Abstract
Background
Case reports suggest a relationship between amphetamine abuse/dependence and aortic dissection, but no population-based epidemiologic studies have examined this link. Our objective was to test the hypothesis that young adults with a diagnosis of amphetamine abuse or dependence would be at higher risk for aortic dissection, after accounting for known risk factors.
Methods
In this population-based case control study of 30,922,098 discharges from the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS) from 1995 to 2007, among persons aged 18 to 49 years, we identified 3,116 thoracic and thoracoabdominal aortic dissections using ICD-9-CM codes 441.01 and 441.03. The SURVEYLOGISTIC procedure in SAS 9.2 was used to account for the NIS sampling methodology.
Results
In a multiple logistic regression analysis, while controlling for known risk factors, amphetamine abuse/dependence was significantly associated with aortic dissection (adjusted odds ratio = 3.33; 95% CI=2.37—4.69, p < 0.0001).
Conclusions
This statistically significant association suggests that amphetamine abuse/dependence may play a role in aortic dissection in young adults in the United States.
Abuse of amphetamine-like stimulants is a global problem. The United Nations Office on Drugs and Crime estimate that between 16 and 51 million people worldwide aged 15 to 64 years consumed amphetamine-type stimulants in 2007.1 The National Survey on Drug Use and Health reported that, in 2008, 2.6 million Americans had used an illicit or prescription-type stimulant nonmedically in the past year.2 Misuse of prescription-type stimulants among adolescents has been associated with use of illicit drugs, crime, and mental illness treatment.3
Aortic dissection is a rare, but catastrophic event. The incidence of aortic dissection has been estimated at 2.9 cases per 100,000 person-years.4 Aortic dissection has a high mortality rate.5 While aortic dissection is typically a disease of older age groups, it does occur among young adults. Among 951 patients diagnosed with aortic dissection in the International Registry of Aortic Dissection from 1996 to 2001, 68 (7%) patients were less than 40 years old.6
There have been limited case reports and case series of amphetamines linked to aortic dissection.7-9 For example, a review of autopsies in San Diego County, California, netted 84 cases of aortic dissection from 1987 to 1996.10 Of the 84 cases, 35 were screened for drug use, and of those, 7 (20%) tested positive for methamphetamine. It was noted that while the average age of the patients in these cases was 52 years, the average age of patients for the methamphetamine-associated cases was 41 years. Wako et al. (2007) have reported a case series of six patients with methamphetamine-associated aortic dissection. The six cases represented 5.5% of all the aortic dissection cases seen, and varied in age from 35 to 44 years.11 Dihmis et al. have reported the case of a 27 year old amphetamine user who died of acute aortic dissection.12 Ecstasy (MDMA) has also been linked to aortic dissection in a case report.13 A link between methamphetamine use and carotid artery dissection has been reported.14
A link between other risk factors and aortic dissection has also been reported in previous studies.4, 15, 16 For example, age, hypertension, cocaine use, smoking, dyslipidemia, connective tissue disorders (Marfan's syndrome and Ehlers-Danlos syndrome), hereditary vascular diseases (bicuspid aortic valve and aortic coarctation), vascular inflammation (giant cell arteritis, Takayasu arteritis, and cardiovascular syphilis), trauma, and Turner's syndrome are presumed risk factors of aortic dissection.17
In the current study, our primary aim was to determine whether amphetamine abuse/dependence was associated with thoracic and thoracoabdominal aortic dissections in a national inpatient population, 18 to 49 years of age, after adjusting for known risk factors. Our secondary aim was to describe temporal trends in both amphetamine abuse and aortic dissection.
Methods
Study Design and Patients
A population-based case control study design was used to test the association between amphetamine abuse/dependence and aortic dissection. National inpatient administrative data in the form of the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS) were obtained and analyzed.18 Eligibility requirements for entrance into the study population were (1) aged 18 to 49 years and (2) hospitalization from 1 January 1995 to 31 December 2007, regardless of diagnosis. The Institutional Review Board of The University of Texas Southwestern Medical Center at Dallas granted a waiver of approval for this study of de-identified hospital discharge data.
Nationwide Inpatient Sample and Study Population
The NIS, produced by the Healthcare Cost and Utilization Project (HCUP) through the Agency for Healthcare Research and Quality, is the largest all-payer inpatient database in the United States. It is a stratified sample of community hospitals in the United States, from 1988 to 2007. Discharge-level weights are included with the NIS (so that estimated parameters, in part, reflect the broader, national population). On a contractual basis, states provide HCUP with inpatient administrative data. In 1995, 19 states participated. This increased to a total of 40 states in 2007. In the 2007 NIS database, 90% of all hospital discharges in the United States were sampled. The database is an approximate 20% sampling of all community hospitals.19 The NIS is ideal for studying rare conditions, because of its large sample size.
Primary and secondary discharge diagnoses (up to 15 total) are coded using International Classification of Disease, Ninth Edition, Clinical Modification (ICD-9-CM).
The population used in the current study was all discharges in the NIS from 1 January 1995 to 31 December 2007, for persons aged 18 to 49 years. The study population consisted of 30,922,098 discharges of patients 18 to 49 years of age during this period.
Dependent Variable
The primary outcome measure was aortic dissection, defined using ICD-9-CM codes (Table I). We used only codes 441.01 and 441.03, which indicate thoracic and thoracoabdominal dissections of the aorta, respectively. We did not use codes 441.00 (unspecified site) and 441.02 (abdominal). In this study, aortic dissection was a binomial variable operationally defined as the presence or absence of aortic dissection in the principal discharge diagnosis within each hospital discharge. This strategy of using only thoracic and thoracoabdominal aortic dissections documented as the principal discharge diagnosis is conservative and designed to select those aortic dissections that were the primary cause of admission. Thus, we identified 3,116 aortic dissections from 1995 to 2007.
Table I.
Definition of Aortic Dissection, Substance Abuse, and Risk Factors from ICD-9-CM codes
| Condition | ICD-9 code |
|---|---|
| Aortic Dissection | 441.01, 441.03 |
| Substance Abuse* | |
| Amphetamines | 304.40 to 304.42, 305.70 to 305.72 |
| Cocaine | 304.20 to 304.22, 305.60 to 305.62 |
| Risk Factors | |
| Tobacco | 305.1, 989.84 |
| Hypertension | 401.0 to 405.99 |
| Lipid Disorder | 272.0 to 272.9 |
| Marfan's Syndrome | 759.82 |
| Ehlers-Danlos Syndrome | 756.83 |
| Biscuspid Aortic Valve† | 746.4 |
| Coarctation of the Aorta | 747.1, 747.10 |
| Giant Cell Arteritis | 446.5 |
| Takayasu's Disease | 446.7 |
| Cardiovascular Syphilis | 093.0 to 093.9 |
| Turner's Syndrome | 758.6 |
| Trauma (Motor Vehicle Traffic Accident) | E810.0 to E819.9 |
Codes indicating "in remission" were not used. Nonspecific codes of substance abuse or dependence not indicating the specific substance (304.8, 304.9, and 305.9) were not used.
Also includes congential aortic insufficiency.
Independent Variable and Covariates
The primary independent variable was active amphetamine abuse or dependence (ICD-9-CM codes 304.40 to 304.42, and 305.70 to 305.72; see Table I). Agents typically coded as amphetamines include methamphetamine, amphetamine, and ecstasy. Codes indicating remission of abuse or dependence were not used. We identified risk factors that might predispose a person to aortic dissection: increased age, hypertension, active cocaine abuse or dependence, smoking, dyslipidemia, connective tissue disorders (Marfan's Syndrome and Ehlers-Danlos Syndrome), hereditary vascular diseases (bicuspid aortic valve and aortic coarctation), vascular inflammation (Giant cell arteritis, Takayasu arteritis, and cardiovascular syphilis), trauma, and Turner's Syndrome.4, 15, 16 Age (in years) was a continuously measured variable. The other covariates, including the primary independent variable of amphetamine abuse/dependence, were coded binomially and, thus, operationally defined as the presence or absence of the condition.
Data Analysis
Secular Trends
The prevalence of amphetamine abuse/dependence and incidence of aortic dissection were calculated using the Surveymeans procedure in SAS 9.2 to find weighted estimates from 1995 to 2007. Simple linear regression (with assessment for correlated and heteroscedastic error terms) was then used to estimate the mean change in the prevalence of amphetamine abuse/dependence and incidence of aortic dissection, respectively, from year, with the null hypothesis stating that the population slope of the prevalence/incidence was equal to zero. The level of significance was set at α= 0.05 (two-tailed).
The annual prevalence of amphetamine abuse/dependence was calculated for patient discharges from 1995 to 2007. The incidence of aortic dissection was determined for patients aged 18 to 49 years. Post hoc, the incidence of aortic dissection was also determined for patients aged 50 years and older (49,206,331 discharges). This was done to determine whether the same secular trend observed in younger adults was also present among older adults.
Multiple Logistic Regression
Multiple logistic regression was used to estimate the odds of aortic dissection with an amphetamine abuse diagnosis while controlling for known risk factors. As a point of reference, the unadjusted odds ratios were also estimated for each risk factor and aortic dissection. The 95% Wald confidence intervals (CIs) were calculated, and the Wald Chi-square statistic was used to test for a significant association between each risk factor and aortic dissection. In a separate model, we also tested the interaction effect between amphetamine and cocaine abuse/dependence on aortic dissection, while controlling for the known risk factors.
The SURVEYLOGISTIC procedure in SAS 9.2 (SAS Institute, Cary, NC), with the STRATA and WEIGHT statements, was used to account for the NIS sampling methodology. The level of significance for all tests was set at α = 0.05 (2-tailed).
Population Attributable Risk
The multivariate population attributable risk percentage (PARP) of aortic dissection accounted for by amphetamine abuse/dependence and other significant risk factors from 1995 to 2007 was calculated from risk factor prevalences and adjusted odds ratios using a modified version of Bruzzi et al. (1985),20 that accounted for the NIS sampling methodology (sampling weights and stratification), using the Surveylogistic procedure in SAS 9.2.21 The PARP estimates the public health impact of individual risk factors in a given population under the causal assumption.
Funding and Authorship
This study was supported by NIH funding (CTSA Grant UL1 RR024982). The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
Results
Trends in Amphetamine Abuse/Dependence and Aortic Dissection
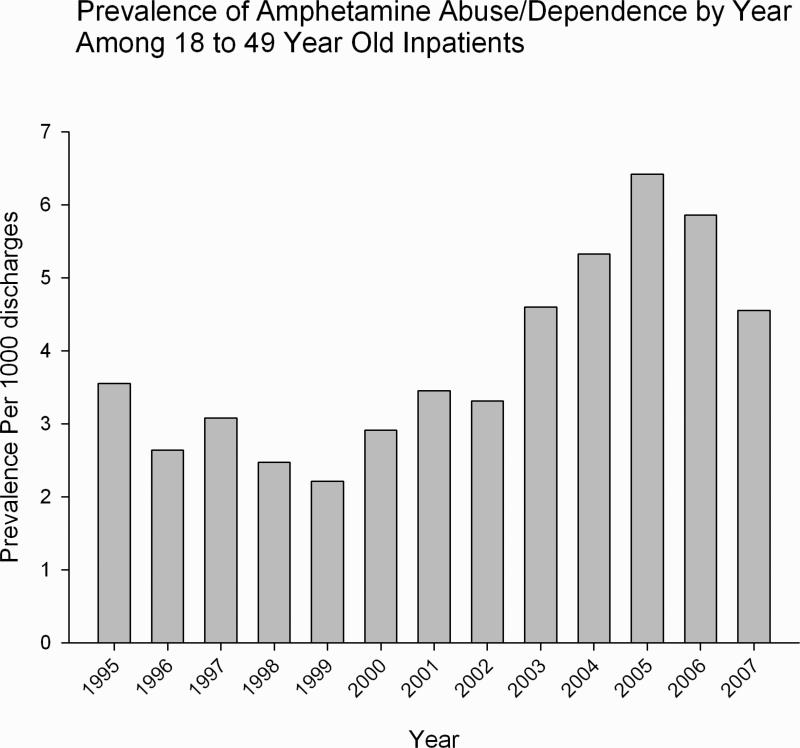
From 1995 to 2007, for patients aged 18-49 years in the NIS, prevalence of amphetamine abuse/dependence increased on average per 1,000 population (estimated slope = 0.27026, SE=0.06557, 95% CI = 0.12595 to 0.41458; t=4.12, p=0.0017; see Figure I).
Figure I.
Prevalence of Amphetamine Abuse/Dependence by Year Among Patients 18 to 49 Years of Age.
Footnote: in discharges of persons 18-49 years of age in Nationwide Inpatient Sample, 1995-2007.
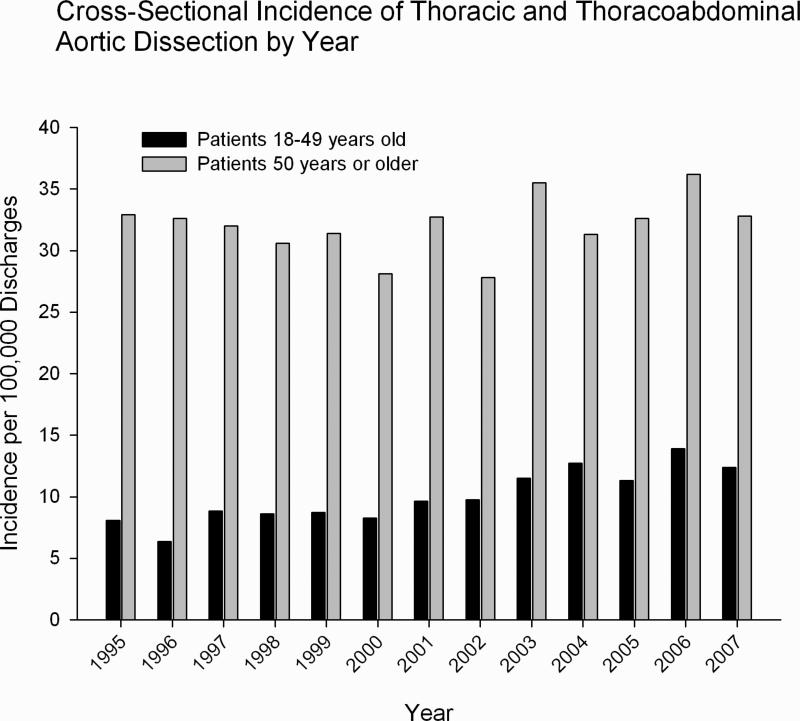
Among patients aged 18-49 years, incidence of aortic dissection was observed to increase on average from 1995 to 2007, with an estimated mean increase in aortic dissection of 0.51039 (SE=0.07029, 95% CI = 0.35568 to 0.66511) per 100,000 population per one year increase (t=7.26, p<0.0001; see Figure II). Among patients 50 years or older, however, no significant increase in aortic dissection incidence by year was observed (estimated slope = 0.16374, SE=0.17783, 95% CI = -0.22767 to 0.55514; t=0.92, p=0.3769; see Figure II).
Figure II.
Incidence of Thoracic and Thoracoabdominal Aortic Dissection Per Year.
Footnote: in discharges of persons 1) 18-49 years of age and 2) 50 years of age and over in Nationwide Inpatient Sample, 1995-2007.
Multiple logistic regression
In a multiple logistic regression model of inpatients aged 18-49 years in the NIS from 1995 to 2007, amphetamine abuse/dependence was significantly associated with aortic dissection (adjusted odds ratio = 3.33; 95% CI = 2.37—4.69, p<0.0001). The adjusted odds ratio for the association between amphetamine abuse and aortic dissection (adjusted OR = 3.33) was about twice as large as that for the association between cocaine abuse/dependence and aortic dissection (adjusted odds ratio = 1.60; 95% CI = 1.35—1.89, p<0.0001; Table II). The association between aortic dissection and amphetamine abuse/dependence became stronger after adjusting for other risk factors (unadjusted odds ratio = 2.89; 95% CI = 2.07—4.04). Increasing age was associated with a higher risk for aortic dissection (adjusted odds ratio = 1.06; 95% CI = 1.06—1.07, p<0.0001), as was hypertension (adjusted odds ratio = 7.68; 95% CI 7.05—8.37, p<0.0001). Marfan's Syndrome, in particular, was strongly associated with aortic dissection (adjusted odds ratio = 374.71; 95% CI = 324.88—432.17, p<0.0001). Finally, in a separate model we also tested the interaction effect between amphetamine and cocaine abuse/dependence on aortic dissection and found that the interaction was nonsignificant (Wald Chi-square=0.2997, p=0.5840).
Table II.
Multiple Logistic Regression Models for Aortic Dissection For Patients Aged 18 to 49 Years, 1995 to 2007
| Aortic Dissection (N=3,116) | |||||
|---|---|---|---|---|---|
| Risk Factor | Unadjusted OR* | 95 % CI for Unadjusted OR | Adjusted OR† | 95% CI for Adjusted OR | p for Adjusted OR |
| Amphetamine Abuse/Dep. | 2.89 | (2.07—4.04) | 3.33 | (2.37—4.69) | <.0001 |
| Cocaine Abuse/Dep. | 1.94 | (1.65—2.29) | 1.60 | (1.35—1.89) | <.0001 |
| Tobacco | 2.08 | (1.89—2.29) | 1.36 | (1.23—1.49) | <.0001 |
| Age | 1.11 | (1.10—1.11) | 1.06 | (1.06—1.07) | <.0001 |
| Lipid Disorder | 1.75 | (1.52—2.02) | 0.46 | (0.39— 0.53) | <.0001 |
| Hypertension | 11.64 | (10.82—12.52) | 7.68 | (7.05—8.37) | <.0001 |
| Marfan's Syndrome | 484.89 | (429.14—547.87) | 374.71 | (324.88—432.17) | <.0001 |
| Ehlers-Danlos Syndrome | 38.64 | (22.36—66.76) | 12.53 | (5.87—26.76) | <.0001 |
| Turner's Syndrome | 53.83 | (30.46—95.15) | 21.95 | (11.12—43.30) | <.0001 |
| Biscuspid Aortic Valve | 94.73 | (75.61—118.69) | 45.07 | (32.76—62.00) | <.0001 |
| Coarctation of the Aorta | 60.17 | (30.02—120.62) | 4.57 | (1.94—10.76) | 0.0005 |
| Giant Cell Arteritis | 17.46 | (2.46—124.01) | 6.48 | (0.90—46.64) | 0.0634 |
| Takayasu's Disease | 54.69 | (25.45—117.54) | 31.17 | (14.40—67.44) | <.0001 |
| Cardiovascular Syphilis | 190.54 | (27.08—>999.99) | 106.49 | (15.47—733.04) | <.0001 |
| Trauma (Motor Vehicle Traffic Accident) |
1.95 | (1.46—2.60) | 3.57 |
(2.67— 4.76) | <.0001 |
Unadjusted odds ratios were estimated for each risk factor and aortic dissection using PROC SURVEYLOGISTIC to account for NIS sampling methodolgy.
Adjusted odds ratios were estimated for each risk factor and aortic dissection, while controlling for the other risk factors, using PROC SURVEYLOGISTIC to account for NIS sampling methodology.
Population attributable risk
In the NIS from 1995 to 2007, amphetamine abuse/dependence accounted for 0.76% of all aortic dissections. Cocaine abuse/dependence accounted for 1.95%. In the Pacific Division (California, Hawaii, Oregon, Washington) from 1995 to 2007, amphetamine abuse/dependence accounted for three times more aortic dissections than nationally (2.31%). Cocaine abuse/dependence accounted for 3.71% of the aortic dissections in the Pacific Division.
Discussion
The current study examined the relationship between amphetamine abuse/dependence and aortic dissection in patients aged 18-49 years in the NIS from 1995 to 2007. These findings suggest a strong and significant association between amphetamine abuse/dependence and aortic dissection. The strength of the relationship was greater for amphetamines than for cocaine (and the interaction effect between amphetamine and cocaine abuse/dependence was not significant). In this 18-49 year old cross-sectional study population, the hospitalization rate for aortic dissection increased, whereas for patients aged 50 years and older the hospitalization rate did not increase.
Our basic finding is consistent with prior mechanistic evidence for a relationship between aortic dissection and amphetamine abuse/dependence. Hypertension is a known trigger of aortic dissection22 and amphetamines are known to increase blood pressure.23, 24 Thus, it has been suggested by Swalwell et al. that perhaps the hypertensive effect of amphetamines is a cause of aortic dissection.10 An experiment by Hirst et al. demonstrated that intravenous injection of epinephrine (structurally and mechanistically related to amphetamines) in rabbits indeed led to aortic dissection.25 Vasculitis has been associated with aortic dissection, and in experiments and studies,22 methamphetamine has been shown lead to vasculitis.26-30
Cocaine, which is mechanistically similar to amphetamines, is linked to aortic dissection. Amphetamines and cocaine have similar hemodynamic effects; they both increase arterial blood pressure and heart rate, which is mediated through adrenergic receptors.31 Hsue et al. have reported in a chart review of acute aortic dissection from 1981 to 2001, 37% (14/38) of cases were associated with cocaine use.32 Daniel et al. also did a chart review from 1990 to 2006 and found that of 163 cases of acute aortic dissection, 9.8% were associated with cocaine use in the 24 hours prior to symptom onset.33 Singh et al. found that of 46 consecutive patients admitted with acute aortic dissection, 28% (13) were related to cocaine use.34 Divakaran et al. have published a case report of cocaine-associated aortic dissection.35 Possible mechanisms include cocaine-induced relaxation of aortic rings36 as well as cocaine-induced apoptosis of rat aortic vascular smooth muscle cells.37
This study has limitations. The population-based case control study (cross-sectional) design cannot rule out the possibility that other risk factors, measured or unmeasured, besides amphetamine abuse/dependence could have influenced the risk of aortic dissection. We did, however, include the obvious risk factors known to investigators. Race and sex were not entered into the multiple logistic regression model because analyses from the International Registry of Acute Aortic Dissection demonstrated they are not risk factors for aortic dissection.15 This study is also limited by the nature of administrative data and ICD-9-CM diagnoses. To our knowledge, the sensitivity and specificity for ICD-9-CM codes for amphetamine and cocaine abuse/dependence have not been established. We have previously discussed the impact of this.21 Westover AN, McBride S, Haley RW. Stroke in young adults who abuse amphetamines or cocaine: a population-based study of hospitalized patients. Arch Gen Psychiatry. 2007;64:495-502. Additionally, the sensitivity and specificity for ICD-9-CM codes for thoracic and thoracoabdominal aortic dissections have not been established. However, studies have used these codes in analyses.38-40 Additionally, Saad et al., in a study of consecutive autopsy cases, found 75% concordance between clinical and autopsy diagnoses for aortic dissection.41 In this de-identified administrative database, it is not possible to determine whether aortic dissection diagnoses are independent of each other. However, only analyzing aortic dissection diagnoses that were the primary discharge diagnosis somewhat mitigates the concern of readmission of aortic dissections.
Despite these limitations, this study has strengths. The large sample size of the NIS database allows for the study of relatively rare conditions, such as aortic dissection, with sufficient statistical power to test our hypothesis. The NIS, due to its geographic breadth, augments the external validity (generalizability) derived from a national representative population. Finally, our analytic approach properly accounted for the NIS sampling methodology (sampling weights and stratification) in the test of our hypothesis.
Conclusions
To our knowledge, this is the first population-based epidemiologic study of hospital patients to examine the risk of aortic dissection with amphetamine abuse/dependence. The findings indicate a strong and significant association between amphetamine abuse and aortic dissection (even after adjustment for known risk factors) in young adults. This adds to our growing understanding of the cardiovascular risks associated with amphetamine abuse. Young adults presenting with acute aortic dissection should be screened for amphetamine use.
ACKNOWLEDGEMENT
The authors thank Samir Gupta, MD, for his comments and suggestions.
FUNDING SOURCES
Supported in part by NIH CTSA Grant UL1 RR024982.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURES
Dr. Westover and Dr. Nakonezny have no competing interests.
REFERENCES
- 1.United Nations Office on Drugs and Crime World Drug Report 2009. 2009 http://www.unodc.org/documents/wdr/WDR_2009/WDR2009_eng_web.pdf.
- 2.Substance Abuse and Mental Health Services Administration Results from the 2008 National Survey on Drug Use and Health: National Findings. Table G.3. 2009 http://www.oas.samhsa.gov/nsduh/2k8nsduh/2k8Results.pdf.
- 3.Office of Applied Studies, Substance Abuse and Mental Health Administration The NSDUH Report: Nonmedical Stimulant Use, Other Drug Use, Delinquent Behaviors, and Depression among Adolescents. 2008 http://oas.samhsa.gov/2k8/stimulants/depression.pdf.
- 4.Meszaros I, Morocz J, Szlavi J, et al. Epidemiology and Clinicopathology of Aortic Dissection. Chest. 2000;117(5):1271–1278. doi: 10.1378/chest.117.5.1271. [DOI] [PubMed] [Google Scholar]
- 5.Kamalakannan D, Rosman HS, Eagle KA. Acute Aortic Dissection. Critical Care Clinics. 2007;23(4):779–800. doi: 10.1016/j.ccc.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Januzzi JL, Isselbacher EM, Fattori R, et al. Characterizing the young patient with aortic dissection: results from the international registry of aortic dissection (IRAD). Journal of the American College of Cardiology. 2004;43(4):665–669. doi: 10.1016/j.jacc.2003.08.054. [DOI] [PubMed] [Google Scholar]
- 7.Davis GG, Swalwell CI. Acute aortic dissections and ruptured berry aneurysms associated with methamphetamine abuse. J Forensic Sci. 1994;39(6):1481–1485. [PubMed] [Google Scholar]
- 8.Kim MJ, Kim KS, Han SW, Han SB. A Case of Acute Dissection of the Aorta Associated with Methamphetamine Abuse. Journal of The Korean Society of Echocardiography. 1999;7(1):75–79. [Google Scholar]
- 9.Kaye S, McKetin R, Duflou J, et al. Methamphetamine and cardiovascular pathology: a review of the evidence. Addiction. 2007;102(8):1204–1211. doi: 10.1111/j.1360-0443.2007.01874.x. [DOI] [PubMed] [Google Scholar]
- 10.Swalwell CI, Davis GG. Methamphetamine as a risk factor for acute aortic dissection. J Forensic Sci. 1999;44(1):23–26. [PubMed] [Google Scholar]
- 11.Wako E, LeDoux D, Mitsumori L, et al. The Emerging Epidemic of Methamphetamine-Induced Aortic Dissections. Journal of Cardiac Surgery. 2007;22(5):390–393. doi: 10.1111/j.1540-8191.2007.00432.x. [DOI] [PubMed] [Google Scholar]
- 12.Dihmis WC, Ridley P, Dhasmana JP, et al. Acute dissection of the aorta with amphetamine misuse. BMJ. 1997;314(7095):1665. doi: 10.1136/bmj.314.7095.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duflou J, Mark A. Aortic dissection after ingestion of “ecstasy” (MDMA). Am J Forensic Med Pathol. 2000;21(3):261–263. doi: 10.1097/00000433-200009000-00016. [DOI] [PubMed] [Google Scholar]
- 14.McIntosh A, Hungs M, Kostanian V, et al. Carotid artery dissection and middle cerebral artery stroke following methamphetamine use. Neurology. 2006;67(12):2259–2260. doi: 10.1212/01.wnl.0000249180.61312.d3. [DOI] [PubMed] [Google Scholar]
- 15.Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): New Insights Into an Old Disease. JAMA. 2000;283(7):897–903. doi: 10.1001/jama.283.7.897. [DOI] [PubMed] [Google Scholar]
- 16.Nienaber CA, Eagle KA. Aortic dissection: new frontiers in diagnosis and management: Part I: from etiology to diagnostic strategies. Circulation. 2003;108(5):628–635. doi: 10.1161/01.CIR.0000087009.16755.E4. [DOI] [PubMed] [Google Scholar]
- 17.Lin AE, Lippe B, Rosenfeld RG. Further Delineation of Aortic Dilation, Dissection, and Rupture in Patients With Turner Syndrome. Pediatrics. 1998;102(1):e12. doi: 10.1542/peds.102.1.e12. [DOI] [PubMed] [Google Scholar]
- 18.HCUP Nationwide Inpatient Sample (NIS) Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality. 2009 http://www.hcup-us.ahrq.gov/nisoverview.jsp.
- 19.Overview of the Nationwide Inpatient Sample (NIS) HCUP Databases Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality. Rockville, MD: 2009. http://www.hcup-us.ahrq.gov/nisoverview.jsp. [Google Scholar]
- 20.Bruzzi P, Green SB, Byar DP, et al. Estimating the population attributable risk for multiple risk factors using case-control data. Am J Epidemiol. 1985;122(5):904–914. doi: 10.1093/oxfordjournals.aje.a114174. [DOI] [PubMed] [Google Scholar]
- 21.Westover AN, Nakonezny PA, Haley RW. Acute myocardial infarction in young adults who abuse amphetamines. Drug Alcohol Depend. 2008;96(1-2):49–56. doi: 10.1016/j.drugalcdep.2008.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong DR, Lemaire SA, Coselli JS. Managing dissections of the thoracic aorta. Am Surg. 2008;74(5):364–380. [PMC free article] [PubMed] [Google Scholar]
- 23.Wilens TE, Hammerness PG, Biederman J, et al. Blood pressure changes associated with medication treatment of adults with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2005;66(2):253–259. doi: 10.4088/jcp.v66n0215. [DOI] [PubMed] [Google Scholar]
- 24.Biederman J, Mick E, Surman C, et al. A randomized, placebo-controlled trial of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2006;59(9):829–835. doi: 10.1016/j.biopsych.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 25.Hirst AE, Jr., Johns VJ, Jr., Kime SW., Jr. Dissecting aneurysm of the aorta: a review of 505 cases. Medicine (Baltimore) 1958;37(3):217–279. doi: 10.1097/00005792-195809000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Bostwick DG. Amphetamine induced cerebral vasculitis. Hum Pathol. 1981;12(11):1031–1033. doi: 10.1016/s0046-8177(81)80262-6. [DOI] [PubMed] [Google Scholar]
- 27.Brust JC. Vasculitis owing to substance abuse. Neurol Clin. 1997;15(4):945–957. doi: 10.1016/s0733-8619(05)70357-1. [DOI] [PubMed] [Google Scholar]
- 28.Rumbaugh CL, Bergeron RT, Scanlan RL, et al. Cerebral vascular changes secondary to amphetamine abuse in the experimental animal. Radiology. 1971;101(2):345–351. doi: 10.1148/101.2.345. [DOI] [PubMed] [Google Scholar]
- 29.Rumbaugh CL, Bergeron RT, Fang HC, et al. Cerebral angiographic changes in the drug abuse patient. Radiology. 1971;101(2):335–344. doi: 10.1148/101.2.335. [DOI] [PubMed] [Google Scholar]
- 30.Rumbaugh CL, Fang HC, Higgins RE, et al. Cerebral microvascular injury in experimental drug abuse. Invest Radiol. 1976;11(4):282–294. doi: 10.1097/00004424-197607000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Johnson BA, Wells LT, Roache JD, et al. Isradipine Decreases the Hemodynamic Response of Cocaine and Methamphetamine: Results From Two Human Laboratory Studies. American Journal of Hypertension. 2005;18(6):813–822. doi: 10.1016/j.amjhyper.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 32.Hsue PY, Salinas CL, Bolger AF, et al. Acute Aortic Dissection Related to Crack Cocaine. Circulation. 2002;105(13):1592–1595. doi: 10.1161/01.cir.0000012524.44897.3a. [DOI] [PubMed] [Google Scholar]
- 33.Daniel JC, Huynh TT, Zhou W, et al. Acute aortic dissection associated with use of cocaine. J Vasc Surg. 2007;46(3):427–433. doi: 10.1016/j.jvs.2007.05.040. [DOI] [PubMed] [Google Scholar]
- 34.Singh S, Trivedi A, Adhikari T, et al. Cocaine-related acute aortic dissection: patient demographics and clinical outcomes. Can J Cardiol. 2007;23(14):1131–1134. doi: 10.1016/s0828-282x(07)70883-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Divakaran V, Mungee S, Salciccioli L, et al. Bedside ultrasound diagnosis of aortic dissection in a cocaine abuser. European Journal of Internal Medicine. 2007;18(8):595–596. doi: 10.1016/j.ejim.2007.02.022. [DOI] [PubMed] [Google Scholar]
- 36.Li W, Su J, Sehgal S, et al. Cocaine-induced relaxation of isolated rat aortic rings and mechanisms of action: possible relation to cocaine-induced aortic dissection and hypotension. Eur J Pharmacol. 2004;496(1-3):151–158. doi: 10.1016/j.ejphar.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 37.Su J, Li J, Li W, et al. Cocaine Induces Apoptosis in Primary Cultured Rat Aortic Vascular Smooth Muscle Cells: Possible Relationship to Aortic Dissection, Atherosclerosis, and Hypertension. International Journal of Toxicology. 2004;23(4):233–237. doi: 10.1080/10915810490471361. [DOI] [PubMed] [Google Scholar]
- 38.Knipp BS, Deeb GM, Prager RL, et al. A contemporary analysis of outcomes for operative repair of type A aortic dissection in the United States. Surgery. 2007;142(4):524–528. doi: 10.1016/j.surg.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 39.Cowan JA, Dimick JB, Henke PK, et al. Surgical treatment of intact thoracoabdominal aortic aneurysms in the United States: Hospital and surgeon volume-related outcomes. Journal of Vascular Surgery. 2003;37(6):1169–1174. doi: 10.1016/s0741-5214(03)00085-5. [DOI] [PubMed] [Google Scholar]
- 40.Rigberg DA, McGory ML, Zingmond DS, et al. Thirty-day mortality statistics underestimate the risk of repair of thoracoabdominal aortic aneurysms: A statewide experience. Journal of Vascular Surgery. 2006;43(2):217–222. doi: 10.1016/j.jvs.2005.10.070. [DOI] [PubMed] [Google Scholar]
- 41.Saad R, Yamada AT, Pereira da Rosa FHF, et al. Comparison between clinical and autopsy diagnoses in a cardiology hospital. Heart. 2007;93(11):1414–1419. doi: 10.1136/hrt.2006.103093. [DOI] [PMC free article] [PubMed] [Google Scholar]