Abstract
Objective
To prospectively examine the contribution of angina and cardiac history to health-related quality of life (HRQoL) and depression in cardiac patients, over 6 months post-hospitalization.
Methods
Participants were myocardial infarction (MI), percutaneous coronary intervention (PCI), or coronary artery bypass grafting surgery (CABG) out-patients under the age of 70. One hundred and seventy one patients consented to participate, with 121 patients retained 6 months later (71% response rate). The impact of the patient’s cardiac history and the presence of angina on physical, social and emotional HRQoL and depression was examined.
Results
At baseline, cardiac history was not significantly related to any of the dimensions of HRQoL or depression. At 6-months follow-up, cardiac history significantly predicted a higher level of depression, and angina was predictive of a significantly worse emotional, physical, and social HRQoL and a higher level of depression.
Discussion
The presence of a cardiac history is associated with depression 6 months post-cardiac event, and angina is associated with both an adverse HRQoL and higher levels of depression. As past research has demonstrated depression is a risk factor for mortality in patients with established heart disease, it is important both from a clinical and a research perspective to address these issues.
Keywords: angina, cardiac history, coronary heart disease, depression, quality of life
Introduction
The profile of diseases contributing most heavily to death, illness, and disability among western/developed countries has changed dramatically during the last century. Today, chronic diseases — such as cardiovascular disease (primarily heart disease and stroke), — are among the most prevalent, costly, and preventable of all health problems. The prolonged course of illness and disability from chronic disease results in extended pain and suffering, and decreased quality of life for millions of people around the world. Coronary Heart Disease (CHD) is the primary cause of premature death in the western world.1 Due to such a high prevalence and incidence, CHD has taken a high priority in health research.2
As many people live with chronic CHD, health related quality of life (HRQoL) has become an increasingly important outcome measure after hospital admission for a myocardial infarction (MI) or invasive procedures. HRQoL is considered an important outcome measure of medical technology and disease control by patients, clinicians, and society alike.3 Although there is no internationally agreed definition of HRQoL, there is a consensus that it is a multifaceted construct with physiological, psychological, emotional, and social components.4
Although previous research has focused on HRQoL after a cardiac event, to our knowledge, very little research has evaluated the impact of cardiac history on multidimensional HRQoL and depression. To date, it is unclear whether patients whom have suffered a previous event recover differently from patients whom have not suffered this fate with respect to a multifaceted construct of quality of life in cardiac patients.
Angina remains the most common initial manifestation of coronary heart disease. There are still many misconceptions about the continuing importance of angina which results from the success of revascularization and recent clinical trials.5 Not all patients who have angina access medical care or receive a diagnosis. More importantly, not all angina patients are able to undergo revascularization which has been shown to reduce symptoms of chest pain and discomfort.5 Much of the previous literature has focused on the admission of patients with acute coronary syndrome, as this is reasonably well defined, but this is not the case for stable angina.6 Although incident angina may be considered as too soft an endpoint by epidemiologists, it does not dismiss the fact that these patients do suffer adverse affects in the form of decreased quality of life. Pocock et al. [7] found that the patients’ grade of angina had a marked relationship with every aspect of perceived health status. Patients with angina had a worse HRQoL than angina-free patients. Bengtsson et al. [8] found that anginal grade was negatively related to HRQoL. Significant differences were found between patients with and without angina in physical capacity and self-reported general health, where angina grade was negatively related to QoL. As previous literature has described that patients with angina have an increased risk of mortality 5,9 and lower health related-quality of life levels, 7,8,10 additional research is warranted to further investigate health outcomes of patients with angina.
Although angina patients indicate that their HRQoL is affected in many cases, depression is also strongly correlated with the presence of angina within a CHD population.11 Treatment of depression has been shown to reduce chest discomfort, ischemia, and utilization of medical care.7
Previous studies have demonstrated repeatedly that depression is significantly related to morbidity and mortality after cardiac events.12–18 Therefore it is important, both from a clinical and a research perspective to assess depression after a patient has experienced a cardiac event.
The present study examines the impact of angina and cardiac history on physical, social, emotional HRQoL and depression in CHD patients. Moreover, this study attempts to show that patients with angina and a cardiac history may not be recovering at an acceptable rate by 6-months post-hospitalization. More specifically, this study attempts to assess (1) if the fact that patients have had a previous cardiac event (either MI, PCI, or CABG) is associated with an adverse HRQoL and higher depression, both at baseline and at follow-up, and; (2) if the presence of angina pectoris is associated with a poorer HRQoL and higher levels of depression at follow-up.
Materials and Methods
Study population
The subject population were patients under the age of 70 (M = 53.98, SD = 8.39), recruited after having been admitted to either one of two hospitals or one of two cardiac rehabilitation centers in the Netherlands after an MI, PCI or CABG. All patients were recruited about 45-days post-cardiac event.
Two hundred patients were initially approached by their cardiologist for participation in the study. Of these, 171 patients (143 males; 86%) agreed to participate. Seventy-seven patients were admitted for an MI (45%), 61 (36%) for a PCI, and 33 (19%) for a CABG. Patients were not approached for participation if they were unable to give informed consent, unable to understand the Dutch language and if they suffered from a serious organic non-cardiac disease.
The patients who participated at the first measurement were sent a follow-up questionnaire (which was identical to the baseline questionnaire) 6 months later. The response rate at follow-up was 71% (N = 121). The sample characteristics at baseline and follow-up are reported in Table 1. No significant differences were found on any of the sociodemographic and medical variables between the participants for whom baseline and follow-up data were available, and for those participants that dropped out prior to follow-up.
Table 1.
Sociodemographic and Medical Characteristics of the Patient Sample at Baseline and Follow-up
| Sociodemographic characteristics | Baseline (N = 171) | Follow-up (N = 121) |
|---|---|---|
| Age, mean (SD) | 53.98 (8.29) | 54.91 (8.00) |
| Gender | ||
| Male, n (%) | 144 (84.0) | 104 (86.0) |
| Living Situation* | ||
| Living Alone | 12.0 | 9.0 |
| Living with Partner and/or Children | 88.0 | 91.0 |
| Education* | ||
| Primary Education | 12.3 | 11.6 |
| Lower Secondary Education | 46.8 | 51.2 |
| Higher Secondary Education | 25.7 | 23.1 |
| Higher Education | 12.9 | 13.2 |
| Employment Status* a | ||
| Not working | 28.1 | 30.6 |
| 1–20 | 10.6 | 9.9 |
| 21+ | 57.8 | 57.0 |
| Medical characteristics | ||
| Reason for admittance* b | ||
| CABG | 19.0 | 23.0 |
| PCI | 36.0 | 41.0 |
| MI | 45.0 | 36.0 |
| Previous cardiac event * c | ||
| Presence of a previous cardiac event | 22.8 | 22.3 |
| Angina Pectoris (AP)* | ||
| Presence of AP | 32.0 | 24.8 |
| Location of Recruitment* | ||
| Hospital | 67.0 | N/A |
| CR site* d | 33.0 | N/A |
Numbers are percentages. Those percentages that do not add to 100% may have missing values.
Number of hours worked per week,
Myocardial infarction (MI), percutaneous coronary intervention (PCI), coronary artery bypass grafting surgery (CABG).
cardiac event = MI, PCI, or CABG,
Cardiac Rehabilitation (CR).
Data Collection
This was a prospective study that examined participants’ perceptions of their physical, social, emotional HRQoL and psychological well-being. The self-report survey consisted of questions that examined sociodemographic characteristics, HRQoL and depression at 45 days (baseline) and 6 months (follow-up) after the date of admittance. 19 More specifically, the instrument used to measure HRQoL was the Dutch MacNew Questionnaire (MacNew).20 This self-report measure consists of 26 items related to 3 domains of HRQoL, emotional, social, and physical HRQoL. Each item is rated on a 7-point Likert scale, where ‘1’ indicates poor HRQoL and ‘7’ indicates good HRQoL. The Dutch MacNew was demonstrated to have adequate reliability and validity, and the internal consistency was fair to (very) good (ranging between .78 and .95).20 The 90-Item Symptom Checklist (SCL-90R) was used to assess depression.21–23 The depression subscale consists of 16 items. A higher score indicates a higher level of depression. The SCL-90R depression subscale has shown good reliability and validity. 21,22
In the baseline survey, patients were asked to report if they had experienced a previous cardiac event prior to their current admission. Angina pectoris status was also obtained by patient self-report.
Statistics
All statistical analyses were performed with SPSS release 12.0. Data were cleaned and screened to evaluate statistical assumptions. Descriptive examination of the variables was performed using chi-square and Analysis of Variance (ANOVA) as appropriate. Multiple linear regression analyses were used to examine predictors of HRQoL and depression. The regression analyses adjusted for demographic characteristics (age and gender), and reason for admittance (MI, PCI, CABG) as these variables showed significance in the initial descriptives analysis. All predictors were entered into the model using the forced entry method. All statistical tests were two-tailed. P < 0.05 was used for all tests to indicate statistical significance.
Results
Impact of cardiac history on health-related quality of life and depression at baseline
Multiple linear regression analyses revealed that at baseline the presence or absence of a previous cardiac event (cardiac history) was not significantly related to any of the dimensions of HRQoL or depression (see Table 2).
Table II.
Cardiac history as a predictor of impaired HRQL at baseline: A comparison between patients with and without a previous cardiac event (adjusted analyses)
| β | sr2 | 95% Confidence Interval | ||
|---|---|---|---|---|
| Emotional HRQoL | Lower Bound | Upper Bound | ||
| Previous Event (cardiac history) | −.006 | −.006 | −5.118 | 4.768 |
| Gender | −.207+ | −.208 | −11.920 | −1.768 |
| Age | −.052 | −.052 | −.311 | .157 |
| PCI | −.112 | −.048 | −12.051 | 6.445 |
| CABG | .026 | .013 | −8.632 | 10.215 |
| MI | −.046 | −.020 | −10.265 | 7.998 |
| Physical HRQoL | ||||
| Previous Event (cardiac history) | −.004 | −.004 | −4.532 | 4.327 |
| Gender | −.199* | −.203 | −10.538 | −1.440 |
| Age | −.069 | −.069 | −.302 | .117 |
| PCI | −.095 | −.041 | −10.467 | 6.109 |
| CABG | .114 | .059 | −5.282 | 11.607 |
| MI | −.138 | −.059 | −11.276 | 5.090 |
| Social HRQoL | ||||
| Previous Event (cardiac history) | .001 | .001 | −3.317 | 3.357 |
| Gender | −.210+ | −.211 | −8.224 | −1.290 |
| Age | −.056 | −.055 | −.213 | .102 |
| PCI | .013 | .005 | −6.073 | 6.506 |
| CABG | .132 | .067 | −3.684 | 9.190 |
| MI | .023 | .010 | −5.836 | 6.627 |
| SCL-90 Depression | ||||
| Previous Event (cardiac history) | .023 | .021 | −.056 | .073 |
| Gender | .174* | .175 | .009 | .143 |
| Age | .001 | .001 | −.003 | .003 |
| PCI | .295 | .125 | −.024 | .218 |
| CABG | .138 | .070 | −.069 | .180 |
| MI | .230 | .097 | −.046 | .195 |
MI = myocardial infarction; PCI = percutaneuous coronary intervention; CABG = coronary artery bypass grafting
The SCL-90R depression subscale was transformed using LOG10 in order to normalize the data.
p < 0.05;
p < 0.01;
p < 0.001
Gender was shown to be significant on all of the HRQoL subscales as well as the depression measure, where women had significantly worse HRQOL and a higher depression level compared to men. It is also noteworthy to mention that patients with a cardiac history have slightly lower baseline MacNew HRQoL scores and a slightly higher depression mean score on the SCL-90 (see Table 3).
Table 3.
Means and Standard Deviations for HRQoL at Baseline and 6-Month Follow-up, Broken Down by Cardiac History and Gender (N = 121)
| Baseline Mean Score (SD) | Follow-up Mean Score (SD) | ||
|---|---|---|---|
| Emotional HRQoL | |||
| No previous events | men | 54.19 (12.20) | 60.40 (11.71) |
| women | 48.69 (9.01) | 56.45 (13.50) | |
| Total | 53.32 (11.89) | 59.79 (12.01) | |
| At least 1 previous event | men | 51.27 (11.27) | 54.62 (13.30) |
| women | 46.00 (5.29) | 51.00 (9.17) | |
| Total | 50.61 (10.77) | 54.17 (12.75) | |
| Physical HRQoL | |||
| No previous events | men | 49.44(10.83) | 56.35 (10.47) |
| women | 43.00 (10.82) | 52.08 (11.21) | |
| Total | 48.41(11.82) | 55.71 (10.63) | |
| At least 1 previous event | men | 46.70 (10.35) | 50.00 (13.15) |
| women | 43.00 (6.83) | 47.00 (5.00) | |
| Total | 46.24 (9.90) | 49.64 (12.42) | |
| Social HRQoL | |||
| No previous events | men | 37.35 (8.09) | 41.10 (7.01) |
| women | 31.88 (9.76) | 37.14 (9.11) | |
| Total | 36.48 (8.56) | 40.50 (7.44) | |
| At least 1 previous event | men | 36.01(8.10) | 37.82 (7.06) |
| women | 32.17 (2.57) | 35.33 (3.51) | |
| Total | 35.54 (7.72) | 37.52 (6.73) | |
| SCL-90 Depression | |||
| No previous events | men | 1.39 (0.14) | 1.34 (0.13) |
| women | 1.45 (0.17) | 1.39 (0.17) | |
| Total | 1.40 (0.15) | 1.35 (0.14) | |
| At least 1 previous event | men | 1.45 (0.13) | 1.44 (0.13) |
| women | 1.51 (0.11) | 1.47 (0.11) | |
| Total | 1.45 (0.13) | 1.44 (0.13) | |
The SCL-90R depression subscale was transformed using LOG10 in order to normalize the data.
Of note, p values were not incorporated into this table. Significant differences can be found in Table 2.
Health-related quality of life and depression 6 months post-cardiac event
Impact of Cardiac History
Multiple linear regression analyses showed that a cardiac history was not predictive of a worse HRQoL at follow-up. Gender was significant on the social HRQoL subscale (women had lower mean scores compared to men) and the CABG variable was also significant at follow-up on the emotional HRQoL subscale (CABG patients indicated a better emotional HRQoL) (see Table 4). It is noteworthy to mention that patients with a cardiac history did indicate lower follow-up mean scores on the MacNew HRQoL questionnaire (see Table 3).
Table 4.
Cardiac history and angina as predictors of impaired HRQL and psychological distress at follow-up
| β | sr2 | 95% Confidence Interval | ||
|---|---|---|---|---|
| Emotional HRQoL | Lower Bound | Upper Bound | ||
| Cardiac history | −.090 | −.089 | −8.552 | 3.149 |
| Angina Pectoris | .304⊥ | .305 | 3.391 | 13.581 |
| Gender | −.134 | −.145 | −10.666 | 1.464 |
| Age | −.029 | −.031 | −.327 | .237 |
| PCI | −.329 | −.149 | −18.718 | 2.253 |
| CABG | −.367* | −.193 | −21.869 | −.208 |
| MI | −.232 | −.109 | −16.607 | 4.531 |
| Physical HRQoL | ||||
| Cardiac history | −.113 | −.115 | −8.206 | 2.094 |
| Angina Pectoris | .336⊥ | .341 | 4.004 | 13.249 |
| Gender | −.137 | −.151 | −9.995 | 1.204 |
| Age | −.028 | −.030 | −.294 | .215 |
| PCI | −.377 | −.176 | −18.092 | .744 |
| CABG | −.311 | −.169 | −18.161 | 1.156 |
| MI | −.249 | −.120 | −15.386 | 3.564 |
| Social HRQoL | ||||
| Cardiac history | −.113 | −.110 | −5.511 | 1.520 |
| Angina Pectoris | .261+ | .260 | 1.212 | 7.523 |
| Gender | −.187* | −.195 | −7.733 | −.089 |
| Age | −.013 | −.014 | −.186 | .161 |
| PCI | .015 | .007 | −6.206 | 6.652 |
| CABG | .070 | .037 | −5.334 | 7.852 |
| MI | .069 | .032 | −5.391 | 7.545 |
| SCL-90 Depression | ||||
| Cardiac history | .206 * | .199 | .003 | .137 |
| Angina Pectoris | −.204 * | −.206 | −.125 | −.005 |
| Gender | .127 | .135 | −.021 | .120 |
| Age | .019 | .020 | −.003 | .004 |
| PCI | .287 | .121 | −.048 | .211 |
| CABG | .220 | .107 | −.059 | .207 |
| MI | .246 | .107 | −.058 | .203 |
p < 0.05;
p < 0.01;
p < 0.001
The SCL-90R depression subscale was transformed using LOG10 in order to normalize the data.
Moreover, the follow-up analysis showed that cardiac history was significantly predictive of higher depression levels (p = .042) (Table 4). The effect size is 0.2, which is considered a small effect according to Cohen’s standard.
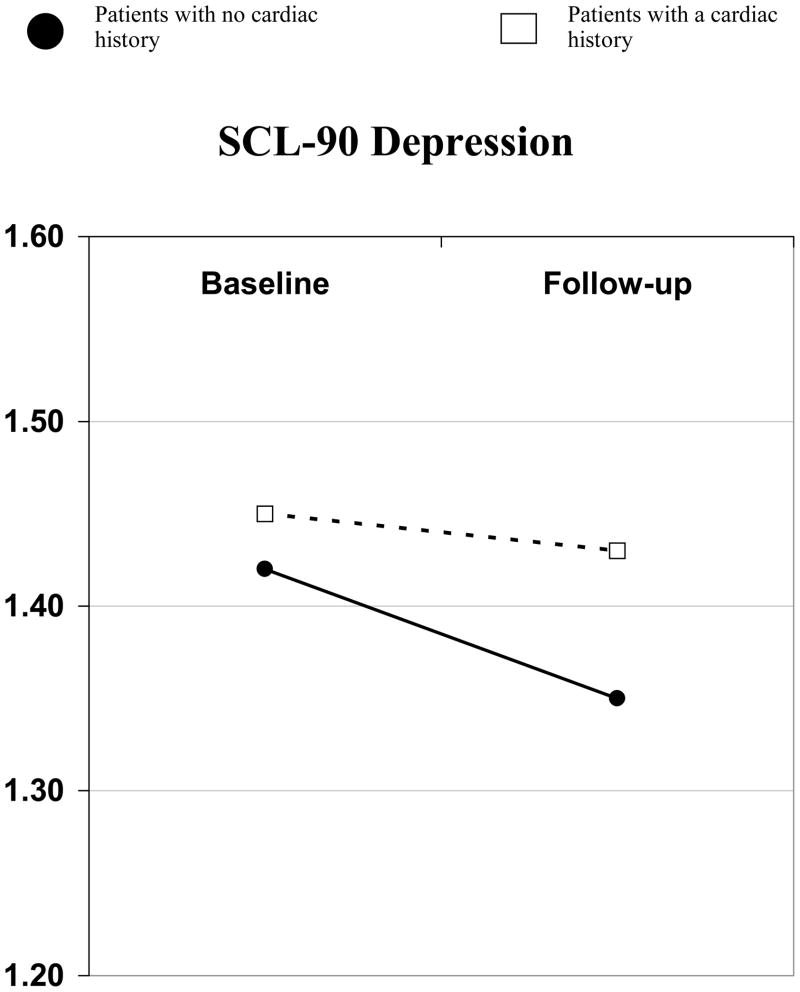
The results suggest that there may be two different basic recovery trajectories based on whether a patient has or has not experienced a prior cardiac event. The results may indicate that patients with a cardiac history are recovering differently than patients with no previous cardiac event (specifically with regard to depression). Figure 1 depicts the different pathways of recovery for depression.
Figure 1. Presence Versus Absence of Previous Cardiac Events Give Rise to Distinct Trajectories of Recovery on Depression Mean Subscale Scores.
Depression at 6 Months stratified by Previous Cardiac History*
* Linear Regression. A higher score indicates higher depression levels.
Angina Pectoris
The angina variable was coded into two groups. The first group consisted of patients that had angina at follow-up. The second group did not have angina at the 6-month measurement.
Descriptive analyses showed that at follow-up, only 2% of bypass patients reported angina, whereas 20% of PCI and 27% of MI patients reported that they were experiencing angina at the second measurement (data not shown).
The linear regression analyses showed that angina at follow-up was predictive of a significantly worse emotional (p = .006), physical (p = .001), and social (p = .042) HRQoL, and a higher depression level on the SCL-90 (p = .041) (See Table 4).
Additional analyses, controlling for HRQoL and depression subscale scores at baseline, revealed that, whereas the impact of angina on overall emotional, physical, and social HRQoL and depression at follow-up remained significant, the impact of cardiac history on depression no longer was (data not shown).
Discussion
Summary of Main Findings
The main objective of the present study was to examine whether a cardiac history (presence versus absence of previous cardiac events), and the presence of angina six months after hospital admittance for an MI, PCI, or CABG have a significant impact on physical, social and emotional HRQoL and depression in a CHD population.
Very little research has been conducted on the impact of cardiac history on multidimensional HRQoL and depression in patients with heart disease. The findings of the present study showed that both at baseline and at follow-up there were no significant differences on emotional, physical and social HRQoL between patients with and without a cardiac history. With respect to depression, significant differences were found at 6 months follow-up on this dimension. The depression scores of patients with a cardiac history seem to remain stable over the 6-month follow-up period, whereas the level of depression in patients without a cardiac history decreases over time (Figure 1).
It is noteworthy to mention that although a significant difference with respect to cardiac history was only found for depression, patients with a cardiac history also had a lower overall HRQoL mean scores compared to patients that had never experienced a cardiac event (linear regression however failed to find significance).
At the six-month follow-up, patients with angina reported significantly worse HRQoL and higher depression levels.
Clinical relevance of working towards improving HRQoL in patients after multiple events - and not just accepting it
The findings suggest that, from a psychological point of view, patients with and without previous cardiac events, may be functioning at similar levels at baseline, but differently at follow-up. Perhaps after experiencing a cardiac event, both groups might be feeling a moment of optimism, thinking that a cardiac procedure and/or lifestyle change will improve their life and life chances. However, as time continues, the fact that symptoms and stresses do not fade easily, might have a bigger impact on patients who have experienced a prior cardiac event.
Existing literature shows that after a cardiac event, patients are confronted with a number of challenges, ranging from the management of chest pain, to coping with imposed lifestyle changes, and an uncertain future. The stress of these challenges results in a significant number of individuals experiencing considerable psychological and life difficulties which interfere with their daily functioning.24 Those patients who had already experienced all the life adjustments and stresses the first time around, only to have another cardiac episode, would most likely experience all the above in an even more intensive manner, particularly a fear of an uncertain future.
The findings in the present study indicate a clinical relevance with respect to patients whom have experienced a repeat cardiac event. As patients with a cardiac history are reporting higher depression levels, it seems critical to identify these patients when developing treatment programs. Identification and targeting of patients with a cardiac history in cardiac rehabilitation (CR) or home-based programs may be important in reducing depression, stress and worry in everyday life. Targeting these patients may help to improve daily functioning and decrease morbidity and mortality rates.
With respect to angina, the results of the present study indicate that patients who continue to experience angina symptoms six months after their cardiac event, report significantly worse emotional, physical and social quality of life, and a significantly higher level of depression than patients without angina. At follow-up only 2% of bypass patients reported angina; however, 20% and 27% of PCI and MI patients reported angina respectively.
With respect to angina, the results of the present study indicate that patients who continue to experience angina symptoms six months after their cardiac event, report significantly worse emotional, physical and social quality of life, and a significantly higher level of depression than patients without angina. At follow-up only 2% of bypass patients reported angina; however, 20% and 27% of PCI and MI patients reported angina respectively. As patients with still existing angina at follow-up are relatively in the MI and PCI groups, this may been an indication of still existing myocardial ischemia resulting from incomplete revascularization or the inability of the patient to be amenable with PCI or CABG after an MI. Not all patients with angina (and heart disease in general) are treatable with revascularization due to the nature of the disease.
The results of worse perceived HRQoL among patients with angina compared to patients without angina support previous findings.7,17,25 Although the present study supports these findings, the results add to the notion that angina patients do have a worse HRQoL, and that this functional status remains impaired on all of the multi-dimensional subscales 6 months post-cardiac event. This study indicates that this group of patients may not be recovering as quickly as the other patients in the sample. This study supports the idea that patients with angina should be frequently monitored in the months after a post-cardiac event, and not just before or immediately after an MI or invasive procedure. The evaluation of physical and mental health remains an important task when managing angina patients. It is important that patients with stable angina do not get lost to follow-up, as these patients are indeed as important to manage as patients with an acute cardiac event.
States of distress (inclusive of depression), have been shown in recent studies to be associated with myocardial ischemia,18,26 as well as an increased rate of morbidity and mortality from cardiac events.13–15,18,27 Therefore, it is important to recognize that CHD patients with angina may be at a higher risk for future complications, and even death. A study by Springer et al. [18] states that ‘refractory angina, in which pain continues to occur even after medication and surgical remedies, can worsen a patient’s functional disability and lead to heightened negative emotional states of stress, anxiety, and depression’. The authors also state that if these conditions continue, then they may negatively affect morbidity and mortality.
Although there seems to be a consensus that angina is associated with depression,11 the direction of this relationship remains unclear. The present study suggests that depression may be the result of angina; however, the review by Ketterer et al. [11] shows that depression was a predictor of anginal chest pain symptoms in at least two studies. 28,29 In fact, it may be proposed from the results of the present study and previous studies, that there is an indication of a vicious circle in the CHD population. A number of studies show that depression may be a predictor of angina, and in other cases, depression may be the result of the angina condition. Ketterer et al. [11] state that depression is common in pain syndromes, specifically angina, and that these psychiatric conditions may worsen symptoms experienced by angina patients. In any case, it seems that research indicates that states of depression and angina influence one another.
Whether a predictor or the result of angina, the treatment of depression is important in patients that are admitted to comprehensive CR programs. The treatment of depression (and also targeting other emotional components such as anger and anxiety) has been shown to reduce anginal symptoms,30–34 hospital readmissions, and recurring cardiac events in angina patients.11 The results of these studies demonstrate the treatment of depression may help break the vicious circle (in which angina symptoms and depression influence one another) in order to prevent, control, and reduce anginal symptoms that are intensified by depression (and other psychiatric conditions).
Limitations of this Study
The results of this study should be interpreted with some caution. Firstly, we did not collect objective medical information such as the presence of comorbid medical conditions (e.g. diabetes mellitus) or family history of heart disease, which are known prognostic indicators. This may have somewhat biased our results. Therefore, future studies within this domain should control for these factors. Secondly, angina status was not assessed in the regression analysis at baseline due to logistical reasons. Thus we do not know what differences - if any - existed between angina and angina-free patients at the first measurement. Nevertheless, assessment of psychological symptoms at the time of a cardiac procedure has not been shown to be an optimal time point, as symptoms may reflect distress related to the procedure.35 In the early months following a cardiac event, it may be difficult for patients to distinguish between chest discomfort caused by anxiety and depression rather than by angina. It is however important to mention that angina has been an established predictor of HRQoL and psychological distress, therefore the results of the current study may not have been affected due to this missing data. Another limitation of the study is that the sample consists of many more men than women. There may be several reasons for the higher inclusion of men in the sample population. Firstly, patients were recruited partly from one of two cardiac rehabilitation (CR) centers. It has been shown in the literature that fewer female patients participate in CR,36,37 thus this could have been part of the reason that fewer women were recruited to participate in this study. Secondly, women are generally older and have more comorbidities than men with heart disease. Older women (over the age of 70) and women with other serious diseases (i.e. cancer or renal failure) would have been excluded from participating. As literature indicates that women are less likely to participate in research that evaluates heart disease, future studies should actively recruit women to be included in the study population.
Conclusions
Implications for Future Research and Clinical Practice
In the current study, angina was measured by self report. It would be useful for future research to consider tracking cardiac patients observationally over time, and having participants wear a Holter monitoring device and/or by administering ECGs at several time points to assess ischemia. Along with self report, these tests may help accurately define angina at an earlier stage after a cardiac event. Further, future research should collect thorough clinical data, and objectively assess anginal frequency at several time points.
The results of the present study indicate that the presence of continuing or recurrent angina symptoms six months after a cardiac event is predictive of worse overall HRQoL and higher levels of depression in CHD patients. In order to prevent the development of a vicious circle characterized by the fact that angina and depression continuously influence each other in a negative way, psychological assessment and interventions are considered to be important components of CR. They may especially be vital in the first months after a cardiac event as patients are beginning their recovery and adjusting to new lifestyle changes. The impact of cardiac history on depression six months after a cardiac event should be further explored, as it may reveal itself to be an important prognostic factor for the development of psychological distress in CHD patients.
Acknowledgments
The present study was based upon data from the Health Psychology Department at Leiden University in the Netherlands. This project was funded by the Netherlands Heart Foundation (2000B040).
Contributor Information
Shannon Gravely-Witte, University Health Network Women’s Health Program, Toronto General Hospital, EN7-235, 200 Elizabeth St., Toronto, ON M5G 2C4, Phone: (416) 340-4800 ext. 6987, Fax: (416) 340-4185.
Véronique De Gucht, Leiden University, KLIG, 2300 RB Leiden, The Netherlands.
Willem Heiser, Leiden University, KLIG, 2300 RB Leiden, The Netherlands.
Sherry L Grace, York University, Faculty of Health, TGRI Behavioural Sciences Bethune, 4700 Keele St. Toronto, ON M3J 1P3, Canada.
Thérèse van Elderen, Leiden University, KLIG, 2300 RB Leiden, The Netherlands.
References
- 1.Sampalis J, Boukas S, Liberman M, Reid T, Dupuis G. Impact of waiting time on the quality of life of patients awaiting coronary artery bypass grafting. Can Med Assoc J. 2001;165 (4):429. [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor S. Health Psychology. Los Angeles: McGraw Hill; 2003. [Google Scholar]
- 3.Sieber WJ, Kaplan RM. Assessing the Utility of Behavioral Medicine Interventions: Quantifying Health-Related Quality of Life. Brunner – Routledge. 2001 [Google Scholar]
- 4.Roebuck A, Furze G, Thompson DR. Health-related quality of life after myocardial infarction: an interview study. J Adv Nurs. 2001;34(6):787–94. doi: 10.1046/j.1365-2648.2001.01809.x. [DOI] [PubMed] [Google Scholar]
- 5.Timmis AD, Feder G, Hemingway H. Prognosis of stable angina pectoris: why we need larger population studies with higher endpoint resolution. Heart. 2006 doi: 10.1136/hrt.2006.103119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts R. Stable angina as a manifestation of ischemic heart disease: medical management. Circulation. 1985 Dec;72(6 Pt 2):V145–54. [PubMed] [Google Scholar]
- 7.Pocock SJ, Henderson RA, Seed P, Treasure T, Hampton JR. Quality of life, employment status, and anginal symptoms after coronary angioplasty or bypass surgery. Circulation. 1996;94(2):135–41. doi: 10.1161/01.cir.94.2.135. [DOI] [PubMed] [Google Scholar]
- 8.Bengtsson I, Hagman M, Wedel H. Age and angina as predictors of quality of life after myocardial infarction. Scand Cardiol J. 2001;35:252–58. doi: 10.1080/14017430152581369. [DOI] [PubMed] [Google Scholar]
- 9.Niamh F, Murphy NF, Stewart S, Hart CL, MacIntyre KP, Hole D, McMurray JJV. A population study of the long-term consequences of Rose angina: 20 year follow-up of the Renfrew-Paisley study. Heart Published Online First. 2006 Jun 28; doi: 10.1136/hrt.2006.090118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brorsson B, Bernstein SJ, Brook RH, Werko L. Quality of life of patients with chronic stable angina before and four years after coronary revascularisation compared with a normal population. Heart. 2002;87:140–145. doi: 10.1136/heart.87.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ketterer MW, Mahr G, Cao JJ, Hudson M, Smith S, Knysz W. What’s unstable in unstable angina? Psychosomatics. 2004 Jun;45(3):1–12. doi: 10.1176/appi.psy.45.3.185. [DOI] [PubMed] [Google Scholar]
- 12.Blumenthal JA, Lett HS, Babyak MA, White W, Smith PK, Mark DB, Jones R, Mathew JP, Newman MF NORG Investigators. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet. 2003;362(9384):604–9. doi: 10.1016/S0140-6736(03)14190-6. [DOI] [PubMed] [Google Scholar]
- 13.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction: impact on 6-month survival. JAMA. 1993;270:1819–25. [PubMed] [Google Scholar]
- 14.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after a myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- 15.Frasure-Smith N, Lesperance F, Talajic M. The impact of negative emotions on prognosis following myocardial infarction: is it more than depression? Health Psychol. 1995;14:388–98. doi: 10.1037//0278-6133.14.5.388. [DOI] [PubMed] [Google Scholar]
- 16.Sadovsky R. Depression after AMI increases mortality risk. Family Physician. 2002. Feb 15, Retreived April 24, 2004, from www.findarticles.com.
- 17.Schrader G, Cheo F, Hordacre AL, Guiver N. Predictors of depression three months after cardiac hospitalization. J Psychosom Med. 2004;66(4):514–20. doi: 10.1097/01.psy.0000128901.58513.db. [DOI] [PubMed] [Google Scholar]
- 18.Springer S, Fife A, Lawson W, Hui J, Jandorf L, Cohn P, Fricchione G. Psychological Effects of Enhanced External Counterpulsation in the Angina Patient: A second Study. Psychosomatics. 2001;42:124–32. doi: 10.1176/appi.psy.42.2.124. [DOI] [PubMed] [Google Scholar]
- 19.Van Elderen T, Maes S, Boersma S. Leiden Screening Questionnaire for Heart Patients. Leiden University, Department of Health Psychology; 2000. [Google Scholar]
- 20.De Gucht V, Van Elderen T, Van Der Kamp L, Oldridge N. Quality of life after myocardial infarction: Translation and validation of the MacNew Questionnaire for a Dutch population. Quality of Life Research. 2004;13:1483–88. doi: 10.1023/B:QURE.0000040792.25240.38. [DOI] [PubMed] [Google Scholar]
- 21.Arrindell WA, Ettema JMH. SCL-90: Handeling bij een multidimensionele psychopathologie-indicator. Lisse: Swets & Zeitlinger; 1986. [Google Scholar]
- 22.Arrindell WA, Ettema JMH. SCL-90: Handeling bij een multidimensionele psychopathologie-indicator. Lisse: Swets Test Publishers; 2003. [Google Scholar]
- 23.Derogratis LR. SCL-90R: Administration, scoring and procedures manual-II. 2. Baltimore: Clin Psych Res; 1983. [Google Scholar]
- 24.Kaoukis GT. The role of psychological factors in adjusting to cardiovascular events. Newsbeat Newsletter. 2001 Apr;9(1) Retrieved March 25, 2004, from www.findarticles.com. [Google Scholar]
- 25.Wahrborg P. Quality of life after coronary angioplasty or bypass surgery. 1-year follow-up in the Coronary Angioplasty versus Bypass Revascularization investigation (CABRI) trial. Eur Heart J. 1999;20(9):653–58. doi: 10.1053/euhj.1998.1237. [DOI] [PubMed] [Google Scholar]
- 26.Rozanski A, Bairey CN, Krantz DS. Mental stress and the induction of silent myocardial ischemia in patients with coronary artery disease. N Engl J Med. 1988;318:1005–12. doi: 10.1056/NEJM198804213181601. [DOI] [PubMed] [Google Scholar]
- 27.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 28.Hallstrom T, Lapidus L, Bengtsson C, Edstrom K. Psychosocial factors and risk of ischemic heart disease and death in women: a twelve-year follow-up of participants in the population study of women in Gothenburg, Sweden. J Psychosom Res. 1986;39:451–9. doi: 10.1016/0022-3999(86)90084-x. [DOI] [PubMed] [Google Scholar]
- 29.Ladwig KH, Roll G, Breithardt G, Borggrefe M. Extracardiac contributions to chest pain perception in patients 6 months after acute myocardial infarction. Am Heart J. 1999;136:528–35. doi: 10.1016/s0002-8703(99)70502-8. [DOI] [PubMed] [Google Scholar]
- 30.Amorosa-Tupler B, Tapp JT, Cardia RV. Stress management through relaxation and imagery in the treatment of angina pectoris. J Cardiopulm Rehab. 1989;11:257–64. [Google Scholar]
- 31.Blumenthal JA, Jiang W, Babyak MA, Krantz DS, Frid DJ, Coleman RE, Waugh R, Hanson M, Appelbaum M, O’Connor C, Morris JJ. Stress management and exercise training in cardiac patients with myocardial ischemia. Arch Intern Med. 1997;157:2213–23. [PubMed] [Google Scholar]
- 32.Gallacher JEJ, Hopkinson CA, Bennett P, Burr ML, Elwood PC. Effect of stress management on angina. Psychol Health. 1997;12:523–32. [Google Scholar]
- 33.Ketterer MW, Fitzgerald F, Keteyian S, Thayer B, Jordon M, McGowan C, Mahr G, Manganas A, Goldberg AD. Chest pain and the treatment of psychosocial/emotional distress in CAD patients. J Behav Med. 2000;23:437–50. doi: 10.1023/a:1005521014919. [DOI] [PubMed] [Google Scholar]
- 34.Lewin RJ, Furze G, Robinson J, Griffith K, Wiseman S, Pye M, Boyle R. A randomized controlled trial of a self-management plan for patients with newly diagnosed angina. Br J Gen Pract. 1994;52:194–6. [PMC free article] [PubMed] [Google Scholar]
- 35.Poston WS, Haddock CK, Conard MW, Jones P, Spertus J. Assessing depression in the cardiac patient: When is the appropriate time to assess depression in the patient undergoing coronary revascularization? Behav Mod. 2003 Jan;27(1):26–36. doi: 10.1177/0145445502238691. [DOI] [PubMed] [Google Scholar]
- 36.Grace SL, Evindar A, Kung TN, Scholey PE, Stewart DE. Automatic referral to cardiac rehabilitation. Med Care. 2004 Jul;42(7):661–9. doi: 10.1097/01.mlr.0000129901.05299.aa. [DOI] [PubMed] [Google Scholar]
- 37.Halm M, Penque S, Doll N, Beahrs M. Women and cardiac rehabilitation: referral and compliance patterns. J Cardiovasc Nurs. 1999 Apr;13(3):83–92. doi: 10.1097/00005082-199904000-00008. [DOI] [PubMed] [Google Scholar]