Abstract
We sought to assess continuity of care for elderly patients in Korea and to examine any association between continuity of care and health outcomes (hospitalization, emergency department visits, health care costs). This was a retrospective cohort study using the Korea National Health Insurance Claims Database. Elderly people, 65-84 yr of age, who were first diagnosed with diabetes mellitus (n=268,220), hypertension (n=858,927), asthma (n=129,550), or chronic obstructive pulmonary disease (COPD, n=131,512) in 2002 were followed up for four years, until 2006. The mean of the Continuity of Care Index was 0.735 for hypertension, 0.709 for diabetes mellitus, 0.700 for COPD, and 0.663 for asthma. As continuity of care increased, in all four diseases, the risks of hospitalization and emergency department visits decreased, as did health care costs. In the Korean health care system, elderly patients with greater continuity of care with health care providers had lower risks of hospital and emergency department use and lower health care costs. In conclusion, policy makers need to develop and try actively the program to improve the continuity of care in elderly patients with chronic diseases.
Keywords: Continuity of Patient Care; Hospitalization; Health Care Costs; Diabetes Mellitus; Hypertension; Asthma; Pulmonary Disease, Chronic Obstructive
INTRODUCTION
Health care spending for the elderly population in Korea increased by 100% in 4 yr, from 5,109 billion Won in 2004 to 10,490 billion Won in 2008, and its proportion of total health insurance spending also rose, from 22.9% in 2004 to 29.9% in 2008 (1). Elderly people, aged 65 yr and over, currently represent 9.6% (approximately 4.6 million) of total health insurance beneficiaries, but they are responsible for a quarter of total health insurance expenditures (1). The elderly population is expected to grow faster over the next decades as the post-Korean War baby boomers begin to retire in large numbers. Thus, appropriate strategies are urgently required to promote the efficient spending of health care budgets for elderly people.
Previous studies have reported that enhanced continuity of care prevented a sudden worsening in progress among chronic disease patients, and as a result was favorable for efficient spending of health care funds (2). Continuity of care is not only a key factor in delivering good health care, but also an attribute emphasized in common in various definitions of primary care (3). The implication is that a high level of continuity of primary care could have a positive impact on the process of care, outcomes, and costs (4). Maintaining and enhancing continuity of care, primary health care in particular, has become an important goal of health care policy in many countries, and a number of studies on the association between continuity of care and health outcomes have been reported (5-10).
However, most studies were conducted in children or adults aged under 65 yr (5-8), not in elderly patients aged 65 and over (9, 10). Even studies of elderly patients have focused little attention on the association between continuity of care and health outcomes (10).
The aim of this study was to assess the continuity of outpatient service use by elderly patients in Korea and to examine any association between the continuity of care and health outcomes (hospitalization, emergency department visits, health care costs) and ultimately provide useful information for health care policy makers.
MATERIALS AND METHODS
Study setting
Health care institutions under the Korea National Health Insurance are classified according to the number of beds into clinics (fewer than 30 beds), hospitals (30-99 beds), and general hospitals (more than 99 beds); all of these can provide outpatient services. Under the current health care delivery system, patients can select any practitioner or any medical care institution. However, when a patient wants to receive medical care at a secondary hospital, called a specialized general hospital, the patient must present a referral slip issued from the doctor who saw the patient first. Specialized general hospitals are designated among general hospitals when they meet standards of teaching hospitals and other requirements (number of specialized general hospitals in 2007=43) (11). Exceptions to the referral system are in the case of childbirth, emergency medical care, dental care services, rehabilitation, family medicine services, and medical services for a patient with hemophilia, in which case any health care institution can be utilized without limitation (11).
The health care delivery system in Korea is quite different from the managed care delivery system of the United States of America, in which a patient's selection of health care provider is regulated and restricted. Above all, because most clinical practitioners in Korea are specialists, they do not perform the function of a primary care physician as seen in America. In Korea, 91% of clinical practitioners (28,733/31,578) were specialists, and 98% of clinics (25,168/25,789) were sole practices in the year 2006 (12). In terms of outpatient services, clinics compete against other clinics, hospitals, and some general hospitals.
Study data
Study data were collected from the Korea National Health Insurance Claims Database of the Health Insurance Review & Assessment Service, for the period 2002 to 2006. The International Classification of Disease, 10th edition (ICD 10) was used as the coding system for diagnosis.
As typical chronic diseases of elderly patients in Korea, diabetes mellitus (E10-14), hypertension (I10), asthma (J45-46), and chronic obstructive pulmonary disease (COPD, J41-J44, J47), were selected. These four diseases have shown a sharp increase in the elderly population associated with population aging, presumably causing an increased burden of disease (1). They are also included in ambulatory care-sensitive conditions (ACSCs).
ACSCs are defined as those conditions for which the provision of timely and effective outpatient care, primary health care in particular, can help to reduce the risk of hospitalization (13). This study followed the classifications by Shi et al., who classified ACSCs by conditions applicable to adults (13).
The study dataset was constructed for each disease with insurance claims for patients whose disease was marked as a primary disease or a secondary disease, but not as a diagnosis by exclusion. When physicians complete the medical care cost statement to make an insurance claim for care service provided to a patient, they are required to enter the diagnosis code for the patient in accordance with the Korean classification of diseases. The primary disease is written in the first column, and the secondary disease in the next. If two or more secondary diseases are diagnosed, they are written in order of importance. The primary disease refers to a disease for which the patient made the strongest demands for treatment or testing, and the secondary disease indicates a disease or diseases diagnosed together with the primary disease during the period of care. In this study, the first disease listed in the order of diagnostic-code entry was selected as a primary disease, and the second disease as a secondary disease (14).
Study subjects were followed for 4 yr, the first 3 for continuity of care and the last year for health outcomes (hospitalization, emergency department visits, health care costs). Although the same duration was applied to all study subjects, the dates of actual follow up periods could be different. For example, in the case of a patient who was first diagnosed on January 1, 2002, his or her follow-up period would be from January 1, 2002 to December 31, 2005, whereas another patient first diagnosed on May 1, 2002 would be followed up until April 30, 2006.
This study was approved by the Institutional Review Boards of the Health Insurance Review and Assessment Service (HIRA: K53-58).
Study population
The study subjects were recruited with the following criteria: 1) they were first diagnosed with diabetes mellitus (E10-14), hypertension (I10), asthma (J45-46), or chronic obstructive pulmonary disease (J41-J44, J47) in 2002; 2) they were 65 to 84 yr of age at the end of 2002; and 3) they were not hospitalized, nor had they visited an emergency department or died during first 3 yr of the 4-yr follow-up period. Additionally, because a minimum of four ambulatory care visits was required for measuring continuity of care (15), patients who made fewer than four ambulatory care visits during the first 3 yr were excluded. The exclusion of patients who died or had hospitalizations or emergency department visits during the first 3 yr of the 4-yr follow up was intended to reveal causality between the independent variable and the dependent variable. The restriction on the number of visits was intended to ensure the accuracy of diagnosis and to allow the calculation of the Continuity of Care (COC) Index in a structurally reasonable and meaningful manner (7, 8). First-diagnosed patients were defined as those who had no record for a diagnosis of the disease concerned between 1995, the year in which the Korea National Health Insurance Claims Database was constructed, and 2001, and then were first diagnosed with the disease in 2002.
Measures
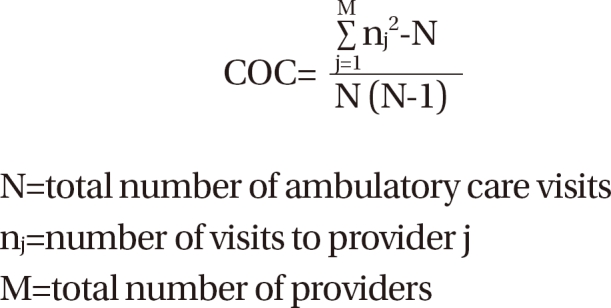
Independent variable: continuity of care index
Many tools are available to assess continuity of care (16). In this study, continuity of care for elderly patients was quantified using the COC Index. The COC Index is a widely used measure that incorporates the idea that personal continuity of care is affected by both the total number of providers and the total number of ambulatory care visits (6, 15). The COC Index ranges from 0 to 1. If a patient concentrates all ambulatory care visits with the same provider, the index equals 1, whereas if visits are dispersed to all different providers, it becomes 0.
To facilitate the analysis and description of the association between continuity of care and health outcomes, the COC level in this study was categorized into high, medium, and low tertiles (5, 8).
Dependent variables
Health outcomes, which were dependent variables in this study, consisted of data on hospitalization, emergency department visits, and health care costs. Hospitalization and emergency department visits were recorded as dichotomous variables, indicating whether or not a patient had a hospital admission or an emergency visit due to the disease concerned during the last year of the 4-yr follow up. If patients were hospitalized with the disease concerned as a primary disease or a secondary disease during the last year, they were regarded as having health outcome events regardless of the number of hospitalizations (17). This rule was also applied to emergency department visits.
Health care costs refer to the total amount claimed for care services extended to study subjects under the National Health Insurance (NHI) during the last year of the 4-yr follow up. Health care costs included costs for procedures, therapies, and medications spent for the treatment of all diseases, including the disease concerned, but excluded non-covered costs under the NHI.
Covariates
Control variables were divided into demographic variables and disease severity variables. Demographic variables were gender (male, female), age (65-69, 70-74, 75-59, 80-84 yr), and type of insurance (health insurance, Medical Aid). Variables for disease severity were the number of ambulatory care visits, main attending medical institution, and comorbidities. The number of ambulatory care visits and the presence of comorbidities were included here because both variables are associated with health care utilization behavior and disease severity and influence hospitalization and emergency department visits (8). Comorbid conditions for the four diseases were selected from relevant references (17-20), and if patients were diagnosed with a comorbid condition at a health care institution during first 3 yr of the 4-yr follow-up, they were classified as having a comorbidity. The selected comorbid conditions were:
diabetes mellitus: hypertension (I10-13), heart disease (I20-25), stroke (I60-64), and renal disease (N10-12,15-19) (17);
hypertension: heart disease (I20-25), stroke (I60-64), renal disease (N10-12,15-19), heart failure (I50), and diabetes mellitus (E10-14) (18);
asthma: obstructive pulmonary disease (J40-44,47), pneumonia (J10-18), cardiac dysrhythmias (I47-49), hypertension (I10-13), diabetes (E10-14), and heart failure (I50) (19); and
chronic obstructive pulmonary disease: pneumonia (J10-18), hypertension (I10-13), diabetes (E10-14), heart failure (I50), heart disease (I20-25), pulmonary vascular disease (I26-28), thoracic malignancies (C30-34,C37-39), renal disease (N10-12,15-19), stroke (I60-64), and gastrointestinal bleeding (K92) (20).
Main attending medical institutions were defined as the health care institutions that patients visited most often during the first 3 yr. These were classified into specialized general hospitals, general hospitals, hospitals, clinics, and public health centers.
Statistical analyses
Continuity level was compared by demographic properties and disease severity using the t-test or ANOVA. Differences in hospitalization, emergency department visits, and health care costs by patient characteristics were also examined using the t-test or ANOVA.
The association between continuity of care and health outcomes (hospitalization, emergency department visits) was evaluated through a multiple logistic regression analysis. Factors affecting continuity of care and the relationship between continuity of care and health care costs were examined through a multiple regression analysis. Health care costs were log-transformed to consider the linearity of the regression model and the outliers among the observational values. The SAS System (Version 8.1 for Microsoft Windows) was used as statistical software.
RESULTS
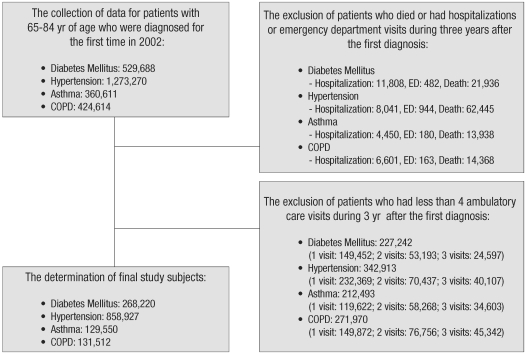
Through the selection procedures presented in Fig. 1, 268,220 patients with diabetes mellitus, 858,927 patients with hypertension, 129,550 patients with asthma, and 131,512 patients with COPD were recruited as study subjects.
Fig. 1.
Flowchart of the selected study subjects.
COPD, chronic obstructive pulmonary disease; ED, emergency department visits.
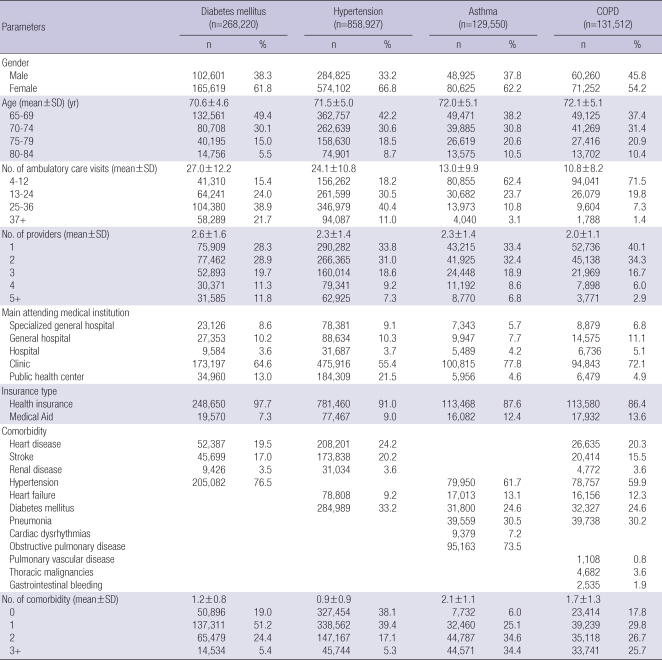
The characteristics of patients with diabetes, hypertension, asthma, and COPD are shown in Table 1. In all four diseases, the majority of study subjects were female, and the mean age of patients was approximately 70 yr. The mean number of visits to providers during the follow-up period was 27.0 for diabetes mellitus, 24.1 for hypertension, 13.0 for asthma, and 10.8 for COPD. The mean number of providers was approximately two in all four diseases (2.6 for diabetes mellitus, 2.3 for hypertension, 2.3 for asthma, and 2.0 for COPD). Clinics were the main attending medical institution used by the largest number of patients in all four diseases; in asthma and COPD, in particular, more than 70% of patients were using clinics. Health insurance beneficiaries represented approximately 90% of the total study subjects. The mean number of comorbidities was 2.1 for asthma, 1.7 for COPD, 1.2 for diabetes mellitus, and 0.9 for hypertension.
Table 1.
Study subject characteristics
COPD, chronic obstructive pulmonary disease.
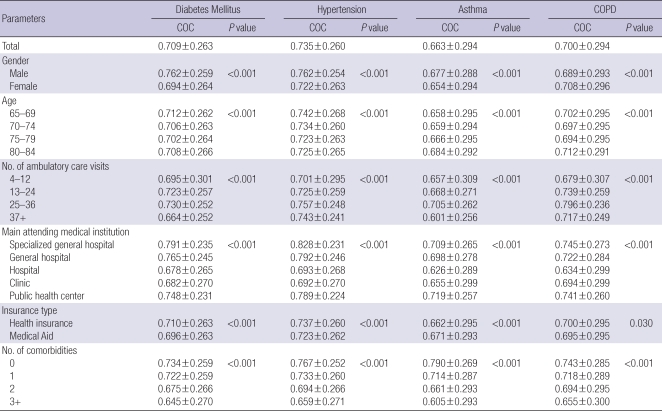
Continuity of care by patient characteristics is compared in Table 2. The highest level of continuity among the four diseases was measured in hypertension (mean±SD of the COC Index, 0.735±0.260), followed by diabetes mellitus (0.709±0.263), COPD (0.700±0.294), and asthma (0.663±0.294). Generally, continuity of care was higher for male patients than for female patients, and the continuity tended to decrease as the age of the patients increased. The level of continuity kept rising up to 36 visits and declined thereafter. Patients whose main attending medical institutions were specialized general hospitals showed the highest level of continuity, whereas the continuity for patients using hospitals was the lowest. Health insurance beneficiaries showed a higher level of continuity than did Medical Aid recipients. As the number of comorbidities increased, continuity of care decreased.
Table 2.
Level of continuity by patient characteristics
COPD, chronic obstructive pulmonary disease; COC, continuity of care.
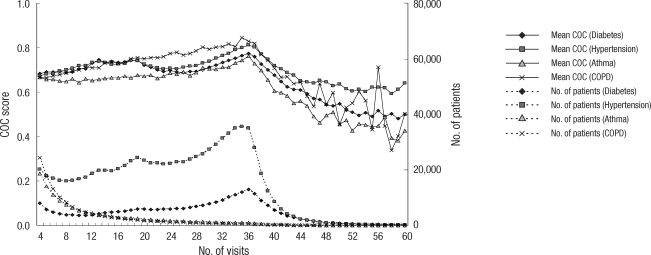
Fig. 2 indicates the level of continuity and the number of patients by the number of visits during the first 3 yr of the 4-yr follow up. The level of continuity increased up to 36 visits for all four diseases but drastically declined thereafter. Number of patients with diabetes mellitus and hypertension continued to increase up to 36 visits and dwindled thereafter, whereas that of patients with asthma and COPD was highest at four visits and declined continuously thereafter.
Fig. 2.
Continuity of care scores and the number of patients by the number of ambulatory care visits during the first 3 yr of the 4-yr follow up.
COC, continuity of care; COPD, chronic obstructive pulmonary disease.
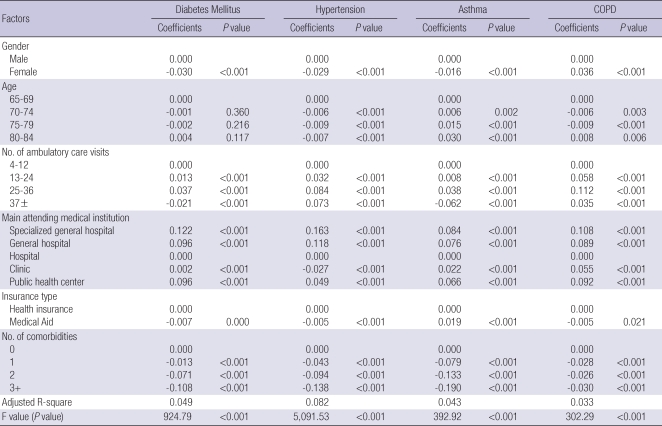
Factors affecting continuity of care were analyzed for the four diseases using a multiple regression analysis (Table 3). For diabetes mellitus, hypertension, and asthma, women showed a statistically significantly lower level of continuity than men. For COPD, however, women had a higher level of continuity than men. Age affected continuity of care differently. Compared to the 65-69 age group, the 70-74 and 75-79 age groups showed decreased continuity for hypertension and COPD, but increased continuity for asthma. Continuity did not differ with age for diabetes mellitus. The number of ambulatory care visits also influenced continuity of care. Because continuity of care sharply declined from 37 ambulatory care visits in all four diseases, ambulatory care visits were first divided according to those patients doing ≤36 and those doing 37+ visits, and then the ≤36 visits level was further divided into 4-12, 13-24, and 25-36 visits. Compared to continuity for patients doing 4-12 visits, those doing 13-24 visits and 25-36 visits showed increased continuity for all four diseases. The 37+ visit category had lower continuity than the 4-12 visit category for diabetes mellitus and asthma (diabetes mellitus: β=-0.021, asthma: β=-0.062). Although no negative relationship was found between continuity and number of ambulatory visits in hypertension and COPD, a less positive relationship was observed at 37+ visits than at 25-36 visits. Compared to patients whose main attending medical institutions were hospitals, those who used other medical institutions, including general hospitals and specialized general hospitals, showed enhanced continuity. For diabetes mellitus, hypertension, and COPD, Medical Aid recipients showed lower continuity than did health insurance beneficiaries, whereas in asthma, the opposite results were shown. In all four diseases, the level of continuity decreased with the increasing number of comorbidities.
Table 3.
Analysis of factors affecting continuity of care; a multiple linear regression model
COPD, chronic obstructive pulmonary disease.
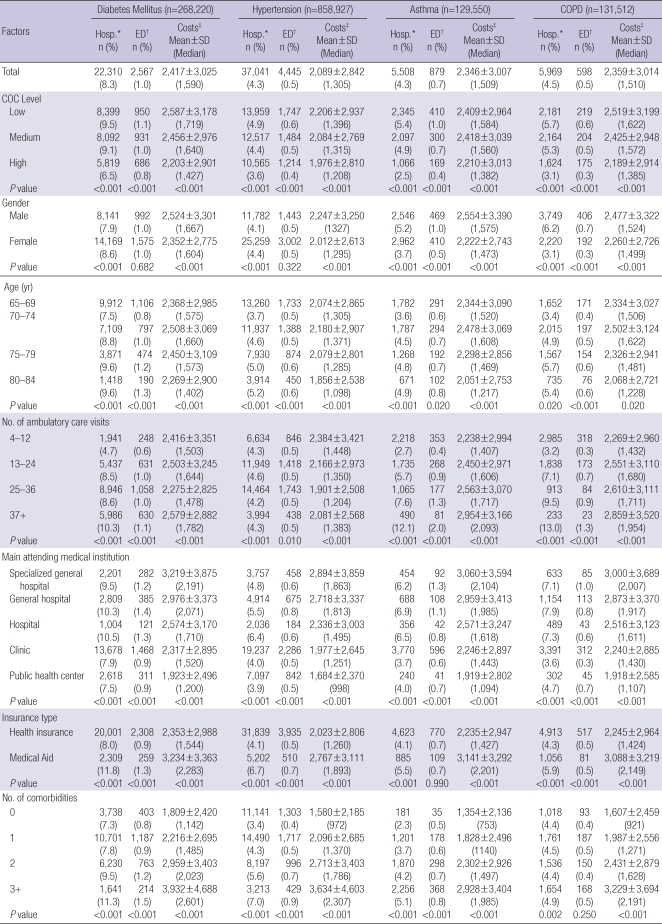
In Table 4, we examined differences in hospitalization, emergency department visits, and health care costs by patient characteristics. As the level of continuity decreased for all four diseases, hospitalization, emergency department visits, and mean health care costs increased. Women showed a higher hospitalization rate than men for diabetes mellitus and hypertension, whereas men had higher rate of hospitalization and emergency department visits than women for asthma and COPD. The rate of hospitalization and emergency department visits increased with increasing age and increasing number of ambulatory care visits. Patients whose main attending medical institutions were hospitals, general hospitals, or specialized general hospitals showed a higher rate of hospitalization and emergency department visits than those who used clinics and public health centers. For Medical Aid recipients and with increasing number of comorbidities, the rate of hospitalization and emergency department visits increased. More average health care costs were spent for men, patients who made 37 or more ambulatory care visits, patients whose main attending medical institutions were specialized general hospitals, and Medical Aid recipients. Mean health care costs decreased as age increased, and increased as the number of comorbidities increased.
Table 4.
Differences in hospitalization, emergency department visits, and health care costs by patient characteristics
*Hospitalization; †Emergency department visits; ‡Health care costs (unit: 1,000 won [KRW]).
COPD, chronic obstructive pulmonary disease.
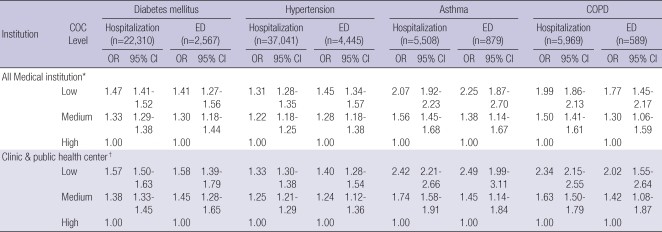
The association between continuity of care and health outcomes, adjusted for confounders, is presented in Table 5. Compared to the high continuity group, in all four diseases, the low continuity group showed a higher risk of hospitalization (diabetes mellitus odds ratio [OR], 1.47, 95% confidence interval [CI], 1.41-1.52; hypertension OR, 1.31, 95% CI, 1.28-1.35; asthma OR, 2.07, 95% CI, 1.92-2.23; COPD OR, 1.99, 95% CI, 1.86-2.13) and a higher risk of emergency department visits (diabetes mellitus OR, 1.41, 95% CI, 1.27-1.56; hypertension OR, 1.45, 95% CI, 1.34-1.57; asthma OR, 2.25, 95% CI, 1.87-2.70; COPD OR, 1.77, 95% CI, 1.45-2.17) than did the high continuity group. The medium continuity group also had higher risks of hospitalization and emergency department visits than did the high continuity group, but lower risks than the low continuity group. As continuity of care is an important attribute in primary care and clinics, and public health centers are important primary care providers in Korea, we made a separate analysis for patients whose main attending medical institutions were clinics and public health centers (5). As continuity of care decreased, risks of hospitalization and emergency department visits increased in this separate analysis as well.
Table 5.
Association between continuity of care and health outcomes (hospitalization and emergency department visits)
*Adjusted for gender, age (65.69, 70.74, 75.79, 80.84 yr), the number of ambulatory care visits (4.12, 13.24, 25.36, 37+), main attending medical institution (specialized general hospital, general hospital, hospital, clinic, public health center), insurance type (health insurance, Medical Aid), and the number of comorbidities (0, 1, 2, 3+); †An alyzed for patients whose main attending medical institutions were clinics and public health centers only. Adjusted for gender, age (65.69, 70.74, 75.79, 80.84 yr), the number of ambulatory care visits (4.12, 13.24, 25.36, 37+), main attending medical institution (clinic, public health center), insurance type (health insurance, Medical Aid), and the number of comorbidities (0, 1, 2, 3+).
COPD, chronic obstructive pulmonary disease; ED, Emergency department visits; COC, continuity of care.
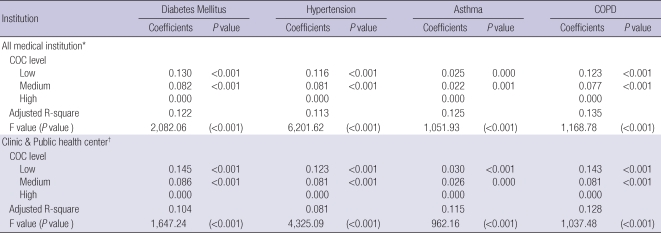
Table 6 shows the association between continuity of care and health care costs after adjusting for confounders. Compared to the high continuity group, in all four diseases, health care costs increased in both the medium continuity group and the low continuity group. Similar results were also obtained in a separate analysis for patients whose main attending medical institutions were clinics and public health centers.
Table 6.
Association between continuity of care and health care costs (from multiple linear regression models)
Health care cost was log-transformed.
*Adjusted for gender, age (65.69, 70.74, 75.79, 80.84 yr), the number of ambulatory care visits (4.12, 13.24, 25.36, 37+), main attending medical institution (specialized general hospital, general hospital, hospital, clinic, public health center), insurance type (health insurance, Medical Aid), and the number of comorbidities (0, 1, 2, 3+); †Analyzed for patients whose main attending medical institutions were clinics and public health centers only. Adjusted for gender, age (65.69, 70.74, 75.79, 80.84 yr), the number of ambulatory care visits (4.12, 13.24, 25.36, 37+), main attending medical institution (clinic, public health center), insurance type (health insurance, Medical Aid), and the number of comorbidities (0, 1, 2, 3+).
COPD, chronic obstructive pulmonary disease; COC, continuity of care.
DISCUSSION
Our study showed that the mean (±SD) of the COC Index for elderly patients was, in descending order, 0.735±0.260 for hypertension, 0.709±0.263 for diabetes mellitus, 0.700±0.294 for COPD, and 0.663±0.294 for asthma. In a previous study, continuity over a year for Medicaid patients aged 0-64 yr in the United States was measured as 0.51 by the COC Index (6). Another study by Magill and Senf found that the measure of continuity for family medicine outpatients at some university hospitals was approximately 0.41 (21). The level of continuity in the study by Patten and Friberg was 0.21 (22). These studies, however, differed from ours in terms of age and condition of the study subjects. Our study measured continuity for patients who were aged 65 yr and above, had selected chronic diseases (diabetes mellitus, hypertension, asthma, or COPD), and used outpatient services. In previous studies, however, continuity was measured for patients of all age groups who used outpatient services with any kind of disease. According to Sloane and Egelhoff, continuity was lowest in patients under 19 yr and highest in patients over 54 yr (23). Fleming et al. (24) and Godkin and Rice (25) reported that continuity varied according to condition, and it was higher for chronic diseases than for acute diseases. Thus, no direct comparison between the results of this study and those of the previous studies is possible. Although a few other studies have addressed the association between continuity of care and health outcomes in elderly patients (9, 10), they also provided measures of continuity for different diseases or with a different continuity index than did the current study.
In this study, the level of continuity increased up to 36 visits and started to decrease thereafter. Thirty-six visits over 3 yr can be interpreted as one ambulatory care visit every month. As seen in Fig. 2, for diabetes mellitus and hypertension, the highest number of patients and the highest level of continuity were all shown at 36 visits for 3 yr. In all four diseases, high continuity was maintained above a certain level at 4-36 ambulatory care visits. Most patients (diabetes mellitus, 78.3%; hypertension, 89.0%; asthma, 96.9%; COPD, 98.6%) made 4-36 ambulatory care visits. Continuity of care declined sharply from 37 ambulatory care visits. When we examined continuity of care using a multiple linear regression analysis for patients who made 37 or more ambulatory care visits, the level of continuity still decreased after adjusting for comorbidities. This result implies that factors other than disease severity may be acting on the sharp decline; thus, further studies are required to clarify those factors (26).
When the study subjects were divided into Medical Aid recipients and health insurance beneficiaries, in diabetes mellitus, hypertension, and COPD, Medical Aid recipients showed lower continuity than did health insurance beneficiaries. The Medical Aid program is a social security system in Korea, providing basic medical services to people with incomes below a low-income threshold (11). Medical Aid recipients belong to a socio-economically lower class and have a higher probability for comorbidities (27). Such characteristics of Medical Aid recipients may have affected their lower continuity (27). In addition, recipients of Medical Aid make only small or no out-of-pocket payments, and thus they can visit as many health care institutions as they desire without financial burden. The continuity for Medical Aid recipients could decrease due to this financial reason as well. In our analysis of factors affecting continuity of care using a multiple linear regression analysis, even after adjusting for disease severity including comorbidities, Medical Aid recipients had a lower level of continuity than health insurance beneficiaries. This result implies that other factors, not disease severity, might have been involved in creating differences in continuity between health insurance beneficiaries and Medical Aid recipients; thus, further studies are required to explore the reasons (26).
As for main attending medical institutions, the level of continuity was lowest for patients using hospitals. A previous study reported the same results, suggesting that the lower continuity of care in hospitals resulted from a relatively higher proportion of patients with comorbidities among hospital patients (26, 27). In our study, however, even after adjusting for comorbidities, continuity of care in hospitals was still lowest; thus, further studies are necessary to clarify the reasons for the lower continuity of care in hospitals.
In this study, as continuity of care increased, the risks of hospitalization and emergency department visits decreased in all four diseases. Similar results were obtained from the groups of health insurance beneficiaries and Medical Aid recipients (data not shown). Many previous studies have also reported that the increased continuity of care reduced the risk of hospitalization or emergency department visits (5-8).
The lowered risk of hospitalization can be explained in the following way. A patient undergoes complex procedures until a decision about hospitalization is made. Factors influencing the decision include the patient's current health condition(s), past illnesses, possible disease worsening, and adherence to ambulatory care recommendations. A physician who has a continuing relationship with a patient will have more knowledge of these factors and will be able to make a better decision as to whether hospitalization is required or outpatient treatment is sufficient. Thus, a physician who has a continuous relationship with a patient is likely to reduce disease progression through appropriate disease management and reduce or prevent unnecessary hospitalization. Thus, higher continuity of care lowers the risk of hospitalization (6).
The result that patients with higher continuity also had a lower risk of emergency department visits can also be explained to some degree by the same reasoning. When a patient has seen a physician frequently, the patient would likely visit the physician first, instead of going directly to an emergency department. This is likely to reduce the risk of emergency department visits.
When the association between continuity of care and health care costs was examined, as continuity of care increased, health care costs decreased for all four diseases. Many previous studies have reported similar results, indicating that enhanced continuity can reduce hospitalizations and unnecessary visits to health care institutions (2, 9).
This study has some limitations. First, because we could not obtain data on disease-specific costs paid for the study subjects during the last year, we used total costs instead. Furthermore, non-covered costs under the NHI were not included in health care costs. When Raddish et al. (2) divided health care costs into total cost and disease-specific costs and examined the association between continuity of care and both types of costs, they found that both costs decreased as continuity of care increased. They supposed that the patient with a high continuity of care for a disease would probably have high continuity for another disease, and health care costs would decrease accordingly. Thus, despite the lack of above cost data, it is still meaningful that this study used health care costs for all diseases to examine whether health care costs decreased as continuity of care increased (2, 9).
Second, this study was limited to those who were first diagnosed in 2002, had four or more ambulatory care visits, and neither died nor had a hospitalization or an emergency department visit during first 3 yr of the 4-yr follow up. Such limitations in recruiting study subjects may cause difficulties in generalizing study outcomes over all patients with the diseases concerned. However, the restriction on the number of visits was intended to ensure the accuracy of diagnosis and to allow the calculation of the COC Index in a structurally reasonable and meaningful manner (7, 8). Previous studies also found that the COC Index became more stable, or less subject to significant change as a result of minor perturbations in care dispersion, as the number of visits increased (7, 8). The exclusion of patients who had hospitalizations or emergency department visits during the first 3 yr of the 4-yr follow up may have led to a loss of information contained in raw data by not considering such hospitalizations or emergency department visits as outcome variables. Not considering continuity of care during the last year also may be an information-loss problem. Additionally, we only considered whether or not hospitalization or emergency department visits occurred during the last year regardless of the frequency; thus, we may not have seen the information contained in the raw data to evaluate the risk of hospitalization or emergency department visits (5). However, the exclusion of patients who died or had hospitalizations or emergency department visits during the first 3 yr of the 4-yr follow up was intended to reveal causality between the independent variable and the dependent variable (7). In the case of patients who died, it was not possible to identify whether the cause of their death was due to the disease concerned. Further, patients who had hospitalizations and emergency department visits represented only 1-2% of all study subjects.
Third, the analysis of disease severity in the study subjects with the adjustment for comorbidities may be insufficient. In an effort to minimize bias from other conditions, this study confined its analysis to ambulatory care visits and health outcomes (hospitalization and emergency department visits) caused by the diseases concerned (17, 27).
The fourth limitation of this study was the validity of diagnosis. Our study used the Korea National Health Insurance Claims Database, and the raw data were not prepared for research, but for insurance claims; thus, the validity of the diagnosis can be challenged. Kim, with the Korean Diabetes Association, obtained samples from patients who were diagnosed with diabetes mellitus from the Korea National Health Insurance Claims Database and investigated their medical records (28). He found that the proportion of patients who were verified as diabetes patients was 87.2% among hospitalized patients and 72.3% among ambulatory care patients (28). Given the problem of the validity of diagnosis, it is recommended that studies using administrative databases, such as the Korea National Health Insurance Claims Database, be used to limit study subjects to patients who used the outpatient service at least twice (29). In our study, patients who had four or more ambulatory care visits during the study period were selected. Thus, the validity of diagnosis may be of little concern in our study.
Fifth, we could not consider all of the factors affecting continuity of care and health outcomes. Our study only used the characteristics of patients that could be obtained from the Korea National Health Insurance Claims Database. As a result, our analysis of factors affecting continuity of care or the association between continuity of care and health care costs had a low R-square value (26, 27). Moreover, confounding variables were not fully considered when analyzing the association between continuity of care and the risk of hospitalization or emergency department visits. According to previous studies, continuity of care was affected by the characteristics of the health care providers (physician's age and gender, generalist or specialist, the period of clinic operation, etc.) as well as the characteristics of patients (5, 27). Health care satisfaction, the physician's understanding of patient's problems and the reliability of medical institutions were also shown to affect continuity of care (27). To collect such information, further qualitative studies using questionnaires or interviews with patients and health care providers are necessary (26). In previous studies, the kind of disability, insurance premium, and residence areas were also considered as confounding variables when analyzing the association between continuity of care and health outcomes (2, 5), whereas they were not considered in our study due to the limitation of our data. Such information can be obtained from the health insurance eligibility data, and further studies linking the eligibility data are required.
Sixth, the unit of continuity measured in this study was a medical institution, not a physician. The reason for defining a health care provider as a medical institution was because we could not identify the individual physician who provided health care service to a patient from the information available in the Korea National Health Insurance Claims Database. Our study, which measured continuity of care between medical institutions and patients, may be different from previous studies in other countries that explored continuity of care between individual physicians and patients (5). In particular, differences may be found in definitions of continuity of care between clinics in which solo practices are prevalent and all kinds of hospitals in which many physicians are working. Additionally, medical institution based analyses of continuity have a risk for exaggerating continuity of care at large-scale hospitals with many physicians. The COC Index used in this study was originally used to measure relationship continuity between physicians and patients. Nevertheless, considering the continuity of information, it is also meaningful to measure the continuity between medical institutions and patients with the COC Index. Further studies with identified individual physicians are necessary (5).
Finally, this study considered cases of hospitalization or emergency department visits with the disease concerned designated as a primary disease or a secondary disease in health insurance claims. These diseases, however, may act as a risk factor for worsening or developing related diseases, which can also cause hospitalization or emergency department visits to increase. Accordingly, it is uncertain whether hospitalization or emergency department visits, which were dependent variables in this study, were measured fairly. Further studies need to address hospitalization or emergency department visits caused by related diseases.
Despite these limitations, this study has some advantages. First, the study subjects were the total number of elderly patients in Korea who were first diagnosed with diabetes mellitus, hypertension, asthma, or COPD in 2002. Second, the analysis was conducted through a long-term follow up (4 yr). Many previous studies had limitations in proving causality because they were cross-sectional studies using one- or two-year claim data and took no account of past diagnosis experiences before observation started (2, 7). To address such limitations, this study followed patients, who were first diagnosed with the diseases concerned in 2002, for 4 yr. Third, this study is rare in that it confirms the association between continuity of care and health outcomes in the elderly population.
In conclusion, this study suggests that as health care utilization by a patient becomes more concentrated with the same provider, the risk of hospitalization or emergency department visits decreases and health care costs are reduced. It also indicates that increasing continuity of care may be a good strategy for promoting the efficient spending of health care budgets and enhancing the quality of health care for elderly patients in this aging society. Therefore, policy makers need to develop and try actively the program to improve the continuity of care in elderly patients with chronic diseases.
References
- 1.Health Care Cost Statistics 2008. Health Insurance Review & Assessment Service. 2008. [accessed on 4 Nov 2009]. Available at: http://www.hira.or.kr/common/dummy.jsp?pgmid=HIRAF010304010000.
- 2.Raddish M, Horn SD, Sharkey PD. Continuity of care: is it cost effective? Am J Manag Care. 1999;5:727–734. [PubMed] [Google Scholar]
- 3.Myers BA. A guide to medical care administration Vol. I: Concepts and principles. revised ed. Washington, D.C.: American Public Health Association, INC.; 1965. pp. 32–36. [Google Scholar]
- 4.Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. New York: Oxford University Press; 1998. p. 286. [Google Scholar]
- 5.Choi YJ, Kang SH, Kim YI. Association of higher continuity of primary care with lower risk of hospitalization among child and adolescent patients. Korean J Health Policy Adm. 2008;18:85–107. [Google Scholar]
- 6.Gill JM, Mainous AG, 3rd, Diamond JJ, Lenhard MJ. Impact of provider continuity on quality of care for persons with diabetes mellitus. Ann Fam Med. 2003;1:162–170. doi: 10.1370/afm.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gill JM, Mainous AG., 3rd The role of provider continuity in preventing hospitalizations. Arch Fam Med. 1998;7:352–357. doi: 10.1001/archfami.7.4.352. [DOI] [PubMed] [Google Scholar]
- 8.Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107:524–529. doi: 10.1542/peds.107.3.524. [DOI] [PubMed] [Google Scholar]
- 9.Weiss LJ, Blustein J. Faithful patients: the effect of long-term physician-patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1996;86:1742–1747. doi: 10.2105/ajph.86.12.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Worrall G, Knight J. Continuity of care for older patients in family practice: how important is it? Can Fam Physician. 2006;52:754–755. [PMC free article] [PubMed] [Google Scholar]
- 11.National Health Insurance Corporation. National Health Insurance Program of Korea. Seoul: Health Care Delivery System; 2007. p. 25. [Google Scholar]
- 12.Health Insurance Index 2007. Health Insurance Review & Assessment Service. [accessed on 15 May 2007]. Available at: http://www.hira.or.kr/ICSFiles/afieldfile/2008/03/04/DATA_2007.xls.
- 13.Shi L, Samuels ME, Pease M, Bailey WP, Corley EH. Patient characteristics associated with hospitalizations for ambulatory care sensitive conditions in South Carolina. South Med J. 1999;92:989–998. doi: 10.1097/00007611-199910000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Health Insurance Review & Assessment Service. 2009. Guidelines of Application for Health Care Cost Reimbursement - Review Application, Statement Form, and Completion Instructions. [Google Scholar]
- 15.Bice TW, Boxerman SB. A quantitative measure of continuity of care. Med Care. 1977;15:347–349. doi: 10.1097/00005650-197704000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Saultz JW. Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003;1:134–143. doi: 10.1370/afm.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim J, Kim H, Kim H, Min KW, Park SW, Park IB, Park JH, Baik SH, Son HS, Ahn CW, Oh JY, Lee S, Lee J, Chung CH, Choi KM, Choi I, Kim DJ. Current status of the continuity of ambulatory diabetes care and its impact on health outcomes and medical cost in Korea using National Health Insurance Database. Korean Diabetes J. 2006;30:377–387. [Google Scholar]
- 18.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 19.Thomas SD, Whitman S. Asthma hospitalizations and mortality in Chicago: an epidemiologic overview. Chest. 1999;116(4 Suppl 1):135S–141S. doi: 10.1378/chest.116.suppl_2.135s. [DOI] [PubMed] [Google Scholar]
- 20.Holguin F, Folch E, Redd SC, Mannino DM. Comorbidity and mortality in COPD-related hospitalizations in the United States, 1979 to 2001. Chest. 2005;128:2005–2011. doi: 10.1378/chest.128.4.2005. [DOI] [PubMed] [Google Scholar]
- 21.Magill MK, Senf J. A new method for measuring continuity of care in family practice residencies. J Fam Pract. 1987;24:165–168. [PubMed] [Google Scholar]
- 22.Patten RC, Friberg R. Measuring continuity of care in a family practice residency program. J Fam Pract. 1980;11:67–71. [PubMed] [Google Scholar]
- 23.Sloane P, Egelhoff C. The relationship of continuity of care to age, sex, and race. J Fam Pract. 1983;16:402, 404–405. [PubMed] [Google Scholar]
- 24.Fleming MF, Bentz EJ, Shahady EJ, Abrantes A, Bolick C. Effect of case mix on provider continuity. J Fam Pract. 1986;23:137–140. [PubMed] [Google Scholar]
- 25.Godkin MA, Rice CA. Relationship of physician continuity to type of health problems in primary care. J Fam Pract. 1981;12:99–102. [PubMed] [Google Scholar]
- 26.Hong JS, Kang HC, Kim J. Continuity of ambulatory care among adult patients with type 2 diabetes and its associated factors in Korea. Korean J Health Policy Adm. 2009;19:51–70. [Google Scholar]
- 27.Yoon CH, Lee SJ, Choo S, Moon OR, Park JH. Continuity of care of patient with diabetes and its affecting factors in Korea. J Prev Med Pub Health. 2007;40:51–58. doi: 10.3961/jpmph.2007.40.1.51. [DOI] [PubMed] [Google Scholar]
- 28.Kim J. Diabetes in Korea 2007. Seoul: Health Insurance Review & Assessment Service, Korean Diabetes Association; 2007. [Google Scholar]
- 29.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]