Abstract
Background and objectives: Ongoing randomized trials seek to validate the efficacy of rituximab as an induction agent for anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV). However, no studies directly address the role of rituximab as maintenance therapy.
Design, setting, participants, & measurements: This retrospective study reports the authors' experience with continuous rituximab administration in 39 patients in complete or partial remission at the time of rituximab initiation. All 39 patients had at least 1 year of follow-up, and 20 had 2 years of follow-up.
Results: Disease activity, as measured by a modified Birmingham Vasculitis Activity Score, decreased from a median of 1 at baseline to 0 at 12 (P < 0.001) and 24 months (P = 0.02). Three patients experienced nonorgan-threatening flares during 708 patient-months of follow-up. Each flare occurred after at least 20 months of follow-up. The percentage of patients on cytotoxic immunosuppression decreased from 87% at baseline to 41% at 12 months (P < 0.001) and 30% at 24 months (P = 0.002). The percentage of patients on prednisone decreased from 92% at baseline to 59% at 12 months (P < 0.001) and 55% at 24 months (P = 0.02). Two patients developed late-onset neutropenia; both responded to treatment with recombinant granulocyte colony-stimulating factor.
Conclusions: The successful use of continuous anti-B cell therapy in patients with AAV in complete or partial remission is reported. This extends the potential role of rituximab beyond induction to include maintenance therapy. However, more data are required regarding the delayed adverse effects of rituximab.
Anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is a chronic, relapsing, and systemic disease. Current evidence supports the use of cytotoxic therapy (e.g., cyclophosphamide) in conjunction with glucocorticoids for primary therapy of AAV (1,2). Maintenance of remission requires less toxic alternatives to cyclophosphamide, including azathioprine, methotrexate, mycophenolate mofetil, or leflunomide (3–5). Although this array of treatment options has dramatically improved outcomes with AAV, adverse effects related to these medications can arise as competing concerns.
Increasing appreciation for the role of ANCA in AAV pathogenesis has been reinforced by the clinical efficacy of B cell depletion using rituximab (6–9). Rituximab is a chimeric monoclonal antibody directed against the B cell specific antigen CD20 and is currently approved for the treatment of B cell lymphoma and rheumatoid arthritis (10,11). Small studies of rituximab in AAV have focused on patients with refractory disease and have generally described high rates of remission (12–18). Recently, a multicenter study of 65 patients with refractory AAV demonstrated a 75% complete remission rate with rituximab (19).
Interest in rituximab as a primary agent has motivated ongoing randomized clinical trials that include its use in the treatment of newly diagnosed AAV, as well as refractory AAV. In RITUXVAS, rituximab is added to an induction regimen that includes cyclophosphamide, whereas in RAVE, it is compared directly against cyclophosphamide (20). Full results of these important trials are eagerly awaited.
As the efficacy of rituximab as initial or rescue therapy in AAV continues to be defined, an open question remains regarding its role in maintenance of remission. Such an approach has the potential to control disease activity and decrease the cumulative toxicity of other immunosuppressive agents. However, little attention has been directed to this strategy thus far. In this retrospective study, we report the continuous use of rituximab in 39 patients in complete or partial remission at the time of rituximab initiation. Specific attention is directed to disease control, medication burden, and adverse effects with continuous anti-B cell therapy.
Materials and Methods
We conducted a retrospective review of the electronic medical record of all patients in our practice with AAV treated with rituximab. Study inclusion required continuous therapy with rituximab for ≥1 year after attainment of complete or partial remission. Patients receiving rituximab at initial diagnosis as primary therapy were excluded. All patients were initiated on rituximab between April 2006 and September 2008. Disease activity was assessed using the Disease-Specific Activity Index for Wegener's Granulomatosis: Modification of the Birmingham Vasculitis Activity Score (BVAS/WG) (21). Complete remission was defined as a BVAS/WG of 0. Partial remission was defined as a BVAS/WG ≤50% of the value at disease diagnosis. Disease flare was defined as an increase in BVAS/WG of ≥2. Other data, collected at baseline and at each rituximab infusion, included medications, complete blood counts, and ANCA titers. Flow cytometry to monitor B cell clearance was followed approximately every 4 months. ANCA testing was performed on-site and included indirect immunofluorescence and ELISAs for anti-proteinase 3 (PR3) and anti-myeloperoxidase (MPO) antibodies (22). For PR3, a titer ≥20 is considered positive. For MPO, a titer ≥2.8 is considered positive.
Thirty-five of 39 patients were initiated on rituximab with two 1-g doses given 2 weeks apart; the other four were given four weekly doses of 375 mg/m2. Upon initiation, all patients were scheduled to receive a single 1-g dose every 4 months. Thirty-three of 39 patients followed this schedule without interruption. Five of 39 patients had at least one, but no more than two, 6-month intervals between doses. One patient received two 0.5-g doses, 1 week apart, every 4 months. Each dose was coadministered with 100 mg of intravenous hydrocortisone, 25 to 50 mg of oral diphenhydramine, and 650 mg of oral acetaminophen. All patients gave written, informed consent for the off-label use of rituximab. After rituximab initiation, other immunosuppression was generally weaned at 4-month intervals as tolerated; specific decisions regarding immunosuppression withdrawal were individualized to each patient.
Statistical analyses were performed using JMP (version 8.01, Cary, NC). Changes in median BVAS/WG scores and medication doses were assessed using the Wilcoxon signed-rank test or Wilcoxon rank-sum test, as appropriate. Changes in ANCA titers (log-transformed) were assessed using the t test. Changes in the proportion of patients on cytotoxic therapy and steroids were compared using McNemar's test. Statistical significance was set at P < 0.05.
Results
Study Population
Table 1 outlines the study population. Because of the uncertainties involved in subclassifying AAV, we did not assign specific diagnoses of Wegener's granulomatosis versus microscopic polyangiitis. However, 30 of the 39 patients did have eye, ear, nose, sinus, or upper airway manifestations consistent with Wegener's granulomatosis. No patients had the Churg–Strauss syndrome. All patients were ANCA positive at initial diagnosis, 24 with a positive c-ANCA (anti-PR3) and 15 with a positive p-ANCA (anti-MPO). The median BVAS/WG at the time of AAV diagnosis was 5. At AAV diagnosis, 17 patients had acute renal failure with biopsy evidence of GN and/or erythrocyte casts on urine sediment. Disease duration before starting rituximab varied widely, with a median of 67 months (range 3 to 506 months) before initiation. At the time of rituximab initiation, median BVAS/WG was 1. Seventeen of 39 subjects were in complete remission at rituximab initiation (BVAS/WG = 0); the remaining 22 subjects had BVAS/WG values from 1 to 4. No subjects had organ-threatening disease at the time of rituximab initiation.
Table 1.
Baseline characteristics of the study sample
| Characteristics | Complete Remission at Rituximab Initiation | Partial Remission at Rituximab Initiation | Combined |
|---|---|---|---|
| Number | 17 | 22 | 39 |
| Number with anti-PR3/anti-MPO | 11/6 | 13/9 | 24/15 |
| Median age (range) | 63 (25 to 87) | 59.5 (39 to 88) | 60 (25 to 88) |
| Women (percent) | 6 (35%) | 14 (64%) | 20 (51%) |
| Median BVAS/WG at AAV diagnosis (range) | 5 (1 to 8) | 4.5 (1 to 9) | 5 (1 to 9) |
| Median BVAS/WG at rituximab initiation (range) | 0 (NA) | 2 (1 to 4) | 1 (1 to 4) |
| Median duration before rituximab, months (range) | 51 (3 to 282) | 71.5 (3 to 506) | 67 (3 to 506) |
| Number of relapses at rituximab initiation | |||
| 0 | 8 | 5 | 13 |
| 1 to 2 | 7 | 11 | 18 |
| >2 | 2 | 6 | 8 |
| 12 months of follow-up available | 11 | 8 | 19 |
| 24 months of follow-up available | 6 | 14 | 20 |
NA, not applicable.
The indications for rituximab initiation were heterogeneous and overlapping (Table 2). For patients in partial remission, a major indication was the persistence of nonorgan-threatening symptoms despite high-dose maintenance immunosuppression. Examples included nasal or sinus complaints (n = 4) and/or arthritis/arthralgias (n = 4). Eleven patients had limiting adverse effects of chronic prednisone use, including significant weight gain and/or cushingoid features (n = 5), worsening control of diabetes (n = 2), avascular necrosis (n = 2), and osteoporotic fracture (n = 2). Five patients experienced dose-limiting bone marrow toxicity with cytotoxic agents, including macrocytic anemia with azathioprine (n = 3), neutropenia with cyclophosphamide (n = 1), and pancytopenia with methotrexate (n = 1). Eight patients had a history of multiple flares on maintenance therapy requiring repeated cycles of cyclophosphamide, including one patient with hemorrhagic cystitis. Fourteen patients had rising or persistently elevated ANCA titers—in most patients, this was accompanied by an additional indication for rituximab initiation. Overall, each decision to use rituximab represented an individualized decision reflecting the patient's disease control, immunosuppressive doses, adverse effects attributable to immunosuppression, and patient preference.
Table 2.
Indications for initiation of rituximab
| Indications | Complete Remission at Rituximab Initiation (n = 17) | Partial Remission at Rituximab Initiation (n = 22) | Combined |
|---|---|---|---|
| Persistent symptoms attributable to AAV | 0 | 8 | 8 |
| Cyclophosphamide dependence (with or without symptoms) | 4 | 4 | 8 |
| Bone marrow toxicity | 2 | 3 | 5 |
| Steroid toxicity (e.g., weight gain, diabetes, avascular necrosis, osteoporotic fracture) | 6 | 5 | 11 |
| Rising or persistently high ANCA | 4 | 10 | 14 |
| Othera | 2 | 2 | 4 |
Other includes severe fatigue (n = 2), patient desire to wean oral immunosuppression (n = 1), and bacterial pneumonia on cyclophosphamide and prednisone (n = 1).
All 39 patients had at least 1 year of follow-up, and 20 patients had at least 2 years of follow-up after the initiation of rituximab. This constitutes 708 patient-months of follow-up, spanning 253 administered doses of rituximab.
Clinical Outcomes
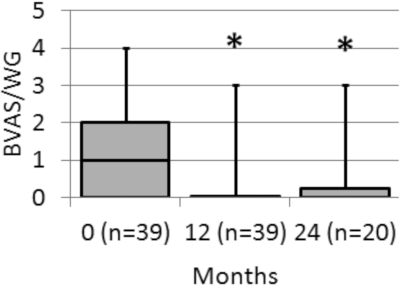
Continuous therapy with rituximab was associated with ongoing disease control. All patients achieved B cell depletion, and remained B cell depleted throughout the course of the study. Median BVAS/WG at initiation was 1, and was 0 at 4, 8, and 12 months of follow-up (P < 0.001 for time 0 versus 12, Figure 1). In the subset of 20 patients with 2 years of follow-up, median BVAS/WG remained at 0 at 24 months (P = 0.02 for time 0 versus 24). All 17 patients who were in complete remission at rituximab initiation (i.e., BVAS/WG = 0) remained in complete remission at 12 months; at 24 months of follow-up, 5 of 6 patients (83%) remained in complete remission. Of the 22 patients who were in partial remission at initiation, 14 (64%) were in complete remission at 12 months; at 24 months, 10 of 14 patients (71%) were in complete remission. No patients experienced organ-threatening disease activity, including no recurrence of GN.
Figure 1.
Median BVAS/WG with rituximab treatment. Box plot shows upper and lower quartiles; whiskers show maximum values. *P < 0.05 compared with time 0.
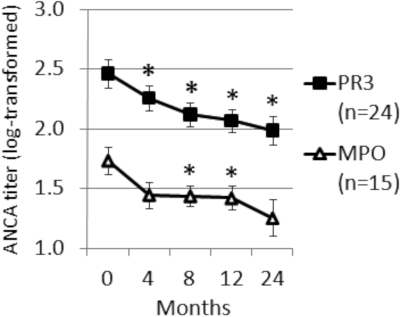
Although most patients experienced control of disease activity, three patients had flares (defined as a rise in BVAS/WG of ≥2) during continuous treatment with rituximab. One of these patients had initiated rituximab while in complete remission. He was able to wean completely off cyclophosphamide and prednisone, but presented with tracheitis and bronchitis at 20 months. A second patient was in partial remission with a BVAS/WG of 1 at the time of rituximab initiation. Although he tolerated gradual cessation of mycophenolate mofetil, he experienced worsening arthritis and recurrent subglottic inflammation and otitis with prednisone withdrawal at 22 months. A third patient experienced a rise in BVAS/WG from 2 to 4 at 23 months. This flare consisted of nasal crusting and sinusitis, along with recurrent subglottic inflammation and a new lung nodule. As with the second patient, this occurred with an attempt to stop prednisone. Although ANCA titers were positive in all three patients at the time of flare, no appreciable rise in ANCA titer was noted at the time of or in the months preceding the flares. Furthermore, flow cytometry performed at the time of disease flares demonstrated no detectable CD20-positive B cells. Figure 2 shows the fall in ANCA titers across all patients during the study period.
Figure 2.
Mean ANCA titers (log-transformed) with rituximab treatment. Error bars show SEM. *P < 0.05 compared with time 0.
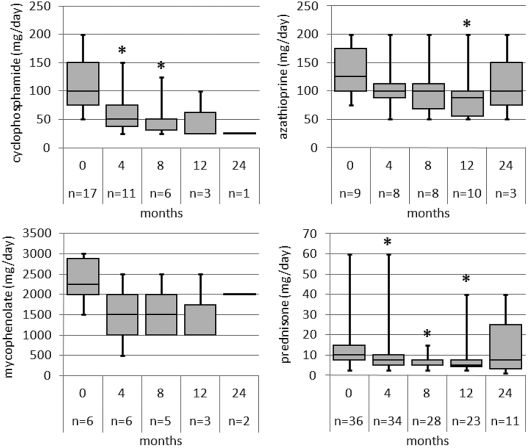
Disease control with the addition of rituximab facilitated the withdrawal of other immunosuppressive agents. Figure 3 depicts the decrease in median doses of immunosuppressive medications at 0, 4, 8, 12, and 24 months (methotrexate is not shown). Among the 39 patients with at least 1 year of follow-up, at time 0, 17 patients were on cyclophosphamide (median dose 100 mg/d), 9 patients were on azathioprine (125 mg/d), 6 patients were on mycophenolate mofetil (2250 mg/d), and 2 patients were on methotrexate (23 mg/d). A total of 34 patients (87%) were on some form of cytotoxic treatment. Thirty-six of the 39 patients (92%) were on prednisone at a median dose of 10 mg/d; only 1 patient was not on any form of immunosuppression. At 12 months of follow-up, a total of 16 patients (41%, P < 0.001 compared with 87% at time 0) remained on cytotoxic therapy, with 3 patients on cyclophosphamide (25 mg/d), 10 on azathioprine (88 mg/d), 3 on mycophenolate mofetil (1000 mg/d), and no patients on methotrexate. A total of 23 patients (59%, P < 0.001 compared with 92% at time 0) remained on prednisone at a median dose of 5 mg/d. A total of 10 patients (26%, P = 0.011 compared with 3% at time 0) were able to wean completely off cytotoxic therapy and prednisone. Among the 20 patients with 2 years of follow-up, 6 patients (30%, P = 0.002 versus time 0) remained on cytotoxic therapy at 24 months and 11 patients (55%, P = 0.02 versus time 0) remained on prednisone; 8 of 20 patients (40%, P = 0.039 versus time 0) were completely off cytotoxic therapy and prednisone. The dose of prednisone at 24 months was not significantly different from baseline, reflecting the decreased number of patients on prednisone and the intensified treatment of three patients with clinical flares.
Figure 3.
Median medication doses with rituximab treatment. Box plot shows upper and lower quartiles; whiskers show maximum and minimum values. *P < 0.05 compared with time 0.
Adverse Events
Rituximab infusions were generally well tolerated. One patient experienced fever, rigors, and hypotension several hours after a 1-g infusion, requiring intensive care unit admission and transient vasopressor support. No infection was identified, and she has subsequently tolerated four 0.5-g infusions. One patient developed cytomegalovirus colitis and viremia 1 month after rituximab was added to her regimen of cyclophosphamide and prednisone. Her infection cleared with a course of ganciclovir along with weaning of her oral immunosuppression (while rituximab was continued). No other infections requiring hospitalization were identified. Late-onset neutropenia (LON) was identified in two patients, both with absolute neutrophil counts of 0 cells/μL, although one episode occurred beyond the 2-year follow-up period circumscribed by this study. This patient presented with fever and neutropenia 3 months after her most recent dose and 32 months after her first dose of rituximab. She was also receiving mycophenolate mofetil at the time of neutropenia. A second patient presented with fever and neutropenia 4 months after her most recent dose and 18 months after her first dose of rituximab. She was on no other cytotoxic medications at the time of neutropenia. For both patients, neutrophil recovery occurred promptly with recombinant granulocyte colony-stimulating factor. No infection was identified in either patient. Finally, because we did not monitor IgG levels in our study, we are unable to comment on the incidence of hypogammaglobulinemia attributable to repeated rituximab administration.
Discussion
Untreated, AAV is a uniformly fatal disease (23). Fortunately, current therapeutic options achieve high rates of remission and dramatically improve the mortality associated with AAV (24). Thus, to some extent, the practitioner's focus has shifted to the competing interests of longitudinal disease control and the adverse effects of immunosuppression (25). Uncertainty about how to weigh these risks translates into uncertainty regarding how long patients should remain on maintenance therapy and has highlighted the need for safer and more effective therapeutic options (24).
Rituximab, a chimeric monoclonal anti-CD20 antibody, has emerged as a promising option in the management of AAV. Several observational studies demonstrate the efficacy of B cell depletion for refractory AAV (12–18). Efficacy has been demonstrated along several axes, including induction of clinical remission, decreasing ANCA titers, and weaning of oral immunosuppression. Furthermore, experience across various autoimmune diseases suggests an acceptable toxicity profile (26). Two ongoing randomized controlled trials seek to more rigorously define the efficacy of rituximab for the induction of remission, either compared with cyclophosphamide (RAVE) or in conjunction with cyclophosphamide (RITUXVAS). However, as with the published case series, these studies will not directly address the role of continuous rituximab as maintenance treatment.
The largest published series on the use of rituximab for refractory AAV demonstrated complete remission in 49 of 65 patients (75%) (19). However, 28 of 49 patients (57%) who achieved full remission experienced relapse at a median of 11.5 months. Twenty of 28 of these relapsing patients achieved remission again with a second course of rituximab. Interestingly, one of the participating centers in this study implemented a strategy of “preemptive” re-treatment of 1 g every 6 months (i.e., in the absence of symptoms or reappearance of circulating B cells). Fifteen patients at this center received at least one preemptive course of rituximab, and no relapses occurred after a median follow-up of 11 months (range 5 to 23 months). These results suggest continuous therapy with rituximab might be a viable option for maintenance of remission.
In the study presented here, we report the initiation and continuous administration of rituximab in 39 patients with AAV who had already achieved complete or partial remission. Follow-up was available in all patients for up to 1 year and for 20 patients for up to 2 years. Disease activity remained quiescent on rituximab, with only three clinical flares, each occurring at or beyond 20 months of follow-up. Direct comparison with other published series of B cell depletion in AAV is limited because our cohort (by definition) had lower disease activity at study onset. However, we believe the disease control achieved is noteworthy given a total of 708 patient-months observed, and because it was achieved despite the significant decrease of other immunosuppressive medications. Indeed, the potential to withdraw oral immunosuppression was a major rationale for switching to rituximab in many patients. Across the 39 patients included in this study, numerous drug-limiting side effects had developed, including bone marrow suppression, cystitis, weight gain, worsening diabetes, osteoporotic fracture, and avascular necrosis. Although these side effects are not captured by disease activity indices like the BVAS/WG score or the Disease Extent Index (27), they make significant contributions to patient morbidity. At 1 year of follow-up, the percentage of patients receiving cytotoxic therapy had decreased from 87% to 41% (P < 0.001), the percentage of patients on prednisone had decreased from 92% to 59% (P < 0.001), and the percentage of patients able to wean completely off cytotoxic therapy and steroids increased from 3% to 26% (P = 0.011). Furthermore, dose reductions accompanied these decreases in pill burden.
Notably, we found that cessation of prednisone preceded all three clinical flares. In general, we have found that complete glucocorticoid withdrawal can be challenging, even in the context of quiescent disease. Several patients developed vague symptoms such as fatigue, aches, and malaise with steroid cessation, raising a differential diagnosis of mild secondary adrenal insufficiency versus low-grade AAV—in each case, symptoms resolved with reinitiation of low-dose prednisone. To date, insufficient data remain regarding dosing and duration of steroid therapy in AAV (28). None of the clinical flares were preceded by a rising ANCA titer or repopulation of circulating B cells.
Although acute allergic and cytokine-mediated reactions with rituximab infusions are well recognized and readily manageable, concerns remain regarding the scope of delayed adverse effects (29). Perhaps the most feared is progressive multifocal leukoencephalopathy, which has been reported with rituximab in patients with systemic lupus erythematosus and rheumatoid arthritis but not AAV (30). Hepatitis B reactivation is another feared outcome (31) and has recently been reported in a patient with AAV (18). To date, we have not identified either complication in our practice. However, we do report two cases of LON at 18 and 32 months of follow-up, respectively. Both patients required hospitalization for fever and neutropenia, and both responded promptly to recombinant granulocyte colony-stimulating factor. Jones et al. (19) also describe two cases of LON in patients with AAV after B cell depletion. Although the incidence of LON in patients with hematologic malignancies has been estimated to be as high as 35% within 1 year of starting rituximab (32), it is believed to be significantly lower in patients with autoimmune diseases (33). However, one study correlates the number of doses with the development of LON, raising concern that repeated rituximab administration will lead to a higher incidence of this complication despite nononcologic indications (34). In our practice, we measure a complete blood count with differential in all patients receiving rituximab who develop a fever.
In summary, we report the successful use of continuous anti-B cell therapy in patients with AAV in complete or partial remission. Although conclusions about comparative efficacy are restricted by the observational nature of the study, these findings suggest a role for rituximab as maintenance therapy. As with standard maintenance regimens, the optimal duration of this approach remains unclear. Advantages to such an approach include attenuating the accumulated morbidity of disease relapses and medication toxicities. However, more data are required regarding delayed adverse events before a thorough risk-benefit analysis can be performed.
Disclosures
None.
Acknowledgments
We thank Katherine Cosgrove, Eleanor Coughlin, Mary Pat Lowe, Caitlin McManus, and Joanne Wilson for their dedicated patient care in the Vasculitis and Glomerulonephritis Clinic. Part of this work was presented as a poster at the annual meeting of the American Society of Nephrology, San Diego, CA, October 27 through November 1, 2009.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Rituximab Treatment for Vasculitis,” on pages 1359–1362.
Access to UpToDate on-line is available for additional clinical information at http://www.cjasn.org/
References
- 1.Fauci AS, Haynes BF, Katz P, Wolff SM: Wegener's granulomatosis: Prospective clinical and therapeutic experience with 85 patients for 21 years. Ann Intern Med 98: 76–85, 1983 [DOI] [PubMed] [Google Scholar]
- 2.Hoffman GS, Kerr GS, Leavitt RY, Hallahan CW, Lebovics RS, Travis WD, Rottem M, Fauci AS: Wegener granulomatosis: An analysis of 158 patients. Ann Intern Med 116: 488–498, 1992 [DOI] [PubMed] [Google Scholar]
- 3.Jayne D, Rasmussen N, Andrassy K, Bacon P, Tervaert JW, Dadoniene J, Ekstrand A, Gaskin G, Gregorini G, de Groot K, Gross W, Hagen EC, Mirapeix E, Pettersson E, Siegert C, Sinico A, Tesar V, Westman K, Pusey C: A randomized trial of maintenance therapy for vasculitis associated with antineutrophil cytoplasmic autoantibodies. N Engl J Med 349: 36–44, 2003 [DOI] [PubMed] [Google Scholar]
- 4.Metzler C, Miehle N, Manger K, Iking-Konert C, de Groot K, Hellmich B, Gross WL, Reinhold-Keller E: Elevated relapse rate under oral methotrexate versus leflunomide for maintenance of remission in Wegener's granulomatosis. Rheumatology (Oxford) 46: 1087–1091, 2007 [DOI] [PubMed] [Google Scholar]
- 5.Pagnoux C, Mahr A, Hamidou MA, Boffa JJ, Ruivard M, Ducroix JP, Kyndt X, Lifermann F, Papo T, Lambert M, Le Noach J, Khellaf M, Merrien D, Puechal X, Vinzio S, Cohen P, Mouthon L, Cordier JF, Guillevin L: Azathioprine or methotrexate maintenance for ANCA-associated vasculitis. N Engl J Med 359: 2790–2803, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Bosch X, Guilabert A, Font J: Antineutrophil cytoplasmic antibodies. Lancet 368: 404–418, 2006 [DOI] [PubMed] [Google Scholar]
- 7.Golbin JM, Specks U: Targeting B lymphocytes as therapy for ANCA-associated vasculitis. Rheum Dis Clin North Am 33: 741–754, v, 2007 [DOI] [PubMed] [Google Scholar]
- 8.Wong CF: Rituximab in refractory antineutrophil cytoplasmic antibody-associated vasculitis: What is the current evidence? Nephrol Dial Transplant 22: 32–36, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Hinze CH, Colbert RA: B-cell depletion in Wegener's granulomatosis. Clin Rev Allergy Immunol 34: 372–379, 2008 [DOI] [PubMed] [Google Scholar]
- 10.Cheson BD, Leonard JP: Monoclonal antibody therapy for B-cell non-Hodgkin's lymphoma. N Engl J Med 359: 613–626, 2008 [DOI] [PubMed] [Google Scholar]
- 11.Smolen JS, Keystone EC, Emery P, Breedveld FC, Betteridge N, Burmester GR, Dougados M, Ferraccioli G, Jaeger U, Klareskog L, Kvien TK, Martin-Mola E, Pavelka K: Consensus statement on the use of rituximab in patients with rheumatoid arthritis. Ann Rheum Dis 66: 143–150, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brihaye B, Aouba A, Pagnoux C, Cohen P, Lacassin F, Guillevin L: Adjunction of rituximab to steroids and immunosuppressants for refractory/relapsing Wegener's granulomatosis: A study on 8 patients. Clin Exp Rheumatol 25: S23–S27, 2007 [PubMed] [Google Scholar]
- 13.Eriksson P: Nine patients with anti-neutrophil cytoplasmic antibody-positive vasculitis successfully treated with rituximab. J Intern Med 257: 540–548, 2005 [DOI] [PubMed] [Google Scholar]
- 14.Keogh KA, Wylam ME, Stone JH, Specks U: Induction of remission by B lymphocyte depletion in eleven patients with refractory antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 52: 262–268, 2005 [DOI] [PubMed] [Google Scholar]
- 15.Keogh KA, Ytterberg SR, Fervenza FC, Carlson KA, Schroeder DR, Specks U: Rituximab for refractory Wegener's granulomatosis: Report of a prospective, open-label pilot trial. Am J Respir Crit Care Med 173: 180–187, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roccatello D, Baldovino S, Alpa M, Rossi D, Napoli F, Naretto C, Cavallo R, Giachino O: Effects of anti-CD20 monoclonal antibody as a rescue treatment for ANCA-associated idiopathic systemic vasculitis with or without overt renal involvement. Clin Exp Rheumatol 26: S67–S71, 2008 [PubMed] [Google Scholar]
- 17.Stasi R, Stipa E, Del Poeta G, Amadori S, Newland AC, Provan D: Long-term observation of patients with anti-neutrophil cytoplasmic antibody-associated vasculitis treated with rituximab. Rheumatology (Oxford) 45: 1432–1436, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Lovric S, Erdbruegger U, Kumpers P, Woywodt A, Koenecke C, Wedemeyer H, Haller H, Haubitz M: Rituximab as rescue therapy in anti-neutrophil cytoplasmic antibody-associated vasculitis: A single-centre experience with 15 patients. Nephrol Dial Transplant 24: 179–185, 2009 [DOI] [PubMed] [Google Scholar]
- 19.Jones RB, Ferraro AJ, Chaudhry AN, Brogan P, Salama AD, Smith KG, Savage CO, Jayne DR: A multicenter survey of rituximab therapy for refractory antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 60: 2156–2168, 2009 [DOI] [PubMed] [Google Scholar]
- 20.Holle JU, Gross WL: ANCA-associated vasculitides: Pathogenetic aspects and current evidence-based therapy. J Autoimmun 32: 163–171, 2009 [DOI] [PubMed] [Google Scholar]
- 21.Stone JH, Hoffman GS, Merkel PA, Min YI, Uhlfelder ML, Hellmann DB, Specks U, Allen NB, Davis JC, Spiera RF, Calabrese LH, Wigley FM, Maiden N, Valente RM, Niles JL, Fye KH, McCune JW, St Clair EW, Luqmani RA: A disease-specific activity index for Wegener's granulomatosis: Modification of the Birmingham Vasculitis Activity Score. International Network for the Study of the Systemic Vasculitides (INSSYS). Arthritis Rheum 44: 912–920, 2001 [DOI] [PubMed] [Google Scholar]
- 22.Merkel PA, Polisson RP, Chang Y, Skates SJ, Niles JL: Prevalence of antineutrophil cytoplasmic antibodies in a large inception cohort of patients with connective tissue disease. Ann Intern Med 126: 866–873, 1997 [DOI] [PubMed] [Google Scholar]
- 23.Fries JF: Advances in management of rheumatic disease. 1965 to 1985. Arch Intern Med 149: 1002–1011, 1989 [PubMed] [Google Scholar]
- 24.Bosch X, Guilabert A, Espinosa G, Mirapeix E: Treatment of antineutrophil cytoplasmic antibody associated vasculitis: A systematic review. JAMA 298: 655–669, 2007 [DOI] [PubMed] [Google Scholar]
- 25.Turnbull J, Harper L: Adverse effects of therapy for ANCA-associated vasculitis. Best Pract Res Clin Rheumatol 23: 391–401, 2009 [DOI] [PubMed] [Google Scholar]
- 26.Fleischmann RM: Safety of biologic therapy in rheumatoid arthritis and other autoimmune diseases: Focus on rituximab. Semin Arthritis Rheum 38: 265–280, 2009 [DOI] [PubMed] [Google Scholar]
- 27.de Groot K, Gross WL, Herlyn K, Reinhold-Keller E: Development and validation of a disease extent index for Wegener's granulomatosis. Clin Nephrol 55: 31–38, 2001 [PubMed] [Google Scholar]
- 28.Jayne D: Review article: Progress of treatment in ANCA-associated vasculitis. Nephrology (Carlton) 14: 42–48, 2009 [DOI] [PubMed] [Google Scholar]
- 29.Ram R, Ben-Bassat I, Shpilberg O, Polliack A, Raanani P: The late adverse events of rituximab therapy—Rare but there! Leuk Lymphoma 50: 1083–1095, 2009 [DOI] [PubMed] [Google Scholar]
- 30.Carson KR, Evens AM, Richey EA, Habermann TM, Focosi D, Seymour JF, Laubach J, Bawn SD, Gordon LI, Winter JN, Furman RR, Vose JM, Zelenetz AD, Mamtani R, Raisch DW, Dorshimer GW, Rosen ST, Muro K, Gottardi-Littell NR, Talley RL, Sartor O, Green D, Major EO, Bennett CL: Progressive multifocal leukoencephalopathy after rituximab therapy in HIV-negative patients: A report of 57 cases from the Research on Adverse Drug Events and Reports project. Blood 113: 4834–4840, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pei SN, Chen CH, Lee CM, Wang MC, Ma MC, Hu TH, Kuo CY: Reactivation of hepatitis B virus following rituximab-based regimens: A serious complication in both HBsAg-positive and HBsAg-negative patients. Ann Hematol 89: 255–262, 2010 [DOI] [PubMed] [Google Scholar]
- 32.Dunleavy K, Hakim F, Kim HK, Janik JE, Grant N, Nakayama T, White T, Wright G, Kwak L, Gress R, Tosato G, Wilson WH: B-cell recovery following rituximab-based therapy is associated with perturbations in stromal derived factor-1 and granulocyte homeostasis. Blood 106: 795–802, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rios-Fernandez R, Gutierrez-Salmeron MT, Callejas-Rubio JL, Fernandez-Pugnaire M, Ortego-Centeno N: Late-onset neutropenia following rituximab treatment in patients with autoimmune diseases. Br J Dermatol 157: 1271–1273, 2007 [DOI] [PubMed] [Google Scholar]
- 34.Cattaneo C, Spedini P, Casari S, Re A, Tucci A, Borlenghi E, Ungari M, Ruggeri G, Rossi G: Delayed-onset peripheral blood cytopenia after rituximab: Frequency and risk factor assessment in a consecutive series of 77 treatments. Leuk Lymphoma 47: 1013–1017, 2006 [DOI] [PubMed] [Google Scholar]