence with a home exercise programme prescribed as part of physical therapy rehabilitation. | ||
| Fekete et al. (2006) | Subjects whose spouses used more positive control adhered less with treatment when spouses also provided high levels of problematic support, but adhered more when spouses provided low levels of problematic support | ||
| Being unmarried | Stenstrom et al. (1997) | In subjects with inflammatory rheumatoid disease, being unmarried predicted compliance with a one year home exercise programme | |
| Ethnicity | Rejeski et al. (1997) | In subjects with OA knee, ethnicity predicted attendance at a resistance training programme and continued resistance training at 9 months follow-up. It was not made clear which ethnics groups were more or less likely to adhere with exercise. | |
| Greater number of barriers to exercise | Strong | Alexandre et al. (2002) | In subjects with LBP, those who could foresee difficulties with the proposed treatment plan were 8 times less likely to adhere with treatment than those patients who could foresee no difficulties |
| Sluijs et al. (1993) | In subjects with musculoskeletal pain (mainly LBP), the barriers patients perceived and encountered (i.e. time, convenience, costs, forgetting, etc) predicted non-adherence with a home exercise programme prescribed during physical therapy rehabilitation. | ||
| Dobkin cohort | In women with fibromyalgia, a greater number of barriers faced during a 12 week exercise programme predicted a significant decrease in post-treatment participation with exercise. | ||
| Patients pursuing compensation | Kolt and McEvoy (2003) | In an LBP cohort, compensable subjects were estimated by the therapist to be less adherent with clinic based rehabilitation activities than non-compensable counterparts. | |
| No sex education at school | Alewijnse et al. (2003) | In subjects with urinary incontinence, women who had received sex education at school were more likely to adhere to a pelvic floor exercise programme in the long term than those who had received no sex education at school. | |
| Being employed | Oliver and Cronan (2002) | In women with fibromyalgia, unemployment at baseline significantly predicted subjects who engaged with exercise behaviour in the first 3 months | |
| Lower educational level (high school or lower) | Oliver and Cronan (2002) | In women with fibromyalgia, lower educational standard significantly predicted subjects who maintained exercise behaviour subsequent to participation in an exercise class. | |
| Clinical barriers | |||
| Presence of co-morbidity | Alexandre et al. (2002) | In subjects with LBP, presence of other medical illnesses predicted poorer adherence with treatment compared with no co-morbidity. | |
| Greater perception of the severity of injury | Taylor and May (1996) | In an athletic population, the subject's perception of the greater severity of condition predicted the physiotherapists reduced estimate of patient compliance with prescribed modalities and rest. | |
| Greater pain at baseline | Conflicting | Dobkin cohort | In women with fibromyalgia, more lower body pain at baseline predicted less adherence with a stretching programme over time. However more upper body pain at baseline predicted greater adherence with an aerobic programme. |
| Rejeski et al. (1997) | In subjects with OA knee, greater levels of baseline pain predicted reduced time spent undertaking aerobic exercise at 3 months follow-up. | ||
| Worsening of pain during exercise | Strong | Minor and Brown (1993) | In subjects with OA/RA, improvements in pain following participation in an exercise class positively predicted exercise behaviour 18 months later. |
| Dobkin cohort | In women with fibromyalgia, increases in upper body pain during treatment predicted worse maintenance of aerobic exercise in the 3 months following treatment. | ||
| Fatigue | Dobkin cohort | In women with fibromyalgia, high levels of baseline fatigue predicted lower average time stretching, and performing aerobic exercise and lower average metabolic output during a 12 week exercise programme. | |
| Having a diagnosis of joint pathology | Kenny (2000) | In a sample of workers with a variety of injuries, those subjects with a diagnosis of joint pathology were less likely to complete a supervised physical activity programme. | |
| Longer treatment duration | Alexandre et al. (2002) | In subjects with LBP, treatment duration of 5–6 weeks predicted poor adherence with LBP treatment compared with treatment duration 2–3 weeks. | |
| First time injury | Milne et al. (2005) | In an athletic population, those with first time injury were less likely to adhere with treatment than those who had reported 3 or more injuries. | |
| Low perceived level of susceptibility | Taylor and May (1996) | In an athletic population, perceived susceptibility predicted patients estimated adherence with rest. | |
| Greater BMI | Rejeski et al. (1997) | In subjects with OA knee, greater BMI predicted poorer attendance in an aerobic exercise class and less time performing aerobic exercise. | |
| Greater mobility | Shaw et al. (1994) | In subjects with OA, having a greater level of mobility predicted poorer attendance at an education group. | |
| Fewer weekly episodes of incontinence | Alewijnse et al. (2003) | In women with urinary incontinence, subjects with frequent weekly wet episodes before and after therapy were more likely to have high adherence levels to a pelvic floor exercise programme than women with fewer wet episodes. | |
Note: OA = Osteoarthritis, BMI = Body Mass Index, VO2peak = maximal oxygen uptake, RA = Rheumatoid arthritis, PT/AT = Physical therapist/athletic trainer, ACL = anterior cruciate ligament, QWB = quality of well being, TMJ = Tempeoromandibular joint, LBP = Low back pain.
4. Discussion
This systematic review summarised the results from 20 high quality studies and found strong evidence that low levels of physical activity at baseline or in previous weeks, low in-treatment adherence with exercise, low self-efficacy, depression, anxiety, helplessness, poor social support or activity, greater perceived number of barriers to exercise and increased pain levels during exercise are barriers to treatment adherence. There was conflicting evidence regarding age and pain at baseline. Many other variables had limited evidence of being barriers to adherence.
The results of this review are in line with others which have found that non-adherent individuals were likely to have lower levels of prior activity, lower exercise self-efficacy, greater number of barriers and low levels of social support (Martin and Sinden, 2001; Jackson et al., 2005). These reviews vary from our own in that psychological variables such as anxiety, stress and helplessness did not emerge as predictive. In the review by Martin and Sinden (2001) few studies investigated whether psychological variables predicted adherence of non-clinical populations of older adults to exercise intervention. In the review by Jackson et al. (2005) there was conflicting evidence for depression and anxiety in patients attending Cardiopulmonary Rehabilitation (CPR). One reason for this could be that these traits are more likely to be present in women, who are less likely to be referred to CPR. Therefore these symptoms may be less likely to emerge as predictors of non-adherence in CPR (Benz Scott et al., 2002).
4.1. Strengths and limitations of this review
This review was conducted in accordance with guidelines from the Centre for Reviews & Dissemination (CRD, 2001), however the possibility of publication bias cannot be excluded (Altman, 1991). Unpublished studies and studies from lesser known databases or published in languages other than English may have been missed. Our review considered a range of musculoskeletal conditions and study populations. Motivation to adhere with treatment and therefore the barriers may vary between different pathology types and populations (Shaw et al., 2005). We have not attempted to analyse these differences.
4.2. Strengths and limitations of reviewed studies
Whilst all studies included in this review were rated as high quality, some limitations were apparent. The studies had sample sizes ranging from n = 34 (Laubach et al., 1996) to n = 695 (Sluijs et al., 1993) with only five (25%) studies exceeding 300 subjects. Whilst there are no universally agreed methods of calculating sample sizes for multivariate analysis, smaller studies with large numbers of predictive variables may allow less confidence in the findings (Tabachnick and Fidell, 2001). Some studies included in this review may be subject to this limitation.
Many potential predictors have not been investigated by the studies in our review. For example, low socioeconomic status (SES) emerged as a predictor of non-adherence with CPR (Jackson et al., 2005) and may warrant further investigation in populations with musculoskeletal disorders. In addition, much of the research has focussed on patient factors and little research has investigated the barriers introduced by health professionals or health organisations (Miller et al., 1997). Further research to investigate potential barriers such as SES, health professional factors and health organisation factors would be appropriate.
The most commonly used measures of adherence were attendance at appointments, adherence with home programmes and in-clinic adherence. Whilst attendance at appointments is standardised it provides no information about patient attitude and behaviour towards rehabilitation e.g. adherence with home exercise programmes or within clinic adherence (Kolt et al., 2007). Patient self-reports using paper diaries were the most common measure of adherence with home programmes. However, poor real time compliance with diary completion and recall accuracy may lead to data of questionable validity (Stone et al., 2003). It is possible that the use of electronic diaries with compliance enhancing features may improve the quality and accuracy of data collected (Broderick and Stone, 2006; Green et al., 2006). The most common measure of in-clinic adherence was the therapist-rated Sports Injury Rehabilitation Adherence Scale (SIRAS). However patients and practitioners may disagree on the level of patient adherence (Donovan, 1995; Carr, 2001) and this variation between patient self-rating and therapist-rating of patient adherence leaves scope for considerable inaccuracy (Kolt and McEvoy, 2003). The use of therapist-rated adherence measures in conjunction with exercise diaries to corroborate patient self-reports (Kolt and McEvoy, 2003) may improve assessment of adherence (Shaw et al., 2005).
4.3. Clinical implications
4.3.1. Pain
Worsening pain during exercise was a barrier to adherence with exercise (Minor and Brown, 1993; Dobkin et al., 2006) indicating that strategies to minimise initial pain are important. In most cases the appropriate use of simple analgesics, heat or ice coupled with passive physiotherapy treatments, e.g. acupuncture, manual therapy, etc may help to alleviate pain sufficiently to allow patients to adopt more active treatment strategies (Moffett and McLean, 2006). In the rare case of a patient with severe pain an analgesic review with their GP or consultant may be required in order to allow participation in rehabilitation.
Many people believe that activities that cause pain must be harmful. Clinicians need to gain a clear understanding of the patient's pain experience and beliefs about pain (Eccleston and Eccleston, 2004) and counter those which are mal-adaptive. Clinicians should reinforce messages which reduce fear or anxiety about pain, e.g. that the presence of pain should not prevent most patients from safely participating in therapeutic exercise (Waddell et al., 2004) and may lead to reduction in symptoms (Guzman et al., 2002), improved function and return to work (van Tulder et al., 2000). Those who participate in regular exercise are also less likely to experience progressive problems (McLean et al., 2007). Patients should be encouraged to start exercise gently and advised to progress to moderate or even high intensity levels of exercise over a period of time (Pernold et al., 2005). This evidence could counter the fears held by many pain sufferers that movement could be damaging or lead to re-injury.
4.3.2. Physical activity levels and exercise
Low levels of physical activity at baseline (Minor and Brown, 1993; Rejeski et al., 1997; Stenstrom et al., 1997; Schoo et al., 2005) or in previous weeks (Rejeski et al., 1997; Oliver and Cronan, 2002) and low in-treatment adherence with exercise (Alewijnse et al., 2003; Schoo et al., 2005; Dobkin et al., 2006) were barriers to treatment adherence. Physiotherapists need to recognise and be ready to mitigate the many barriers to initiating and adhering to exercise programmes; these include poor programme organisation and leadership, poor education, poor history of exercise, perceived physical frailty, perceived poor health and readiness to change (Duncan and McAuley, 1993; Courneya and McAuley, 1995; Boyette et al., 1997; Hellman, 1997; Rhodes et al., 1999).
Several strategies may be employed to improve patient adherence. Firstly providing explicit verbal instruction, checking the patient's recall and supporting this with additional written instructions may be effective at improving exercise adherence (Schneiders et al., 1998). Secondly, employing motivational techniques such as counselling sessions, positive feedback, reward, written treatment contracts and exercise diaries may also be helpful (Friedrich et al., 1998). Setting goals and drawing up action plans and coping plans which have been agreed collaboratively between the clinician and patient may be effective with patients who intend to participate in exercise (Bassett and Petrie, 1999; Evans and Hardy, 2002; Ziegelmann et al., 2006). Identifying potential barriers to exercising can support the development of action plans to initiate an exercise programme, whilst coping plans can help to overcome the difficulties that may arise over time and help patients to maintain that exercise programme (Gohner and Schlicht, 2006; Ziegelmann et al., 2006).
4.3.3. Self-efficacy
Low self-efficacy was identified as a barrier to treatment adherence (Shaw et al., 1994; Taylor and May, 1996; Stenstrom et al., 1997; Chen et al., 1999; Oliver and Cronan, 2002; Milne et al., 2005). Poor self-efficacy could explain a patient's low confidence in their ability to overcome obstacles to initiating, maintaining or recovering from relapses in exercise (Sniehotta et al., 2005). Low self-efficacy could be identified by clinicians using simple questions such as “How confident are you that you can…” (a) “overcome obstacles to exercising?” or (b) “return to exercise, despite having relapsed for several weeks?” Strategies to address low self-efficacy should be specific to the individual's stage of exercise behaviour or perceived obstacles (Scholz et al., 2005). The use of strategies such as agreeing realistic expectations (Jensen and Lorish, 1994), setting treatment goals (Evans and Hardy, 2002), action planning (Sniehotta et al., 2005), coping planning and positive reinforcement (Gohner and Schlicht, 2006) may help increase patient self-efficacy and adherence.
4.3.4. Anxiety, depression and helplessness
Depression (Minor and Brown, 1993; Shaw et al., 1994; Rejeski et al., 1997; Oliver and Cronan, 2002), anxiety (Minor and Brown, 1993; Dobkin et al., 2006) and helplessness (Sluijs et al., 1993; Castenada et al., 1998) were barriers to treatment adherence. Physiotherapists should be sensitive to the presence of anxiety, depression and helplessness and ensure that these patients are referred to relevant healthcare services for appropriate management as required. Simultaneously ensuring that pain is being effectively managed may be helpful in reducing anxiety or depression which is pain related. Additionally it may be helpful to reinforce the message that exercise is an effective way of countering both low mood and negative thoughts, whilst simultaneously improving pain and function (Lim et al., 2005). Greater social support and encouragement for exercise in this group of patients may provide motivation, role models and guidance that may be important (Castenada et al., 1998).
4.3.5. Social or family support/activity
Low levels of social activity (Funch and Gale, 1986; Minor and Brown, 1993; Sluijs et al., 1993; Rejeski et al., 1997; Oliver and Cronan, 2002) and social or familial support (Shaw et al., 1994) were barriers to treatment adherence. Some patients believe they would more readily exercise if accompanied by someone else during their activity (Milroy and O'Neil, 2000; Campbell et al., 2001). The support provided by the physiotherapist, the development of the patient–practitioner relationship and positive feedback from the physiotherapist may also increase adherence (Sluijs et al., 1993; Campbell et al., 2001). Clinicians could consider organising rehabilitation programmes which incorporate social contact and support. For example group based rehabilitation, exercise referral schemes, expert patient programmes and exercise classes based in the community may be an ideal way of providing some patients with the social stimulation and long term encouragement to continue their exercise progression. For other patients, actively involving partners in the rehabilitation process to encourage and motivate the patient may help (Fekete et al., 2006).
4.3.6. Barriers to exercise
Envisaging a greater number of barriers to participating in exercise predicted non-adherence with treatment (Sluijs et al., 1993; Alexandre et al., 2002). Barriers included transportation problems, child care needs, work schedules, lack of time, family dependents, financial constraints, convenience and forgetting. Physiotherapists need to be aware of difficulties that patients foresee in relation to adhering with a proposed treatment plan and act collaboratively with their patients to design treatment plans which are customised to the patient's life circumstances (Turk and Rudy, 1991). The addition of coping plans may help patients to overcome difficulties that may arise and allow them to maintain the treatment programme (Gohner and Schlicht, 2006; Ziegelmann et al., 2006).
4.3.7. Research implications
There was limited evidence for many barriers and a lack of research into other potential predictors, e.g. socioeconomic status and the barriers introduced by health professionals or health organisations. Adherence has been identified as a priority in physiotherapy research (Taylor et al., 2004) therefore further high quality research is required in order to investigate the predictive validity of these barriers within musculoskeletal settings.
Poor attendance at clinic appointments is an objective measure with quantifiable cost implications to the health service. The extent to which patients actually carry out a programme of exercises recommended by a physiotherapist is an important research question which is methodologically more difficult to answer. These two different aspects of adherence may be related to different barriers and may require different strategies to overcome them, therefore these different aspects of adherence may be better addressed individually.
5. Conclusion
This review identified 20 studies investigating barriers which predicted non-adherence with musculoskeletal treatment. Strong evidence was found that low levels of physical activity at baseline or in previous weeks, low in-treatment adherence with exercise, low self-efficacy, depression, anxiety, helplessness, poor social support or activity, greater perceived number of barriers to exercise and increased pain levels during exercise are all barriers to treatment adherence. Identification of these barriers during patient assessments may be important in order to adopt appropriate management strategies which help to counteract their effects and improve treatment outcome. The results of this review suggest that physiotherapists should be concerned about the attitudes, beliefs and barriers facing their patients and act collaboratively with their patients to design realistic treatment plans which are customised to the patient's life circumstances. There was conflicting evidence regarding age and pain at baseline and limited evidence for many other barriers. In addition there is a lack of research investigating barriers introduced by health professionals and health organisations. Further high quality research is required to increase our understanding of all the factors which contribute to patient non-adherence.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.math.2009.12.004.
Appendix. Supplementary data
References
- Alewijnse D., Mesters I., Metsemakers J., van den Borne B. Predictors of long-term adherence to pelvic floor muscle exercise therapy among women with urinary incontinence. Health Education Research. 2003;18(5):511–524. doi: 10.1093/her/cyf043. [DOI] [PubMed] [Google Scholar]
- Alexandre N.M., Nordin M., Hiebert R., Campello M. Predictors of compliance with short-term treatment among patients with back pain. Pan American Journal of Public Health. 2002;12(2):86–94. doi: 10.1590/s1020-49892002000800003. [DOI] [PubMed] [Google Scholar]
- Altman D.G., editor. Practical Statistics for Medical Research. Chapman & Hall; London: 1991. [Google Scholar]
- Ariens G.A., van Mechelen W., Bongers P.M., Bouter L.M., van der Wal G. Physical risk factors for neck pain. Scandinavian Journal of Work, Environment & Health. 2000;26(1):7–19. doi: 10.5271/sjweh.504. [DOI] [PubMed] [Google Scholar]
- Bassett S., Petrie K. The effects of treatment goals on patients compliance with physiotherapy exercise programmes. Physiotherapy. 1999;85(3):130–137. [Google Scholar]
- Benz Scott L.A., Ben-or K., Allen J.K. Why are women missing from outpatient cardiac rehabilitation programmes? A review of multilevel factors affecting referral, enrolment, and completion. Journal of Womens Health. 2002;11(9):773–791. doi: 10.1089/15409990260430927. [DOI] [PubMed] [Google Scholar]
- Borghouts J.A., Koes B.W., Bouter L.M. The clinical course and prognostic factors of non-specific neck pain: a systematic review. Pain. 1998;77(1):1–13. doi: 10.1016/S0304-3959(98)00058-X. [DOI] [PubMed] [Google Scholar]
- Boyette L.W., Sharon B.F., Brandon L.J. Exercise adherence for a strength training program in older adults. The Journal of Nutrition, Health & Aging. 1997;1(2):93–97. [PubMed] [Google Scholar]
- Brewer B.W., Van Raalte J.L., Cornelius A.E., Petitpas A.J., Sklar J.H., Pohlman M.H. Psychological factors, rehabilitation adherence and rehabilitation outcome after anterior cruciate ligament reconstruction. Rehabilitation Psychology. 2000;45(1):20–37. [Google Scholar]
- Brewer B.W., Cornelius A.E., Van Raalte J.L., Petitpas A.J., Sklar J.H., Pohlman M.H., Krushell R.J., Ditmar T.D. Age-related differences in predictors of adherence to rehabilitation after anterior cruciate ligament reconstruction. Journal of Athletic Training. 2003;38(2):158–162. [PMC free article] [PubMed] [Google Scholar]
- Broderick J.E., Stone A.A. Paper and electronic diaries: too early for conclusions on compliance rates and their effects. Psychological Methods. 2006;11(1):106–111. doi: 10.1037/1082-989X.11.1.106. [DOI] [PubMed] [Google Scholar]
- Campbell R., Evans M., Tucker M., Quilty B., Dieppe P., Donovan J. Why don't patients do their exercises? understanding non-compliance with physiotherapy in patients with osteoarthritis of the knee. Journal of Epidemiology and Community Health. 2001;55(2):132–138. doi: 10.1136/jech.55.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr A. Barriers to the effectiveness of any intervention in OA. Best Practice & Research Clinical Rheumatology. 2001;15(4):645–656. doi: 10.1053/berh.2001.0179. [DOI] [PubMed] [Google Scholar]
- Castenada D.M., Bigatti S., Cronan T.A. Gender and exercise behaviour among women and men with osteoarthritis. Womens Health. 1998;27(4):33–53. doi: 10.1300/J013v27n04_03. [DOI] [PubMed] [Google Scholar]
- Chen C.Y., Neufeld P.S., Feely C.A., Skinner C.S. Factors influencing compliance with home exercise programs among patients with upper-extremity impairment. The American Journal of Occupational Therapy. 1999;53(2):171–180. doi: 10.5014/ajot.53.2.171. [DOI] [PubMed] [Google Scholar]
- Courneya K.S., McAuley E. Cognitive mediators of the social influence-exercise adherence relationship: a test of the theory of planned behavior. Journal of Behavioral Medicine. 1995;18(5):499–515. doi: 10.1007/BF01904776. [DOI] [PubMed] [Google Scholar]
- CRD . University of York; 2001. Undertaking Systematic Reviews of Research on Effectiveness: CRDs Guidance for those Carrying Out or Commissioning Papers, NHS Centre for Reviews and Dissemination. [Google Scholar]
- Dobkin P.L., Abrahamowicz M., Fitzcharles M.A., Dritsa M., da Costa D. Maintenance of exercise in women with fibromyalgia. Arthritis and Rheumatism. 2005;53(5):724–731. doi: 10.1002/art.21470. [DOI] [PubMed] [Google Scholar]
- Dobkin P.L., Da Costa D., Abrahamowicz M., Dritsa M., Du Berger R., Fitzcharles M.A., Lowensteyn I. Adherence during an individualized home based 12-week exercise program in women with fibromyalgia. The Journal of Rheumatology. 2006;33(2):333–341. [PubMed] [Google Scholar]
- Donovan J.L. Patient decision making: the missing ingredient in compliance research. International Journal of Technology Assessment in Health Care. 1995;11(3):443–455. doi: 10.1017/s0266462300008667. [DOI] [PubMed] [Google Scholar]
- Duncan T.E., McAuley E. Social support and efficacy cognitions in exercise adherence: a latent growth curve analysis. Journal of Behavioral Medicine. 1993;16(2):199–218. doi: 10.1007/BF00844893. [DOI] [PubMed] [Google Scholar]
- Eccleston Z., Eccleston C. Interdisciplinary management of adolescent chronic pain: developing the role of the physiotherapist. Physiotherapy. 2004;90(2):77–81. [Google Scholar]
- Evans L., Hardy L. Injury rehabilitation: a goal-setting intervention study. Research Quarterly for Exercise and Sport. 2002;73(3):310–319. doi: 10.1080/02701367.2002.10609025. [DOI] [PubMed] [Google Scholar]
- Fekete E.M., Stephens M.A., Druley J.A., Greene K.A. Effects of spousal control and support on older adults' recovery from knee surgery. Journal of Family Psychology. 2006;20(2):302–310. doi: 10.1037/0893-3200.20.2.302. [DOI] [PubMed] [Google Scholar]
- Friedrich M., Gittler G., Halberstadt Y., Cermak T., Heiller I. Combined exercise and motivation program: effect on the compliance and level of disability of patients with chronic low back pain: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 1998;79(5):475–487. doi: 10.1016/s0003-9993(98)90059-4. [DOI] [PubMed] [Google Scholar]
- Funch D.P., Gale E.N. Predicting treatment completion in a behavioral therapy program for chronic temporomandibular pain. Journal of Psychosomatic Research. 1986;30(1):57–62. doi: 10.1016/0022-3999(86)90066-8. [DOI] [PubMed] [Google Scholar]
- Gohner W., Schlicht W. Preventing chronic back pain: evaluation of a theory-based cognitive-behavioural training programme for patients with subacute back pain. Patient Education and Counseling. 2006;64(1–3):87–95. doi: 10.1016/j.pec.2005.11.018. [DOI] [PubMed] [Google Scholar]
- Green A.S., Rafaeli E., Bolger N., Shrout P.E., Reis H.T. Paper or plastic? data equivalence in paper and electronic diaries. Psychological Methods. 2006;11(1):87–105. doi: 10.1037/1082-989X.11.1.87. [DOI] [PubMed] [Google Scholar]
- Guzman J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary bio-psycho-social rehabilitation for chronic low back pain. Cochrane Database of Systematic Reviews 2002; (1):CD000963. [DOI] [PubMed]
- Hayden J.A., van Tulder M.W., Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Annals of Internal Medicine. 2005;142(9):776–785. doi: 10.7326/0003-4819-142-9-200505030-00014. [DOI] [PubMed] [Google Scholar]
- Hellman E.A. Use of the stages of change in exercise adherence model among older adults with a cardiac diagnosis. Journal of Cardiopulmonary Rehabilitation. 1997;17(3):145–155. doi: 10.1097/00008483-199705000-00001. [DOI] [PubMed] [Google Scholar]
- Jackson L., Leclerc J., Erskine Y., Linden W. Getting the most out of cardiac rehabilitation: a review of referral and adherence predictors. Heart (British Cardiac Society) 2005;91(1):10–14. doi: 10.1136/hrt.2004.045559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen G.M., Lorish C.D. Promoting patient cooperation with exercise programs: linking research, theory, and practice. Arthritis Care and Research. 1994;7(4):181–189. doi: 10.1002/art.1790070405. [DOI] [PubMed] [Google Scholar]
- Karjalainen K., Malmivaara A., van Tulder M., Roine R., Jauhiainen M., Hurri H., Koes B. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain in working-age adults: a systematic review within the framework of the cochrane collaboration back review group. Spine. 2001;26(3):262–269. doi: 10.1097/00007632-200102010-00011. [DOI] [PubMed] [Google Scholar]
- Kenny D.T. Exercise-based rehabilitation for injured workers: programme efficacy and identification of factors predicting programme completion and outcome. International Journal of Rehabilitation Research. 2000;23(1):7–17. [PubMed] [Google Scholar]
- Kolt G.S., Brewer B.W., Pizzari T., Schoo A.M.M., Garrett N. The sport injury rehabilitation adherence scale: a reliable scale for use in clinical physiotherapy. Physiotherapy. 2007;93(1):17–22. [Google Scholar]
- Kolt G.S., McEvoy J.F. Adherence to rehabilitation in patients with low back pain. Manual Therapy. 2003;8(2):110–116. doi: 10.1016/s1356-689x(02)00156-x. [DOI] [PubMed] [Google Scholar]
- Laubach W.J., Brewer B.W., Van Raalte J.L., Petitpas A.J. Attributions for recovery and adherence to sport injury rehabilitation. Australian Journal of Science and Medicine in Sport. 1996;28(1):30–34. [PubMed] [Google Scholar]
- Lim H.J., Moon Y.I., Lee M.S. Effects of home-based daily exercise therapy on joint mobility, daily activity, pain, and depression in patients with ankylosing spondylitis. Rheumatology International. 2005;25(3):225–229. doi: 10.1007/s00296-004-0536-z. [DOI] [PubMed] [Google Scholar]
- Martin K.A., Sinden A.R. Who will stay and who will go? A review of older adults' adherence to randomized controlled trials of exercise. Journal of Aging and Physical Activity. 2001;9(2):91–114. [Google Scholar]
- McLean S.M., May S., Klaber Moffett J., Sharp D., Gardiner E. Prognostic factors for progressive non-specific neck pain. Physical Therapy Reviews. 2007;12(3):207–220. [Google Scholar]
- Miller N.H., Hill M., Kottke T., Ockene I.S. The multilevel compliance challenge: recommendations for a call to action. A statement for healthcare professionals. Circulation. 1997;95(4):1085–1090. doi: 10.1161/01.cir.95.4.1085. [DOI] [PubMed] [Google Scholar]
- Milne M., Hall C., Forwell L. Self efficacy, imagery use and adherence to rehabilitation by injured athletes. Journal of Sport Rehabilitation. 2005;14(2):150–167. [Google Scholar]
- Milroy P., O'Neil G. Factors affecting compliance to chiropractic prescribed home exercise: a review of the literature. Journal of Canadian Chiropractic Association. 2000;44(3):141–148. [Google Scholar]
- Minor M.A., Brown J.D. Exercise maintenance of persons with arthritis after participation in a class experience. Health Education Quarterly. 1993;20(1):83–95. doi: 10.1177/109019819302000108. [DOI] [PubMed] [Google Scholar]
- Moffett J., McLean S. The role of the physiotherapist in the management of non-specific back pain and neck pain. Rheumatology. 2006;45(4):371–378. doi: 10.1093/rheumatology/kei242. [DOI] [PubMed] [Google Scholar]
- Oliver K., Cronan T. Predictors of exercise behaviors among fibromyalgia patients. Preventive Medicine. 2002;35(4):383–389. doi: 10.1006/pmed.2002.1084. [DOI] [PubMed] [Google Scholar]
- Pernold G., Mortimer M., Wiktorin C., Tornqvist E.W., Vingard E. Musculoskeletal intervention Center-Norrtalje study group. Neck/shoulder disorders in a general population. natural course and influence of physical exercise: a 5-year follow-up. Spine. 2005;30(13):E363–E368. doi: 10.1097/01.brs.0000167819.82642.f7. [DOI] [PubMed] [Google Scholar]
- Rejeski W.J., Brawley L.R., Ettinger W., Morgan T., Thompson C. Compliance to exercise therapy in older participants with knee osteoarthritis: implications for treating disability. Medicine and Science in Sports and Exercise. 1997;29(8):977–985. doi: 10.1097/00005768-199708000-00001. [DOI] [PubMed] [Google Scholar]
- Rhodes R.E., Martin A.D., Taunton J.E., Rhodes E.C., Donnelly M., Elliot J. Factors associated with exercise adherence among older adults: an individual perspective. Sports Medicine. 1999;28(6):397–411. doi: 10.2165/00007256-199928060-00003. [DOI] [PubMed] [Google Scholar]
- Schneiders A.G., Zusman M., Singer K. Exercise therapy compliance in acute low back pain. Manual Therapy. 1998;3(3):147–152. [Google Scholar]
- Scholten-Peeters G.G., Verhagen A.P., Bekkering G.E., van der Windt D.A., Barnsley L., Oostendorp R.A., Hendriks E.J. Prognostic factors of whiplash-associated disorders: a systematic review of prospective cohort studies. Pain. 2003;104(1–2):303–322. doi: 10.1016/s0304-3959(03)00050-2. [DOI] [PubMed] [Google Scholar]
- Scholz U., Sniehotta F.F., Schwarzer R. Predicting physical exercise in cardiac rehabilitation: the role of phase-specific self-efficacy beliefs. Journal of Sport & Exercise Psychology. 2005:27135–27151. [Google Scholar]
- Schoo A.M.M., Morris M.E., Quang M.B. Predictors of home exercise adherence in older people with osteoarthritis. Physiotherapy Canada. 2005;57(3):179–187. [Google Scholar]
- Shaw T., Williams M.T., Chipchase L.S. A review and user's guide to measurement of rehabilitation adherence following anterior cruciate ligament reconstruction. Physical Therapy in Sport. 2005;6(1):45–51. [Google Scholar]
- Shaw W.S., Cronan T.A., Christie M.D. Predictors of attrition in health intervention research among older subjects with osteoarthritis. Health Psychology. 1994;13(5):421–431. doi: 10.1037//0278-6133.13.5.421. [DOI] [PubMed] [Google Scholar]
- Sluijs E.M., Kok G.J., van der Zee J. Correlates of exercise compliance in physical therapy. Physical Therapy. 1993;73(11):771–782. doi: 10.1093/ptj/73.11.771. (discussion 783–86) [DOI] [PubMed] [Google Scholar]
- Sniehotta F.F., Scholz U., Schwarzer R. Bridging the intention-behavior gap: planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychology and Health. 2005;20(2):143–160. [Google Scholar]
- Stenstrom C.H., Arge B., Sundbom A. Home exercise and compliance in inflammatory rheumatic diseases: a prospective clinical trial. The Journal of Rheumatology. 1997;24(3):470–476. [PubMed] [Google Scholar]
- Stone A.A., Shiffman S., Schwartz J.E., Broderick J.E., Hufford M.R. Patient compliance with paper and electronic diaries. Controlled Clinical Trials. 2003;24(2):182–199. doi: 10.1016/s0197-2456(02)00320-3. [DOI] [PubMed] [Google Scholar]
- Tabachnick B.G., Fidell L.S. Allyn and Bacon; Boston: 2001. Using Multivariate Statistics. [Google Scholar]
- Taylor A.H., May S. Threat and coping appraisal as determinants of compliance with sports injury rehabilitation: an application of protection motivation theory. Journal of Sports Sciences. 1996;14(6):471–482. doi: 10.1080/02640419608727734. [DOI] [PubMed] [Google Scholar]
- Taylor N., Dodd K., McBurney H., Kerr Graham H. Factors influencing adherence to a home based strength training programme for young people with cerebral palsy. Physiotherapy. 2004:9057–9063. [Google Scholar]
- Turk D.C., Rudy T.E. Neglected topics in the treatment of chronic pain patients – relapse, noncompliance, and adherence enhancement. Pain. 1991;44(1):5–28. doi: 10.1016/0304-3959(91)90142-K. [DOI] [PubMed] [Google Scholar]
- van Tulder M., Malmivaara A., Esmail R., Koes B. Exercise therapy for low back pain: a systematic review within the framework of the cochrane collaboration back review group. Spine. 2000;25(21):2784–2796. doi: 10.1097/00007632-200011010-00011. [DOI] [PubMed] [Google Scholar]
- Vasey L. DNAs and DNCTs – why do patients fail to begin or complete a course of physiotherapy treatment? Physiotherapy. 1990:76575–76578. [Google Scholar]
- Verhagen AP, Scholten-Peeters GG, de Bie RA, Bierma-Zeinstra SM. Conservative treatments for whiplash. Cochrane Database of Systematic Reviews 2004;(1): CD003338. [DOI] [PubMed]
- Vermeire E., Hearnshaw H., Van Royen P., Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. Journal of Clinical Pharmacy and Therapeutics. 2001;26(5):331–342. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- Viera A.J., Garrett J.M. Understanding interobserver agreement: the kappa statistic. Family Medicine. 2005;37(5):360–363. [PubMed] [Google Scholar]
- Waddell G., Klaber Moffett J., Burton A. The Stationary Office; London: 2004. The Neck Book. [Google Scholar]
- WHO . World Health Organisation; Geneva: 2003. Adherence to Long Term Therapies – Evidence for Action. [Google Scholar]
- Ziegelmann J.P., Lippke S., Schwarzer R. Subjective residual life expectancy in health self-regulation. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2006;61(4):P195–P201. doi: 10.1093/geronb/61.4.p195. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.