Abstract
Purpose
The transobturator adjustable tape (TOA) sling operation is a new procedure that allows for the adjustment of tension after surgical intervention, thus permitting correction of postoperative incontinence or obstruction. The aim of this study was to compare the efficacy and safety of TOA with that of the transobturator tape (TOT) procedure.
Materials and Methods
Between 2008 and 2009, women with stress urinary incontinence (SUI) underwent TOT (n=63) or TOA (n=40). The preoperative evaluation included history taking, physical examination, voiding diary, stress and 1-hour pad tests, and a comprehensive urodynamic examination. Postoperative evaluation was performed at the 1-week and 3-month postoperative follow-up visits.
Results
The overall cure rate was 90.0% for the TOA group and 85.7% for the TOT group. The rate of satisfaction was higher in the TOA group than in the TOT group (95.0% vs. 85.6%). Four patients in the TOA group needed reduced tension as the result of urinary obstruction. The tension of the mesh was tightened in 1 patient because of a certain degree of continuing incontinence. The residual urine volume was significantly lower in the TOA group than in the TOT group (7.8 ml vs. 43 ml, p=0.01).
Conclusions
TOA allowed postoperative readjustment for a number of days after surgical intervention, which allowed for good short-term treatment outcomes. These data suggest that better subjective and objective results and residual urine volume can be obtained in the TOA group than those achieved with the traditional non-adjustable mesh and without significant postoperative complications.
Keywords: Stress urinary incontinence, Suburethral slings, Treatment outcome
INTRODUCTION
Stress urinary incontinence (SUI) is defined as the involuntary leakage of urine on effort, exertion, or coughing [1,2]. These symptoms always cause a negative impact on quality of life, such as the physical, psychological, and social well-being of the affected women. Surgery is the most effective treatment for SUI.
In 2001, Delorme described an attempt to reduce the morbidity of retropubic needle passage, an alternative approach with a transobturator tape (TOT) [3]. The TOT procedure has been progressively developing to avoid bladder injury, nerve injury, and operation wound complications [4]. With the TOT procedure, however, it is difficult to apply the correct degree of tension during surgery. Davila et al noted that there was less voiding dysfunction after TOT than after the tension-free vaginal tape (TVT) procedure [5]. But others did not find any significant differences [6,7]. When the tape is too loose, incontinence persists. On the other hand, when the tape is too tight, urinary obstruction occurs. But tension adjustment is difficult with this method. Thus, the adjustable sling operation was developed. Errando et al noted that the REMEEX system (Mechanical External Regulation) allows the readjustment to be performed 24 hours after the operation [8]. In an initial report on 21 cases at 12 months of follow-up, Iglesias et al reported a subjective cure rate of 90% [9]. The procedure was safe and successful, but serious though rare complications have been reported with this technique, including bladder injury and wound infection [9]. Thus, the transobturator adjustable tape (TOA) was developed to reduce these complications. The adjustable transobturator tape has been shown to allow for adjustment of tension for several days after surgical intervention, thus permitting correction of postoperative symptoms. Several different midurethral sling systems are commercially available, but the new adjustable sling operation has not been well studied. In this study, we present a retrospective comparison of the results and complications associated with the TOA and TOT procedures by one urologist after short-term follow-up.
MATERIALS AND METHODS
We reviewed the files of 103 women referred to our hospital for suburethral tape between June 2008 and June 2009. Each patient underwent one of two techniques (TOA: A.M.I TOA Sling®, Agency for Medical Innovations GmbH, Austria; TOT: Tension Free Obturator Tape®, Dowmedics, Korea) in accordance with the scheduling order. All patients were given a routine workup for incontinence, including history, physical examination, stress cough test, standard 1-hour pad test, uroflowmetry, post-void residual (PVR) urine measurement, and the complete multi-channel urodynamic study. All medical charts were retrospectively reviewed for certain data, including age, body weight, height, urodynamic study, and type of suburethral tape. We reviewed complications, postoperative urinary symptoms, and outcomes. Our study excluded the presence of any urinary tract infection, urgency incontinence, detrusor overactivity, intrinsic sphincteric deficiency (ISD), impaired detrusor contraction, previous anti-incontinence, and pelvic support surgery. We excluded patients who had pelvic prolapse greater than stage I on the International Continence Society (ICS) grading system.
During the pelvic examination, the severity of the vaginal wall defect was determined by using the pelvic organ prolapse quantification (POP-Q) system [10]. The stress cough test was performed with the patient in the standing position with 300 ml bladder filling. Urodynamic study was performed with the patient in a birthing chair at a 45-degree angle. After catheterization, cystometry was performed by using a Laborie 8 Fr double-lumen urodynamic catheter at a fill rate of 50 ml per minute. First desire, strong desire, and maximal cystometric capacity were recorded. The Valsalva leak point pressure (VLPP), a measurement of the lowest abdominal pressure required to produce urine leakage, was also recorded. The VLPP was obtained with the subject seated when the total infused volume of sterile water reached 300 ml. A VLPP value of less than 60 cmH2O was used as the urodynamic criterion for the diagnosis of ISD.
Routine postoperative follow-up for all patients included office visits at postoperative 7 days and at 3 months. At postoperative 7 days, patients underwent a stress cough test and uroflowmetry and residual urine volume measurement. At the 3-month follow-up, a 1-hour pad test was added to the previous tests. Objective outcomes were assessed with the cough stress test and 1-hour pad test. SUI cure was defined as no leakage of urine during cough stress testing and a pad weight gain of less than 2 g on a 1-hour pad test during the follow-up visit. Improvement was defined as a more than 50% reduction of urine weight on a 1-hour pad test and a positive result on the stress cough test. Failure was defined as less than a 50% reduction on a 1-hour pad test and a positive result on the cough stress test. Subjective outcomes were classified as very satisfied, satisfied, fair, or dissatisfied. Patients who checked 'very satisfied' or 'satisfied' were placed in the satisfaction group. Groin and thigh pain was another potential problem after transobturator sling operations. Severe pain was defined as the presence of pain still requiring analgesic therapy 1 week after surgery.
TOA is a macroporous, polypropylene, monofilament non-elastic type tape. The TOA method is similar to the TOT procedure. The TOA tape is situated below the mid-urethra via a small incision in the anterior vaginal wall. Two strings on either side are situated 1.5 cm from the midline of the tape, which is externalized via the anterior vaginal wall. When it is pulled down to reduce tension, the TOA group is formed of three strings in each branch of the tape situated at the same distance from both thighs. These are externalized via the same orifice through which the mesh is, when pulled up, to increase the tension. The tension is adjusted with minimal tension by placing the scissors between the tape and the urethra. The plastic envelope is removed, and the redundant portion of the mesh is cut. Depending on the distance from the urethra to the skin, one or two of the lateral superior strings are also cut. Cystoscopy was performed during the procedure. The Foley catheter was removed the next day, and the patients underwent studies that included measurements of flow rate and PVR before being discharged home.
SPSS version 12.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for statistical analyses. Comparison of baseline patient characteristics as well as baseline uroflowmetric parameters was performed by using the independent t-test and chi-square test. The repeated-measures ANOVA test was used to compare changes in clinical outcomes between the two groups. Statistical significance was set at p<0.05.
RESULTS
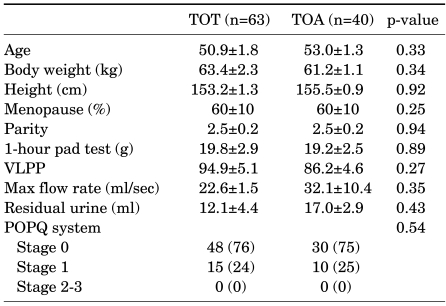
A total of 103 participants underwent the TOA procedure (n=40) or the TOT procedure (n=63). There were no significant differences in preoperative characteristics between patients in the TOA and TOT groups (Table 1). The Mean±SD operating time was 20.4±2.5 minutes in the TOT group and 22.5±2.7 minutes in the TOA group. The mean hospitalization duration was. 3.0 days in the TOT group and 3.2 days in the TOA group. There was no significant difference.
TABLE 1.
Patient characteristics of the TOT and TOA groups
TOT: transobturator tape, TOA: transobturator adjustable tape VLPP: Valsalva leakage pressure point, POPQ: Pelvic Organ Prolapse Quantification system. Data are presented as Mean±SEM. Numbers in parentheses are percentages.
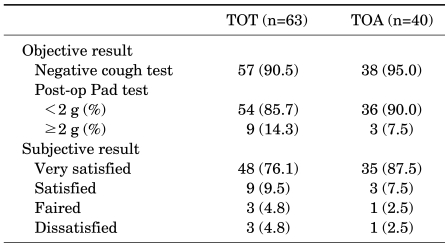
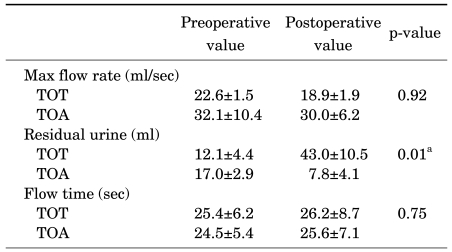
Table 2 shows the objective and subjective outcomes of both groups 3 months after surgery. Notably, no statistically significant differences were found between the two types. The overall cure rate was 90% at 3 months in the TOA group vs. 85.7% in the TOT group. The satisfaction rate was higher in the TOA group than in the TOT group (95.0% vs. 85.6%). Lee et al noted that the cure rate of the TOT procedure was 92% and the satisfaction rate was 98% [11]. Four patients in the TOA group (10%) needed loosening of the mesh because of urinary obstruction (flow <10 ml/s and/or residual urine>50 ml) after postoperative day 1. In 2 patients (5.0%) in the TOA group, the tension of the mesh was tightened because of a certain degree of continuing incontinence after postoperative day 1. Uroflowmetry tests performed before and after surgery showed that flow in the TOT group ranged from 22.6±1.5 ml/s to 18.9±1.9 ml/s, whereas that in the TOA group ranged from 32.1±10.4 ml/s to 30.0±6.2 ml/s (Table 3). Maximal urine flow decreased to an insignificant degree. The change in residual urine volume was significantly lower in the TOA group than in the TOT group (7.8 ml vs. 43 ml, p=0.01, repeated-measures ANOVA test). There was no definite difference in voiding volume or maximal urine flow between the two groups.
TABLE 2.
Objective and subjective success rates of the TOT and TOA groups at postoperative 3 months
TOT: transobturator tape, TOA: transobturator adjustable tape. Data are presented as frequencies (percentages).
TABLE 3.
Changes in uroflowmetric parameters at postoperative 3 months
TOT: transobturator tape, TOA: transobturator adjustable tape, Data are presented as Mean±SEM. a: significant (<0.05), repeated-measures ANOVA test
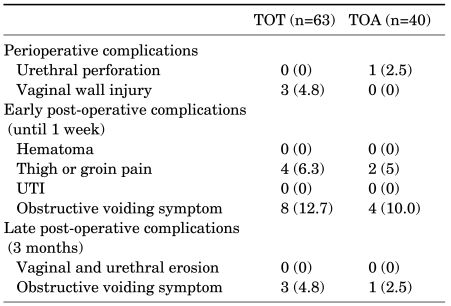
Postoperative complications are shown in Table 4. Vaginal wall injury occurred in 3 patients (4.8%) in the TOT group and urethral perforation occurred in 1 patient (2.5%) in the TOA group. We promptly repaired the vaginal wall injury, and the patient with urethral perforation was catheterized for 3 days. There were no cases of wound infection, tape erosion, or urinary tract infection (WBC>5 in urine analysis) in either group. Five patients (12.5%) in the TOA group tended to still have continuing groin pain 3 days after surgery. The incidence of such pain was 6.3% of the TOT group compared with 5% of the TOA group 7 days after surgery. The cause of these results may have been that with the TOA procedure the strings remained until the end of the adjustment period. The patients received analgesic agents for 7 days. Three patients in the TOA group had improved pain 1 week after surgery, but two patients (5%) had persistent groin pain until 1 week after surgery. Four patients (6.4%) in the TOT group had thigh pain, and we continued to order analgesic agents 1 week after surgery. The pain was improved at 2 weeks after surgery in all patients. Postoperative urinary obstruction was seen in 8 patients (12.8%) in the TOT group. Three patients (4.8%) in the TOT group had persistent obstructive voiding symptoms (flow rate<10 ml/s and/or residual urine>50 ml) at the 3-month follow-up visit. These patients still showed no improvement, so we performed urethrolysis at 3-5 months after surgery. One patient (2.5%) in the TOA group had a complication of urethral obstruction at 3 months after surgery; this case required urethrolysis at 5 months after surgery.
TABLE 4.
Comparison of operation-related complications between the TOT and TOA groups
TOT: transobturator tape, TOA: transobturator adjustable tape, UTI: urinary tract infection. Data are presented as frequencies (percentages).
DISCUSSION
We retrospectively reviewed the data for 103 women referred to our hospital for suburethral tape operation only. The mean age, parity, height, body weight, preoperative clinical parameters, and preoperative urodynamic parameters were similar in both groups. The patients did not have pelvic organ prolapse (POP: stage≥2), ISD, bladder outlet obstruction, or impaired detrusor muscle contraction. The cure rate of the TOT procedure varies from 51% to 97%, depending on the definition used for success, the outcome instruments, and discrepancies in the studied populations [5,12-15]. Maroto et al noted in their results of the TOA procedure that 90% of the patients were objectively stress continent [12], 6.5% of the patients had considerable improvement, and 3.5% of the patients experienced failure during the mean follow-up period of 24.7 months. In the present study, the cure rate associated with the TOA procedure was 90% and was comparable to the 85.7% cure rate associated with the TOT procedure. The high cure rate of the TOA procedure resulted from the adjustable system after the immediate postoperative period. We noted a higher satisfaction rate for the TOA group (TOT: 85.6%; TOA: 95%).
The two most frequent problems after stress incontinence surgery are persistence of incontinence and voiding dysfunction, both of which are related to how loose or how tight the tape is implanted [16]. Despite all the improvements achieved with synthetic slings, Stanton et al said as follows: "Thus the ideal sling should be of consistent strength, readily available, adjustable and removable [17]." Readjustment was easily performed under local anesthesia. For the TOA sling operation, loosening of the mesh resulted in a significant increase in flow and elimination of residual urine. Tightening of the mesh resulted in continence. Although most urinary retention resolves with conservative treatment including medication, urethral dilation, or intermittent catheterization, refractory urethral obstruction ultimately requires midline or lateral excision of the tape [18]. Davila et al found de novo voiding symptoms after the TOT procedure in 6.7% of their operation cases, and in 7%, the preoperative voiding symptoms worsened [5]. Tape cutting or tape adjustment were necessary in up to 5% after the TOT procedure [13]. In the present study, eight patients (12.7%) in the TOT group had undergone urethral pull-down after postoperative 1 day. In urethral pull-down, a Hegar dilator is inserted in the urethra and pulled down with the aim of moving downward and loosening the tape in the TOT group. If the maximum flow rate is less than 10 ml/s or there is more than 50 ml of residual urine after the TOA procedure, tension is released from the mesh by pulling down on one side only of the vaginal strings, approximately 1 cm [14]. We performed the same method after postoperative 1 day (Fig. 1). The patients were checked again by uroflowmetry and residual urine volume after 3 hours. If the patients showed SUI in the cough stress test, then we immediately pulled up the strings on each side, approximately 0.5 cm (Fig. 1). Continence was tested, and the procedure was repeated until the patient was continent with a maximum flow rate equal to or greater than 10 ml/s and when there was less than 50 ml of residual urine. The strings were cut and extracted, and the patient was discharged. We rechecked the results of the cough test and uroflowmetry and residual urine at postoperative 1 week and 3 months. In another study, the tension was adjusted in 44% of patients: in 34%, the tension was increased, and in 10%, the tension was decreased [14]. In the present study, 10% of the patients in the TOA group needed a decrease in the tension and 5% of the patients needed an increase in the tension due to a certain degree of continuing incontinence. After tightening or loosening of the mesh, the patients had higher satisfaction and continence and a higher flow rate.
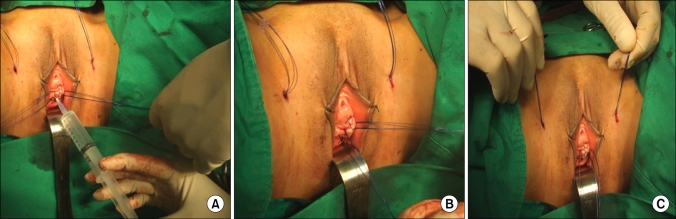
FIG. 1.
(A) Lidocaine injection on Rt. vaginal wall before loosening of the mesh. (B) Rt. vaginal string was pulled down 1 cm for loosening of the mesh due to obstruction. (C) Both superior strings were pulled up 0.5 cm for tightening of the mesh due to stress urinary incontinence (SUI).
A randomized study from Finland revealed that 16% of the TOT patients had groin pain compared with 1.5% of the TVT patients, which led to an increased need for analgesia in the transobturator group [19].
Three cases of vaginal wall injury in the TOT group were encountered, indicating that the needle passed through the dissection space between the vagina and the urethra. We performed surgical implantation of the tape with a view of avoiding urethral injury, so the needle passed close to the vaginal surface. Urethral injuries are believed to occur because of poor surgical technique, which damages the integrity of the urethral tissue or its blood supply; because of excessive tension placed on the tape; or as the result of local infection [20]. The transobturator sling procedure has been shown to have a lower incidence of bladder injury (0.5%), urethral injury (0.5%), and lower urinary tract injuries (1%) than does the TVT procedure [20]. We think the recommendation for cystoscopy after passage of the trocars cannot be overemphasized, even if the rate of urethral injury was very low, because these complications can be treated promptly in the operation field.
We conclude that TOA is an effective and simple procedure because the procedure had minimal complications and a high success rate. Our results show that the persistence of stress incontinence and the development of obstruction after surgery depend largely on the tension applied to the mesh, looser or tighter, during the procedure. TOA allows for postoperative adjustment of tension, thus permitting correction of postoperative incontinence or obstruction. The present study was limited in that the results were recorded until only 3 months after surgery. Hence, the study may not properly indicate long-term prospective outcomes. Clearly, further follow-up is required, and more comparative studies are warranted to evaluate the outcome and safety of these novel procedures for the treatment of SUI.
CONCLUSIONS
The TOA procedure allowed postoperative readjustment of the suburethral sling pressure for a number of days after surgical intervention, which resulted in good short-term results. These data suggest that better objective and subjective results and residual urine volume can be obtained with the TOA procedure than are achieved with the traditional non-adjustable mesh and without significant postoperative complications. However, these data had a short postoperative follow-up period and excluded women with SUI with co-morbid status. Long-term follow-up will be required to fully evaluate the results and safety associated with these procedures.
Footnotes
The authors have nothing to disclose.
References
- 1.Hannestad YS, Rortveit G, Sandvik H, Hunskaar S Epidemiology of Incontinence in the County of Nord-Trøndelag. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. J Clin Epidemiol. 2000;53:1150–1157. doi: 10.1016/s0895-4356(00)00232-8. [DOI] [PubMed] [Google Scholar]
- 2.Minassian VA, Drutz HP, Al-Badr A. Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet. 2003;82:327–338. doi: 10.1016/s0020-7292(03)00220-0. [DOI] [PubMed] [Google Scholar]
- 3.Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol. 2001;11:1306–1313. [PubMed] [Google Scholar]
- 4.Delorme E, Droupy S, de Tayrac R, Delmas V. Transobturator tape (Uratape): a new minimally-invasive procedure to treat female urinary incontinence. Eur Urol. 2004;45:203–207. doi: 10.1016/j.eururo.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Davila GW, Johnson JD, Serels S. Multicenter experience with the Monarc transobturator sling system to treat stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:460–465. doi: 10.1007/s00192-005-0039-9. [DOI] [PubMed] [Google Scholar]
- 6.Porena M, Costantini E, Frea B, Giannantoni A, Ranzoni S, Mearini L, et al. Tension-free vaginal tape versus transobturator tape as surgery for stress urinary incontinence: results of a multicentre randomised trial. Eur Urol. 2007;52:1481–1490. doi: 10.1016/j.eururo.2007.04.059. [DOI] [PubMed] [Google Scholar]
- 7.Zullo MA, Plotti F, Calcagno M, Marullo E, Palaia I, Bellati F, et al. One-year follow-up of tension-free vaginal tape (TVT) and trans-obturator suburethral tape from inside to outside (TVT-O) for surgical treatment of female stress urinary incontinence: a prospective randomised trial. Eur Urol. 2007;51:1376–1382. doi: 10.1016/j.eururo.2006.10.066. [DOI] [PubMed] [Google Scholar]
- 8.Errando C, Rodriguez-Escovar F, Gutierrez C, Baez C, Araño P, Villavicencio H. A re-adjustable sling for female recurrent stress incontinence and sphincteric deficiency: outcomes and complications in 125 patients using the Remeex sling system. Neurourol Urodyn. 2010 doi: 10.1002/nau.20879. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Iglesias X, Espuña M. Surgical treatment of urinary stress incontinence using a method for postoperative adjustment of sling tension (Remeex System) Int Urogynecol J Pelvic Floor Dysfunct. 2003;145:326–330. doi: 10.1007/s00192-003-1072-1. [DOI] [PubMed] [Google Scholar]
- 10.Auwad W, Freeman RM, Swift S. Is the pelvic organ prolapse quantification system (POPQ) being used? A survey of members of the International Continence Society (ICS) and the American Urogynecologic Society (AUGS) Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:324–327. doi: 10.1007/s00192-004-1175-3. [DOI] [PubMed] [Google Scholar]
- 11.Lee YS, Lee HN, Lee KS. The evolution of surgical treatment for female stress urinary incontinence: era of mid-urethral slings. Korean J Urol. 2010;51:223–232. doi: 10.4111/kju.2010.51.4.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maroto JR, Gorraiz MO, Bueno JJ, Perez LG, Bru JJ, Chaparro LP. Transobturator adjustable tape (TOA) permits to correct postoperatively the tension applied in stress incontinence surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:797–805. doi: 10.1007/s00192-009-0872-3. [DOI] [PubMed] [Google Scholar]
- 13.Juang CM, Yu KJ, Chou P, Yen MS, Twu NF, Horng HC, et al. Efficacy analysis of trans-obturator tension-free vaginal tape (TVT-O) plus modified Ingelman-Sundberg procedure versus TVT-O alone in the treatment of mixed urinary incontinence: a randomized study. Eur Urol. 2007;51:1671–1678. doi: 10.1016/j.eururo.2007.01.035. [DOI] [PubMed] [Google Scholar]
- 14.Costa P, Grise P, Droupy S, Monneins F, Assenmacher C, Ballanger P, et al. Surgical treatment of female stress urinary incontinence with a trans-obturator-tape (T.O.T.) Uratape: short term results of a prospective multicentric study. Eur Urol. 2004;46:102–106. doi: 10.1016/j.eururo.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 15.de Tayrac R, Deffieux X, Droupy S, Chauveaud-Lambling A, Calvanese-Benamour L, Ferandez H. A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol. 2004;190:602–608. doi: 10.1016/j.ajog.2003.09.070. [DOI] [PubMed] [Google Scholar]
- 16.Nitti VW, Carlson KV, Blaivas JG, Dmochowski RR. Early results of pubovaginal sling lysis by midline sling incision. Urology. 2002;59:47–51. doi: 10.1016/s0090-4295(01)01559-x. [DOI] [PubMed] [Google Scholar]
- 17.Stanton SL, Brindley GS, Holmes DM. Silastic sling for urethral sphincter incompetence in women. Br J Obstet Gynaecol. 1985;92:747–750. doi: 10.1111/j.1471-0528.1985.tb01459.x. [DOI] [PubMed] [Google Scholar]
- 18.Wheeler TL, 2nd, Richter HE, Greer WJ, Bowling CB, Redden DT, Varner RE. Predictors of success with postoperative voiding trials after a mid urethral sling procedure. J Urol. 2008;179:600–604. doi: 10.1016/j.juro.2007.09.080. [DOI] [PubMed] [Google Scholar]
- 19.Laurikainen E, Valpas A, Kivelä A, Kalliola T, Rinne K, Takala T, et al. Retropubic compared with transobturator tape placement in treatment of urinary incontinence: a randomized controlled trial. Obstet Gynecol. 2007;109:4–11. doi: 10.1097/01.AOG.0000249607.82768.a1. [DOI] [PubMed] [Google Scholar]
- 20.Daneshgari F, Kong W, Swartz M. Complications of mid urethral slings: important outcomes for future clinical trials. J Urol. 2008;180:1890–1897. doi: 10.1016/j.juro.2008.07.029. [DOI] [PubMed] [Google Scholar]