Abstract
Seroprevalence of the IgG antibodies for Clonorchis sinensis, Paragonimus westermani, Taenia solium metacestode (cysticercus), and Spirometra erinacei plerocercoid (sparganum) was measured using enzyme-linked immunosorbent assay (ELISA) in sera of patients in Korea from 1993 to 2006. A total of 74,448 specimens referred nationwide from 121 hospitals revealed an IgG positive rate of 7.6% for the 4 parasites. The IgG positive rate (18.7%) for the 4 parasites in 1993 decreased gradually to 6.6% in 2006. Individual positive rate decreased from 5.2% (1993) to 1.6% (2006) for C. sinensis, from 2.8% (1993) to 1.1% (2006) for P. westermani, from 8.3% (1993) to 2.2% (2006) for cysticercus, and from 2.6% (1993) to 1.6% (2006) for sparganum. The positive rate was highest (21.2%) in the group of patients who ranged in age from 50-59 yr old, and in the group that was referred from the Seoul area (55.9%). In conclusion, our results suggest that tissue invading parasitic infections should always be included in differential diagnosis for patients with eosinophilia associated lesions of the central nervous system, liver, and lungs in Korea.
Keywords: Seroepidemiologic Studies, Tissue Invading Parasitic Infections, Enzyme-Linked Immunosorbent Assay, Clonorchis sinensis, Paragonimus westermani, Taenia solium metacestode, Spirometra erinacei Plerocercoid
INTRODUCTION
In the past, parasitic infections were regarded as a major health problem in Korea. Before the 1970s, human parasitic infections, particularly soil-transmitted helminthiases, such as ascariasis, trichuriasis, and hookworm infections, were highly prevalent in the Korean population (1, 2). During the last three decades, prevalence of parasitic infections in Korea has decreased dramatically, largely due to nationwide control activities involving mass stool examination and selective mass treatment schemes for students (3).
However, in Korea, tissue invading parasitic infections remain relatively high compared to soil-transmitted parasitic infections. The infection rate of Clonorchis sinensis remains high along riverside areas, egg positive rate in Hamyang-gun was 16% and in Okcheon-gun was 14.2% (4). As ranges of freshwater crabs and crayfish have been rapidly reduced due to pollution of water bodies with environmental wastes, sources of human paragonimiasis infection have also diminished. In recent years, cases of clinical paragonimiasis have been found in a few patients after eating homemade "kejang" (5, 6). As for Taenia solium metacestode infection, the IgG positive rate was 4.0% in randomly-selected epilepsy patients. The positive rate (8.4%) was highest in patients living in Jeju-do (7).
Because the parasite-specific IgG antibody test using the ELISA method has been developed at our university since 1982, patients from hospitals nationwide are referred our hospital for diagnosis and monitoring of four tissue invading parasitic infections. The present study was conducted to determine the seroprevalence of IgG antibody against C. sinensis, Paragonimus westermani, T. solium metacestode, and sparganum by ELISA according to region, age, and clinical aspects in patients referred to Chung-Ang University Hospital from 1993 to 2006. We examined changes and trends associated with tissue invading parasitic infections in Korea.
MATERIALS AND METHODS
Subjects
A total of 74,448 specimens (4,943 patients were referred with serum and CSF together) were collected from patients (57,828 men and 16,620 women) suspected of having parasitic infections. From January 1993 to December 2006, patients were referred on a nationwide basis from 121 hospitals. Age of the subjected patients ranged 1 to 102 yr, with an average of 52±16.3 yr. Each age group of <10, 10-19, 20-29, 30-39, 40-49, 50-59, 60-69, and >70 yr-olds comprised 0.7%, 2.1%, 6.9%, 13.7%, 19.2%, 21.2%, 20.3%, and 15.8% of the referred cases. Clinical findings were as follows: neurologic (37.6%), pulmonary (17.9%), or gastrointestinal symptoms (1.1%), abnormal liver function test (12.9%), or eosinophilia (23.4%). Regionally, patients were referred from Seoul (53.6%), Gyeonggi-do (15.6%), Chungchungnam-do (4.5%), Chungcheongbuk-do (0.3%), Gyeongsangnam-do (1.7%), Gyeongsangbuk-do (1.5%), Jeollanam-do (2.1%), Jeollabuk-do (1.7%), Gangwon-do (1.9%), and Jeju-do (1.4%). The majority of cases were referred from general hospitals and commercial clinical laboratories.
Patients initially enrolled were included, and patients with follow-up tests were excluded. This study was approved by the Institutional Review Board of Chung-Ang University (IRB No. 10-005-01-01).
ELISA
IgG antibody levels against C. sinensis, P. westermani, T. solium metacestode, and sparganum in sera and cerebrospinal fluid (CSF) were measured using ELISA (8). Wells in the 96-well microtiter plate were coated with a protein concentration of 2.5 µg/mL in carbonate buffer (pH 9.6) overnight at 4℃. After washing, patient sera at a 1:100 dilution or undiluted CSF were added to each well and incubated for 2 hr at 36℃ in phosphate buffered saline/0.05% Tween 20 (PBS/T, pH 7.4). After washing, peroxidase-conjugated anti human IgG (Caltag Lab., South San Francisco, CA, USA) at 1:1,000 dilution in PBS/T was added and reacted for 2 hr at 36℃. Cutoff values for cases that were positive for serum and CSF were set at 0.25, 0.25, 0.18, and 0.22 for clonorchiasis, paragonimiasis, cysticercosis, and sparganosis, respectively (8-10). Cases that were positive for both serum and CSF were counted as one positive case.
Statistical analysis
Statistical analyses were performed using SPSS version 13.0 (SPSS, Chicago, IL, USA). A value of P<0.05 was considered statistically significant.
RESULTS
Positive rates of tissue-invading parasites
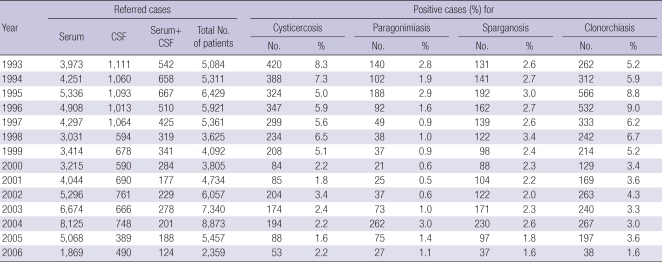
For all 74,448 specimens examined, cumulative positive rate for the 4 parasitic infections was 7.6%. Cross reactions observed included double positive (13%), triple positive (6%) and quadruple positive (1%). Positive rates for clonorchiasis, paragonimiasis, cysticercosis, and sparganosis were 5.0%, 1.4%, 4.2%, and 2.4%, respectively. Annual changes in the number of referred patients were not statistically significant (P=0.410), but the numbers were relatively large in 1995, 2003, and 2004 (Table 1). Males showed higher positive antibody rates than females (12.6% vs. 4.1%, P=0.001). Overall positive rates for parasites decreased from 18.7% in 1993 to 6.6% in 2006. The decreasing slope of the positive rate was the steepest in cysticercosis (decreased from 8.3% in 1993 to 2.2% in 2006). The positive rate of clonorchiasis decreased slowly from 5.2% in 1993 to 1.6% in 2006. Positive rates of sparganosis and paragonimiasis decreased from around 2.6% in 1993 to about 1.6% in 2006, but appeared to remain in plateau. The overall positive rate for sparganosis was higher than for paragonimiasis (Table 1).
Table 1.
Number of referred samples and seropositive rates for tissue invading parasitic infections from 1993 to 2006 in Korea
CSF, cerebrospinal fluid.
Positive rates in age groups
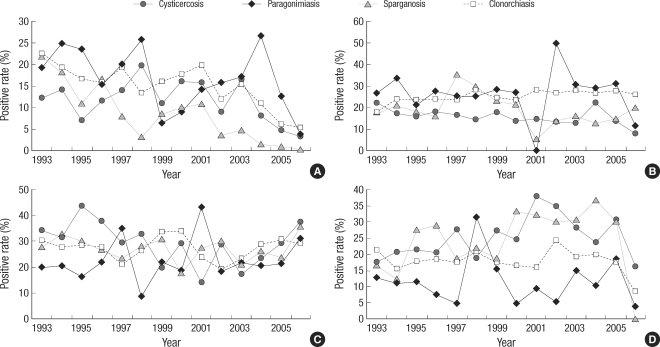
Overall antibody positive rates for the 4 parasites varied according to patient age group. The overall positive rate was the highest (26.5%) in patients who were in their fifties, followed by 21.7% in patients who were in their forties, and 19.5% in patients who were in their sixties. The antibody positive rate of clonorchiasis was higher than that of cysticercosis in patients in their thirties and forties, but this pattern was reversed in patients in their fifties and sixties. Since 2000, the positive rate for sparganosis has increased in patients in the over-forty age group, particularly for those in their sixties. For paragonimiasis, the positive rate increased from 2003 in patients in their fifties and sixties, and a high peak was observed in 2003 in patients in their thirties and forties. The overall positive rate for patients under twenty was similar to that of patients in their thirties, and that of patients over seventy was similar to that of patients in their sixties (Fig. 1).
Fig. 1.
Seropositive rates of the 4 parasitic infections by age groups. (A) 30-39 yr-old, (B) 40-49 yr-old, (C) 50-59 yr-old, and (D) 60-69 yr-old groups. The antibody positive rate of clonorchiasis was higher than that of cysticercosis in patients in their thirties and forties (A, B), but this pattern was reversed in patients in their fifties and sixties (C, D).
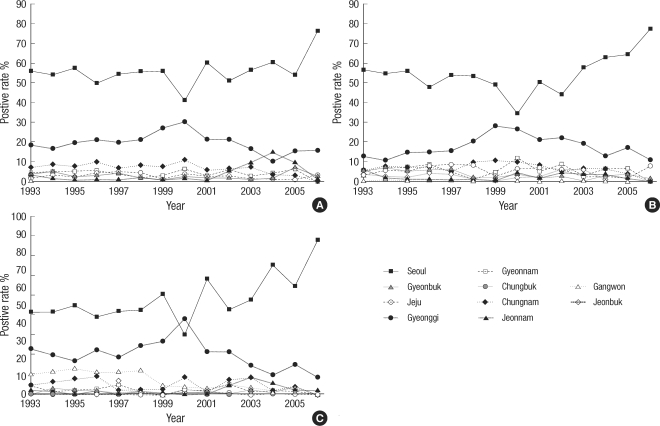
Positive rates by administrative region
Antibody positive rates for the 4 parasitic infections varied significantly according to the referred areas. The highest rate was observed in Seoul, followed in decreasing order by Gyeonggi-do, Chungcheongnam-do, and Jeollanam-do. Some differences in positive rates of parasitic infections were observed among these areas. The antibody positive rate for cysticercosis was higher in Chungcheongnam-do, followed by Gyeongsangnam-do. The positive rate of sparganosis was higher in Gangwon-do, followed by Chungcheongnam-do (Fig. 2).
Fig. 2.
Seropositive rates of parasitic infections according to the referred areas. (A) Total positive rate, (B) cysticercosis, and (C) sparganosis.
DISCUSSION
Due to successful control of soil-transmitted helminthiasis, both lay people and medical professionals in Korea often ignore the presence of parasitic agents of disease. A nationwide stool examination survey conducted in 2004 reported a total helminth egg positive rate of 3.7%, while egg positive rate for C. sinensis was 2.4% (11). Overall IgG antibody positive rates of clonorchiasis and paragonimiasis, 5.0% and 1.4% in the present study, were higher than the egg positive rates of the nationwide stool examination survey in 2004.
This difference could be explained by the following reasons. First, nationwide egg positive rates were obtained by examination of stools collected from randomly selected and representative Korean residents, whereas the present data was collected from patients referred by physicians due to clinically suspicious parasitic infections. Second, examination methods differed. Stool microscopy for eggs was a standard technique, not only in clinical diagnosis but also in epidemiological studies. However antibody tests, such as ELISA, were developed because egg examinations showed low sensitivity. For this reason our study showed higher positive rates than the national stool examination survey in 2004.
Cross reactions observed included double positive (13%), triple positive (6%), and quadruple positive (1%). After review of clinical findings from multiple positive cases, we decided which parasitic infection was the most probable. When radiological images, biopsy interpretation, and parasite collection for the cross-reacting case showed evidence of infection with a parasite, the case was diagnosed as a respective parasitic infection. However, it is obvious that serological cross reactions often cause serious problems with regard to the specificity of serological tests. This study was limited by its retrospective nature, and the inability to confirm cross reactive cases by other methods.
In the present study, the seropositive rate of clonorchiasis was 5.0% (1.6-9.0%) in total subjects, and markedly decreased during the years of observation. The most practical method of clonorchiasis prevention is avoidance of eating raw, freshly pickled, or undercooked freshwater fish. Due to the habit of eating raw fish, enforcement of this guideline for prevention is difficult. However, following continuous education and mass treatment, the status of clonorchiasis has shown significant improvement (12).
A previous serological survey reported that the positive rate of cysticercosis was 2.1% in normal subjects and 4% in patients with chronic epilepsy (7). In another serological study in Seoul, the positive rate of cysticercosis was reported as 3.0% (13). However, in the present study, the positive rate was found to be as high as 4.2%. In our study, the major cause for referral was neurologic problems, which may have been a reason for the high positive rate. Most neurocysticercosis could be diagnosed by computerized tomography (CT). Even by CT, however, many cases escaped recognition or findings were too ambiguous for a definitive diagnosis. For this reason, serological tests may provide valuable information. Therefore, it is already well known that criteria for diagnosis of cysticercosis should be established based on a combination of neuroimaging studies, serological tests, clinical presentation, and exposure history.
For the years 1993 and 1994, the positive rate for cysticercosis was higher than for other parasites, due to an especially high proportion of referrals for neurologic problems (47.7% in 1993 and 1994 vs. 35.4% in 1995-2006). Neurocysticercosis without extracranial infection may reveal a negative reaction when only serum is tested. In other words, T. solium metacestode specific IgG antibody did not cross over the blood-CSF barrier in a significant amount, even when the level was sufficiently high in blood. The ELISA test for detection of the specific IgG antibody using paired samples of serum and CSF was very helpful for clinical differentiation of neurocysticercosis from neurologic diseases of other causes (8).
Incidence of paragonimiasis has been significantly reduced, but new cases continue to occur sporadically. The present study revealed that the seropositive rate for paragonimiasis was 1.6%. The positive rate rose in 2003-2005, and subsided in 2006. During 2003-2005, referred cases with eosinophlia increased proportionally. Therefore, paragonimiasis should be included in differential diagnosis of parasitic disease in patients with lung lesions associated with eosinophilia and/or elevated IgE level.
Interestingly, seropositive rates for all 4 parasites were highest in Seoul area, even the rate for clonorchiasis was higher than that of the known endemic areas. Korea has recently become the entire nation into an one-day life zone, and has experienced changes in life style, advances in transportation, and people frequently move between the provinces and Seoul. Using this transportation system, many patients who lived in rural areas visited university hospitals and large scale hospitals locating in large cities such as Seoul and Busan. By this behavior pattern, a large proportion of referred patients were from the metropolitan Seoul and Gyeonggi-do, and pushed up IgG seropositive rates for all 4 parasites. Some differences were observed in the positive rates of the 4 parasitoses among the referred areas. The seropositive rate of cysticercosis was higher in Chungcheongnam-do, and that of sparganosis was higher in Gangwon-do. Positive rates of the other parasitoses were similar to those reported previously (14). However, our positive rates were not the exact meaning of regional positive rates because of our positive rates of referred areas.
In conclusion, our results suggest new cases have occurred sporadically and nationwidely. Therefore, tissue invading parasitic infections should always be included in the differential diagnosis for patients with eosinophilia associated lesions of the CNS, liver, and lung.
Footnotes
This research was supported by Chung-Ang University Research Grant 2010.
References
- 1.Seo BS, Rim HJ, Loh SH, Cho SY, Park SC, Bae JW, Kim JH, Lee JS, Koo BY, Kim KS. Study on the status of helminthic infections in Koreans. Korean J Parasitol. 1969;7:53–70. doi: 10.3347/kjp.1969.7.1.53. [DOI] [PubMed] [Google Scholar]
- 2.Kim CH, Park CH, Kim HJ, Chun HB, Min HK, Koh TY, Soh CT. Prevalence of intestinal parasites in Korea. Korean J Parasitol. 1971;9:25–38. doi: 10.3347/kjp.1971.9.1.25. [DOI] [PubMed] [Google Scholar]
- 3.Hong ST, Chai JY, Choi MH, Huh S, Rim HJ, Lee SH. A successful experience of soil-transmitted helminth control in the Republic of Korea. Korean J Parasitol. 2006;44:177–185. doi: 10.3347/kjp.2006.44.3.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cho SH, Lee KY, Lee BC, Cho PY, Cheun HI, Hong ST, Sohn WM, Kim TS. Prevalence of clonorchiasis in southern endemic areas of Korea in 2006. Korean J Parasitol. 2008;46:133–137. doi: 10.3347/kjp.2008.46.3.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shim YS, Cho SY, Han YC. Pulmonary paragonimiasis: a Korean perspectives. Sem Resp Med. 1991;12:35–45. [Google Scholar]
- 6.Cho SY, Kong Y, Kang SY. Epidemiology of paragonimiasis in Korea. Southeast Asian J Trop Med Public Health. 1997;28(Suppl 1):32–36. [PubMed] [Google Scholar]
- 7.Kong Y, Cho SY, Cho MS, Kwon OS, Kang WS. Seroepidemiological observation of Taenia solium cysticercosis in epileptic patients in Korea. J Korean Med Sci. 1993;8:145–152. doi: 10.3346/jkms.1993.8.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cho SY, Kim SI, Kang SY, Choi DY, Suk JS, Choi KS, Ha YS, Chung CS, Myung HJ. Evaluation of enzyme-linked immunosorbent assay in serological diagnosis of human neurocysticercosis using paired samples of serum and cerebrospinal fluid. Korean J Parasitol. 1986;24:25–41. doi: 10.3347/kjp.1986.24.1.25. [DOI] [PubMed] [Google Scholar]
- 9.Cho SY, Hong ST, Rho YH, Choi SY, Han YC. Application of micro-ELISA in serodiagnosis of human paragonimiasis. Korean J Parasitol. 1981;19:151–156. doi: 10.3347/kjp.1981.19.2.151. [DOI] [PubMed] [Google Scholar]
- 10.Kim H, Kim SI, Cho SY. Serological diagnosis of human sparganosis by means of micro-ELISA. Korean J Parasitol. 1984;22:222–228. doi: 10.3347/kjp.1984.22.2.222. [DOI] [PubMed] [Google Scholar]
- 11.Kim TS, Cho SH, Huh S, Kong Y, Sohn WM, Hwang SS, Chai JY, Lee SH, Park YK, Oh DK, Lee JK Working Groups in National Institute of Health and Korea Association of Health Promotion. A nationwide survey on the prevalence of intestinal parasitic infections in the Republic of Korea, 2004. Korean J Parasitol. 2009;47:37–47. doi: 10.3347/kjp.2009.47.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rim HJ. Clonorchiasis: an update. J Helminthol. 2005;79:269–281. doi: 10.1079/joh2005300. [DOI] [PubMed] [Google Scholar]
- 13.Lee SH, Kim MN, Back BY, Chai JY, Kim TH, Hwang YS. Analysis of parasite-specific antibody positive patients for Clonorchis sinensis, Paragonimus westermani, cysticercus and sparganum using ELISA. Korean J Lab Med. 2003;23:126–131. [Google Scholar]
- 14.Lee KJ, Bae YT, Kim DH, Deung YJ, Ryang YS. A seroepidemiologic survey for human sparganosis in Gangweon-do. Korean J Parasitol. 2002;40:177–180. doi: 10.3347/kjp.2002.40.4.177. [DOI] [PMC free article] [PubMed] [Google Scholar]