Abstract
OBJECTIVE
To examine the impact of birth at night, on the weekend, and during July or August – the first months of the academic year – and the impact of resident duty-hour restrictions on mortality and morbidity of VLBW infants.
METHODS
Outcomes were analyzed for 11,137 infants with birth weight 501–1250 grams enrolled in the NICHD Neonatal Research Network registry 2001–2005. Approximately half were born before the introduction of resident duty-hour restrictions in 2003. Follow-up assessment at 18–22 months was completed for 4,508 infants. Mortality (7-day and 28-day), short-term morbidities, and neurodevelopmental outcome were examined with respect to the timing of birth: night vs day, weekend vs weekday, and July or August vs other months, and after vs before implementation of resident duty-hour restrictions.
RESULTS
There was no effect of hour, day, or month of birth on mortality and no impact on the risks of short-term morbidities except the risk of ROP requiring operative treatment was lower for infants born during the late night hours than during the day. There was no impact of timing of birth on neurodevelopmental outcome except the risk of hearing impairment or death was slightly lower among infants born in July or August compared with other months. The introduction of resident and fellow duty-hour restrictions had no impact on mortality or neurodevelopmental outcome. The only change in short-term morbidity after duty-hour restrictions were introduced was an increase in the risk of ROP (stage 2 or higher).
CONCLUSION
In this network of academic centers, the timing of birth and the introduction of duty-hour restrictions had little effect on the risks of mortality and morbidity of VLBW infants, suggesting that staffing patterns were adequate to provide consistent care.
Keywords: Neonatal, preterm infants, morbidity/mortality, resident education/training, workforce
INTRODUCTION
The delivery of consistently high-quality care regardless of hour, day, and month is a priority in health care systems, including intensive care units. Physician staffing patterns in intensive care units vary with time of day and day of the week. The physicians on duty in the hospital at night and on weekends are fewer in number and generally less experienced. In teaching hospitals, the academic year begins in July. New physicians begin working in the summer, and the clinical experience of these young physicians is lowest in July and August. Previous studies have suggested that the timing of birth has significant effects on the risks of perinatal and neonatal mortality, but these findings have not been consistent when comparing day versus night,1–14 weekday versus weekend,1,2,5,15–20 and July and August versus the rest of the year.5,21,22
Most studies have focused on overall perinatal or neonatal mortality, with few analyses of the effects of timing of birth on the mortality risk of very-low-birth-weight (VLBW) infants,1,12,21,22 the group at greatest risk of mortality. Even less is known about the impact of timing of birth on morbidity among surviving VLBW infants.12,14,22 If significant effects of timing of birth on mortality and morbidity were demonstrated, this would suggest potentially modifiable factors, such as staffing policies and delivery room management, that could be addressed with the goal of improving outcomes. The impact of timing of birth on outcome is particularly important at a time of continued national discussion on the topic of optimal resident duty hours for patient safety and physician training.23,24
We evaluated the impact of timing of birth on the mortality and morbidity of VLBW infants born in centers of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network (NRN) from 2001 through 2005. We also compared outcomes for these infants before and after introduction of resident duty-hour restrictions, as mandated by the Accreditation Council for Graduate Medical Education (ACGME) in 2003.25
METHODS
Study Population
The infants studied were born at one of the NRN centers between January 1, 2001 and December 31, 2005 with birth weight 501–1250 grams and were enrolled in a registry of VLBW infants maintained by the NRN. This was the largest recent time span available for which the same versions of the registry data forms were used. The parents of surviving infants with birth weight 1000 grams or less were asked to bring their children for follow-up evaluation at 18 to 22 months corrected age. Infants with birth weight 1001–1250 grams did not participate in the follow-up evaluations. Centers with multiple hospitals were considered as single entities except for one center where the usual composition of teams attending newborn infants at delivery differed between its two hospitals; thus, 17 delivery sites were included in the analysis. The registry was approved by the institutional review board at each center. Informed consent for collecting data for the registry was waived by the institutional review boards at all but one site, where consent was obtained. Written informed consent was obtained for the follow-up evaluation at all sites.
Outcomes and Definitions
Data collected included pregnancy complications, type of delivery, multiple birth, infant birth weight (BW), gestational age (GA), sex, race, Apgar scores, and in-hospital morbidities including necrotizing enterocolitis (NEC), late-onset sepsis, bronchopulmonary dysplasia (BPD), intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL), and retinopathy of prematurity (ROP). BPD was defined as the need for supplemental oxygen at 36 weeks postmenstrual age. NEC was defined as Bell’s stage IIA or higher.26 Late-onset sepsis was defined by positive blood culture after the age of 72 hours with antibiotic therapy for 5 days or more. Infants were defined as small for gestational age (SGA) if their BW was below the 10th percentile for sex and GA.27
Centers were surveyed to identify the date when resident and fellow duty-hour restrictions were implemented. Fourteen centers implemented resident duty-hour restrictions on July 1, 2003; two centers implemented restrictions earlier and one later.
The follow-up visit included assessment of cognitive and neuromotor development using a standardized neurologic examination and the Bayley Scales of Infant Development-II.28 Bayley scale scores were recorded for the Mental Developmental Index (MDI) and the Psychomotor Developmental Index (PDI). The results of vision and hearing examinations were noted. A composite outcome, neurodevelopmental impairment (NDI), was defined as one or more of the following: MDI<70, PDI<70, moderate or severe cerebral palsy (CP), blindness with no useful vision in either eye, or hearing aid use in both ears.
Timing of birth variables were defined as:
Birth hour: Day (08:00–17:00), early night (17:01–23:59), or late night (00:00–07:59);
Day of the week: Saturday or Sunday versus Monday-Friday;
Month: July or August versus other months;
Epoch: Before implementation of resident and fellow duty-hour restrictions versus after implementation of duty-hour restrictions.
Statistical Analysis
Associations between each timing of birth variable and mortality within 7 days and 28 days of birth were examined in the entire cohort and separately within three birth weight groups: 501–750 grams, 751–1000 grams, and 1001–1250 grams.
We examined associations between timing of birth and each of the following short-term morbidities and with composite outcomes of each morbidity or death: NEC, late-onset sepsis, BPD, IVH or PVL, ROP stage 2 or higher, and ROP requiring operative treatment. Among surviving infants with birth weight 501–1000 grams who returned for follow-up examination at 18–22 months corrected age, the impact of timing of birth was examined on the composite outcome of NDI or death and for each of the component measures of NDI with death in composite outcomes.
Statistical significance for unadjusted comparisons was determined by chi-square or Fisher’s exact test. Adjusted associations between timing of birth and outcomes were examined with robust Poisson regression models using generalized estimating equations.29 Adjusted relative risks and 95% confidence intervals were reported based on the estimates and variance estimators from these models; statistical significance was determined by Score and Wald tests. Characteristics examined in group comparisons and included as adjustment variables in the models were selected from prenatal and postnatal variables collected shortly after birth that have been associated with mortality.30 Along with each of the timing of birth variables defined above, covariates included in each model were study center, infant BW group, GA (≤24 wk, 25–28 wk, or ≥29 wk), sex, race, maternal antepartum hemorrhage, maternal hypertension or preeclampsia-eclampsia, multiple birth, and 1-minute Apgar score <5. A continuous time variable with each unit change representing 6 months was included in order to adjust for time trends over the period of the study.
Initial models fit to each outcome included interaction terms aimed at examining whether timing of birth effects or general time trends varied by epoch. Interactions were not significant and were omitted from the final models. No adjustment was made for multiple comparisons.
RESULTS
During the period of study, 11,679 infants were born in 19 NRN study centers with birth weight 501–1250 grams and enrolled in the VLBW registry. Of these, 511 infants with major congenital anomalies, 28 infants from two centers that left the Network early in the period, and 3 infants with missing time of birth were excluded. Thus, the cohort studied included 11,137 infants from 17 centers.
Overall, 40% of infants were born during the day, 32% during early night, and 28% during late night. Infants born at night were of lower BW and GA than those born in the day, and a higher percentage had Apgar scores < 5 at 1 minute and 5 minutes (Table 1). A greater proportion of infants born during the day were from multiple births or SGA and more were white. Mothers of infants born in the night were less likely to have had hypertension or preeclampsia-eclampsia and to have had Cesarean section delivery. A greater percentage of mothers who delivered in the late night had an antepartum hemorrhage.
TABLE 1.
Maternal and neonatal characteristics among infants 501–1250 grams birth weight by timing of birth
| Hour of Birtha | Day of Birth | Month of Birth | Before or After Duty-Hour Restrictionsb |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Late Night N=3128 |
Early Night N=3578 |
Day N=4431 |
P- valuec |
Saturday or Sunday N=2982 |
Monday- Friday N=8155 |
P- value |
July or August N=1897 |
Other Month N=9240 |
P- value |
Before N=5290 |
After N=5847 |
P- value |
||||||||||
|
Maternal Characteristicd | ||||||||||||||||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |||||
| Antepartum hemorrhage | 590 | (19) | 570 | (16) | 698 | (16) | <0.001 | 516 | (17) | 1342 | (16) | 0.3 | 306 | (16) | 1552 | (17) | 0.5 | 822 | (16) | 1036 | (18) | 0.002 |
| Hypertension or preeclampsia-eclampsia | 705 | (23) | 1011 | (28) | 1402 | (32) | <0.001 | 810 | (27) | 2308 | (28) | 0.3 | 496 | (26) | 2622 | (28) | 0.053 | 1404 | (27) | 1714 | (29) | 0.001 |
| Cesarean section | 1714 | (55) | 2316 | (65) | 2984 | (67) | <0.001 | 1796 | (60) | 5218 | (64) | <0.001 | 1213 | (64) | 5801 | (63) | 0.4 | 3192 | (60) | 3822 | (65) | <0.001 |
|
Neonatal Characteristice | ||||||||||||||||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |||||
| Multiple birth | 736 | (24) | 903 | (25) | 1233 | (28) | <0.001 | 724 | (24) | 2148 | (26) | 0.03 | 519 | (27) | 2353 | (25) | 0.09 | 1392 | (26) | 1480 | (25) | 0.2 |
| BW (grams) | ||||||||||||||||||||||
| 501–750 | 1082 | (35) | 1164 | (33) | 1341 | (30) | 0.002 | 958 | (32) | 2629 | (32) | 0.4 | 605 | (32) | 2982 | (32) | 0.7 | 1766 | (33) | 1821 | (31) | 0.2 |
| 751–1000 | 971 | (31) | 1169 | (33) | 1501 | (34) | 1014 | (34) | 2627 | (32) | 643 | (34) | 2998 | (32) | 1660 | (31) | 1981 | (34) | ||||
| 1001–1250 | 1075 | (34) | 1245 | (35) | 1589 | (36) | 1010 | (34) | 2899 | (36) | 649 | (34) | 3260 | (35) | 1864 | (35) | 2045 | (35) | ||||
| GA (weeks) | ||||||||||||||||||||||
| ≤24 | 739 | (24) | 743 | (21) | 804 | (18) | <0.001 | 603 | (20) | 1683 | (21) | 0.04 | 398 | (21) | 1888 | (20) | 0.3 | 1096 | (21) | 1190 | (20) | 0.3 |
| 25–28 | 1721 | (55) | 1985 | (56) | 2442 | (55) | 1710 | (57) | 4438 | (54) | 1061 | (56) | 5087 | (55) | 2946 | (56) | 3202 | (55) | ||||
| 29–32 | 618 | (20) | 798 | (22) | 1096 | (25) | 640 | (21) | 1872 | (23) | 400 | (21) | 2112 | (23) | 1152 | (22) | 1360 | (23) | ||||
| ≥33 | 49 | (2) | 50 | (1) | 89 | (2) | 28 | (1) | 160 | (2) | 37 | (2) | 151 | (2) | 94 | (2) | 94 | (2) | ||||
| SGA | 385 | (12) | 591 | (17) | 847 | (19) | <0.001 | 422 | (14) | 1401 | (17) | <0.001 | 286 | (15) | 1537 | (17) | 0.1 | 871 | (16) | 952 | (16) | 0.8 |
| Male | 1627 | (52) | 1827 | (51) | 2228 | (50) | 0.3 | 1567 | (53) | 4115 | (50) | 0.054 | 972 | (51) | 4710 | (51) | 0.8 | 2714 | (51) | 2968 | (51) | 0.6 |
| Race | ||||||||||||||||||||||
| Black | 1292 | (41) | 1455 | (41) | 1741 | (39) | 0.002 | 1247 | (42) | 3241 | (40) | 0.3 | 765 | (40) | 3723 | (40) | 0.5 | 2159 | (41) | 2329 | (40) | <0.001 |
| White | 1100 | (35) | 1310 | (37) | 1752 | (40) | 1073 | (36) | 3089 | (38) | 696 | (37) | 3466 | (38) | 1979 | (37) | 2183 | (37) | ||||
| Hispanic | 573 | (18) | 656 | (18) | 728 | (16) | 519 | (17) | 1438 | (18) | 335 | (18) | 1622 | (18) | 961 | (18) | 996 | (17) | ||||
| Other | 161 | (5) | 149 | (4) | 208 | (5) | 141 | (5) | 377 | (5) | 101 | (5) | 417 | (5) | 189 | (4) | 329 | (6) | ||||
| Apgar at 1 minute <5 | 1443 | (46) | 1550 | (44) | 1816 | (41) | <0.001 | 1307 | (44) | 3502 | (43) | 0.4 | 855 | (45) | 3954 | (43) | 0.06 | 2282 | (43) | 2527 | (43) | 0.9 |
| Apgar at 5 minutes <5 | 599 | (19) | 567 | (16) | 607 | (14) | <0.001 | 489 | (16) | 1284 | (16) | 0.4 | 317 | (17) | 1456 | (16) | 0.3 | 849 | (16) | 924 | (16) | 0.7 |
Late night refers to the period from 00:00 to 07:59, early night from 17:01 to 23:59, and day from 08:00 to 17:00
Duty-hour restrictions were implemented on July 1, 2003 at most NRN centers. See Methods for more information.
P-value for a difference between groups by Fisher’s exact test, chi-square test of general association, or for ordinal outcomes (e.g. BW, GA), the Mantel-Haenszel chi-square test for ordinal trends
Information was missing for antepartum hemorrhage (11 infants), maternal hypertension or preeclampsia-eclampsia (10), and Cesarean delivery (9).
Information was missing for GA (3 infants), SGA (3), sex (2), race (12), Apgar score at 1 minute (54), and Apgar score at 5 minutes (49).
Infants born on Saturday or Sunday were of somewhat lower GA than those born during the week, and a smaller percentage were SGA, from a multiple birth, or delivered by Cesarean section. BW and the percent of infants with Apgar scores <5 at 1 minute and 5 minutes were similar for infants born on the weekend and those born during the week.
No significant difference was found between infants born in July or August and those born in other months in any of the maternal and neonatal characteristics examined.
Neonatal characteristics were similar for infants born before and after the duty-hour restrictions were implemented. Mothers of infants born during the years after the restrictions were introduced were more likely to have had antepartum hemorrhage, hypertension or preeclampsia-eclampsia, and Cesarean delivery.
Mortality
Mortality within 7 days of birth
Overall, 1,284 (11.5%) infants died in the first 7 days of life; 165 of these died after 72 hours. The most frequently cited cause of death was immaturity (43%); the second-most common was RDS (32%). Seven-day mortality was stable across the period of study with the proportion of infants who died ranging from 10.7% to 12.3%.
After adjusting for maternal and neonatal characteristics and time trends, no significant difference in 7-day mortality risk was found for late night compared to day births (adjusted RR 1.07, 95% CI 0.96–1.18), nor for early night compared to day births (adjusted RR 1.01, 95% CI 0.90–1.13) (Table 2). Similarly, no significant difference was found in 7-day mortality risk for infants born on Saturday or Sunday compared to those born on other days of the week, nor for infants born in July or August versus those born in other months. No significant change in the risk of dying in the first 7 days of life was found after resident-fellow duty-hour restrictions were implemented compared to before (adjusted RR 0.99, 95% CI 0.84–1.19). Within each of the three birth weight groups, there was no significant effect of timing of birth on the adjusted risk of mortality within the first 7 days.
TABLE 2.
Relative risk of death in the first 7 days among infants 501–1250 grams birth weight by timing of birth
| Timing of birth | N | Death in 7 days |
Adjusted RR (95% CI)a |
P- valuea |
|---|---|---|---|---|
| Birth hour | ||||
| Late night | 3128 | 427 (14%) | 1.07 (0.96–1.18) | 0.4 |
| Early night | 3578 | 405 (11%) | 1.01 (0.90–1.13) | |
| Day | 4431 | 452 (10%) | 1.0 | |
| Day of week | ||||
| Saturday or Sunday | 2982 | 340 (11%) | 1.00 (0.91–1.11) | 0.9 |
| Monday-Friday | 8155 | 944 (12%) | 1.0 | |
| Month | ||||
| July or August | 1897 | 219 (12%) | 0.95 (0.85–1.07) | 0.4 |
| Other | 9240 | 1065 (12%) | 1.0 | |
| Epoch | ||||
| After duty-hour restrictions | 5847 | 647 (11%) | 0.99 (0.84–1.19) | 0.9 |
| Before duty-hour restrictions | 5290 | 637 (12%) | 1.0 | |
Relative risks and p-values are from a modified Poisson regression model that included the four timing of birth indicators as well as study center, BW, GA, sex, race, multiple birth, 1-minute Apgar score < 5, maternal antepartum hemorrhage, maternal hypertension or preeclampsia-eclampsia, and continuous time (to adjust for common time trends).
Mortality within 28 days of birth
Overall, 1,785 (16.0%) infants died in the first 28 days of life. The most common cause of death reported was RDS (33%); the second-most common was immaturity (32%). Twenty-eight day mortality varied little across the period, ranging from 15.2% to 16.9%. No significant difference was found in the risk of 28-day mortality by timing of birth, either overall (Table 3) or among infants in any of the three birth weight groups.
TABLE 3.
Relative risk of death in the first 28 days among infants 501–1250 grams birth weight by timing of birth
| Timing of birth | N | Death in 28 days |
Adjusted RR (95% CI)a |
P- valuea |
|---|---|---|---|---|
| Birth hour | ||||
| Late night | 3128 | 575 (18%) | 1.06 (0.97–1.16) | 0.4 |
| Early night | 3578 | 574 (16%) | 1.03 (0.94–1.12) | |
| Day | 4431 | 636 (14%) | 1.0 | |
| Day of week | ||||
| Saturday-Sunday | 2982 | 473 (16%) | 0.99 (0.92–1.08) | 0.9 |
| Monday-Friday | 8155 | 1312 (16%) | 1.0 | |
| Month | ||||
| July/August | 1897 | 302 (16%) | 0.95 (0.87–1.05) | 0.3 |
| Other | 9240 | 1483 (16%) | 1.0 | |
| Epoch | ||||
| After duty-hour restrictions | 5847 | 920 (16%) | 0.98 (0.85–1.12) | |
| Before duty-hour restrictions | 5290 | 865 (16%) | 1.0 | 0.7 |
Relative risks and p-values are from a modified Poisson regression model that included the four timing of birth indicators as well as study center, BW, GA, sex, race, multiple birth, 1-minute Apgar score < 5, maternal antepartum hemorrhage, maternal hypertension or preeclampsia-eclampsia, and continuous time (to adjust for common time trends).
Short-Term Morbidity
After adjusting for maternal and neonatal characteristics as well as time trends, no significant difference was found in the risk of NEC, late-onset sepsis, BPD, or IVH-PVL by birth hour, day of the week, month, or epoch. For each of these morbidities, there was also no impact of timing of birth on the composite outcome of the morbidity or death.
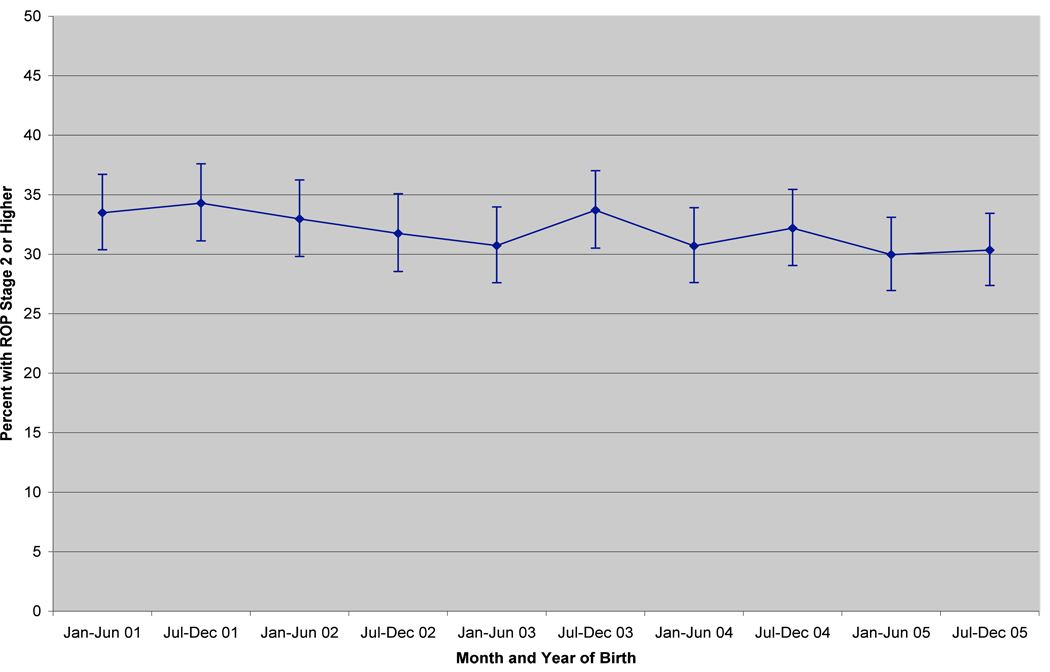
Among 8,294 infants who survived and were evaluated for ROP, 32% were diagnosed with ROP stage 2 or higher in one or both eyes. No significant difference was found in the risk of ROP by birth hour, day of the week, or month. There was a significant time trend (p<0.001), with the rate of ROP decreasing over time (adjusted RR per 6-month interval 0.96, 95% CI 0.95–0.98) (Figure). After adjusting for the time trend, the risk of ROP was significantly increased for infants born after resident-fellow duty-hour restrictions were implemented compared to those born in the period before (adjusted RR 1.22, 95% CI 1.10–1.36; p<0.001). The downward trend in ROP rate was present both before and after the duty-hour restrictions were introduced, at which time there was a step upward in ROP risk (Jul-Dec 2003 period in Figure). An increase after duty-hour restrictions were implemented also was found for the composite outcome of ROP (stage 2 or higher) or death (adjusted RR 1.11, 95% CI 1.04–1.19; p=0.002). Among the infants for whom treatment information was available, 10% had ROP requiring treatment in one or both eyes. The risk of ROP requiring treatment was significantly lower for infants born during the late night versus the day (adjusted RR 0.84, 95% CI 0.73–0.97), but it was not significantly lower for infants born during the early night versus the day. The risk of the composite outcome of ROP requiring treatment or death did not vary by birth hour. Neither the individual nor the composite outcome – ROP requiring treatment or death – varied by day of the week, month, or epoch.
FIGURE 1.
Percent of infants with retinopathy of prematurity stage 2 or higher by interval of birth among infants with birth weight 501–1250 grams born in NICHD Neonatal Research Network centers between Jan. 1, 2001 and Dec. 31, 2005. The vertical bars show 95% confidence intervals for each point estimate.
Neurodevelopmental Outcome
Among 7228 children with birth weight 501–1000 grams, 2145 (30%) died prior to the follow-up evaluation. Of the 5,083 survivors, 4,508 children (89%) were seen at follow-up (September 2002 through April 2008). After adjusting for maternal and neonatal characteristics as well as time trends, no significant difference was found in the risk of MDI<70 or death, PDI<70 or death, moderate or severe CP or death, vision impairment or death, or NDI or death by birth hour, day of the week, month, or epoch. The risk of hearing impairment or death did not vary by birth hour, day of the week, or epoch. However, the risk of hearing impairment or death was slightly reduced for infants born in July or August compared to other months (adjusted RR 0.92, 95% CI 0.85–0.998; p=0.04).
DISCUSSION
In this network of NICUs in major academic centers, we found little effect of timing of birth on the mortality, morbidity, and long-term developmental outcome of VLBW infants. We interpret this to mean that, in these centers, adequate staffing is available at all hours and during weekends as well as weekdays and that adequate supervision of inexperienced trainees is available in July and August. Further, we found no evidence of adverse effect of duty-hour restrictions on VLBW mortality and little, if any, effect on morbidity. It is possible that other factors not included in our analysis had beneficial effect and so neutralized any negative impact of duty-hour restrictions on outcome. As an example, we speculate that any adverse effects of decreased caregiver continuity and practical experience resulting from duty-hour restrictions were offset by reduced fatigue or by increased supervisory surveillance. Other, unrecognized factors might also have played a role. Our database did not include data on the hours actually worked by residents and fellows before and after implementation of the duty-hour restrictions in the participating centers. Although one study found little change in the work hours reported by residents after introduction of duty-hour restrictions,31 another reported significantly decreased work hours of pediatric residents working in the neonatal and pediatric intensive care units.32 If further duty-hour reforms are implemented for trainees, it will be important to assess their impact.33
Insofar as high-risk obstetrics patients are sometimes delivered electively during daytime hours and on weekdays, this practice might be anticipated to influence the impact of timing of birth on infant outcome. We accounted for a number of potential confounding factors in our analyses, but we did not have information on all potential confounders, such as variations in obstetrical practice34 and staffing patterns in the NICU.35
In our study, infants who were SGA, from a multiple birth, or delivered by Cesarean section were more likely to be born during the day and on Monday through Friday than at night or on the weekend, possibly indicating that these infants are more likely than others to be delivered electively. Infants of mothers with hypertension or preeclampsia also were more likely to be born during the day than at night.
Infants born at night were of lower birth weight and gestational age and had lower Apgar scores, and their mothers were more likely to have antepartum hemorrhage. After adjusting for these and other risk factors, they were neither more likely to die nor more likely to experience significant morbidity than infants born at other time periods. We also found no evidence that mortality or morbidity risk was higher among infants born on the weekend or during July or August.
The results of our study are encouraging in that we did not demonstrate adverse effects of implementation of the ACGME duty-hour restrictions for residents and fellows on mortality or morbidity of VLBW infants in the teaching hospitals that comprise the Neonatal Research Network. In the period after the restrictions were introduced, the mothers of VLBW infants were more likely to have had antepartum hemorrhage, hypertension or preeclampsia, and Cesarean delivery. There was no change in the risk of 7-day or 28-day mortality, and there was no change in the risk of any morbidity except ROP. After duty-hour restrictions were introduced, there was an increase in the adjusted risks of ROP (stage 2 or higher) alone and the composite outcome of ROP or death. The risk of hearing impairment or death was slightly lower among infants born in July or August compared to other months. Given the large number of comparisons that were made, caution should be exercised in interpreting these findings.
Previous studies have found improved patient safety and mortality or no effect among adult medical and surgical patients after introduction of duty-hour restrictions.31,36–41 We found little impact of the ACGME duty-hour restrictions on the outcome of VLBW infants in this group of teaching hospitals. Shorter on-call shifts for residents and fellows might be anticipated to have negative effects on the continuity of care and to have increased the potential for problems associated with patient “handoff”.42 The duty-hour restrictions might also result in less practical experience for residents at each level and reduced competence with the technical aspects of patient care that are so important for VLBW infants, such as tracheal intubation. If such potential effects of duty-hour restriction have negative impact on patient outcome, they may be offset by a reduction in the errors that result from fatigue.43–45
CONCLUSION
Despite previous reports of increased perinatal or neonatal mortality among infants born at night, on the weekend, or during July and August, we found no effect of timing of birth on the mortality risk of VLBW infants and little effect on morbidity. In addition, we found no significant change in VLBW outcomes after the introduction of resident and fellow duty-hour restrictions. Variations in mortality and morbidity related to the timing of birth depend on an institution’s capacity to provide a sufficient number of adequately trained and experienced staff at all times. We speculate that the lack of major effects of timing of birth in this analysis indicates that the NICUs of the Neonatal Research Network are able to provide adequate staffing, even at night and on the weekends, and that inexperienced trainees are given sufficient support from more experienced staff. Moreover, the lack of change in VLBW outcome after introduction of resident and fellow duty-hour restrictions suggests that appropriate adjustments in staffing have been made. Matching the need and availability of personnel and other resources is key to maintaining consistently high-quality outcomes.
ACKNOWLEDGEMENTS
Data collected at participating sites of the NICHD Neonatal Research Network (NRN) were transmitted to RTI International, the data coordinating center (DCC) for the Network, which stored, managed, and analyzed the data for this study. On behalf of the NRN, Abhik Das, PhD (DCC Principal Investigator) and Nellie I. Hansen, MPH (DCC Statistician) had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis.
ABBREVIATIONS
- ACGME
Accreditation Council for Graduate Medical Education
- BPD
bronchopulmonary dysplasia
- BW
birth weight
- CI
confidence interval
- CP
cerebral palsy
- DR
delivery room
- GA
gestational age
- IVH
intraventricular hemorrhage
- MDI
motor developmental index
- NDI
neurodevelopmental impairment
- NEC
necrotizing enterocolitis
- NICHD
Eunice Kennedy Shriver National Institute for Child Health and Human Development
- NICU
neonatal intensive care unit
- NRN
Neonatal Research Network
- PDI
psychomotor developmental index
- PVL
periventricular hemorrhage
- RDS
respiratory distress syndrome
- ROP
retinopathy of prematurity
- RR
relative risk
- SGA
small for gestational age
- VLBW
very low birth weight
Appendix
We are indebted to our medical and nursing colleagues and the infants and their parents who agreed to take part in this study. The following investigators, in addition to those listed as authors, participated in this study:
NRN Steering Committee Chair: Alan H. Jobe, MD PhD, University of Cincinnati.
Eunice Kennedy Shriver National Institute of Child Health and Human Development: Linda L. Wright, MD.
University of Iowa: Carver College of Medicine (U10 HD53109, CTSA UL1 RR24979, and GCRC M01 RR59) - Karen J. Johnson, RN.
Case Western Reserve University: Rainbow Babies & Children's Hospital (GCRC M01 RR80, U10 HD21364) – Avroy A. Fanaroff, MD; Nancy S. Newman, RN; Harriet G. Friedman, MA; Bonnie S. Siner, RN; Deanne E. Wilson-Costello, MD.
University of Texas Health Science Center at Houston: Children's Memorial Hermann Hospital, and Lyndon Baines Johnson General Hospital/Harris County Hospital District (U10 HD21373) – Jon E. Tyson, MD MPH; Kathleen A. Kennedy, MD MPH; Patricia W. Evans, MD; Esther G. Akpa, RN BSN; Nora Alaniz, BS; Patty A. Cluff, RN; Claudia I. Franco, RNC MSN; Anna E. Lis, RN BSN; Sarah Martin, RN BSN; Maegan C. Simmons, RN; Georgia E. McDavid, RN; Patti Pierce Tate, RCP; Pamela J. Bradt, MD MPH; Susan Dieterich, PhD; Terri Major-Kincade, MD MPH; Brenda H. Morris, MD; Stacey Reddoch, BA; Laura L. Whitely, MD.
Wayne State University: Hutzel Women’s Hospital and Children’s Hospital of Michigan (U10 HD21385) – Seetha Shankaran, MD; Rebecca Bara, RN BSN; Geraldine Muran, RN BSN; Laura Goldston, MA; Yvette R. Johnson, MD MPH; Athina Pappas, MD; Deborah Kennedy, RN BSN; Rebecca Wheeler.
University of Miami: Holtz Children's Hospital (GCRC M01 RR16587, U10 HD21397) – Charles R. Bauer, MD; Shahnaz Duara, MD; Ruth Everett-Thomas, RN MSN; Maria Calejo, MS; Alexis N. Diaz, BA; Silvia M. Frade Eguaras, MA; Yamiley C. Gideon, BA; Sylvia Hiriart-Fajardo, MD; Ann Londono; Elaine O. Mathews, RN.
Emory University: Children’s Healthcare of Atlanta, Grady Memorial Hospital, and Emory Crawford Long Hospital (GCRC M01 RR39, U10 HD27851) – Susie Buchter, MD; Marcia Berry Bishop, MS NNP-BC; Irma Seabrook, RRT; Ellen C. Hale, RN BS CCRC; Ira Adams-Chapman, MD; Sheena Carter, PhD; Elisabeth Dinkins, PNP; Maureen Mulligan LaRossa, RN; Gloria V. Smikle, PNP.
University of Cincinnati: University Hospital, Cincinnati Children's Hospital Medical Center, and Good Samaritan Hospital (GCRC M01 RR8084, U10 HD27853) – Edward F. Donovan, MD; Barbara Alexander, RN; Kate Bridges, MD; Cathy Grisby, BSN CCRC; Marcia Worley Mersmann, RN CCRC; Holly L. Mincey, RN BSN; Jody Hessling , RN; Teresa L. Gratton, PA; Jean J. Steichen, MD.
Indiana University: Indiana University Hospital, Methodist Hospital, Riley Hospital for Children, and Wishard Health Services (GCRC M01 RR750, U10 HD27856) – Brenda B. Poindexter, MD MS; James A. Lemons, MD; Diana D. Appel, RN BSN; Dianne E. Herron, RN; Lucy C. Miller, RN BSN CCRC; Richard Hooper, RRT; Lon G. Bohnke, MS; Marilyn Bull, MD; Ann B. Cook, MS; Anna M. Dusick, MD FAAP; Greg Eaken, PhD; Darlene Kardatzke, MD; Carolyn Lytle, MD MPH; Heike M. Minnich, PsyD HSPP; Leslie Richard, RN.
Yale University: Yale-New Haven Children’s Hospital (GCRC M01 RR125, U10 HD27871) – Richard A. Ehrenkranz, MD; Patricia Gettner, RN; Monica Konstantino, RN BSN; JoAnn Poulsen, RN; Janet Taft, RN BSN; Nancy Close, PhD; Elaine Romano, MSN; Joanne Williams, RN BSN.
Stanford University: Lucile Packard Children's Hospital and El Camino Hospital (GCRC M01 RR70, U10 HD27880) – David K. Stevenson, MD; Krisa P. Van Meurs, MD; Susan R. Hintz, MD MS; M. Bethany Ball, BS CCRC; Anne M. DeBattista, RN PNP; Joan M. Baran, PhD; Ginger K. Brudos, PhD; Julie C. Lee-Ancajas, PhD; Renee P. Pyle, PhD; Nicholas H. St. John, PhD; Marian M. Adams, MD; Jean G. Kohn, MD MPH; Dharshi Sivakumar, MD.
Brown University: Women & Infants Hospital of Rhode Island (U10 HD27904) – William Oh, MD; Angelita M. Hensman, RN BSN; Barbara Alksninis, PNP; William J. Cashore, MD; Regina A. Gargus, MD; Shabnam Lainwala MD; Theresa M. Leach, MEd CAES; Martha R. Leonard, BA BS; Kalida Mehta MD; James R. Moore, MD; Lucy Noel, Bonnie E. Stephens, MD; Rachel V. Walden, MD; Betty R. Vohr, MD; Victoria E. Watson, MS CAS.
University of Alabama at Birmingham: Health System and Children’s Hospital of Alabama (GCRC M01 RR32, U10 HD34216) – Monica V. Collins, RN BSN MaEd; Shirley S. Cosby, RN BSN; Fred J. Biasini, PhD; Stephanie A. Chopko, PhD; Mary Beth Moses, PT MS PCS; Kathleen G. Nelson, MD; Myriam Peralta-Carcelen, MD MPH; Vivien A. Phillips, RN BSN; Richard V. Rector, PhD; Sally Whitley, MA OTR-L FAOTA.
University of California – San Diego: Medical Center and Sharp Mary Birch Hospital for Women (U10 HD40461) – Neil N. Finer, MD; Maynard R. Rasmussen, MD; Paul R. Wozniak, MD; Kathy Arnell, RNC; Renee Bridge, RN; Clarence Demetrio, RN; Jim Goodmar, RRT; Chris Henderson, RCP CRTT; Wade Rich, BSHS RRT; Rene Barbieri-Welge; Ayala Ben-Tall; Martha G. Fuller, RN MSN; Elaine Ito; Meghan Lukasik; Deborah Pontillo; Donna Posin, OTR/L MPA; Cheryl Runyan; Yvonne E. Vaucher, MD MPH; James Wilkes; Paul Zlotnik, MD.
Duke University School of Medicine: University Hospital, Alamance Regional Medical Center, and Durham Regional Hospital (GCRC M01 RR30, U10 HD40492) – Ronald N. Goldberg, MD; C. Michael Cotten, MD MHS; Kathy J. Auten, MSHS; Ricki F. Goldstein, MD; Kathryn E. Gustafson, PhD; Melody B. Lohmeyer, RN MSN; William F. Malcolm, MD.
Wake Forest University: Baptist Medical Center, Forsyth Medical Center, and Brenner Children’s Hospital (GCRC M01 RR7122, U10 HD40498) – T. Michael O’Shea, MD MPH; Nancy J. Peters, RN CCRP; Deborah Evans Allred, MA LPA; Korinne Chiu, MA; Robert G. Dillard, MD; Donald J. Goldstein, PhD; Raquel Halfond, MA; Cherrie D. Welch, MD MPH; Gail Wiley Hounshell, PhD; Barbara G. Jackson, RN BSN; Melissa Whalen Morris, MA; Carroll Peterson, MA; Ellen L. Waldrep, MS.
University of Rochester School of Medicine and Dentistry: Golisano Children's Hospital at Strong (GCRC M01 RR44, U10 HD40521) – Dale L. Phelps, MD; Linda J. Reubens, RN CCRC; Mary Rowan, RN; Erica L. Burnell, RN; Julie Babish Johnson, MSW; Diane Hust, MS RN CS; Rosemary L. Jensen; Emily Kushner, MA; Joan Merzbach, LMSW; Gary J. Myers, MD; Kelley Yost, PhD; Lauren Zwetsch, RN MS PNP.
University of Texas Southwestern Medical Center at Dallas: Parkland Health & Hospital System and Children's Medical Center Dallas (GCRC M01 RR633, U10 HD40689) – Charles R. Rosenfeld, MD; Walid A. Salhab, MD; Gaynelle Hensley, RN; Susie Madison, RN; Nancy A. Miller, RN; Melissa Martin, RN; James Allen, RRT; Kerry Wilder, RN; Alicia Guzman; R. Sue Broyles, MD; Roy J. Heyne, MD; Sally S. Adams, MS RN CPNP; Catherine Twell Boatman, MS; Cristin Dooley, MS; Elizabeth Heyne, PA; Jackie F. Hickman, RN; Linda A. Madden, BSN, RN, CPNP; Janet S. Morgan, RN.
Data Coordinating Center:
RTI International: (U01 HD36790) – W. Kenneth Poole, PhD; Betty K. Hastings; Carolyn Petrie Huitema, MS; Elizabeth M. McClure, MEd; Jeanette O’Donnell Auman, BS; Kristin M. Zaterka-Baxter, RN BSN; Jamie E. Newman, PhD MPH.
Footnotes
FINANCIAL DISCLOSURE:
The authors have indicated they have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.Stanley FJ, Alberman ED. Infants of very low birthweight. I: Perinatal factors affecting survival. Dev Med Child Neurol. 1978;20(3):300–312. doi: 10.1111/j.1469-8749.1978.tb15220.x. [DOI] [PubMed] [Google Scholar]
- 2.Tyson J, Schultz K, Sinclair JC, Gill G. Diurnal variation in the quality and outcome of newborn intensive care. J Pediatr. 1979;95(2):277–280. doi: 10.1016/s0022-3476(79)80672-1. [DOI] [PubMed] [Google Scholar]
- 3.Domenighetti G, Paccaud F. The night – a dangerous time to be born? Br J Obstet Gynaecol. 1986;(12):1262–1267. doi: 10.1111/j.1471-0528.1986.tb07863.x. [DOI] [PubMed] [Google Scholar]
- 4.Paccaud F, Martin-Béran B, Gutzwiller F. Hour of birth as a prognostic factor for perinatal death. Lancet. 1988;1(8581):340–343. doi: 10.1016/s0140-6736(88)91130-0. [DOI] [PubMed] [Google Scholar]
- 5.Stewart JH, Andrews J, Cartlidge PHT. Numbers of deaths related to intrapartum asphyxia and timing of birth in all Wales perinatal survey, 1993–5. Br Med J. 1998;316(7132):657–660. doi: 10.1136/bmj.316.7132.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heller G, Misselwitz B, Schmidt S. Early neonatal mortality, asphyxia related deaths, and timing of low risk births in Hesse, Germany, 1990–8: observational study. Br Med J. 2000;321(4):274–275. doi: 10.1136/bmj.321.7256.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luo ZC, Karlberg J. Timing of birth and infant and early neonatal mortality in Sweden 1973–95: longitudinal birth register study. Br Med J. 2001;323(7325):1327–1330. doi: 10.1136/bmj.323.7325.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee SK, Lee DSC, Andrews WL, Baboolal R, Pendray M, Stewart S. Canadian Neonatal Network. Higher mortality rates among inborn infants admitted to neonatal intensive care units at night. J Pediatr. 2003;143(5):592–597. doi: 10.1067/s0022-3476(03)00367-6. [DOI] [PubMed] [Google Scholar]
- 9.Stephansson O, Dickman PW, Johansson ALV, Kieler H, Cnattingius S. Time of birth and risk of intrapartum and early neonatal death. Epidemiology. 2003;14(2):218–222. doi: 10.1097/01.EDE.0000037975.55478.C7. [DOI] [PubMed] [Google Scholar]
- 10.Heller G, Schnell R, Misselwitz, Schmidt S. Warum ist die Sterblichkeit von nachts geborenen Kindern erhöht? Z Geburtshilfe Neonatol. 2003;207(4):137–142. doi: 10.1055/s-2003-42804. [DOI] [PubMed] [Google Scholar]
- 11.Gould JB, Qin C, Chavez G. Time of birth and the risk of neonatal death. Obstet Gynecol. 2005;106(2):352–358. doi: 10.1097/01.AOG.0000168627.33566.3c. [DOI] [PubMed] [Google Scholar]
- 12.Abdel-Latif ME, Bajuk B, Oei J, Lui K for the New South Wales and the Australian Capital Territory Neonatal Intensive Care Audit Group. Mortalities and morbidities among very premature infants admitted after hours in an Australian neonatal intensive care unit network. Pediatrics. 2006;117(5):1632–1639. doi: 10.1542/peds.2005-1421. [DOI] [PubMed] [Google Scholar]
- 13.Urato AC, Craigo SD, Chelmow D, O'Brien WF. The association between time of birth and fetal injury resulting in death. Am J Obstet Gynecol. 2006;195(6):1521–1526. doi: 10.1016/j.ajog.2006.03.084. [DOI] [PubMed] [Google Scholar]
- 14.Caughey AB, Urato AC, Lee KA, Thiet MP, Washington AE, Laros RK., Jr Time of delivery and neonatal morbidity and mortality. Am J Obstet Gynecol. 2008;199(5):496e1–496e5. doi: 10.1016/j.ajog.2008.03.046. [DOI] [PubMed] [Google Scholar]
- 15.MacFarlane A. Variations in number of births and perinatal mortality by day of week in England and Wales. Br Med J. 1978;2(6153):1670–1673. doi: 10.1136/bmj.2.6153.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mangold WD. Neonatal mortality by the day of the week in the 1974–75 Arkansas live birth cohort. Am J Public Health. 1981;71(6):601–605. doi: 10.2105/ajph.71.6.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hendry RA. The weekend – a dangerous time to be born? Br J Obstet Gynaecol. 1981;88(12):1200–1203. doi: 10.1111/j.1471-0528.1981.tb01197.x. [DOI] [PubMed] [Google Scholar]
- 18.Mathers CD. Births and perinatal deaths in Australia: variations by day of week. J Epidemiol Community Health. 1983;37(1):57–62. doi: 10.1136/jech.37.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton P, Restrepo E. Sociodemographic factors associated with weekend birth and increased risk of neonatal mortality. J Obstet Gynecol Neonatal Nurs. 2006;35(2):208–214. doi: 10.1111/j.1552-6909.2006.00034.x. [DOI] [PubMed] [Google Scholar]
- 20.Gould JB, Qin C, Marks AR, Chavez G. Neonatal mortality in weekend vs weekday births. JAMA. 2003;289(22):2958–2962. doi: 10.1001/jama.289.22.2958. [DOI] [PubMed] [Google Scholar]
- 21.Bruckner TA, Carlo WA, Ambalavanan N, Gould JB. Neonatal mortality among low birth weight infants during the initial months of the academic year [published online ahead of print July 3 2008] J Perinatol. 2008;28(10):691–695. doi: 10.1038/jp.2008.72. [DOI] [PubMed] [Google Scholar]
- 22.Soltau TD, Carlo WA, Gee J, Gould J, Ambalavanan N. Mortality and morbidity by month of birth of neonates admitted to an academic neonatal intensive care unit. Pediatrics. 2008;122(5):e1048–e1052. doi: 10.1542/peds.2008-0412. [DOI] [PubMed] [Google Scholar]
- 23.Resident duty hours: enhancing sleep, supervision, and safety. Recommendations of the Committee on Optimizing Graduate Medical Trainee (Resident) Hours and Work Schedules to Improve Patient Safety. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- 24.Iglehart JK. Revisiting duty-hour limits – IOM recommendations for patient safety and resident education. N Eng J Med. 2008;359(25):2633–2635. doi: 10.1056/NEJMp0808736. [DOI] [PubMed] [Google Scholar]
- 25.Report of the ACGME work group on resident duty hours. Chicago, IL: Accreditation Council for Graduate Medical Education; 2002. Available at http://www.acgme.org/acWebsite/dutyHours/dh_wkgroupreport611.pdf. February 9. 2009. [Google Scholar]
- 26.Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, Brotherton T. Neonatal necrotizing enterocolitis: therapeutic decisions based on clinical staging. Ann Surg. 1978;187(1):1–7. doi: 10.1097/00000658-197801000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996;87(2):163–168. doi: 10.1016/0029-7844(95)00386-X. [DOI] [PubMed] [Google Scholar]
- 28.Bayley N. Bayley Scales of Infant Development, Second Edition. San Antonio, TX: Psychological Corporation; 1999. [Google Scholar]
- 29.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 30.Ambalavanan N, Carlo WA, Bobashev G, Mathias E, Liu B, Poole L, Fanaroff AA, Stoll BJ, Ehrenkranz R, Wright LL for the NICHD Neonatal Research Network. Prediction of death for extremely low birth weight neonates. Pediatrics. 2005;116(6):1367–1373. doi: 10.1542/peds.2004-2099. [DOI] [PubMed] [Google Scholar]
- 31.Landrigan CP, Fahrenkopf AM, Lewin D, Sharek PJ, Barger LK, Eisner M, Edwards S, Chiang VW, Wiedermann BL, Sectish TC. Effects of the Accreditation Council for Graduate Medical Education duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122(2):250–258. doi: 10.1542/peds.2007-2306. [DOI] [PubMed] [Google Scholar]
- 32.Cull WL, Mulvey HJ, Jewett EA, Zalneraitis EL, Allen CE, Pan RJ. Pediatric residency duty hours before and after limitations. Pediatrics. 2006;118(6):e1805–e1811. doi: 10.1542/peds.2006-0210. [DOI] [PubMed] [Google Scholar]
- 33.Brion LP, Neu J, Adamkin D, Bancalari E, Cummings J, Guttentag S, Juul S, Norwood VF, Ryan RM. Resident duty hour restrictions: is less really more? J Pediatr. 2009;154(5) doi: 10.1016/j.jpeds.2009.02.004. 631–632.e1. [DOI] [PubMed] [Google Scholar]
- 34.Dowding VM, Duignan NM, Henry GR, MacDonald DW. Induction of labour, birthweight and perinatal mortality by day of the week. Br J Obstet Gynaecol. 1987;94(5):413–419. doi: 10.1111/j.1471-0528.1987.tb03118.x. [DOI] [PubMed] [Google Scholar]
- 35.Hamilton KES, Redshaw ME, Tarnow-Mordi W. Nurse staffing in relation to risk-adjusted mortality in neonatal care. Arch Dis Child Fetal Neonatal Ed. 2007;92(2):F99–F103. doi: 10.1136/adc.2006.102988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Poulose BK, Ray WA, Arbogast PG, Needleman J, Buerhaus PI, Griffin MR, Abumrad NN, Beauchamp RD, Holzman MD. Resident work-hour limits and patient safety. Ann Surg. 2005;241(6):847–860. doi: 10.1097/01.sla.0000164075.18748.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Volpp KG, Rosen AK, Rosenbaum PR, Romano PS, Even-Shoshan O, Canamucio A, Bellini L, Behringer T, Silber JH. Mortality among patients in VA hospitals in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9):984–992. doi: 10.1001/jama.298.9.984. [DOI] [PubMed] [Google Scholar]
- 38.Volpp KG, Rosen AK, Rosenbaum PR, Even-Shoshan O, Wang Y, Bellini L, Behringer T, Silber JH. Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9):975–983. doi: 10.1001/jama.298.9.975. [DOI] [PubMed] [Google Scholar]
- 39.Shetty KD, Battacharya J. Changes in hospital mortality associated with residency work-hour regulations. Ann Intern Med. 2007;147(2):73–80. doi: 10.7326/0003-4819-147-2-200707170-00161. [DOI] [PubMed] [Google Scholar]
- 40.Bailit JL, Blanchard MH. The effect of house staff working hours on the quality of obstetric and gynecologic care. Obstet Gynecol. 2004;103(4):613–616. doi: 10.1097/01.AOG.0000119225.57285.c1. [DOI] [PubMed] [Google Scholar]
- 41.Prasad M, Iwashyna TJ, Christie JD, Kramer AA, Silber JH, Volpp KG, Kahn JM. Effect of work-hours regulations on intensive care unit mortality in United States teaching hospitals. Crit Care Med. 2009;37(9):2564–2569. doi: 10.1097/CCM.0b013e3181a93468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kitch BT, Cooper JB, Zapol WM, Marder JE, Karson A, Hutter M, Campbell EG. Handoffs causing patient harm: a survey of medical and surgical house staff. Jt Comm J Qual Patient Saf. 2008;34(10):563–570. doi: 10.1016/s1553-7250(08)34071-9. [DOI] [PubMed] [Google Scholar]
- 43.Gaba DM, Howard SK. Fatigue among clinicians and the safety of patients. N Engl J Med. 2002;347(16):1249–1255. doi: 10.1056/NEJMsa020846. [DOI] [PubMed] [Google Scholar]
- 44.Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, Rothschild JM, Katz JT, Lilly CM, Stone PH, Aeschbach D, Czeisler CA. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351(18):1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 45.Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, Lilly CM, Stone PH, Lockley SW, Bates DW, Czeisler CA. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351(18):1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]