Abstract
Objectives
Determine the impact of fecal incontinence (FI) in health care providers’ decisions to refer patients for nursing home (NH) placement.
Design
Survey of members of the American Geriatrics Society (AGS).
Measurements
The survey presented a clinical scenario of a 70-year-old woman ready for discharge from a hospital and asked their likelihood of making a NH referral if the patient had (a) no incontinence, (b) urinary incontinence (UI) alone, or (c) FI. Subsequent questions modified the clinical situation to include other conditions that might affect the decision to refer. A second survey of respondents to Survey 1 addressed possible moderators of the decision to refer (e.g., family caregiver presence, diarrhea or constipation, other physical or psychiatric limitations). Significance of differences in the relative risk (RR) for NH referral was tested by Chi square.
Results
716 members (24.7% response rate) completed the first survey and 686 of 716 (96%) completed the second. The likelihood of NH referral was increased by FI (RR=4.71, p<0.001) more than UI (RR=1.90, p<0.001). Mobility restrictions, cognitive decline, and multiple chronic illnesses increased the likelihood of NH referral more than FI alone (p<0.001 for each), but in all scenarios, adding FI further increased the likelihood of referral (p<0.001). Having family caregivers willing to help with toileting attenuated the likelihood of referral.
Conclusion
FI increases the probability that geriatricians will refer to a NH. More aggressive outpatient treatment of FI could possibly delay or prevent NH referral, improve quality of life, and reduce healthcare costs.
Keywords: Fecal Incontinence, Nursing Home referral, Hospital discharge, Physician survey, Caregiver, Urinary incontinence
INTRODUCTION
The prevalence of fecal incontinence (FI) is approximately 3-fold greater in nursing home (NH) residents (45%1 to 47%2) compared to the non-institutionalized population aged 70 or older (15%3). This has contributed to the belief that FI is a major risk factor for NH referral4, but there is little direct evidence to support this belief. Thom and colleagues5 reported that incontinence is a significant contributor to NH referral, but this study did not distinguish between FI and urinary incontinence (UI). Friedman et al6 reported that bowel incontinence was a significant predictor of NH referral among participants in the Program for All-inclusive Care of the Elderly (PACE), which is a community-based intensive program that enrolls only NH certifiable patients and is designed as an alternative to NH referral. Similarly, Tsuji and colleagues7 found FI to be a significant predictor of NH admission in the Johns Hopkins Elder House-call Program, another intensive community-based treatment program designed to keep patients out of NHs. Because these populations were highly specialized, we do not know how much impact FI has on NH admission in a representative sample of community residing elderly patients. This is an important question because institutionalization is acknowledged to be the greatest health care cost associated with continence care8, and because most elderly people try to avoid NH admission and believe it causes a major reduction in quality of life9. Moreover, FI is treatable; if it is confirmed to be a significant contributor to NH referral, it may be possible to delay or prevent NH admission through outpatient treatment of FI.
The aims of this study were (1) to determine the impact of FI, alone and in combination with other patient characteristics (cognitive impairment, mobility restrictions and presence of two or more chronic illnesses), in the health care provider’s decision to admit to a NH; (2) to compare FI to UI with respect to their impact on NH referral; and (3) to study the moderating influence of family social support, functional limitations, neuropsychiatric, and other chronic conditions on the relationship between FI and NH referral.
METHODS
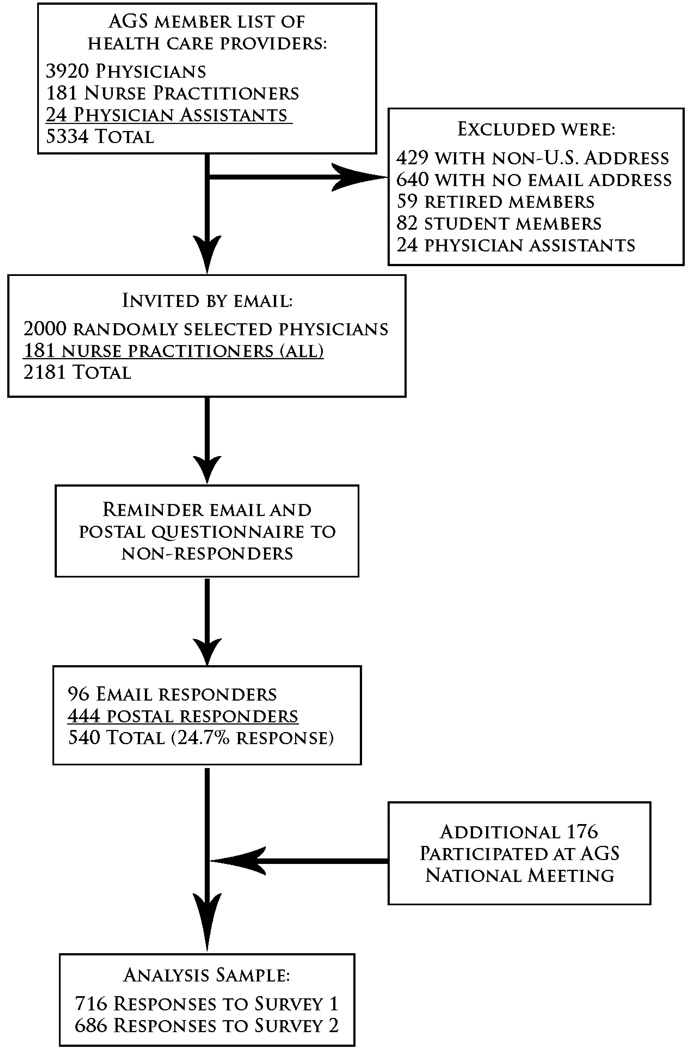
We surveyed a random sample of 2000 active, non-retired U.S. physicians and all 181 U.S. nurse practitioners from the American Geriatrics Society (AGS) membership list (Figure 1) because these health care providers are frequently involved in the decision to refer an elderly patient to a NH or skilled care facility. The invitation to participate in the survey was initially sent by e-mail, but participants were given the option to request a paper questionnaire instead of completing the on-line survey. A reminder e-mail was sent 2 weeks later. At the end of 4 weeks, non-responders were sent a postal survey. The 540 responses collected in this way (24.7% response rate) were supplemented by 176 surveys collected on-site at the annual AGS conference in 2008. (Duplicate surveys by the same individual were not permitted.) Ten dollars was offered for completing each of two surveys, and participants were given an opportunity to donate the money to the AGS. The cover letter accompanying the surveys also stated that answering the survey questions would be interpreted as consent to participate in the study and that their responses would be kept confidential. The study protocol was approved by the institutional review board of the University of North Carolina at Chapel Hill.
Figure 1.
Participation in the surveys. AGS is American Geriatrics Society.
Participants in Survey 1 were asked if they would complete a second, more detailed questionnaire (Survey 2) to explore additional factors in the decision to refer patients with FI to a NH. This second questionnaire was available either through e-mail or post. To maximize the response rate a “total design approach” was used10 which included personalized cover letters, first-class stamps on the envelopes, enclosed first-class stamped return envelopes, closed-ended questions, and a financial incentive for survey completion. The survey vignettes were pre-tested in a group of geriatric medicine fellows and faculty who were not allowed to participate in the final survey. A schematic of the study design is shown in Figure 1.
The questionnaire collected information on health care provider characteristics including provider type (physician, physician assistant, nurse practitioner), gender, age, type of practice (private practice solo, multi-specialty, hospitalist or academic), practice location (urban, semi-urban or rural), training (in-training or completed), and years in practice. Next, the survey presented providers with a clinical scenario. “A 70-year-old Caucasian female is hospitalized for community acquired pneumonia. She has a history of coronary artery disease and hypertension. She was living at her home prior to this admission. She has recovered well after 10 days stay and is now ready for discharge. Imagine yourself as the clinician in charge of this patient’s care and discharge process. What decision will you make regarding nursing home or skilled care facility referral under the following circumstances?” These circumstances were; (a) in the absence of incontinence, (b) with the addition of UI alone, and (c) with the addition of FI. Subsequent questions modified the clinical situation to include other conditions (cognitive decline, mobility restrictions and ≥2 medical co-morbidities) that might affect the decision to refer. The providers were asked to assume that they were in charge of the case and responsible for discharge decisions. The respondents were asked to rate the likelihood that they would refer the patients to a NH on a 5-point Likert scale (definitely not, probably not, uncertain, probably yes, definitely yes).
The purpose of the second questionnaire was to identify factors that might moderate the impact of FI on NH referral. This survey included questions on (1) bowel related factors such as severity of FI, bowel movement frequency, and fecal impaction; (2) family and social factors such as proximity to family and willingness of family members to assist with toileting, as well as past history of NH placement, and insurance coverage; (3) other chronic conditions such as poor nutritional status, and skin changes; (4) functional limitations such as stroke history with residual weakness and history of falls; and (5) neuropsychiatric conditions such as requiring physical restraints during hospitalization, history of psychiatric disorder, or use of sedatives/hypnotics.
For analysis, responses of “probably yes” and “definitely yes” were pooled and interpreted as “yes, provider would refer” while responses of “definitely not”, “probably not” and “uncertain” were pooled and interpreted as “no, provider unlikely to refer”. Chi square tests were used to compare the likelihood of referring in particular scenarios, and Relative Risk (RR) estimates with 95% confidence intervals were calculated. Statistical analyses employed SPSS version 15 software. A p-value <0.01 was considered statistically significant.
RESULTS
The enrollment of survey responders is shown in Figure 1. Overall, 540 of 2181 responded to the survey invitation (24.7% response rate). In combination with the responses obtained at the AGS meeting there were 716 responses to Survey 1, and 686 (95.8%) of those who completed Survey 1 also completed Survey 2. There was broad representation of providers across age groups, sex, years in practice, private vs. academic, and urban vs. rural and suburban practice settings (Table 1). Only 15% were trainees. Overall, 251 participants donated their honoraria to the AGS.
Table 1.
Characteristics of Responders (Survey 1)
| Provider Characteristic | Percent of Providers |
|---|---|
| Responses | |
| Survey 1 | 32.8 (n=716 of 2,181) |
| Survey 2 | 95.8 (n=686 of 716) |
| Age | |
| 25–35 | 20.7 |
| 36–45 | 26.8 |
| 46–55 | 27.8 |
| 56–65 | 18.7 |
| 66 or older | 6.1 |
| Sex | |
| Female | 52.4 |
| Male | 47.6 |
| Practice Setting | |
| Urban | 60.0 |
| Suburban | 29.3 |
| Rural | 10.7 |
| Practice Type | |
| Private practice solo | 11.6 |
| Multispecialty | 12.3 |
| Academic | 45.1 |
| Hospitalist | 4.7 |
| Other | 26.4 |
| Years in Practice | |
| 0–5 | 31.3 |
| 6–10 | 16.4 |
| 11–15 | 10.7 |
| 16–20 | 9.7 |
| >20 | 32.0 |
| Profession | |
| Physician | 85.6 |
| Physician Assistance | 3.1 |
| Nurse Practitioners | 11.3 |
| Trainee | |
| Yes | 15.5 |
| No | 84.5 |
The effects of urinary and fecal incontinence on the probability that geriatricians would refer to a NH are shown in Table 2. In the base case scenario, UI increased the probability of referring from 2.9% to 5.9% (p<0.001), and the addition of FI further increased the probability of referring to 14.6% (p<0.001). In Survey 2, we tested the effects of variations in FI severity: Having FI 1–2 times per month with small volumes was associated with a 6.7% likelihood of referral to a NH (lower than in the base case of unspecified FI), but this increased to 35.2% if FI occurred weekly and consisted occasionally of large volumes of stool lost (p<0.001).
Table 2.
Impact of Fecal Incontinence and Urinary Incontinence on Nursing Home Referral by Health Status
| Probability of Referral | Relative Risk of Referral | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| With vs. without UI | With vs. without FI | ||||||||
| Continent | UI only | FI | RR | CI | p | RR | CI | P | |
| Base case | 21 (2.9%) |
42 (5.9%) |
104 (14.6%) |
2.00 | 1.20– 3.34 |
0.005 | 4.95 | 3.13– 7.82 |
<0.001 |
| ≥2 chronic illnesses |
95 (13.3%) |
151 (21.2%) |
223 (31.3%) |
1.59 | 1.26– 2.01 |
<0.001 | 2.35 | 1.89– 2.92 |
<0.001 |
| Cognitively impaired |
247 (34.6%) |
300 (42.0%) |
367 (51.5%) |
1.21 | 1.06– 1.39 |
0.002 | 1.49 | 1.31– 1.68 |
<0.001 |
| Mobility impaired |
411 (57.6%) |
482 (67.6%) |
528 (74.1%) |
1.17 | 1.08– 1.27 |
<0.001 | 1.28 | 1.19– 1.38 |
<0.001 |
UI=Urinary Incontinence; FI=Fecal Incontinence
Cognitive impairment, mobility impairment, and having multiple chronic illnesses were stronger risk factors than UI or FI (Table 2), but in each clinical scenario, the presence of UI and FI significantly increased the likelihood of NH referral. In all scenarios, FI had a greater impact on referral to a NH than did UI.
Survey 2 investigated moderators of the effect of FI on NH referral. The base case clinical scenario for this survey included FI of unspecified severity for the past 2 years, and this was associated with a 10.4% likelihood of referral. If the patient did not have a family member living nearby, the probability of referring to a NH increased to 54.0% (RR=5.19, p<0.001), and if the caregiver was unwilling to help, the probability of referring was 80.2% (RR=7.71, p<0.001). Patients with a prior NH admission were more likely to be referred (28.3%, RR=2.72, p<0.001). Patients with inadequate insurance coverage were also more likely to be referred (26.3%, RR=2.53, p<0.001). As shown in Table 3, additional moderating factors that increased the probability of referral to a NH were frequent bowel movements, history of fecal impaction, presence of other chronic illnesses, neuropsychiatric disorders, and functional limitations.
Table 3.
Additional Factors Moderating the Impact of Fecal Incontinence on Nursing Home Referral
| Probability of Referral (%) |
RR | C.I. | p-value | |
|---|---|---|---|---|
| Bowel habits: | ||||
| Base case: unspecified FI | 10.4 | |||
| Severe FI: Weekly, consisted occasionally of large volumes of stool |
35.2 | 3.32 | 2.56–4.01 | <0.001 |
| Diarrhea: frequent loose or watery stools | 32.2 | 3.11 | 2.43–3.97 | <0.001 |
| Fecal impaction: frequent occurrence | 50.2 | 4.84 | 3.84–6.11 | <0.001 |
| Other chronic conditions: | ||||
| Base case: unspecified FI | 10.4 | |||
| Poor nutritional status | 74.7 | 7.21 | 5.76–9.03 | <0.001 |
| Decubitus ulceration | 74.2 | 7.16 | 5.72–8.96 | <0.001 |
| Functional limitations: | ||||
| Base case: unspecified FI | 10.4 | |||
| History of stroke with residual weakness | 52.2 | 5.04 | 4.00–6.35 | <0.001 |
| Fell during hospitalization | 20.2 | 1.95 | 1.50–2.54 | <0.001 |
| History of falls at home | 58.9 | 5.68 | 4.52–7.15 | <0.001 |
| Neuropsychiatric disorders: | ||||
| Base case: unspecified FI | 10.4 | |||
| History of any psychiatric illness | 29.8 | 2.88 | 2.25–3.67 | <0.001 |
| Required physical restraints in hospital | 35.8 | 3.46 | 2.71–4.40 | <0.001 |
| On psychotropic drugs | 19.6 | 1.89 | 1.45–2.47 | <0.001 |
DISCUSSION
This is the first study to demonstrate that FI has a significant, independent impact on the probability that geriatricians will refer elderly patients to a NH. Previous studies have shown that unspecified incontinence is a risk factor for referral to a NH5,11, but these studies did not distinguish the contribution of FI from that of UI. By using clinical scenarios to isolate the factors influencing the decision to refer, we were able to show that FI has a significantly greater impact on the probability of referring than does UI. Severe FI, frequent bowel movements, and history of fecal impaction added further to the probability of referring to a NH. Fecal impaction and diarrhea are treatable conditions, and good medical practice would involve a trial of treatment prior to referring to a NH. Our survey did not allow providers to communicate whether they would attempt to treat fecal impaction or diarrhea medically before referring to a NH.
Two prior studies6,7 have reported that FI has a significant impact on the decision to refer to a NH, but both of these studies were carried out in highly specialized clinical settings where all the participants were NH-certifiable and where the clinical objective was to keep patients out of NHs by offering an intensive outpatient treatment program. We were unable to find studies that assessed the separate impact of FI on NH referral in more typical community-dwelling elderly people.
Some previous authors4 have speculated that FI is second only to dementia as a reason for referring patients to a NH. Our study shows that mobility impairment and multiple chronic illnesses as well as dementia are greater risk factors for NH referral than FI. However, FI is a significant risk factor by itself that is associated with a 10% to 15% likelihood of referral, and it adds approximately 17% to the probability of referring to a NH when these other risk factors are present (Table 2). Thus, it is reasonable to expect that early diagnosis and treatment of FI in the community could reduce or delay NH admissions; this deserves further study.
We observed that the decision to refer an elderly patient to a NH is strongly influenced by whether there are family caregivers in the home or living nearby and whether these caregivers are willing to provide assistance with toileting. This underscores the importance of caregivers in the outpatient treatment of FI. Currently most behavioral treatments for FI rely on training the identified patient and do not involve family caregivers. Our findings suggest that outcomes might be improved by including family caregivers in designing and carrying out treatment plans.
This study has limitations: We assessed geriatricians’ responses to hypothetical clinical scenarios rather than their actual behaviors. While this approach has advantages for isolating variables that may influence decision making, it is subject to bias related to the perception that some responses may be more socially desirable than others. A second limitation is that the survey did not state clearly that referral was for long term care rather than short term rehabilitation. Because our question asked about referral to a “nursing home or skilled care facility” which usually implies a long term care facility, and because rehabilitation services do not normally include incontinence training, we assumed respondents would infer that they were being asked about referral for long term care. However, this ambiguity may have confused some respondents. A third limitation is the relatively low participation rate, which allows for possible bias due to self-selection. Low participation rates are common in physician surveys12. Because of these limitations, our conclusions regarding the importance of FI in the decision to refer to a NH require confirmation.
In conclusion, this survey shows that FI has a significant impact on the decision to refer an elderly patient to a NH. FI is treatable in frail elderly patients13–15. Especially, triggers such as diarrhea and fecal impaction can certainly be therapeutically targeted16,17. More aggressive screening and treatment of FI could potentially prevent or delay NH referral, thereby improving patients’ quality of life and reducing health care costs. There is a need for investigations to understand factors important in NH referral and trials of interventions to reduce nursing home referral.
ACKNOWLEDGMENTS
Supported by grant R24 DK067674 from the National Institutes of Diabetes and Digestive and Kidney Diseases, and an Investments for the Future award from the University of North Carolina at Chapel Hill School of Medicine. The American Geriatrics Society provided access to its membership list, without which this survey could not have been done.
Footnotes
Presentations: Abstracts of this work were presented at the 2009 Annual meeting of the American Geriatrics Society in Chicago, April 29–May 2, 2009 and at Digestive Disease Week in Chicago May 29–June 2, 2009.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Authors Contribution:
Madhusudan Grover: study concept and design, analysis and interpretation of data, and preparation of manuscript.
Jan Busby-Whitehead: study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, and preparation of manuscript.
Mary H. Palmer: study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, and preparation of manuscript.
Steve Heymen: study concept and preparation of manuscript.
Olafur S. Palsson: study concept and design, acquisition of subjects and/or data, analysis and interpretation of data.
Patricia S. Goode: study concept and design, analysis and interpretation of data, and preparation of manuscript.
Marsha Turner: study concept and design, acquisition of subjects and/or data
William E. Whitehead: study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, and preparation of manuscript.
Sponsor’s Role: None
REFERENCES
- 1.Dey AN. Characteristics of elderly nursing home residents: Data from the 1995 National Nursing Home Survey. Advance data from vital and health statistics; no. 289. 1997. Hyattsville, Maryland: National Center for Health Statistics; 1997. [PubMed] [Google Scholar]
- 2.Nelson R, Furner S, Jesudason V. Fecal incontinence in Wisconsin nursing homes: prevalence and associations. Dis Colon Rectum. 1998;41:1226–1229. doi: 10.1007/BF02258218. [DOI] [PubMed] [Google Scholar]
- 3.Whitehead WE, Borrud L, Goode PS, et al. Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology. 2009;137:512–517. doi: 10.1053/j.gastro.2009.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheskin LJ, Schuster MM. Fecal incontinence. In: Hazzard WR, Andres R, Bierman EL, Blass JP, editors. Principles of Geriatric Medicine and Gerontology. 2nd ed. New York: McGraw Hill; 1990. pp. 1143–1145. [Google Scholar]
- 5.Thom DH, Haan MN, Van Den Eeden SK. Medically recognized urinary incontinence and risks of hospitalization, nursing home admission and mortality. Age Ageing. 1997;26:367–374. doi: 10.1093/ageing/26.5.367. [DOI] [PubMed] [Google Scholar]
- 6.Friedman SM, Steinwachs DM, Rathouz PJ, et al. Characteristics predicting nursing home admission in the program of all-inclusive care for elderly people. Gerontologist. 2005;45:157–166. doi: 10.1093/geront/45.2.157. [DOI] [PubMed] [Google Scholar]
- 7.Tsuji I, Whalen S, Finucane TE. Predictors of nursing home placement in community-based long-term care. J Am Geriatr Soc. 1995;43:761–766. doi: 10.1111/j.1532-5415.1995.tb07046.x. [DOI] [PubMed] [Google Scholar]
- 8.Borrie MJ, Davidson HA. Incontinence in institutions: costs and contributing factors. CMAJ. 1992;147:322–328. [PMC free article] [PubMed] [Google Scholar]
- 9.Krothe JS. Giving voice to elderly people: community-based long-term care. Public Health Nurs. 1997;14:217–226. doi: 10.1111/j.1525-1446.1997.tb00294.x. [DOI] [PubMed] [Google Scholar]
- 10.Field TS, Cadoret CA, Brown ML, et al. Surveying physicians: do components of the "Total Design Approach" to optimizing survey response rates apply to physicians? Med Care. 2002;40:596–605. doi: 10.1097/00005650-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Anpalahan M, Gibson SJ. Geriatric syndromes as predictors of adverse outcomes of hospitalization. Intern Med J. 2008;38:16–23. doi: 10.1111/j.1445-5994.2007.01398.x. [DOI] [PubMed] [Google Scholar]
- 12.Field TS, Cadoret CA, Brown ML, et al. Surveying physicians: do components of the "Total Design Approach" to optimizing survey response rates apply to physicians? Med Care. 2002;40:596–605. doi: 10.1097/00005650-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Whitehead WE, Wald A, Norton NJ. Treatment options for fecal incontinence. Dis Colon Rectum. 2001;44:131–142. doi: 10.1007/BF02234835. [DOI] [PubMed] [Google Scholar]
- 14.Norton C, Chelvanayagam S, Wilson-Barnett J, et al. Randomized controlled trial of biofeedback for fecal incontinence. Gastroenterology. 2003;125:1320–1329. doi: 10.1016/j.gastro.2003.09.039. [DOI] [PubMed] [Google Scholar]
- 15.Heymen S, Scarlett Y, Jones K, et al. Randomized controlled trial shows biofeedback to be superior to pelvic floor exercises for fecal incontinence. Dis Colon Rectum. 2009;52:1730–1737. doi: 10.1007/DCR.0b013e3181b55455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harford WV, Krejs GJ, Santa Ana CA, et al. Acute effect of diphenoxylate with atropine (Lomotil) in patients with chronic diarrhea and fecal incontinence. Gastroenterology. 1980;78:440–443. [PubMed] [Google Scholar]
- 17.Remes-Troche JM, Ozturk R, Philips C, et al. Cholestyramine--a useful adjunct for the treatment of patients with fecal incontinence. Int J Colorectal Dis. 2008;23:189–194. doi: 10.1007/s00384-007-0391-y. [DOI] [PubMed] [Google Scholar]