Abstract
In this paper, we conceptualized fatalism as a set of health beliefs that encompass the dimensions of predetermination, luck and pessimism. A 20-item scale was developed as a measurement instrument. Confirmatory factor analyses were performed to test the dimensionality of the scale. Three external variables (i.e., genetic determinism, perceived benefits of lifestyle change, and intention to engage in healthy behavior) were used as reference variables to test the construct validity of the scale. Data from a web-based national survey (N=1218) showed that the scale was unidimensional on the second order, and with good reliability (α =.88). The relationships between the external variables and the first- and second-order factors provided evidence of the scale’s external consistency and construct validity.
Keywords: fatalism, confirmatory factor analysis, construct validity, genetic determinism, perceived benefits, behavioral intention
Recent research has shown an increasing interest in the role of fatalism in health behavior, both as an independent and a dependent variable (Powe & Finnie, 2003). This interest has been generated by the fact that fatalistic beliefs are correlated with lower intentions to change behavior and with a variety of negative health outcomes regarding cancer (see Powe & Finnie, 2003 for a review), cardiovascular diseases (Urizar & Sears 2006), diabetes (Egede & Bonadonna, 2003), coping with extreme stress (Yeh, Inman, Kim, & Okubo, 2006; Zimrin, 1986); coping with HIV/AIDS risks (Varga, 2001), smoking attitudes and behavior (Schnoll et al., 2002; Unger et al., 2002), lower social function (Urizar & Sears, 2006), suicidal behavior (Roberts, Roberts, & Chen, 1998), quality of life among HIV-infected women (Sowell et al., 1997), attitude toward safety and accident prevention (Rundmo & Hale, 2003), and unsafe sex practices (Kalichman, Kelly, Morgan, & Rompa, 1997). The interest is heightened by the identification of disproportionate fatalism among low income and minority populations who are impacted negatively by health disparities (Powe & Johnson, 1995; Mechanic, 2002).
Thus, reducing or eliminating one’s fatalistic beliefs not only might help increase likelihood of behavioral change, but also has the potential to reduce health disparities. A clear conceptualization and valid measurement of fatalism is prerequisite to such research projects. Although fatalism has been conceived and operationalized in a variety of ways, the most fully elaborated treatment is provided by Powe and her associates with regard to cancer fatalism (Powe, 1995; Powe & Johnson 1995; Powe & Weinrich, 1999; Powe, Daniels, & Finnie, 2005). Building on Powe’s analyses and scale development efforts, we sought to conceptualize and build a measure for fatalism that might be applicable across a wider range of health conditions and with a broader set of cultures.
Our aims in this paper were twofold. First, we sought to develop a fatalism scale based on existing scales and evaluate its dimensional structure. Second, we hoped to locate the scale in a nomological network of situational variables for the purpose of evaluating its validity. The concept of fatalism will be explicated first. Existing scales will be evaluated and development of a new scale presented. Data from a national survey were analysed to explore the psychometric property of the new fatalism scale, and to assess its validity and reliability.
Scale Development
Conceptualization of Fatalism
Fatalism has been defined in a range of ways from “passively denying personal control” (Neff & Hoppe, 1993) to the belief that death is inevitable when a serious disease is present (Powe et al., 2005). In existing literature, the nature of fatalism encompasses one, or some combination of the following dimensions: (a) the individual’s perceived lack of (internal) control over external events in his or her life (Chavez, Hubbell, Mishra, & Valdez, 1997; Davison, Fankel, & Smith, 1992; Neff & Hoppe, 1993; Straughan & Seow, 1998), (b) notions of fate, luck, destiny and predetermination of a disease or health condition (Cohen & Nisbett, 1998; Davison et al., 1992; Straughan & Seow, 1998), and (c) perceptions of powerlessness, hopelessness, and meaninglessness due to expectations of negative health consequences(Scheier & Bridges, 1995; Powe & Johnson, 1995). Despite the differences, these scholars tend to agree that fatalism is cognitive in nature. Also, this body of literature as a whole suggests that fatalism can be conceptualized as a set of health beliefs that encompasses such dimensions as predetermination, pessimism, and attribution of one’s health (life events) to luck.
Evaluation of Existing Fatalism Scales
The credibility of substantive research findings derives from the reliability and validity of the instruments on which those findings are based. Accordingly, evaluation of the psychometric properties of a scale to measure fatalism is an important precursor to building a body of knowledge focused on individual differences in dispositional fatalistic beliefs. Judgments of the dimensionality of a measure should be based on three criteria: item content, associations among the items, and associations between the items and external variables (Hunter & Gerbing, 1982).
Quite a few scholars have developed scales to measure fatalism (see Powe & Finnie, 2003 for a review). The most widely used measurement instrument has been the 15-item Powe Fatalism Inventory (PFI, Powe, 1995). The majority of these scales capture one single dimension in the construct of fatalism, and to our knowledge none of them has undergone a systematic development through rigid content assessment and psychometric development. In contrast, the PFI captures multiple dimensions, and has demonstrated good reliabilities; however, our assessments showed that the PFI also has some limitations: (a) the PFI is problematic in content validity; (b) the unidimensionality of the scale has not been established; and (c) there is a lack of test of or evidence for the scale’s construct validity.
Content validity
Powe originally conceptualized the PFI among African American samples based on four philosophical components: fear, predetermination, pessimism, and inevitable death (Powe, 1995). Such a conceptualization is problematic in several ways. First, the meaning of fatalism might be unstable when it comes to other cultures. As Powe and Finnie (2003) noted, when working with other groups, especially of Chinese heritage, the PFI produced slightly different implications. Second, the four components of fatalism do not seem to reflect the construct well. As a set of beliefs, fatalism is cognitive in nature; hence, fear should not be a sub-dimension. Cognition and affect are distinct constructs, although there is evidence that the two are intertwined (Phelps, 2006) and controversy exists over the primacy of the two (see Lazarus, 1999). It is more appropriate to conceptualize fear1 as an immediate consequence of fatalism. The other three components also seem to overlap with each other (inevitable death and pessimism, inevitable death and predetermination), and might not be mutually exclusive. Additionally, other scholars have suggested the dimension of luck in fatalism (Cohen & Nisbett, 1998; Davison et al., 1992; Straughan & Seow, 1998); however, it is not captured by the PFI.
A final content constraint of the PFI is that it is disease constrained. The PFI was developed solely with regard to cancer, and the scale requires researchers to specific a single, specific disease. The focus on “death” in the scale may be appropriate to cancer, but other diseases may have a wider range of potential outcomes of issue. Recent efforts at “bundling” disease messages and the overlap between the causes of many common diseases and particular health behaviors related to them also make non-disease specific scales desirable for some applications.
Unidimensionality
The criterion regarding associations among the items of the scale requires that the scale should demonstrate a simple factor structure. Powe (1996) reported unpublished factor analyses findings and claimed that the 15 items of PFI loaded on a single factor, except that two of them had low loadings. Powe did not provide much detail about her factor analysis. However, we suspect that the single factor could be the artifact of three of the four dimensions (i.e., inevitable death, pessimism, and predetermination) overlapping with each other and that the two items with low factor loadings were the fear dimension. Without further information, it was also impossible to assess if factor loadings demonstrated a simple structure.
In addition, obviously what Powe reported was from exploratory factor analyses. Although exploratory analysis is appropriate when there are no prior hypotheses concerning factor structure, the confirmatory approach provides a more meaningful test by requiring the researcher to specify the number of factors according to theoretical and substantive knowledge, then to constrain some of the factor loadings to zero (Bollen, 1989; DeVellis, 1991). Good reliabilities (Mayo, Ureda, & Parker, 2001; Powe, 1995, 1997, 2001; Powe & Weinrich, 1999) provided little support for the unidimensionality claim. Finally, the claim of first-order unidimensionality obviously contradicted her four components of fatalism, which suggest that the construct has four (first order) factors.
Based on analyses of the literature and our own conceptualization, we argue that fatalism is better conceptualized as multi-dimensional on the first order (i.e., predetermination, luck, and pessimism), and that second order unidimensionality has to be established before the scale can be used as a single construct. Otherwise, it would be more appropriate and more meaningful to use and interpret the sub-factors, instead of the scale as a whole.
Construct validity
The criterion of correlations between the scale items and external variables assess the construct validity of a measurement instrument. Although there is evidence that the PFI is correlated with external variables such as demographics (Powe, 2001), spirituality (Powe, 1997) and screening behavior (Mayo et al., 2001; Powe, 1995), they provide little support for the scale’s construct validity, given that the scale’s unidimensionality has yet to be established.
Developing & Validating a New Scale
Given the problems in PFI, there is need to develop a fatalism scale that has better content validity (i.e., better reflect the semantic meaning of the construct), clear psychometric property (i.e., unidimensionality clearly established), and better construct validity (i.e., relationships with external variables investigated). Built upon the work of Powe and other researchers, we developed a new fatalism scale and attempted to provide evidence with regard to the construct validity of the scale by examining its behavior with such variables as genetic determinism, perceived benefits of lifestyle change, and intention to engage in healthy behaviors.
Genetic determinism is a set of rigid views that one’s health status and life as a whole follow a predetermined course because of one’s genetic heredity (Peters, 2002). Some argue that genetic determinism could be a cause of fatalism (Alper & Beckwith, 1993; Emery, 2001; Senior, Marteau, & Peters, 1998). Hence it is predicted that fatalism is positively associated with genetic determinism (H1). More fatalistic individuals tend to be pessimistic about benefits of lifestyle change, and less likely to adopt health behaviors such as health lifestyles (Niederdeppe & Levy, 2007; Straughton & Seow, 1998). Therefore, it is predicted that fatalism is negatively associated with estimated benefits of lifestyle change (H2) and intention to engage in healthy behaviors (H3).
Method
Development of a New Fatalism Scale
A new fatalism scale was developed in three steps to measure fatalism conceptualized as the combination of predetermination, pessimism and luck. In Step One, some of the PFI items on predetermination and pessimism were adapted and new items (for all three dimensions) were created by a research team that consisted of two faculty members and eight graduate students. The items were presented to a multi-cultural Community Advisory Board (CAB) for comments. The CAB members included 4 Chinese Americans, 3 Hispanic Americans, 3 African Americans, and 3 White Americans. CAB members were asked to review items for the level of clarity (including readability), cultural appropriateness, and cultural inclusion. In Step Two, the items were pre-tested with a sample of college students recruited from introductory communication classes at University of XXXX. Items that were perceived to be awkward in wording, low in face validity, or difficult to respond to were dropped, reducing the total number of items to 20. Table 1 presents the items and corresponding dimensions of fatalism. In Step Three, data were collected as a part of a web-based national survey, where individuals responded on Likert scales (1=strongly disagree, 5=strongly agree) to measures of fatalism, genetic determinism, perceived benefits of adopting healthy lifestyle, and their intentions to engage in healthy behaviors, in addition to reporting their demographic information.
Table 1.
Items and Dimensions of the Fatalism Scale
| Dimension | Item |
|---|---|
| Predetermination | 1. If someone is meant to get a serious disease, it doesn’t matter what kinds of food they eat, they will get that disease anyway. |
| 2. If someone is meant to get a serious disease, they will get it no matter what they do. | |
| 3. If someone gets a serious disease, that’s the way they were meant to die. | |
| 4. If someone is meant to have a serious disease, they will get that disease. | |
| 5. If someone has a serious disease and gets treatment for it, they will probably still die from it. | |
| 6. If someone was meant to have a serious disease, it doesn’t matter what doctors and nurses tell them to do, they will get the disease anyway. | |
| 7. How long I live is predetermined. | |
| 8. I will die when I am fated to die. | |
| 9. My health is determined by fate. | |
| 10. My health is determined by something greater than myself. | |
| Luck | 11. I will get diseases if I am unlucky. |
| 12. My health is a matter of luck. | |
| 13. How long I live is a matter of luck. | |
| 14. I will stay healthy if I am lucky. | |
| Pessimism | 15. Everything that can go wrong for me does. |
| 16. I will have a lot of pain from illness. | |
| 17. I will suffer a lot from bad health. | |
| 18. I often feel helpless in dealing with the problems of life. | |
| 19. Sometimes I feel that I’m being pushed around in life. | |
| 20. There is really no way I can solve some of the problems I have. |
Data Collection
Participants
The participants were randomly selected from a nationally representative panel by a professional research company, Knowledge Networks. The participants received hardware equipment and free Internet access to participate in the panel, and other incentives to complete the survey. The participants in this study came from 800 general population samples with two 200 over-samples from Hispanic and African-American respondents. The survey took place from June 26 to July 22, 2007, and 1218 surveys were completed during this period of time. The response rate was 75% for the general population samples, 66% for the Hispanic samples, and 67% for the African American samples. The N was reduced to 1145 in subsequent data analyses due to missing values.
Among the participants, 212 (17.4%) were from the Northeast, 267 (21.9%) from the Midwest, 455 (37.4%) from the South, and 284 (23.3%) from the West. They were all above 18 years of age (M= 46.73, SD=16.45), and 48.2% were male. Six hundred and seven of them (49.8%) identified themselves as “White, Non-Hispanic,” 272 (22.3%) as “Black, Non-Hispanic”, 289 (23.7%) as “Hispanic,” and 23 (1.9%) as “2 and more races, Non-Hispanic.” Thirty-nine (3.2%) of them had less than high school education, 157 (12.9%) had some high school, but no diploma, 384 (31.5%) graduated from high school, 264 (21.7%) had some college, but no degree, 84 (6.9%) had associate degree, 179 (14.7%) had bachelor’s degree, 82 (6.7%) had master’s degree, 16 (1.3%) had professional degree and 13 (1.1%) had doctoral degree. Their annual household income ranged from less than $5,000 (3.6%) to over $175, 000 (1.0%), 44.7% were below $35,000.
Other Measures
Genetic determinism
Genetic determinism was measured by nine Likert scale items (1=strongly disagree, 5=strong agree) adapted from Parrott et al. (2004). Example items were: “Genes determine how a person’s behavior impacts their health,” “Genes are the most important contributor to one’s health,” and “Genes are more important than one’s own behavior in determining one’s health.” The nine items yielded a unidimensional structure in confirmatory factor analysis and were averaged into an index for genetic determinism. The alpha reliability of the scale was 78
Benefits of lifestyle change
Two open-ended, counter-factual questions asked about perceived benefits of lifestyle change. The exact wording of the first question was, “Person X is an average adult who eats two servings of fruits or vegetables a day and gets heart disease. If they had been eating five servings of fruits and vegetables a day, how many years do you think that would have delayed their getting heart disease?” The exact wording of the other question was, “Person Z is an average adult who did not exercise and got heart disease. If they had taken a brisk walk for about a half hour a day, how many years do you think that would have delayed their getting heart disease?” Individuals’ responses to the two questions were correlated at r=.75, p<.001. The z-score of the two were averaged into an index of benefits of lifestyle change.
Intention to engage in healthy behaviors
Four Likert scale items (1=strongly disagree, 5=strongly agree) measured individuals’ intention to engage in healthy behaviors. The items were: “I will eat five servings of fruit and vegetables almost everyday,” “I am going to do 30 minutes brisk exercise almost everyday,” “Throughout my life I will maintain a healthy weight,” and “I intend to maintain a healthy lifestyle by making healthy choices everyday.” The four items yielded a unidimensioanl structure in confirmatory factor analysis and were averaged into an index for intention to engage in healthy behavior. Alpha reliability for the scale was 73.
Results
Confirmatory Factor Analysis
Unless unidimensionality of the fatalism scale is established on the first order, evidence in support of its second order unidimensionality needs to come from two sources: (a) a first order oblique three-factor model should fit to the data and the correlations among the three factors should be similar (i.e., a simple factor structure), and (b) statistical equivalence has to be established between the first order three-factor model and a second order single-factor model. Because a factor model with three indicators is just-identified (i.e., d.f.=0), the second order single-factor model would have the same degrees of freedom and the exact model fit indices as the first order oblique three-factor model. To test the statistical equivalence of the two, instrumental variables have to be introduced such that the two models would differ in degrees of freedom. All three external variables, namely, perceived benefits from lifestyle change, behavioral intention and genetic determinism were entered in the structural equation models together with the 20 fatalism items. The three instrumental variables gave six degrees of freedom between the first order three-factor model and the second-order single factor model. With a sample size of 1145, these parameters led to a statistical power of over .80 in testing the equivalence of the two factor models (Loehlin, 1998; MacCallum, Browne, & Sugawara, 1996).
Input and model specifications
Together with the instrumental variables of genetic determinism, perceived benefits from lifestyle change, and behavioral intention, individuals’ responses to the fatalism items were submitted to LISREL 8.70 for confirmatory factor analyses. Table 2 presents the means, standard deviations, and correlation matrix of the 20 fatalism items. A covariance matrix was constructed, then used as input to LISREL, which estimated the parameters of the models using maximum likelihood procedures. First, a first order oblique three-factor model was estimated, where the three factors (i.e., predetermination, luck and pessimism) were allowed to correlate with each other and each with the three external variables as well. The external variables were also allowed to be associated with each other. Second, a second order single-factor model was estimated, where only the second order factor was allowed to be associated with the external variables, but not the three first order factors. Again, association among the external variables were allowed.
Table 2.
Means, Standard Deviations and Correlation Matrix of the Fatalism Items (N=1145)
| Item | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2.72 | .99 | 1.0 | |||||||||||||||||||
| 2 | 2.73 | 1.01 | .62 | 1.0 | ||||||||||||||||||
| 3 | 2.45 | .93 | .41 | .46 | 1.0 | |||||||||||||||||
| 4 | 2.84 | .98 | .59 | .63 | .46 | 1.0 | ||||||||||||||||
| 5 | 2.36 | .82 | .28 | .29 | .37 | .28 | 1.0 | |||||||||||||||
| 6 | 2.58 | .99 | .58 | .58 | .42 | .56 | .29 | 1.0 | ||||||||||||||
| 7 | 2.97 | 1.16 | .32 | .38 | .32 | .35 | .13 | .38 | 1.0 | |||||||||||||
| 8 | 3.31 | 1.09 | .40 | .40 | .35 | .46 | .14 | .39 | .44 | 1.0 | ||||||||||||
| 9 | 2.41 | .96 | .41 | .45 | .43 | .40 | .26 | .44 | .33 | .40 | 1.0 | |||||||||||
| 10 | 3.11 | 1.13 | .36 | .39 | .29 | .36 | .14 | .36 | .48 | .40 | .36 | 1.0 | ||||||||||
| 11 | 2.25 | .94 | .25 | .26 | .26 | .28 | .24 | .25 | .09 | .17 | .36 | .11 | 1.0 | |||||||||
| 12 | 2.09 | .87 | .28 | .27 | .27 | .25 | .27 | .22 | .05 | .21 | .44 | .12 | .51 | 1.0 | ||||||||
| 13 | 2.24 | .95 | .24 | .23 | .23 | .21 | .23 | .19 | .02 | .18 | .39 | .09 | .51 | .62 | 1.0 | |||||||
| 14 | 2.72 | .98 | .21 | .23 | .19 | .18 | .15 | .17 | .06 | .20 | .29 | .13 | .47 | .43 | .48 | 1.0 | ||||||
| 15 | 2.10 | .99 | .24 | .25 | .31 | .24 | .25 | .25 | .12 | .18 | .34 | .18 | .34 | .32 | .29 | .19 | 1.0 | |||||
| 16 | 2.57 | .96 | .18 | .24 | .24 | .24 | .25 | .21 | .09 | .18 | .28 | .16 | .27 | .25 | .24 | .15 | .44 | 1.0 | ||||
| 17 | 2.41 | .96 | .16 | .20 | .25 | .23 | .23 | .21 | .06 | .16 | .23 | .12 | .27 | .27 | .25 | .14 | .44 | .60 | 1.0 | |||
| 18 | 2.38 | 1.05 | .20 | .18 | .23 | .18 | .19 | .20 | .09 | .16 | .27 | .12 | .31 | .29 | .27 | .13 | .57 | .37 | .43 | 1.0 | ||
| 19 | 2.42 | 1.05 | .17 | .18 | .23 | .17 | .22 | .17 | .07 | .11 | .28 | .14 | .29 | .30 | .27 | .15 | .55 | .36 | .39 | .59 | 1.0 | |
| 20 | 2.50 | 1.09 | .23 | .23 | .21 | .19 | .19 | .24 | .12 | .14 | .23 | .21 | .23 | .27 | .27 | .20 | .39 | .33 | .31 | .44 | .33 | 1.0 |
Criteria for evaluating the models
To evaluate the overall fit of the models to the data, we considered four fit indices. First, the Goodness of Fit Index (GFI) produces values ranging from 0 to 1 with values in excess of .90 indicating good fit. Second, the Comparative Fit Index (CFI) produces values ranging from 0 to 1 with values larger than .90 indicating good fit. Third, Browne and Cudeck (1993) contend that values of the Root Mean Square Error of Approximation (RMSEA) of .08 or lower indicate reasonable fit, though values of .06 or below should be preferred. Fourth, the Bayesian Information Criterion (BIC) is constructed such that negative values provide evidence of model fit, while positive BIC values suggest problematic model fit. Differences in BIC of 2 are thought to provide some evidence favoring one model over another; 6 or more, strong evidence; and 10 or more, very strong evidence for the superiority of one model over another (Raftery, 1995).
Results
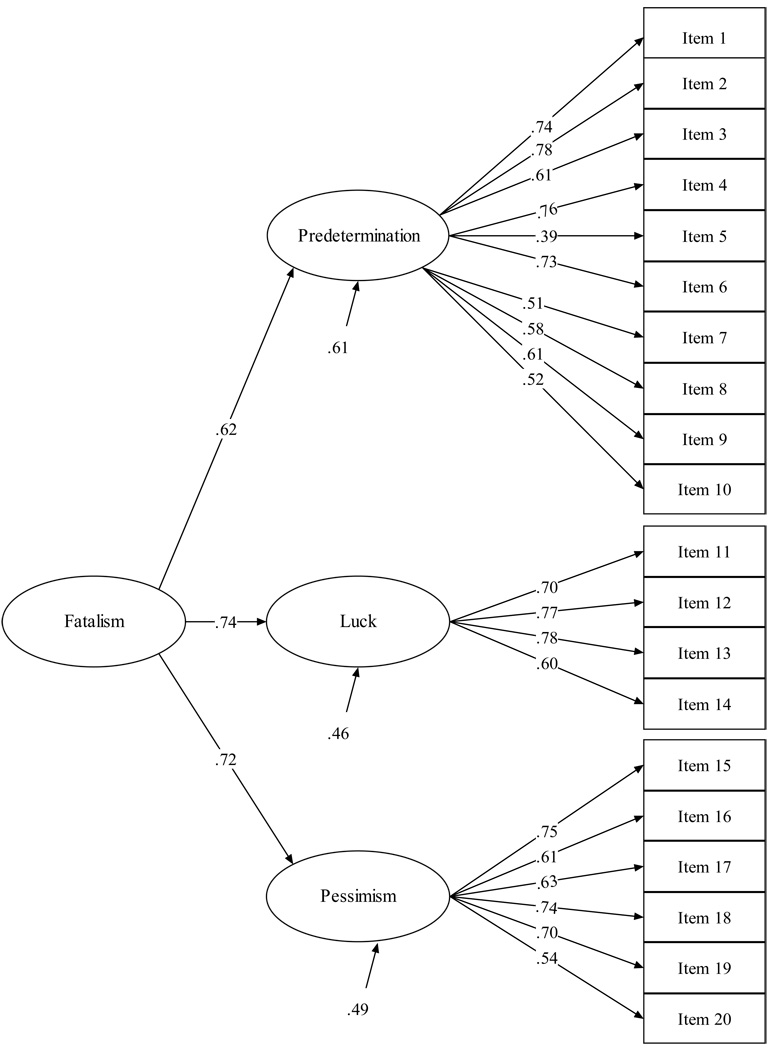
Table 3 presents the fit indices of the two factor models. Figure 1 gives the standardized path coefficients for the second order single-factor model. The model fit indices suggested that the first order three-factor model was a good fit to the data: d.f.=218, χ2=1064.68, RMSEA=.06, GFI=.92, CFI=.96, and BIC=−470.73.2 Additional evidence came from the standardized factor loadings: The three factors had similar and reasonably high loadings on the indicators, and the substantive correlations among the three factors. For predetermination, the loadings were all above .50 except for Item 5 (loading=.39). For luck, the loadings ranged from .60 to .78. And for pessimism, the loadings ranged from .54 to .75. The correlations among the three factors ran from .44 to .53, thereby providing clear indication of non-orthogonality.
Table 3.
Fit Indices and Model Comparisons of the Fatalism Scale (N=1145)
| Model | χ2 | d.f. | RMSEAa | CFIb | GFIc | BICd | BIC Difference |
|---|---|---|---|---|---|---|---|
| 1st order Oblique 3-Factor Oblique |
1064.68 | 218 | .06 | .96 | .92 | −470.73 | |
| 2nd Order Single- Factor Model |
1084.95 | 224 | .06 | .96 | .91 | −492.72 | 21.99 |
Root Mean Squared Error Approximation.
Comparative Fit Index.
Goodness of Fit Index.
Bayesian Information Criterion =χ2 - ln(N) × d.f., where χ2 is the Minimum Function Chi-square, N is the sample size, and d.f. is the degree of freedom of the model.
Figure 1.
Standardized Parameter Estimates of the Second Order Single-Factor Model
The second order single-factor model is nested in the oblique first order three-factor model. We used two sets of indices to evaluate the second order model: (a) RMSEA, GFI, CFI, and BIC, and (b) the BIC difference between the oblique three-factor model and the second order single-factor model. The absolute indices showed that the second order model (with the instrumental variables3) was also a good fit: d.f.=224, χ2 =1084.95, RMSEA=.06, GFI=.91, CFI=.96, and BIC= −492.72. The values for RMSEA, GFI, and CFI were the same for the second order single-factor model as the first order three-factor model. More importantly, the BIC difference was 21.99 and in favor of the second order unidimensional model. Together, these values indicated that the second order model provided a plausible account of the data. The factor loadings of the three first order factors on the second order factor provided additional evidence: The factor loadings ranged from .62 to .74. These results provided evidence that the second order single-factor model is adequate for the fatalism scale, and can be considered as statistically equivalent to the first order three-factor model.
Scale Reliability
Among the three first order factors, the alpha reliabilities was .86 for predetermination, .80 for luck, and .82 for pessimism. The reliability for the whole scale was .88. Alpha if item deleted fell around .88 for each of the 20 items. These results provided evidence that the 20-items fatalism scale was reliable.
Construct Validity
Three external variables, one potential cause (i.e., genetic determinism) and two possible outcomes (i.e., perceived benefits of lifestyle change and intention to engage in healthy behavior) of fatalism, were used to investigated the construct validity of the scale. Table 4 presents the associations between the first order factors and the external variables and that between the second order factor and the external variables. These correlations demonstrated some evidence for the construct validity of the fatalism scale.
Table 4.
Scale Reliabilities and Correlations between the Fatalism Factors and External Variables
| Factor | Genetic Determinism |
Perceived benefits |
Behavioral Intention |
2nd Order Factor |
Predetermination | Luck | Pessimism |
|---|---|---|---|---|---|---|---|
| 2nd Order Factor | .22*** | −.19*** | .22*** | .88a | |||
| Predetermination | .18*** | −.13** | .13*** | .87*** | .86a | ||
| Luck | .19*** | −.15** | .08*** | .74*** | .46*** | .80a | |
| Pessimism | .17*** | −.12** | .23*** | .72*** | .44*** | .53*** | .82a |
Note:
Alpha reliabilities
p<.05,
p<.01,
p<.001
Genetic determinism
A positive correlation was predicted between genetic determinism and fatalism. The correlations between genetic determinism and the first order factors were positive and significant at p<.001: .18 for predetermination, .19 for luck, and .17 for pessimism. The magnitude of the correlation between the second order factor and genetic determinism (.22, p<.001) was the biggest. The differences among the four correlation coefficients were not statistically significant, demonstrating the scale’s external consistency.
Perceived benefits of lifestyle change
A negative association was expected between perceived benefits of lifestyle change and fatalism. Perceived benefits was negatively correlated with the three first order factors (p<.01) as well as the second order factor (p<.001):−.13 for predetermination, −15 for luck, and−.12 for pessimism. The magnitude of the association between perceived benefits and the second order factor (−.19) was larger than that between any first order factor and perceived benefits. These results also provide evidence for the scale’s external consistency.
Intention to engage in healthy behaviors
The correlation between intention to engage in healthy behaviors and fatalism factors was predicted to be negative. This hypothesis did not receive support. Behavioral intention was positively associated with the first order factors as well as the second order factor (p<.001): .13 for predetermination, .08 for luck, .23 for pessimism and .22 for the second order factor. However, the correlations between this external variable and the fatalism factors exhibited a parallel pattern—they are similar to each other except for luck. We consider that as evidence for the scale’s construct validity as well, albeit weaker (because the direction of the correlations was complete opposite to what we predicted).
Demographics and Fatalism
It is believed that fatalism might be a function of demographic variables, especially education and income such that low-income and low-education individuals are more fatalistic than those with higher income and better education (Powe, 2001; Mayo et al., 2001). It is also believed that certain ethnic groups such as Latinos and African Americans are more likely to be fatalistic (Powe, 1996; Niederdeppe & Levy, 2007). To explore the association between fatalism and demographic variables, a generalized linear model was estimated, with fatalism as the criterion, age, education and income as covariates, and gender, race, and geographic region as fixed factors. Pairwise comparisons were conducted via the Bonferroni method. Assuming α =.05(two-tailed), with N=1145, and six independent variables, the statistical power to detect an effect size equivalent to r=.10 exceeded .89. The data was weighted to reflect national demographic characteristics.
There was no main effect of gender or geographic region. Education (β =−.06, p<.001) and income (β =−.03, p<.001) negatively predict fatalism. There was a main effect of ethnicity: F (4, 1124) = 4.84, p<.001, η2=.02. Those who categorized themselves as “Non-Hispanic Other” reported significantly higher scores in fatalism (M=2.91, SD=.08) than the other four groups, namely, non-Hispanic White (M=2.58, SD=.02), non-Hispanic Black (M=2.51, SD=.06), Hispanic (M=2.51, SD=.07), and non-Hispanic more than two races (M=2.52, SD=.11), whose scores were not significantly different from each other.
There was a significant interaction between gender and geographic region: F (3, 1124) = 2.15, p<.001, η2=.02. For males, individuals living in the south were by far the most fatalistic (M=2.81, SD=.06), and those living in the Midwest were the least fatalistic (M=2.38, SD=.10). For females, those live in the South were the least fatalistic (M=2.47, SD=.06) while women in the other three regions ranged between 2.63 to 2.69. These effects were qualified by a gender × ethnicity × region three-way interaction: F (10, 1124) = 4.84, p<.001, η2=.04. Non-Hispanic other females from the Midwest were the most fatalistic (M=3.89, SD=.30), followed by non-Hispanic other male from the South (M=3.44, SD=.20). Non-Hispanic two-race females from the South were the least fatalistic (M=2.08, SD=.20).
Discussion
Psychometric Properties of the Fatalism Scale
According to Hunter and Gerbing (1982), assessment of measurement instruments should be based on content validity, internal consistency and external consistency. With items adapted from existing scales and new items added, we believe the new fatalism scale not only exhibits good semantic correspondence with the fatalism construct, but also constitute a reasonable sampling of that conceptual domain.
The primary method for examining relationships among the items has been factor analysis. Confirmatory factor analyses led us to the conclusion that a second order single-factor model provides a good fit to the 20 fatalism items. This conclusion was based on a number of criteria. First, the correlations among the first order factors were all positive and substantial, ranging from .44 to .53. Second, such absolute fit indices as RMSEA, GFI, and CFI for the three-factor first order model and the second order model were almost identical to each other. Third, the BIC difference was larger than 10 and in favor of the second order model. Fourth, the reliability of the second order factor was better than that of any of the first order factors. Finally, the three first order factors exhibited reasonable consistency in their relationships with external variables. This parallelism was notable with respect to the variables that are potential cause and consequences of fatalistic beliefs—genetic determinism, perceived benefits of lifestyle change, and intention to engage in healthy behaviors.
Demographics and Fatalism
Among the demographic variables behind fatalism, the driving forces were education and income. Consistent with the literature, lower education and lower income are associated with higher degrees of fatalism. It was believed that certain ethnic groups are more fatalistic than others. Our data showed that above and beyond the effects of income and education, Hispanics and African Americans are not among the most fatalistic ethnic groups. Individuals from different geographic regions of the United States also did not differ in fatalism. This suggests that income and education, rather than race or ethnicity, should be used as the basis for interventions aimed at reducing fatalism and enhancing behavioral changes.
Genetic Determinism and Fatalism
With the mapping and sequencing of the human genome now complete, it is sensible to expect that the practice of public health is likely to become “geneticized” such that information about genetic risks is widely available. This dramatic increase in information regarding genetically-induced illness brings with it numerous social, psychological, and ethical challenges (Visser & Bleiker, 1997). There have been concerns that communication of genetic information could lead to fatalism among lay individuals, which might be an obstacle to healthy lifestyle change (Alper & Beckwith, 1993; Emery, 2001; Senior et al., 1998). Our findings showed that genetic determinism was indeed positively correlated with fatalism; however, the association between the two (r=.22) was less than moderate according to Cohen’s (1992) criteria (i.e., .10=small, .30=moderate, and .50=large). Such an association between genetic determinism and fatalism should not constitute strong warrant against communication of genetic information to lay individuals.
Fatalism and Behavioral Intention
Both the conceptualization of construct and empirical evidence (Niederdeppe & Levy, 2007; Straughton & Seow, 1998, see also Powe & Finnie, 2003 for a review) indicate that fatalism can function as a barrier to cancer prevention and screening behaviors. The relationship between behavioral intention and fatalism and its dimensions exhibited a parallel pattern. However, they positively predicted individuals’ intention to engage in healthy behaviors such as eating fruit and vegetables, brisk exercise, maintaining a healthy weight and making healthy choices everyday. The method employed in this study suggested that sampling error was an unlikely cause of this positive association. And the fact that the effects of genetic determinism and perceived benefits of lifestyle change, and that of demographic variables were partialled out indicated that this positive association was probably not spurious. There are several plausible explanations for this apparent inconsistency.
The first explanation lies in a possible disconnection between actual behavior and behavioral intention. Ajzen and Fishbein (1980) suggest that the association between intention and behavior is determined by the degree of correspondence in the measurement of the two constructs, specifically, the target, action, context, and time (see also Kim & Hunter, 1993). First, our measure of behavioral intention lacked specific contexts. Behavioral intention with a particular situation is called implementation intention and is more predictive of future behavior (Warshaw & Davis, 1985). Fatalistic individuals might have a higher intention to engage in such healthy behaviors without specific situations, but less likely to act upon their intention when they anticipate negative outcomes. Second, temporal stability is one property of behavioral intention (Sheeran, 2002). The theory of reasoned action (Ajzen & Fishbein, 1980) suggests that one’s intention can fluctuate over time and does not necessarily provide accurate predictions of behavior. Our measure of intention refers to long-term and repeated commitments, while behavior measures in the literature (Niederdeppe & Levy, 2007; Powe & Finnie, 2003; Straughton & Seow, 1998) tend to be short-term and require one-time commitment only. Therefore, the measurement correspondence between intention and behavior was rather low, which might have been the cause of the inconsistent findings.
The second explanation takes the perspective of efficacy. Response-efficacy refers to the effectiveness of a behavior in preventing/reducing certain health risks. Self-efficacy can be defined as individuals’ perceived ability to enact behaviors that might prevent/reduce health risks (Bandura, 1982; Rogers, 1983). The health belief model contends that enactment of health behaviors requires both response- and self-efficacy (Janz & Becker, 1984). Fatalistic individuals tend to be low in both: The dimension of pessimism suggests low response-efficacy and the notions of lack of control and predetermination indicate low self-efficacy. It is plausible that individuals are well aware of the right course of action and indeed intend to follow the various recommendations; however, their fatalistic beliefs lead to low levels of perceived response-efficacy, as reflected in the negative association between fatalism and perceived benefits of lifestyle change; and hence lack of behavior. In other words, low response-efficacy might be the main cause of inaction.
The third explanation originates from the optimistic bias (Weinstein, 1982) and egocentric thinking. Unrealistic optimism and egocentrism might lead to overestimates in likelihood of positive things and underestimate in likelihood of negative events happening to oneself, while the pattern would be reserved for others: Positive things are less likely, and negative things are more likely to happen. It is possible that individuals’ fatalistic beliefs might concern others more than oneself—they underestimate other people’s control over and luck with one’s health, but overestimate their own control over and luck with health and life events. The referents in the measures in the current study suggested that this might be a possibility: The fatalism items concerned both unspecific members of the general public (i.e., “someone”) as well as oneself. The measure of perceived benefits of lifestyle change focused on an unspecific other; and the benefit-fatalism relation was as predicted. The measure of behavioral intention referred to oneself, and the intention-fatalism association was inconsistent with our prediction.
Limitations & Directions for Future Research
Despite the random sampling and considerable sample size, one obvious limitation of this study is that the sample was drawn from United States residents. It is questionable if the scale can be applied to populations outside of the U.S. Second, the fact that the scale items are in English might cause some concerns because English might not be the native language of participants who were Asian or Hispanic, which could be a threat to the validity of the scale. The scale would receive stronger support from future research that tests the scale in different populations and in participants’ native languages. Third, the positive association between fatalism and intention for healthy behaviors was the exact opposite to our prediction. However, it would be premature to consider our results as challenging the empirical findings regarding negative association between fatalism and health behaviors, or as refuting the conclusion that fatalism might function as a potential inhibitor of healthy lifestyle/changes. Our data do suggest, however, there might be more nuances in the construct of fatalism (i.e., fatalism about self vs. others, fatalism in general vs. fatalism regarding a specific disease/health condition), which could have important implications for health interventions. Future research on fatalism and its psychological correlates should further our understanding on this issue.
Conclusion and Summary
We proposed that fatalism is cognitive in nature and conceptualized the construct as a set of health beliefs that consist of three dimensions: predetermination, luck and pessimism. A 20-item scale for fatalism was developed and validated with web-based national survey data. We analyzed the structure of the 20 items via confirmatory factor analyses, the reliabilities of the first order and second order factors and the relationship of these factors with external variables. The results led us to the conclusion that the scale can be treated as a valid and reliable measurement instrument for fatalism.
Acknowledgments
This research is supported by NIH grant # HG003961-01 to Celeste Condit and CDC Center of Excellence Grant # 1P01CD000242-01 to Vicki Freimuth. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIH or the Southern Center for Communication, Health and Poverty. The authors offer their thanks to Dr. Barbara Powe for generously sharing her cancer fatalism instrument with us and to the other research team members who participated in development of instrument items, including Youyou Cheng, David Cisneros, Samantha Barrientos, Dr. Tina Harris, Marita Gronnvoll and Jamie Landau
Footnotes
The two items for fear are: Item 8, “I think getting checked for bowel cancer makes people scared that they may really have bowel cancer” and Item 10, “I think some people don't want to know if they have bowel cancer because they don't want to know they may be dying from it.”
The model fit indices of the first order three-factor model without the instrumental variable were also very similar: d.f.=167, χ2=1062.44, RMSEA=.07, CFA=.84, GFI=.68, BIC=−113.77.
The model fit indices of the second order single-factor model without the instrumental variable were exactly the same as those of the first order oblique three-factor model because a factor model with three indicators is just-identified.
References
- Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- Alper JS, Beckwith J. Genetic fatalism and social policy: The implications of behavior genetics research. The Yale Journal of Biology and Medicine. 1993;66:511–524. [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy mechanism in human agency. American Psychologist. 1982;37:122–147. [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Chavez LR, Hubbell FA, Mishra SI, Valdez RB. The influence of fatalism on self-reported use of Papanicolaou smears. American Journal of Preventive Medicine. 1997;13:418–424. [PubMed] [Google Scholar]
- Cohen D, Nisbett R. Are there differences in fatalism between rural Southerners and Midwesterners? Journal of Applied Social Psychology. 1998;28:2181–2195. [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:1550159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Davison C, Frankel S, Smith G. The limits of lifestyle: Re-assessing `fatalism' in the popular culture of illness prevention. Social Science & Medicine. 1992;34:675–685. doi: 10.1016/0277-9536(92)90195-v. [DOI] [PubMed] [Google Scholar]
- DeVellis RF. Scale development: Theory and applications. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Egede LE, Bonadonna RJ. Diabetes self-management in African Americans: An exploration of the role of fatalism. Diabetes Educator. 2003;29:105–115. doi: 10.1177/014572170302900115. [DOI] [PubMed] [Google Scholar]
- Emery J. Is informed choice in genetic testing a different breed of information decision-making? A discussion paper. Health Expectations. 2001;4:81–86. doi: 10.1046/j.1369-6513.2001.00124.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter JE, Gerbing DW. Unidimensional measurement, second order factor analysis, and causal models. In: Staw BM, Cummings LL, editors. Research in organizational behavior. vol. 4. Greenwich, CT: JAI Press; 1982. [Google Scholar]
- Janz N, Becker M. The health belief model: A decade later. Health Education and Behavior. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Kalichman S, Kelly J, Morgan M, Rompa D. Fatalism, current life satisfaction, and risk for HIV infection among gay and bisexual men. Journal of Consulting and Clinical Psychology. 1997;65:542–546. [PubMed] [Google Scholar]
- Kim MS, Hunter JE. Relationships among attitudes, behavioral intentions, and behavior: A meta-analysis of past research, Part 2. Communication Research. 1993;20:331–364. [Google Scholar]
- Lazarus RS. The cognition-emotion debate: A bit of history. In: Dalgleish T, Power M, editors. Handbook of cognition and emotion. Chichester: Wiley; 1999. pp. 3–19. [Google Scholar]
- Loehlin JC. Latent variable models: An introduction to factor, path, and structural analysis. Mahwah, NJ: Lawrence Erlbaum Associates; 1998. [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modelling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- Mayo R, Ureda J, Parker V. Importance of fatalism in understanding mammography screening in rural elderly women. Journal of Women & Aging. 2001;13:57–72. doi: 10.1300/J074v13n01_05. [DOI] [PubMed] [Google Scholar]
- Mechanic D. Disadvantage, inequality, and social policy: Major initiatives intended to improve population health may also increase health disparities. Health Affairs. 2002;21:48–59. doi: 10.1377/hlthaff.21.2.48. [DOI] [PubMed] [Google Scholar]
- Neff JA, Hoppe SK. Race/ethnicity, acculturation, and psychological distress: Fatalism and religiosity as cultural resources. Journal of Community Psychology. 1993;21(1):3–20. [Google Scholar]
- Niederdeppe J, Levy AG. Fatalistic beliefs about cancer prevention and three preventive behaviors. Cancer Epidemiology Biomarkers and Prevention. 2007;16:998–1003. doi: 10.1158/1055-9965.EPI-06-0608. [DOI] [PubMed] [Google Scholar]
- Parrott R, Silk K, Weiner J, Condit C, Harris T, Bernhardt J. Deriving lay models of uncertainty about genes’ role in illness causation to guide communication about human genetics. Journal of Communication. 2004;54:105–122. [Google Scholar]
- Peters T. Playing God? Genetic determinism and human freedom. New York: Routledge; 2002. [Google Scholar]
- Phelps EA. Emotion and cognition: Insights fromStudies of the Human Amygdala. Annual Review of Psychology. 2006;57:27–53. doi: 10.1146/annurev.psych.56.091103.070234. [DOI] [PubMed] [Google Scholar]
- Powe BD. Fatalism among elderly African Americans: Effects on colorectal screening. Cancer Nursing. 1995;18:385–392. [PubMed] [Google Scholar]
- Powe BD. Cancer fatalism: Spiritual perspectives. Journal of Religion and Health. 1997;36:135–144. [Google Scholar]
- Powe BD. Cancer fatalism among elderly African American women: Predictors of the intensity of the perceptions. Journal of Psychosocial Oncology. 2001;19:85–96. [Google Scholar]
- Powe BD, Finnie R. Cancer fatalism: The state of the science. Cancer Nursing. 2003;26:454–465. doi: 10.1097/00002820-200312000-00005. [DOI] [PubMed] [Google Scholar]
- Powe BD, Johnson A. Fatalism as a barrier to cancer screening among African-Americans: Philosophical perspectives. Journal of Religion and Health. 1995;34(2):119–126. doi: 10.1007/BF02248767. [DOI] [PubMed] [Google Scholar]
- Powe BD, Weinrich S. An intervention to decrease cancer fatalism among rural elders. Oncology Nursing Forum. 1999;26:583–588. [PubMed] [Google Scholar]
- Powe BD, Daniels EC, Finnie R. Comparing perceptions of cancer fatalism among African American patients. Journal of the American Academy of Nurse Practitioners. 2005;17:318–324. doi: 10.1111/j.1745-7599.2005.0049.x. [DOI] [PubMed] [Google Scholar]
- Raftery AE. Bayesian model selection in social research. In: Marsden PV, editor. Sociological methodology. Cambridge: Basil Blackwell; 1995. pp. 111–163. [Google Scholar]
- Roberts RE, Roberts CR, Chen RY. Suicidal thinking among adolescents with a history of attempted suicide. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:1294–1300. doi: 10.1097/00004583-199812000-00013. [DOI] [PubMed] [Google Scholar]
- Rogers RW. Cognitive and physiological processes in fear appeals and attitude change: A revised theory of protection motivation. In: Cacioppo JT, Petty RE, editors. Social psychophysiology: A source book. New York: The Guilford Press; 1983. pp. 153–176. [Google Scholar]
- Rundmo T, Hale AR. Manager's attitudes towards safety and accident prevention. Safety Science. 2003;41:557–574. [Google Scholar]
- Scheier M, Bridges M. Person variables and health: Personality predispositions and acute psychological states as shared determinants for disease. Psychosomatic Medicine. 1995;57:255–268. doi: 10.1097/00006842-199505000-00007. [DOI] [PubMed] [Google Scholar]
- Schnoll RA, Malstrom M, James C, Rothman R, Miller S, Ridge J, Movsas B, Unger M, Langer C, Goldberg M. Correlates of tobacco use among smokers and recent quitters diagnosed with cancer. Patient Education and Counseling. 2000;2:137–145. doi: 10.1016/s0738-3991(01)00157-4. [DOI] [PubMed] [Google Scholar]
- Senior V, Marteau T, Peters TJ. Will genetic testing for predisposition for disease result in fatalism? A qualitative study of parents’ responses to neonatal screening for familial hypercholesterolaemia. Social Science & Medicine. 1998;48:1857–1860. doi: 10.1016/s0277-9536(99)00099-4. [DOI] [PubMed] [Google Scholar]
- Sheeran P. Intention-behavior relations: A conceptual and empirical review. European Review of Social Psychology. 2002;12:1–36. [Google Scholar]
- Sowell RL, Seals BF, Moneyham L, Demi A, Cohen L, Brake S. Quality of life in HIV-infected women in the south-eastern United States. AIDS Care. 1997;9:501–512. doi: 10.1080/713613191. [DOI] [PubMed] [Google Scholar]
- Straughan PT, Seow A. Fatalism reconceptualized: A concept to predict health screening behavior. Journal of Gender, Culture, and Health. 1998;3:85–100. [Google Scholar]
- Unger JB, Ritt-Olson A, Teran L, Huang T, Hoffman BR, Palmer P. Cultural values and substance use in a multiethnic sample of California adolescents. Addiction Research and Theory. 2002;10(3):257–280. [Google Scholar]
- Urizar G, Sears S. Psychosocial and cultural influences on cardiovascular health and quality of life among Hispanic cardiac patients in south Florida. Journal of Behavioral Medicine. 2006;29:255–268. doi: 10.1007/s10865-006-9050-y. [DOI] [PubMed] [Google Scholar]
- Varga CA. Coping with HIV/AIDS in Durban's commercial sex industry. AIDS Care. 2001;13:351–365. doi: 10.1080/09540120120044008. [DOI] [PubMed] [Google Scholar]
- Visser A, Bleiker E. Introduction: Genetic education and counseling. Patient Education and Counseling. 1997;32:1–7. doi: 10.1016/s0738-3991(97)00069-4. [DOI] [PubMed] [Google Scholar]
- Warshaw PR, Davis FD. Disentangling behavioral intention and behavioral expectation. Journal of Experimental Social Psychology. 1985;21:213–218. [Google Scholar]
- Weinstein ND. Unrealistic optimism about susceptibility to health problems. Journal of Behavioral Medicine. 1982;5:441–460. doi: 10.1007/BF00845372. [DOI] [PubMed] [Google Scholar]
- Yeh CJ, Inman AC, Kin AB, Okubo Y. Asian American Families' ollectivistic Coping Strategies in Response to 9/11. Cultural Diversity & Ethnic Minority Psychology. 2006;12:134–148. doi: 10.1037/1099-9809.12.1.134. [DOI] [PubMed] [Google Scholar]