Abstract
Dendritic cells (DCs) are the most effective antigen-presenting cells (APCs) and are used in a variety of immunotherapeutic approaches. Adoptive cellular immunotherapy (ACI) of cancer using DCs has attracted much interest due to their capacity to promote immunity in prophylactic and therapeutic protocols. As one approach, DCs are injected into patients or tumor-bearing animals, to trigger specific antitumor immunity. In that framework, several approaches to DC delivery have been reported, including direct intratumoral injection; this has yielded positive but variable results. The underlying reasons for this have not been fully determined, but major hypotheses include technical difficulties in delivering cells into tumors and tumor-mediated immunosuppression. Image-guided ACI offers the potential to establish that DCs are efficiently delivered to the tumor site, which might eliminate some of the variability. Therefore, we developed highly sensitive methods for monitoring the injection or trafficking of DCs into tumors using a clinically approved formulation of a gadolinium-based magnetic resonance imaging (MRI) contrast agent, Gd(III)-HP-DO3A (ProHance™). We determined the labeling efficiency of DCs with this formulation; that labeling DCs with this agent did not inhibit expression of surface markers important for antigen presentation and activation of naive T cells; that their capacity to interact with natural killer (NK) cells was not reduced; and that their migration was not diminished. Further, we determined that ProHance™-labeled DCs can be effectively imaged in vivo in established central nervous system tumors.
Keywords: dendritic cells, magnetic resonance imaging, immunotherapy, glioma, central nervous system, cell trafficking
Many clinical trials have made use of adoptive cellular immunotherapy (ACI) to treat cancer in both prophylactic and therapeutic settings (1–6). A variety of approaches to cell delivery have been investigated; in the instance of the use of autologous dendritic cells (DCs), they have been injected into patients or animals, intravenously (7), intradermally (8,9), intralymphatically (10), or intratumorally (11–15), particularly in the case of treatment of gliomas (16–22). There are distinct advantages to the use of adoptively transferred cells for therapy per se, or as vehicles for delivery of therapeutic agents. For instance, cells mediate many complex biologic functions, and can both respond to, and influence, the surrounding tissue in an organ or tumor. DCs are the most effective antigen presenting cells (APCs) and are used to promote antitumor immunity in both prophylactic and therapeutic applications (23–26). While there have been some successes in experimental models and clinical trials, there is not a clear understanding of the reasons for success vs. failure of this approach. The variability in effects could be due to a variety of reasons, including failure to deliver sufficient number of cells to the tumor site, or complex biological interactions resulting in DC death or deregulation. As for the simpler aspects of these questions, an efficient means for monitoring direct injection or trafficking of DCs into tumors has not been fully developed. Lack of accumulation of DCs in the tumor, from missing the tumor bed, negligible cell trafficking, or poor dose/timing would result in treatment failure in some individuals, and might explain the variability in results with this approach. There are many works addressing the use of adoptively transferred cells for cancer therapy (1–6) and the ability to establish, noninvasively, that adoptively transferred DCs actually are in the tumor and/or when the next injection should be made has the potential to significantly affect or alter treatment. In the case of direct, intratumoral injection of DCs, some investigators used ultrasound as a means of image-guided delivery of DCs (12,27). However, this approach was limited in utility as the sensitivity and resolution of ultrasound was viewed as insufficient for highly effective monitoring of cell delivery into tumors (28).
There is limited information on the improvement in efficacy of therapy with DCs using image-guided delivery of DCs. It is easily envisioned that effectively delivering DCs to their intended target could have a substantial effect on the outcome of this therapy. Magnetic resonance imaging (MRI) is an excellent modality for monitoring biological cancer therapy. Many new MRI-based methods are available for monitoring the injection or trafficking of adoptively transferred cells. They all involve visualizing adoptively transferred cells in vivo following their in vitro labeling with nanoparticle-based contrast agents (CAs) (29–33). Tracking the movement of DCs in vivo has been predominately accomplished by labeling these cells with iron oxide particles (34) or perfluorocarbon nanoparticulate emulsions (7). Iron oxide CAs are extremely sensitive, but their use is limited based upon their susceptibility effect in T2-weighted images, resulting in a dark area, i.e., a signal void.
The use of iron oxide–labeled DCs in the clinic has also illustrated a clear need for image-guided ACI; a recent publication documented that 50% of the attempts at delivering DCs, guided by ultrasound, were unsuccessful in delivering the DCs directly into lymph nodes (28). These data suggest that results in preclinical and clinical trials, to date, have not yielded uniformly interpretable data regarding the efficacy of DCs for treatment of cancer.
Gadolinium-based CAs have several inherent advantages over nanoparticles. They are considered positive CAs in T1-weighted images because they brighten the tissues upon their accumulation by increasing the water signal intensity of the tissue. They do not have the signal void problems associated with nanoparticles but are much less sensitive, as they work by shortening the T1 of the water protons in the tissue in which they accumulate. In spite of the lower sensitivity, Gd(III)-chelate complexes have been used to load and monitor cells in animals. Himmelreich et al. (35) used a particulate that is rendered soluble following uptake, Crich et al. (36) used the gadolinium chelate HP-DO3A in endothelial stem cells and pancreatic islets (36,37), and Louie et al. (38) used the activatable galactopyranose-protected gadolinium-tetraazacyclododecane tetraacetic acid (Gd-DOTA) complex (known as EgadMe) to label Xenopus embryos and monitor beta-galactosidase activity.
We present our recent efforts on the development of a method for monitoring intratumoral injection, cell tracking, and biological therapy. Our focus is on techniques with the potential for rapid translation into clinical trials of adoptive immunotherapy using DCs that are currently being conducted. We have therefore modified the method of Crich et al. (36) by substituting the clinical formulation of Gd(III)-HP-DO3A for the pure chelate complex. We established methods for labeling DCs with a gadolinium-based CA commercially known as ProHance™ (Gd-CA, a clinically approved formulation of Gd(III)-HP-DO3A), which allows monitoring of intratumoral injection and potentially the tracking of these cells in vivo using MRI. We demonstrate the use of Gd-CA for monitoring intratumoral injection of DCs.
MATERIALS AND METHODS
Culture of DCs
Immature DCs (iDCs) were cultured from rat (male Fisher 344; weight ~135 g) bone marrow (BM) as previously described (39). BM was suspended in Roswell Park Memorial Institute (RPMI) medium 1640 containing 10% fetal bovine serum (FBS), penicillin/streptomycin (100 U/ml), 2 mM L-glutamine, 1 mM sodium pyruvate, 0.1 mM nonessential amino acids, 1000 µM [4-(2-hydroxyethyl)-1-piperazine ethanesulfonic acid] (HEPES) buffer, 5 × 10−5 M 2-mercaptoethanol (2-ME), and 0.5 mM NG mono-methyl-L-arginine (L-NMMA) (a nitric oxide synthase inhibitor). Cells were cultured in six-well, flat-bottomed plates at 2 million cells/ml using 3 to 4 ml of complete media per well. The medium was further supplemented with 500 U/ml recombinant granulocyte-macrophage colony-simulating factor (rGM-CSF), 500 U/ml recombinant interleukin-4 (rIL-4), and 25 ng/µl Flt3-L. The cultures were supplied with 50% fresh medium and cytokines every 48 h for a total of 7 d in culture. At this time point, DCs were confirmed to have an iDC phenotype by flow cytometry.
Labeling of DCs with Gd-CA
After 6 d of culture, cells were incubated in known concentrations (6.25, 25, or 50 mM) of Gd-CA for 24 h at 37°C. Suspensions of treated cells were centrifuged and the supernatants discarded. The cell pellets were washed three times with fresh media (20 ml each time) to remove any excess of extracellular Gd-CA. The cell pellets were resuspended in phosphate-buffered saline (PBS) and the cell counts adjusted to 200 × 106 per ml.
Determination of Gd-CA Uptake
Approximately 2 × 106 DCs (pelleted at 400g for 5 min) were incubated in 250 µl of 10% HNO3 at 25°C for 48 h. Cell lysates were centrifuged (400g for 5 min), the T1 of the supernatant measured, and the relaxivity of water protons determined at 22°C and 20 MHz (Bruker Minispec20 Relaxometer). The Gd-CA uptake was determined from a standard curve obtained using known concentrations of Gd-CA in 10% HNO3 at 22°C. The Gd uptake was further validated by inductively-coupled plasma (ICP) mass spectral analyses.
Analyses of the Effects of Gd-CA Labeling on DC Phenotype
Flow cytometric analyses of labeled DCs were carried out to monitor expression of major histocompatibility complex (MHC) class I (OX18), MHC class II (OX6), costimulatory markers CD80, and CD86, and DC cell-surface markers CD161, OX62, and OX42, as previously described (39).
Determination of the Effects of Gd-CA on DC Interactions with Natural Killer Cells
Day 6 DCs were labeled with Gd-CA as described above, and then cultured for 24 h with freshly isolated populations of nonadherent splenic mononuclear cells enriched for natural killer (NK) cells (10–15%) at various NK:DC ratios (1.25:1, 2.5:1, 5:1, and 10:1). Cocultured NK cells were assayed for lytic activity against YAC-1 target cells in 4 h, 51Cr-release assays at 100:1 and 50:1 effector:target (E:T) ratios. YAC-1 target cells were labeled with 50 to 100 µCi of ** for 1 h, washed 2× and resuspended in culture media at 2 × 104 cells/ml. Radiolabeled target cells (2 × 103) were seeded in triplicate into wells of a 96-well microtiter plate in 100 µl. Effector cells in triplicate, at the indicated effector:target cell ratios, were added to wells in 100 µl. Plates were then gently centrifuged at 100g for 5 min, and incubated for 4 h in an humidified incubator at 37°C with 5% CO2 tension. Then, 50 µl of supernatant from wells was harvested and counted in a microplate scintillation counter, and the percentage of specific cytotoxicity was calculated using the formula:
| [1] |
Brain Tumor Implantation
Brain tumors were seeded by stereotactically injecting 9L gliosarcoma cell suspensions into the right frontal lobe of 12 male Fisher 344 rats (11,40). The rats were anesthetized with a mixture of ketamine (87 mg/kg) and xylazine (13 mg/kg). The cells were injected using a Kopf® stereotaxic frame and a Hamilton® syringe. A 10-µl volume of PBS containing 5 × 104 tumor cells was injected 2 mm anterior and 2 mm lateral of the bregma at a depth of 4 mm over a period of 5 min. A 1-min waiting period was observed before slowly withdrawing the needle. The holes in the skull were sealed with bone wax and the skin closed with stitches. After the procedure, buprenorphine (0.5 mg/kg) was injected intramuscularly two times a day for 4 d. The tumor was allowed to grow for 2 weeks before DCs (~2 × 106 in 10 µl PBS, untreated or treated with Gd-CA) were injected using the same protocol. The 12 tumor-bearing animals were split into two groups: five animals were injected with untreated or control DCs and seven animals were injected with DCs loaded with Gd-CA.
MRI
A 7T Bruker AVANCE DBX MRI System equipped with a 12-cm actively shielded gradient set (400 mT/m at 200A, 100 µs rise-time) and a Bruker 7.2-cm birdcage coil was used in this study.
In Vitro Imaging
DCs, 3.8 × 106 (untreated and treated with Gd-CA) were suspended in 300 µl of 5% gelatin in PBS at 37°C (prepared by dissolving 2.5 g of gelatin bloom 175 [Sigma], in 50 ml of PBS [Sigma]). A plug of suspended DCs was sandwiched between two layers of 5% gelatin in NMR tubes (5-mm diameter, cell plug length ~2.5 mm) and imaged using a T1-weighted spin-echo protocol (typical parameters: slice thickness [ST] = 2 mm, field of view [FOV] = 3 cm × 3 cm, matrix size = 128 × 128, number of excitations [NEX] = 2). To get the best contrast and T1 relaxation parameters, repetition time (TR = 50 ms to 7 s) and echo time (TE = 6–15 ms) were varied.
In Vivo Imaging
Imaging of rat brains bearing 9L gliosarcoma cells were carried out under anesthesia following intramuscular administration of a mixture of ketamine (68 mg/kg), xylazine (14 mg/kg), and acepromazine (2.3 mg/kg). Body temperature of the animals was maintained using an automated, forced warm air circulator. Rat brains were initially imaged to locate tumor using a spin-echo protocol (TR/TE = 500 ms/10 ms, ST = 1 mm, FOV = 3.5 cm × 3.5 cm, matrix size = 256 × 128 for T1-weighted images; and TR/TE = 3,500 ms/40 ms for T2-weighted images). At day 14 postimplantation, tumor localization was determined by MRI following intravenous injection of Gd-CA (0.3 mmol/kg of animal weight) via the tail vein.
Following tumor localization (24 h), iDCs were injected directly into the tumor bed. Control or Gd-CA–labeled DCs (2 × 106) were suspended in 10 µl of PBS and stored over ice for no more than 30 min. The head skin was opened to locate the needle hole created originally for injection of tumor cells and was used for the injection of the 10-µl DC suspension directly into the tumor. Injections of DCs were performed stereotactically at a depth of 4 to 5 mm under the skull. Cells were delivered at a flow rate of 10 µl/5 min to avoid backflow and/or cell damage due to shear forces generated by flow out of the syringe. Following DC delivery (within 30 min post–DC injection), animals were anesthetized, placed inside the magnet bore, maintained at 37°C using a computer-controlled warm air circulator, and imaged using the parameters described above. After imaging tumors with DCs a bolus of Gd-CA (0.3 mmol/kg) was injected intravenously via the tail vein, followed by using a T1-weighted imaging protocol (described above) to define the tumor location and size.
The percent contrast enhancement (%CE) due to injected DCs, before the intravenous (i.v.) injection of ProHance™ via the tail vein, is defined as:
| [2] |
where S = signal intensity, region of interest (ROI) 1 = region of interest in the right hemisphere of brain where DCs (labeled or control) were present, and ROI 2 = region of interest in the left hemisphere or contralateral side of the brain where no DCs were injected. ROI1 in the DC injections were selected using the area near the injection site. ROI2 were selected in the contralateral side by using the same area units (signal intensity/pixel) as covered by ROI1.
RESULTS
Labeling of DCs With Gd-CA and In Vitro Imaging
Our initial experiments sought to determine whether we could efficiently label DCs with a Gd-based MR CA, and to determine whether we could image DCs by MRI using CA levels that would not affect their phenotype and function. To label DCs, we used a modification of a method developed by Crich et al. (36). This modification made use of a clinically approved formulation of Gd(III)-HP-DO3A (Gd-CA), commercially known as ProHance™. As illustrated in Fig. 1, we determined that there was a dose-dependent relationship between extracellular concentration of Gd(III)-HP-DO3A and the average number of Gd ions that DCs accumulate following labeling with a variety of concentrations of Gd-CA. Using 6.25 mM Gd(III)-HP-DO3A, we determined that there was an uptake measured at 0.0058 µmol/106 cells. Extracellular concentrations of Gd-CA at 25 mM and 50 mM resulted in an uptake of 0.0142 and 0.0248 µmol/106 cells, respectively (an analysis of variance between groups gave P = 0.000349). This results in an intracellular concentration of Gd(III) of approximately 5.9 to 3.9, 14 to 9.5, and 25 to 16.5 mM for cells incubated with extracellular Gd-CA concentrations of 6.25, 25, and 50 mM, respectively (Fig. 1). This was based upon the calculation of the amount of Gd on a per cell basis using a DC volume of ~1 to 1.5µl/106 cells (41,42).
FIG. 1.
Efficacy of uptake of Gd-CA by dendritic cells. Immature, bone marrow–derived dendritic cells (DCs; day 6) were cultured with varying concentrations of Gd-CA (0–50 mM) for 24 h. An analysis of variance (ANOVA) between groups resulted in P: P = 0.000349.
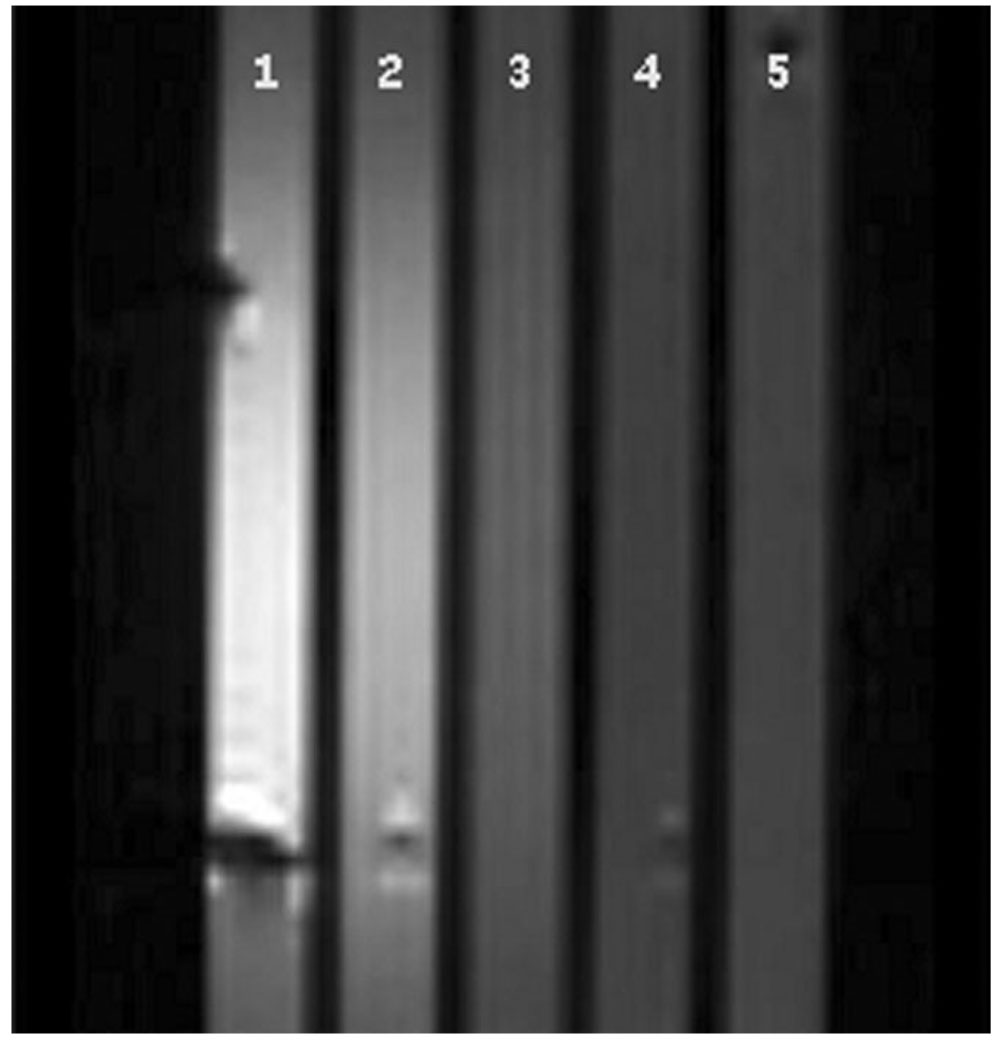
As a prelude to in vivo imaging of DCs, we evaluated the efficacy of in vitro MRI of DCs (3.8 × 106) suspended in 300 µl of 5% gelatin in PBS at room temperature and sandwiched between layers of gelatin. This provided a simulation of the relative volume vs. number of cells in which we would seek to image DCs or other immune cells in situ in tumors. MRI of gelatin-suspended DCs treated with Gd-CA showed significant differences in the signal intensity as compared to untreated DCs in T1-weighted images (Fig. 2). We observed that the longitudinal relaxation rate (1/T1) of DCs labeled with 6.25, 25, and 50 mM Gd-CA increased by nearly 1.5-fold, three-fold, and four-fold relative to the 1/T1 of the control DCs (Fig. 2).
FIG. 2.
T1-weighted (TR = 350 ms and TE = 6.67 ms) image of Gd-CA labeled DCs. Tubes: 1 = 50 mM, 2 = 25 mM, 3 = 6.25 mM, 4 = unlabeled control DCs, and 5 = gelatin. Values for the longitudinal relaxation time (T1) obtained from saturation-recovery maps at room temperature were as follows: 410 (±41) ms, 603 (±68) ms, 1030(±218) ms, 1610 (±336) ms, and 1541 (±314) ms for tubes 1, 2, 3, 4, and 5, respectively. An analysis of variance (ANOVA) for T1 values between groups resulted in P = 1.3 × 10−9.
A comparison of the contrast enhancement as a function of repetition time (TR) is presented in Fig. 3. At the appropriate TR, the %CE of the DCs labeled with the lowest extracellular concentration of Gd-CA (6.25 mM) was higher than 100%. Specifically, we determined that the %CEs of DCs labeled with an extracellular Gd-CA concentration of 6.25, 25, or 50 mM were 115%, 220%, and 360%, at a TR of 350, 350, and 150 ms, respectively, relative to control DCs. These data suggest that this approach can successfully be used to monitor the injection of cells by MRI.
FIG. 3.
Contrast enhancement with variable TR in the gel suspension of Gd-CA–labeled DCs compared to unlabeled control DCs (TE = 10 ms, TR varied from 60 ms to 4000 ms). An analysis of variance (ANOVA) with each TR as a group for a particular loading concentration gave P values between groups: P = 1.01 × 10−15, 0.0004, and 0.0003, for 50, 25, and 6.25 mM, respectively. That is, the %CE values obtained at each TR are significantly different from each other for a given loading concentration. Another ANOVA with each loading concentration as a group for a given TR gives P values between groups: P = 2.3 × 10−6, 2.3 × 10−6, 2.0 × 10−5, 0.00016, 0.00067, 0.022, and 0.76, for 60, 150, 350, 800, 1500, 2500, and 4000 ms, respectively. That is, for a given repetition time the %CE values of the cells loaded with the different extracellular Gd-CA concentrations are significantly different from each other except for those obtained at 4000 ms.
The data obtained from Fig. 2 implies that if the agent is in a cellular compartment with fast water exchange, then a 0.67% DC cell volume will cause a 26% and 33% change in the tumor longitudinal relaxation rate (1/T1) at 1.5T and 7T, respectively, given cells labeled with the lowest extracellular concentration, 6.25 mM. Alternatively, we could get the same change in 1/T1 with one-third of the cells labeled with 25 mM extracellular Gd-CA. While the above analyses are not entirely quantitative, the data still conclusively indicate that DCs can be labeled with enough Gd(III)-chelate to visualize these cells using MRI.
Effect of Gd-CA On DC Phenotype and Function
To determine whether labeling of DCs with Gd-CA at levels suitable for MRI would affect cell physiology, we carried out experiments assessing DC expression of cell surface molecules important for their role in antigen presentation and assessing interactions with other cells in the immune system. DCs are mostly notably viewed as APCs that have the capacity for effectively interacting with naive T cells to provoke adaptive immunity (43). To begin the assessment of whether our approach to labeling DCs with MR contrast agents would affect their function, we performed flow cytometric analyses of expression of various cell markers on DCs labeled with varying concentrations of Gd-CA. As illustrated in Table 1, we determined that expression of MHC class I (OX18) and class II (OX6), and costimulatory molecules CD80 and CD86, were not reduced by Gd-CA. These data indicate that DCs can be labeled with Gd-CA for monitoring the injection site with the expectation that the cells will retain normal capacity for carrying out their role in the induction of adaptive immune responses. We also determined that Gd-CA labeling did not negatively affect expression of markers useful for identification of DCs, including CD161, OX42, and OX62. These data indicate that this contrast agent could provide a desirable means of labeling functionally normal DCs for monitoring their in vivo location following injection using MRI.
Table 1.
Effects of Gd-CA Labeling on Expression of MHC Class I (OX18) and II (OX6), Costimulatory Molecules (CD80 and CD86), and DC Markers (OX62, OX42, and CD161) on DCs*
| %+ | OX18 | OX6 | CD80 | CD86 | CD161 | OX62 | OX42 |
|---|---|---|---|---|---|---|---|
| DC | 45.7 | 32.8 | 18.2 | 38.1 | 9.5 | 61.0 | 47.8 |
| DC6.25 | 68.0 | 55.2 | 25.1 | 50.0 | 11.2 | 75.5 | 62.2 |
| DC12.5 | 60.3 | 44.2 | 22.9 | 50.1 | 15.5 | 70.7 | 54.6 |
| DC25 | 60.7 | 51.1 | 19.2 | 50.8 | 19.9 | 66.2 | 55.6 |
| DC50 | 61.2 | 56.6 | 27.0 | 47.6 | 21.0 | 73.2 | 62.8 |
Data are from a representative experiment of three similar experiments using different populations of DCs. There were no statistically significant differences in comparing percent positive DCs among control and Gd-CA–loaded cultures using any of the markers indicated.
Gd-CA = gadolinium contrast agent, DC, dendritic cell, MHC = major histocompatibility complex.
In addition to serving as the primary APCs in the induction of adaptive immunity, DCs cooperate with cells of the nonadaptive immune system in the induction of adaptive responses. We therefore set up experiments examining the effect that DC labeling with Gd-CA had on their capacity for reciprocal coactivation of NK cells. In this instance, coculture of NK cells and DCs for 24 h results in an increased capacity of NK cells for lysis of some tumor target cells. This phenomenon requires both direct contact of NK cells and DCs, as well as production of interleukin-12 (IL12) by DCs and interferon gamma (IFNγ), and tumor necrosis factor alpha (TNFα) by NK cells (24,44–46). To test this function, day 6 DCs were labeled with Gd-CA and cultured for 24 h with freshly isolated populations of splenocytes enriched for NK cells using various NK:DC ratios (1.25:1, 2.5:1, 5:1, and 10:1). Cocultured NK cells were assayed for lytic activity against YAC-1 target cells in 4 h, 51Cr-release assays at a 100:1 effector cell:target cell ratio. As illustrated in Table 2, we observed that coculture of control DCs with NK cells resulted in an enhanced level of cytotoxicity in which basal levels of NK lytic function were increased by 4.1-fold at an NK:DC ratio of 1.25:1, by 3.1-fold at an NK:DC ratio of 2.5:1, by 3.3-fold at an NK:DC ratio of 5:1, and by 2.9-fold at an NK:DC ratio of 10:1. When assessing the effects of labeling DCs with Gd(III)-HP-D03A on their capacity to interact with NK cells, we observed that there was no effect at any NK:DC ratio or any concentration of Gd-CA. In only one of more than five experiments (each performed in triplicate), the 1.25:1 NK:DC ratio at a concentration of 25 mM Gd-CA, did we observe a reduction in the boost from 4.1-fold to 2.4-fold (Table 2). No statistical significance was observed when comparing the unlabeled cells with cells labeled at the three different concentrations. These data indicate that any potential effects of Gd-CA on DC interactions with NK cells are not a significant concern as far as using this agent in the assessment of DC localization and function. As a final aspect of investigating the effects of Gd-CA on DC function, we assessed whether labeling DCs with this agent affect their capacity for migration. In these experiments, we determined that Gd-CA did not affect DC migration in Neuro Probe plates (Neuro Probe, Inc., Gaithersburg, MD, USA) at any concentration tested (data not shown).
Table 2.
DCs Labeled With Gd-CA Are Capable of Mediating Reciprocal Coactivation of NK Cells*
| Control | 25 mMa | 12.5 mMa | 6.25 mMa | |
|---|---|---|---|---|
| NK cellsb | 7 ± 1.5 | ND | ND | ND |
| NK:DC 1.25:1c | 29 ± 4.5 | 17 ± 3.2 | 25 ± 6.5 | 24 ± 2.9 |
| NK:DC 2.5:1c | 22 ± 2.6 | 20 ± 1.2 | 24 ± 0.8 | 21 ± 1.7 |
| NK:DC 5.0:1c | 23 ± 3.2 | 20 ± 6.1 | 25 ± 1.2 | 21 ± 1.4 |
| NK:DC 10:1c | 20 ± 3.0 | 21 ± 2.3 | 23 ± 1.6 | 19 ± 5.7 |
Data are from a representative experiment of more than five similar experiments using different populations of DCs and NK cells. Values are means from one experiment performed in triplicate of % specific cytotoxicity + SD. No statistical difference was found between the control cells and those labeled with Gd-CA (between groups).
Concentration of extracellular Gd-CA for labeling DCs.
NK cell:target cell effector:target ratio was 100:1, for all 51Cr-release cytotoxicity assays included.
Ratio of NK cells:DCs in cocultures.
DC = dendritic cell, Gd-CA = gadolinium contrast agent, NK cell = natural killer cell, ND = not done.
In Vivo MRI
Representative images of tumors injected with unlabeled DCs (Fig. 4) followed by i.v. injection of Gd-CA (Fig. 4c and d) are shown. In most cases, the tumor bed was localized 2 to 5 mm into the brain parenchyma. In all animals no contrast enhancement was observed after the injection of unloaded DCs prior to the i.v. injection of Gd(III)-CA. A total of five control animals were imaged following the injection of the unlabeled DCs. The injection of Gd-CA was used to highlight the tumor after the injection of DCs and all image analysis for %CE was performed on the pre-i.v.-injected images. Clearance of any detectable Gd-CA by MRI from the vasculature, including tumor vasculature, was observed within 2 h (data not shown). This is consistent with the reported plasma half-life in rats of these low molecular weight CAs.
FIG. 4.
Selective intratumoral injection of unlabeled DCs into rat brain tumor. T1-weighted (see Materials and Methods) images of the same rat brain injected with control DCs (a,b) and later intravenously with Gd-CA to show the tumor rim–enhancement (c,d).
In Fig. 5 we present representative images following the injection of DCs labeled with 25 mM extracellular of ProHance. Most of the contrast was observed near the site of injection (Fig. 5a–c) and was localized at the end of the needle track (Fig. 5b) spanning nearly 3 mm in diameter, while less contrast was apparent around the site of injection ≤4–5 mm in diameter (Fig. 5a–c). After imaging of DCs, a bolus of Gd-CA was injected intravenously via tail vein, which highlighted the tumor rim in T1-weighted images, indicating that the injection of labeled DCs was in the tumor bed (Fig. 5d–f). Comparison of the localization of injected DCs in relation to the highlighted tumor rim indicated that we were indeed able to image the labeled DCs inside the tumor. A significant difference was observed between the %CE of tumors injected with labeled DCs vs. tumors injected with untreated DCs and an analysis of variance (ANOVA) gave P = 0.00085. Seven animals injected with labeled DCs were imaged, resulting in a 103% %CE. This compared with no contrast enhancement observed in the five animals injected with the control DCs. Enhancement was observed in all the animals injected with loaded or labeled DCs and imaged 0.5 and 24 h postinjection of labeled DCs, The mean enhancements for the animals were 103 ± 49 and 90 ± 8.4 for the 0.5-h and 24-h postinjection of labeled DCs, respectively. There was no significant difference in the %CE between these two groups as analyzed by ANOVA for the two groups.
FIG. 5.
Selective intratumoral injection of Gd-CA–labeled DCs (labeled with 25 mM extracellular concentration of Gd-CA) into rat brain tumor. T1-weighted (see Materials and Methods) images of the same rat brain injected with Gd-CA–labeled DCs (a–c) and later intravenously with Gd-CA to show the tumor rim–enhancement (d–f).
DISCUSSION
There is general acknowledgement that ACI has significant potential for the treatment of some cancers. Harnessing that potential and putting it into standard clinical practice has not been readily accomplished. The reasons for this failure include things as simple as failure to efficiently deliver adoptively transferred cells to the tumor, to things as complex as systemic modulation by the tumor of the capacity of immune cells to curb initiation of an antitumor response. Several reports on the use of iron oxide, perfluorinated polyether, or Gd(III)-chelates appear in the literature. Of these, only those using iron oxide use a clinically-approved CA formulation. While iron oxide–based methods have advantages, several disadvantages also exist.
We therefore sought to address the issue of developing an efficient means of monitoring the delivery of cells to CNS tumors via intratumoral injection, making use of a Gd-based, clinically-approved, MR CA. We labeled populations of DCs generated ex vivo and demonstrated that this approach has potential for monitoring injection of either autologous or allogeneic cell populations; both of which are used in current, ongoing clinical trials.
Our results demonstrated uptake and retention of significant amounts of Gd-CA by ex vivo cultured iDCs derived from rat BM. Uptake of Gd-CA by DCs occurred in a predictable fashion. The intracellular [Gd(III)-CA] varied from 5.9 to 25 mM depending on the extracellular Gd-CA concentration. Such large concentrations would be expected given the cell type. DCs are able to internalize particulate and soluble material by a variety of processes, including receptor mediated endocytosis, micropinocytosis, and macropinocytosis. Micropinocytosis occurs constitutively in all cells, while the process of macropinocytosis is limited to a few cells, including DCs (41,47–49). Macropinocytosis is a critical aspect of uptake of soluble materials by DCs and it has been reported that DCs concentrate soluble materials nonspecifically from a large volume of extracellular fluid, approaching 1000 to 1500 µm3 [total cell volume]/h (41). This is well beyond the capacity for constitutive uptake of soluble materials by almost all other cells. These levels were maintained for at least 24 h postloading and sufficient to allow both in vitro and in vivo imaging of implanted DCs labeled with agent for 24 h. Contrast lasted for at least 24 h postinjection of DCs into the tumor bed and could be easily imaged (data not shown). This long-term retention of hyperintensity is consistent with the results reported by Crich et al. (36), who reported that they could image Gd(III)-HP-DO3A–loaded endothelial progenitor cells 1 d after implantation, and Biancone et al. (37), who reported that pancreatic islet cells loaded with Gd(III)-HP-DO3A could be imaged 65 d post injection. Our imaging studies indicated that we could monitor the relative efficacy of delivery of DCs into the tumor bed of CNS tumors when used serially with i.v. injection of the Gd-CA to define the tumor boundaries. We first imaged tumors within 30 min of injecting Gd-labeled DCs intratumorally. Following the imaging of tumors injected with loaded DCs we injected ProHance via the tail vein and collected images without any movement in the position of the animal. Superimposing these serially captured images allowed us to determine in 2D analyses whether we had delivered the DCs to the tumor bed. This approach should be useful in both preclinical and clinical settings in addressing one potential reason for the failure of ACI.
The ability to monitor the successful implantation of biological therapies would be useless if the method for labeling cells interfered with the biological outcome. The results presented in Tables 1 and 2 demonstrate that loading the DCs with Gd-based CAs does not negatively impact the DC cell phenotype or function. DCs efficiently take up and process antigens and present them in the context of MHC class I and class II molecules to naive T cells. They also express costimulatory receptors such as CD80 and CD86, which provide the so-called “second signals” important for activating naive T cells. Labeling the DCs with Gd-CA did not result in a loss of expression of either MHC class I or class II molecules or costimulatory receptors. Loading DCs with Gd-CA did not reduce expression of molecules such as CD161, OX42, or OX62, which would be useful for additional studies on localization of cells using immunohistochemistry. We also determined that the migration of DCs was unaffected by labeling with Gd-CA. Finally, the data presented in Table 2 demonstrates that DCs loaded with Gd-CA are still capable of cooperating with cells of the nonadaptive immune system and coactivating NK cells. Cumulatively, these data strongly support the continued development of the use of the clinically-approved formulation of Gd(III)-HP-DO3A as a means of labeling DCs, or other immune cells, for assessment of their delivery, trafficking, and localization in ACI of cancer.
ACKNOWLEDGMENTS
We are grateful to Dr. Tianbing Yang for his help with stereotactic surgeries. Drs. Kevin Hitchens and Chien Ho are acknowledged for their assistance with MRI at the Pittsburgh NMR Center for Biomedical Research, Carnegie-Mellon University, Pittsburgh, PA, USA, which is supported by National Institutes of Health (NIH) grant P41-EB001977.
Grant sponsor: National Institutes of Health (NIH); Grant numbers: CA098717, CA47904, P41-EB001977; Grant sponsor: James S. McDonnell Foundation.
REFERENCES
- 1.Parajuli P, Mathupala S, Sloan AE. Systematic comparison of dendritic cell-based immunotherapeutic strategies for malignant gliomas: in vitro induction of cytolytic and natural killer-like T cells. Neurosurgery. 2004;55:1194–1204. doi: 10.1227/01.neu.0000141082.20865.48. [DOI] [PubMed] [Google Scholar]
- 2.Coccoris M, de Witte MA, Schumacher TN. Prospects and limitations of T cell receptor gene therapy. Curr Gene Ther. 2005;5:583–593. doi: 10.2174/156652305774964730. [DOI] [PubMed] [Google Scholar]
- 3.Foster AE, Rooney CM. Improving T cell therapy for cancer. Expert Opin Biol Ther. 2006;6:215–229. doi: 10.1517/14712598.6.3.215. [DOI] [PubMed] [Google Scholar]
- 4.Gattinoni L, Powell DJ, Jr, Rosenberg SA, Restifo NP. Adoptive immunotherapy for cancer: building on success. Nat Rev Immunol. 2006;6:383–393. doi: 10.1038/nri1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knutson KL, Wagner W, Disis ML. Adoptive T cell therapy of solid cancers. Cancer Immunol Immunother. 2006;55:96–103. doi: 10.1007/s00262-005-0706-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tey SK, Bollard CM, Heslop HE. Adoptive T-cell transfer in cancer immunotherapy. Immunol Cell Biol. 2006;84:281–289. doi: 10.1111/j.1440-1711.2006.01441.x. [DOI] [PubMed] [Google Scholar]
- 7.Ahrens ET, Flores R, Xu H, Morel PA. In vivo imaging platform for tracking immunotherapeutic cells. Nat Biotechnol. 2005;23:983–987. doi: 10.1038/nbt1121. [DOI] [PubMed] [Google Scholar]
- 8.Barratt-Boyes SM, Zimmer MI, Harshyne LA, Meyer EM, Watkins SC, Capuano S, 3rd, Murphey-Corb M, Falo LD, Jr, Donnenberg AD. Maturation and trafficking of monocyte-derived dendritic cells in monkeys: implications for dendritic cell-based vaccines. J Immunol. 2000;164:2487–2495. doi: 10.4049/jimmunol.164.5.2487. [DOI] [PubMed] [Google Scholar]
- 9.Condon C, Watkins SC, Celluzzi CM, Thompson K, Falo LD., Jr DNA-based immunization by in vivo transfection of dendritic cells. Nat Med. 1996;2:1122–1128. doi: 10.1038/nm1096-1122. [DOI] [PubMed] [Google Scholar]
- 10.Brown K, Gao W, Alber S, Trichel A, Murphey-Corb M, Watkins SC, Gambotto A, Barratt-Boyes SM. Adenovirus-transduced dendritic cells injected into skin or lymph node prime potent simian immunodeficiency virus-specific T cell immunity in monkeys. J Immunol. 2003;171:6875–6882. doi: 10.4049/jimmunol.171.12.6875. [DOI] [PubMed] [Google Scholar]
- 11.Yang T, Witham TF, Villa L, Erff M, Attanucci J, Watkins S, Kondziolka D, Okada H, Pollack IF, Chambers WH. Glioma-associated hyaluronan induces apoptosis in dendritic cells via inducible nitric oxide synthase: implications for the use of dendritic cells for therapy of gliomas. Cancer Res. 2002;62:2583–2591. [PubMed] [Google Scholar]
- 12.Chi KH, Liu SJ, Li CP, Kuo HP, Wang YS, Chao Y, Hsieh SL. Combination of conformal radiotherapy and intratumoral injection of adoptive dendritic cell immunotherapy in refractory hepatoma. J Immunother. 2005;28:129–135. doi: 10.1097/01.cji.0000154248.74383.5e. [DOI] [PubMed] [Google Scholar]
- 13.Kianmanesh A, Hackett NR, Lee JM, Kikuchi T, Korst RJ, Crystal RG. Intratumoral administration of low doses of an adenovirus vector encoding tumor necrosis factor alpha together with naive dendritic cells elicits significant suppression of tumor growth without toxicity. Hum Gene Ther. 2001;12:2035–2049. doi: 10.1089/10430340152677395. [DOI] [PubMed] [Google Scholar]
- 14.Vera M, Razquin N, Prieto J, Melero I, Fortes P, Gonzalez-Aseguinolaza G. Intratumoral injection of dendritic cells transduced by an SV40-based vector expressing interleukin-15 induces curative immunity mediated by CD8+ T lymphocytes and NK cells. Mol Ther. 2005;12:950–959. doi: 10.1016/j.ymthe.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 15.Tatsumi T, Huang J, Gooding WE, Gambotto A, Robbins PD, Vujanovic NL, Alber SM, Watkins SC, Okada H, Storkus WJ. Intratumoral delivery of dendritic cells engineered to secrete both interleukin (IL)-12 and IL-18 effectively treats local and distant disease in association with broadly reactive Tc1-type immunity. Cancer Res. 2003;63:6378–6386. [PubMed] [Google Scholar]
- 16.Ehtesham M, Kabos P, Gutierrez MA, Samoto K, Black KL, Yu JS. Intratumoral dendritic cell vaccination elicits potent tumoricidal immunity against malignant glioma in rats. J Immunother. 2003;26:107–116. doi: 10.1097/00002371-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Murakami T, Tokunaga N, Waku T, Gomi S, Kagawa S, Tanaka N, Fujiwara T. Antitumor effect of intratumoral administration of bone marrow-derived dendritic cells transduced with wild-type p53 gene. Clin Cancer Res. 2004;10:3871–3880. doi: 10.1158/1078-0432.CCR-03-0599. [DOI] [PubMed] [Google Scholar]
- 18.Ali S, Curtin JF, Zirger JM, Xiong W, King GD, Barcia C, Liu C, Puntel M, Goverdhana S, Lowenstein PR, Castro MG. Inflammatory and anti-glioma effects of an adenovirus expressing human soluble Fms-like tyrosine kinase 3 ligand (hsFlt3L): treatment with hsFlt3L inhibits intracranial glioma progression. Mol Ther. 2004;10:1071–1084. doi: 10.1016/j.ymthe.2004.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmed SU, Okamoto M, Oshikawa T, Tano T, Sasai A, Kan S, Hiroshima T, Ohue H, Moriya Y, Ryoma Y, Saito M, Sato M. Anti-tumor effect of an intratumoral administration of dendritic cells in combination with TS-1, an oral fluoropyrimidine anti-cancer drug, and OK-432, a streptococcal immunopotentiator: involvement of toll-like receptor 4. J Immunother. 2004;27:432–441. doi: 10.1097/00002371-200411000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Tsugawa T, Kuwashima N, Sato H, Fellows-Mayle WK, Dusak JE, Okada K, Papworth GD, Watkins SC, Gambotto A, Yoshida J, Pollack IF, Okada H. Sequential delivery of interferon-alpha gene and DCs to intracranial gliomas promotes an effective antitumor response. Gene Ther. 2004;11:1551–1558. doi: 10.1038/sj.gt.3302300. [DOI] [PubMed] [Google Scholar]
- 21.Kuwashima N, Nishimura F, Eguchi J, Sato H, Hatano M, Tsugawa T, Sakaida T, Dusak JE, Fellows-Mayle WK, Papworth GD, Watkins SC, Gambotto A, Pollack IF, Storkus WJ, Okada H. Delivery of dendritic cells engineered to secrete IFN-alpha into central nervous system tumors enhances the efficacy of peripheral tumor cell vaccines: dependence on apoptotic pathways. J Immunol. 2005;175:2730–2740. doi: 10.4049/jimmunol.175.4.2730. [DOI] [PubMed] [Google Scholar]
- 22.Choi GS, Lee MH, Kim SK, Kim CS, Lee HS, Im MW, Kil HY, Seong DH, Lee JR, Kim WC, Lee MG, Song SU. Combined treatment of an intratumoral injection of dendritic cells and systemic chemotherapy (Paclitaxel) for murine fibrosarcoma. Yonsei Med J. 2005;46:835–842. doi: 10.3349/ymj.2005.46.6.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Janjic BM, Lu G, Pimenov A, Whiteside TL, Storkus WJ, Vujanovic NL. Innate direct anticancer effector function of human immature dendritic cells. I. Involvement of an apoptosis-inducing pathway. J Immunol. 2002;168:1823–1830. doi: 10.4049/jimmunol.168.4.1823. [DOI] [PubMed] [Google Scholar]
- 24.Fernandez NC, Lozier A, Flament C, Ricciardi-Castagnoli P, Bellet D, Suter M, Perricaudet M, Tursz T, Maraskovsky E, Zitvogel L. Dendritic cells directly trigger NK cell functions: cross-talk relevant in innate anti-tumor immune responses in vivo. Nat Med. 1999;5:405–411. doi: 10.1038/7403. [DOI] [PubMed] [Google Scholar]
- 25.Mailliard RB, Son YI, Redlinger R, Coates PT, Giermasz A, Morel PA, Storkus WJ, Kalinski P. Dendritic cells mediate NK cell help for Th1 and CTL responses: two-signal requirement for the induction of NK cell helper function. J Immunol. 2003;171:2366–2373. doi: 10.4049/jimmunol.171.5.2366. [DOI] [PubMed] [Google Scholar]
- 26.Akasaki Y, Black KL, Yu JS. T cell immunity in patients with malignant glioma: recent progress in dendritic cell-based immunotherapeutic approaches. Front Biosci. 2005;10:2908–2921. doi: 10.2741/1747. [DOI] [PubMed] [Google Scholar]
- 27.Mazzolini G, Alfaro C, Sangro B, Feijoό E, Ruiz J, Benito A, Tirapu I, Arina A, Sola J, Herraiz M, Lucena F, Olagüe C, Subtil J, Quiroga J, Herrero I, Sádaba B, Bendandi M, Qian C, Prieto J, Melero I. Intratumoral injection of dendritic cells engineered to secrete interleukin-12 by recombinant adenovirus in patients with metastatic gastrointestinal carcinomas. J Clin Oncol. 2005;23:999–1010. doi: 10.1200/JCO.2005.00.463. [DOI] [PubMed] [Google Scholar]
- 28.de Vries IJ, Lesterhuis WJ, Barentsz JO, Verdijk P, van Krieken JH, Boerman OC, Oyen WJ, Bonenkamp JJ, Boezeman JB, Adema GJ, Bulte JW, Scheenen TW, Punt CJ, Heerschap A, Figdor CG. Magnetic resonance tracking of dendritic cells in melanoma patients for monitoring of cellular therapy. Nat Biotechnol. 2005;23:1407–1413. doi: 10.1038/nbt1154. [DOI] [PubMed] [Google Scholar]
- 29.Yeh TC, Zhang W, Ildstad ST, Ho C. Intracellular labeling of T-cells with superparamagnetic contrast agents. Magn Reson Med. 1993;30:617–625. doi: 10.1002/mrm.1910300513. [DOI] [PubMed] [Google Scholar]
- 30.Yeh TC, Zhang W, Ildstad ST, Ho C. In vivo dynamic MRI tracking of rat T-cells labeled with superparamagnetic iron-oxide particles. Magn Reson Med. 1995;33:200–208. doi: 10.1002/mrm.1910330209. [DOI] [PubMed] [Google Scholar]
- 31.Ahrens ET, Feili-Hariri M, Xu H, Genove G, Morel PA. Receptor-mediated endocytosis of iron-oxide particles provides efficient labeling of dendritic cells for in vivo MR imaging. Magn Reson Med. 2003;49:1006–1013. doi: 10.1002/mrm.10465. [DOI] [PubMed] [Google Scholar]
- 32.Kircher MF, Allport JR, Graves EE, Love V, Josephson L, Lichtman AH, Weissleder R. In vivo high resolution three-dimensional imaging of antigen-specific cytotoxic T-lymphocyte trafficking to tumors. Cancer Res. 2003;63:6838–6846. [PubMed] [Google Scholar]
- 33.Bulte JW, Arbab AS, Douglas T, Frank JA. Preparation of magnetically labeled cells for cell tracking by magnetic resonance imaging. Methods Enzymol. 2004;386:275–299. doi: 10.1016/S0076-6879(04)86013-0. [DOI] [PubMed] [Google Scholar]
- 34.Metz S, Bonaterra G, Rudelius M, Settles M, Rummeny EJ, Daldrup-Link HE. Capacity of human monocytes to phagocytose approved iron oxide MR contrast agents in vitro. Eur Radiol. 2004;14:1851–1858. doi: 10.1007/s00330-004-2405-2. [DOI] [PubMed] [Google Scholar]
- 35.Himmelreich U, Aime S, Hieronymus T, Justicia C, Uggeri F, Zenke M, Hoehn M. A responsive MRI contrast agent to monitor functional cell status. Neuroimage. 2006;32:1142–1149. doi: 10.1016/j.neuroimage.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 36.Crich SG, Biancone L, Cantaluppi V, Duo D, Esposito G, Russo S, Camussi G, Aime S. Improved route for the visualization of stem cells labeled with a Gd-/Eu-chelate as dual (MRI and fluorescence) agent. Magn Reson Med. 2004;51:938–944. doi: 10.1002/mrm.20072. [DOI] [PubMed] [Google Scholar]
- 37.Biancone L, Crich SG, Cantaluppi V, Romanazzi GM, Russo S, Scala-brino E, Esposito G, Figliolini F, Beltramo S, Perin PC, Segoloni GP, Aime S, Camussi G. Magnetic resonance imaging of gadolinium-labeled pancreatic islets for experimental transplantation. NMR Biomed. 2007;20:40–48. doi: 10.1002/nbm.1088. [DOI] [PubMed] [Google Scholar]
- 38.Louie AY, Huber MM, Ahrens ET, Rothbacher U, Moats R, Jacobs RE, Fraser SE, Meade TJ. In vivo visualization of gene expression using magnetic resonance imaging. Nat Biotechnol. 2000;18:321–325. doi: 10.1038/73780. [DOI] [PubMed] [Google Scholar]
- 39.Brissette-Storkus CS, Kettel JC, Whitham TF, Giezeman-Smits KM, Villa LA, Potter DM, Chambers WH. Flt-3 ligand (FL) drives differentiation of rat bone marrow-derived dendritic cells expressing OX62 and/or CD161 (NKR-P1) J Leukoc Biol. 2002;71:941–949. [PubMed] [Google Scholar]
- 40.Chambers WH, Bozik ME, Brissette-Storkus SC, Basse P, Redgate E, Watkins S, Boggs SS. NKR-P1+ cells localize selectively in Rat 9L gliosarcomas but have reduced cytolytic function. Cancer Res. 1996;56:3516–3525. [PubMed] [Google Scholar]
- 41.Sallusto F, Cella M, Danieli C, Lanzavecchia A. Dendritic cells use macropinocytosis and the mannose receptor to concentrate macromolecules in the major histocompatibility complex class II compartment: downregulation by cytokines and bacterial products. J Exp Med. 1995;182:389–400. doi: 10.1084/jem.182.2.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Baey A, Lanzavecchia A. The role of aquaporins in dendritic cell macropinocytosis. J Exp Med. 2000;191:743–748. doi: 10.1084/jem.191.4.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kalinski P, Hilkens CM, Wierenga EA, Kapsenberg ML. T-cell priming by type-1 and type-2 polarized dendritic cells: the concept of a third signal. Immunol Today. 1999;20:561–567. doi: 10.1016/s0167-5699(99)01547-9. [DOI] [PubMed] [Google Scholar]
- 44.Kapsenberg ML, Kalinski P. The concept of type 1 and type 2 antigen-presenting cells. Immunol Lett. 1999;69:5–6. doi: 10.1016/s0165-2478(99)00096-6. [DOI] [PubMed] [Google Scholar]
- 45.Fanger NA, Maliszewski CR, Schooley K, Griffith TS. Human dendritic cells mediate cellular apoptosis via tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) J Exp Med. 1999;190:1155–1164. doi: 10.1084/jem.190.8.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ferlazzo G, Tsang ML, Moretta L, Melioli G, Steinman RM, Munz C. Human dendritic cells activate resting natural killer (NK) cells and are recognized via the NKp30 receptor by activated NK cells. J Exp Med. 2002;195:343–351. doi: 10.1084/jem.20011149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Racoosin EL, Swanson JA. Macrophage colony-stimulating factor (rM-CSF) stimulates pinocytosis in bone marrow-derived macrophages. J Exp Med. 1989;170:1635–1648. doi: 10.1084/jem.170.5.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Racoosin EL, Swanson JA. M-CSF-induced macropinocytosis increases solute endocytosis but not receptor-mediated endocytosis in mouse macrophages. J Cell Sci. 1992;102(Pt 4):867–880. doi: 10.1242/jcs.102.4.867. [DOI] [PubMed] [Google Scholar]
- 49.West MA, Bretscher MS, Watts C. Distinct endocytotic pathways in epidermal growth factor-stimulated human carcinoma A431 cells. J Cell Biol. 1989;109:2731–2739. doi: 10.1083/jcb.109.6.2731. [DOI] [PMC free article] [PubMed] [Google Scholar]