Abstract
Objective
Few studies have documented the incidence and significance of non-sustained hypotension in emergency department (ED) patients with sepsis. We hypothesized that ED non-sustained hypotension increases risk of in-hospital mortality in patients with sepsis.
Methods
Secondary analysis of a prospective cohort study. ED patients aged >17 years admitted to the hospital with explicitly defined sepsis were prospectively identified.
Inclusion criteria
Evidence of systemic inflammation (>1 criteria) and suspicion for infection. Patients with overt shock were excluded. The primary outcome was in-hospital mortality.
Results
Seven hundred patients with sepsis were enrolled, including 150 (21%) with non-sustained hypotension. The primary outcome of in-hospital mortality was present in 10% (15/150) of patients with non-sustained hypotension compared with 3.6% (20/550) of patients with no hypotension. The presence of non-sustained hypotension resulted in three times the risk of mortality than no hypotension (risk ratio = 2.8, 95% CI 1.5–5.2). Patients with a lowest systolic blood pressure <80 mmHg had a threefold increase in mortality rate compared with patients with a lowest systolic blood pressure ≥80 mmHg (5 vs. 16%). In logistic regression analysis, non-sustained hypotension was an independent predictor of in-hospital mortality.
Conclusion
Non-sustained hypotension in the ED confers a significantly increased risk of death during hospitalization in patients admitted with sepsis. These data should impart reluctance to dismiss non-sustained hypotension, including a single measurement, as not clinically significant or meaningful.
Keywords: Hypotension, Sepsis, Shock, Mortality, Emergency medicine
Introduction
Sepsis disrupts cardiovascular homeostasis through multiple mechanisms including dehydration, altered vasoregulation and distribution of blood flow, and variable effect on energy metabolism and mechanical contraction of heart [1]. With severe sepsis, the cumulative effect of these mechanisms results in arterial hypotension. From a taxonomic standpoint, hypotension per se is necessary but not sufficient to diagnose septic shock. Septic shock requires persistent arterial hypotension despite adequate volume resuscitation [2]. Many patients with recognized, overt septic shock are given vasopressor therapy. Large epidemiological studies have documented the association between septic shock and mortality [3–6]. In critical care settings, clinicians may be prone to believing that non-sustained hypotension does not have particular significance in terms of acuity of illness or outcome; however, no previous study has investigated the association between the presence, degree and duration of early hypotension in the absence of shock and outcome in sepsis. In the present study, we tested the hypothesis that in sepsis patients without overt shock, the presence of non-sustained SBP < 100 mmHg in the emergency department (ED) will be associated with an increased incidence of in-hospital mortality when compared to patients with sepsis and no hypotension.
Methods
Study setting and subjects
We performed a secondary analysis of a prospective cohort of patients admitted from the ED of a single, large urban teaching hospital with >100,000 patient visits per year. The study was reviewed and approved by the Institutional Review Board and Privacy Board at Carolinas Medical Center.
The method of subject enrollment and data collection has been described in detail elsewhere [7]. Briefly, the cohort consisted of adults (>17 years) who were admitted to the hospital from the ED and had criteria for sepsis including: (1) high suspicion of infection evidenced by administration of antibiotics in the ED; (2) at least two criteria for systemic inflammation in response to the infection as defined by Levy et al. [2]. Patients were not enrolled if they had trauma in the previous 24 h or if no vital signs were recorded in the ED. Enrollment occurred from July 2004 through June 2005. Data collected included chief complaint, co-morbidities, all vital signs with times of measurement, and all therapies administered in the ED. Hospital vital status was determined through a query of the hospital clinical database (HBOC Star Navigator, McKesson, San Francisco, CA).
Outcome measures and data analysis
The primary outcome measure was in-hospital mortality. To determine the significance of non-sustained hypotension on mortality among patients without shock, we excluded patients with overt shock (hypotension present for ≥60 consecutive minutes or vasopressor administration). The remaining patients were categorized into two groups: (1) non-sustained hypotension defined as one or more occurrence of systolic blood pressure (SBP) < 100 mmHg; or (2) no hypotension (all SBP > 100 mmHg in the ED). We then calculated the risk ratio (RR) for the primary outcome of death by dividing the cumulative incidence in the non-sustained hypotension group by that of the group with no hypotension. Secondary outcomes evaluated included the relationship between the duration and decile of lowest documented ED systolic blood pressure and in-hospital mortality. The duration of ED hypotension was determined by dividing patients into two groups: (1) transient—only one documented SBP < 100 mmHg; (2) episodic—more than one documented SBP < 100 mmHg that was non-sustained (present for less than 60 continuous minutes) and not requiring intervention with vasopressors [7–9].
Odds ratios (OR) were calculated in order to determine independent predictors of in-hospital death using multivariate logistic regression with 95% confidence intervals (Online Supplement A). In the logistic regression analysis, organ dysfunction was defined according to any abnormality in the individual criteria included in the sequential organ failure assessment (SOFA) score [10].
Continuous data are presented as means or medians, while categorical data are presented as proportions and 95% confidence interval (CI). Data were compared using t tests, Mann–Whitney U test, or Chi-square test where appropriate. For all statistical testing, P < 0.05 was considered significant and analyses were performed using StatsDirect (version 2.6.6, Cheshire, UK).
Results
A total of 774 patients met inclusion criteria for sepsis. Seventy-four patients had overt shock (55 with sustained hypotension and 19 requiring vasopressors) and were excluded from the analysis. The remaining 700 subjects were analyzed of which 150 (21%) had non-sustained hypotension and 550 had no hypotension. The clinical and demographic characteristics of each group are shown in Table 1.
Table 1.
Patient demographics and clinical characteristics
| Variable | No hypotension (N = 550) |
Non-sustained hypotension (N = 150) |
P value |
|---|---|---|---|
| Age (years)a | 53 ± 19 | 56 ± 20 | 0.119 |
| Female (%) | 47 (42–51) | 53 (44–61) | 0.23 |
| Caucasian (%) | 43 (39–47) | 47 (40–56) | 0.35 |
| African American (%) | 52 (48–56) | 43 (35–51) | 0.04 |
| Hispanic (%) | 4 (2–6) | 8 (4–14) | 0.04 |
| Lowest SBP (mmHg)a | 127 ± 42 | 90 ± 8 | <0.0001 |
| Highest pulse (beats/min)a | 110 ± 19 | 112 ± 20 | 0.31 |
| Number of SIRS criteriab | 3 (2–3) | 3 (2–3) | 0.005 |
| ICU admission (%) | 18 (15–21) | 30 (23–38) | 0.0013 |
| HIV positive (%) | 9 (7–12) | 10 (6–16) | 0.73 |
| Active malignancy (%) | 7 (5–10) | 5 (2–9) | 0.29 |
| Hypertension (%) | 41 (37–45) | 33 (26–41) | 0.08 |
| Diabetes mellitus (%) | 23 (19–27) | 27 (20–35) | 0.28 |
| Cirrhosis (%) | 5 (3–7) | 5 (2–9) | 0.83 |
| Coronary artery disease (%) | 10 (8–13) | 13 (8–19) | 0.35 |
| Congestive heart failure (%) | 9 (7–12) | 11 (6–17) | 0.56 |
| SAPS II scoreb | 20 (13–27) | 29 (22–35) | <0.0001 |
| Crystalloid administereda | 840 ± 840 | 1240 ± 1140 | 0.0001 |
| Hospital daysb | 4 (3–7) | 5 (3–10) | 0.004 |
| Number of SBP measurementsb | 3 (2–4) | 5 (3–9) | <0.0001 |
Values are expressed as amean ± standard deviation or bmedian and inter-quartile ranges for continuous variables or percentages and 95% confidence intervals for dichotomous variables. HIV status, active malignancy, hypertension, diabetes, liver disease, coronary artery disease and congestive heart failure were all patient-reported diagnoses at time of hospitalization. Data were compared using t tests, Mann–Whitney U test, or Chi-square test where appropriate
SBP systolic blood pressure, min minute, mmHg millimeters of mercury, SIRS systemic inflammatory response syndrome, ICU intensive care unit, HIV human immunodeficiency syndrome, SAPS simplified acute physiologic score
The incidence of death in the non-sustained hypotension group was 10% (15/150) and 3.6% (20/550) in the no hypotension group (proportion difference 6.4%, 95% CI 2–12%). Patients in the non-sustained group had three times the risk of in-hospital death mortality than did patients in the no-hypotension group (RR = 2.8; 95% CI 1.5–5.2).
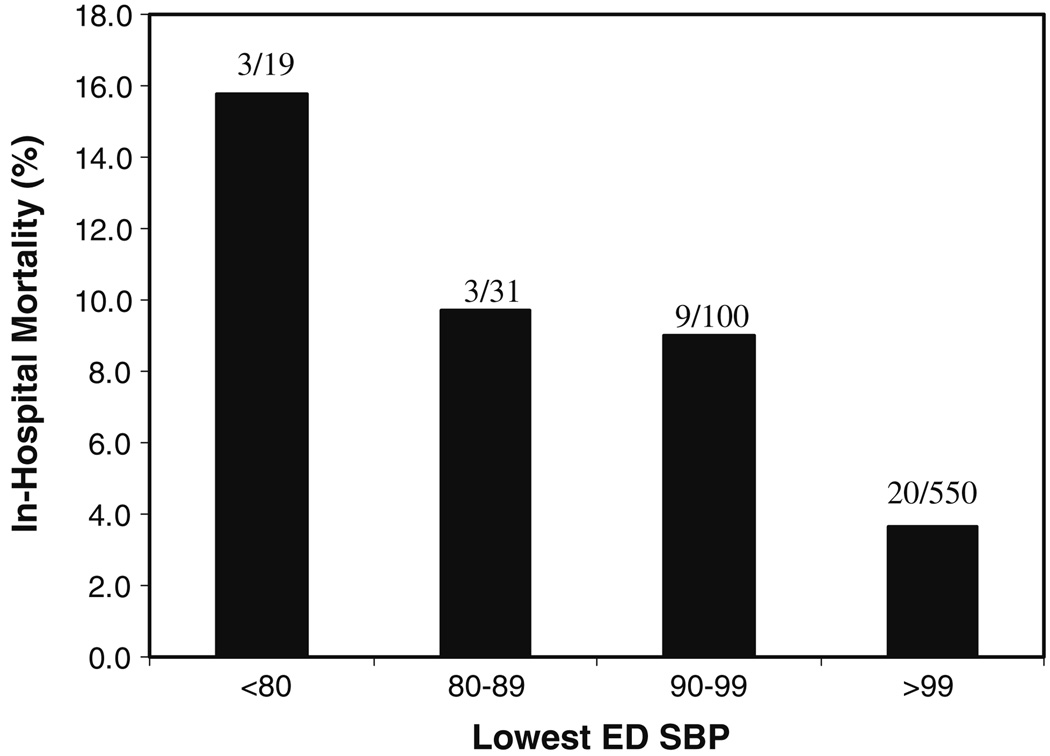
Patients with hypotension manifested an inverse relationship between the nadir of the ED systolic blood pressure and the frequency of in-hospital death (Fig. 1). Patients with a lowest systolic blood pressure <80 mmHg had a threefold increase in mortality rate compared with patients with a lowest systolic blood pressure ≥80 mmHg (5 vs. 16%). When the duration of hypotension was examined, the mortality rate among subjects with transient hypotension (8/86; 9%) and episodic hypotension (7/64; 11%) was not significantly different.
Fig. 1.
Relationship between the lowest ED systolic blood pressure and in-hospital mortality (N = 700). ED emergency department, SBP systolic blood pressure (mmHg)
Multivariate logistic regression analysis was conducted in order to assess the independent predictive value of hypotension on in-hospital mortality when controlling for other organ dysfunctions. The presence of hypotension was a significant independent predictor of death (Table 2).
Table 2.
Results of logistic regression analysis for the endpoint of in-hospital mortality
| Variable | OR | 95% CI |
|---|---|---|
| Hypotension | 2.7 | 1.2–5.8 |
| Respiratory dysfunction | 1.4 | 0.5–2.9 |
| CNS dysfunction | 2.3 | 0.6–5.8 |
Hypotension is defined as occurrence of transient or episodic hypotension; organ dysfunction was defined according to the sequential organ failure assessment (SOFA) score. Model analysis: Pearson Chi-square goodness of fit = 2.184797, df = 4, P = 0.7018; deviance goodness of fit = 2.976413, df = 4, P = 0.5618; Hosmer–Lemeshow test = 0.352313, df = 2, P = 0.8385
OR odds ratio, CI confidence interval, CNS central nervous system
Discussion
In this study, we document the association between cardiovascular dysfunction and in-hospital death in patients with sepsis but without clinically obvious shock. In a large sample of well-defined subjects with sepsis identified in the ED, non-sustained hypotension was associated with a threefold increase risk of death in the hospital.
The importance of the findings we report lies in their simplicity. The use of blood pressure measurements is one of the most common and fundamental methods of both assessing physiologic stability and communicating severity of illness among medical care providers. In patients with sepsis, the presence of non-sustained systolic blood pressure of <100 mmHg results in a marked increase in risk of death. Thus, our findings give clinicians a simple, routinely measured and widely available marker to indicate the presence of higher illness severity.
An important finding in our study is the statistically similar incidence of death across both the transient and episodic hypotension groups. In this study, a patient who had any non-sustained hypotension, even a single measurement, was subject to an approximately 2.5–3-fold increase risk of in-hospital mortality. We believe clinicians should consider any hypotension in the setting of sepsis to herald worse outcome. This knowledge should, therefore, impart reluctance to dismiss non-sustained hypotension, including a single measurement, as not clinically significant or meaningful.
Another important finding in our study was the relationship between the depth of hypotension and death. The lower the nadir of blood pressure the higher the mortality rate observed. This suggests a dose–response relationship between blood pressure and outcome. Patients who had lowest systolic blood pressure of <80 mmHg had a 16% rate of in-hospital death, which is more than three times higher than if the lowest blood pressure was ≥80 mmHg. This provides important information to clinicians suggesting that not only the presence of hypotension marks severity but also the lowest blood pressure provides additional important prognostic information.
While the association between septic shock and mortality has been previously established [3–6], to our knowledge, this is the first report to document the association between documented non-sustained hypotension (hypotension without overt shock) and higher mortality. This finding highlights the importance of clinicians carefully considering the importance of overt manifestations of cardiovascular dysfunction (hypotension), particularly in clinical scenarios in which obvious intervention, such as starting vasopressors, is not indicated.
This report has several important limitations that should be considered. First, this report is from a single urban tertiary center which may limit the generalizability. Second, we only document an association between hypotension and death and thus a cause and effect relationship has not been demonstrated. Third, this study did not investigate the potential clinical response to the presence of hypotension and thus it is unknown if a measured response to this abnormality would result in changes in patient-oriented outcomes. Fourth, the blood pressure measurements analyzed in this study were only those that were recorded and thus measurements that were potentially performed but not recorded were not considered in our data. Additionally, almost all of the blood pressure measurements we used were taken via automated cuff sphygmomanometer, which may be somewhat inaccurate at the extremes (high or low) of measurement. Finally, this study was conducted in 2004 and 2005, when visibility on new treatments for sepsis was emerging [11]. It is unknown if changes in practice patterns potentially associated with new treatment recommendations could effect our data.
Although blood pressure is routinely measured in the treatment of patients with infection, this is the first large study to systematically document the value in considering non-sustained hypotension for the prediction of in-hospital death in ED patients with sepsis. We found that non-sustained hypotension confers significantly increased risk of death during hospitalization. The more severe the hypotension the higher the risk of death.
Supplementary Material
References
- 1.Parrillo JE. Pathogenetic mechanisms of septic shock. N Engl J Med. 1993;328:1471–1477. doi: 10.1056/NEJM199305203282008. [DOI] [PubMed] [Google Scholar]
- 2.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G SCCM/ESICM/ACCP/ATS/SIS. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med. 2003;29:530–538. doi: 10.1007/s00134-003-1662-x. [DOI] [PubMed] [Google Scholar]
- 3.Guidet B, Aegerter P, Gauzit R, Meshaka P, Dreyfuss D on behalf of the CUB-Rea Study Group. Incidence and impact of organ dysfunctions associated with sepsis. Chest. 2005;127:942–951. doi: 10.1378/chest.127.3.942. [DOI] [PubMed] [Google Scholar]
- 4.Silva E, Pedro M, Sogayar ACB, Mohovic T, Silva CL, Janiszewski M, Cal RG, de Sousa EF, Abe TP, de Andrade J, de Matos JD, Rezende E, Assuncao M, Avezum A, Rocha PCS, de Matos GFJ, Bento AM, Correa AD, Vieira PCBKE. Brazilian sepsis epidemiological study (BASES study) Crit Care. 2004;8:R251–R260. doi: 10.1186/cc2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The EPISEPSIS Study Group. EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med. 2004;30:580–588. doi: 10.1007/s00134-003-2121-4. [DOI] [PubMed] [Google Scholar]
- 6.Brun-Buisson C, Doyon F, Carlet J, Dellamonica P, Gouin F, Lepoutre A, Mercier J-C, Offenstadt G, Regnier B for the French ICU Group for Severe Sepsis. Incidence, risk factors, and outcome of severe sepsis and septic shock in adults. A multicenter prospective study in intensive care units. JAMA. 1995;274:968–974. [PubMed] [Google Scholar]
- 7.Jones AE, Yiannibas V, Johnson CL, Kline JA. Emergency department hypotension predicts sudden unexpected in-hospital mortality: a prospective cohort study. Chest. 2006;130:941–946. doi: 10.1378/chest.130.4.941. [DOI] [PubMed] [Google Scholar]
- 8.Jones AE, Stiell IG, Nesbitt LP, Spaite DW, Hasan N, Watts BA, Kline JA. Nontraumatic out-of-hospital hypotension predicts inhospital mortality. Ann Emerg Med. 2004;43:106–113. doi: 10.1016/j.annemergmed.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Jones AE, Aborn LS, Kline JA. Severity of emergency department hypotension predicts adverse hospital outcome. Shock. 2004;22:410–414. doi: 10.1097/01.shk.0000142186.95718.82. [DOI] [PubMed] [Google Scholar]
- 10.Vincent JL, Moreno R, Takala J, Willats S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (Sepsis-related organ failure assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 11.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent J-L. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Intensive Care. 2008;34:17–60. doi: 10.1007/s00134-007-0934-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.