Abstract
Introduction
Stress and burnout are endemic to post-graduate medical training but little research is available to guide supportive interventions. The identification of longitudinal emotional and developmental coping needs of internal medicine residents could assist in better designing and implementing supportive interventions.
Methods
In this retrospective, exploratory study, six internal medicine resident support groups (n = 62 PGY1-3 residents) were followed for a period of two years. Qualitative data were extracted from monthly support group process notes to identify common themes, stressors, emotions, coping strategies, and developmental challenges faced during training. Quantitative questionnaire data were collected on burnout, group attendance, and resident satisfaction.
Results
Using professional identity development models and classic stress and coping theory as a starting point, a derivation of Grounded Theory was used to identify common themes and emotions contained in support group process notes. The most common themes included understanding resident roles and responsibilities, developing an identity as a resident and physician, building professional confidence, cognitive and behavioral responses to stress, and concerns about flaws in local and national health care training and delivery systems. Anxiety and guilt were the most commonly reported emotions, followed by positive emotions and anger. Burnout scores were highest for the second half of the PGY1 year, but improved over subsequent training years. Support group attendance and satisfaction were both high. Residents overwhelmingly pointed to peer relationships as the most critical source of support throughout postgraduate training.
Conclusions
Developmentally-informed programmatic adaptations could better support the emotional growth and personal/professional development of postgraduate medical trainees. Future directions should include a controlled trial of resident support groups, assessments of “active ingredients” (i.e. what supportive interventions are most effective), and/or evaluations of programmatic adaptations.
Keywords: Support Groups, Group Process, Burnout, Coping, Graduate Medical Education
Recent attention to resident work hours, sleep deprivation, medical errors, and trainee impairment has highlighted the stress endemic to current models of physician training. As many as 76% of medical residents report burnout and consequent suboptimal patient care.1 Empathy decreases over the course of internship, while anger, depression, and fatigue increase.2 Well-being in residency impacts relationships with patients, peers, and overall performance.3 The U.S. Accreditation Council for Graduate Medical Education has responded with work hour regulations and requirements for training programs to provide support for resident wellness.
In comprehensive review of the resident stress literature, Levey4 and the Association of Program Directors in Internal Medicine5 describe the leading causes of stress and impairment divided into three main categories: (1) Situational Stressors such as work hours, sleep deprivation, and staff conflicts; (2) Personal Stressors such as conflicts with family or friends, financial difficulties, or moving to a new city; and (3) Professional Stressors such as patient responsibilities, teaching or supervisory responsibilities, and information overload. Potentially disruptive, special situations such as the “marginal” resident who knows s/he is not performing well, the “mismatched” resident whose skills do not fit the selected specialty, and the “disruptive” resident who is medically competent but interpersonally abrasive were also noted. In an 11 year longitudinal study of physicians followed from medical school into clinical practice, self-criticism and avoidant coping were strong predictors of future stress and depression. Main stressors perceived by practicing physicians included relationships with senior doctors, making medical mistakes, conflict of career with personal life, and litigation fears. Nearly all felt overwhelmed by work demands and work load.6
More recent studies have noted that although stress appears to be universal for all medical trainees, the “critical events” of training can be both a source of distress and a source of personal growth. Ackerman et al7 identify critical event categories that include confidence, life balance, connections, emotional responses, managing expectations, and facilitating teamwork – all of which can be “high points, low points, or conflicts” depending on the situation and the resident. Modifiable predictors for personal growth included agreeing that reflection is important during residency, having a strong desire to develop personally and professionally, feeling supported by one’s program director, and feeling socially connected.8
Although a number of intervention program descriptions are available, little empirical guidance is offered on program structure or content.4–6,9,12 Potentially important elements of a resident assistance program include screening and assessment for distress, short-term counseling, ongoing monitoring with follow-up support, referrals to long term specialty care, and programmatic assurance of confidentiality and schedule release to attend appointments.4,9 Pitt et al10 make explicit links between medical errors, patient safety, and resident mental health as a means of both explaining resident stress (as a consequence and cause of making medical errors) and to leverage support for a comprehensive psychiatric treatment program. By ensuring confidentiality and addressing financial and scheduling barriers, 170 residents used the mental health program over a 4 year period with nearly 60% meeting DSM-IV criteria for Major Depression.
In a systematic review of stress management interventions for medical trainees, Shapiro et al11 identified over 600 articles discussing trainee stress but found only 24 that reported an intervention program for residents or medical students. Of the 24, only 6 studies were rigorously designed and all pertained to medical students. 5 of the 6 studies showed positive effects on stress for the intervention group. Nearly all interventions were delivered in a group context and varied in length from 2 hours to over 50 hours total over the course of a year. Optimal duration and intensity could not be determined. Content varied considerably and included relaxation training, mindfulness, hypnosis, supportive discussions, ways to challenge cognitions, time management, social activities, etc. The most effective and efficient content or interventions could not be determined. The most commonly reported outcome measure, trainee satisfaction, was nearly universally high for all intervention programs.
Although data on design and effectiveness are sparse, resident support groups continue to be a common component of many well-being programs.13 Prior studies on medical trainee stress can predict what sorts of issues might arise and potentially point to evidence-based or otherwise clinically sound interventions to employ. With a few notable exceptions, most studies have been cross-sectional survey studies that lack the depth and complexity of longitudinal, qualitative or ethnographic studies that follow trainees throughout the ups and downs of residency. Moreover, the focus has been almost exclusively on distress, depression, and anxiety with little notice of the occurrence and cultivation of positive emotions. To determine the full potential of support groups, it is essential to closely analyze emerging themes, emotions, and coping needs expressed by trainees during real support groups. By better understanding the challenges postgraduate trainees face in this critical time of professional development, we hope to promote more efficient and effective support interventions.
This paper presents a mixed methods, longitudinal examination of theoretically and empirically-derived medical resident support groups. Results are used to determine and validate the primary developmental challenges, stressors, emotions, and broad ways of coping experienced by residents over the course of training. As in other studies, content and interventions were multi-faceted but, unlike other studies, interventions were guided by ongoing quantitative reports of burnout and emerging coping challenges. Moreover, both positive and negative emotions were tracked over time with linked interventions to facilitate processing of negative emotions and “savoring” of positive emotions and experiences. By richly identifying both the content and timing of support group issues, other program directors and support group facilitators may be able to design supportive interventions to better meet the ever evolving needs of trainees.
Methods
Subjects
All primary care internal medicine interns and residents in a large, urban, U.S. academic medical center were invited to join the newly developed support groups. 62 out of 62 possible residents agreed to participate (total two year n=62 unique residents: in year 1 n=20 PGY3, 14 PGY2, 14 PGY1; in year 2, 14 new PGY1’s were added and all PGY3’s from the prior year graduated). Group members were 68% female and 47% Caucasian. Resident age ranged from 27 to 35yo. 67% were in a committed relationship and 11% had children. None were international medical graduates. IRB approval was obtained and all ethical guidelines for subject protection were followed.
Support group structure
Each group consisted of 7–10 members of the same training year (PGY1-3) who shared an outpatient ambulatory clinic. There were two support groups for each training year – i.e. two intern groups, two PGY2 groups, and two PGY3 groups. Attendance was voluntary, and groups met for one hour per month. To increase the likelihood of attendance, all support groups were scheduled for the first hour of an outpatient clinic and residents were excused from patient care for that hour. All groups were facilitated by the first author, a licensed clinical psychologist and group therapist. Each session started with the completion of the quantitative burnout measure followed by a 3–4 minute check-in by each resident in attendance. Residents shared primary coping challenges and notable emotionally-charged experiences encountered over the past month as part of the check-in. Residents were taught to take responsibility for asking for more or less group time depending on how well they were doing.
Qualitative Measures
2–3 pages of de-identified group process notes were completed by the group facilitator during and after each session (total number of sessions over two years = 72). Formal, structured guidelines for process note generation were followed. Process notes included primary challenges and emotions shared by each resident during check-in, information on style, tone, and content of discussions, emotions expressed during the group, group process variables (e.g. cohesion, subgroup formation, group stage), direct quotes from participants, and any structured exercises used.
Qualitative Analysis
A variant of grounded theory14 was used to inform the initial analytic process. Seminal works on professional identity development, resident stress, physician wellness, and general stress and coping theories were particularly instructive as a starting point for possible thematic categories.7,11–12, 15–16 Process notes from all 72 group sessions were broken into single, analyzable “extractions” by the first author – i.e. a sentence or fragment containing one idea, thought, event, or emotion. Extractions consisted of direct quotations and descriptions of group phenomena. Sample extractions are found below. A total of n=729 extractions were assigned a code number and randomly shuffled across all years and groups. A random subsample of 250 extractions was independently analyzed by each author to create an initial coding scheme of broad themes and more specific categories within each theme. Using an iterative, consensus building process, both authors (AA, BB) collaboratively examined the coded extractions and created and/or revised emotions, themes, and subcategories as needed. While existing literature informed initial category choices, unique and revised categories emerged from the data. All remaining extractions were independently classified by each author using the consensual coding scheme. Initial interrater reliability was 80.1%. Coding disagreements (19.9% of the extractions) were discussed until consensus was reached. 62 extractions were classified as belonging in more than one theme and 28 described more than one emotion.
Quantitative Measures
Quantitative measures assessed burnout and resident satisfaction. Monthly burnout was measured using the Tedium Index.17 The Tedium Index is a 21-item, self-report questionnaire that assesses physical, emotional, and mental exhaustion. It has been cross-culturally validated in over 3,900 professionals from a wide range of disciplines, including health care, social work, and education. It has shown good test-retest reliability (0.89 at one-month) and a high internal consistency with a Cronbach’s alpha of 0.91 to 0.93.17 Attendance was recorded to calculate percent in attendance. Resident satisfaction was measured at the end of each academic year using open ended questions and two 1–7 Likert scales including “How satisfied are you with your support group experience” and “What impact (if any) did the group have on your well-being.”
Results
Residents attended 85% of the support groups (10.19/12 each year), and reported a mean satisfaction score of 6.56 (7 = very satisfied). Support group had a strong positive impact on well-being (mean = 6.34; 7 = strong positive impact, 1 = strong negative impact). Building supportive relationships with peers was frequently noted as the most important strength, while the short duration (1 hour) and low frequency of meetings (once per month) were seen as the greatest weaknesses.
The 729 extractions were coded using 6 broad themes and further subdivided into 23 subcategories (see Table 1). A total of 791 thematic codes and categories were assigned. When an emotion was clearly articulated (“e.g. I feel so angry right now”), it was also coded into one of 12 possible emotion categories – guilt, anger, sadness, numbness/affective blunting, anxiety/fear, hopelessness, overwhelmed/stressed out, bored/apathetic, lonely, upset (generall feeling bad but not specified), any positive emotion (happy, excited, inspired, confident, proud), other emotion (shocked, disappointed). A total of 270 clearly articulated emotions were coded.
Table 1.
Support Group Themes and Categories
| Broad Themes | Categories | Examples |
|---|---|---|
| 1. Practice of Medicine | 1.1 End of Life Issues | I’m on the CCU now and just had a pt die. I hate having to be strong. I just want to cry. |
| 1.2 Medical Mistakes | I left the wire in a femoral line and it was found the next day. I felt so bad. | |
| 1.3 Medical Decision Making | Should I have called anesthesia? Did I make the wrong decision?… | |
| 1.4 Medical Ethics | My patient wants me to lie so he can get disability. He deserves it but can I do that? | |
| 2. Professional Development | 2.1 Professional Competence/Skills | I need to learn more. I hardly know anything about HIV…. |
| 2.2 Professional Confidence | Who am I to be making life and death decisions? This is insane! | |
| 2.3 MD/Resident Identity | I have my DEA number now. I feel so official. So like a real doctor! | |
| 2.4 MD/Resident Role and Responsibility | I feel like I shouldn’t be relaxing. I should be studying or reading or something. | |
| 2.5 Peer Relationships | Somehow just knowing all you guys are in the hospital helps me get through all this. | |
| 2.6 Relationships with Patients | I make it a point to say goodbye to all my patients…just hold their hand and honor them. | |
| 2.7 Career Path | I think I might join the peace corp…that’s my career path. | |
| 3. Personal Development | 3.1 Self-Esteem | If I suck at this, I must just suck. |
| 3.2 Personal Confidence | Does he think I’m a mess? Why is he coming over here? | |
| 3.3 Self-Awareness | I’m a lot more aware of my limitations and my strengths now. I can’t do everything and that’s hard to accept. | |
| 3.4 Attitudes and Values | Resident develops migraines and value placed on self-care changes. | |
| 3.5 Intimacy (personal relationships) | I feel like a scar is forming between me and my non-MD friends. They just can’t understand what I’m going through. | |
| 3.6 Assertiveness | I’m learning to say no more often…. | |
| 4. Coping and Other Stressor Responses | 4.1 Emotional Management | We have to process emotions with the faucet method–turn them on and off in an instant…. |
| 4.2 Cognitive Responses to Stress | Just remember to take this one day at a time. Don’t look too far ahead into the future. It is just about surviving day by day. | |
| 4.3 Behavioral Responses to Stress | I call my partner and have him light a candle after every death. | |
| 4.4 Other Psychological Defenses | I finally slipped and let myself be bitter. | |
| 5. Program, Faculty, Staff Issues | 5.1 Health Care System | The system is so dysfunctional. It’s so broken. |
| 5.2 Local Program Issues and Complaints | Why are my resident and attending always criticizing me? Why can’t they just do a little more to help?” | |
| 6. Personal Stressors and Events | No Subcategories | My grandmother is going to pass away soon. |
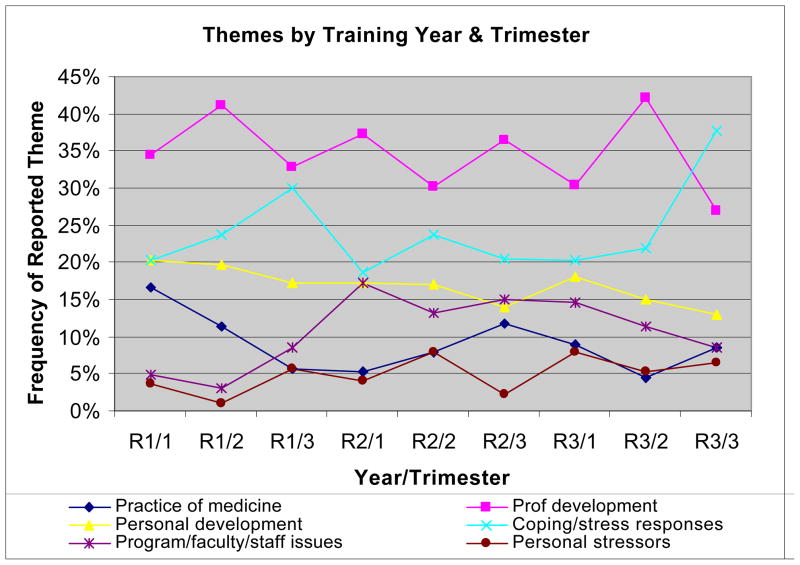
The frequencies of themes, categories, and emotions were noted over time by year of training. Not surprisingly, the theme most commonly present was the theme of Professional Development. The one exception occurred in the final third of PGY3 with Coping and Other Stressor Responses becoming the most frequent theme (See Figure 1 with the X-axis reflecting year of training starting with internship and proceeding through the end of the third year). Within the Professional Development theme, the most common categories were Professional Confidence (2.2) and MD/Resident Role and Responsibility (2.4). As trainees become more comfortable in their roles over time, MD/Resident Role and Responsibility drops to its lowest point in PGY3. The second-most frequent theme across all years was Coping and Other Stressor Responses. The most common categories within this theme were Cognitive Responses to Stress and Behavioral Responses to Stress.
Fig 1.
Support Group Themes by Training Year
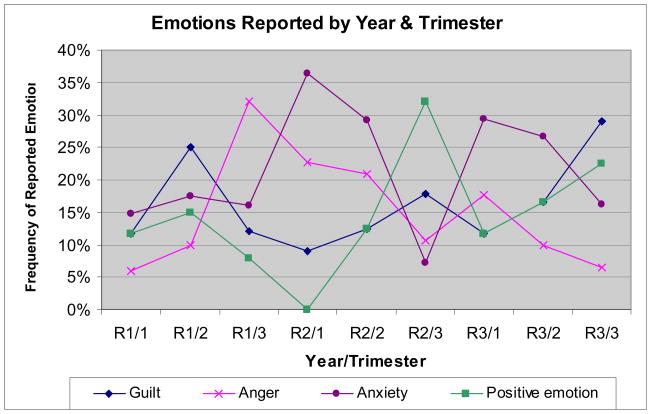
The most commonly expressed emotions over all training years were anxiety/fear, guilt, positive emotion, and anger (See Figure 2). Anxiety peaked at the beginning of the PGY2 (e.g. fear over running a team) and PGY3 years (e.g. job anxiety) but remained fairly consistent throughout the intern year. Guilt was highest in the middle of the intern year and at the end of PGY3 when residents were terminating their relationship with patients. Positive emotions (hope, pride, gratitude, happiness, feeling inspired) were concurrently present throughout all years but rose dramatically in PGY2 and PGY3. Anger steadily increased during the last third of the intern year and peaked during the transition from intern to PGY2 and did not notably drop until the last third of PGY2.
Figure 2.
Emotion Frequencies by Trimester of Each Training Year
Qualitative Findings for PGY1
For interns, the most common subcategories were MD/Resident Role and Responsibility (Category 2.4; 9.2% of extractions), Cognitive Responses to Stress (Category 4.2; 8.8%), Professional Confidence (Category 2.2; 8.4%), and Behavioral Responses to Stress (Category 4.3; 7.6%). End-of-life issues and insufficient time with family and friends were frequent issues in the first trimester. Forming and navigating relationships with peers emerged as a more dominant theme in the second trimester. Attitudes and Values (category 3.4) was increasingly present over the course of the year, as interns reported struggling with their reasons for going into medicine and feeling disillusioned.
Stressors included the death of patients, feeling isolated from family and friends, challenges to self-esteem and confidence, and the erosion of an idealized view of medicine. Common cognitive responses to stress included remembering the “power and prestige of being a physician,” reframing (e.g. internship as an investment), normalization, suppression, changing expectations (e.g. “I don’t have to be perfect”), looking to the future, complaining, and escape fantasies (e.g. “It would be so incredible to work in a coffee shop all day.) Interns found little time or energy for common behavioral responses to stress such as exercise or time with family or friends. Behavioral responses included marking completed days off a calendar, sleeping through days off, and displacing anger onto nursing staff, family, or strangers.
The most frequently expressed emotions over the course of the entire year were guilt (17.2%), anxiety/fear (16.2%), feeling generally “upset” (14.1%), anger (14.1%), and positive emotions (12.1%). As the year progressed, anger became more prominent while guilt and positive emotions peaked in the middle trimester and dropped to their lowest points in the final third of the year. Guilt was triggered by not performing competently, losing compassion, or from placing work over time with family and friends. The lack of time and/or capacity to process intense emotions provoked by clinical situations often left the intern feeling overwhelmed and upset. Anger was most frequently directed at the program, program directors, or the general health care system. Positive emotions included hope (e.g. “Seeing people get better and leave the hospital gives me hope”), confidence (“I’ve really learned a lot here…I’m feeling a lot more confident”), and happiness.
Qualitative Findings for PGY2
For the PGY2 year overall, the most common categories were Local Program Issues and Complaints (Category 5.2; 13.9% of extractions), Cognitive Responses to Stress (Category 4.2; 10.2%), MD/Resident Role and Responsibility (Category 2.4; 9.0%), and Behavioral Responses to Stress (Category 4.3; 7.8%). Professional Confidence (Category 2.2) was an issue in the first trimester as new R2’s began leading a team. Residents continued to struggle with defining their professional roles and expectations, but unlike the intern year, end-of-life issues and medical mistakes were discussed less. Coping strategies included seeking professional counseling, seeking social support, taking SSRI’s, reading more journal articles or clinical guidelines, taking more time for self care (e.g. dental appointments, taking a sick day), and scheduling more social activities.
The most frequently expressed emotions over the course of the R2 year were anxiety/fear (23.0%), anger (17.6%), positive emotion (16.2%), and guilt (13.5%). Anxiety dropped dramatically over the course of the year as did anger. Guilt showed modest increases from first to last trimester. While positive emotions were entirely absent in the first trimester, they represented nearly 1/3 of all articulated emotions in the final trimester. Common triggers for anxiety were leading an inpatient team, feeling solely responsible for decisions regarding patient care, and worry about future career directions. First trimester anger still focused on the program, directors, and the health care system. The rising frequency of positive emotions was due to asserting themselves, getting fellowships or more clarity on career directions, increasing the number of peer-peer social contacts, and a growing sense of professional competence as evidenced by patient outcomes and feedback.
Qualitative Findings for PGY3
For PGY3’s, the most common categories were Cognitive Responses to Stress (Category 4.2; 13.2%), Local Program Issues and Complaints (Category 5.2; 10.5%), Career Path (Category 2.7; 9.5%), and Professional Confidence (Category 2.2; 8.8%). High levels of program complaints are seen initially, but decrease over the course of the year as career goals are pursued (and achieved) and more perspective is developed (e.g. “I’m not feeling so angry anymore. I’ve grown a lot. In a way I think I was mad at a loss of innocence.”). Both professional confidence and career issues peak in the middle trimester when most residents began finding jobs or settled further training plans. While R3’s may feel more competent and confident, there was still substantial worry about becoming autonomous practitioners with no clear “plan.”
Although cognitive and behavioral responses to stress are common categories across all years, their frequencies surge in the final trimester. As residents began to feel more secure and to reflect more on their training experiences, these coping strategies often mitigated their more negative emotions and supported important insights – e.g. “Did we make residency harder than it has to be? I mean, is part of our suffering because we were so neurotic and so perfectionistic? Was our anger part of the drama that was unnecessary?” The categories of Self-Awareness (3.3) and Attitudes and Values (3.4) were higher than in any other point in training as PGY3’s recognize how training has impacted them and their practice of medicine (e.g. “When I was an intern I could have told you hundreds of patient stories – the stories were the most salient. I couldn’t remember labs or algorithms to save my life. Now I remember the labs and all the patients just blur together. What happened?”).
The most frequently expressed emotions were anxiety/fear (24.2%), guilt (18.9%), positive emotion (16.8%), and anger (11.6%). While guilt and positive emotions increased over the course of the year, anxiety and anger decreased. The most common trigger for guilt was graduating and “abandoning” a panel of outpatients. Positive emotions were triggered by a realization of how much they had learned and grown, the increased appreciation of peer relationships, and being able to see the “finish line.”
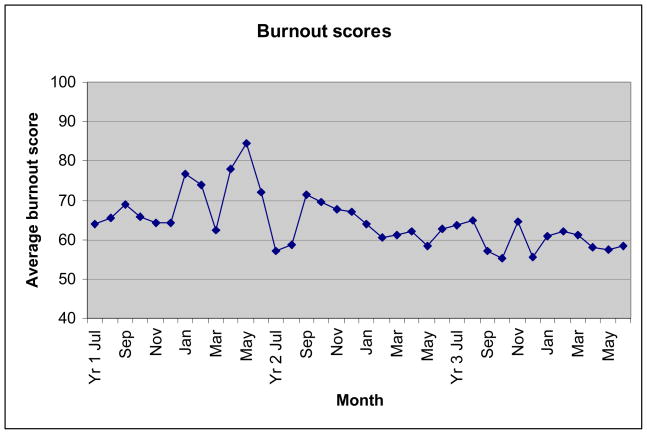
Quantitative Analysis
On average, burnout scores were higher for PGY1’s than any other group (see burnout averages chronologically arranged in Fig. 3). All 4 PGY1 cohorts (two PGY1 groups per year) had bimodal peaks of burnout near January and again in April/May. By January, most interns spent 5 of the past 6 months on the wards with frequent call nights resulting in cumulative fatigue. In late spring, the pressure and anxiety of leading an R2 ward team worsened burnout. Burnout scores for PGY2’s were lower than PGY1’s in the first two months but rise to similar levels in months 3–6. PGY2’s show lower burnout for the second half of the training year. Although PGY3’s generally have less burnout in the first half of the year, they are at similar levels to PGY2’s in the second half of the year.
Figure 3.
Monthly Mean Burnout Scores
Discussion
The resident support groups were a well-utilized forum for airing concerns, sharing developmental professional struggles, and eliciting support. Professional identity development and understanding resident role(s) were paramount. Emotional management and cognitive-behavioral responses to stress were key elements in understanding how residents responded to sometimes intense patient care issues, interpersonal peer conflicts, programmatic complaints, threats to work-life balance, and the ongoing challenges to professional confidence and personal self-esteem.
In general, all cohorts could have benefited from greater time devoted to the development of emotional processing skills around situations such as death and dying, medical mistakes, guilt, and anxiety. Successful processing could include the skillful detection of emotions in the self, understanding or developing insight into both the cause and meaning of these emotions, and learning skills to manage these emotions using strategies drawn from one of the many available emotion skills curricula.18–19
Anger was common and often had multiple causes. Trainee anger was sometimes displacement – i.e. re-directing anger to a more appropriate or safer target. Anger also served as a mechanism for building group cohesion with residents bonding by vilifying others. At other times, anger motivated residents to seek corrective action when faced with an interpersonal threat or social violation. Understanding the causes and functions of anger could be important skills to teach along with improved communication and conflict resolution. It is particularly challenging to encourage residents to share responsibility in system dysfunction rather than blaming others and perpetuating the problem.
Traditionally, residency has been conceptualized as something to “survive” rather than a time to thrive, grow, or even enjoy. The appreciation of the more positive and meaningful aspects of medicine were thought to emerge as a physician matures. However, our sample showed frequent positive emotions triggered by peers and patient care. Time for relationship building, reflection, and carefully guided prompts to elicit and savor positive emotions could be essential tools to deepen this capacity.
Implications by Training Year
For PGY1’s, early interventions could include coverage of death and dying issues and ample time for processing this often painful but critical aspect of medicine. As PGY1’s settle into their new roles and struggle for work-life balance, it could be helpful to include significant others and/or family members in joint sessions designed to build support and relay information about the coping challenges that PGY1’s will face. Considering the importance of peer-peer supports and the challenges of working in teams, early interventions could assist in building initial social ties and improving communication and teamwork.
The affective and cognitive load experienced during internship year makes time for reflection critical.7–8, 20 However, interns typically have the least amount of time for constructive processing or even minimal self-care. Restructuring the internship year to be less loaded or more gradually loaded might allow trainees to build new relationships, learn the hospital system, stay connected to existing social supports, develop skills in coping with end-of-life issues, build meaningful relationships with faculty and patients, and develop a more nuanced understanding of the health care training program.
As PGY2’s move past the anxiety of leading an inpatient team, they could benefit from further training in understanding team dynamics and group processes. Many have never led a team before and fail to recognize the importance of managing group dynamics. As the scope of responsibilities broaden, PGY2’s have the opportunity to experience important confidence building situations as long as sufficient support and titrated supervision are provided.
The core challenges of the PGY3 year include filling gaps in clinical knowledge and skills, “packaging” or marketing oneself, and navigating the sometimes difficult process of saying goodbye to peers, mentors, and patients. As PGY3’s become more competent and confident in their clinical, teaching, and leadership skills, they are better equipped to maturely self-reflect and re-address their coping habits. Moreover, the processing of unresolved resentments, grief, and other emotions could be facilitated in a support group format in this year of greater maturity while simultaneously helping residents to savor the more moving and inspiring aspects of medical practice. Although this study only looked at residency, it is possible that “recovery” continues after graduation.21
There are a number of important limitations to this study. First, although multiple groups of trainees across all three years of training were followed, cohort effects cannot be eliminated. It is possible these trainees are not representative of primary care internal medicine trainees at large. Structural and programmatic factors unique to the time periods studied might also have had an impact. Secondly, as in any qualitative study, definitive “answers” are not provided using a thematic analysis. Many other codebooks could have been developed. Moreover, the raw data used for the thematic analysis was taken from support group process notes rather than complete transcripts which may have created an unintentional filter leading to bias. While process notes are substantially condensed, a study comparing process notes and complete transcripts found that the major themes identified did not differ substantially as determined by independent raters. 22
Ultimately, this study provides an important look into the inner workings of resident support groups and illustrates the challenges faced by these trainees. We hope that this imperfect picture may stimulate programs to better tailor interventions and better support trainees in this critical developmental window.
Acknowledgments
Sources of funding: NIH/OBSSR/NCCAM grant (K07 AT003131-01 awarded to Dr. Satterfield.
Footnotes
Both authors contributed to the conceptualization, data collection, analysis, and write-up of the manuscript. Full criteria for authorship were met by each author.
Full IRB approval was obtained from the UCSF Committee on Human Research. Approval #H545306-3312-01.
References
- 1.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 2.Bellini LM, Baime M, Shea JA. Variation of mood and empathy during internship. JAMA. 2002;287:3143–3146. doi: 10.1001/jama.287.23.3143. [DOI] [PubMed] [Google Scholar]
- 3.Ratanawongsa N, Wright SM, Carrese JA. Well-being in residency: Effects on relationships with patients, interactions with colleagues, performance, and motivation. Patient Educ and Counseling. 2008;72:194–200. doi: 10.1016/j.pec.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 4.Levey RE. Sources of stress for residents and recommendations for programs to assist them. Acad Med. 2001;76:142–150. doi: 10.1097/00001888-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 5.APDIM. Stress and impairment during residency training: Strategies for reduction, identification, and management. Ann Intern Med. 1988;109:154–161. doi: 10.7326/0003-4819-109-2-154. [DOI] [PubMed] [Google Scholar]
- 6.Firth-Cozens J. Interventions to improve physicians’ well-being and patient care. Soc Science and Med. 2001;52:215–222. doi: 10.1016/s0277-9536(00)00221-5. [DOI] [PubMed] [Google Scholar]
- 7.Ackerman A, Graham M, Schmidt H, Stern DT, Miller SZ. Critical events in the lives of interns. J Gen Intern Med. 2008;24:27–32. doi: 10.1007/s11606-008-0769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wright SM, Levine RB, Beasley B, Haidet P, Gress TW, Caccamese S, Brady D, Marwaha A, Kern DE. Personal growth and its correlates during residency training. Medical Education. 2006;40:737–745. doi: 10.1111/j.1365-2929.2006.02499.x. [DOI] [PubMed] [Google Scholar]
- 9.Mushin IC, Matteson MT, Lynch EC. Developing a resident assistance program: Beyond the support group model. Arch Int Med. 1993;153:729–733. [PubMed] [Google Scholar]
- 10.Pitt E, Rosenthal MM, Gay TL, Lewton E. Mental health services for residents: More important than ever. Acad Med. 2004;79:840–844. doi: 10.1097/00001888-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Shapiro SL, Shapiro DE, Schwarz GER. Stress Management in Medical Education:A Review of the Literature. Acad Med. 2000;75:748–759. doi: 10.1097/00001888-200007000-00023. [DOI] [PubMed] [Google Scholar]
- 12.Novack DH, Suchman AL, Clark W, Epstein R, Najberg E, Kaplan C. Calibrating the physician: Personal awareness and effective patient care. JAMA. 1997;278:502–509. doi: 10.1001/jama.278.6.502. [DOI] [PubMed] [Google Scholar]
- 13.Alexander D, Skinner B. A pilot study using the group environment scale to evaluate first-year resident support groups. Fam Med. 2002;34:732–7. [PubMed] [Google Scholar]
- 14.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York: Aldine De Gruyter; 1996. [Google Scholar]
- 15.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- 16.Quill TE, Williamson PR. Healthy approaches to physician stress. Arch Intern Med. 1990;150:1857–1861. [PubMed] [Google Scholar]
- 17.Pines AM, Aronson E, Kafry D. Burnout: From Tedium to Personal Growth. New York: Free Press; 1981. [Google Scholar]
- 18.Satterfield JM, Hughes E. Emotion Skills Training for Medical Students: A Systematic Review. Medical Education. 2007;41:935–941. doi: 10.1111/j.1365-2923.2007.02835.x. [DOI] [PubMed] [Google Scholar]
- 19.Gabbard GO. The role of compulsiveness in the normal physician. JAMA. 1985;254:2926–2929. [PubMed] [Google Scholar]
- 20.Levine RB, Haidet P, Kern DE, Beasley BW, Bensinger L, Brady D, Gress T, Hughes J, Marwaha A, Nelson J, Wright SM. Personal growth during internship: A qualitative analysis of interns responses to key questions. JGIM. 2006;21:564–569. doi: 10.1111/j.1525-1497.2006.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ratanawongsa N, Wright SM, Carrese JA. Well-being in residency: a time for temporary imbalance? Medical Education. 2007;41:237–280. doi: 10.1111/j.1365-2929.2007.02687.x. [DOI] [PubMed] [Google Scholar]
- 22.Wolfson A, Sampson H. A Comparison of Process Notes and Tape Recordings: Implications for Therapy Research. Arch Gen Psychiatry. 1976;33(5):558–563. doi: 10.1001/archpsyc.1976.01770050026003. [DOI] [PubMed] [Google Scholar]