Abstract
In this study, we examined if children's food selection met the School Meals Initiative (SMI) standards and the recently released Institute of Medicine (IOM) recommendations. Mean food selection, plate waste, and food intake were also examined. Food intake of 2049 4th–6th grade students was measured objectively at lunch over 3 d with digital photography in 33 schools. The percent of children whose food selection met the SMI standards and IOM recommendations for energy (kJ), fat and saturated fat, calcium, iron, and vitamin A and C were calculated. The SMI standards provide lower limits for most nutrients; the IOM provides a range of values, including an upper limit for energy. Seventy-seven percent of children's energy selection met the SMI lower limit, but only 16% of children met the IOM's recommended range and 74% of children exceeded the upper limit. More than 70% of children exceeded the SMI and IOM's saturated fat recommendations. Children selected (mean ± SD) 3168 ± 621 kJ, discarded 882 ± 581 kJ, and consumed 2286 ± 716 kJ. Children were less likely to discard fat than carbohydrate, resulting in proportionally more fat being consumed. Most children met SMI and IOM recommendations for protein, calcium, iron, and vitamin A. With few exceptions, energy selection was similar among groups of children, but plate waste differed (P < 0.001), resulting in greater energy intake among boys compared with girls, Caucasians compared with African Americans, and heavier compared with lighter children. Children's selection was high in saturated fat and, based on IOM criteria, included excess energy.
Introduction
The prevalence of overweight and obesity among children has increased in the US (1), with ∼32% of children and adolescents classified as overweight or obese (2, 3). Among subgroups of children of low socioeconomic status or who live in rural locations, the prevalence of overweight and obesity appears higher. For example, our group found that 45% of children living in rural Louisiana were overweight or obese (4).
Obesity prevention efforts will likely be most effective if young children are targeted (5, 6), and the Institute of Medicine (IOM)8 notes the influential role of the school environment on food intake and exercise behaviors (7). Children spend ∼180 d/y in school and most receive breakfast and/or lunch from school cafeterias. The National School Lunch Program (NSLP), part of the USDA Food and Nutrition Service, is the nation's second largest food and nutrition assistance program. In 2007, it operated in over 95,000 schools (grades K–12) and provided reduced-cost or free lunches to over 30 million children/d (8). In 1995, the USDA issued the final School Meals Initiative (SMI) for Healthy Children regulations (9), which requires that meals under the NSLP meet the Dietary Guidelines for Americans. The SMI regulations apply to foods offered to students and lower limits of energy, protein, calcium, iron, and vitamins A and C were established without maximum upper limits being recommended (upper limits were established for fat and saturated fat). Recent recommendations by the IOM, however, apply to the foods actually selected by students and lower and upper limits are recommended for energy as well as percent of energy from total fat (10). Despite the presence of these regulations and recommendations, it is difficult to quantify adherence, because few methods can be used to accurately and unobtrusively measure food selection and food intake in school cafeterias.
The purpose of the study reported herein was to examine if food selection, measured objectively in school cafeterias, met the SMI standards and IOM recommendations in 33 elementary schools in Louisiana. Mean food selection, plate waste, and food intake, as well as the percent of selected foods actually consumed by children, were also examined. Based on previous research (11, 12), we hypothesized that most children's food selection would meet energy, protein, and vitamin and mineral standards, with a minority meeting the fat and saturated fat standards. The effects of grade level, sex, race, and weight status on the probability of meeting the SMI standards was investigated and compliance with the IOM recommendations was examined by age group. To our knowledge, this is the first study examining compliance with the SMI standards and IOM recommendations when food selection was measured objectively in school cafeterias and the first to determine whether different groups of children are more likely to meet these standards and recommendations.
Methods
Ethics
The study was approved by the Pennington Biomedical Research Center's Institutional Review Board and a Data and Safety Monitoring Board. Participants’ parents provided written informed consent and children provided written assent. The study was performed following guidelines for the ethical treatment of humans.
Participants
Participants were 4th–6th grade students enrolled in the Louisiana Health (LA Health) study, a cluster randomized research study testing the efficacy of strategies to prevent inappropriate weight gain (13). Twenty-three school clusters were invited to participate and 17 enrolled, resulting in enrollment of children from 33 public schools in small towns and rural (14) areas of Louisiana (no children were enrolled from large cities). All schools were in school districts encompassing large geographic areas. Data for this paper were collected from September 2006 to December 2006 during the baseline assessment for the LA Health study. Supplemental Figure 1 includes a CONSORT diagram outlining recruitment of participants for the current analysis, which included baseline data from the LA Health study.
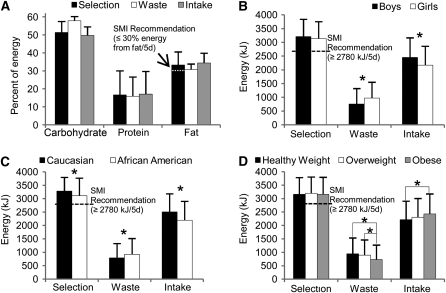
FIGURE 1.
Percentages of energy selected, discarded, and consumed by children in school cafeterias from carbohydrate, protein, and fat (A), and the amounts of energy selected, discarded, and consumed by sex (B), race (C), and BMI percentile category (D). Bars represent means ± SD, n = 1998–2049. *Means differed, P < 0.001.
Measures
BMI percentile.
Height was measured using a stadiometer and weight was measured using a Tanita (model TBF-310) scale that uploaded data directly into a computer. These measurements were collected at school. Height and weight were converted to BMI (kg/m2), which was converted to percentile scores based on sex and age using norms from the CDC (15). Classification of BMI percentile followed the American Academy of Pediatrics (16) criteria for childhood underweight (<5th BMI percentile), overweight (≥85th and <95th percentile), and obese (≥95th percentile).
Digital photography of foods.
The digital photography of foods method (17, 18) was used to objectively measure the food selection (the food actually taken by students during lunch), plate waste (the food discarded and not consumed by students), and food intake (the food actually consumed during lunch) of participants in school cafeterias. At lunch, foods selected by the students prior to eating were photographed with digital video cameras. Plate waste was photographed with a second camera after children ate and returned their trays. Study personnel also captured photographs of weighed standard reference portions of the foods served. Each food was identified and linked to the USDA nutrient database (19) or a custom recipe.
Food intake was estimated at a later date in the laboratory using a computer application that simultaneously displayed photographs of a child's food selection and plate waste as well as the reference portion. Registered dietitians estimated the percent of the reference portion of food selection and plate waste and entered these estimates into the application, which quantified the amount (grams and energy) and macro- and micronutrient information of food selection, plate waste, and food intake. The digital photography method has been found to be highly reliable and accurate when used to measure the food intake of adults (17, 18) and children (20, 21).
Food intake was measured at lunch between 1045 and 1245 over 3 consecutive days (lunch lasted 30–40 min and 2 grades were typically served lunch at the same time). Food was prepared onsite at all schools and a minority of schools had morning recess that lasted 10 min. Food service workers are expected to serve standard portion sizes, although there was considerable variability in the size of the portions served to the children and the children were allowed to select from a number of foods that differed in macronutrient composition and energy density. If participants selected second servings, their food selection and plate waste from second servings also was quantified with the digital photography method.
Data analytic plan
All statistical analyses were performed using SAS software, version 9.1 or 9.2 (SAS Institute). Mean food selection and intake over the 3 d of measurement were analyzed. A pilot study that used identical methods found that 3 d of measurement provided a reliable and representative estimate of food selection and intake (20, 21); therefore, data presented in this paper can be interpreted as representative of 5 d of data collection. Descriptive characteristics of the study sample are expressed as mean ± SD.
Three series of analyses were conducted. First, a mixed model logistic regression was used to determine whether the likelihood of meeting the SMI standards differed by grade level, sex, race, and weight status when adjusting for a random effect for individual school. Multiple odds ratio comparisons were performed using Tukey-Kramer adjustments. Results were considered significant at the 0.05 level and presented as the percent of students whose food selection met the SMI standards.
Second, the percent of children meeting the recently released IOM recommendations (10) was quantified. Differences in the percent of children meeting the recommendations by age group were examined using χ2 analysis, with the significance level set at 0.01 due to multiple comparisons.
Third, separate ANOVA models determined if food selection, plate waste, and food intake differed by grade level, sex, race, and weight status after adjusting for random school effects. These analyses included the 8 components of the SMI standards and the percent of energy from carbohydrate and protein. The results from the ANOVA were presented as mean ± SD and α was set at 0.001 due to multiple comparisons. Finally, the percent of selected food that was actually consumed was quantified and differences among groups of children were examined using ANOVA and t tests with the significance level set at 0.001 (these results are expressed as mean ± SD). Similarly, the mean percent of selected food that was discarded was compared across food categories. The food categories were defined using the food pyramid approach, which is based on the Dietary Guidelines (22), and included discretionary fat, total grains, dairy, added sugar, and total fruits and vegetables. Differences among food categories of the percent of food discarded and eaten were examined with ANOVA that included school as a random effect and an α level set at 0.005 based on Bonferroni correction. This 3rd series of analyses determined if children selectively consumed certain macronutrients while discarding others.
Results
Characteristics of the study sample
The age of the sample (n = 2049) was 10.5 ± 1.2 y, the BMI percentile was 69.5 ± 29.6, and body weight was 46.8 ± 16.5 kg. The sample was 58% female, 68% African American (Table 1), and 87% of children received free or reduced-cost lunch. The SMI standards are applied at the school level and the food selection and intake of NSLP participants (children receiving free or reduced lunch) were very similar to children who did not receive free or reduced-cost lunch. Therefore, the analyses included the entire study sample.
TABLE 1.
Characteristics of the study sample1
| Characteristic | n(%) |
| School grade level | |
| 4th | 751 (36.7) |
| 5th | 675 (32.9) |
| 6th | 623 (30.4) |
| Gender | |
| Male | 852 (41.6) |
| Female | 1197 (58.4) |
| Race | |
| Caucasian | 617 (30.1) |
| African American | 1398 (68.2) |
| Other | 34 (1.7) |
| BMI percentile group | |
| Underweight (<5th) | 51 (2.5) |
| Healthy weight (5th to <85th) | 1083 (52.9) |
| Overweight (85th to <95th) | 350 (17.1) |
| Obese (≥95th) | 565 (27.6) |
n = 2049.
Compliance with the SMI standards
Total sample.
All children were in the 4th through 6th grades at the time of testing; therefore, the children's food selection was compared with the SMI standards for children in grades K through 6 (the standards are provided in Table 2). Approximately 77% of children's food selections met the SMI standard for energy and almost all participants met the protein standard. Fewer than 30% of children met fat and saturated fat standards (Table 2), indicating they selected more energy from fat than recommended. More than 85% of children met calcium and iron standards and 53 and 42% of children met vitamin A and C standards, respectively (Table 2).
TABLE 2.
Percent of boys and girls whose food selection at lunch from school cafeterias met the SMI standards
| Food selection1 | Total sample, n = 2049 | Sex |
P2 | Race |
P2 | ||
| Boys, n = 852 | Girls, n = 1197 | Caucasian, n = 617 | African American, n = 1398 | ||||
| % | % | ||||||
| Energy | 76.8 | 78.3 | 75.8 | 0.21 | 87.5 | 72.2 | 0.09 |
| Total Fat | 26.7 | 26.9 | 26.6 | 0.92 | 15.2 | 31.8 | 0.30 |
| Saturated fat | 28.8 | 28.6 | 29.0 | 0.65 | 20.6 | 32.3 | 0.26 |
| Protein | 100.0 | 99.9 | 100.0 | 0.96 | 100.0 | 99.9 | 0.97 |
| Calcium | 86.1 | 89.4 | 83.8 | <0.001 | 92.4 | 83.4 | <0.01 |
| Iron | 93.9 | 94.6 | 93.3 | 0.41 | 98.4 | 91.9 | <0.0001 |
| Vitamin A | 53.3 | 54.7 | 52.3 | 0.70 | 68.4 | 46.6 | <0.001 |
| Vitamin C | 42.3 | 40.5 | 43.6 | 0.35 | 25.8 | 49.7 | 0.02 |
The SMI lunch standards are: energy ≥ 2780 kJ (664 kcal)/5 d, ≤30% energy from fat/5 d, <10% energy from saturated fat/5 d, ≥10 g protein/5 d, ≥286 mg of calcium/5 d, ≥3.5 mg of iron/5 d, ≥224 g of vitamin A/5 d, and ≥15 mg of vitamin C/5 d.
The significance level was set at 0.05 after Tukey-Kramer adjustment.
Sex and race.
Boys’ food selection had greater odds of meeting the calcium SMI standard than girls (Table 2). Due to the small numbers of children whose race was other than Caucasian or African American, comparisons were made only between Caucasian and African American children. Caucasian children had greater odds of meeting SMI standards for calcium, iron, and vitamin A compared with African American children, whereas African American children were more likely than Caucasian children to meet the standard for vitamin C (Table 2).
BMI percentile and grade level.
The odds of meeting SMI standards did not differ by BMI percentile category (Supplemental Table 1). Fourth graders had better odds of meeting the standard for calcium than 5th graders, and 6th graders had worse odds of meeting the vitamin C standard compared with 4th and 5th graders (Supplemental Table 1).
Compliance with IOM recommendations
Total sample.
Only 10% of the sample's energy selection was below the age-specific lower limit, but 74% of children exceeded the upper limit recommended by the IOM (Table 3, which also includes the IOM recommendations). Hence, only 16% of children were within the recommended range of energy selection. There were 58% of children meeting the recommended range for percent of energy from fat and 37% exceeded the upper limit. Over 70% of children exceeded the upper limit for percent of energy from saturated fat (Table 3). Over one-half of the children met or exceeded the target for protein, calcium, iron, and vitamin A, but only 19% of children met or exceeded the target for vitamin C (Table 3).
TABLE 3.
Percent of children whose food selection at lunch from school cafeterias met or failed to meet the recommended targets from the IOM recommendations (10)
| Food selection1 | Total sample | 5–10 y | 11–13 y | P2 |
| n | 2049 | 1055 | 974 | |
| Energy | ||||
| <Lower limit | 10.0 | 8.4 | 10.8 | 0.07 |
| Met recommendation | 16.2 | 14.4 | 18.3 | 0.02 |
| >Upper limit | 73.8 | 77.2 | 70.9 | 0.001 |
| Total fat | ||||
| <Lower limit | 4.8 | 4.6 | 4.8 | 0.85 |
| Met recommendation | 59.0 | 57.9 | 60.6 | 0.22 |
| >Upper limit | 36.2 | 37.4 | 34.6 | 0.18 |
| Saturated fat | ||||
| Met recommendation | 28.8 | 28.0 | 29.9 | 0.34 |
| >Upper limit | 71.2 | 72.0 | 70.1 | |
| Protein | ||||
| <Target | 29.4 | 0.4 | 60.2 | <0.001 |
| ≥Target | 70.6 | 96.6 | 39.8 | |
| Calcium | ||||
| <Target | 37.4 | 18.4 | 57.2 | <0.001 |
| ≥Target | 62.6 | 81.6 | 42.8 | |
| Iron | ||||
| <Target | 29.7 | 6.6 | 53.5 | <0.001 |
| ≥Target | 70.3 | 93.4 | 46.5 | |
| Vitamin A | ||||
| <Target | 42.4 | 34.8 | 50.6 | <0.001 |
| ≥Target | 57.6 | 65.2 | 49.4 | |
| Vitamin C | ||||
| <Target | 81.1 | 78.1 | 84.1 | <0.001 |
| ≥Target | 18.9 | 21.9 | 15.9 | |
Many of the IOM recommendations (10) differ by age group (5–10, 11–13, and 14–18 y). The sample included only 20 children in the 14–18 y old category; therefore, these data are not reported. The IOM recommendations for percent of energy from total fat (25–35% energy/5 d) and saturated fat (<10% energy/5 d) are the same for 5- to 10- and 11- to 13-y-old children. The IOM recommendations for 5- to 10-y-old children are: energy, 2302–2721 kJ/5 d; protein, 15.2 g/5 d; calcium, 332 mg/5 d; iron, 3.4 mg/5 d; vitamin A, 192 g/5 d; and vitamin C, 24 mg/5 d. The IOM recommendations for 11- to 13-y-old children are: energy, 2511–2930 kJ/5 d; protein, 32.2 g/5 d; calcium, 440 mg/5 d; iron, 5.2 mg/5 d; vitamin A, 241 μg/5 d; and vitamin C, 30 mg/5 d. P-values indicate if the proportion of children who failed to meet or met the recommendations differed by age group, P < 0.01.
P-values indicate if the proportion of children who failed to meet or met the recommendations differed by age group, P < 0.01.
Age.
Compared with children who are 11–13 y, a larger proportion of children who are 5–10 y exceeded the upper limit for energy and met or exceeded the protein, calcium, iron, and vitamins A and C targets (Table 3).
Mean food selection, plate waste, and food intake
Total sample.
Children selected 3168 ± 621 kJ (757 ± 148 kcal), discarded 882 ± 581 kJ (211 ± 139 kcal), and consumed 2286 ± 716 kJ (546 ± 171 kcal) (Table 4). Children's mean fat selection and intake were 33.3 and 34.3% of energy, respectively. This indicates that children were less likely to discard fat than carbohydrate, resulting in proportionally more fat in the meals actually being consumed (Table 4; Fig. 1A). The analysis of food categories indicated that children discarded a significantly larger percent of fruits and vegetables compared with all other food categories and a significantly smaller percent of discretionary fat was discarded compared with dairy, added sugar, and total fruits and vegetables (Table 5).
TABLE 4.
Food selection and intake at lunch in school cafeterias for the entire sample and by sex, school grade level, race, and BMI percentile group1
| Total sample | Sex |
School grade level |
Race |
BMI percentile group |
||||||||
| Boys | Girls | 4th | 5th | 6th | Caucasian | African American | Underweight (<5th) | Healthy weight (5th to <85th) | Overweight (85th to <95th) | Obese (≥95th) | ||
| n (%) | 2049 (100) | 852 (41.6) | 1197 (58.4) | 751 (36.7) | 675 (32.9) | 623 (30.4) | 617 (30.1) | 1398 (68.2) | 51 (2.5) | 1083 (52.9) | 350 (17.1) | 565 (27.6) |
| Food selection | ||||||||||||
| Energy, kJ | 3168 ± 621 | 3207 ± 633 | 3139 ± 612 | 3068 ± 554 | 3206 ± 638 | 3246 ± 664 | 3288 ± 510 | 3115 ± 655 | 3251 ± 445 | 3158 ± 626 | 3197 ± 610 | 3161 ± 633 |
| Total fat, % energy | 33.3 ± 4.8 | 33.2 ± 4.8 | 33.4 ± 4.9 | 33.2 ± 4.7 | 33.5 ± 4.6 | 33.4 ± 5.1 | 34.3 ± 4.0 | 32.9 ± 5.1 | 33.2 ± 4.8 | 33.4 ± 4.8 | 33.6 ± 4.8 | 33.1 ± 4.8 |
| Saturated fat, % energy | 11.3 ± 2.3 | 11.3 ± 2.2 | 11.2 ± 2.3 | 11.2 ± 2.3 | 11.2 ± 2.3 | 11.3 ± 2.2 | 11.6 ± 2.0 | 11.1 ± 2.4 | 11.4 ± 2.1 | 11.3 ± 2.3 | 11.3 ± 2.3 | 11.2 ± 2.3 |
| Protein, g | 31.2 ± 7.2 | 31.4 ± 7.1 | 31.0 ± 7.2 | 30.7 ± 6.3 | 31.4 ± 7.3 | 31.6 ± 7.8 | 32.2 ± 5.9 | 30.8 ± 7.6 | 31.7 ± 5.9 | 31.2 ± 7.3 | 31.4 ± 7.0 | 31.0 ± 7.0 |
| Calcium, mg | 413.4 ± 120.3 | 424.7 ± 117.7 | 405.3 ± 121.5* | 408.3 ± 113.4 | 420.3 ± 127.5 | 412.0 ± 120.1 | 438.6 ± 99.0 | 402.2 ± 126.5 | 430.7 ± 87.7 | 409.1 ± 121.7 | 411.9 ± 115.4 | 420.9 ± 123.0 |
| Iron, mg | 5.2 ± 1.3 | 5.2 ± 1.3 | 5.2 ± 1.3 | 5.0 ± 1.2a | 5.4 ± 1.3b | 5.2 ± 1.3ab | 5.4 ± 1.2 | 5.1 ± 1.3 | 5.2 ± 0.9 | 5.2 ± 1.3 | 5.2 ± 1.3 | 5.2 ± 1.3 |
| Vitamin A, μg | 306.4 ± 223.0 | 315.9 ± 233.1 | 299.6 ± 215.4 | 301.0 ± 211.5 | 320.2 ± 242.4 | 297.8 ± 214.0 | 404.4 ± 274.7 | 263.7 ± 181.2 | 325.6 ± 220.9 | 299.0 ± 222.1 | 309.4 ± 236.7 | 317.0 ± 216.1 |
| Vitamin C, mg | 18.4 ± 13.7 | 18.0 ± 13.8 | 18.7 ± 13.6 | 18.7 ± 14.4 | 19.1 ± 14.6 | 17.3 ± 11.4 | 14.7 ± 8.5 | 20.0 ± 15.2 | 19.3 ± 15.6ab | 17.3 ± 12.4a | 19.3 ± 14.2ab | 19.8 ± 15.3b |
| Food intake | ||||||||||||
| Energy, kJ | 2286 ± 716 | 2448 ± 717 | 2170 ± 693* | 2215 ± 669 | 2291 ± 711 | 2365 ± 768 | 2502 ± 679 | 2199 ± 709* | 2137 ± 785a | 2213 ± 691a | 2304 ± 701ab | 2427 ± 747b |
| Total fat, % energy | 34.3 ± 5.5 | 34.0 ± 5.3 | 34.6 ± 5.7 | 34.1 ± 5.5 | 34.5 ± 5.23 | 34.4 ± 5.9 | 35.0 ± 4.7 | 34.0 ± 5.9 | 34.0 ± 5.4 | 34.4 ± 5.7 | 34.6 ± 5.6 | 34.1 ± 5.3 |
| Saturated fat, % energy | 11.6 ± 2.7 | 11.7 ± 2.6 | 11.5 ± 2.8 | 11.6 ± 2.7 | 11.6 ± 2.7 | 11.7 ± 2.7 | 12.2 ± 2.4 | 11.4 ± 2.8 | 11.5 ± 2.6 | 11.6 ± 2.8 | 11.5 ± 2.5 | 11.6 ± 2.7 |
| Protein, g | 23.1 ± 7.7 | 24.5 ± 7.5 | 22.1 ± 7.7* | 22.7 ± 7.3 | 23.0 ± 7.5 | 23.8 ± 8.4 | 24.9 ± 7.4 | 22.3 ± 7.7 | 21.0 ± 8.4a | 22.5 ± 7.6a | 23.1 ± 7.5ab | 24.5 ± 7.8b |
| Calcium, mg | 289.6 ± 132.8 | 324.1 ± 130.6 | 265.0 ± 128.9* | 284.9 ± 129.6 | 293.3 ± 133.9 | 291.3 ± 135.4 | 343.6 ± 121.3 | 265.6 ± 130.5* | 270.0 ± 128.5ab | 278.6 ± 131.2a | 286.2 ± 126.2a | 314.5 ± 137.1b |
| Iron, mg | 3.7 ± 1.3 | 3.9 ± 1.3 | 3.6 ± 1.3* | 3.6 ± 1.2 | 3.8 ± 1.4 | 3.8 ± 1.3 | 4.0 ± 1.3 | 3.6 ± 1.3 | 3.4 ± 1.2a | 3.6 ± 1.3a | 3.7 ± 1.3a | 3.9 ± 1.4b |
| Vitamin A, μg | 180.2 ± 146.9 | 202.1 ± 160.4 | 164.6 ± 134.4* | 177.8 ± 137.7ab | 170.8 ± 135.5a | 193.3 ± 167.4b | 234.2 ± 183.8 | 156.7 ± 121.0* | 155.8 ± 113.6ab | 172.3 ± 140.0a | 177.4 ± 148.2ab | 199.4 ± 159.6a |
| Vitamin C, mg | 11.6 ± 10.7 | 11.8 ± 11.2 | 11.6 ± 10.4 | 12.3 ± 11.9 | 11.9 ± 11.3 | 10.7 ± 8.3 | 9.2 ± 6.8 | 12.7 ± 11.9 | 11.8 ± 12.7ab | 10.8 ± 9.3a | 11.8 ± 10.9ab | 13.3 ± 12.6b |
Values are means ± SD. *Different from boys or Caucasian children, < 0.001. Within a grade level or BMI percentile row, means with superscripts without a common letter differ, P < 0.001.
TABLE 5.
Number of food pyramid servings at lunch in school cafeterias that were selected, discarded, and consumed1
| Selected (servings) | Plate waste (servings) | % discarded | Consumed (servings) | % consumed | |
| Discretionary fat2 | 22.8 | 5.9 | 26.5a | 16.9 | 73.5d |
| Total grains3 | 2.7 | 0.7 | 27.0ab | 2.0 | 73.0dc |
| Dairy4 | 1.0 | 0.3 | 30.0bc | 0.7 | 70.0cb |
| Added sugar5 | 3.6 | 1.1 | 31.1c | 2.5 | 68.9b |
| Total fruit and vegetables4 | 1.1 | 0.4 | 37.1d | 0.7 | 63.0a |
Servings were defined following the Dietary Guidelines for Americans (22). Within the percent discarded and percent consumed columns, percents with superscripts without a common letter differ, < 0.005.
Discretionary fats are in grams.
Total grains are in ounce equivalents (1 ounce = 1/2 to 1 cup or 1 slice of bread, depending on the food).
Dairy and total fruit and vegetables are in cups.
Added sugar is in teaspoon equivalents of table sugar. Metric equivalents are: 1 teaspoon of sugar = 4.2 g, 1 ounce = 28.4 g, and 1 cup = 237 mL.
Sex and race.
Boys selected similar amounts of energy compared with girls but discarded less plate waste, resulting in greater energy intake (Table 4; Fig. 1B). Boys consumed significantly more protein, calcium, iron, and vitamin A than girls (Table 4). Compared with African American children, Caucasian children selected more and discarded less energy, resulting in greater energy intake (Fig. 1C), although the food selection comparison was nonsignificant (P = 0.15) after adjusting for the random effect of school (Table 4). Caucasian children also consumed more calcium and vitamin A compared with African American children.
BMI percentile and grade level.
Mean energy selected did not differ by BMI percentile category, but obese children discarded less plate waste than healthy-weight and overweight children, and obese children consumed more than healthy-weight and underweight children (Table 4; Fig. 1D). Energy selection and intake did not vary among 4th, 5th, and 6th graders (Table 4).
Percent of food selected that was consumed
Total sample.
Children consumed 72 and 74% of selected energy and protein, respectively, and they consumed no less than 63% of other nutrients and vitamins (Table 6). As noted earlier, children discarded less discretionary fat and more dairy, added sugar, and fruits and vegetables (Table 5).
TABLE 6.
Selected food that was consumed at lunch in school cafeterias for the entire sample and by sex, school grade level, race, and BMI percentile group1
| Total sample | Sex |
School grade level |
Race |
BMI percentile group |
||||||||
| Boys | Girls | 4th | 5th | 6th | Caucasian | African American | Underweight (<5th) | Healthy Weight (5th to <85th) | Overweight (85th to <95th) | Obese (≥95th) | ||
| n | 2049 | 852 | 1197 | 751 | 675 | 623 | 617 | 1398 | 51 | 1083 | 350 | 565 |
| Energy | 72.0 ± 17.6 | 76.3 ± 16.8 | 69.0 ± 17.6* | 72.2 ± 17.8 | 71.5 ± 17.5 | 72.4 ± 17.7 | 75.8 ± 16.7 | 70.5 ± 17.8 | 64.8 ± 19.8a | 70.2 ± 17.6a | 71.9 ± 17.2a | 76.4 ± 17.1b |
| Total fat2 | 103.1 ± 8.5 | 102.3 ± 7.1 | 103.6 ± 9.4 | 103.0 ± 8.6 | 103.2 ± 8.4 | 103.1 ± 8.6 | 102.0 ± 7.2 | 103.5 ± 9.0 | 102.6 ± 7.8 | 103.1 ± 9.1 | 102.8 ± 8.6 | 103.1 ± 7.4 |
| Saturated fat2 | 103.2 ± 13.2 | 103.7 ± 12.4 | 102.9 ± 13.7 | 102.8 ± 13.4 | 103.8 ± 12.9 | 103.1 ± 13.2 | 104.3 ± 11.4 | 102.5 ± 13.1 | 100.2 ± 11.6 | 103.2 ± 14.0 | 102.7 ± 11.9 | 103.8 ± 12.4 |
| Protein | 74.0 ± 18.4 | 78.2 ± 17.2 | 71.0 ± 18.6* | 73.9 ± 18.3 | 73.5 ± 18.4 | 74.7 ± 18.5 | 77.2 ± 17.8 | 72.7 ± 18.4 | 65.3 ± 20.9a | 72.2 ± 18.5ab | 73.3 ± 18.0b | 78.7 ± 17.2c |
| Calcium | 69.3 ± 22.8 | 75.7 ± 20.8 | 64.8 ± 23.1* | 69.0 ± 23.1 | 69.3 ± 22.6 | 69.7 ± 22.6 | 77.5 ± 19.5 | 65.7 ± 23.3* | 61.1 ± 25.3a | 67.4 ± 22.9a | 69.0 ± 22.3ab | 73.9 ± 22.0b |
| Iron | 72.1 ± 19.4 | 75.5 ± 18.9 | 69.7 ± 19.4* | 72.5 ± 19.6 | 71.1 ± 19.6 | 72.7 ± 19.0 | 74.0 ± 19.0 | 71.3 ± 19.4 | 64.4 ± 20.3a | 70.3 ± 19.6a | 71.6 ± 18.6ab | 76.4 ± 18.8b |
| Vitamin A | 62.7 ± 25.6 | 68.1 ± 25.0 | 58.9 ± 25.5* | 63.1 ± 25.6 | 60.2 ± 26.1 | 65.1 ± 24.9 | 64.2 ± 27.0 | 62.1 ± 25.0 | 54.1 ± 26.6ab | 62.0 ± 25.7a | 61.2 ± 25.0ab | 65.8 ± 25.5b |
| Vitamin C | 64.4 ± 24.4 | 66.4 ± 25.0 | 62.9 ± 23.9 | 66.3 ± 25.5 | 63.0 ± 24.1 | 63.5 ± 23.3 | 63.3 ± 23.6 | 64.9 ± 24.7 | 56.6 ± 25.3 | 63.5 ± 24.3 | 63.7 ± 25.5 | 67.2 ± 23.7 |
Values are means ± SD percent of selected food that was consumed (the units of measure used in these calculations were kJ for energy; percent of energy for fat and saturated fat; g for protein; mg for calcium, iron, and vitamin C; and g for vitamin A).
Because the total fat and saturated fat values are ratios of the percent of energy in the food consumed relative to the percent of energy in the food selected, values > 100 indicate that proportionally more fat was consumed than served. *Different from boys or Caucasian children, < 0.001. Within a grade level or BMI percentile row, means with superscripts without a common letter differ, P < 0.001.
Sex and race.
Boys consumed a larger percent of selected energy, protein, calcium, iron, and vitamin A than girls (Table 6). Caucasian children consumed a larger percent of calcium than African American children (Table 6).
BMI percentile and grade level.
Obese children consumed a larger percent of energy than underweight, healthy-weight, and overweight children. The percent of selected protein, calcium, iron, and vitamin A that was consumed differed significantly by BMI percentile categories, with heavier children consuming larger percentages of selected nutrients (Table 6). No significant differences were noted among grade levels (Table 6).
Discussion
The results indicate that 77% of participants’ food selection met the SMI standard for energy, which provides a lower limit and therefore cannot be used to determine whether children are being served energy in excess of a criterion, such as estimated energy requirements (EER). The IOM recommendations (10), however, provide an age-dependent range of energy selection that was developed taking into consideration energy requirements. When the IOM recommendations were referenced, only 16% of children were within the recommended energy selection range and 74% of children exceeded the upper limit. These results indicate that the presence of an upper limit in the IOM criteria provides important information that is not available when the SMI standards are referenced.
The likelihood of meeting the SMI standard for energy was not influenced by sex, race, grade level, or BMI percentile group. Similarly, mean energy selection did not differ by sex, race, grade level, or BMI percentile group, but differences in plate waste contributed to energy intake differences among groups; e.g. obese children discarded less and consumed more energy than leaner children. This finding, in addition to the finding that 28% (882 kJ) of selected energy was discarded, suggests that the amount of food being provided to, or being selected by, children might contribute to food waste and higher levels of energy intake. The mean BMI percentile of this sample was 69.5 and the most frequent BMI percentiles were 98 and 99 (4); hence, it is possible that many children were consuming energy in excess of their age-appropriate EER. This possibility is consistent with another study that found that elementary school children, but not middle and high school children, reported energy intake that exceeded their EER (11).
Unlike energy, the SMI standards provide an upper limit for percent of energy from fat (≤30%) and saturated fat (<10%). A range for total dietary fat (25–35% of energy) with a higher upper limit is recommended by the IOM and the saturated fat recommendation is the same as the SMI standards. The results indicate that <30% of children met the SMI fat standard, suggesting overselection of fat. This is consistent with another study that found that <33% of schools met the fat standards (12). Over one-half of children met the IOM recommendations for total fat, however. When both standards are referenced, <30% of children meet the saturated fat recommendations, indicating that children are selecting excess saturated fat. Furthermore, 11.6% of energy consumed was from saturated fat, a finding that is consistent with another study that found that 80% of students consumed diets high in saturated fat based on 24-h food recall (11). The present study also found that children were less likely to discard fat than carbohydrate, resulting in proportionally more fat in the meals actually being consumed.
More than 86% of children met the SMI standards for protein, calcium, and iron, with 53 and 42% of children meeting the vitamins A and C standards, respectively. Similar results were obtained when the IOM recommendations were referenced, with a smaller percent of children meeting or exceeding the protein (71%) and vitamin C (19%) targets. Different SMI standards apply to children in kindergarten through 6th grade and 7th through 12th grade, while the IOM recommendations are specific to children in 3 age ranges: 5–10 y, 11–13 y, and 14–18 y. In this study, all children were in grades 4–6, but their ages spanned all 3 IOM age categories. The IOM's target for most nutrients increases with age, which helps explain differences between results when SMI and IOM recommendations were utilized.
Results from this study indicate that the nutritional quality of children's meals could be improved, particularly concerning saturated fat and vitamin C. Nutrition could be improved by systemically changing the types and amounts of certain foods offered to children, such as serving foods higher in nutrient density and lower in energy density. This can be accomplished by adding vegetables into the foods provided to children (23) and by increasing the variety of fruits and vegetables offered. These suggestions and the conclusions from this study are consistent with the IOM (10), which recommends increasing the amount and variety of fruits, vegetables, and whole grains. It is unclear, however, if children will consume a larger amount of nutritious foods when these foods are offered in greater abundance unless foods of poorer nutritional value are served in smaller portions, because children in this study discarded a smaller percent of discretionary fats and a larger percent of fruits and vegetables.
The results of the study must be interpreted in the context of it limitations. First, the SMI and IOM standards apply to food selection over 5 d and food intake was measured for 3 d in the present study. Nevertheless, we previously found that measuring food intake over 3 d in school cafeterias produces reliable and representative estimates of food intake (20, 21). Second, the IOM recommendations were developed to guide mean food selection; therefore, the recommendations can be met even if many individual children do not meet the criteria. Third, all 33 schools were located in rural (14) areas of Louisiana, limiting generalizability of the results. Fourth, there are production and administrative costs to changing school menu policy and practices, and these costs must be considered when implementing changes. Finally, the IOM recommendations were recently released and it is unlikely that food service managers know of or have had a chance to modify menus to meet the recommendations.
In summary, <30% of children met the saturated fat recommendations and children discarded a smaller percent of fat and a larger percent of foods high in carbohydrates, such as fruits and vegetables. On average, children consumed 72% of food selected, resulting in 882 ± 581 kJ (211 ± 139 kcal) being discarded per student per lunch. The IOM recommendations include upper and lower limits for energy, which provides important information that is not available when only minimum values are suggested.
Supplementary Material
Acknowledgments
C.M. analyzed and interpreted data, and wrote the paper. J.T. and H.H. provided essential services, analyzed and interpreted data, and helped write the paper. M.L., T.S., R.N., A.S., and C.C. provided essential services, including writing and editing the paper. D.W. designed the project, conducted the research, provided essential services, interpreted data, and helped write the paper. All authors read and approved the final manuscript.
Footnotes
Supported by NIH grants R01 HD048483 (PI: D. Williamson) and K23 DK068052 (PI: C. Martin) and by the USDA (58-6435-4-90). In addition, this work was partially supported by the Nutrition Obesity Research Center (NORC) (grant no. 1P30 DK072476) entitled “Nutritional Programming: Environmental and Molecular Interactions” sponsored by National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
C. K. Martin, J. L. Thomson, M. M. LeBlanc, T. M. Stewart, R. L. Newton, H. Han, A. Sample, C. M. Champagne, and D. A. Williamson, no conflicts of interest.
This trial was registered at clinicaltrials.gov as NCT00289315.
Supplemental Figure 1 and Supplemental Table 1 are available with the online posting of this paper at jn.nutrition.org
Abbreviations used: EER, estimated energy requirements; IOM, Institute of Medicine; LA Health, Louisiana Health; NSLP, National School Lunch Program; SMI, School Meals Initiative.
Literature Cited
- 1.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288:1728–32 [DOI] [PubMed] [Google Scholar]
- 2.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–50 [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–5 [DOI] [PubMed] [Google Scholar]
- 4.Williamson DA, Champagne CM, Han H, Harsha D, Martin CK, Newton RL, Ryan DH, Sothern MS, Stewart TM, et al. Increased obesity in children living in rural communities of Louisiana. Int J Pediatr Obes. 2009;4:160–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dietz WH. The obesity epidemic in young children. Reduce television viewing and promote playing. BMJ. 2001;322:313–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hassink S. Problems in childhood obesity. Prim Care. 2003;30:357–74 [DOI] [PubMed] [Google Scholar]
- 7.Koplan JP, Liverman CT, Kraak VI. Institute of Medicine, Committee on Prevention of Obesity in Children and Youth. Preventing childhood obesity: health in the balance. Washington, DC: National Academic Press; 2005 [PubMed] [Google Scholar]
- 8.Ralston K, Newman C, Clauson A, Guthrie J, Buzby J. The National School Lunch Program background, trends, and issues. Available from: http://purl.umn.edu/56464 2008
- 9.Office of the Federal Register, National Archives and Records Administration National School Lunch Program and School Breakfast Program: School Meals Initiative for Healthy Children. Final Rule. Federal Register. 1995;60:31188–222 [Google Scholar]
- 10.Stallings VA, Suitor CW, Taylor CL. School meals: building blocks for healthy children. Washington, DC: The National Academies Press; 2010 [PubMed] [Google Scholar]
- 11.Clark MA, Fox MK. Nutritional quality of the diets of US public school children and the role of the school meal programs. J Am Diet Assoc. 2009;109:S44–56 [DOI] [PubMed] [Google Scholar]
- 12.Crepinsek MK, Gordon AR, McKinney PM, Condon EM, Wilson A. Meals offered and served in US public schools: do they meet nutrient standards? J Am Diet Assoc. 2009;109:S31–43 [DOI] [PubMed] [Google Scholar]
- 13.Williamson DA, Champagne CM, Harsha D, Han H, Martin CK, Newton R, Jr, Stewart TM, Ryan DH. Louisiana (LA) Health: design and methods for a childhood obesity prevention program in rural schools. Contemp Clin Trials. 2008;29:783–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005;95:1149–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CDC CDC growth charts: United States. 2000[cited 2007 Oct 31]. Available from: http://www.cdc.gov/nchs/about/major/nhanes/growthcharts/datafiles.htm [PubMed]
- 16.Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120Suppl 4:S193–228 [DOI] [PubMed] [Google Scholar]
- 17.Williamson DA, Allen HR, Martin PD, Alfonso AJ, Gerald B, Hunt A. Comparison of digital photography to weighed and visual estimation of portion sizes. J Am Diet Assoc. 2003;103:1139–45 [DOI] [PubMed] [Google Scholar]
- 18.Williamson DA, Allen HR, Martin PD, Alfonso A, Gerald B, Hunt A. Digital photography: a new method for estimating food intake in cafeteria settings. Eat Weight Disord. 2004;9:24–8 [DOI] [PubMed] [Google Scholar]
- 19.USDA, Agricultural Research Service Continuing survey of food intakes by individuals, 1994–1996, 1998. Beltsville (MD): Food Surveys Research Group; 2000 [Google Scholar]
- 20.Martin CK, Newton RL, Jr, Anton SD, Allen HR, Alfonso A, Han H, Stewart T, Sothern M, Williamson DA. Measurement of children's food intake with digital photography and the effects of second servings upon food intake. Eat Behav. 2007;8:148–56 [DOI] [PubMed] [Google Scholar]
- 21.Williamson DA, Copeland AL, Anton SD, Champagne C, Han H, Lewis L, Martin C, Newton RL, Jr, Sothern M, et al. Wise Mind project: a school-based environmental approach for preventing weight gain in children. Obesity (Silver Spring). 2007;15:906–17 [DOI] [PubMed] [Google Scholar]
- 22.USDA and Department of Health and Human Services Dietary guidelines for Americans. 6th ed Washington, DC: U.S. Government Printing Office; 2005 [Google Scholar]
- 23.Leahy KE, Birch LL, Fisher JO, Rolls BJ. Reductions in entree energy density increase children's vegetable intake and reduce energy intake. Obesity (Silver Spring). 2008;16:1559–65 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.